Abstract
Background
Geographic access – the travel burden required to reach medical care – is an important aspect of care. Studies, which typically rely on geographic information system (GIS) calculated travel times, have found some evidence of racial disparities in spatial access to care. However, the validity of these studies depends on the accuracy of travel times by patient race.
Objectives
To determine if there are racial differences when comparing patient-reported and geographic information system (GIS)-calculated travel times.
Research Design
Data came from the Philadelphia Area Prostate Cancer Access Study (P2 Access), a cohort study of men diagnosed with localized prostate cancer. We conducted cross-sectional analysis of 2136 men using multivariable linear mixed-effects models to examine the effect of race on differences in patient-reported and GIS-calculated travel times to urology and radiation oncology cancer providers.
Results
Patient-reported travel times were, on average, longer than GIS-calculated times. For urology practices, median patient-reported travel times were 12.7 minutes longer than GIS-calculated travel times for blacks vs. 7.2 minutes longer for whites. After adjusting for potential confounders, including socioeconomic status and car access, the difference was significantly greater for black patients than white patients (2.0 minutes, 95 percent confidence interval: 0.58, 3.44).
Conclusion
GIS-calculated travel time may underestimate access to care, especially for black patients. Future studies that use GIS-calculated travel times to examine racial disparities in spatial access to care might consider including patient-reported travel times and controlling for factors that might affect the accuracy of GIS-calculated travel times.
Keywords: race disparities, travel burden, access to care, prostate cancer
Introduction
Geographic access – the travel burden required to reach medical care – is an important and potentially modifiable aspect of care. Longer travel times and greater distances to obtain medical care are associated with receiving guideline discordant or inappropriate care for a variety of health conditions (1–5), poorer health outcomes (6, 7), and lower quality of life among cancer patients (4). Researchers have also investigated how differences in spatial access may contribute to racial disparities (8–12), frequently finding that black patients experience longer travel times than white patients (8–10), which may contribute to worse quality of care and disparate outcomes.
Studies that incorporate racial/ethnic differences in travel burden typically rely on geographic information system (GIS) road network data and standard impedances to calculate the travel times between two longitude-latitude point locations geocoded from addresses (13). Studies have found that GIS-calculated travel times were, overall, generally well correlated with patient-reported travel time, though the correlation was higher among patients with access to cars and good public transportation (14). To our knowledge, no study has considered whether the accuracy of GIS-calculated travel times varies by patient race/ethnicity. However, the validity of studies examining racial disparities in spatial access depends on the accuracy of travel times by patient race.
Racial/ethnic difference between GIS-calculated and patient-reported travel times may arise through several mechanisms. For example, racial/ethnic minorities are less likely to live in households that own cars (15) and may be more reliant on public transportation. Other important factors that may affect travel time include differences in the time of day that people travel, which may impact traffic conditions, and whether certain populations are more likely to travel to medical care providers from their home address rather than from their workplace or other location. This study aimed to determine whether differences in GIS-calculated and patient-reported travel time differ between black and white patients.
Methods
Data source and study sample
Data for this study came from the Philadelphia Area Prostate Cancer Access Study (P2 Access): a cohort study of black and white men newly diagnosed with localized prostate cancer from the Greater Philadelphia Area. Prostate cancer is an important case study as there is a large burden of disease with well-documented racial disparities, and greater travel burden to urologic care has been associated with higher rates of more advanced prostate cancer, especially among black patients (16). The University of Pennsylvania and Johns Hopkins Institutional Review Boards approved this study.
Men were identified from the Pennsylvania Cancer Registry (PCR) and were eligible to participate in this study if they 1) were diagnosed with localized prostate cancer between January 1, 2012, and December 31, 2014, 2) were a resident of the greater Philadelphia region (Berks, Bucks, Chester, Delaware, Lancaster, Lehigh, Montgomery, and Philadelphia counties), and 3) classified as white or black in the registry data. Men were excluded if they had military insurance or received chemotherapy for treatment. We excluded men with military insurance due to small sample size (n = 8) and because our provider inventory did not specifically include military providers. We excluded men who received chemotherapy as these men often have metastatic disease and are typically treated by medical oncologists, resulting in different travel patterns.
