Abstract
The pancreas is comprised of exocrine and endocrine components. Despite the fact that they are derived from a common origin in utero, these two compartments are often studied individually because of the different roles and functions of the exocrine and endocrine pancreas. Recent studies have shown that not only type 1 diabetes (T1D), but also type 2 diabetes (T2D), is characterized by a deficit in beta-cell mass, suggesting that pathological changes in the pancreas are critical events in the natural history of diabetes. In both patients with T1D and those with T2D, pancreas mass and exocrine function have been reported to be reduced. On the other hand, pancreas volume and pancreatic fat increase with obesity. Increased beta-cell mass with increasing obesity has also been observed in humans, and ectopic fat deposits in the pancreas have been reported to cause beta-cell dysfunction. Moreover, neogenesis and transdifferentiation from the exocrine to the endocrine compartment in the postnatal period are regarded as a source of newly formed beta-cells. These findings suggest that there is important interplay between the endocrine and exocrine pancreas throughout life. This review summarizes the current knowledge on physiological and pathological changes in the exocrine and endocrine pancreas (i.e., beta-cell mass), and discusses the potential mechanisms of the interplay between the two compartments in humans to understand the pathophysiology of diabetes better.
Keywords: diabetes, endocrine pancreas, exocrine pancreas, interplay, beta-cell mass, pancreatic fat, aging, obesity
Abbreviations: BCM - beta-cell mass; BMI - body mass index; CCK - cholecystokinin; CT - computed tomography; DPP-4 - dipeptidyl peptidase-4; DM - diabetes mellitus; ER - endoplasmic reticulum; FDA - Food and Drug Administration; FFA - free fatty acids; F/P - fat/parenchymal; GI - gastrointestinal; GIP - glucose-dependent insulinotrophic polypeptide; GLP-1 - glucagon-like peptide 1; GLP-1RA - GLP-1 receptor agonist; HbA1c - glycated hemoglobin; HOMA-IR - homeostasis model assessment of insulin resistance; HOMA-β - homeostatis model assessment of beta-cell function; IFG - impaired fasting glucose; IGT - impaired glucose tolerance; MRI - magnetic resonance imaging; MRS - magnetic resonance spectrometry; NDM - non-diabetes mellitus; NGT - normal glucose tolerance; OGTT - oral glucose tolerance test; PACAP - pituitary adenylate cyclase activating polypeptide; PDX1 - pancreatic and duodenal homeobox factor 1; PET - positron emission tomography; PP - pancreatic polypeptide; T1D - type 1 diabetes; T2D - type 2 diabetes; TNF - tumor necrosis factor
1. Introduction
The pancreas comprises the exocrine and endocrine compartment, with most of the pancreatic mass included in the former. The exocrine pancreas contains acinar cells that secrete digestive fluid and a duct system through which the fluid drains into the intestine. The endocrine compartment includes the islets of Langerhans, which are scattered throughout the exocrine pancreas, and which comprise only 1-2% of the pancreas. The endocrine pancreas secretes various hormones such as insulin, glucagon, and somatostatin, and plays a key role in glucose metabolism. Because of the different roles and functions of the endocrine and exocrine pancreas, these two components have usually been studied separately. While diabetes can occur because of pancreatic disease such as pancreatitis or pancreatic cancer [1], recent studies have shown that type 1 diabetes (T1D) and type 2 diabetes (T2D) are characterized by a deficit in beta-cells, an endocrine cell that secretes insulin [2-5], suggesting that pathological changes in the pancreas are critical for the natural history of the disease.
Given that endocrine and exocrine pancreas are derived from the same origin in utero, neogenesis and transdifferentiation from the exocrine to the endocrine compartment in the postnatal period have been reported in animal studies [6-10], suggesting that there is continuous interplay between the endocrine and exocrine pancreas throughout life. Therefore, it is important to assess the endocrine and exocrine compartments simultaneously to understand the disease better. This review summarizes recent knowledge regarding physiological and pathological changes in the exocrine and endocrine pancreas in humans, and discusses the interplay between these two compartments of the pancreas.
2. Development of exocrine and endocrine pancreas
During human embryonic development, dorsal and ventral pancreatic buds arise from the distal foregut endoderm around 30 days post-conception (embryonic day (e) 9-9.5 in mice); this event coincides with the first detection of a key transcription factor for pancreatogenesis, pancreatic and duodenal homeobox factor 1 (Pdx1) [11, 12]. The ventral bud then rotates around the gut and merges with the dorsal bud into a single organ (e12.5 in mice). Around 50 days post-conception (e15-15.5 in mice), endocrine progenitor cells expressing neurogenin 3 (Ngn3), a transcription factor required for endocrine cell development, are firstly detected in the duct wall (trunk epithelium). Ngn3 upregulation results in separation of endocrine cells from the duct lineage. During this period, the pancreatic epithelium continues to expand and branch into a highly ordered tubular network.
These morphologic changes are paralleled by the differentiation of endocrine, acinar, and ductal cells, all of which are derived from a common origin from progenitor cells in the gut endoderm. Endocrine cells arise from Ngn3-expressing progenitor cells, and the transcription factors Pax4, Pdx1, and Nkx6.1 act as critical beta-cell determinants, whereas Arx determines alpha-cell identity. Endocrine cells become separated from the duct, and cluster to form aggregates, eventually maturing into islets of Langerhans. Beta-cell clusters are well vascularized by 10 weeks post-conception. At 12-13 weeks post-conception, islets containing each type of endocrine cell are apparent. Endocrine cells other than beta- and alpha-cells include delta-cells, pancreatic polypeptide (PP) cells and epsilon-cells, which secrete somatostatin, PP, and ghrelin, respectively. Ngn3 expression is transient, peaking around the end of the first trimester, and is not detected in human fetuses after 35 weeks post-conception. On the other hand, Pdx1 is exclusively expressed by beta-cells in the postnatal period. Finally, beta-cells comprise about 60-80% of endocrine cells in each islet, with the exception of the ventral portion of the pancreatic head, in which PP cells are the major component of the endocrine cells [3, 5].
3. Physiological and pathological changes in exocrine pancreas mass
3.1 Growth in childhood and changes with aging
Pancreas mass is measured anatomically at autopsy or by the use of imaging techniques such as ultrasonography, computed tomography (CT), or magnetic resonance imaging (MRI). Of note, pancreas volume measured using CT or MRI is generally smaller (~70 ml) than that measured anatomically (~100 g) [13]. This difference may result from the fact that the pancreas is made up of retroperitoneal tissue surrounded by fat tissue. Thus, resected pancreas contains interlobular fat, resulting in a greater mass of pancreas compared with that measured by CT or MRI imaging.
Pancreas mass is approximately 10 g at birth, and then increases linearly with age in childhood and adolescence [13] (Figure 1). Pancreas mass reaches a plateau around 20 years of age, at approximately 70 g [13], and then declines in the elderly, from about 60 years of age [13]. The pancreas of older subjects is characterized by atrophy of acinar cells, fibrosis, and fat infiltration in the exocrine pancreas [14]. Thus, parenchymal pancreas mass estimated by CT density, which presumably consists of acinar and duct compartments, but not fat tissue, declines, and the ratio of fat to parenchymal pancreas increases in the elderly [13] (Figure 2). A recent study showed that the ratio of pancreas weight to body weight is constant across a wide range of ages and BMIs [15]. This finding is useful to assess the impact of diabetes on pancreas/beta-cell mass in a mixed population (with varying ages and BMI values) since pancreas mass and volume is reduced in patients with (longstanding and recently diagnosed) T1D compared to that of non-diabetic controls [16, 17]. However, since the portions of parenchyma and fat change with aging and degree of obesity, as described above, pancreas mass and single components of the pancreas should be taken into account when investigating diabetes pathogenesis [18].
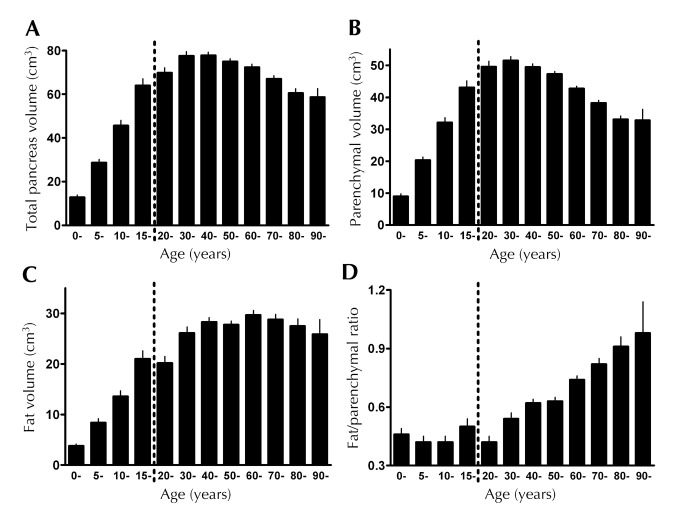
Figure 1. Age-related distribution of pancreas volume and fat volume over time.
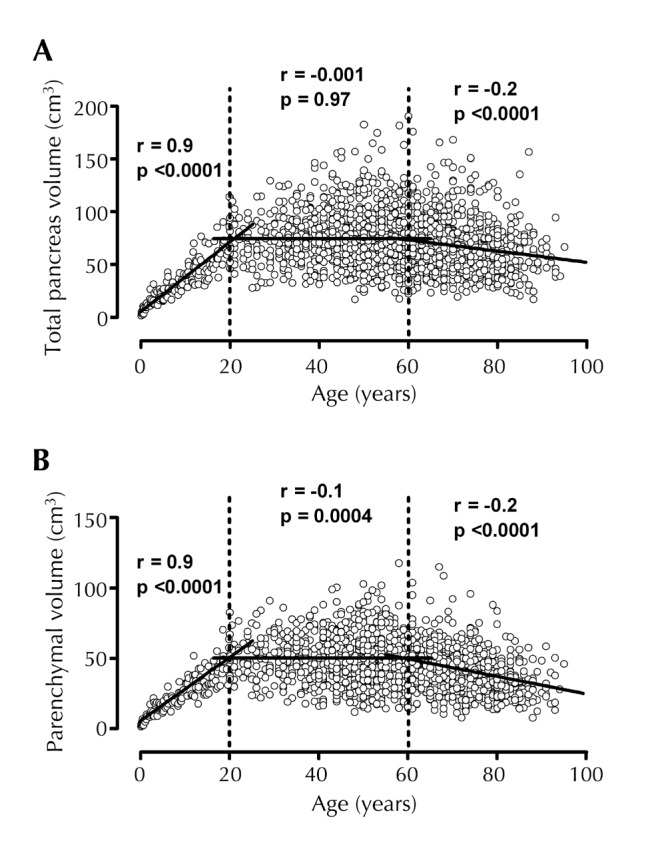
Total (A) and parenchymal (B) pancreas volume from birth to age 100 years measured on the basis of CT scan images (n = 1,856) showed a strong correlation between age and total as well as parenchymal pancreas volume from birth to age 20 years (y (volume; cm3) = 5.5 + 3.31x (age; years) and y = 4.3 + 2.25x, respectively). There is a negative correlation between age and total as well as parenchymal volume after age 60 years (y = 106.0 - 0.53x and y = 71.7 - 0.45x, respectively). There is no significant correlation between age and total pancreas volume between age 20 and 60 years. Reproduced with permission from the authors of reference [13]
Figure 2. Total, parenchymal, and pancreatic fat volumes in each age decile.
