Abstract
We introduce a mixed-methods approach for determining how people weigh tradeoffs in values related to health and technologies for health self-management. Our approach combines interviews with Q-methodology, a method from psychology uniquely suited to quantifying opinions. We derive the framework for structured data collection and analysis for the Q-methodology from theories of self-management of chronic illness and technology adoption. To illustrate the power of this new approach, we used it in a field study of nine older adults with type 2 diabetes, and nine mothers of children with asthma. Our mixed-methods approach provides three key advantages for health design science in HCI: (1) it provides a structured health sciences theoretical framework to guide data collection and analysis; (2) it enhances the coding of unstructured data with statistical patterns of polarizing and consensus views; and (3) it empowers participants to actively weigh competing values that are most personally significant to them.
Author Keywords: Design methodology, Q-methodology, Health attitudes, Technology adoption, Mixed-methods, Health Informatics
ACM Classification Keywords: H.5.2 [Information interfaces and presentation]: User interfaces—evaluation/methodology, theory and methods, user-centered design
INTRODUCTION
Personal health technologies are designed to support people to attain personally significant health goals, such as staying fit, aging in place, and managing chronic diseases. However, it is challenging for designers to support personal health goals with new technologies because, unlike objectively measured productivity goals, health goals are highly subjective, contextual, and situated within competing values. For designers of personal health technologies, it is critical to understand people’s subjective perspectives that are likely to influence health goals and subsequent behaviors, such as attitudes toward personal accountability, health information use, and technology adoption in the context of health self-management.
Current HCI and social scientific methods for gathering subjective perspectives to inform the design of personal health technologies include interviews, focus groups, attitude measurement scales, and participatory design techniques. However, these methods are not always optimal for gathering highly structured data for understanding design tradeoffs based on how individuals weigh and compare the relative value of health information and technology to attain health goals.
We introduce a mixed-methods approach that combines ethnographic interviews with Q-methodology [21], a quantitative technique for finding clusters of subjective perspectives distinguished by polarizing opinions. We followed each in-depth interview with the Q-methodology procedure wherein participants chose how to normally distribute a set of statements about health and technology. This structured data collection method empowered participants by allowing them to weigh the statements most closely aligned with their personal beliefs, and to guide the discussion in explaining their health beliefs and attitudes with the interviewer. The relative ranking of subjective statements about health within a forced distribution forms the foundation of our mixed-methods approach. The quantitative analysis techniques of Q-methodology provided statistical patterns of statement rankings that we applied to thematic analysis of the ethnographic interviews. Thus our approach enhances qualitative data analysis with powerful statistical techniques for the purposes of creating a rich, holistic picture of polarizing and consensus health and technology attitudes.
We leveraged Q-methodology specifically for personal health technology design in HCI in the following three ways: (1) to discover how patients understand, value, and relate concepts from health sciences theories; (2) to provide structure for qualitative data analysis that enhances subjective coding of unstructured data with statistically significant patterns of polarizing and consensus attitudes; and (3) to provide opportunity for participants to take control and actively define and prioritize the health and technology values that are most significant to them.
We demonstrate the use of our mixed-methods approach in an ethnographic study of attitudes toward self-management of chronic diseases. In this study, we conducted 18 in-home interviews using Q-methodology: 9 with older adults with diabetes, and 9 with mothers of children with asthma. Using Q-methodology to structure the data collection and analysis of interviews, we observed and quantified how people prioritize competing values related to accountability, information, and technology for personal health care. We also identified and probed apparent contradictions in beliefs that can influence health behaviors and technology adoption. We demonstrate how these insights are unique to our mixed-methods approach, and how they are applicable to technology design for personal health care.
BACKGROUND TO Q-METHODOLOGY
Q-methodology uses a set of statements about a topic to elicit people’s points of view [21,22]. The purpose of Q is to understand what attitudes people feel most strongly about. Participants rank the statements in a forced distribution from Most Disagree to Most Agree, with statements of relative insignificance in the middle. This ranking procedure is captured in a table, called a “forced distribution” because participants are forced to place the statements in a normally distributed pattern around a zero-point, with a standard deviation (Figure 1). The advantage of the forced distribution is that each person’s point of view can be compared using the powerful statistical technique of factor analysis to reveal patterns of subjective opinion.
Figure 1.
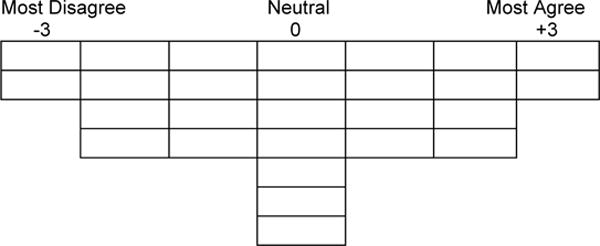
Forced distribution for ranking statements.
Factor analysis is a statistical technique for reducing large amounts of data by clustering similar data and extracting a small number of unique clusters that explain most of the variance, or differences, in the data. Thus, factor analysis can be used to objectively discover patterns in large data sets and to focus attention on the most statistically significant comparisons and contrasts in the data. Q-methodology is unique in its application of factor analysis to the discovery of patterns in subjectivity.
