Abstract
Occult bacterial infections represent a worldwide health problem. Differentiating active bacterial infection from sterile inflammation can be difficult using current imaging tools. Present clinically viable methodologies either detect morphologic changes (CT/ MR), recruitment of immune cells (111In-WBC SPECT), or enhanced glycolytic flux seen in inflammatory cells (18F-FDG PET). However, these strategies are often inadequate to detect bacterial infection and are not specific for living bacteria. Recent approaches have taken advantage of key metabolic differences between prokaryotic and eukaryotic organisms, allowing easier distinction between bacteria and their host. In this report, we exploited one key difference, bacterial cell wall biosynthesis, to detect living bacteria using a positron-labeled D-amino acid. After screening several 14C D-amino acids for their incorporation into E. coli in culture, we identified D-methionine as a probe with outstanding radiopharmaceutical potential. Based on an analogous procedure to that used for L-[methyl-11C]methionine ([11C] L-Met), we developed an enhanced asymmetric synthesis of D-[methyl-11C]methionine ([11C] D-Met), and showed that it can rapidly and selectively differentiate both E. coli and S. aureus infections from sterile inflammation in vivo. We believe that the ease of [11C] D-Met radiosynthesis, coupled with its rapid and specific in vivo bacterial accumulation, make it an attractive radiotracer for infection imaging in clinical practice.
Introduction
A common clinical problem for practicing infectious disease specialists and radiologists is differentiating active infection from other causes of inflammation. This problem is of critical importance because the treatments for infection and sterile inflammation are diametrically opposed, with antibiotics being indicated in one case and immunosuppression in the other. Definitive diagnosis requires tissue sampling, but the diagnostic accuracy of this procedure can be low, and the associated morbidity may be high, for example in biopsies of the central nervous system (CNS). Noninvasive anatomic imaging techniques, especially computed tomography (CT) and magnetic resonance imaging (MRI) are also frequently used in the workup of acute infection. Although many infections have a characteristic imaging appearance on CT and MRI, it is often impossible to distinguish bacterial infection from other disease entities. For example, active bone infection may look similar on MRI to radiation-induced necrosis, rheumatologic disease or age-related degeneration1, 2. Several molecular imaging methods have been applied to this problem, in particular 111In or 99mTc white blood cell (WBC) scanning, in which the patient’s own immune cells are radiolabeled and planar gamma camara imaging or single-photon emission computed tomography (SPECT) is performed3. Recently, the workup of fever of unknown origin (FUO) has included full-body positron emission tomography (PET) using 2-[18F]-fluorodeoxyglucose (FDG), the most common radiotracer applied to oncologic imaging4. Like cancer cells, activated immune cells are highly glycolytic, and thus may be detected using FDG-PET. However, lack of specificity is the major problem for both SPECT and PET approaches. Furthermore, these imaging techniques are dependent on host inflammatory responses to infection, which may be reduced or absent in immunosuppressed patients (e.g. chemotherapy, HIV/AIDS, organ transplant) who are most at risk for infection.
In order to overcome these barriers, there has been a long and sustained interest in developing specific probes that can be used to label bacteria in vivo during active infection5. Many innovative strategies have been reported including radiolabeled antibodies6, antimicrobial peptides7, antibiotics8, specific enzyme ligands9, nucleic acids10, metabolized compounds11 and even bacteriophages12. To date, no agent has been accepted into clinical practice for routine differentiation of infection from sterile inflammation.