A: total pancreas volume, B: parenchymal volume, C: fat volume, D: fat/parenchyma (F/P) ratio. The total pancreas volume increases with age until ~30 years, and then reaches a plateau. After age 60, total pancreas volume declines due to a decrease in parenchymal pancreas volume. Pancreatic fat remains proportional to pancreas parenchyma volume until the age of ~50 years, after which the F/P ratio increases because of the loss of pancreas parenchyma, while the pancreatic fat amount remains constant. Reproduced with permission from the authors of reference [13].
3.2 Effects of obesity and diabetes on pancreas mass
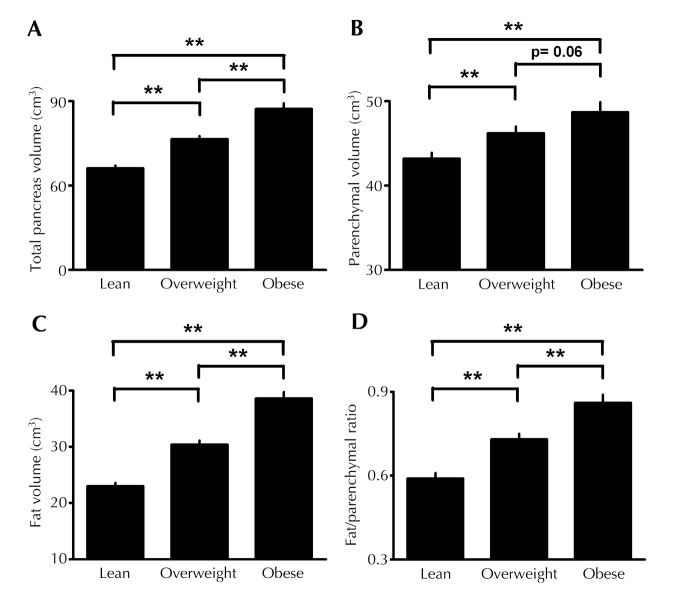
Pancreas mass increases with obesity [13]. The pancreas of obese subjects is mainly characterized by fat infiltration within exocrine pancreas and interlobular spaces [14]. However, the acinar component also increases with obesity. An analysis of CT images showed that parenchymal pancreas mass increases by about 10-15% in the presence of obesity, whereas pancreatic fat mass increases by ~70%, resulting in ~30% increase in total pancreas mass with obesity [13] (Figure 3), which is comparable among different ethnic groups [19, 20].
Figure 3. Effects of obesity on pancreatic volumes.
Total pancreas volume (A), parenchymal volume (B), fat volume (C) and fat/parenchymal (F/P) ratio (D) were measured on the basis of CT scan images in lean (n = 230), overweight (n = 460), and obese individuals (n = 230). All components of the pancreatic volume were significantly increased in overweight and obese subjects compared to lean subjects. ** p < 0.01. Reproduced with permission from the authors of reference [13].
Pancreas mass is decreased by 30-40% in subjects with T1D [15-17]. Histological analysis showed atrophy of acinar cells in the pancreas [21-23] and impaired exocrine function in patients with T1D [24-26]. Pancreas mass is also decreased in subjects with T2D compared to age- and BMI-matched controls. However, the degree of reduction is smaller (8-20%) than that observed in subjects with T1D [13, 27] (Table 1). Impaired exocrine function in patients with T2D has also been reported [25, 26], but to a lesser degree than in patients with T1D, similarly to pancreas mass. Philippe et al. reported that pancreas volume is correlated with chymotrypsin activity and stimulated C-peptide level in patients with diabetes, suggesting a close correlation between exocrine and endocrine pancreas [28]. Together, these studies suggest that both T1D and T2D lead to a reduction in pancreas mass and exocrine cell function. The potential mechanisms are discussed in more detail below.
Table 1. Comparison of pancreas volume measured on the basis of CT scan images between humans with type 2 diabetes and age-, sex-, and BMI-matched controls.
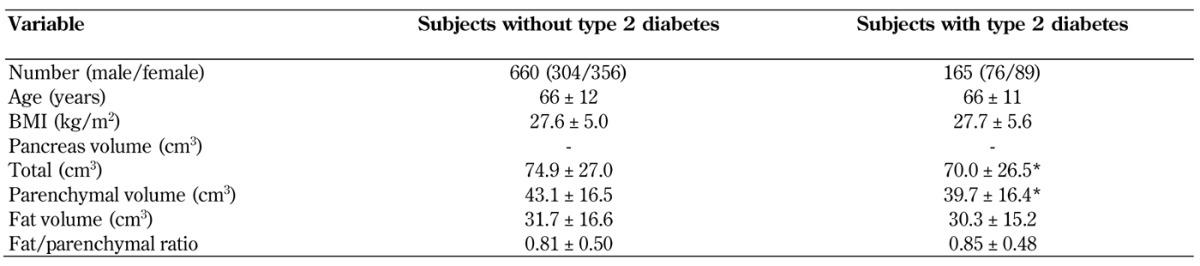
Legend: Values are presented as mean ± SD. * p < 0.05 vs. subjects without type 2 diabetes. Abbreviations: BMI - body mass index, CT - computed tomography. Reproduced with permission from the authors of reference [13].
4. Relationship between pancreas mass and beta-cell mass and their pathophysiological changes
Since it is impossible to measure human beta-cell mass (BCM) in vivo, BCM is estimated to be the product of beta-cell area in relation to pancreas area measured by histological analysis (i.e., fractional beta-cell area) and pancreas mass. BCM at birth is approximately 0.1 g, and increases gradually with age in childhood and adolescence [29], reaching a plateau at around the age of 20 at approximately 1 g [14]. In adulthood, BCM remains constant. In the elderly, islet architecture is relatively well preserved and BCM remains stable [14], or is only slightly reduced [3, 30]. This is in contrast to the marked decline in exocrine pancreas mass, which is due to acinar atrophy and fibrotic changes. Since insulin sensitivity decreases with aging, the lack of compensatory BCM with aging may result in worsening glucose tolerance in the elderly [31]. However, recent studies have suggested that beta-cell function increases with aging through age-dependent epigenetic modulation [32] or p16Ink4a-induced senescence of beta-cells [33], which may contribute to compensatory changes in beta-cell function to preserve normoglycemia with aging. Further studies are needed to clarify the change in "functional" BCM with aging in humans.
In subjects with T1D, most of the beta-cells are destroyed via autoimmune reaction, and BCM eventually decreases to nearly, but usually not absolute, zero [21-23]. Studies have shown that BCM is also decreased in subjects with T2D by 30-60% compared to that in non-diabetic subjects [2-5]. Changes in other endocrine cells are less clear. Both increase and decrease in alpha-cell mass in subjects with T2D have been reported [34-38]. Taken together, these findings indicate that both endocrine and exocrine mass decrease with the natural course of diabetes.
Since BCM is estimated as a product of fractional beta-cell area and pancreas mass, pancreas mass should always be considered when findings of histological analysis are interpreted. For example, fractional beta-cell area has been reported to be decreased by 40-65% in patients with T2D [2]. If pancreas mass were increased, BCM might not be reduced in these patients. However, since pancreas mass is decreased usually in patients with T2D, BCM is confirmed to be decreased to an even greater degree in these patients.
In the presence of obesity, fractional beta-cell area is increased by ~30% [14]. Since pancreatic parenchymal mass is increased by ~15% [13], the estimated BCM is thus assumed to be increased by 50% in the presence of obesity [14]. Of note, we have observed that fractional beta-cell area tends to be increased in older subjects [14]. However, given that pancreatic parenchymal mass is decreased in older subjects, we concluded that net BCM was not increased in these subjects [14]. Thus, understanding the physiological and pathological changes in pancreas mass is important for the determination of BCM.
The change in BCM during the development of T2D remains largely unknown. Obesity is an established risk factor for T2D [39-41]. It results from excess energy intake and physical inactivity, and decreases insulin sensitivity. To maintain normoglycemia, insulin secretion increases with obesity. We and others have shown that, in humans, BCM increases by 20-50% with obesity in the Caucasian population [4, 14], while there is little increase in BCM in the Japanese population [30, 38, 42]. Considering that insulin secretion is increased 2- to 3-fold with obesity [43], the compensatory increase in insulin secretion appears mainly attributable to an increase in insulin secretion per individual beta-cell, resulting in increased workload of beta-cells. Excess beta-cell workload may eventually result in beta-cell damage through various mechanisms such as oxidative stress, endoplasmic reticulum (ER) stress, and amyloid deposition in individuals susceptible to T2D, which may cause beta-cell apoptosis and reduction in BCM even in the absence of hyperglycemia [44]. Indeed, a reduction in BCM in patients with prediabetes has been reported [2, 45, 46], and a significant correlation between glycated hemoglobin (HbA1c) and BCM was observed in both patients with diabetes and those without diabetes [47]. If the reduction in BCM and beta-cell function has started, the "functional BCM" can no longer compensate for insulin resistance, causing hyperglycemia to develop. Hyperglycemia further contributes to beta-cell damage by so-called glucotoxicity, and functional BCM further decreases, contributing to the progressive nature of T2D. An inverse association between BCM and duration of T2D has also been reported, consistent with the progressive loss of beta-cell function during T2D progression [4].
Since both T1D and T2D are characterized by a deficit in beta-cells, fostering beta-cell regeneration is the key to curing both types of diabetes. However, the source of new beta-cells in the postnatal period remains unclear [44, 48]. BCM is regulated by the balance of newly formed beta-cells and beta-cell loss. Beta-cell replication and neogenesis are considered to be sources of newly-formed beta-cells, while beta-cell apoptosis is considered a major cause of beta-cell loss [2, 49]. A recent rodent study has suggested beta-cell dedifferentiation to be another mechanism of beta-cell loss in diabetes [50]. In the postnatal period, beta-cell replication is frequently seen within the first five years of life [29, 51], but it is rarely seen thereafter in humans [14, 38]. Based on the finding that endocrine and exocrine pancreas have a common origin during pancreas development, as described above, the presence of cellular plasticity in the adult pancreas has been suggested and reviewed elsewhere [52]. Cellular plasticity such as beta-cell neogenesis from duct cells or transdifferentiation from acinar cells or other endocrine cells (e.g., alpha-cells) may contribute to newly formed beta-cells, in addition to beta-cell replication. Although the role of beta-cell neogenesis as a source of new beta-cells remains to be established, an increase in insulin-positive duct cells, a surrogate marker for beta-cell neogenesis, has been observed in patients with impaired glucose tolerance [46]. Thus, the exocrine pancreas may have an important role as a source of endocrine cells in beta-cell regeneration.
5. Mechanisms of the interplay between endocrine and exocrine pancreas
5.1 Effects of islet hormones on exocrine pancreas
Pancreatic parenchymal mass is increased with obesity [13]. Although exocrine mass and function are regulated by numerous factors, studies conducted in the last decades have revealed that islet hormones act as trophic factors in the exocrine pancreas. Insulin is one of the major regulators of exocrine growth and function, impacting the exocrine pancreas locally in a paracrine manner [53]. Thus, reduced pancreas mass in patients with T1D is likely to be mediated by reduced endogenous insulin secretion in these subjects, although a recent study suggested that pancreas volume is already reduced years before the clinical onset of T1D [15, 17]. On the other hand, the increase in pancreas mass with obesity may also be explained by insulin hypersecretion from beta-cells.