In Q-methodology studies, a factor is a cluster of participants who have ranked statements in a similar pattern, and therefore share a common point of view on a topic. Each cluster has a set of “distinguishing statements” that characterizes the unique point of view it represents. The distinguishing statements for each cluster are statistically significant, meaning that participants ranked those statements much higher or lower than participants in other clusters, at a minimum threshold of p<0.05. Thus Q-methodology affords the use of quantitative analysis techniques to reveal differences in subjective perspectives. Q-methodology is not an inferential statistical technique. Rather, it is similar to qualitative techniques because it works with a small-sample size (n<50), and has limited generalizability. The clusters that emerge from factor analysis reveal statistically significant variations in patterns among statements, not patterns among populations of people. Q-methodology provides many of the same advantages of qualitative methods, such as discovering themes in rich subjective data. However, it accomplishes this theme detection by leveraging the objective pattern identification afforded by quantitative analysis.
Q-methodology Adapted for Health Technology Design
Our mixed-methods approach to using Q-methodology with ethnographic interviews introduces two enhancements of traditional Q technique: (1) a health-sciences theoretical framework for structuring Q data collection, and (2) an application of Q factor analysis to coding interview data.
First, to enhance Q data collection for health technology design, we created a health-sciences theoretical framework to guide selection and creation of the statement set. We analyzed concepts from self-care literature to find high-level categories (e.g. accountability) that grouped similar concepts. We focused on concepts informed by grounded theory analyses of patients living with chronic illness [14], and on validated constructs from the Patient Assessment of Chronic Illness Care [7], and the Patient Activation Measure [9]. We created a range of statements for each high-level category to capture the theoretical polarity of self-care attitudes, e.g., high to low accountability. Our previous research with these participants [5,10] helped us to create relevant, naturalistic statements using participants’ words. The theoretical framework helped us to ensure that we sampled a representative and comprehensive set of statements—the two cornerstones of validity in Q [22]. Moreover, the intersecting categories in the framework helped us to gain a greater understanding of trade-offs in how patients prioritize self-care and technology in everyday life (see Table 2). We describe the framework in more detail below.
Table 2.
Participants grouped by attitude.
| Attitude | ID | Age | Gender | Race | Education |
|---|---|---|---|---|---|
| 1 | A3* | 36 | F | Black | HS |
| 1 | A9 | 36 | F | White | 4YR |
| 1 | A1 | 38 | F | White | 4 YR |
| 1 | A7 | 46 | F | Hispanic | HS |
| 1 | D3 | 85 | F | Black | +4YR |
| 1 | D9 | 88 | F | White | Some HS |
| 2 | D1 | 69 | F | Hispanic | +4YR |
| 2 | D2 | 82 | F | Black | +4YR |
| 3 | D6 | 71 | M | White | HS |
| 3 | D4 | 88 | M | White | Some HS |
| 4 | A5t | 31 | F | Black | Some College |
| 4 | A2 | 38 | F | Black | +4YR |
| 4 | A6 | 40 | F | White | 4YR |
| 4 | A4 | 41 | F | White | +4YR |
| 4 | A8 | 42 | F | Black | +4YR |
| 4 | D7 | 73 | M | White | HS |
| X | D5 | 89 | M | Asian | +4YR |
| X | D8 | 74 | M | White | Some College |
X=confounded;
=low vision;
=low literacy.
Second, to enhance the analysis of interview data with significant differences in health perspectives, we applied the distinguishing statements discovered in the Q statistical analysis to the coding of interview data. Statements such as “I want to be educated about my health,” that distinguished the unique attitude of a cluster of participants, were linked with corresponding utterances in those participants’ interview transcripts that confirmed or contradicted this point of view. This novel data analysis technique allowed us to observe nuances in participants’ perspectives and to understand their most polarizing opinions in the context of other competing values and beliefs. We illustrate this technique and its advantages below.
RELATED WORK
Q-methodology Studies in HCI
An adaptation of Q-methodology for HCI, called HCI-Q [17], was tailored for the specific purpose of empowering stakeholders to critically reflect on designers’ assumptions about desirable and undesirable features of a design. The topic of the statements for HCI-Q studies is the designer’s a priori hypotheses about the implications and uses of a design idea that are likely to be significant to stakeholders. HCI-Q is well-suited to design ideation with stakeholders, and supports designers in being transparent about their biases. Furthermore, it reveals the features of a design that are most controversial among stakeholders and provides practical insights for what to design and for whom. However, HCI-Q relies on concrete design ideation to create statements for ranking, and focuses on gathering attitudes toward design features, rather than attitudes toward behaviors and beliefs that may influence technology adoption and use. Our approach to using Q-methodology is different from HCI-Q in that we used a structured theoretical framework, informed by theories of chronic illness and the Technology Adoption Model [3], to create a set of statements specifically tailored to revealing insights for designing health technologies. We also differentiated our situated ethnographic approach from the online HCI-Q approach by using a set of paper cards that participants sorted and ranked on their kitchen tables during in-home interviews.
Q-methodology Studies in Health Sciences
Q-methodology has been used in health sciences research to investigate patient perspectives of a variety of health topics, including chronic pain [18], cancer-related fatigue [13], medication adherence [2], weight [6], and symptoms of acute myocardial infarction [19]. These studies feature the traditional data collection procedure of Q-methodology, including the common practice of conducting short interviews or surveys after participants rank-order subjective statements in a forced distribution. In the traditional approach, interviewers use the ranked data to probe further into statements that the participant ranked highly. For example, after the ranking procedure, Bullington et al [2] instructed participants: “In a sentence or two, describe why you selected the two items that are scored ‘most like my feelings.’” This structured qualitative data is used to interpret why participants felt strongly about particular statements. We pursue an alternative mixed-methods approach that significantly deepens the role of qualitative data collection for the purposes of understanding strong attitudes toward health self-management. We used the standard Q data collection procedure, but we conducted semi-structured interviews before participants rank-ordered the statements. Our approach enables researchers to understand participant’s significant opinions in the context of their broader health goals and experiences.