Participants were mailed surveys between February 2014 and August 2015 asking about their access to and the quality of their prostate cancer care. Participants received up to two mailings of the survey, followed by a phone call to all non-responders. An unconditional $2 incentive was provided with the first mailing. Participants received $15 upon completing the survey. The survey response rate was 51.1% (n = 2386).
For this analysis, our sample included respondents who 1) answered survey questions about travel time to their cancer specialist (either their urologist, or both urologist and radiation oncologist if they received radiation therapy) and 2) provided their home address and urologist and/or radiation oncologist practice address that could be geocoded. We excluded men who did not describe themselves as Non-Hispanic (NH) white or NH black for this analysis (n = 63). The final analytic cohort included 2,136 men; 2,136 with travel time information to their urologist and 1,280 with travel time information to their radiation oncologist.
Measures
Outcomes of Interest
Our primary outcome of interest was the calculated difference between patient-reported travel time and GIS-calculated travel time to their prostate cancer specialists. To further understand the potential differences in travel time measures by race, we also examined the components separately: a) patient-reported travel time, and b) GIS-calculated travel times.
For patient-reported travel time, men were asked: “About how many minutes did it take to get to this [their main] urologists’ office?” Men who received treatment from a radiation oncologist were similarly asked about the travel time to their radiation oncologists’ office. For patients who reported a range of times, we used the midpoint of the range (e.g., if a patient reported 15–20 minutes, we used 17.5 minutes).
GIS-calculated travel times were calculated from the patient’s home to their urology and/or radiation oncology practice. Patient home addresses were obtained from the PCR. Patients were asked the name and address of the cancer specialists and matched to an inventory of practices in the greater Philadelphia region and surrounding counties. The inventory was constructed using data from the National Provider Identifier (NPI) database and a frequently updated proprietary database of physicians organized by specialty and location from SK&A (17). All practices were called to confirm that they diagnose and/or treat patients with prostate cancer and to verify their addresses.
Patient and practice addresses were geocoded using ArcGIS 10.2 (18). We manual geocoded addresses that did not automatically geocode (7.2% geocoded manually). Drive times were calculated using ArcGIS 10.2 Network Analyst (18) based on average road conditions, travel speeds, and standard impedances.
Primary Independent Variable
The primary independent variable was patient-reported race/ethnicity, derived from two survey questions asking participants about race and Hispanic origin.
Potential confounding variables
We controlled for respondent and area-level characteristics, which have been identified in prior studies as impacting calculated and/or patient-reported travel time. Educational attainment (less than high school degree, high school degree, 4-year college degree or beyond), insurance coverage (no insurance, private insurance, Medicare, Medicaid), age (continuous), and car access (yes, no) were assessed through the patient survey. Census tract population density was obtained from the American Community Survey (19) and categorized into quartiles.
Statistical Analysis
We estimated descriptive statistics of means and proportions for all potential confounding variables stratified by patient race/ethnicity. We calculated race/ethnicity-stratified median patient-reported and GIS-calculated travel times to urology and to radiation oncology clinics, separately.
We conducted bivariate and multivariable linear mixed effects models with random intercepts to assess unadjusted and adjusted associations between patient race/ethnicity and the following outcomes: 1) the difference in patient-reported and GIS-calculated travel times 2) patient-reported travel times, and 3) GIS-calculated travel times. Random effects accounted for clustering within each patient since each patient could report up to two travel times (for a urology and/or radiation oncology clinic) and clustering of patients within census tract. To address missing data in our confounding variables, we used multiple imputation with chained equations and statistically combined five imputed datasets. All statistical analyses were performed using Stata 14.1 (20).
Results
Among the 2,136 participants, 359 (17%) were black (Table 1). Black participants were significantly less likely to have a college education or beyond compared to whites (21.3% vs. 50.0%), less likely to have private insurance (32.6% vs. 50.9%), and less likely to report having access to a car (74.5% vs. 95.1%). Blacks lived in more densely populated census tracts. The study sample came from 958 census tracts. The sample size for each census tract ranged from 1 to 11 participants.