The interplay between the endocrine and exocrine pancreas may also be mediated by other islet-derived hormones such as PP and somatostatin, other humoral factors including pancreastatin and ghrelin, and neurotransmitters such as nitric oxide, peptide YY, substance P, pituitary adenylate cyclase activating polypeptide (PACAP), and galanin released by nerves innervating the pancreas, as reviewed elsewhere [54]. Further investigation is needed to clarify the effects of these factors on pancreas mass in humans.
5.2 Beta-cell area and function in pancreatic diseases
Conversely, pathological changes in the exocrine pancreas also affect endocrine pancreas and glucose metabolism. Pancreatic diseases such as pancreatitis and pancreatic cancer often cause hyperglycemia, referred to as pancreatic or pancreatogenic diabetes [55-59]. The mechanisms by which pancreatitis and pancreatic cancer promote hyperglycemia remain to be fully clarified, but insulin secretion is often impaired in these patients [60]. The pancreas of patients with chronic pancreatitis shows atrophic and fibrotic change of the exocrine pancreas [61]. In these patients, although islet architecture is relatively well preserved, fractional beta-cell area is decreased [61]. On the other hand, atrophy of the exocrine pancreas is not obvious in patients with pancreatic cancer, and the effects of pancreatic cancers on islet architecture remain unclear [62, 63].
By examining pancreata from 99 subjects who underwent pancreatic surgery, we found that the fractional beta-cell area in the resected pancreas was significantly decreased in patients with pancreatic cancer compared to that in patients with other pancreatic tumors, and that the reduction was independent of the presence or absence of diabetes [38]. Humoral factors such as amylin and inflammatory cytokines produced by tumors may induce beta-cell dysfunction [59]. Recent studies suggest that adrenomedullin is a mediator of beta-cell dysfunction and impaired glucose metabolism in patients with pancreatic cancer [64].
5.3 Obesity-induced inflammation in exocrine pancreas
Obesity and diabetes are also associated with an increased risk of pancreatitis and pancreatic cancer [65]. While the underlying mechanisms remain unclear, rodent studies have shown that a high-fat diet induces inflammation and fibrosis in the exocrine pancreas [66]. Oxidative stress, impaired autophagy, and ER stress induced by various types of fatty acids have been proposed as mechanisms of inflammation in exocrine tissue [65, 67-69].
While an increase in immune cell infiltration within the exocrine pancreas is a typical event in T1D [70], recent studies have also shown evidence of islet inflammation in patients with T2D [71-76]. A recent rodent study has shown that intestinal bacteria entering the pancreatic duct system could trigger an adverse innate immune response towards beta-cells, leading to the development of T1D [77]. These findings indicate that the interaction between the endocrine and exocrine pancreas may be in part mediated by inflammatory change within the pancreas. It is possible that obesity-induced chronic inflammation in the exocrine pancreas may induce islet inflammation and beta-cell dysfunction, and thus contribute to the changes in pancreas volume observed with obesity and diabetes. Since beta-cell neogenesis from pancreatic ducts and acinar cells has been reported [78], inflammatory changes in the exocrine pancreas may also affect beta-cell neogenesis and influence beta-cell mass.
5.4 Anti-diabetic medication and exocrine pancreas
Recent advances in the development of anti-diabetic agents have provided new therapeutic options for the management of diabetes. Because of the interplay between endocrine and exocrine pancreas, anti-diabetic medication may affect the exocrine pancreas by either changing endocrine function or off-target effects of the agent.
Incretin hormones, glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide (GIP), are secreted from the intestine, and enhance insulin secretion in a glucose-dependent manner [79]. In rodents, administration of GLP-1 or GIP promotes beta-cell proliferation and increase in BCM [80]. Incretin-based medicine, including dipeptidyl peptidase-4 (DPP-4) inhibitors and GLP-1 receptor agonists (GLP-1RAs), is now widely used for the treatment of T2D. DPP-4 inhibitors prevent the degradation of incretin through DPP-4 inhibition, thereby enhancing endogenous incretin action. GLP-1RAs are injectable drugs that activate the GLP-1 receptor at a supraphysiological level. Incretin-based medicine is associated with a low risk of hypoglycemia and a favorable weight profile (weight reduction by GLP-1RAs) in addition to its glucose-lowering effect [79].
However, since the launch of incretin-based medicine several case reports on the development of acute pancreatitis have been published, and the US Food and Drug Administration (FDA) has issued a "black box warning" for these drugs [81]. Incretin-induced pancreatitis and subsequent oncogenesis have been suggested by some animal studies [82-85], but the results are conflicting [86-90]. It has also been shown that the GLP-1 receptor is expressed in some but not all pancreatic exocrine cells [91], while DPP-4 is expressed in some (~30%) duct cells [92]. To date, no significant association between incretin therapy and pancreatitis or pancreatic cancer has been confirmed in either large-scale cohort studies or randomized controlled trials [93-95].
Using autopsy pancreas, Butler et al. reported that pancreas mass was increased by ~40% in subjects with T2D who had been treated with incretin-based medicine [96], although these results may have been confounded by other factors [97, 98]. A recent rodent study showed that incretin therapy increases pancreas mass by ~30% as a result of enhanced protein synthesis [99]. Although we have reported that there was no change in pancreas volume measured by CT scan 6 months after the initiation of liraglutide treatment [100], a slight increase in amylase or lipase after treatment with GLP-1RA has been consistently observed [100-103]. The mechanisms by which incretin therapy increases pancreatic enzyme levels remain unclear. Further studies are needed to clarify the effect of incretin-based therapy on pancreas mass.
6. Components of the pancreas: role of pancreatic fat deposition
6.1 Ectopic fat deposition and diabetes: the lipotoxicity hypothesis
Obesity, especially visceral adiposity, is associated with the development of T2D [104]. The combination of excessive caloric intake and minimal physical activity results in increased fat storage. When fat supply exceeds the capacity of subcutaneous fat storage, spillover of fat leads to ectopic fat deposits in various tissues such as visceral tissue, liver, heart, and skeletal muscle. Ectopic fat deposition also occurs in the pancreas [105-108], which is known as pancreatic steatosis [109].
The association of ectopic fat deposition in various tissues with tissue dysfunction and metabolic derangements is known as the lipotoxicity hypothesis [110-112]. Therefore, fat deposits in the pancreas are an area of active investigation, besides pancreas mass. Pancreatic fat content is increased with obesity, and intra- and interlobular adipocytes, acinar cell fat content, and islet fat content appear to increase proportionally with obesity [105, 108]. Lee et al. reported that the accumulation of fat in islets causes beta-cell dysfunction and diabetes in rodents [113]. It has also been shown that the incubation of beta-cells with free fatty acids impairs insulin secretion and promotes beta-cell apoptosis [114]. Furthermore, leptin, tumor necrosis factor (TNF)-alpha, and other adipocytokines secreted from adipocytes within the pancreas may induce beta-cell damage in a paracrine manner. These findings point to a deleterious impact of lipotoxicity on beta-cells, which needs to be clarified in vivo in more detail. Currently, the association between fat accumulation in the pancreas and glucose metabolism is an area of ongoing investigation.
6.2 Pancreatic fat, beta-cell function, and glucose intolerance
It has been reported that pancreatic fat quantified by either sonography, CT, MRI, or MR spectrometry (MRS) is increased in patients with dysglycemia [115-122], and pancreatic fat content is negatively correlated with beta-cell function [123-127] (Table 2). Honka et al. have recently studied pancreatic metabolism and blood flow in obese subjects, using positron emission tomography (PET) [128]. The obese individuals showed increased pancreatic fatty acid uptake and fat accumulation and reduced pancreatic blood flow; both of these effects were inversely associated with beta-cell function [128]. The same group also reported improvement in these factors and beta-cell function in patients with T2D who had received bariatric surgery [129]. Thus, not only pancreatic fat, but also pancreatic blood flow, may be associated with impaired beta-cell function in obese subjects.
Table 2. Studies reporting an association between pancreatic fat and glucose metabolism.
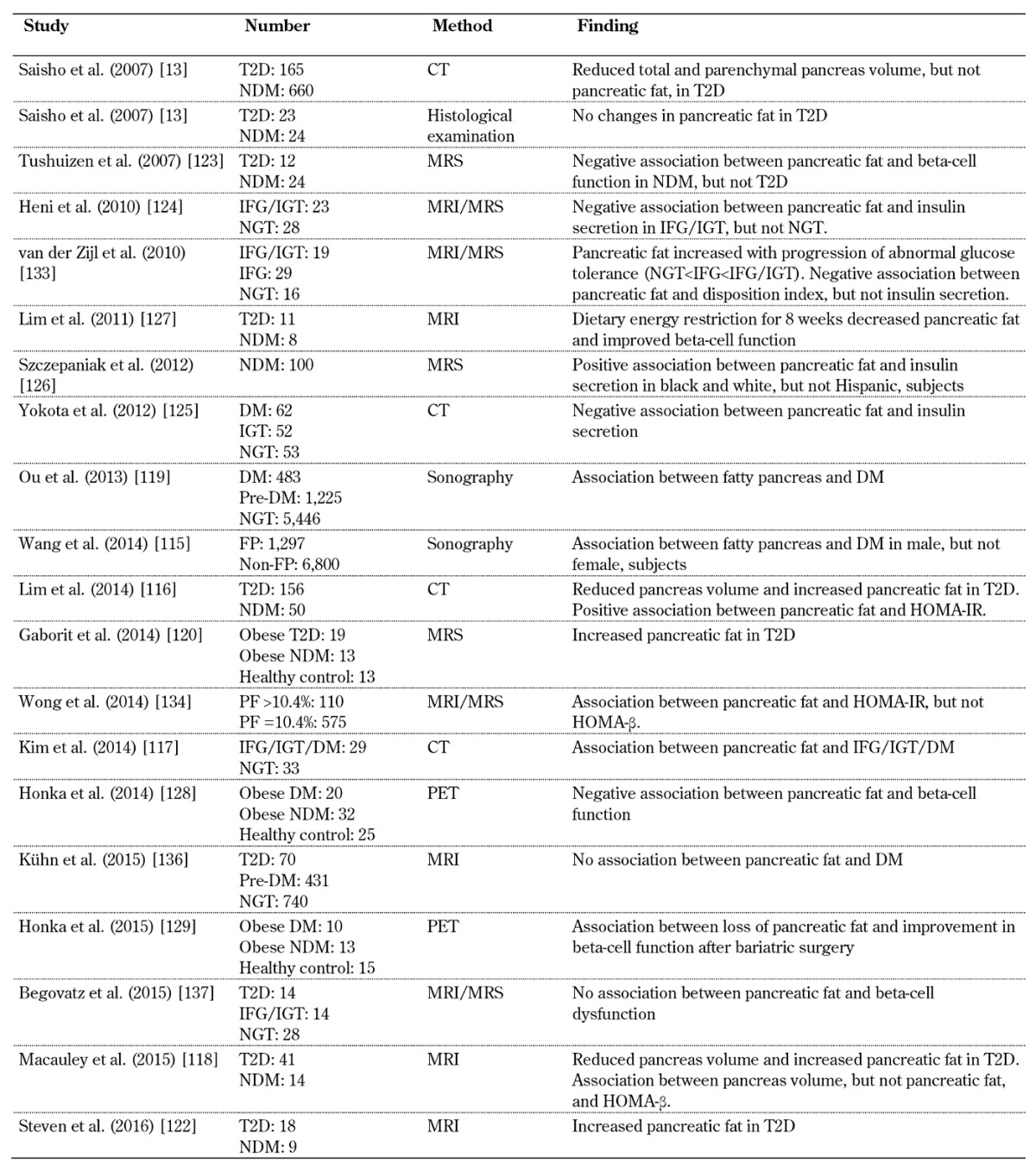
Legend: CT – computed tomography, DM – diabetes mellitus, FP – fatty pancreas, IFG – impaired fasting glucose, IGT – impaired glucose tolerance, MRI – magnetic resonance imaging, MRS – magnetic resonance spectroscopy, NDM – non-diabetes mellitus, NGT – normal glucose tolerance, HOMA-IR – homeostasis model assessment of insulin resistance, HOMA-β – homeostatis model assessment of beta-cell function, PET – positron emission tomography, T2D – type 2 diabetes.