Moreover, our mixed-methods approach uses the quantitative data from Q-methodology to help interpret the qualitative data. This new approach to qualitative data analysis offers the advantages of a structured coding scheme derived from statistical patterns of polarizing and consensus opinions. These patterns, which were captured by the Q-methodology, then provide valuable insight about how participants make tradeoffs among their health and technology values. Not only is this approach to qualitative coding efficient, it also builds a rich and nuanced picture of participant experiences based on the values that they asserted to be most significant.
Design Studies of Health Self-Management
Researchers in HCI have explored a range of patient perspectives to inform technology designs that empower patients to take control of their chronic illness. Their studies have yielded valuable insights for technology designers to support people with a chronic illness. For example, in a study of people with cancer, Klasnja et. al. [12] found that patients need health information management support for easy capture of a range of informal information, for integration among that data, and for linking the data to upcoming events. In another example, Maitland et al [15] used ethnographic interviews and inductive analysis to discover tensions and competing values that influenced the heath-related behaviors of cardiac rehabilitation patients. For people with diabetes, Mamykina et. al. [16] used interviews, observations, and a cognitive probe to discover that people need help in understanding the connection between their everyday activities and blood sugar values. However, the methods used in those studies do not help us understand the relative value or priorities that patients place among the discovered technology needs, attitudes, and beliefs and the patient’s health goals or attitudes.
In studies of health self-management, like those listed above, researchers commonly apply qualitative methods, such as interviews and focus groups, to explore stakeholders’ perspectives of technologies and health. Unstructured data is collected and then analyzed using an inductive approach, allowing themes to emerge through a reflexive coding process. In our study, we demonstrate that one of the advantages of applying Q-methodology during ethnographic interviews is that researchers can directly observe participants negotiate and weigh the tradeoffs of competing values. Additionally, researchers can use a deductive analytic approach to categorize themes and surface competing and conflicting viewpoints. By affording a structured way to capture participants’ views of health, our mixed-methods approach can enrich qualitative data collection and analysis procedures with statistical patterns of significant differences in patient perspectives.
Understanding patients’ priorities is important for designers and developers who will need to make resource-allocation and design decisions about which opinions are most important to support. We contribute an approach that supports designers in making those choices by capturing the ways in which participants relate health and technology attitudes in the context of chronic disease self-management.
THEORETICAL FRAMEWORK
The health-sciences theoretical framework, with statements arranged in a grid of intersecting categories (see Figure 2), was designed to highlight attitudes and tensions that can influence technology adoption and provide insights for design. To observe how attitudes toward accountability and resource use interact with the acceptance and use of technology for health self-management, we used the concept of performance expectancy from the Technology Adoption Model (TAM) [3] to reveal attitudes toward future technology adoption to support heath goals.
Figure 2.
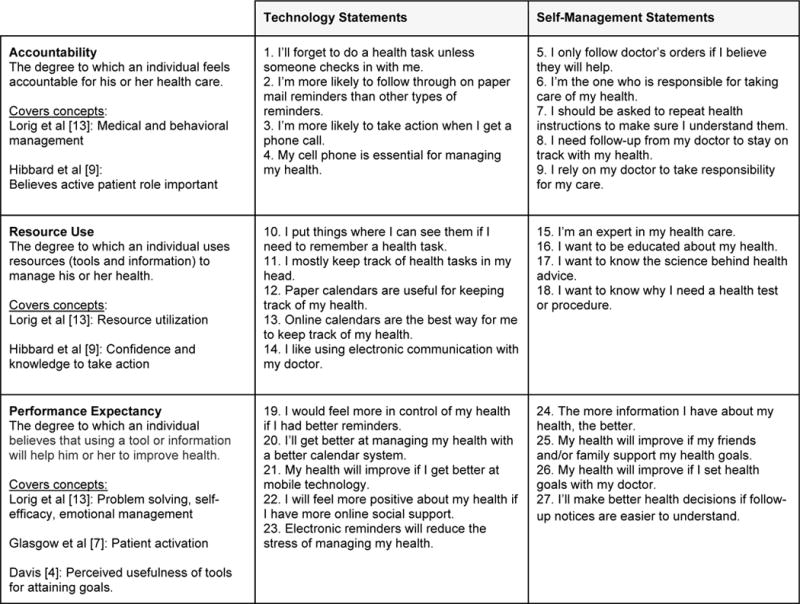
Theoretical framework with statements for eliciting participant’s opinions during the Q-methodology task.
The concepts of accountability, resource use, and performance expectancy are inherently entwined in the management of chronic conditions. Based on our synthesis of self-management theories [1,4,7,8,9,14], we define accountability as the degree to which an individual feels accountable for his or her health care; resource use as the degree to which an individual uses resources (tools and information) to manage his or her health; and performance expectancy as the degree to which an individual believes that using a tool or information will help him or her to improve health outcomes. We used these three concepts to frame the statements for the Q-methodology data collection procedure and to frame our interpretation of results. Figure 2 shows how we categorized the statements for the Q-methodology procedure into six intersecting categories of the framework. Below, we describe the use of the framework and mixed-methods approach in the context of an ethnographic study of attitudes toward self-management of chronic diseases.
