Abstract
Introduction:
The concomitance of ipsilateral physeal fractures of the distal femur and the proximal tibia is an extremely scarce entity. It is conceptually similar to floating knee in the pediatric population.
Case Report:
One case with this injury is reported in a 16-year-old teenager. He was treated surgically by close reduction and internal fixation. The diagnosis of the tibial fracture was initially missed, and the fracture was seen on the post-operative radiographs. Orthopedic treatment was made for this injury. 2 years after, no angular deformity neither shortening of the limb were found.
Conclusion:
These rare injuries could have serious immediate and remote complication with a considerable functional impact. The diagnosis of proximal tibia physeal fracture could be missed in the context of a concomitant more impressive distal femur fracture. The possibility of a combination of these two injuries should then be kept in mind. Anatomic reduction should be made as soon as possible using a gentle technique, and attention should be given to the diagnosis of the neurovascular complications.
Keywords: Knee, physeal fracture, operative treatment, infants
What to Learn from this Article?
Take your time in front of X-rays: Impressive limb-threatening fractures could hide discreet but function-threatening ones.
Introduction
Physeal fractures are rarely encountered around the knee [1]. However, they are dangerous in this localization because of the proximity of the arteria poplitea and the risk of premature physeal closure. Physeal fracture of the distal femur and the proximal tibia is scarce for each one apart and is often caused by a high-velocity trauma. The combination of these two injuries is extremely rare. As far as we know, only three papers reported four cases of this entity, called pediatric floating knee [2, 3, 4]. We report a case of ipsilateral physeal fractures of the distal femur and proximal tibia. We focus on the diagnosis difficulties of this lesion and the potential immediate and remote complications.
Case Report
A 16-year-old obese male, with no medical history, presented in emergency room with a closed trauma of the left knee secondary to a traffic accident. He was hit by a car while biking. The mechanism of the injury was a hyperextension and a valgus stress of the left knee. General examination revealed no other significant injury. On physical examination, the patient was totally unable to step on or move his left lower limb. There was a significant swelling around his left knee with no skin defect. The pulses of the arteria poplitea, the arteria tibialis posterior, and the arteria dorsalis pedis were well palpable. The capillary filling of the toes was present. No motor or sensitive defect was found. Plain radiographs of the left knee showed a Salter and Harris type I physeal fracture of the distal femur with an important displacement of the metaphyseal fragment (Fig. 1). At that time, in front of the spectacular femoral injury, the diagnosis of a type III slightly displaced that physeal fracture of the proximal tibia was missed. The patient was operated in the same day. Under general anesthesia, the patient was placed in supine position with the left lower limb pulled in its axis using a fracture table. After a gentle continuous traction, a downward pressure was applied on the distal epiphysis of the femur with the tight been locked. The reduction was found good when checked using the fluoroscopy. Fixation was done using two-crossing 24 mm K-wires. A long leg cast was made. Post-operative radiographs showed a good reduction of the distal femur (Fig. 2). At this time, the tibial injury was diagnosed. The slight displacement of the epiphyseal fragment of distal tibia was accepted. Close physical observation in the first post-operative 24 h found no secondary vascular thrombosis. The cast was kept for 6 weeks. After the same period, healing of the fracture was obtained (Fig. 3), hardware was removed, and full weight bearing was allowed. 2 years later, the patient was pain free, with a complete range of motion of the left knee. No angular deformity or shortening of the left lower limb was noted (Fig. 4).
Figure 1.
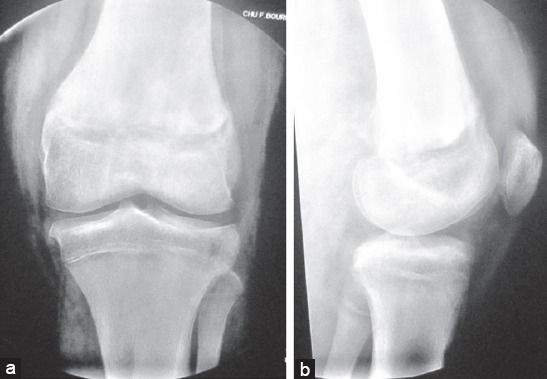
(a and b) Pre-operative plain radiograph of the left knee showing a Salter and Harris type I physeal fracture of the distal femur with an important posterior displacement of the epiphysis together with a displaced type III physeal fracture of the proximal tibia interesting the lateral tibial plateau (1a front view, 1b lateral view)
Figure 2.