Most bacteria produce and incorporate significant amounts of D-amino acids (DAAs), in particular D-Ala and D-Glu, which are used in peptidoglycan synthesis. Peptidoglycan is a strong and elastic polymer of the bacterial wall that maintains cell shape and anchors components of the cell envelope13. Interestingly, DAA within peptidoglycan appear to protect the bacterial cell against peptidase and protease attacks and also serve important and specific roles in cell-cell signaling14. Many antimicrobial agents (both synthetic and natural products) work by antagonizing the DAA synthesis, dimerization, and incorporation pathway, most notably beta-lactam antibiotics and other cell wall active agents like vancomycin and cycloserine15. Remarkably, other DAA are incorporated into peptidoglycan via a mechanism that is independent of the normal biosynthetic pathway, inducing structural alterations16. These DAAs include D-Met and D-Phe, which are readily incorporated into Escherechia coli muropeptides and likely serve important roles in cell signaling in addition to structural function14. In particular D-Met has been shown to be released by a diverse array of stationary phase bacteria, which use it as a specific signal to alter the growth of neighboring cells. Importantly, D-Met released into the media is avidly taken up by bacteria and incorporated into peptidoglycan14. D-amino acids have been shown to be powerful agents for in vitro labeling of peptidoglycan17 and their incorporation is very rapid (~30 sec in E. coli) and highly specific18 prompting us to consider the possibility of using these compounds in vivo for diagnostic imaging (Fig. 1). Adapting methods previously described19, we synthesized [11C] D-Met and applied it to the detection of both E. coli and S. aureus bacteria in vivo.
Figure 1.
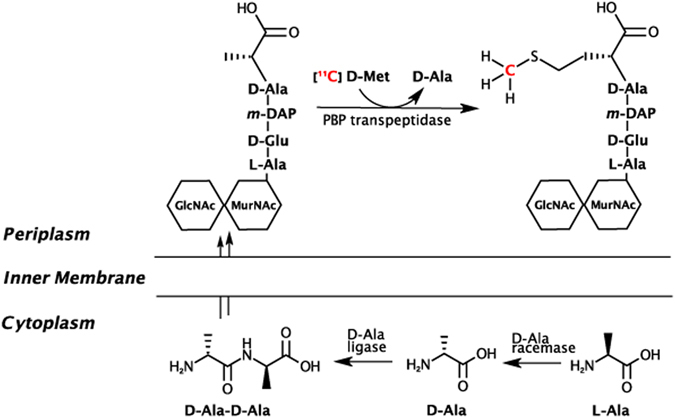
Incorporation of D-amino acids into peptidoglycan via racemase-dependent and racemase-independent pathways. The intracellular processing of D-alanine is contrasted with the perpiplasmic addition of D-methionine, which is “swapped” at the C-terminus of peptidoglycan, mediated by the transpeptidase domains of penicillin binding proteins (PBPs). D-Met may be incorporated into peptidoglycan muropeptides by exogenous administration or by physiologic production, with the latter associated with transition into the stationary phase and downregulation of peptidoglycan synthesis. The putative pathway of 11C retention following [11C] D-Met administration to infected animals is highlighted in red. GlcNAc = N-acetylglucosamine, MurNAc = N-acetyl- muramic acid, m-DAP = meso-diaminopimelic acid.
Results
[14C] D-Met is readily accumulated in both E. coli and S. aureus
An in vitro screen of [14C] D-amino acids was performed in small-volume E. coli and S. aureus cultures, to identify promising structures for 11C or 18F incorporation (Fig. 2A). E. coli and S. aureus were chosen as representative gram-negative and gram-positive bacteria; the pathogenic strains of these organisms are frequent culprits in human infection20, 21. Based on a prior report documenting rapid incorporation of DAAs into E. coli muropeptides via a racemase-independent pathway, [14C] D-Val, [14C] D-Phe and [14C] D-Met were studied16. Incorporation of 14C was quantified by liquid scintillation counting. This study showed the highest percent cell associated activity for [14C] D-Met, which was identified as the best candidate for PET tracer development. Importantly, this screen also showed D-Met was readily incorporated by both E. coli and S. aureus. Of note, D-Ala and D-Glu were considered as potential cell-wall labeling agents, since they are both components of native peptidoglycan. However, pursuing PET versions of these molecules had significant drawbacks: significant in vivo defluorination for 18F versions of alanine22, 23, modest enantiomeric excess (48% ee; 74%-L, 26%-D) for reported [11C] L-Ala asymmetric synthesis24, and lack of homology between reported 18F versions of glutamate and the native amino acid25, 26. The development of stable, high enantiomeric excess PET versions of these metabolites is an important goal for future studies.
Figure 2.