METHOD
Participants
We recruited nine older adults with Type 2 diabetes, and nine mothers of children with asthma. Older adults (5 male) had a median age of 82 years old (μ=79.89), and mothers had a median age of 38 years old (μ=38.67). Participants were from diverse races and educational backgrounds (see Table 2). This maximum variation sampling strategy had two purposes: (1) to identify challenges and opportunities for designing technologies that are meaningful to a broad spectrum of users, and (2) to highlight edge cases that may usefully bound the design space of technologies for self-management of chronic illnesses.
Apparatus and Procedure
We travelled around Washington State to people’s homes in urban and rural settings, and sat at their kitchen tables to conduct the interview and Q-methodology procedure. Each session lasted 45–75 minutes in length, and was structured as follows: (1) a semi-structured interview to understand participants’ personal health goals and preferences for information; (2) an artifact discussion about a health task list to probe whether nationally recommended health care activities for diabetes and asthma management matched with their most significant health concerns and priorities; and (3) facilitation of the Q-methodology procedure.
We began with a series of semi-structured questions prior to the Q procedure to help the participants reflect on their health goals. This gave participants time to think about their health activities and reduced the likelihood that the structured statements in Q would solely frame the conversation. This strategy also gave the interviewer an opportunity to follow-up on the Q ranking procedure with questions that incorporated both participant comments at the beginning of their interview and during their sorting of statements.
For the Q procedure, we gave participants 27 statements printed in large font (size 16) on laminated cards. We chose to be conservative with the number of statements in our theoretical framework to avoid fatiguing participants, half of whom were over 70 years old, and 2 had low literacy and low vision. This approach is validated by Watts & Stenner [22] who demonstrate a robust analysis derived from a 25-item Q-set. In accordance with standard Q protocol, we instructed participants to read and sort the statements about health and technology into three piles: agree, disagree, and neutral.
Then, we instructed participants to place statements from their disagree pile into the nine spaces available in the table for disagreeable statements, along a spectrum from Most Disagree (−3) to Disagree (−1). They then repeated this procedure for their agree pile (+3 to +1), and iterated the process until they were satisfied with the result. Participants moved statements in and out of the neutral pile (0) as necessary to normally distribute the statements in the table. After the participants had ranked all statements, we took a picture to capture their data (Figure 3). Mothers found that their self-care attitudes differed from those when caring for their child’s health, so we directed them to do 2 sorts—one for themselves (the one used in this paper) and for their child. Many participants commented on the method, and we have included those comments in our discussion.
Figure 3.
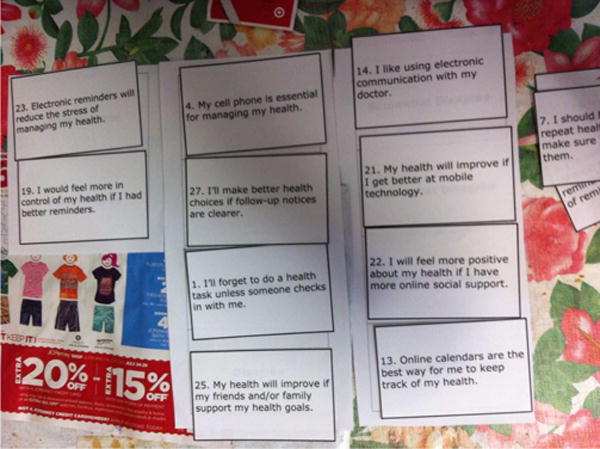
D4’s distribution of disagreeable statements.
Analysis
Data analysis began with factor analysis of the Q-methodology data. Pictures of each participant’s arrangement of statements were transcribed and entered into PQMethod software, a common statistical package for analyzing Q data [20]. Factors, which are clusters of similar perspectives, were identified using Principal Components Analysis, and rotated using the varimax method [11]. Then, we used the distinguishing statements (Table 1) for each cluster to code the interview transcripts. Each distinguishing statement was associated with three sub-codes: “Q” for quotes from the Q procedure directly related to the statement; “Complement” for quotes from the interview that complimented the sentiment of the statement; and “Conflict” for quotes that conflicted with the sentiment of the statement. We grouped and coded transcripts by cluster, for example, distinguishing statements for the first cluster (called “Attitude 1”) were used to code transcripts for participants grouped in that cluster.
Table 1.
Distinguishing statements used for coding.
| Attitude Cluster | Statement | Ranking (−3 ‐ +3) |
|---|---|---|
| Attitude 1 | I want to be educated about my health. | +3 |
| I want to know the science behind health advice. | +2 | |
| I’ll forget to do a health task unless someone checks in with me. | −2 | |
| I’m more likely to follow through on paper mail reminders than other types of reminders. | −3 | |
| Attitude 2 | My health will improve if I set health goals with my doctor. | +3 |
| I need follow‐up from my doctor to stay on track with my health. | +3 | |
| I mostly keep track of health tasks in my head. | −3 | |
| Attitude 3 | I mostly keep track of health tasks in my head. | +3 |
| Electronic reminders will reduce the stress of managing my health. | −3 | |
| Attitude 4 | I want to know why I need a health test or procedure. | +3 |
| My cell phone is essential for managing my health. | +2 | |
| I rely on my doctor to take responsibility for my care. | −3 |
FINDINGS
We used the factor analysis of the Q methodology to identify four clusters that represent four different attitudes toward health and technology for self-management of chronic illness. The four attitude clusters accounted for 68% of the variance in the data. Attitudes 1 and 4 were shared by members from both age cohorts suggesting that, for our sample of participants, health attitudes were not necessarily age or disease specific. Attitudes 2 and 3 were each represented by two members of the older cohort whose perspectives differed significantly from each other. Health perspectives represented by these four unique attitudes do not appear to differ based on characteristics such as education level, gender, or race, as each cluster has a diverse demographic profile (See Table). Two participants were confounded (D8 and D5) meaning that they had too much in common with every cluster, rather than correlating highly with one cluster. These participants were therefore excluded from further analysis because their perspectives were ambiguous.
