Previous studies have shown that cancer awareness and screening rates in Iran did not improve despite of the Comprehensive National Cancer Control Program launched in 2007. To better understand the public's attitude towards cancer, we conducted a general population survey for evaluating public attitudes toward cancer and cancer patients in Isfahan, Iran as the first report in Middle East.
Keywords: Cancer stigma, Disparities, Cancer awareness, Social support, Public education
Abstract
Background.
Because of the significant incidence and mortality of cancer in Iran, a Comprehensive National Cancer Control Program for the prevention and early detection of cancer was launched in 2007. However, cancer awareness and screening rates in Iran did not improve. This study aimed to evaluate public attitudes toward cancer and cancer patients in Iran.
Materials and Methods.
We conducted a cross‐sectional survey among 953 non‐institutionalized individuals in Isfahan, Iran, from November 2014 to February 2015. We collected data on attitudes toward cancer in three domains (impossibility of recovery, cancer stereotypes, and discrimination), as well as questions on willingness to disclose a cancer diagnosis.
Results.
Among all participants, 33.9% agreed that it is very difficult to regain one's health after a cancer diagnosis, 17.4% felt uncomfortable with a cancer patient, and 26.9% said that they would avoid marrying people whose family members had cancer. While 88.9% of study participants said that cancer patients deserve to be protected in society, 53.3% and 48.4% of participants agreed that they would not disclose a cancer diagnosis to neighbors and coworkers, respectively.
Conclusion.
Negative attitudes with respect to impossibility of recovery and discrimination toward cancer and cancer patients were common among urban Iranians. Most people would not disclose a cancer diagnosis to others in spite of advancements in cancer diagnosis and treatment, reflecting unfavorable attitudes toward cancer and cancer patients in society. Successful implementation of cancer awareness and prevention programs in Iran may require social changes based on adequate information on cancer and cancer patients.
Implications for Practice.
Public attitudes toward cancer and cancer patients are an important factor affecting cancer control programs as well as quality of life and recovery of cancer patients. The issue has not been studied in Iran and the surrounding countries in the Middle East. This is the first report presented on the subject. These findings can be used by health policy makers, health managers, and clinicians for better practice.
Introduction
Cancer is a leading cause of death and burden of disease worldwide [1]. Despite advances in early detection and treatment, a cancer diagnosis is often considered a death sentence, and negative images and myths regarding cancer persist [2], [3], [4]. Cancer patients frequently do not disclose their diagnosis to avoid discrimination or problems at home, in the workplace, or in society in general [5], [6], [7], [8], [9], [10], [11]. Furthermore, general population surveys show that a substantial proportion of people feel uncomfortable in the presence of cancer patients and tend to avoid interacting or working with them [12]. Discriminatory behavior toward cancer may alienate patients from their community [13], [14], complicate returning to work after treatment [5], [6], [7], and have adverse physical and mental health consequences for cancer survivors [10], [15], [16], [17].
Cancer is the third leading cause of death in Iran [18], with annual incidence rates of 120.1 and 134.7 per 100,000 in women and men, respectively, and annual mortality rates of 41.2 and 60 per 100,000 in women and men, respectively [19]. Although more than 90% of Iranian people have health insurance coverage, cancer care is assumed by patients to be costly for them due to copayments at time of service [20]. However, access to cancer care centers is possible for most cancer patients and they are mostly satisfied by the provided services [20].
In response to the high incidence and mortality of cancer in Iran, Iran's Ministry of Health launched the Comprehensive National Cancer Control Program in 2007 [21], which included programs for prevention and early detection such as pilot screening programs for breast, colorectal, prostate, and bladder cancers [21]. Cancer awareness and screening rates in Iran, however, did not improve [22], [23], [24], partly due to limited strategies for primary prevention, lack of support from senior managers, and financial burden associated with the program [21], [22], [25]. Misinformation about cancer screening, negative attitudes toward cancer, lack of health seeking behaviors, and cultural taboos were also found to be a barrier to cancer control in Iran [25], [26]. Nevertheless, most of these studies were qualitative with highly selected samples of cancer patients. To better understand the public's attitude toward cancer, we conducted a general population survey for evaluating public attitudes toward cancer and cancer patients in Isfahan, Iran.
Materials and Methods
Study Population
We conducted a cross‐sectional survey of the non‐institutionalized population in Isfahan, central Iran, from November 2014 to February 2015. In order to recruit participants across all city districts, we recruited study participants in three main areas of Isfahan where main squares and transportation pathways leading to different areas of the city converge. Trained researchers approached people passing through the areas and explained the study. Once a person agreed to participate in the study, he or she was asked to complete a survey questionnaire. During the study period, 1,300 men and women were approached and 1,164 (89.5%) agreed to participate in the study. We excluded participants who did not provide information on age and gender (n = 83), who were less than 18 years old (n = 95), who had had cancer (n = 9), and who lived in rural areas (n = 24). The final sample included 953 participants. This study was approved by the regional bioethics committee of Isfahan University of Medical Sciences and verbal informed consent was obtained from all study participants.