Table 1.
Sample Charateristics
| Mean or proportion | p-value | ||
|---|---|---|---|
| NH White (n = 1777) |
NH Black (n = 359) |
||
| Age, mean (SD) | 66.0 (8.3) | 63.7 (8.2) | < 0.001 |
| Education, % | |||
| Less than high school degree | 5.2 | 15.6 | < 0.001 |
| High school degree | 44.7 | 63.1 | |
| 4-year college degree or beyond | 50.0 | 21.3 | |
| Insurance Type, % | |||
| No insurance | 0.6 | 2.6 | < 0.001 |
| Private | 50.9 | 32.6 | |
| Medicare | 38.6 | 29.7 | |
| Medicaid | 9.8 | 35.2 | |
| Car Access | |||
| No access to car | 4.9 | 26.5 | < 0.001 |
| Yes access to car | 95.1 | 73.5 | |
| CT Population Density, mean (SD) | 4620 (7608) | 15467 (10499) | < 0.001 |
| Has a radiation oncologist, % | 58.6 | 66.3 | 0.007 |
Median self-reported travel time to urology clinics was the same for white and black men (20 minutes) while median GIS-calculated times were larger for whites (13.0 minutes) than blacks (7.4 minutes) (Figure 1). The calculated difference between self-reported and GIS-calculated was 7.8 minutes over all and 12.7 minutes for blacks versus 7.2 minutes for whites. Median self-reported travel time to radiation oncology clinics was larger for blacks (25 minutes) than whites (20 minutes). Median GIS-calculated travel time was larger for whites (13.8 minutes) than blacks (7.0 minutes) (Figure 2). The calculated difference between self-reported and GIS-calculated was 9.3 minutes overall, and 14.0 minutes for blacks versus 8.1 minutes for whites.
Figure 1.
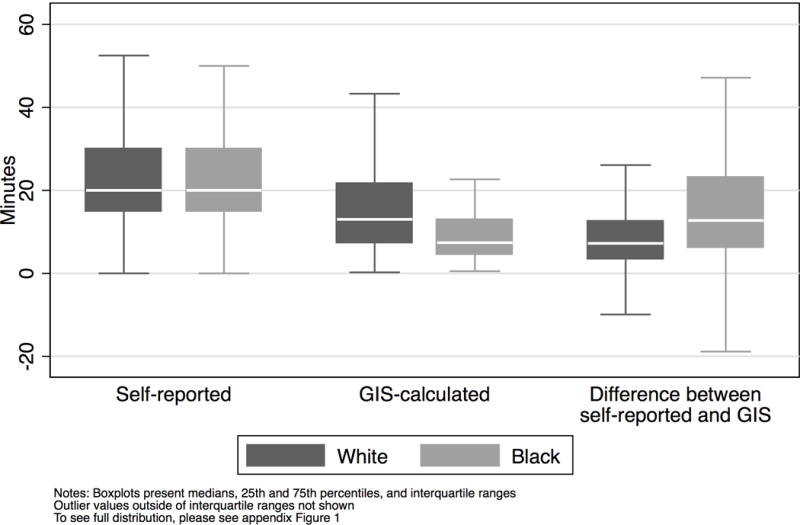
Boxplots of travel time measures and calculated difference by patient race for travel to urology clinics
Figure 2.