However, inconsistent results have been obtained regarding the association between pancreatic fat and glucose metabolism in humans. Pancreatic fat is characterized by adipocyte infiltration in the interlobular and intralobular pancreas [14, 105, 109]. Since a major part of the pancreatic fat is due to adipocyte infiltration, fat distribution in the pancreas is often heterogeneous, which complicates the determination of fat content and distribution in the pancreas, and which may provide a reason for the inconsistencies.
It has also been reported that fat deposits are larger in the body and tail than in the head of the pancreas [130]. However, since pancreatic fat content may also be affected by age and obesity, a causal association between pancreatic fat content and glucose intolerance or beta-cell dysfunction is difficult to establish [106, 131-136]. In our analysis, using CT scan, there was a significant correlation between pancreatic fat content and BMI, but no significant difference in pancreatic fat volume between subjects with and without T2D who were matched for age, sex, and BMI [13] (Table 1 and Figure 4). Histological analysis also showed no significant difference in intralobular pancreatic fat area between age- and BMI-matched subjects with and without T2D [13]. In a recent study, pancreatic intralobular fat was measured carefully by using MRI/MRS techniques and excluding interlobular and peripancreatic fat. There was no association between total or intralobular pancreatic fat and beta-cell function, fasting glucose level, or 2-h glucose level during a 75-g oral glucose tolerance test (OGTT) in patients with and without dysglycemia, while total and intralobular pancreatic fat was positively correlated with age [137]. Consequently, although pancreatic fat has been postulated as a potential cause of beta-cell damage, a causal association between pancreatic fat, beta-cell dysfunction, and glucose intolerance in humans remains to be established. Further investigation is warranted.
Figure 4. Relationship between BMI and pancreatic volume measured on the basis of CT scan images.
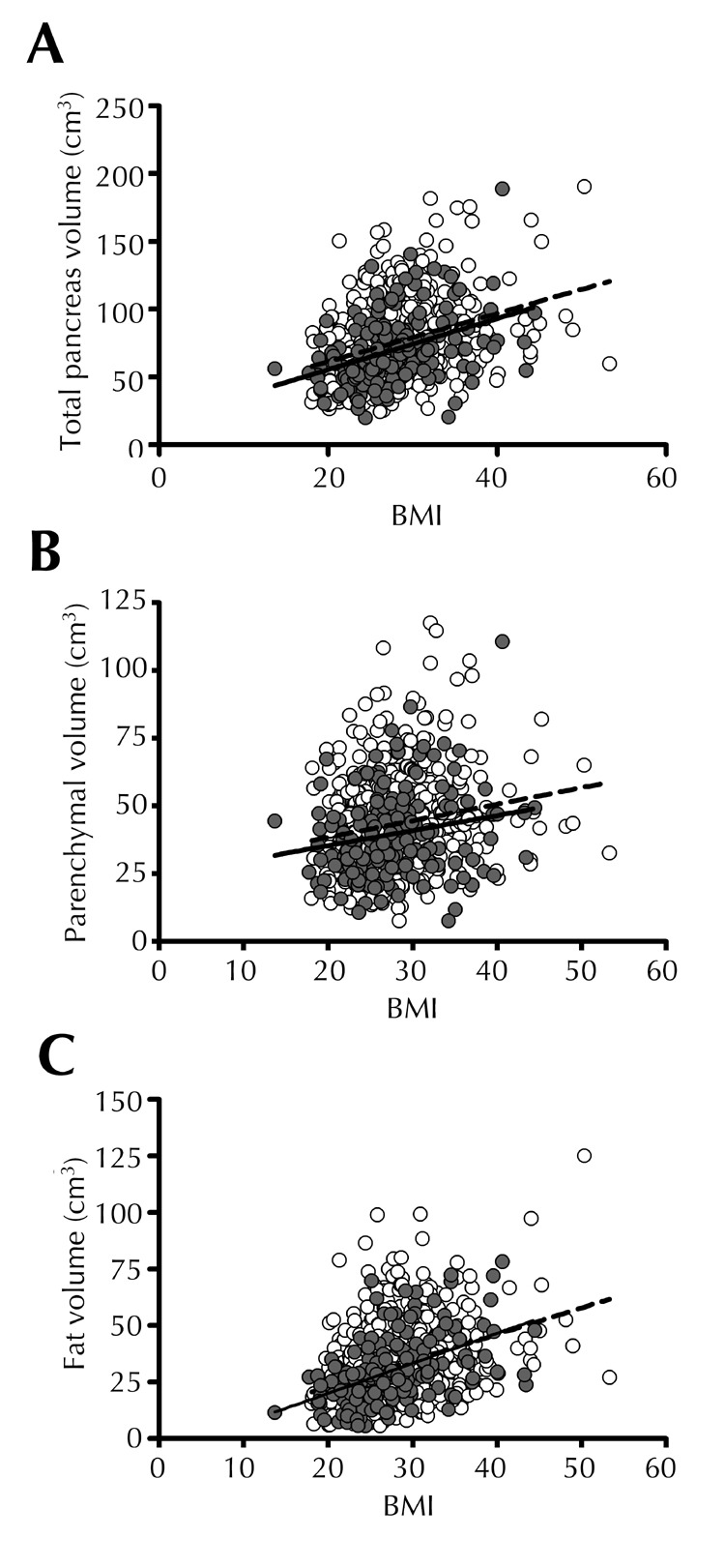
^Despite considerable individual variance, there is a significant relationship between BMI and total (A), parenchymal (B), and fat (C) volumes in non-diabetic subjects (white dots, broken line) and subjects with type 2 diabetes (T2D) (gray dots, solid line). The relationships are comparable in individuals with T2D and non-diabetics (NDM). A: NDM, r = 0.3, p < 0.0001; T2D, r = 0.4, p < 0.0001. B: NDM, r = 0.2, p < 0.0001; T2D, r = 0.2, p = 0.01. C: NDM, r = 0.4, p < 0.0001; T2D, r = 0.5, p < 0.0001. Reproduced with permission from the authors of reference [13].
7. Conclusions
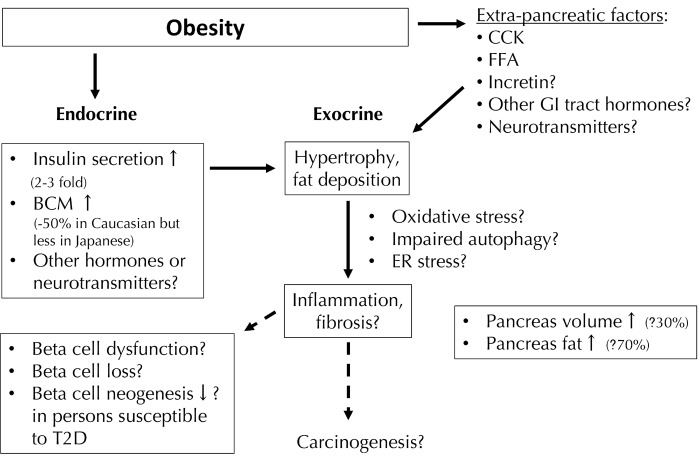
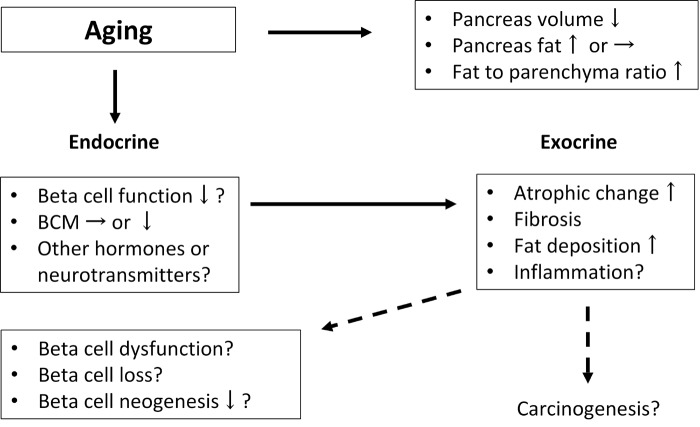
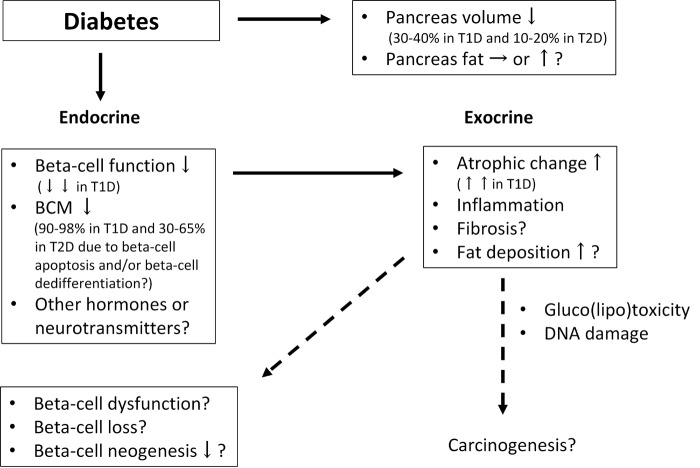
This review has summarized the physiological and pathological changes in exocrine pancreas and beta-cell mass in response to fat accumulation in the pancreas, and has discussed potential biological mechanisms. The changes in pancreas volume and fat deposition in diabetes as opposed to normal physiology, and the potential mechanisms of the interplay between the endocrine and exocrine pancreas are summarized in Figures 5-7. Since these two compartments of the pancreas arise from the same origin, changes in one compartment are considered to affect the other.
Figure 5. Pathophysiological changes in pancreas volume in the presence of obesity and potential mechanisms of the interplay between endocrine and exocrine pancreas.
Pancreas volume increases with obesity. Insulin acts as a trophic factor on the exocrine pancreas. Inflammatory changes in the exocrine pancreas may affect endocrine function and/or mass. Abbreviations: BCM – beta-cell mass, CCK – cholecystokinin, ER – endoplasmic reticulum, FFA – free fatty acid, GI – gastrointestinal, T2D – type 2 diabetes.
Figure 7. Pathophysiological changes in pancreas volume in the presence of aging and potential mechanisms of the interplay between endocrine and exocrine pancreas.
Pancreas volume decreases in the presence of aging and beta-cell function reduces. Abbreviation: BCM – beta-cell mass.
It is well known that there are several causes of reduced endocrine pancreatic function, including aging, obesity, and diabetes. However, it remains largely unclear how beta-cell mass and function are affected exactly by these factors. Pancreas volume, pancreatic fat content, and beta-cell mass change with aging, with fat content being increased and beta-cell mass reduced. The harmful effect of increased pancreatic fat content may be caused by acinar atrophy and fibrosis in the exocrine pancreas, which may negatively affect endocrine cell function and cell formation. As mentioned above, obesity is another cause of declined beta-cell mass and impaired function. The reason is that pancreatic fat content can be increased in obesity, suggesting that pancreatic fat deposits have a deleterious effect on beta-cell mass and function. However, this hypothesis also remains controversial, and needs to be verified by further studies.