Data Collection
We assessed attitudes toward cancer and cancer patients using the questionnaire developed by Cho et al. [12], which consists of 12 items in three domains: (a) impossibility of recovery; (b) stereotypes; and (c) discrimination. Prior to the actual survey, we performed translation and back‐translation, content validation, expert review, and a pilot study of the questionnaire. All questions were asked using a four‐point Likert scale ranging from 1 (strongly disagree) to 4 (strongly agree). Internal consistency of the questionnaire items in the study sample was satisfactory, with Cronbach's alpha coefficients for impossibility of recovery, stereotypes, and discrimination of 0.67, 0.38, and 0.66, respectively.
In addition, we measured the willingness to disclose a cancer diagnosis by asking individuals whether they would divulge their diagnosis to families, friends, neighbors, and coworkers if they had cancer. Response choices were assigned a numeric score from 1 (strongly disagree) to 4 (strongly agree). Higher scores represented decreased willingness to disclose a cancer diagnosis.
We also collected data regarding factors associated with attitudes toward cancer or other stigmatized diseases or conditions identified in previous studies, including gender, age, family history of cancer, marital status, education, employment, average family income, insurance type, smoking status, and perceived health status [12].
Statistical Analysis
Impossibility of recovery, stereotypes, and discrimination toward cancer patients were dichotomized at their median values. Participants who reported scores at or above median values for each of the three domains were considered to have negative attitudes toward cancer (impossibility of recovery, stereotypes, and discrimination). We then used multivariate logistic regression models to identify the factors associated with the presence of negative attitudes. All statistical analyses were performed using STATA 12.0 (StataCorp LLC, College Station, TX, http://www.stata.com). We considered the results as statistically significant if p < .05.
Results
Characteristics of Participants
The average age (standard deviation) of study participants was 33.8 (11.7) years, 74.7% of participants were female, and 59.3% were married. One third of participants had at least one family member with cancer (Table 1). In terms of education, 14.2% of participants had less than a middle school education, 23.2% had a high school education, 59.6% were college or university graduates, and 3.0% had a higher than graduate school education. About half of participants (50.9%) were currently employed, 57.4% reported monthly incomes below 15 million Iranian Rials (∼U.S. $500), and 10.5% had no health insurance. The majority of participants were nonsmokers (93.4%) and perceived their health status as good (74.9%).
Table 1. Characteristics of study participants (n = 953).