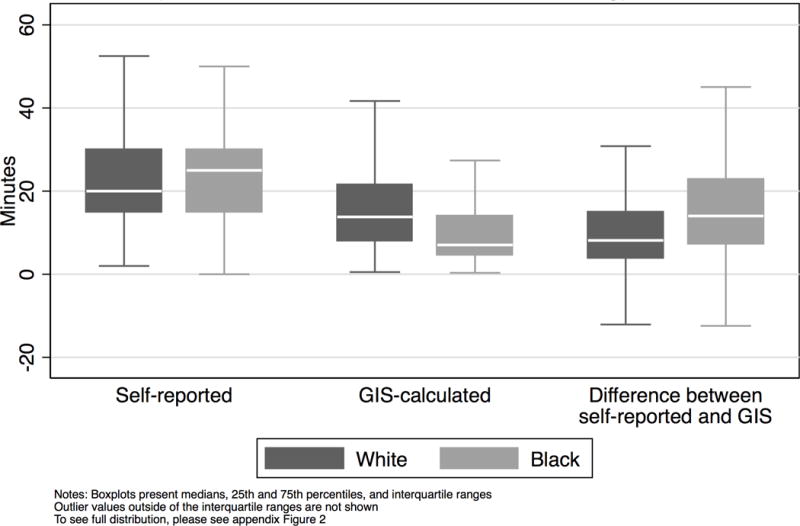
Boxplots of travel time measures and calculated difference by patient race for travel to radiation oncology clinics
In our unadjusted analysis, after accounting for within census tract and patient clustering (Table 2), the difference between patient-reported and GIS-calculated travel times was 5.7 minutes larger for blacks than white (95% Confidence Intervals (CI): 4.46, 6.99). After adjusting for potential confounders (Table 2), the difference between patient-reported and GIS-calculated travel times was 2.0 minutes larger for blacks than whites (95% CI: 0.58, 3.44). Additionally, the difference between patient-reported and GIS-calculated travel times was larger for men without access to a car (4.5 minutes, 95% CI: 2.85, 6.18), as age increased (0.13 minutes for each year increase, 95% CI: 0.06, 0.19), and as census tract population density increased (vs. Q1 (least populated quartile) Q2: 1.3 minutes, 95% CI: 0.02, 2.6; Q3: 3.6 minutes, 95% CI: 2.27, 4.85; Q4: 6.8 minutes, 95% CI: 5.36, 8.28).
Table 2.
Unadjusted and adjusted associations of the difference in patient-reported and GIS-calculated travel times
| Unadjusted analysis | Adjusted analysis | |||||
|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | |
| Race/ethnicity | ||||||
| NH White | ref | – | – | ref | – | – |
| NH Black | 5.73 | (4.46, 6.99) | <0.001 | 2.01 | (0.58, 3.44) | 0.006 |
| Educational Attainment | ||||||
| Less than high school degree | ref | – | – | |||
| High school degree | −0.94 | (−2.77, 0.88) | 0.309 | |||
| 4-year college degree or beyond | 0.51 | (−1.36, 2.38) | 0.593 | |||
| Insurance status | ||||||
| No insurance | ref | – | – | |||
| Private insurance | −3.68 | (−8.71, 0.86) | 0.112 | |||
| Medicare | −3.41 | (−7.98, 1.17) | 0.145 | |||
| Medicaid | −2.20 | (−6.84, 2.44) | 0.353 | |||
| Age | 0.13 | (0.06, 0.19) | <0.001 | |||
| Car access | ||||||
| Yes access to car | ref | – | – | |||
| No access to car | 4.52 | (2.85, 6.18) | <0.001 | |||
| Population density | ||||||
| Quartile 1 | ref | – | – | |||
| Quartile 2 | 1.32 | (0.02, 2.63) | 0.047 | |||
| Quartile 3 | 3.57 | (2.27, 4.85) | <0.001 | |||
| Quartile 4 | 6.82 | (5.36, 8.28) | <0.001 | |||
| Intraclass Correlation Coefficient | ||||||
| Individual | 0.04 | (0.02, 0.11) | ||||
| Census tract | 0.47 | (0.42, 0.51) | ||||
Notes: Adjusted models controlled for patient race, educational attainment, insurance coverage, age, car access, and census tract population density
Bold text denotes significance at p< 0.05
Outcome (patient-reported travel time minus GIS-calculated travel time) combines responses for both urology and radiation oncology practices
After accounting for potential confounders, patient-reported travel time was 2.11 minutes longer for blacks (95% CI: 0.15, 4.07) than whites (Table 3). The GIS-calculated travel times were not significantly different between race groups (0.23, 95% CI: −1.02, 1.48).