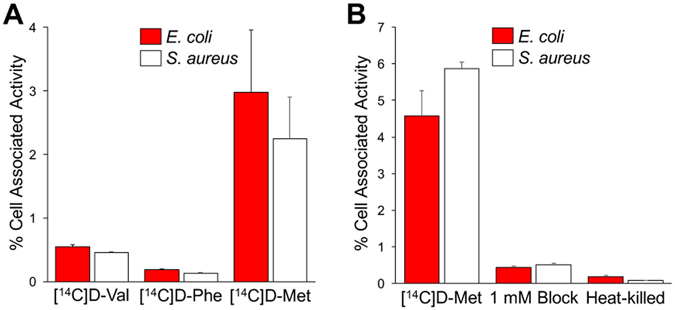
In vitro accumulation of 14C D-amino acids in E. coli and S. aureus. (A) Panel of 14C amino acids studied for relative uptake. (B) Dedicated 14C D-Met study in E. coli and S. aureus including incubation with heat-killed organisms and in the presence of 1 mM unlabeled D-methionine.
The behavior of [14C] D-Met was further studied in competition (blocking) experiments, evaluated in heat-killed bacteria, and compared to that of [14C] L-Met. Heat-killed bacteria did not accumulate [14C] D-Met and the uptake of the radiotracer was effectively blocked by co-incubation with 1 mM concentrations of unlabeled D-Met in normal bacteria (Fig. 2B), confirming specificity to metabolically active organisms (p < 0.05). Comparing bacterial uptake of [14C] D-Met and [14C] L-Met yielded discrepant results, depending on the media used. In F12 media (low amino-acid concentration), there was no significant difference between [14C] D-Met and [14C] L-Met accumulation (p > 0.05) (Supp. Fig. 1A ). In contrast, marked selectivity for [14C] D-Met over [14C] L-Met was observed in lysogeny broth (LB) (p < 0.05) (Supp. Fig. 1B). The reason for this difference is unknown and may be related to the lower amino acid content in F12 media. However, the D/L selectivity in LB observed in vitro was recapitulated by in vivo studies as discussed subsequently.
[11C] D-Met can be produced rapidly and efficiently via an automated radiosynthesis
Several radiosyntheses of [11C] L-Met have been described, first by Langstrom et al. in 1997 using a Na/NH3 reduction of an S-benzyl protected homocysteine precursor27. For our study, we chose the method most frequently applied to automated radiopharmaceutical preparation of [11C] L-Met for patient studies, namely [11C] CH3I methylation of an L-homocysteinethiolactone precursor19. After synthesis of the corresponding D-homocysteinethiolactone, we first optimized this radiosynthesis for enhanced enantiomeric excess of [11C] D-Met via gas-phase produced [11C] CH3I on a GE FX/C Pro™. Base-catalyzed hydrolysis of D-homocysteinethiolactone is prone to racemization, as has been previously reported28. As the central hypothesis of this study was in vivo differential identification of bacteria using the D enantiomer, we explored different hydrolysis conditions to optimize enantiomeric excess (%ee) of the final product (Supp. Fig. 2 and Supp. Table 1). We found that a final concentration of 3.3 mM NaOH gave us the highest enantiomeric excess of [11C] D-Met. For our optimized protocol, gas-phase produced [11C] CH3I was reacted with the D-thiolactone precursor and NaOH in an acetone/H2O mixed solvent for 2 minutes at 100 °C, followed by quenching with AcOH. For subsequent studies using these conditions (n = 4), we isolated [11C] D-Met in 21 min (EOB) in a 20.3 ± 1.2% non-decay corrected (41.6% corrected) radiochemical yield with a specific activity of 4.5 ± 3.2 Ci/μmol and 92.6% ± 2.4% D-enantiomer (85% enantiomeric excess). For all [11C] D-Met in vivo studies reported chiral HPLC confirmed greater than 90% D-enantiomer (Fig. 3).
Figure 3.
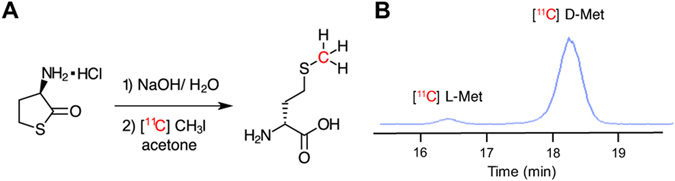
Radiosynthesis of [11C] D-Met from D-homocystinethiolactone precursor. (A) Synthetic scheme. (B) Chiral stationary-phase HPLC showing enhanced enantiomeric excess synthesis of [11C] D-Met.