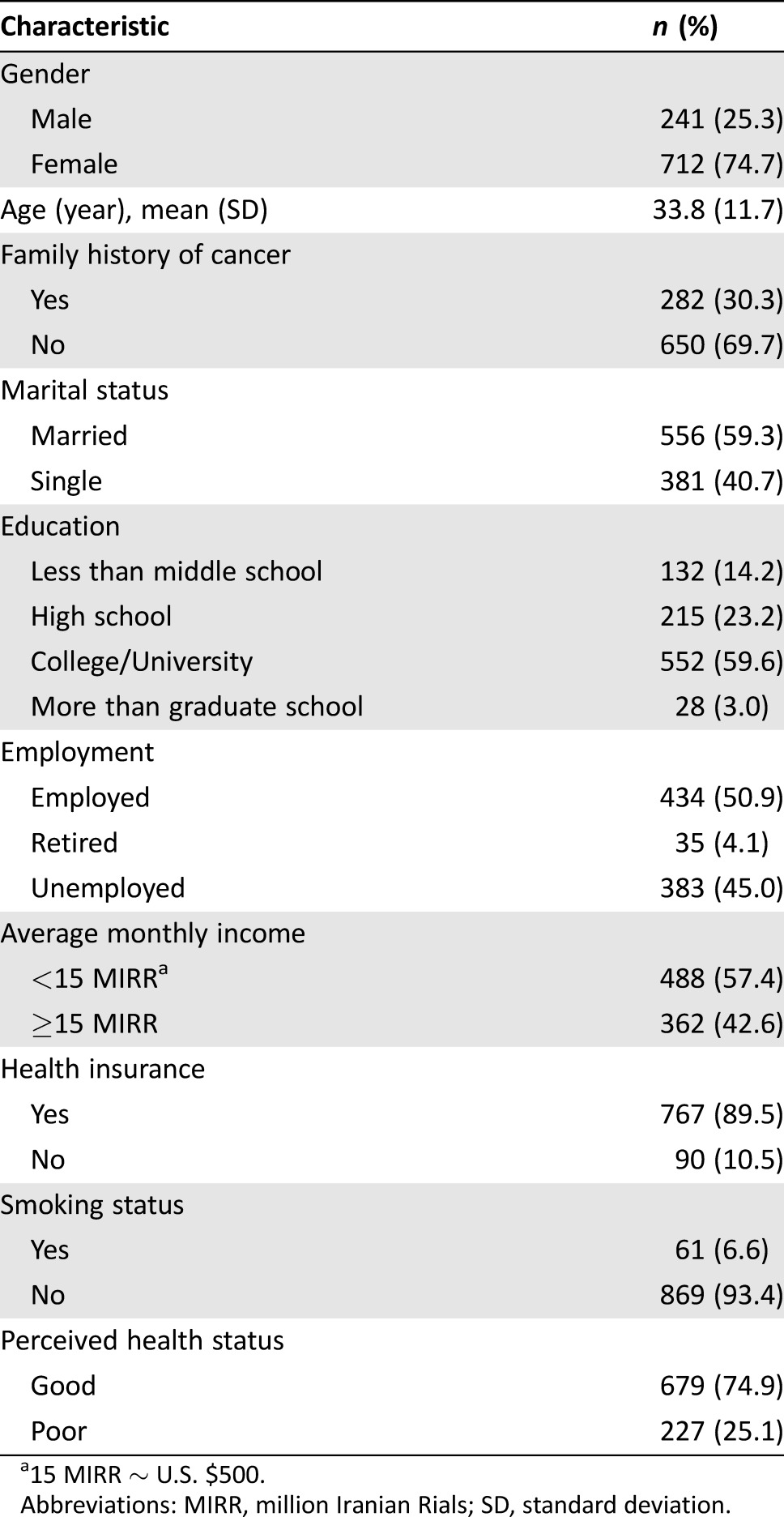
15 MIRR ∼ U.S. $500.
Abbreviations: MIRR, million Iranian Rials; SD, standard deviation.
Attitudes Toward Cancer and Cancer Patients
The percentage of participants who agreed or strongly agreed that it is impossible to treat cancer regardless of highly developed medical science was 19.5%. About one third (33.9%) of participants agreed or strongly agreed that it is very difficult to regain health after a cancer diagnosis, and 37.1% of participants agreed or strongly agreed that workplace task ability of cancer patients may decrease even after successful treatment (Table 2).
Table 2. Attitudes toward cancer and cancer patients (n = 953).
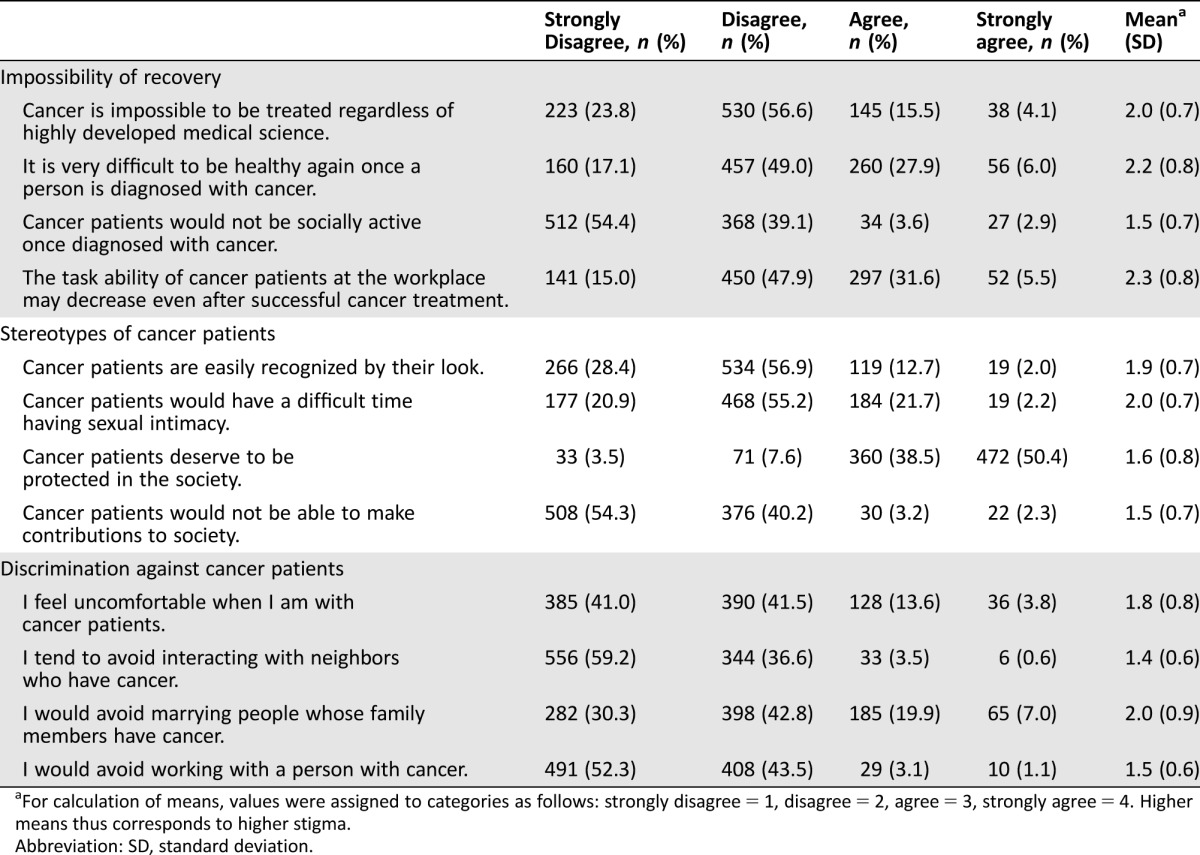
For calculation of means, values were assigned to categories as follows: strongly disagree = 1, disagree = 2, agree = 3, strongly agree = 4. Higher means thus corresponds to higher stigma.