In contrast, the effects of diabetes on beta-cell mass and function are largely common; both T1D and T2D are characterized by a deficit in beta-cell mass. Therefore, prevention or reversal of beta-cell loss could be possible therapies for both types of diabetes. In this regard, a better understanding of the interplay between exocrine and endocrine pancreas may help to clarify the mechanisms regulating the pancreatic components, and eventually to cure diabetes through beta-cell preservation or even regeneration.
Figure 6. Pathophysiological changes in pancreas volume in the presence of diabetes and potential mechanisms of the interplay between endocrine and exocrine pancreas.
Pancreas volume decreases in the presence of diabetes. Insulin acts as a trophic factor on the exocrine pancreas. Inflammatory changes in the exocrine pancreas may affect endocrine function and/or mass. Abbreviations: BCM – beta-cell mass, DNA – deoxyribonucleic acid, T1D – type 1 diabetes, T2D – type 2 diabetes.
Acknowledgments
Acknowledgments
The author thanks Dr. Wendy Gray for editing the manuscript.
Disclosures
The author reported no conflict of interests.
References
- 1.Chen N, Unnikrishnan I R, Anjana RM, Mohan V, Pitchumoni CS. The complex exocrine-endocrine relationship and secondary diabetes in exocrine pancreatic disorders. J Clin Gastroenterol. 2011;45(10):850–861. doi: 10.1097/MCG.0b013e31822a2ae5. [DOI] [PubMed] [Google Scholar]
- 2.Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes. 2003;52(1):102–110. doi: 10.2337/diabetes.52.1.102. [DOI] [PubMed] [Google Scholar]
- 3.Sakuraba H, Mizukami H, Yagihashi N, Wada R, Hanyu C, Yagihashi S. Reduced beta-cell mass and expression of oxidative stress-related DNA damage in the islet of Japanese type 2 diabetic patients. Diabetologia. 2002;45(1):85–96. doi: 10.1007/s125-002-8248-z. [DOI] [PubMed] [Google Scholar]
- 4.Rahier J, Guiot Y, Goebbels RM, Sempoux C, Henquin JC. Pancreatic beta-cell mass in European subjects with type 2 diabetes. Diabetes Obes Metab. 2008;10(Suppl 4):32–42. doi: 10.1111/j.1463-1326.2008.00969.x. [DOI] [PubMed] [Google Scholar]
- 5.Yoon KH, Ko SH, Cho JH, Lee JM, Ahn YB, Song KH, Yoo SJ, Kang MI, Cha BY, Lee KW. et al. Selective beta-cell loss and alpha-cell expansion in patients with type 2 diabetes mellitus in Korea. J Clin Endocrinol Metab. 2003;88(5):2300–2308. doi: 10.1210/jc.2002-020735. [DOI] [PubMed] [Google Scholar]
- 6.Xu X, D'Hoker J, Stange G, Bonne S, De Leu N, Xiao X, Van de Casteele M, Mellitzer G, Ling Z, Pipeleers D. et al. Beta cells can be generated from endogenous progenitors in injured adult mouse pancreas. Cell. 2008;132(2):197–207. doi: 10.1016/j.cell.2007.12.015. [DOI] [PubMed] [Google Scholar]
- 7.Inada A, Nienaber C, Katsuta H, Fujitani Y, Levine J, Morita R, Sharma A, Bonner-Weir S. Carbonic anhydrase II-positive pancreatic cells are progenitors for both endocrine and exocrine pancreas after birth. Proc Natl Acad Sci USA. 2008;105(50):19915–19919. doi: 10.1073/pnas.0805803105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Minami K, Okuno M, Miyawaki K, Okumachi A, Ishizaki K, Oyama K, Kawaguchi M, Ishizuka N, Iwanaga T, Seino S. Lineage tracing and characterization of insulin-secreting cells generated from adult pancreatic acinar cells. Proc Natl Acad Sci USA. 2005;102(42):15116–15121. doi: 10.1073/pnas.0507567102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Zhou Q, Brown J, Kanarek A, Rajagopal J, Melton DA. In vivo reprogramming of adult pancreatic exocrine cells to beta-cells. Nature. 2008;455(7213):627–632. doi: 10.1038/nature07314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Baeyens L, Lemper M, Leuckx G, De Groef S, Bonfanti P, Stange G, Shemer R, Nord C, Scheel DW, Pan FC. et al. Transient cytokine treatment induces acinar cell reprogramming and regenerates functional beta cell mass in diabetic mice. Nat Biotechnol. 2014;32(1):76–83. doi: 10.1038/nbt.2747. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 11.Jennings RE, Berry AA, Strutt JP, Gerrard DT, Hanley NA. Human pancreas development. Development. 2015;142(18):3126–3137. doi: 10.1242/dev.120063. [DOI] [PubMed] [Google Scholar]
- 12.Shih HP, Wang A, Sander M. Pancreas organogenesis: from lineage determination to morphogenesis. Annu Rev Cell Dev Biol. 2013;29:81–105. doi: 10.1146/annurev-cellbio-101512-122405. [DOI] [PubMed] [Google Scholar]
- 13.Saisho Y, Butler AE, Meier JJ, Monchamp T, Allen-Auerbach M, Rizza RA, Butler PC. Pancreas volumes in humans from birth to age one hundred taking into account sex, obesity, and presence of type-2 diabetes. Clin Anat. 2007;20(8):933–942. doi: 10.1002/ca.20543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Saisho Y, Butler AE, Manesso E, Elashoff D, Rizza RA, Butler PC. Beta-cell mass and turnover in humans: Effects of obesity and aging. Diabetes Care. 2013;36(1):111–117. doi: 10.2337/dc12-0421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Campbell-Thompson ML, Kaddis JS, Wasserfall C, Haller MJ, Pugliese A, Schatz DA, Shuster JJ, Atkinson MA. The influence of type 1 diabetes on pancreatic weight. Diabetologia. 2016;59(1):217–221. doi: 10.1007/s00125-015-3752-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Goda K, Sasaki E, Nagata K, Fukai M, Ohsawa N, Hahafusa T. Pancreatic volume in type 1 and type 2 diabetes mellitus. Acta Diabetol. 2001;38(3):145–149. doi: 10.1007/s005920170012. [DOI] [PubMed] [Google Scholar]
- 17.Williams AJ, Thrower SL, Sequeiros IM, Ward A, Bickerton AS, Triay JM, Callaway MP, Dayan CM. Pancreatic volume is reduced in adult patients with recently diagnosed type 1 diabetes. J Clin Endocrinol Metab. 2012;97(11):E2109–E2113. doi: 10.1210/jc.2012-1815. [DOI] [PubMed] [Google Scholar]
- 18.Saisho Y. The pancreas in humans with and without diabetes. Diabetologia. 2016;59(4):868–869. doi: 10.1007/s00125-016-3881-z. [DOI] [PubMed] [Google Scholar]
- 19.Saisho Y. Pancreas volume with obesity in Asians: comparison with whites. Pancreas. 2014;43(4):657–659. doi: 10.1097/MPA.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 20.Kou K, Saisho Y, Jinzaki M, Itoh H. Relationship between body mass index and pancreas volume in Japanese adults. JOP. 2014;15(6):626–627. doi: 10.6092/1590-8577/2858. [DOI] [PubMed] [Google Scholar]
- 21.Meier JJ, Bhushan A, Butler AE, Rizza RA, Butler PC. Sustained beta cell apoptosis in patients with long-standing type 1 diabetes: indirect evidence for islet regeneration? Diabetologia. 2005;48(11):2221–2228. doi: 10.1007/s00125-005-1949-2. [DOI] [PubMed] [Google Scholar]
- 22.Butler AE, Galasso R, Meier JJ, Basu R, Rizza RA, Butler PC. Modestly increased beta cell apoptosis but no increased beta cell replication in recent-onset type 1 diabetic patients who died of diabetic ketoacidosis. Diabetologia. 2007;50(11):2323–2331. doi: 10.1007/s00125-007-0794-x. [DOI] [PubMed] [Google Scholar]
- 23.Gianani R, Campbell-Thompson M, Sarkar SA, Wasserfall C, Pugliese A, Solis JM, Kent SC, Hering BJ, West E, Steck A. et al. Dimorphic histopathology of long-standing childhood-onset diabetes. Diabetologia. 2010;53(4):690–698. doi: 10.1007/s00125-009-1642-y. [DOI] [PubMed] [Google Scholar]
- 24.Frier BM, Faber OK, Binder C, Elliott HL. The effect of residual insulin secretion on exocrine pancreatic function in juvenile-onset diabetes mellitus. Diabetologia. 1978;14(5):301–304. doi: 10.1007/BF01223020. [DOI] [PubMed] [Google Scholar]
- 25.Hardt PD, Krauss A, Bretz L, Porsch-Özcürümez M, Schnell-Kretschmer H, Mäser E, Bretzel RG, Zekorn T, Klör HU. Pancreatic exocrine function in patients with type 1 and type 2 diabetes mellitus. Acta Diabetologica. 2000;37(3):105–110. doi: 10.1007/s005920070011. [DOI] [PubMed] [Google Scholar]
- 26.Larger E, Philippe MF, Barbot-Trystram L, Radu A, Rotariu M, Nobecourt E, Boitard C. Pancreatic exocrine function in patients with diabetes. Diabet Med. 2012;29(8):1047–1054. doi: 10.1111/j.1464-5491.2012.03597.x. [DOI] [PubMed] [Google Scholar]
- 27.Burute N, Nisenbaum R, Jenkins DJ, Mirrahimi A, Anthwal S, Colak E, Kirpalani A. Pancreas volume measurement in patients with Type 2 diabetes using magnetic resonance imaging-based planimetry. Pancreatology. 2014;14(4):268–274. doi: 10.1016/j.pan.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 28.Philippe MF, Benabadji S, Barbot-Trystram L, Vadrot D, Boitard C, Larger E. Pancreatic volume and endocrine and exocrine functions in patients with diabetes. Pancreas. 2011;40(3):359–363. doi: 10.1097/MPA.0b013e3182072032. [DOI] [PubMed] [Google Scholar]
- 29.Meier JJ, Butler AE, Saisho Y, Monchamp T, Galasso R, Bhushan A, Rizza RA, Butler PC. Beta-cell replication is the primary mechanism subserving the postnatal expansion of beta-cell mass in humans. Diabetes. 2008;57(6):1584–1594. doi: 10.2337/db07-1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mizukami H, Takahashi K, Inaba W, Osonoi S, Kamata K, Tsuboi K, Yagihashi S. Age-associated changes of islet endocrine cells and the effects of body mass index in Japanese. J Diabetes Investig. 2014;5(1):38–47. doi: 10.1111/jdi.12118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cobelli C, Toffolo GM, Dalla Man C, Campioni M, Denti P, Caumo A, Butler P, Rizza R. Assessment of beta-cell function in humans, simultaneously with insulin sensitivity and hepatic extraction, from intravenous and oral glucose tests. Am J Physiol Endocrinol Metab. 2007;293(1):E1–E15. doi: 10.1152/ajpendo.00421.2006. [DOI] [PubMed] [Google Scholar]