[11C] D-Met PET can differentiate active bacterial infection from sterile inflammation in vivo
Based on the promising results from our in vitro studies, we next investigated whether [11C] D-Met was a suitable imaging agent for differentiating bacterial infection from sterile inflammation in vivo, using a murine myositis model similar to that previously reported11. Confirmations of the validity of this model included both repeating in vivo results using 2-[18F]-fluorodeoxysorbitol (FDS), and postmortem tissue homogenization and plating to confirm the presence of living bacteria. Mice were inoculated with live E. coli or S. aureus in the left deltoid muscle and a 10-fold higher burden of heat-killed bacteria in the contralateral deltoid (sterile inflammation). After the infection was allowed to progress for 12 hours, the mice were imaged by μPET-CT using a single time-point study similar to clinical protocols. [11C] D-Met rapidly and specifically accumulated in the infected region-of-interest (ROI), while no detectable accumulation above background was observed in the sterile, inflamed right deltoid (Fig. 4). Spherical ROIs were drawn to quantify the accumulation of D-Met in the infected deltoid, the contralateral sterile inflammation site, and normal muscle. When normal muscle ROI’s were used to normalize the data, dramatic differences between infection and sterile inflammation were seen (Fig. 4B). Uncorrected data showed [11C] D-Met produced >2-fold higher counts in the infected ROI as compared to the sterile inflammation site (Supp. Fig. 3), with representative maximum intensity projection (MIP) images shown in Supp. Fig. 4. In contrast, no significant difference was seen between infected versus sterile sites when using [11C] L-Met (Fig. 4C,D) (p > 0.05). This ROI analysis was corroborated by biodistribution studies on animals following euthanasia (Fig. 5A).
Figure 4.
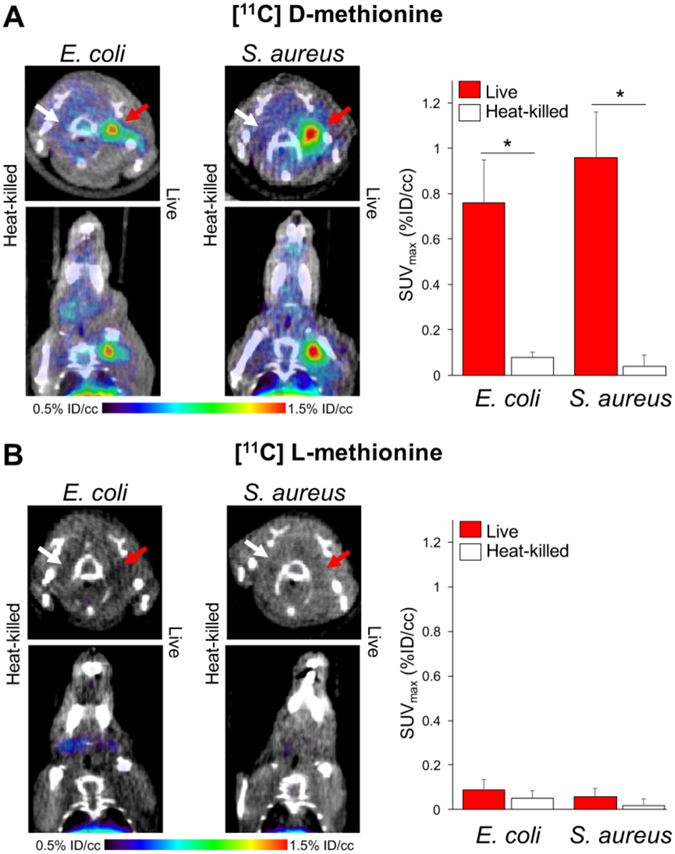
In vivo studies using [11C] D-Met and [11C] L-Met a murine myositis model (n = 4 for each condition studied). In all cases the site of live bacterial inoculation is denoted by a red arrow, while the site of 10X heat-killed bacterial inoculation is denoted by a white arrow. (A) [11C] D-Met studies in E. coli and S. aureus-infected animals. Representative images show marked uptake in areas corresponding to live bacterial injection (left deltoid), in contrast to sterile inflammation (right deltoid) and normal muscle. ROI analysis of E. Coli and S. aureus [11C] D-Met cohorts, corrected using normal muscle uptake. (B) [11C] L-Met studies in E. coli and S. aureus. There is no observable difference in signals from the left (infected) and right (sterile inflammation) deltoid muscles. ROI analysis of E. Coli and S. aureus [11C] L-Met cohorts, showing no significant difference in accumulation between infection and sterile inflammation.