Attitude 1: “It’s my decision, my body”
The participants in this cluster had a strong preference for education (+3), scientific evidence (+2), information (+2), and taking responsibility (+3). They agreed that online calendars (+1) and electronic communication with providers (+2) are important for managing their health. Despite having a dislike of paper calendars (−1) and paper mail reminders (−3), they disagreed that cell phones (−2) or better use of mobile technology (−3) are related to health outcomes, and do not necessarily expect that electronic reminders will reduce the stress of managing health (0).
Participants explicitly voiced relationships between significant concepts, especially between health information, education, and responsibility. For example, D9 said of the importance of being educated about her health: “if I went in and the doctor’s over here, deciding everything and not telling me anything, it’s not doing me a bit of good. I’ve got to know what’s going on and why my body is acting that way. I guess that’s the same as number 6, ‘I’m responsible for taking care of it.’” A3 agreed, “Yeah, because I feel like as individuals we are responsible for ourselves, so being educated and knowing options—.” A7 articulated the relationship between responsibility and resource use in a similar way to A3, “If there’s a decision to be made, I feel ultimately it’s my decision, my body, right? I like to know the science behind what the options are.”
This cluster is characterized by a strong sense of responsibility and resource use for health self-care. However, participants that defined this factor felt uncertain about whether they are experts in their health care (0). The qualitative data helped us to dig deeper into this apparent contradiction. A9 explained that she gets the doctor’s opinion after she gathers health information from multiple sources: “The Internet, the nurse hotline, my mother-in-law. Those will probably be my first three…You can put them together and see what feels right, kind of thing…then you get into the doctor, and he puts all of it together even better”.
A1’s comment about her preference for speaking with a nurse, also sheds light on the difference between the role of patient, doctor, and technology in health self-management: “I’m not big on Dr. Google, I’m much more likely to call the consulting nurse if it’s something more urgent. I correctly self-diagnosed my lupus in the early days of the Internet. But that scared me so much with everybody’s stories…” These perspectives helped us to understand that performance expectancy for self-management was not highly related to technology for this cluster.
The interview data also helped to corroborate the surprising finding that, despite being a cluster of participants that is very diverse by traditional demographics, they indeed shared the same preference for health information. For example, a 46-year-old Hispanic female with a high school education (A7) and an 85-year old African American female with more than 4 years of college (D3) shared the practice of comparing different sources of information. A7 said, “I guess for me, finding different resources that say the same thing helps back what was said, you know, the [doctor’s] answer.” In a similar vein, D3 said “I use just about every source I can. I’ll go to friends who have been in the profession that I’m interested in just finding out about, I’ll go to friends. I’ll go to the Internet. I’ll go to my physicians, my providers. I’ll go to family. I’ll seek it wherever I can.” It is hardly surprising to find that people who value health information are comparing information sources; however, it is surprising evidence that people with less than a high school education share similar attitudes toward health information as people with doctorate degrees. This finding displays the strength of Q for undermining stereotypes and for facilitating universal design approaches that emphasize diversity. It also suggests that there is value in combining participants from different generations who may adopt similar strategies to using health information and technologies to manage their care.
Attitude 2: “I’m assuming my doctor will tell me”
Participants with Attitude 2 felt most strongly that they need follow-up from their doctor to stay on track with their health (+3), and that their health will improve if they set goals with their doctor (+3). Their preference for doctor engagement in their care was reinforced by their strong disagreement with the statement “I’m an expert in my health care” (−3). In contrast to Attitude 1, the two participants who shared Attitude 2 expressed low self-efficacy, for example, during the interview, D1 said: “I’m not an MD, I don’t have any clue. I just try to learn, but I really don’t know.”
This attitude appears to have a low sense of responsibility and resource use for their care. However, surprisingly, they did not perceive themselves as reliant on their doctors, as evidenced by their disagreement with the statement “I rely on my doctor to take responsibility for my care” (−1). This finding appeared contradictory, but the interview data helped us to understand nuances in health accountability from the patient perspective. For example, D1 explained how goal-setting helped her to clarify her responsibility: “I think that’s important to know what the expectations are…I know she [the doctor] sets goals, like your A1c needs to be under 8, she says, so when it gets close to 8 I have to start watching it. I watch it anyway, but just be more diligent.” This contradiction between the Q statement and the participant’s interview statement demonstrates the value of our mixed-methods approach for discovering how patients prioritize and operationalize core health self-management concepts like accountability.
Similarly, in the interview, D2 explained how having goals set by her doctor is at the core of self-management: “Whatever the major problem was the doctors can see in the past year, and say… ‘why don’t we work on X, Y or Z because there’s been very little change in that’… That’s what to me self-care management should be.” Rather than viewing self-management as a personal responsibility, participants with Attitude 2 perceived it as a partnership with the doctor who is “watching over us,” as D1 put it. In the interview, she reinforced this attitude by saying that, when she needs health information, “I’m assuming my doctor will tell me when I don’t have enough.”