- 32.Avrahami D, Li C, Zhang J, Schug J, Avrahami R, Rao S, Stadler MB, Burger L, Schubeler D, Glaser B, Kaestner KH. Aging-dependent demethylation of regulatory elements correlates with chromatin state and improved beta cell function. Cell Metab. 2015;22(4):619–632. doi: 10.1016/j.cmet.2015.07.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Helman A, Klochendler A, Azazmeh N, Gabai Y, Horwitz E, Anzi S, Swisa A, Condiotti R, Granit RZ, Nevo Y. et al. p16Ink4a-induced senescence of pancreatic beta cells enhances insulin secretion. Nat Med. 2016;22(4):412–420. doi: 10.1038/nm.4054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Henquin JC, Rahier J. Pancreatic alpha cell mass in European subjects with type 2 diabetes. Diabetologia. 2011;54(7):1720–1725. doi: 10.1007/s00125-011-2118-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mizukami H, Takahashi K, Inaba W, Tsuboi K, Osonoi S, Yoshida T, Yagihashi S. Involvement of oxidative stress-induced DNA damage, endoplasmic reticulum stress, and autophagy deficits in the decline of beta-cell mass in Japanese type 2 diabetic patients. Diabetes Care. 2014;37(7):1966–1974. doi: 10.2337/dc13-2018. [DOI] [PubMed] [Google Scholar]
- 36.Sato S, Saisho Y, Inaishi J, Kou K, Murakami R, Yamada T, Itoh H. Effects of glucocorticoid treatment on beta- and alpha-cell mass in Japanese adults with and without diabetes. Diabetes. 2015;64(8):2915–2927. doi: 10.2337/db15-0151. [DOI] [PubMed] [Google Scholar]
- 37.Kilimnik G, Zhao B, Jo J, Periwal V, Witkowski P, Misawa R, Hara M. Altered islet composition and disproportionate loss of large islets in patients with type 2 diabetes. Plos One. 2011;6(11):e27445. doi: 10.1371/journal.pone.0027445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Inaishi J, Saisho Y, Sato S, Kou K, Murakami R, Watanabe Y, Kitago M, Kitagawa Y, Yamada T, Itoh H. Effects of obesity and diabetes on alpha and beta cell mass in surgically resected human pancreas. J Clin Endocrinol Metab. 2016;101(7):2874–2882. doi: 10.1210/jc.2016-1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Field AE, Coakley EH, Must A, Spadano JL, Laird N, Dietz WH, Rimm E, Colditz GA. Impact of overweight on the risk of developing common chronic diseases during a 10-year period. Arch Intern Med. 2001;161(13):1581–1586. doi: 10.1001/archinte.161.13.1581. [DOI] [PubMed] [Google Scholar]
- 40.Zimmet P, Alberti KG, Shaw J. Global and societal implications of the diabetes epidemic. Nature. 2001;414(6865):782–787. doi: 10.1038/414782a. [DOI] [PubMed] [Google Scholar]
- 41.Hu Y, Bhupathiraju SN, de Koning L, Hu FB. Duration of obesity and overweight and risk of type 2 diabetes among US women. Obesity. 2014;22(10):2267–2273. doi: 10.1002/oby.20851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kou K, Saisho Y, Satoh S, Yamada T, Itoh H. Change in beta-cell mass in Japanese nondiabetic obese individuals. J Clin Endocrinol Metab. 2013;98(9):3724–3730. doi: 10.1210/jc.2013-1373. [DOI] [PubMed] [Google Scholar]
- 43.Polonsky KS, Given BD, Van Cauter E. Twenty-four-hour profiles and pulsatile patterns of insulin secretion in normal and obese subjects. J Clin Invest. 1988;81(2):442–448. doi: 10.1172/JCI113339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Saisho Y. Beta cell dysfunction: Its critical role in prevention and management of type 2 diabetes. World J Diabetes. 2015;6(1):109–124. doi: 10.4239/wjd.v6.i1.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Meier JJ, Breuer TG, Bonadonna RC, Tannapfel A, Uhl W, Schmidt WE, Schrader H, Menge BA. Pancreatic diabetes manifests when beta cell area declines by approximately 65% in humans. Diabetologia. 2012;55(5):1346–1354. doi: 10.1007/s00125-012-2466-8. [DOI] [PubMed] [Google Scholar]
- 46.Yoneda S, Uno S, Iwahashi H, Fujita Y, Yoshikawa A, Kozawa J, Okita K, Takiuchi D, Eguchi H, Nagano H. et al. Predominance of beta-cell neogenesis rather than replication in humans with an impaired glucose tolerance and newly diagnosed diabetes. J Clin Endocrinol Metab. 2013;98(5):2053–2061. doi: 10.1210/jc.2012-3832. [DOI] [PubMed] [Google Scholar]
- 47.Kou K, Saisho Y, Sato S, Yamada T, Itoh H. Islet number rather than islet size is a major determinant of beta- and alpha-cell mass in humans. J Clin Endocrinol Metab. 2014;99(5):1733–1740. doi: 10.1210/jc.2013-3731. [DOI] [PubMed] [Google Scholar]
- 48.Saisho Y. Obesity, type 2 diabetes and beta cell failure: An Asian perspective. J Mol Genet Med. 2014;S1:008. [Google Scholar]
- 49.Butler AE, Dhawan S, Hoang J, Cory M, Zeng K, Fritsch H, Meier JJ, Rizza RA, Butler PC. Beta-cell deficit in obese type 2 diabetes, a minor role of beta-cell dedifferentiation and degranulation. J Clin Endocrinol Metab. 2016;101(2):523–532. doi: 10.1210/jc.2015-3566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Talchai C, Xuan S, Lin HV, Sussel L, Accili D. Pancreatic beta cell dedifferentiation as a mechanism of diabetic beta cell failure. Cell. 2012;150(6):1223–1234. doi: 10.1016/j.cell.2012.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Gregg BE, Moore PC, Demozay D, Hall BA, Li M, Husain A, Wright AJ, Atkinson MA, Rhodes CJ. Formation of a human beta-cell population within pancreatic islets is set early in life. J Clin Endocrinol Metab. 2012;97(9):3197–3206. doi: 10.1210/jc.2012-1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stanger BZ, Hebrok M. Control of cell identity in pancreas development and regeneration. Gastroenterology. 2013;144(6):1170–1179. doi: 10.1053/j.gastro.2013.01.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Williams JA, Goldfine ID. The insulin-pancreatic acinar axis. Diabetes. 1985;34(10):980–986. doi: 10.2337/diab.34.10.980. [DOI] [PubMed] [Google Scholar]
- 54.Barreto SG, Carati CJ, Toouli J, Saccone GT. The islet-acinar axis of the pancreas: more than just insulin. Am J Physiol Gastrointest Liver Physiol. 2010;299(1):G10–G22. doi: 10.1152/ajpgi.00077.2010. [DOI] [PubMed] [Google Scholar]
- 55.Das SL, Singh PP, Phillips AR, Murphy R, Windsor JA, Petrov MS. Newly diagnosed diabetes mellitus after acute pancreatitis: a systematic review and meta-analysis. Gut. 2014;63(5):818–831. doi: 10.1136/gutjnl-2013-305062. [DOI] [PubMed] [Google Scholar]
- 56.Cui Y, Andersen DK. Pancreatogenic diabetes: special considerations for management. Pancreatology. 2011;11(3):279–294. doi: 10.1159/000329188. [DOI] [PubMed] [Google Scholar]
- 57.Rickels MR, Bellin M, Toledo FG, Robertson RP, Andersen DK, Chari ST, Brand R, Frulloni L, Anderson MA, Whitcomb DC. Detection, evaluation and treatment of diabetes mellitus in chronic pancreatitis: recommendations from PancreasFest 2012. Pancreatology. 2013;13(4):336–342. doi: 10.1016/j.pan.2013.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chen N, Unnikrishnan IR, Anjana RM, Mohan V, Pitchumoni CS. The complex exocrine-endocrine relationship and secondary diabetes in exocrine pancreatic disorders. J Clin Gastroenterol. 2011;45(10):850–861. doi: 10.1097/MCG.0b013e31822a2ae5. [DOI] [PubMed] [Google Scholar]
- 59.Meisterfeld R, Ehehalt F, Saeger HD, Solimena M. Pancreatic disorders and diabetes mellitus. Exp Clin Endocrinol Diabetes. 2008;116(Suppl 1):S7–S12. doi: 10.1055/s-2008-1080918. [DOI] [PubMed] [Google Scholar]
- 60.Chari ST, Zapiach M, Yadav D, Rizza RA. Beta-cell function and insulin resistance evaluated by HOMA in pancreatic cancer subjects with varying degrees of glucose intolerance. Pancreatology. 2005;5(2-3):229–233. doi: 10.1159/000085276. [DOI] [PubMed] [Google Scholar]
- 61.Schrader H, Menge BA, Schneider S, Belyaev O, Tannapfel A, Uhl W, Schmidt WE, Meier JJ. Reduced pancreatic volume and beta-cell area in patients with chronic pancreatitis. Gastroenterology. 2009;136(2):513–522. doi: 10.1053/j.gastro.2008.10.083. [DOI] [PubMed] [Google Scholar]
- 62.Katsumichi I, Pour PM. Diabetes mellitus in pancreatic cancer: is it a causal relationship? Am J Surg. 2007;194(4 Suppl):S71–S75. doi: 10.1016/j.amjsurg.2007.05.024. [DOI] [PubMed] [Google Scholar]
- 63.Saruc M, Iki K, Pour PM. Morphometric studies in human pancreatic cancer argues against the etiological role of type 2 diabetes in pancreatic cancer. Histol Histopathol. 2010;25(4):423–432. doi: 10.14670/HH-25.423. [DOI] [PubMed] [Google Scholar]
- 64.Aggarwal G, Ramachandran V, Javeed N, Arumugam T, Dutta S, Klee GG, Klee EW, Smyrk TC, Bamlet W, Han JJ. et al. Adrenomedullin is up-regulated in patients with pancreatic cancer and causes insulin resistance in beta cells and mice. Gastroenterology. 2012;143(6):1510–1517. doi: 10.1053/j.gastro.2012.08.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gumbs AA. Obesity, pancreatitis, and pancreatic cancer. Obes Surg. 2008;18(9):1183–1187. doi: 10.1007/s11695-008-9599-3. [DOI] [PubMed] [Google Scholar]
- 66.Matsuda A, Makino N, Tozawa T, Shirahata N, Honda T, Ikeda Y, Sato H, Ito M, Kakizaki Y, Akamatsu M. et al. Pancreatic fat accumulation, fibrosis, and acinar cell injury in the Zucker diabetic fatty rat fed a chronic high-fat diet. Pancreas. 2014;43(5):735–743. doi: 10.1097/MPA.0000000000000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gukovsky I, Li N, Todoric J, Gukovskaya A, Karin M. Inflammation, autophagy, and obesity: Common features in the pathogenesis of pancreatitis and pancreatic cancer. Gastroenterology. 2013;144(6):1199–1209. doi: 10.1053/j.gastro.2013.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Danino H, Ben-Dror K, Birk R. Exocrine pancreas ER stress is differentially induced by different fatty acids. Exp Cell Res. 2015;339(2):397–406. doi: 10.1016/j.yexcr.2015.09.022. [DOI] [PubMed] [Google Scholar]