Abbreviation: SD, standard deviation.
With respect to stereotypes, 14.7% of participants agreed or strongly agreed that cancer patients could be easily recognized by looking at them, 23.9% agreed or strongly agreed that cancer patients would have a difficult time being sexually intimate, and 5.5% agreed or strongly agreed that cancer patients would not be able to make contributions to society. However, 88.9% agreed or strongly agreed that cancer patients deserve to be protected in society (Table 2).
With respect to discrimination, 17.4% of participants agreed or strongly agreed that they felt uncomfortable with cancer patients, 4.1% reported that they tended to avoid interacting with neighbors who had cancer, 26.9% would avoid marrying people whose family members had cancer, and 4.2% would avoid working with individuals with cancer (Table 2).
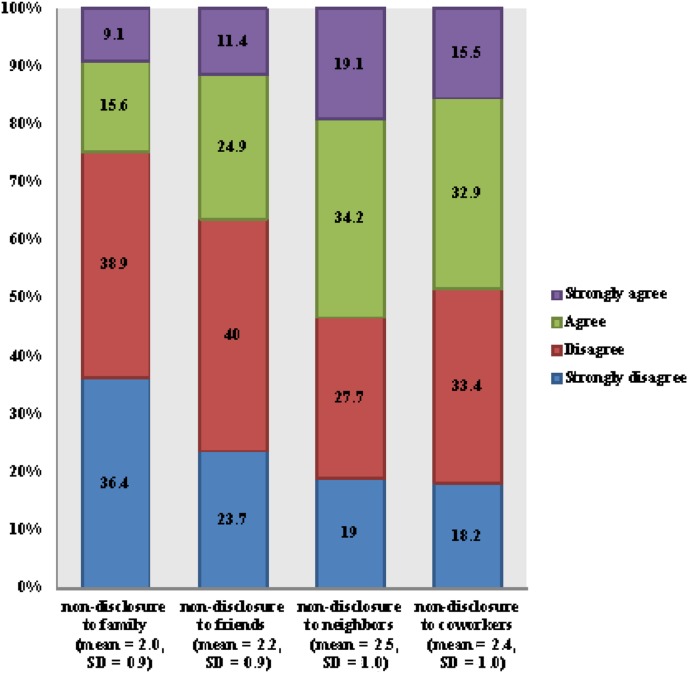
Willingness to Disclose a Cancer Diagnosis
Among all participants, 24.7% agreed or strongly agreed that they would not disclose a cancer diagnosis to family members, 36.3% would not disclose it to friends, 55.3% would not disclose it to neighbors, and 48.4% would not disclose it to coworkers (Fig. 1).
Figure 1.
Willingness to disclose a cancer diagnosis (n = 953). Categories higher in each bar graph represent lower willingness to disclose cancer diagnosis. For calculation of means, values were assigned to categories as follows: strongly disagree = 1, disagree = 2, agree = 3, strongly agree = 4. Higher means thus corresponds to higher stigma.
Abbreviation: SD, standard deviation.
Factors Associated with Attitudes Toward Cancer and Cancer Patients
Compared with women, male participants were more likely to have negative attitudes with respect to discrimination (odds ratio [OR] 1.65, 95% confidence interval [CI] 1.15–2.37), adjusting for age, family history of cancer, marital status, education, employment, and perceived health status (Table 3). People who were 50 years of age or older were less likely to have negative attitudes with respect to impossibility of recovery (OR 0.48, 95% CI 0.29–0.79) than people younger than 50 years old, and participants who had a family history of cancer were less likely to have negative attitudes with respect to discrimination (OR 0.69, 95% CI 0.50–0.96) than participants without family history of cancer. In relation to socioeconomic status, participants who were single were more likely to have negative stereotypes of cancer patients (OR 1.47, 95% CI 1.06–2.02) than married participants, and those with high school (OR 0.41, 95% CI 0.24–0.69) and more than college education (OR 0.38, 95% CI 0.24–0.63) were less likely to hold stereotypical views of cancer patients compared with participants with less than middle school studies.
Table 3. Factors associated with public attitudes toward cancer (n = 953).