People with Attitude 2 made primary use of visual and paper systems like wall calendars and sticky notes to manage their care; however, they had moderate performance expectancy regarding future use of electronic reminders (+1) and calendars (+1). The interviews revealed that both participants in this cluster used email with their providers to stay on track with their health. D2 described how she asks for follow-up from her doctor by email: “if I have an ailment I don’t call for an appointment, I send an email and tell him what it is, how long I’ve had it, how I feel with it and what steps I have taken for it, and then I’ll say ‘recommendation?’” This example illustrates the strong connection between technology use and self-management attitudes for Attitude 2.
Attitude 3: “It’s just automatic”
Attitude 3 was characterized by self-reliance and a strong preference to be independent with their care. The participants who shared this attitude preferred to be in control of defining their goals and priorities for health. This was the only cluster that agreed with the statement “I only follow doctor’s orders if I believe they will help” (+1), which gives evidence of their strong sense of independence in their care. Their self-reliance did not stem from a belief that they are experts in their health (−2), rather, it was rooted in a desire to manage their chronic disease without compromising a sense of identity. D4 explained in the interview, “It’s just I get up in the morning and do the daily routine. There’s no - basically my life has been the same for the last 88 years, I don’t really dwell on any - just get up and do my routine and what I normally do, a little slower than I used to and that’s about it.”
In contrast to Attitude 2, participants who shared Attitude 3 did not desire follow-up from providers to stay on track (−1), and had personalized strategies and habits for keeping track of their chronic diseases. For example, D4 showed us the paper form that he created to track his blood pressure and glucose “I’ll show you I’ve got a blood pressure machine and a glucose machine in my office…so that’s what I do with getting up in the morning and making a record of and take that in [to the doctor] at the end of the month and start over the following month, do that over again.”
In the interview, D6 shared how he responds to doctor’s orders: “When I need to do something that I can fathom, they seem to get it through to me and it’s my choice to ignore it or do something about it, and for the most part I try to get in and take care of it.” He emphasized his sense of self-reliance again in the interview, when asked whether he would speak with his doctor about weight management, “I guess I would. I don’t like it, but I need to, I know that.”
Participants who shared Attitude 3 kept track of health tasks in their heads (+3), and used visual cues (+1) and paper calendars (+3) to remember health tasks. D4 explained in the interview, “I don’t have a computer so they send me out the mail, they’ll give me a date when to go for the appointment and mail the results of the blood test.” Their strong sense of responsibility for their health (+2) was characterized by low resource use. They strongly disagreed with relying on cell phones (−3) and electronic reminders (−3) for managing their health. The dislike of technology is not surprising considering the ages of the participants who defined this cluster (71 and 88 years old). However, the 62- and 88-year old participants who defined Attitude 2 had a significantly different point of view, characterized by reliance on health providers. The Q technique is valuable for observing such significant differences in perspectives for the purposes of understanding the very different roles that technology might play in the health self-management of elder patients.
Attitude 4: “When should I be worried?”
This cluster had a strong sense of responsibility for their care (+3) and had a strong preference for technology such as cell phones (+2) and electronic communication with their doctors (+2). They want to be educated about their health (+2) but, unlike the participants with Attitude 1, they do not have a preference for knowing the science behind health advice (0). Like the people with Attitude1, the people with Attitude 4 had as strong sense of responsibility (+3), but they were not as confident about their self-management.
For example, in contrast to participants with Attitude 1, their need for information and sense of responsibility stemmed from a desire to feel at ease with the care process. A2 explained, “I want to know…When should I be worried? When is it okay to say that’s a fine result? Those things really matter to me.” In the interview she provided a story that reinforced the significance of the need to feel reassured, “We were getting [daughter’s] test in for celiac disease. That just sounds really scary we get a piece of paper that has numbers - that doesn’t tell me whether she has it or doesn’t have it.” A4 also shared a story to explain why she needs to be informed: “I don’t know that these health care providers have my best interest in mind,” she continued, “I had a really bad experience with my dad who was diagnosed really late with cancer and it went for a long time undetected and he was rushed to the emergency room and I know that a lot of that could have been prevented if someone had been at the office with him.” Our mixed-methods approach helped us to identify these narratives underlying the patients’ most deeply held beliefs and values.
Other narratives were more positive. For example, in the interview, D7 explained how his doctor helped him to understand the need for his knee surgery: “when he talked to me about doing that, he went in his office and pulled open a drawer that had a bunch of plastic replacement parts in it and showed me how they were worn differently and whatnot, and how important it was. Yeah, he did a heck of a job.” Individuals who shared this attitude valued information for forming realistic expectations and for building empathetic relationships with providers.
Finally, Attitude 4 was the only cluster characterized by a strong reliance on cell phones for the purposes of scheduling and remembering health tasks. A2 said “I like ease. It’s really easy to communicate electronically because I’m busy, so it helps.” A6 said, “My cell phone is essential for managing my life,” and A4 agreed, “I do everything on my phone.” However, in the interviews, participants shared two barriers to using their cell phones for health – one was that keys were too small for typing, and the other was that the health system’s mobile application had limited functionality, and was not usable for scheduling. The use of the theoretical framework to structure the Q-methodology data collection procedure helped us to observe that participants sharing Attitude 4 had a strong interaction of high performance expectancy for self-management and technology use. Unlike their highly motivated peers in Attitude 1, participants of Attitude 4 emphasized a strong relationship between mobile technology and personally significant health goals.