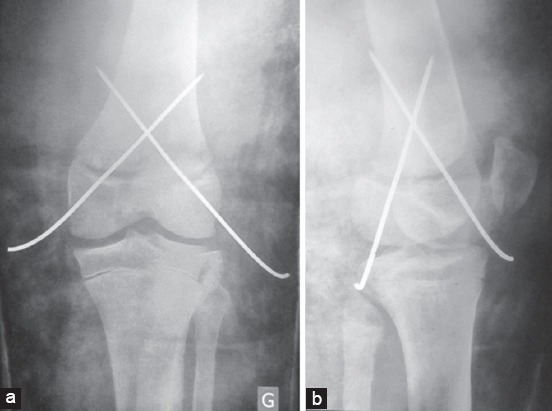
(a and b) Post-operative plain radiograph of the left knee showing a good reduction of the distal femur fracture stabilized using two crossing k-wires and a long leg cast (2a front view, 2b lateral view)
Figure 3.
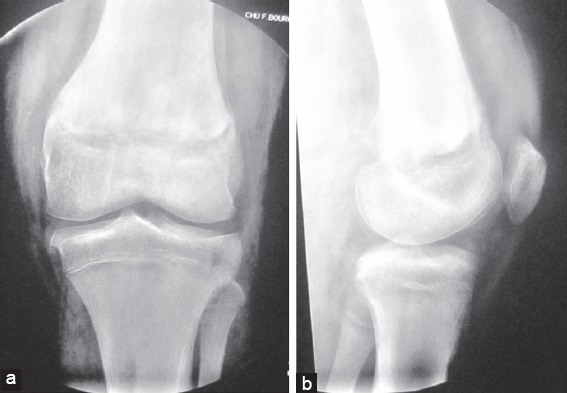
(a and b) Follow-up plain radiograph of the left knee showing the healing of the fractures 6 weeks after the surgery (3a front view, 3b lateral view)
Figure 4.

(a-d) Last follow-up patient photographs showing no angular deformity of the left lower limb (2a and 2b) and a normal range of motion of the left knee (2c and 2d).
Discussion
Epiphyses around the knee are responsible of 65% of the growth of the lower limb, 40% in the distal femur, and 25% in the proximal tibia [4]. Distal femoral epiphysis is seen at birth [4]. The femur then grows intensely in the first 5 years of life. Between the age of five and the puberty, the growth slows down and remains uniform at two centimeters per year, to eventually reach five times the initial length [5]. Proximal tibia epiphysis appears later between the first and the third months of life. It has two ossification centers that fuse at the age of 17 [4]. The proximal tibia has only a few ligamentous attaches and is stabilized laterally by the head of the fibula and medially by the medial collateral ligament and the semimembranosus musculus distal insertion [5].
Physeal fractures of the distal femur and the proximal tibia are rare. They count for less than two percent of all pediatric long-bone fractures [6]. Very few reports describing the concomitant occurrence of these two lesions have been reported [3, 4]. This entity has been called pediatric floating knee. Physeal fractures around the knee are mostly seen after the age of ten [6] and are more often seen in males [5]. Salter and Harris type I and II fractures represent 80% of all physeal fractures in distal femur and 67% in proximal tibia [5].
The most frequent mechanism of physeal fractures of the distal femur is lateral stress (varus or valgus). These injuries could also occur after a hyperextension of the knee leading to posterior displacement of the metaphysic [6]. This is the mechanism seen in the present case. Important displacement could lead to hazardous outstretching or compression of the posterior neurovascular elements. Concerning physeal fractures of the proximal tibia and sport accidents are in cause in the half of cases while high-velocity street accidents are responsible for the other half [5]. Since it has very few ligamentous insertions, the proximal tibia is not exposed to lateral stresses. That explains the scarcity of physeal fractures in this site [4]. Consequently, the mechanism is rather an avulsion in the insertions of ligamentous structures. However, this seems not to be the case in our patient since the detached fragment is anterolateral and there is not any ligamentous insertion in this site. The fracture could result from a violent impact of the lateral femoral condyle on the lateral tibial plateau due to a valgus stress.