Figure 5.
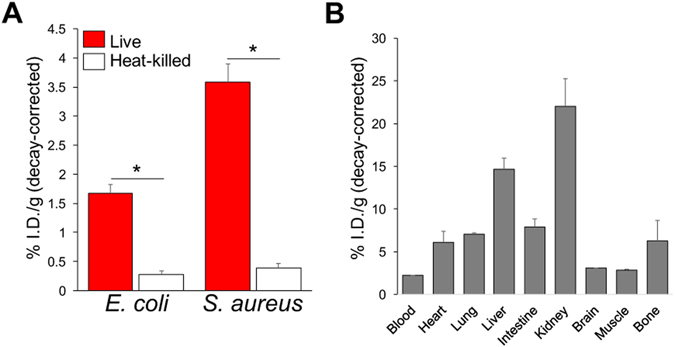
Ex vivo analysis of both infected and normal mice, obtained via tissue harvesting and gamma-counting. In all cases mice injected intravenously with [11C] D-Met were sacrificed at 70 minutes. (A) Analysis of harvested deltoid muscles, performed immediately following the imaging studies described in this manuscript. The deltoid muscles corresponding to inoculation with live bacteria were compared with the contralateral side (heat-killed). (B) The biodistribution of [11C] D-Met was also studied in a separate cohort of normal CBA/J female mice. The highest accumulation was observed in the kidneys and liver, similar to previously reported findings for [11C] L-Met34.
Postmortem tissue histology (hematoxylin and eosin, Gram-stain) for both strains of bacteria in mice thighs verified the presence of inflammatory cells and bacteria in the infected thigh, and inflammatory cells without bacteria in the contralateral uninfected thigh. Representative data for E. Coli and S. aureus inoculations (n = 4 animals studied per organism) are shown in Supp. Fig. 5 and Fig. 6 respectively. We further demonstrated the presence of sterile inflammation in this model using FDG. Since Weinstein et al. previously applied FDG to murine E. coli infection11, we studied a cohort of S. aureus infected mice (n = 4, Supp. Fig. 6). We demonstrated concordant results, namely that similar FDG uptake was seen in muscle inoculated with live and 10X heat-killed bacteria (p > 0.05). Both showed increased tracer accumulation versus normal muscle by ex vivo analysis (dissection and gamma counting), p < 0.05).
Figure 6.
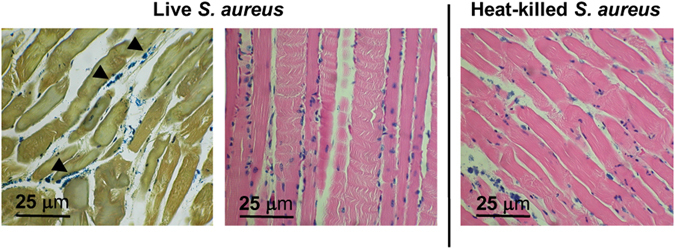
Representative histology for an S. aureus infected mouse sampled from deltoid muscle, using Gram-staining (left image) and hematoxylin & eosin (H&E, center and right image). In live inoculations, scattered inflammatory cells and intact bacteria are seen, best identified by Gram-staining and denoted by arrowheads. In heat-killed inoculations (right), several inflammatory cells are present on H&E staining without discernible bacteria. Images are representative of four animals.