DISCUSSION
Our study demonstrates that our mixed-methods approach has several advantages for investigating attitudes toward health and technology in the context of chronic disease management. First, the factor analysis allowed us to find meaningful comparisons and contrasts within an extremely diverse cohort of participants, with ages ranging from 31 to 89, with two different chronic diseases, and with a variety of racial and educational backgrounds. Attitude 1 was a good example of the ways in which factor analysis identified meaningful connections among diverse participants. Their preference for scientific evidence and education was especially surprising given that three of the participants in the Attitude 1 cluster had a high school education or less. Without the objective assessments that the Q-methodology affords, researchers’ bias could easily cause us to overlook such strong values and preferences that do not match our preconceived notions.
Second, the factor analysis in Q provided an efficient way to identify a small number of statistically significant and unique attitudes toward health self-management among these patient stakeholders. For example, each cluster was characterized by different values and motivations for both engaging in self- management and using technology to manage chronic illness. The analysis helped to tease apart not only the more obvious differences in motivations—such as the motivation to have shared responsibility with providers in Attitude 2 versus the strong sense of self-reliance in Attitude 3—but also more nuanced perspectives on the role of information in chronic disease management. For example, the participants with Attitude 1 were highly intrinsically motivated by an intellectual desire to be informed about medications, diagnoses, and treatments. They also used a variety of resources to satisfy their desire to learn about options for their health. In contrast, the participants with Attitude 4 were motivated by an emotional desire to feel comfortable with the care plan. They sought transparency about realistic expectations and empathy for the anxiety experienced when receiving test results.
Finally, our use of a theoretical framework—combining theories for self-management of chronic illnesses and technology adoption—helped us to understand how traditional concepts of self-management in chronic illness are intertwined with use and perceptions of technologies. For example, the self-reliance evident in Attitude 3 can be interpreted as self-reliance of necessity because those participants also tended to be relatively isolated from electronic communication and information. In contrast, the significance of communication technology for self-management in participants with Attitude 4 can be understood in light of their desire to be reassured; the communication technology serves to enhance an empathetic relationship with providers. For Attitude 2, the expectation of improved health performance with new technologies makes sense when understood in relation to their need for follow-up and structured guidance from their providers. Finally, the high resource use yet low salience of technology found in participants with Attitude 1 can be reconciled in light of their emphasis on the in-clinic educational dimension of the doctor-provider relationship.
By having participants weigh the tradeoffs of competing values regarding their health and their use of technology for self-care, our approach provides implications for health technology design. The most extreme-ranked statements (i.e. ranked −3 or +3) and related qualitative data provide strong rationales for the type and range of designs during prototyping. For example, Attitudes 2 and 4 helped us to understand that, rather than encourage independence from health providers, technologies could be most beneficially designed to enhance the relationship between providers and patients by supporting follow-up communication that is actionable and empathetic. Attitudes 1 and 2 suggest that technologies for health self-management, such as for tracking health indicators, need to support both patient and provider-directed goal-setting, depending on the patient’s motivation for taking responsibility for their health. Attitude 3 suggests that technology are desirable only when memory or routines become unreliable aids, such as when people are on vacation or during significant changes in medications—scenarios in which patients are situationally impaired.
Strengths and Weaknesses of the Approach
Q-methodology provides advantages over pure qualitative research, but it comes with limitations as well. One limitation is that some participants had a difficult time sorting the statements because they either agreed or disagreed with most of the statements in the initial sorting phase. For example, D2 had an overwhelming number of statements in her disagree pile to choose from. She asked, “So you want two here [in Most Disagree]? I could put all of these in those.” Another limitation is that the theoretical framework is designed for investigating subjective perspectives of chronic disease self-management, and might not be applicable to technology design studies focused on supporting wellness.
Our approach of combining Q-methodology with interviews provided several advantages over other approaches to health technology design. First, the playfulness of Q-methodology resonated with participants and changed the dynamic of the interviews by engaging them in an activity. For example, D8 jokingly suggested, “Should I get the poker chips out?” Second, the Q-methodology helped participants take control over the direction of the conversation. For example, D6 expressed his authority: “The first one is easy, ‘My cell phone is essential’ - I don’t believe in that at all. And then ‘I’m an expert in my health’ is probably the next one I would mostly disagree with.”
In addition, our inclusion of observations and interviews regarding participants’ reflections allowed us to understand their interpretations of each statement, such as when D9 commented on relying on her doctor to take responsibility for her care: “I guess I’m having trouble, not understanding them [the statements], but the way I feel about them. I expect my doctors to take responsibility when I ask him a question - but he’s not a super being, all he can do is do what I tell him.” As another example, at the end of the procedure, A2 commented on the first-person wording of the statements, “I had to keep [the statements] in perspective, too. It kept saying ‘my’ - so it’s me, not my child’s, so my opinions are different.” We had each mother conduct two sorts – from the perspective of her role in her child’s health and her own health – so that we can conduct a future analysis of the differences in perspectives based on different roles in care.
In addition, we used our mixed-methods approach with a diverse set of people. We demonstrate that it is accessible to adult and elderly individuals, including people with low vision, low education level, and low literacy. This flexibility for use with a diverse population is an asset for health-related research that engages a broad spectrum of patients, clinicians, and caregivers. Our work demonstrates that using Q-methodology can help designers to quickly and efficiently identify commonalities and differences that are not based on traditional participant segmentation by age, ability, gender, or disease.
CONCLUSION
In this paper, we introduced a new approach that combines the quantitative advantages of the Q-methodology with the nuanced interpretations afforded by interviews. We see several ways to build upon this work in the future. For example, the identification of the factors using the Q-methodology could be used to develop personas that are grounded in the perspectives of study participants. Personas created with our technique could provide designers with highly opinionated representative users to inform personal health technology design.