- 69.Navina S, Acharya C, DeLany JP, Orlichenko LS, Baty CJ, Shiva SS, Durgampudi C, Karlsson JM, Lee K, Bae KT. et al. Lipotoxicity causes multisystem organ failure and exacerbates acute pancreatitis in obesity. Sci Transl Med. 2011;3(107):107–110. doi: 10.1126/scitranslmed.3002573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rodriguez-Calvo T, Ekwall O, Amirian N, Zapardiel-Gonzalo J, von Herrath MG. Increased immune cell infiltration of the exocrine pancreas: A possible contribution to the pathogenesis of type 1 diabetes. Diabetes. 2014;63(11):3880–3890. doi: 10.2337/db14-0549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Homo-Delarche F, Calderari S, Irminger JC, Gangnerau MN, Coulaud J, Rickenbach K, Dolz M, Halban P, Portha B, Serradas P. Islet inflammation and fibrosis in a spontaneous model of type 2 diabetes, the GK rat. Diabetes. 2006;55(6):1625–1633. doi: 10.2337/db05-1526. [DOI] [PubMed] [Google Scholar]
- 72.Eguchi K, Manabe I. Macrophages and islet inflammation in type 2 diabetes. Diabetes Obes Metab. 2013;15(s3):152–158. doi: 10.1111/dom.12168. [DOI] [PubMed] [Google Scholar]
- 73.Morris DL. Minireview: Emerging concepts in islet macrophage biology in type 2 diabetes. Mol Endocrinol. 2015;29(7):946–962. doi: 10.1210/me.2014-1393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Donath MY, Dalmas E, Sauter NS, Boni-Schnetzler M. Inflammation in obesity and diabetes: islet dysfunction and therapeutic opportunity. Cell Metab. 2013;17(6):860–872. doi: 10.1016/j.cmet.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 75.Kamata K, Mizukami H, Inaba W, Tsuboi K, Tateishi Y, Yoshida T, Yagihashi S. Islet amyloid with macrophage migration correlates with augmented beta-cell deficits in type 2 diabetic patients. Amyloid. 2014;21(3):191–201. doi: 10.3109/13506129.2014.937857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ehses JA, Perren A, Eppler E, Ribaux P, Pospisilik JA, Maor-Cahn R, Gueripel X, Ellingsgaard H, Schneider MK, Biollaz G. et al. Increased number of islet-associated macrophages in type 2 diabetes. Diabetes. 2007;56(9):2356–2370. doi: 10.2337/db06-1650. [DOI] [PubMed] [Google Scholar]
- 77.Korsgren S, Molin Y, Salmela K, Lundgren T, Melhus A, Korsgren O. On the etiology of type 1 diabetes: a new animal model signifying a decisive role for bacteria eliciting an adverse innate immunity response. Am J Pathol. 2012;181(5):1735–1748. doi: 10.1016/j.ajpath.2012.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Weir GC, Bonner-Weir S. Islet beta cell mass in diabetes and how it relates to function, birth, and death. Ann N Y Acad Sci. 2013;1281:92–105. doi: 10.1111/nyas.12031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368(9548):1696–1705. doi: 10.1016/S0140-6736(06)69705-5. [DOI] [PubMed] [Google Scholar]
- 80.Vilsboll T. The effects of glucagon-like peptide-1 on the beta cell. Diabetes Obes Metab. 2009;11(Suppl 3):11–18. doi: 10.1111/j.1463-1326.2009.01073.x. [DOI] [PubMed] [Google Scholar]
- 81.Parks M, Rosebraugh C. Weighing risks and benefits of liraglutide - the FDA's review of a new antidiabetic therapy. N Engl J Med. 2010;362(9):774–777. doi: 10.1056/NEJMp1001578. [DOI] [PubMed] [Google Scholar]
- 82.Matveyenko AV, Dry S, Cox HI, Moshtaghian A, Gurlo T, Galasso R, Butler AE, Butler PC. Beneficial endocrine but adverse exocrine effects of sitagliptin in the human islet amyloid polypeptide transgenic rat model of type 2 diabetes: interactions with metformin. Diabetes. 2009;58(7):1604–1615. doi: 10.2337/db09-0058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Gier B, Matveyenko AV, Kirakossian D, Dawson D, Dry SM, Butler PC. Chronic GLP-1 receptor activation by exendin-4 induces expansion of pancreatic duct glands in rats and accelerates formation of dysplastic lesions and chronic pancreatitis in the KrasG12D mouse model. Diabetes. 2012;61(5):1250–1262. doi: 10.2337/db11-1109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mondragon A, Davidsson D, Kyriakoudi S, Bertling A, Gomes-Faria R, Cohen P, Rothery S, Chabosseau P, Rutter GA, da Silva Xavier G. Divergent effects of liraglutide, exendin-4, and sitagliptin on beta-cell mass and indicators of pancreatitis in a mouse model of hyperglycaemia. Plos One. 2014;9(8):e104873. doi: 10.1371/journal.pone.0104873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nachnani JS, Bulchandani DG, Nookala A, Herndon B, Molteni A, Pandya P, Taylor R, Quinn T, Weide L, Alba LM. Biochemical and histological effects of exendin-4 (exenatide) on the rat pancreas. Diabetologia. 2010;53(1):153–159. doi: 10.1007/s00125-009-1515-4. [DOI] [PubMed] [Google Scholar]
- 86.Koehler JA, Baggio LL, Lamont BJ, Ali S, Drucker DJ. Glucagon-like peptide-1 receptor activation modulates pancreatitis-associated gene expression but does not modify the susceptibility to experimental pancreatitis in mice. Diabetes. 2009;58(9):2148–2161. doi: 10.2337/db09-0626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Tatarkiewicz K, Smith PA, Sablan EJ, Polizzi CJ, Aumann DE, Villescaz C, Hargrove DM, Gedulin BR, Lu MG, Adams L. et al. Exenatide does not evoke pancreatitis and attenuates chemically induced pancreatitis in normal and diabetic rodents. Am J Physiol Endocrinol Metab. 2010;299(6):E1076–E1086. doi: 10.1152/ajpendo.00479.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Roy D, Chadwick KD, Tatarkiewicz K, Lacerte C, Bergholm AM, Brodie T, Mangipudy RS, Parkes D, Graziano MJ, Reilly TP. The glucagon-like peptide-1-based therapeutics exenatide and saxagliptin did not cause detrimental effects on the pancreas in mice, rats, dogs and monkeys. Diabetes Obes Metab. 2014;16(10):910–921. doi: 10.1111/dom.12294. [DOI] [PubMed] [Google Scholar]
- 89.Gotfredsen CF, Molck AM, Thorup I, Nyborg NC, Salanti Z, Knudsen LB, Larsen MO. The human GLP-1 analogs liraglutide and semaglutide: Absence of histopathological effects on the pancreas in nonhuman primates. Diabetes. 2014;63(7):2486–2497. doi: 10.2337/db13-1087. [DOI] [PubMed] [Google Scholar]
- 90.Fiorentino TV, Owston M, Abrahamian G, La Rosa S, Marando A, Perego C, Di Cairano ES, Finzi G, Capella C, Sessa F. et al. Chronic continuous exenatide infusion does not cause pancreatic inflammation and ductal hyperplasia in non-human primates. Am J Pathol. 2015;185(1):139–150. doi: 10.1016/j.ajpath.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Richards P, Parker HE, Adriaenssens AE, Hodgson JM, Cork SC, Trapp S, Gribble FM, Reimann F. Identification and characterization of GLP-1 receptor-expressing cells using a new transgenic mouse model. Diabetes. 2014;63(4):1224–1233. doi: 10.2337/db13-1440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Augstein P, Naselli G, Loudovaris T, Hawthorne WJ, Campbell P, Bandala-Sanchez E, Rogers K, Heinke P, Thomas HE, Kay TW, Harrison LC. Localization of dipeptidyl peptidase-4 (CD26) to human pancreatic ducts and islet alpha cells. Diabetes Res Clin Pract. 2015;110(3):291–300. doi: 10.1016/j.diabres.2015.10.010. [DOI] [PubMed] [Google Scholar]
- 93.Meier JJ, Nauck MA. Risk of pancreatitis in patients treated with incretin-based therapies. Diabetologia. 2014;57(7):1320–1324. doi: 10.1007/s00125-014-3231-y. [DOI] [PubMed] [Google Scholar]
- 94.Faillie JL, Azoulay L, Patenaude V, Hillaire-Buys D, Suissa S. Incretin-based drugs and risk of acute pancreatitis in patients with type 2 diabetes: cohort study. BMJ. 2014;348:g2780. doi: 10.1136/bmj.g2780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Raz I, Bhatt DL, Hirshberg B, Mosenzon O, Scirica BM, Umez-Eronini A, Im K, Stahre C, Buskila A, Iqbal N. et al. Incidence of pancreatitis and pancreatic cancer in a randomized controlled multicenter trial (SAVOR-TIMI 53) of the dipeptidyl peptidase-4 inhibitor saxagliptin. Diabetes Care. 2014;37(9):2435–2441. doi: 10.2337/dc13-2546. [DOI] [PubMed] [Google Scholar]
- 96.Butler AE, Campbell-Thompson M, Gurlo T, Dawson DW, Atkinson M, Butler PC. Marked expansion of exocrine and endocrine pancreas with incretin therapy in humans with increased exocrine pancreas dysplasia and the potential for glucagon-producing neuroendocrine tumors. Diabetes. 2013;62(7):2595–2604. doi: 10.2337/db12-1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Kahn SE. Incretin therapy and islet pathology: a time for caution. Diabetes. 2013;62(7):2178–2180. doi: 10.2337/db13-0520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bonner-Weir S, In't Veld PA, Weir GC. Reanalysis of study of pancreatic effects of incretin therapy: methodological deficiencies. Diabetes Obes Metab. 2014;16(7):661–666. doi: 10.1111/dom.12257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Koehler JA, Baggio LL, Cao X, Abdulla T, Campbell JE, Secher T, Jelsing J, Larsen B, Drucker DJ. Glucagon-like peptide-1 receptor agonists increase pancreatic mass by induction of protein synthesis. Diabetes. 2015;64(3):1046–1056. doi: 10.2337/db14-0883. [DOI] [PubMed] [Google Scholar]
- 100.Tanaka K, Saisho Y, Manesso E, Tanaka M, Meguro S, Irie J, Sugiura H, Kawai T, Jinzaki M, Cobelli C, Itoh H. Effects of liraglutide monotherapy on beta cell function and pancreatic enzymes compared with metformin in Japanese overweight/obese patients with type 2 diabetes mellitus: A subpopulation analysis of the KIND-LM randomized trial. Clin Drug Invest. 2015;35(10):675–684. doi: 10.1007/s40261-015-0331-5. [DOI] [PubMed] [Google Scholar]
- 101.Lando HM, Alattar M, Dua AP. Elevated amylase and lipase in patients using GLP-1 receptor agonists or DPP-4 inhibitors in the outpatient setting. Endocr Pract. 2012;18(4):472–477. doi: 10.4158/EP11290.OR. [DOI] [PubMed] [Google Scholar]
- 102.Mathieu C, Rodbard HW, Cariou B, Handelsman Y, Philis-Tsimikas A, Ocampo Francisco AM, Rana A, Zinman B BEGIN VICTOZA ADD-ON (NN1250-3948) study group. A comparison of adding liraglutide versus a single daily dose of insulin aspart to insulin degludec in subjects with type 2 diabetes (BEGIN: VICTOZA ADD-ON) Diabetes Obes Metab. 2014;16(7):636–644. doi: 10.1111/dom.12262. [DOI] [PubMed] [Google Scholar]