Discussion
The imaging of infection using bacteria-specific metabolic pathways has tremendous clinical potential. A PET probe for bacterial infection would be most useful in the clinic if it could distinguish bacterial infection (all organisms) from common mimics. Thus, we sought to develop a PET probe that is accumulated by representative gram-negative and gram-positive pathogenic bacteria, to distinguish infection from other CT and MR mimics. Encouraging data are emerging from other groups investigating potentially broad-spectrum maltose and maltodextrin-derived tracers29–31, but to date no lead tracer has emerged with wide microorganism sensitivity, facile radiosynthesis, and good in vivo stability. Therefore, in this study we developed a D-amino acid derived PET probe that is accumulated by both E. coli and S. aureus infections, as a starting point for more detailed study of (1) microorganism sensitivity and (2) other D-amino acid derived scaffolds. This strategy has not been previously applied to in vivo imaging, despite the numerous antibiotics (for example vancomycin) targeting bacterial cell wall synthesis.
The findings of this study set the stage for additional D-amino acid derived PET tracers. Several studies have indicated that many unnatural D-amino acids are incorporated into bacterial peptidoglycan at a high rate, including work performed in the Bertozzi laboratory, showing the incorporation of R-propargylglycine into E. coli peptidoglycan17. Recently, Pidgeon et al. demonstrated that transpeptidases catalyze the metabolic incorporation of exogenous D-amino acids onto bacterial cell surfaces with vast promiscuity for C-terminus variations32. This tolerance for structural differences will facilitate incorporation of 11C, 18F, and other nuclei into related radiotracers. Eventually, the incorporation of a set of unique tracers could be used to differentiate bacteria and guide treatment decisions in settings where bacterial culture and sensitivity is not immediately available.
A limitation of infection imaging strategies is that human microbiomes contain huge numbers of non-pathogenic bacteria that colonize the internal and external surfaces of human bodies33. The presence of these bacteria in our respiratory and gastrointestinal tracts may limit detection of pathogenic bacteria in these locations. Furthermore, some tracers including [11C] D-Met have significant background uptake in normal organs, most notably the kidney and liver (Fig. 5B). Fortunately, several of the most challenging infections from a diagnostic standpoint occur in normally sterile environments, for example within the nervous, biliary and musculoskeletal systems. The workup of these conditions might benefit greatly from [11C] D-Met, particularly in conjunction with multi-modality imaging (PET-CT and PET-MR).
Methods
[14C] D-amino acid uptake studies in E. coli and S. aureus
E. coli strain ATCC 25922 and S. aureus strain ATCC 12600 were used for all in vitro and in vivo studies. The in vitro studies evaluating both E. coli and S. aureus for relative [14C] substrate accumulation were prepared identically. Each condition reported was a measure of four replicates containing 20 million bacteria. Bacteria were inoculated in LB broth and grown overnight to OD600 = 1.0. The bacteria were then pelleted by centrifugation at 13.2 rpm for 60 seconds. The supernatant was removed, and the pellet was resuspended in 1 mL of F12 media or LB broth. For blocking experiments, four replicates were prepared in the same manner with 20 million bacteria, 100uL of 10 mM D-Met, and 1 mL of F12 or LB broth. The vials were incubated with 0.1 µCi of [14C] D-amino acid (Moravek Inc.) at 37 °C for 2 hours. The bacterial suspensions were removed from the incubator and centrifuged at 13.2 rpm for 60 seconds. The supernatant was removed, and 1 mL of ice-cold phosphate-buffered saline (PBS) was added to the samples and vortexed gently for 3 seconds. The suspension was centrifuged at 13.2 rpm for 60 seconds, the supernatant was removed, and the wash cycle was repeated one additional time. Upon removal of the supernatant, 500 μL 1 M NaOH was added to the bacterial pellets. Each pellet was vortexed for 3 seconds and incubated at 37 °C for 5 minutes. A 400 μL aliquot was transferred to a scintillation vial and diluted with 3 mL of MP Biomedicals Ecolyte liquid scintillation cocktail. Samples were counted on a Beckman LS 6500 scintillation counter.