Table 3.
Adjusted associations for patient-reported travel time and GIS-calculated travel time
| Patient-reported travel time | GIS-calculated travel time | ||||||
|---|---|---|---|---|---|---|---|
| Coefficient | 95% CI | p-value | Coefficient | 95% CI | p-value | ||
| Race/ethnicity | |||||||
| NH White | ref | – | – | ref | – | – | |
| NH Black | 2.11 | (0.15, 4.07) | 0.035 | 0.23 | (−1.02, 1.48) | 0.718 | |
| Educational Attainment | |||||||
| Less than high school degree | ref | – | – | ref | – | – | |
| High school degree | −0.53 | (−2.99, 1.94) | 0.676 | 0.27 | (−1.22, 1.76) | 0.726 | |
| 4-year college degree or beyond | 1.67 | (−0.88, 4.22) | 0.199 | 1.14 | (−0.41, 2.70) | 0.150 | |
| Insurance status | |||||||
| No insurance | ref | – | – | ref | – | – | |
| Private insurance | −1.79 | (−7.94, 4.37) | 0.570 | 2.12 | (−1.62, 5.86) | 0.266 | |
| Medicare | −2.50 | (−8.69, 3.68) | 0.428 | 1.10 | (−2.64, 4.84) | 0.565 | |
| Medicaid | −1.92 | (−8.20, 4.36) | 0.549 | 0.34 | (−3.45, 4.13) | 0.860 | |
| Age | −0.02 | (−0.11, 0.07) | 0.625 | −0.14 | (−0.19, −0.08) | <0.001 | |
| Car access | |||||||
| Yes access to car | ref | – | – | ref | – | – | |
| No access to car | 3.09 | (0.84, 5.34) | 0.007 | 1.19 | (−0.19, −0.08) | 0.087 | |
| Population density | |||||||
| Quartile 1 | ref | – | – | ref | – | – | |
| Quartile 2 | −4.74 | (−6.60, −2.88) | <0.001 | −6.18 | (−7.52, −4.83) | <0.001 | |
| Quartile 3 | −4.51 | (−6.33, −2.69) | <0.001 | −8.04 | (−9.33, −6.74) | <0.001 | |
| Quartile 4 | −6.28 | (−8.32, −4.24) | <0.001 | −13.24 | (−14.65, −11.84) | < 0.001 | |
Notes: Adjusted models controlled for patient race, educational attainment, insurance coverage, age, car access, and census tract population density
Bold text denotes significance at p< 0.05
Outcome (patient-reported travel time minus GIS-calculated travel time) combines responses for both urology and radiation oncology practices
Discussion
We found that patient-reported travel times were generally longer than GIS-calculated times for all patients. However, the difference between these two travel times was larger for black patients compared to white patients, a difference that was driven black patients tending to self-report longer travel times. This study builds on existing work that has considered how other patient characteristics such as car and public transportation access, patient age, and household income may affect the accuracy of GIS-calculated measures of spatial access to care (14). It further suggests that studies that rely exclusively on GIS-calculated travel times may potentially underestimate black-white disparities in spatial access to care.
It has been hypothesized that differences in spatial access for minority patients may contribute to documented racial/ethnic disparities in access to care and health outcomes (21, 22). Multiple studies assessing racial differences in spatial access to care, which relied on GIS-calculated travel times or distances, have yielded mixed findings. While some studies have found that blacks have longer travel times and distances (9, 10, 23), others have either found no difference by race (24, 25), or that blacks actually have shorter travel times and distances (26, 27). Our finding of racial differences between travel time measures may help to explain some of these mixed findings. It is plausible that some of the null or negative findings may be different if these studies had also considered patient-reported travel times. To our knowledge, no study has used patient-reported travel times to assess racial differences in spatial access to care.