We contribute a mixed-methods approach that is uniquely suited to understanding how people weigh competing health values, and how they articulate connections between self-efficacy and performance expectancy for health self-management. These insights lead to understanding design tradeoffs for health technologies based on the values and motivations that govern different strategies for self-care. With our mixed-methods approach, researchers can start from core self-care theories that help structure data collection and analysis, to discover meaningful connections among stakeholders, regardless of age or disease. Our technique can support designers to understand the polarizing and consensus views that influence stakeholders’ adoption and use of personal health technologies for chronic disease management.
Acknowledgments
This work was supported in part by the AHRQ grant (R01 HS 021590). We also thank the iMed research group and the REMIND team at the Group Health Research Institute.
References
- 1.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev American Psychological Association. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 2.Bullington P, Pawola L, Walker R, Valenta A, Briars L, John E. Identification of medication non-adherence factors in adolescent transplant patients: the patient’s viewpoint. Pediatric Transplantation. 2007;11:8. 914–21. doi: 10.1111/j.1399-3046.2007.00765.x. [DOI] [PubMed] [Google Scholar]
- 3.Davis FD. Perceived Usefulness, Perceived Ease of Use, and User Acceptance of Information Technology. MIS Quarterly. 1989;13:3. [Google Scholar]
- 4.Deci E, Ryan R. The support of autonomy and the control of behavior. In: Higgins E, Kruglanski A, editors. Motivational Science: Social and Personality Perspectives. Psychology Press; Philadelphia, PA: 2000. pp. 128–146. [Google Scholar]
- 5.Eschler J, Kendall L, O’Leary K, et al. Shared calendars for home health management. CSCW’. 2015;15 doi: 10.1145/2675133.2675168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Van Exel NJa, de Graaf G, Brouwer WBF. Everyone dies, so you might as well have fun!Attitudes of Dutch youths about their health lifestyle. Social science & medicine. 2006;63(10):2628–39. doi: 10.1016/j.socscimed.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 7.Glasgow RE, Wagner EH, Schaefer J, Mahoney LD, Reid RJ, Greene SM. Development and validation of the Patient Assessment of Chronic Illness Care (PACIC) Medical care. 2005;43(5):436–44. doi: 10.1097/01.mlr.0000160375.47920.8c. [DOI] [PubMed] [Google Scholar]
- 8.H L, Nerenz DR, Steele D, Taylor S, Singer J. Illness representation and coping with health threats. In: Baum A, editor. Handbook of Psychology and Health. Lawrence Erlbaum Associates; Killsdale, NJ: 1984. pp. 219–252. [Google Scholar]
- 9.Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development testing of a short form of the patient activation measure. Health services research. 2005;40(6 Pt 1):1918–30. doi: 10.1111/j.1475-6773.2005.00438.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kendall L, Eschler J, Lozano P, et al. Engineering for reliability in at-home chronic disease management. AMIA’. 2014;14 [PMC free article] [PubMed] [Google Scholar]
- 11.Kim J, Mueller CW. Factor analysis: Statistical methods and practical issues. Sage; Newbury Park, CA: 1978. [Google Scholar]
- 12.Klasnja P, Hartzler AC, Unruh KT, Pratt W. Blowing in the wind: unanchored patient information work during cancer care. CHI’. 2010;10:193–202. doi: 10.1145/1753326.1753355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lai JS, Kupst MJ, Cella D, Brown SR, Peterman A, Goldman S. Using Q-methodology to understand perceived fatigue reported by adolescents with cancer. Psycho-oncology. 2007;16(5):437–47. doi: 10.1002/pon.1071. [DOI] [PubMed] [Google Scholar]
- 14.Lorig KR, Holman H. Self-management education: history, definition, outcomes, and mechanisms. Annals of behavioral medicine : a publication of the Society of Behavioral Medicine. 2003;26(1):1–7. doi: 10.1207/S15324796ABM2601_01. [DOI] [PubMed] [Google Scholar]
- 15.Maitland J, Chalmers M. Self-monitoring, self-awareness, and self-determination in cardiac rehabilitation. CHI’. 2010;10:1213–1222. [Google Scholar]
- 16.Mamykina L, Mynatt ED, Kaufman DR. Investigating health management practices of individuals with diabetes. CHI’. 2006;06:927–936. [Google Scholar]
- 17.O’Leary K, Wobbrock JO, Riskin EA. Q-methodology As a Research and Design Tool for HCI. CHI’. 2013;13:1941–1950. [Google Scholar]
- 18.Risdon A, Eccleston C, Crombez G, McCracken L. How can we learn to live with pain? A Q-methodological analysis of the diverse understandings of acceptance of chronic pain. Social science & medicine. 2003;56(2):375–86. doi: 10.1016/s0277-9536(02)00043-6. [DOI] [PubMed] [Google Scholar]
- 19.Ryan CJ, Zerwic JJ. Knowledge of symptom clusters among adults at risk for acute myocardial infarction. Nursing research. 2004;53(6):363–9. doi: 10.1097/00006199-200411000-00004. [DOI] [PubMed] [Google Scholar]
- 20.Schmolk P. PQMethod Software. 2014 http://schmolck.org/qmethod.
- 21.Stephenson W. The study of behavior: Q-Technique and its methodology. Univ. of Chicago Press; Chicago, IL: 1953. [Google Scholar]
- 22.Watts S, Stenner P. Doing Q methodological research: Theory, method and interpretation. Sage; Los Angeles: 2012. [Google Scholar]