The diagnosis of physeal fractures could be problematic in some cases. This concerns mainly non-displaced Salter and Harris type I or II fractures with potential need for dynamic stress radiographs under anesthesia. Nevertheless, the diagnosis of type V fractures is usually made in the stage of late complications [5]. In the present case, the diagnosis of the Salter type III physeal fracture of the proximal tibia was initially missed. Sferopouos [3] reported a similar case where the tibial fracture was diagnosed in the late stage of premature closure of the growth plate eventually leading to a varus deformity. Misdiagnosis could be explained by the concomitance of the impressive limb-threatening femoral injury that retains all the attention. The scarcity of every lesion apart and even more the scarcity of their combination makes this entity poorly known and consequently contributes to the diagnosis delay. In general, undiagnosed physeal fractures of the proximal tibia could endanger the growth prognosis of the tibia with the risks of shortening and angular deformities [7]. However, despite the fact that it protects from severe deformities, even anatomic reduction of these fractures does not guarantee the avoidance of growth disturbance [8]. In the last follow-up, we found none of these complications in our patient. In fact, he was in the end of his growth period, which minimizes the impact of a potential premature closure of the growth plate.
Physeal fractures of the distal femur could be assimilated to knee dislocations when there is an important posterior displacement of the metaphysis like in the present case [5]. While the positive diagnosis of this injury is obvious, the diagnosis of its immediate neurovascular complications remains a challenge. The morbidity associated to these complications is, however, important, and the consequences of a misdiagnosis are limb threatening [9].
In knee injuries with posterior displacement, the arteria poplitea could be damaged. The best strategy for detecting vascular injuries complicating knee injuries is still subject of debate [9]. The findings of physical evaluation and even Doppler sonography could miss latent but serious injuries such as intimal tears of the arteria poplitea with possible subsequent late thrombosis [10]. This is the argument of authors that recommended systematic use of angiography [11]. This method, however, has some risks such as acute renal failure and arteriovenous fistula formation. In addition, its economic cost is important [9]. Sfeir et al. [12] found no superiority of systematic angiography in terms of limb salvage in young patients with otherwise normal arteries. In this situation, ankle-brachial index seems to be a good alternative. It is a safe, simple, and reproducible method with interesting sensitivity and specificity in terms of diagnosis of arterial injuries needing surgery [13]. For the present patient, we preferred not to delay the fracture reduction with the realization of imaging studies since normal pulse was present. However, the pulses were closely observed in the first 24 h to detect signs of secondary thrombosis.
The second limb-threatening complication to look for is fibular nerve palsy. It could have a heavy impact on functional outcome, on neuropathic pain, and eventually on the quality of life. Obese male patients and those having a fracture of the fibular head are more exposed to this complication [14]. Full spontaneous recovery is possible. It is seen in 14 to 56% of cases and is more likely in younger patients [14, 15, 16]. If palsy is found in the first evaluation, fibular nerve should be explored peroperatively in purpose to repair a frank rupture or perform a neurolysis if the nerve appears in continuity.
Gentle anatomic reduction and stable fixation are the principles of the treatment of physeal fractures [8]. Salter and Harris type I and II fractures of the distal femur are extra-articular and therefore may be treated by closed reduction [6]. In the present case, the reduction was made the knee being in extension using a fracture table that allowed progressive traction. A downward pressure was then applied on the epiphyseal fragment to drive it into normal position. Albert and Drvaric [8] described a similar technique without the use of fracture table. We think that it is difficult to realize a continuous progressive traction without the use of this device. The manual traction could lead to multiple attempts which may cause iatrogenic injuries of the growth plate. In their described technique, Albert and Drvaric [8] recommended progressively driving the knee into flexion as a last step of the reduction using the intact anterior periosteum as an internal splint. In the present case, flexion of the knee was not performed. However, a good stable reduction was obtained. We think, therefore, that this step is not always necessary. Nevertheless, hyperflexion could endanger posterior elements in the popliteal fossa [8].
After reduction, the necessity of internal fixation is assessed. The stability of the reduction, the weight, and the corpulence of the child are the factors to consider [6]. In the present case, a crossing k-wire fixation was made to avoid redisplacement of the fracture regarding the obesity of the patient. In other cases, a well-modeled long-leg cast could be enough allowing then to avoid the iatrogenicity of k-wires passing through the growth plate [8].
Conclusion
In summary, physeal fractures around the knee are rare but dangerous injuries that concern the most fertile growth plates of the lower limb. The diagnosis of proximal tibia physeal fracture could be missed in the context of a concomitant more impressive distal femur fracture. The possibility of a combination of these two injuries should then be kept in mind. The potential risks of limb-threatening neurovascular immediate complications and long-term growth disturbance are to be considered, prevented, and eventually treated in an emergency. Finally, follow-up must be carried out up to the end of the growth period.