There currently is no agreed upon “gold standard” for measuring patient travel time to their providers. Both GIS-calculated and patient-reported measures have limitations. For example, GIS-calculated measures often do not account for traffic conditions based on the time of day of travel or different modes of transportation, (e.g., walking or public transportation). Patient-reported measures may be subject to recall bias, particularly if substantial time has elapsed since patients visited their providers. Despite these limitations, self-report – which captures patient perceptions of travel burden – is important. Previous studies have found that perception that influences patient treatment choices, including whether, where, and when patients may access care (14). Using both patient-reported and GIS-based approaches can provide a more comprehensive assessment of racial disparities in patient travel burdens.
The unadjusted race difference between the patient-reported and GIS-calculated travel times decreased substantially after we controlled for confounding characteristics, including car access, and urbanicity. In our fully adjusted model, the black-white difference in these two measures of travel time, while statistically significant, was quite small. This might suggest that the accuracy of GIS-calculated travel times can be improved by accounting for important confounders, such as urbanicity, car access, or other technological additions such as improved traffic congestion and roadway impedance parameters that are becoming increasingly available in commercial GIS software packages. While our study did not specifically investigate potential mechanisms, the substantial decrease in the black-white difference in adjusted models suggests that these characteristics might be, in part, driving the observed relationship. Blacks are more likely to live in metropolitan areas (28), and have lower access to cars (15), both of which might affect the accuracy of GIS-calculated travel times.
Our study had several limitations. Patient self-reported travel times to providers’ offices may be subject to recall biases or rounding errors. Recall bias might increase as the time between diagnosis and survey response increased. However, there were no difference patient-reported travel times between men who took the survey more than a year versus a year or less after their diagnosis (Appendix table A1). Sensitivity analysis that also controlled for the time between diagnosis and survey responses yielded similar results (Appendix table A2). Measurement error may have arisen in patient-reported travel time among patients who reported a range of times and may differ by patient characteristics. However, the proportion of patients who reported a range of times was small (urology: 4.1%; radiation oncologist: 6.0%). Most patients reported a small range of 5 minutes or less. We found few differences in reporting ranges by patient race (Appendix table A3) and time between diagnosis and survey response (Appendix table A4). Consistent with prior studies, our GIS-calculated time was calculated from patients’ homes to their providers’ offices. In reality, patients may travel to their providers from a variety of different locations, such as from work. Additionally, we were unable to account for the time of day when patients traveled (e.g., rush hour versus non-rush hour times), which might contribute to the difference between patient-reported and GIS-calculated travel times. There might be potential selection or recruitment bias in the men who chose to respond to our survey compared to men who chose not to respond to the survey. For example, black men were less likely to respond to our survey than white men (Appendix table A5). Finally, our study was conducted among a population of men receiving care for their prostate cancer treatment in the Philadelphia metro area, a diverse area comprising 5.3 million residents living in urban and suburban census tracts. Our findings may not be generalizable to other geographic areas or for patients receiving care in other therapeutic areas.
Our study is the first to assess whether the difference between patient-reported and GIS-calculated travel times differ by patient race. Future studies that assess racial differences in spatial access to care with GIS-calculated travel times might consider ways to improve the accuracy of this measurement. To the extent possible, studies assessing racial differences in spatial access might include patient-reported travel times among their populations of interest and control for factors, such as car-ownership and urbanicity, that might affect the accuracy of GIS-calculated travel times by race/ethnicity.
Supplementary Material
Acknowledgments
We would like to thank Xinwei Chen for helping to manage the datasets.
Funding: This work was supported by the National Institute on Minority Health and Health Disparities (P60 MD006900). Ms. Wong’s salary is supported by the National Institute Of Diabetes And Digestive And Kidney Diseases of the National Institutes of Health (T32DK062707). Dr. Radhakrishnan’s salary is supported by the National Heart, Lung, and Blood Institute (T32H1007180). Dr. Pollack’s salary is supported by the National Cancer Institute (K07CA151910).
Footnotes
Disclosure of conflicts of interest: The authors report no conflicts of interest
Contributor Information
Michelle S. Wong, Department of Health Policy and Management, Johns Hopkins School of Public Health, 624 N. Broadway, Baltimore, MD 21205.