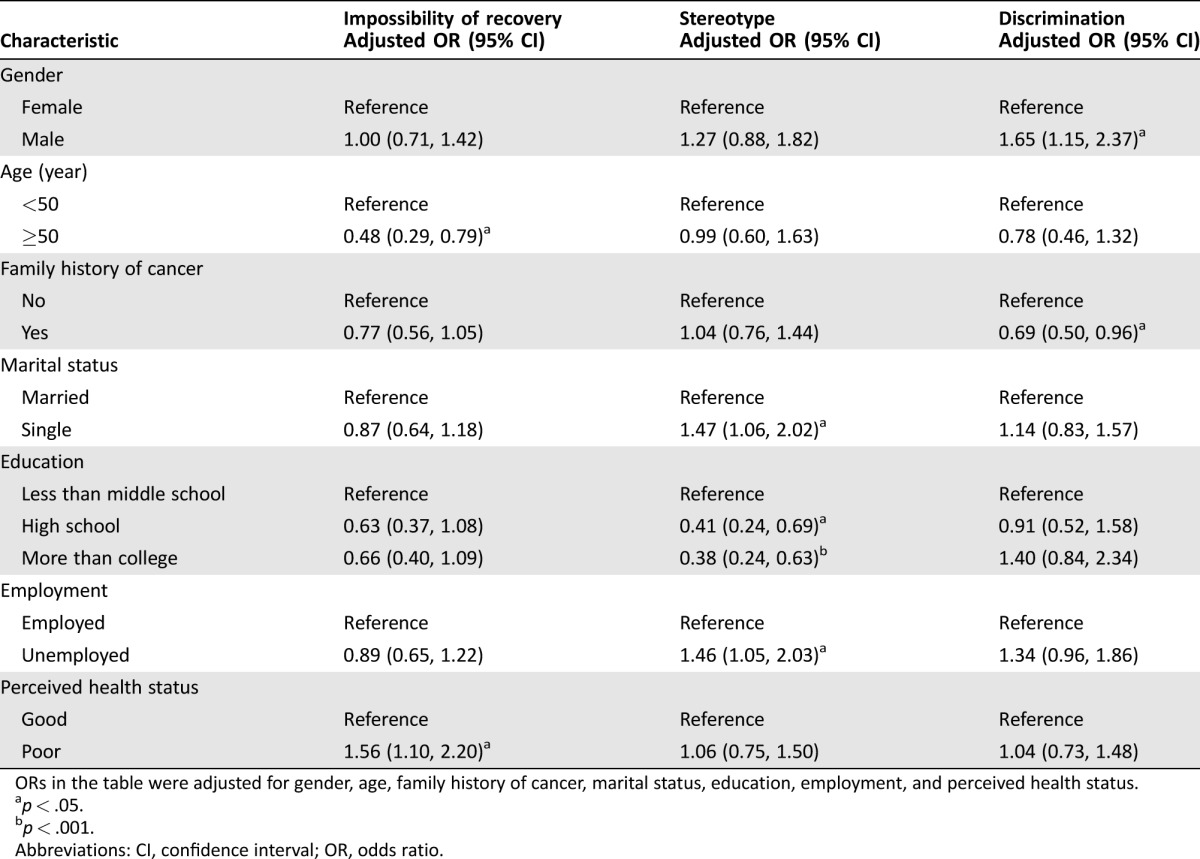
ORs in the table were adjusted for gender, age, family history of cancer, marital status, education, employment, and perceived health status.
p < .05.
p < .001.
Abbreviations: CI, confidence interval; OR, odds ratio.
Unemployed participants were more likely to have negative attitudes toward cancer with respect to discrimination (OR 1.46, 95% CI 1.05–2.03) compared with employed participants. Participants who reported poor health status were more likely to have negative attitudes toward impossibility of recovery compared with participants who reported good health status (OR 1.56, 95% CI 1.10–2.20).
Discussion
In this survey conducted among urban Iranians, negative attitudes with respect to impossibility of recovery from cancer and discrimination toward cancer patients were common. Although most study participants said that cancer patients deserve protection in society, one fourth and more than half of participants agreed or strongly agreed that they would not disclose a cancer diagnosis to family and neighbors, respectively, reflecting an unfavorable culture toward cancer patients.
In our study, about 20% of participants believed that it is impossible to treat cancer effectively, and about one third believed that it is very difficult for cancer patients to regain their health. While direct comparisons with other studies are not possible due to differences in design and study population, this is somewhat lower than results previously reported in Iran. In qualitative studies, Iranian women did not attend cervical cancer screening [27], and breast cancer patients delayed seeking treatment [28] because they believed it was impossible to treat cancer. Moreover, a study evaluating Iranian women's beliefs about breast cancer showed that many of them considered the disease incurable [29]. A similar quantitative survey in a representative sample in Korea [12] found that over 50% of participants believed that cancer was impossible to treat or that it is very difficult for a cancer patient to regain their health, and a recent qualitative study in the U.K. found that despite recognizing improvements in outcomes, visceral fear of cancer was ubiquitous and people had difficulties controlling negative thoughts related to cancer [30]. The more favorable attitudes toward cancer recovery in our study might be due to recent cancer awareness and screening programs in Iran, which have been heavily focused on urban areas [21]. Interestingly, younger people had negative attitudes regarding the impossibility of recovery. This may be due to negative attention in Iranian media concerning the occurrence and mortality of cancer, which has been described as a “cancer tsunami” in Iran [31]. Younger people may be more likely to be exposed to health‐related social media and more affected by negative media reports on cancer [32].