Radiochemical synthesis of [11C] D-Met
[11C] CO2 was produced in target by the 14N(p, α)11C nuclear reaction of 17 MeV protons on N2 in the UCSF radiopharmaceutical facility. [11C] CO2 was converted to [11C] CH3I using the gas-phase method on a GE FX/C Pro automated synthesis module. [11C] CH3I (g) was transferred from a Porapak N into a glass reactor vial, previously charged with 500 µL of acetone, while maintaining the reactor vial temperature at 0 °C during the transfer. After 3 minutes, 0.2 mg of D-homocysteine thiolactone hydrochloride, dissolved in 100 µL of 20 mM NaOH (aq), were transferred to the reactor vial. The reactor vial was sealed and heated at 100 °C for 2 min. The reactor vial was cooled to 40 °C and acetone is evaporated over the course of 3 minutes. The aqueous reactor vial solution was neutralized with 320 µL of 10 mM acetic acid (previously loaded in V2) and the contents of the reactor vial are transferred through a C18 Sep-Pak® Plus and collected in a vial for use. Enantiomeric excess of the final product was analyzed using a Phenomenex Chirex-33126 D-penicillamine HPLC column (4.6 × 250 mm) with a mobile phase of 30:70 methanol:1 mM copper sulfate at a flow rate of 1 mL/min. Retention times of [11C] L-Met and [11C] D-Met were 16.4 and 18.2 minutes, respectively.
Murine Myositis Model
All animal procedures were approved by the UCSF Institutional Animal Care and Use Committee. Veterinary services for the study were provided by the UCSF Laboratory Animal Resource Center (LARC) and all studies were performed in accordance with UCSF guidelines regarding animal housing, pain management, and euthanasia. All mice used were CBA/J females (Jackson Laboratory) aged between 8–10 weeks. Single colonies of E. coli or S. aureus were placed in LB broth shaking cultures at 37 °C overnight prior to inoculations. Cultures were incubated until they reached OD600 of 1.0. 1 mL portions of the culture were heat killed by incubating at 90 °C for 30 minutes. The heat-killed bacteria were then spun down and resuspended in 100 μL of LB broth. Mice were placed under isoflurane anesthesia on a warming pad. Approximately 8 hours before imaging, 100 μL of live bacterial culture and 100 μl of 10X concentrated heat-killed bacteria were injected with tuberculin syringes into the right and left shoulder musculature, respectively. Mice were then removed from anesthesia and allowed to recover and intermittently monitored prior to imaging.
PET imaging
Under isoflurane anesthesia, a tail vein catheter was placed. For methionine studies, approximately 1 mCi of [11C] D-Met or [11C] L-Met were injected via the tail vein catheter. The animals were placed on a heating pad to minimize shivering. Mice were allowed to recover, micturate, and at 45 minutes post-injection, placed back under isoflurance anesthesia. At 1 hour post-injection, the animals were transferred to a Siemens Inveon micro PET-CT system (Siemens, Erlangen, Germany), and imaged using a single static 10 min acquisition (60–70 minutes post-injection), followed by micro-CT scan for attenuation correction and anatomical co-registration. Studies using FDG were performed using a similar protocol; 200 μCi of FDG were injected via tail vain catheter and the animals imaged using a static 15 minute acquisition (45–60 minutes post-injection). No adverse events were observed during or after injection of any compound. Anesthesia was maintained during imaging using isofluorane. Upon completion of imaging, mice were sacrificed and biodistribution analysis performed using either harvested deltoid muscle (infected mice) or normal organs (wild-type mice). Gamma counting of harvested tissues (n = 4 per organ or tissue) was performed using a Hidex Automatic Gamma Counter (Turku, Finland).
Data analysis and statistical considerations
All PET data were viewed using open source Amide software (amide.sourceforge.net). Quantification of uptake was performed by drawing regions of interest over indicated organs on the CT portion of the exam, and expressed as percent injected dose per gram. All statistical analysis was performed using Microsoft Excel. Four data sets were acquired for all in vitro and in vivo studies (n = 4 in all cases). Data were analyzed using an unpaired two-tailed Student’s t-test. All graphs are depicted with error bars corresponding to the standard error of the mean. Other data including specific activity, radiochemical yield, and % D-enantiomer are also reported as mean ± standard error.
Histopathology
Muscle tissues inoculated with heat-killed or live bacteria were fixed overnight in 4% paraformaldehyde before being sequentially dehydrated and embedded in paraffin. Paraffin embedded tissues were sectioned on a microtome at 4 µm and stained with hematoxylin and eosin or Gram stain.
Electronic supplementary material
Acknowledgements
Grant sponsors R01 CA166766; P41 EB013598; T32 EB001631-12; UCSF Resource Allocation Program; UCSF Open Access Publishing Fund. The authors would also like to thank Prof. Sanjay Jain and Alvaro Ordonez (Johns Hopkins University) for their assistance with animal models.