David T. Grande, Division of General Internal Medicine, University of Pennsylvania, 3641 Locust Walk, Colonial Penn Center 407, Philadelphia, PA 19104, Telephone: 215-573-3804, Fax: 215-898-0229.
Nandita Mitra, Department of Biostatistics and Epidemiology, University of Pennsylvania, 622 Blockley Hall, 423 Guardian Drive, Philadelphia, PA 19104, Telephone: 215-573-4467, Fax: 215-573-4865.
Archana Radhakrishnan, Division of General Internal Medicine, Johns Hopkins School of Medicine, 2024 E. Monument St Suite 2-300C, Baltimore, MD 21287, Telephone: 410-287-9526, Fax: 410-955-0476.
Charles C. Branas, Department of Epidemiology, Columbia University, 722 W. 168th Street, Room 1508, New York, NY 10032.
Katelyn R. Ward, Division of General Internal Medicine, University of Pennsylvania, 1208 Blockley Hall, 423 Guardian Drive, Philadelphia, PA 19104, Telephone: 215-746-1163.
Craig Evan Pollack, Division of General Internal Medicine, Johns Hopkins School of Medicine, 2024 E. Monument St, Suite 2-519, Baltimore, MD 21287, Phone: 410-502-2359, Fax: 410-955-0476.
References
- 1.Lin CC, Bruinooge SS, Kirkwood MK, et al. Association Between Geographic Access to Cancer Care and Receipt of Radiation Therapy for Rectal Cancer. International journal of radiation oncology, biology, physics. 2016;94:719–728. doi: 10.1016/j.ijrobp.2015.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin CC, Bruinooge SS, Kirkwood MK, et al. Association Between Geographic Access to Cancer Care, Insurance, and Receipt of Chemotherapy: Geographic Distribution of Oncologists and Travel Distance. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2015;33:3177–3185. doi: 10.1200/JCO.2015.61.1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Celaya MO, Rees JR, Gibson JJ, et al. Travel distance and season of diagnosis affect treatment choices for women with early-stage breast cancer in a predominantly rural population (United States) Cancer causes & control : CCC. 2006;17:851–856. doi: 10.1007/s10552-006-0025-7. [DOI] [PubMed] [Google Scholar]
- 4.Ambroggi M, Biasini C, Del Giovane C, et al. Distance as a Barrier to Cancer Diagnosis and Treatment: Review of the Literature. The oncologist. 2015;20:1378–1385. doi: 10.1634/theoncologist.2015-0110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin D, Roderick P, Diamond I, et al. Geographical aspects of the uptake of renal replacement therapy in England. International Journal of Population Geography. 1998;4:227–242. [Google Scholar]
- 6.Gumpertz ML, Pickle LW, Miller BA, et al. Geographic patterns of advanced breast cancer in Los Angeles: associations with biological and sociodemographic factors (United States) Cancer causes & control : CCC. 2006;17:325–339. doi: 10.1007/s10552-005-0513-1. [DOI] [PubMed] [Google Scholar]
- 7.Jones AP, Haynes R, Sauerzapf V, et al. Travel times to health care and survival from cancers in Northern England. European Journal of Cancer. 2008;44:269–274. doi: 10.1016/j.ejca.2007.07.028. [DOI] [PubMed] [Google Scholar]
- 8.Probst JC, Laditka SB, Wang JY, et al. Effects of residence and race on burden of travel for care: cross sectional analysis of the 2001 US National Household Travel Survey. BMC health services research. 2007;7:40. doi: 10.1186/1472-6963-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Peipins LA, Graham S, Young R, et al. Racial disparities in travel time to radiotherapy facilities in the Atlanta metropolitan area. Social science & medicine (1982) 2013;89:32–38. doi: 10.1016/j.socscimed.2013.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Onega T, Lee CI, Benkeser D, et al. Travel Burden to Breast MRI and Utilization: Are Risk and Sociodemographics Related? Journal of the American College of Radiology. 2016;13:611–619. doi: 10.1016/j.jacr.2016.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Onega T, Duell EJ, Shi X, et al. Influence of place of residence in access to specialized cancer care for African Americans. Journal of Rural Health. 2010;26:12–19. doi: 10.1111/j.1748-0361.2009.00260.x. [DOI] [PubMed] [Google Scholar]
- 12.Smedley BD, Stith AY, Nelson AR. Unequal treatment: Confronting racial and ethnic disparities in health care (full printed version) National Academies Press; 2002. [PubMed] [Google Scholar]
- 13.ESRI. ArcGIS Network Analyst. 2016 Available at: http://www.esri.com/software/arcgis/extensions/networkanalyst. Accessed September 11, 2016.