About 15% and 25% of participants in our study agreed that it is easy to recognize cancer patients by their appearance and that cancer patients would have a difficult time engaging in sexual intimacy, respectively. In a similar study in Korea, 35% of participants agreed that it is easy to recognize cancer patients by their appearance, and 51% agreed that cancer patients would have a difficult time engaging in sexual intimacy [12]. In a qualitative study in England, most participants held stereotypes of patients with cancer as frail and emaciated [30]. Similar findings have also been reported among cancer survivors of ethnic minorities in the U.S., such as in the black community, where lack of social support and stigmatizing behavior are common [33], [34]. Even among health care professionals, negative cancer stereotypes are still dominant regardless of medical advances and increased survival rates [35].
The lower proportion of participants with negative stereotypes toward cancer patients in our study compared with other studies may be explained because participants in our study were relatively young and educated adults residing in an urban area. In addition, the differences may be related to lifestyle and cultural factors. In Iran, it is not easy to observe the altered appearance of cancer patients in public places, as individuals with disability and sick people often remain at home [36], [37]. Several factors, including lack of rehabilitation services and lack of education on this issue, may contribute to the decision of disabled and sick patients to stay at home [36], [37]. On the other hand, it is possible that strong spirituality and religious beliefs may make Iranians better able to cope with disease and have a more positive attitude [38], [39].
Most participants in our study said that cancer patients deserve to be protected in society. However, about one fifth stated that they feel uncomfortable in the presence of cancer patients, and more than half said that they would not disclose a diagnosis of cancer to neighbors. These attitudes likely result from inadequate social support for cancer patients, and urban Iranians may conceal a cancer diagnosis to avoid unreasonable sympathy, pity, or differential treatment in the community and workplace [9], [11], [12], [40]. Our findings reflect a gap between people's protective attitudes toward cancer patients and actual discrimination in society. However, there is limited research regarding social support or cancer stigma in this region, and further studies are necessary considering the high incidence of cancer.
We also found that one fourth and one third of study participants would not disclose a cancer diagnosis to their family and friends, respectively. Considering that Iranian people tend to feel high levels of intimacy with family members and friends [41], these are quite high proportions. In the past, a cancer diagnosis was equaled to a death sentence [42], but recent advances in cancer diagnosis and treatment, as well as cancer awareness projects, have rendered the disease a more ordinary condition among people [43]. Yet, in Iran, negative perceptions regarding cancer seem to persist and, as a consequence, patients tend to hide their disease and avoid publicizing it [44]. It is important to identify specific barriers to the disclosure of cancer diagnoses and to develop interventions to assist individuals in overcoming these barriers, as these factors could affect quality of life, timely treatment, and adequate support from the workplace and society.
This study has several limitations. First, we recruited study participants from a single urban area of Iran. Therefore, these findings may not be generalizable to other parts of the country, which may have different attitudes toward cancer. Second, we did not use a formal sampling process, and individuals with more positive attitudes and openness to cancer may have been more likely to participate in the survey. Third, answers to our survey may be influenced by social desirability, leading to bias in our results. In spite of these limitations, our findings are consistent with the results of previous studies in other countries, indicating that negative stereotypes and discriminatory attitudes toward cancer are common. Further studies with larger and more representative samples are needed to extend our findings to other areas of the country.
Conclusion
This is the first study to examine public attitudes toward cancer and cancer patients in the Middle East region. We found that urban Iranians frequently had discriminatory attitudes toward cancer patients and negative attitudes toward their possibility of recovery. Although Iranians considered cancer patients as a vulnerable population that needs to be protected, they tend to not like to disclose a cancer diagnosis to relatives, neighbors, friends, or coworkers, suggesting the necessity of public education about cancer and cancer patients. Public education should also be focused on myths about cancer, such as impossibility of recovery, and fear of the disease. In addition, people living with cancer should be encouraged to share their experiences with other people in society. Successful implementation of cancer awareness and prevention programs in Iran may require social changes based on adequate information on cancer and cancer patients.
Acknowledgments
We want to thank Dr. Niloufar Razavi and Dr. Fereshteh Tavakoli for their kind help in conducting the project.
Footnotes
For Further Reading: Pooja Yerramilli, Otgonduya Dugee, Palam Enkhtuya et al. Exploring Knowledge, Attitudes, and Practices Related to Breast and Cervical Cancers in Mongolia: A National Population‐Based Survey. The Oncologist 2015;20:1266‐1273.
Implications for Practice: The rising burden of breast and cervical cancers, particularly in low‐ and middle‐income countries, necessitates the development of effective strategies for cancer control. This paper examines barriers to health service use in Mongolia, a country with a high cancer burden. The 2010 national knowledge, attitude and practices survey data indicate that cancer control efforts should focus on improving health education among lower‐educated, rural, and unemployed populations, who display the least knowledge of breast and cervical cancers. Moreover, the findings support the need to emphasize individual risk for disease in cancer education and ensure that the health‐care infrastructure reflectsMongolia's urbanization.