Clinical Message.
In emergency context, enough time and care should be taken when interpreting radiographs so less impressive, but potentially morbid, injuries are not missed. It should be kept in mind that one train could hide another.
Biography




Footnotes
Conflict of Interest: Nil
Source of Support: None
References
- 1.Mann D, Rajmaira S. Distrubution of physeal and non physeal fractures in 2650 long bone fractures in children aged 0-16 years. J Pediatr Orthop. 1990;10(6):713–716. doi: 10.1097/01241398-199011000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Ng A, Morley JR, Prasad RN, Giannoudis PV, Smith RM. The pediatric floating knee: A case report of ipsilateral epiphyseal injury to the distal femur and proximal tibia. J Pediatr Orthop. 2004;B13(2):110–112. doi: 10.1097/00009957-200403000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Sferopoulos NK. Concomitant physical fracture of the proximal femur and distal tibia. Skeletal Radiol. 2005;34:427–430. doi: 10.1007/s00256-004-0888-1. [DOI] [PubMed] [Google Scholar]
- 4.Gulabi D, Erdem M, Bulut G, Avci CC, Asci M. Ipsilateral distal femoral and proximal tibial epiphyseal growth plate injury: A case report. J Med Case Rep. 2013;7:146. doi: 10.1186/1752-1947-7-146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bérard J, Chotel F, Parot R, Durand JM. Fractures autours du genou chez l’enfant. In: Fontaine C, Vannineuse A, editors. Fractures du Genou. Paris, Berlin, Heidelberg, New York: Springer; 2005. pp. 297–316. [Google Scholar]
- 6.Moran M, Macnicol MF. Paediatric epiphyseal fractures around the knee. Curr Orthop. 2006;20:256–265. [Google Scholar]
- 7.Poulsen TD, Skak SV, Jensen TT. Epiphyseal fractures of the proximal tibia. Injury. 1989;20:111–113. doi: 10.1016/0020-1383(89)90154-x. [DOI] [PubMed] [Google Scholar]
- 8.Albert MJ, Drvaric DM. Reduction and operative fixation of Salter-Harris type II fractures of the distal femur. Oper Tech Orthop. 1995;5(2):145–149. [Google Scholar]
- 9.Medina O, Arom GA, Yeranosian MG, Petrigliano FA, McAllister DR. Vascular and nerve injury after knee dislocation a systematic review. Clin Orthop Relat Res. 2014;472(9):2621–2629. doi: 10.1007/s11999-014-3511-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McDonough EB, Wojtys EM. Multi-ligamentous injuries of the knee and associated vascular injuries. Am J Sports Med. 2009;37(1):156–159. doi: 10.1177/0363546508324313. [DOI] [PubMed] [Google Scholar]
- 11.McCoy GF, Hannon DG, Barr RJ, Templeton J. Vascular injuries associated with low-velocity dislocations of the knee. J Bone Joint Surg Br. 1987;69:285–287. doi: 10.1302/0301-620X.69B2.3818761. [DOI] [PubMed] [Google Scholar]
- 12.Sfeir RE, Koury GS, Haddad FF, Fakih RR, Khalifeh MJ. Injury to the popliteal vessels: The lebanese war experience. World J Surg. 1992;16:1156–1158. doi: 10.1007/BF02067087. [DOI] [PubMed] [Google Scholar]
- 13.Dean EM, Rogers K, Thacker MM, Kruse RW. Inter-observer reliability of the ankle-brachial index in a pediatric setting. Del Med J. 2015;87(3):77–80. [PubMed] [Google Scholar]
- 14.Peskun CJ, Chahal J, Steinfeld ZY, Whelam DB. Risk factors for peroneal nerve injury and recovery in knee dislocation. Clin Orthop Relat Res. 2012;470:774–778. doi: 10.1007/s11999-011-1981-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Plancher KD, Siliski J. Long term functional results and complications in patients with knee dislocations. J Knee Surg. 2008;21:261–268. doi: 10.1055/s-0030-1247829. [DOI] [PubMed] [Google Scholar]
- 16.Meyer MH, Harvey JP. Traumatic dislocation of the knee joint: A study of eighteen cases. J Bone Joint Surg Am. 1975;53:16–29. [PubMed] [Google Scholar]