- 14.Fone DL, Christie S, Lester N. Comparison of perceived and modelled geographical access to accident and emergency departments: a cross-sectional analysis from the Caerphilly Health and Social Needs Study. International journal of health geographics. 2006;5:16. doi: 10.1186/1476-072X-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Raphael S, Berube A, Deakin E. Socioeconomic differences in household automobile ownership rates: Implications for evacuation policy. University of California Transportation Center. 2006 [Google Scholar]
- 16.Holmes JA, Carpenter WR, Wu Y, et al. Impact of Distance to a Urologist on Early Diagnosis of Prostate Cancer Among Black and White Patients. The Journal of Urology. 2012;187:883–888. doi: 10.1016/j.juro.2011.10.156. [DOI] [PubMed] [Google Scholar]
- 17.Pollack CE, Ross ME, Armstrong K, et al. Using a Mystery-Caller Approach to Examine Access to Prostate Cancer Care in Philadelphia. PLOS ONE. doi: 10.1371/journal.pone.0164411. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.ArcGIS 10.2 [mapping program] Redlands, CA: ESRI; 2014. [Google Scholar]
- 19.U.S. Census Bureau. American Community Survey (ACS) 2016 [Google Scholar]
- 20.Stata 14.1 [statistical program] College Station, TX: Stata Corp; 2015. [Google Scholar]
- 21.Lin Y, Zhan FB. Geographic variations of racial/ethnic disparities in cervical cancer mortality in Texas. Southern medical journal. 2014;107:281–288. doi: 10.1097/SMJ.0000000000000100. [DOI] [PubMed] [Google Scholar]
- 22.Brown EJ, Polsky D, Barbu CM, et al. Racial Disparities In Geographic Access To Primary Care In Philadelphia. Health affairs (Project Hope) 2016;35:1374–1381. doi: 10.1377/hlthaff.2015.1612. [DOI] [PubMed] [Google Scholar]
- 23.Probst JC, Laditka SB, Wang J-Y, et al. Effects of residence and race on burden of travel for care: cross sectional analysis of the 2001 US National Household Travel Survey. BMC health services research. 2007;7:1–13. doi: 10.1186/1472-6963-7-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Temkin SM, Fleming SA, Amrane S, et al. Geographic disparities amongst patients with gynecologic malignancies at an urban NCI-designated cancer center. Gynecologic Oncology. 2015;137:497–502. doi: 10.1016/j.ygyno.2015.03.010. [DOI] [PubMed] [Google Scholar]
- 25.Hebert PL, Chassin MR, Howell EA. The contribution of geography to black/white differences in the use of low neonatal mortality hospitals in New York city. Medical Care. 2011;49:200–206. doi: 10.1097/MLR.0b013e3182019144. [DOI] [PubMed] [Google Scholar]
- 26.Bristow RE, Chang J, Ziogas A, et al. Spatial analysis of adherence to treatment guidelines for advanced-stage ovarian cancer and the impact of race and socioeconomic status. Gynecologic Oncology. 2014;134:60–67. doi: 10.1016/j.ygyno.2014.03.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Smith AK, Shara NM, Zeymo A, et al. Travel patterns of cancer surgery patients in a regionalized system. The Journal of surgical research. 2015;199:97–105. doi: 10.1016/j.jss.2015.04.016. [DOI] [PubMed] [Google Scholar]
- 28.Rastogi S. The black population: 2010. US Department of Commerce, Economics and Statistics Administration, US Census Bureau; 2011. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