Author Contributions
Conception/design: Shervin Badihian, Eun‐Kyung Choi, Eliseo Guallar, Juhee Cho
Provision of study material or patients: Shervin Badihian, Eun‐Kyung Choi, Im‐Ryung Kim, Aidin Parnia, Navid Manouchehri, Negin Badihian
Collection and/or assembly of data: Shervin Badihian, Eun‐Kyung Choi, Im‐Ryung Kim, Aidin Parnia, Navid Manouchehri, Negin Badihian
Data analysis and interpretation: Shervin Badihian, Eun‐Kyung Choi, Im‐Ryung Kim, Aidin Parnia, Navid Manouchehri, Negin Badihian, Jila M. Tanha, Eliseo Guallar, Juhee Cho
Manuscript writing: Shervin Badihian, Eun‐Kyung Choi, Im‐Ryung Kim, Aidin Parnia, Navid Manouchehri, Negin Badihian, Jila M. Tanha, Eliseo Guallar, Juhee Cho
Final approval of manuscript: Shervin Badihian, Eun‐Kyung Choi, Im‐Ryung Kim, Aidin Parnia, Navid Manouchehri, Negin Badihian, Jila M. Tanha, Eliseo Guallar, Juhee Cho
Disclosures
The authors indicated no financial relationships.
References
- 1. Jemal A, Bray F, Center MM et al. Global cancer statistics. CA Cancer J Clin 2011;61:69–90. [DOI] [PubMed] [Google Scholar]
- 2. Rosman S. Cancer and stigma: Experience of patients with chemotherapy‐induced alopecia. Patient Educ Couns 2004;52:333–339. [DOI] [PubMed] [Google Scholar]
- 3. Penson RT, Schapira L, Daniels KJ et al. Cancer as metaphor. The Oncologist 2004;9:708–716. [DOI] [PubMed] [Google Scholar]
- 4. Vrinten C, van Jaarsveld CH, Waller J et al. The structure and demographic correlates of cancer fear. BMC Cancer 2014;14:597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ahn E, Cho J, Shin DW et al. Impact of breast cancer diagnosis and treatment on work‐related life and factors affecting them. Breast Cancer Res Treat 2009;116:609–616. [DOI] [PubMed] [Google Scholar]
- 6. Kennedy F, Haslam C, Munir F et al. Returning to work following cancer: A qualitative exploratory study into the experience of returning to work following cancer. Eur J Cancer Care (Engl) 2007;16:17–25. [DOI] [PubMed] [Google Scholar]
- 7. Lee MK, Lee KM, Bae JM et al. Employment status and work‐related difficulties in stomach cancer survivors compared with the general population. Br J Cancer 2008;98:708–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Oksüzoğlu B, Abali H, Bakar M et al. Disclosure of cancer diagnosis to patients and their relatives in Turkey: Views of accompanying persons and influential factors in reaching those views. Tumori 2006;92:62–66. [DOI] [PubMed] [Google Scholar]
- 9. Walters KA. Stigma, shame, and blame experienced by patients with lung cancer: Non‐smoker status should also be declared. BMJ 2004;329:403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Eldeek B, Alahmadi J, Al‐Attas M et al. Knowledge, perception, and attitudes about cancer and its treatment among healthy relatives of cancer patients: Single institution hospital‐based study in Saudi Arabia. J Cancer Educ 2014;29:772–780. [DOI] [PubMed] [Google Scholar]
- 11. Hilton S, Emslie C, Hunt K et al. Disclosing a cancer diagnosis to friends and family: A gendered analysis of young men's and women's experiences. Qual Health Res 2009;19:744–754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cho J, Smith K, Choi EK et al. Public attitudes toward cancer and cancer patients: A national survey in Korea. Psychooncology 2013;22:605–613. [DOI] [PubMed] [Google Scholar]
- 13. Park JH, Park EC, Park JH et al. Job loss and re‐employment of cancer patients in Korean employees: A nationwide retrospective cohort study. J Clin Oncol 2008;26:1302–1309. [DOI] [PubMed] [Google Scholar]
- 14. Greene K, Banerjee SC. Disease‐related stigma: Comparing predictors of AIDS and cancer stigma. J Homosex 2006;50:185–209. [DOI] [PubMed] [Google Scholar]
- 15. Chapple A, Ziebland S, McPherson A. Stigma, shame, and blame experienced by patients with lung cancer: Qualitative study. BMJ 2004;328:1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Else‐Quest NM, LoConte NK, Schiller JH et al. Perceived stigma, self‐blame, and adjustment among lung, breast and prostate cancer patients. Psychol Health 2009;24:949–964. [DOI] [PubMed] [Google Scholar]
- 17. Hamilton JB, Moore CE, Powe BD et al. Perceptions of support among older African American cancer survivors. Oncol Nurs Forum 2010;37:484–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Saadat S, Yousefifard M, Asady H et al. The most important causes of death in Iranian population; A retrospective cohort study. Emerg (Tehran) 2015;3:16–21. [PMC free article] [PubMed] [Google Scholar]
- 19. Ferlay J, Soerjomataram I, Dikshit R et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 2015;136:E359–E386. [DOI] [PubMed] [Google Scholar]