- 103.Wadden TA, Hollander P, Klein S, Niswender K, Woo V, Hale PM, Aronne L. Weight maintenance and additional weight loss with liraglutide after low-calorie-diet-induced weight loss: The SCALE Maintenance randomized study. Int J Obes. 2013;37(11):1443–1451. doi: 10.1038/ijo.2013.120. [DOI] [PubMed] [Google Scholar]
- 104.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 105.Lee Y, Lingvay I, Szczepaniak LS, Ravazzola M, Orci L, Unger RH. Pancreatic steatosis: harbinger of type 2 diabetes in obese rodents. Int J Obes (Lond) 2010;34(2):396–400. doi: 10.1038/ijo.2009.245. [DOI] [PubMed] [Google Scholar]
- 106.van Raalte DH, van der Zijl NJ, Diamant M. Pancreatic steatosis in humans: cause or marker of lipotoxicity? Curr Opin Clin Nutr Metab Care. 2010;13(4):478–485. doi: 10.1097/MCO.0b013e32833aa1ef. [DOI] [PubMed] [Google Scholar]
- 107.Sattar N, Gill JM. Type 2 diabetes as a disease of ectopic fat? BMC Med. 2014;12(1):123. doi: 10.1186/s12916-014-0123-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Pinnick KE, Collins SC, Londos C, Gauguier D, Clark A, Fielding BA. Pancreatic ectopic fat is characterized by adipocyte infiltration and altered lipid composition. Obesity. 2008;16(3):522–530. doi: 10.1038/oby.2007.110. [DOI] [PubMed] [Google Scholar]
- 109.Smits MM, van Geenen EJ. The clinical significance of pancreatic steatosis. Nat Rev Gastroenterol Hepatol. 2011;8(3):169–177. doi: 10.1038/nrgastro.2011.4. [DOI] [PubMed] [Google Scholar]
- 110.Unger RH, Scherer PE. Gluttony, sloth and the metabolic syndrome: a roadmap to lipotoxicity. Trends Endocrinol Metab. 2010;21(6):345–352. doi: 10.1016/j.tem.2010.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Kusminski CM, Shetty S, Orci L, Unger RH, Scherer PE. Diabetes and apoptosis: lipotoxicity. Apoptosis. 2009;14(12):1484–1495. doi: 10.1007/s10495-009-0352-8. [DOI] [PubMed] [Google Scholar]
- 112.Poitout V, Robertson RP. Glucolipotoxicity: fuel excess and beta-cell dysfunction. Endocr Rev. 2008;29(3):351–366. doi: 10.1210/er.2007-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Lee Y, Hirose H, Ohneda M, Johnson JH, McGarry JD, Unger RH. Beta-cell lipotoxicity in the pathogenesis of non-insulin-dependent diabetes mellitus of obese rats: impairment in adipocyte-beta-cell relationships. Proc Natl Acad Sci U S A. 1994;91(23):10878–10882. doi: 10.1073/pnas.91.23.10878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cnop M. Fatty acids and glucolipotoxicity in the pathogenesis of Type 2 diabetes. Biochem Soc Trans. 2008;36(Pt 3):348–352. doi: 10.1042/BST0360348. [DOI] [PubMed] [Google Scholar]
- 115.Wang CY, Ou HY, Chen MF, Chang TC, Chang CJ. Enigmatic ectopic fat: prevalence of nonalcoholic fatty pancreas disease and its associated factors in a Chinese population. J Am Heart Assoc. 2014;3(1):e000297. doi: 10.1161/JAHA.113.000297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lim S, Bae JH, Chun EJ, Kim H, Kim SY, Kim KM, Choi SH, Park KS, Florez JC, Jang HC. Differences in pancreatic volume, fat content, and fat density measured by multidetector-row computed tomography according to the duration of diabetes. Acta Diabetol. 2014;51(5):739–748. doi: 10.1007/s00592-014-0581-3. [DOI] [PubMed] [Google Scholar]
- 117.Kim SY, Kim H, Cho JY, Lim S, Cha K, Lee KH, Kim YH, Kim JH, Yoon YS, Han HS, Kang HS. Quantitative assessment of pancreatic fat by using unenhanced CT: pathologic correlation and clinical implications. Radiology. 2014;271(1):104–112. doi: 10.1148/radiol.13122883. [DOI] [PubMed] [Google Scholar]
- 118.Macauley M, Percival K, Thelwall PE, Hollingsworth KG, Taylor R. Altered volume, morphology and composition of the pancreas in type 2 diabetes. Plos One. 2015;10(5):e0126825. doi: 10.1371/journal.pone.0126825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ou HY, Wang CY, Yang YC, Chen MF, Chang CJ. The association between nonalcoholic fatty pancreas disease and diabetes. Plos One. 2013;8(5):e62561. doi: 10.1371/journal.pone.0062561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Gaborit B, Abdesselam I, Kober F, Jacquier A, Ronsin O, Emungania O, Lesavre N, Alessi MC, Martin JC, Bernard M, Dutour A. Ectopic fat storage in the pancreas using 1H-MRS: importance of diabetic status and modulation with bariatric surgery-induced weight loss. Int J Obes. 2015;39(3):480–487. doi: 10.1038/ijo.2014.126. [DOI] [PubMed] [Google Scholar]
- 121.Lingvay I, Esser V, Legendre JL, Price AL, Wertz KM, Adams-Huet B, Zhang S, Unger RH, Szczepaniak LS. Noninvasive quantification of pancreatic fat in humans. J Clin Endocrinol Metab. 2009;94(10):4070–4076. doi: 10.1210/jc.2009-0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Steven S, Hollingsworth KG, Small PK, Woodcock SA, Pucci A, Aribisala B, Al-Mrabeh A, Daly AK, Batterham RL, Taylor R. Weight loss decreases excess pancreatic triacylglycerol specifically in type 2 diabetes. Diabetes Care. 2016;39(1):158–165. doi: 10.2337/dc15-0750. [DOI] [PubMed] [Google Scholar]
- 123.Tushuizen ME, Bunck MC, Pouwels PJ, Bontemps S, van Waesberghe JH, Schindhelm RK, Mari A, Heine RJ, Diamant M. Pancreatic fat content and beta-cell function in men with and without type 2 diabetes. Diabetes Care. 2007;30(11):2916–2921. doi: 10.2337/dc07-0326. [DOI] [PubMed] [Google Scholar]
- 124.Heni M, Machann J, Staiger H, Schwenzer NF, Peter A, Schick F, Claussen CD, Stefan N, Häring HU, Fritsche A. Pancreatic fat is negatively associated with insulin secretion in individuals with impaired fasting glucose and/or impaired glucose tolerance: a nuclear magnetic resonance study. Diabetes Metab Res Rev. 2010;26(3):200–205. doi: 10.1002/dmrr.1073. [DOI] [PubMed] [Google Scholar]
- 125.Yokota K, Fukushima M, Takahashi Y, Igaki N, Seino S. Insulin secretion and computed tomography values of the pancreas in the early stage of the development of diabetes. J Diabetes Invest. 2012;3(4):371–376. doi: 10.1111/j.2040-1124.2012.00212.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Szczepaniak LS, Victor RG, Mathur R, Nelson MD, Szczepaniak EW, Tyer N, Chen I, Unger RH, Bergman RN, Lingvay I. Pancreatic steatosis and its relationship to beta-cell dysfunction in humans: racial and ethnic variations. Diabetes Care. 2012;35(11):2377–2383. doi: 10.2337/dc12-0701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Lim EL, Hollingsworth KG, Aribisala BS, Chen MJ, Mathers JC, Taylor R. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia. 2011;54(10):2506–2514. doi: 10.1007/s00125-011-2204-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Honka H, Hannukainen JC, Tarkia M, Karlsson H, Saunavaara V, Salminen P, Soinio M, Mikkola K, Kudomi N, Oikonen V. et al. Pancreatic metabolism, blood flow and beta-cell function in obese humans. J Clin Endocrinol Metab. 2014;99(6):E981–E990. doi: 10.1210/jc.2013-4369. [DOI] [PubMed] [Google Scholar]
- 129.Honka H, Koffert J, Hannukainen JC, Tuulari JJ, Karlsson HK, Immonen H, Oikonen V, Tolvanen T, Soinio M, Salminen P. et al. The Effects of bariatric surgery on pancreatic lipid metabolism and blood flow. J Clin Endocrinol Metab. 2015;100(5):2015–2023. doi: 10.1210/jc.2014-4236. [DOI] [PubMed] [Google Scholar]
- 130.Schwenzer NF, Machann J, Martirosian P, Stefan N, Schraml C, Fritsche A, Claussen CD, Schick F. Quantification of pancreatic lipomatosis and liver steatosis by MRI: comparison of in/opposed-phase and spectral-spatial excitation techniques. Invest Radiol. 2008;43(5):330–337. doi: 10.1097/RLI.0b013e31816a88c6. [DOI] [PubMed] [Google Scholar]
- 131.Saisho Y, Butler AE, Butler PC. Pancreatic fat content and beta-cell function in men with and without type 2 diabetes: response to Tushuizen et al. Diabetes Care. 2008;31(5):e38. doi: 10.2337/dc08-0044. [DOI] [PubMed] [Google Scholar]
- 132.van Geenen EJ, Smits MM, Schreuder TC, van der Peet DL, Bloemena E, Mulder CJ. Nonalcoholic fatty liver disease is related to nonalcoholic fatty pancreas disease. Pancreas. 2010;39(8):1185–1190. doi: 10.1097/MPA.0b013e3181f6fce2. [DOI] [PubMed] [Google Scholar]
- 133.van der Zijl NJ, Goossens GH, Moors CC, van Raalte DH, Muskiet MH, Pouwels PJ, Blaak EE, Diamant M. Ectopic fat storage in the pancreas, liver, and abdominal fat depots: Impact on beta-cell function in individuals with impaired glucose metabolism. J Clin Endocrinol Metab. 2011;96(2):459–467. doi: 10.1210/jc.2010-1722. [DOI] [PubMed] [Google Scholar]
- 134.Wong VW, Wong GL, Yeung DK, Abrigo JM, Kong AP, Chan RS, Chim AM, Shen J, Ho CS, Woo J. et al. Fatty pancreas, insulin resistance, and beta-cell function: a population study using fat-water magnetic resonance imaging. Am J Gastroenterol. 2014;109(4):589–597. doi: 10.1038/ajg.2014.1. [DOI] [PubMed] [Google Scholar]
- 135.Pezzilli R, Calculli L. Pancreatic steatosis: Is it related to either obesity or diabetes mellitus? World J Diabetes. 2014;5(4):415–419. doi: 10.4239/wjd.v5.i4.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Kuhn JP, Berthold F, Mayerle J, Volzke H, Reeder SB, Rathmann W, Lerch MM, Hosten N, Hegenscheid K, Meffert PJ. Pancreatic steatosis demonstrated at MR imaging in the general population: clinical relevance. Radiology. 2015;276(1):129–136. doi: 10.1148/radiol.15140446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Begovatz P, Koliaki C, Weber K, Strassburger K, Nowotny B, Nowotny P, Müssig K, Bunke J, Pacini G, Szendrödi J, Roden M. Pancreatic adipose tissue infiltration, parenchymal steatosis and beta cell function in humans. Diabetologia. 2015;58(7):1646–1655. doi: 10.1007/s00125-015-3544-5. [DOI] [PubMed] [Google Scholar]