- 20. Moradian S, Aledavood SA, Tabatabaee A. Iranian cancer patients and their perspectives: A qualitative study. Eur J Cancer Care 2012;21:377–383. [DOI] [PubMed] [Google Scholar]
- 21. Mousavi SM, Alamolhoda AA, Gouya MM et al. Implementation of Comprehensive National Cancer Control Program in Iran: An experience in a developing country. Annals of Oncology 2008;19:398–400. [DOI] [PubMed] [Google Scholar]
- 22. Babu GR, Samari G, Cohen SP et al. Breast cancer screening among females in Iran and recommendations for improved practice: A review. Asian Pac J Cancer Prev 2011;12:1647–1655. [PubMed] [Google Scholar]
- 23. Harirchi I, Kolahdoozan S, Karbakhsh M et al. Twenty years of breast cancer in Iran: Downstaging without a formal screening program. Ann Oncol 2011;22:93–97. [DOI] [PubMed] [Google Scholar]
- 24. Montazeri A, Vahdaninia M, Harirchi I et al. Breast cancer in Iran: Need for greater women awareness of warning signs and effective screening methods. Asia Pac Fam Med 2008;7:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lamyian M, Hydarnia A, Ahmadi F et al. Barriers to and factors facilitating breast cancer screening among Iranian women: A qualitative study. East Mediterr Health J 2007;13:1160–1169. [DOI] [PubMed] [Google Scholar]
- 26. Nasrabadi AN, Bahabadi AH, Hashemi F et al. Views of Iranian patients on life with cancer: A phenomenological study. Nurs Health Sci 2011;13:216–220. [DOI] [PubMed] [Google Scholar]
- 27. Bayrami R, Taghipour A, Ebrahimipour H. Personal and socio‐cultural barriers to cervical cancer screening in Iran, patient and provider perceptions: A qualitative study. Asian Pac J Cancer Prev 2015;16:3729–3734. [DOI] [PubMed] [Google Scholar]
- 28. Rastad H, Khanjani N, Khandani BK. Causes of delay in seeking treatment in patients with breast cancer in Iran: A qualitative content analysis study. Asian Pac J Cancer Prev 2012;13:4511–4515. [DOI] [PubMed] [Google Scholar]
- 29. Vahabi M. Iranian women's perception and beliefs about breast cancer. Health Care Women Int 2010;31:817–830. [DOI] [PubMed] [Google Scholar]
- 30. Robb KA, Simon AE, Miles A et al. Public perceptions of cancer: A qualitative study of the balance of positive and negative beliefs. BMJ Open 2014;4:e005434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Iranian deaths prompt ‘cancer tsunami’ fears. BBC News. 2014. http://www.bbc.co.uk/programmes/p02dws56. Accessed April 23, 2017.
- 32. Thackeray R, Crookston BT, West JH. Correlates of health‐related social media use among adults. J Med Internet Res 2013;15:e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Aziz NM, Rowland JH. Cancer survivorship research among ethnic minority and medically underserved groups. Oncol Nurs Forum 2002;29:789–801. [DOI] [PubMed] [Google Scholar]
- 34. Dein S. Explanatory models of and attitudes towards cancer in different cultures. Lancet Oncol 2004;5:119–124. [DOI] [PubMed] [Google Scholar]
- 35. Simon AE, Wardle J, Miles A. Is it time to change the stereotype of cancer: The expert view. Cancer Causes Control 2011;22:135–140. [DOI] [PubMed] [Google Scholar]
- 36. Chanzanagh HE, Piri A, Garjan EA. The disabled and their everyday life experiences in Iranian culture. Int J Soc Sci Hum Stud 2012;4:175–184. [Google Scholar]
- 37. Abdi K, Arab M, Rashidian A et al. Exploring barriers of the health system to rehabilitation services for people with disabilities in Iran: A qualitative study. Electron Physician 2015;7:1476–1485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Taleghani F, Yekta ZP, Nasrabadi AN. Coping with breast cancer in newly diagnosed Iranian women. J Adv Nurs 2006;54:265–272. [DOI] [PubMed] [Google Scholar]
- 39. Baljani E, Khashabi J, Amanpour E et al. Relationship between spiritual well‐being, religion, and hope among patients with cancer. J Hayat 2011;17:27–37. [Google Scholar]
- 40. Kagawa‐ Singer M, Dadia AV, Yu MC et al. Cancer, culture, and health disparities: Time to chart a new course? CA Cancer J Clin 2010;60:12–39. [DOI] [PubMed] [Google Scholar]
- 41. Javidan M, Dastmalchian A. Culture and leadership in Iran: The land of individual achievers, strong family ties, and powerful elite. Acad Manag Exec 2003;17:127–142. [Google Scholar]
- 42. Khan NF, Harrison S, Rose PW et al. Interpretation and acceptance of the term ‘cancer survivor’: A United Kingdom‐based qualitative study. Eur J Cancer Care (Engl) 2012;21:177–186. [DOI] [PubMed] [Google Scholar]
- 43. Kagawa‐Singer M, Padilla GV, Ashing‐Giwa K. Health‐related quality of life and culture. Semin Oncol Nurs 2010;26:59–67. [DOI] [PubMed] [Google Scholar]
- 44. Mellette SJ. The cancer patient at work. CA Cancer J Clin 1985;35:360–373. [DOI] [PubMed] [Google Scholar]