Author Contributions
D.M.W., M.O. and O.R. proposed and supervised the overall project. K.N., J.V.M., T.K., R.S. obtained in vitro data. K.N., J.B. performed the radiochemistry. J.V.M., C.M., R.F., D.W. performed μPET-CT imaging studies and subsequent data analysis. J.V.M., C.M., performed ex vivo analysis. D.M.W., K.N., J.V.M., H.V.B., R.F., M.O., O.R. wrote and edited the paper.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
Kiel D. Neumann and Javier E. Villanueva-Meyer contributed equally to this work.
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-08415-x
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Oren S. Rosenberg, Email: oren.rosenberg@ucsf.edu
Michael A. Ohliger, Email: michael.ohliger@ucsf.edu
David M. Wilson, Email: david.m.wilson@ucsf.edu
References
- 1.Baker JC, Demertzis JL, Rhodes NG, Wessell DE, Rubin DA. Diabetic musculoskeletal complications and their imaging mimics. Radiographics: a review publication of the Radiological Society of North America, Inc. 2012;32:1959–1974. doi: 10.1148/rg.327125054. [DOI] [PubMed] [Google Scholar]
- 2.Stacy, G. S. & Kapur, A. Mimics of bone and soft tissue neoplasms. Radiologic clinics of North America49, 1261–1286, vii, doi:10.1016/j.rcl.2011.07.009 (2011). [DOI] [PubMed]
- 3.Palestro CJ. Radionuclide imaging of osteomyelitis. Seminars in nuclear medicine. 2015;45:32–46. doi: 10.1053/j.semnuclmed.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 4.Gafter-Gvili, A. et al. [18F]FDG-PET/CT for the diagnosis of patients with fever of unknown origin. QJM: monthly journal of the Association of Physicians, doi:10.1093/qjmed/hcu193 (2014). [DOI] [PubMed]
- 5.van Oosten M, et al. Targeted imaging of bacterial infections: advances, hurdles and hopes. FEMS microbiology reviews. 2015;39:892–916. doi: 10.1093/femsre/fuv029. [DOI] [PubMed] [Google Scholar]
- 6.Becker, W. et al. Rapid imaging of infections with a monoclonal antibody fragment (LeukoScan). Clinical orthopaedics and related research, 263–272 (1996). [DOI] [PubMed]
- 7.Ebenhan T, Gheysens O, Kruger HG, Zeevaart JR, Sathekge MM. Antimicrobial peptides: their role as infection-selective tracers for molecular imaging. BioMed research international. 2014;2014:867381. doi: 10.1155/2014/867381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fuster D, et al. Usefulness of 99mTc-ciprofloxacin scintigraphy in the diagnosis of prosthetic joint infections. Nuclear medicine communications. 2011;32:44–51. doi: 10.1097/MNM.0b013e328340e6fb. [DOI] [PubMed] [Google Scholar]
- 9.Bettegowda C, et al. Imaging bacterial infections with radiolabeled 1-(2′-deoxy-2′-fluoro-beta-D-arabinofuranosyl)-5-iodouracil. Proceedings of the National Academy of Sciences of the United States of America. 2005;102:1145–1150. doi: 10.1073/pnas.0408861102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hernandez FJ, et al. Noninvasive imaging of Staphylococcus aureus infections with a nuclease-activated probe. Nature medicine. 2014;20:301–306. doi: 10.1038/nm.3460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Weinstein EA, et al. Imaging Enterobacteriaceae infection in vivo with 18F-fluorodeoxysorbitol positron emission tomography. Science translational medicine. 2014;6:259ra146. doi: 10.1126/scitranslmed.3009815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bardhan NM, Ghosh D, Belcher AM. Carbon nanotubes as in vivo bacterial probes. Nature communications. 2014;5:4918. doi: 10.1038/ncomms5918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bugg TD, Walsh CT. Intracellular steps of bacterial cell wall peptidoglycan biosynthesis: enzymology, antibiotics, and antibiotic resistance. Natural product reports. 1992;9:199–215. doi: 10.1039/np9920900199. [DOI] [PubMed] [Google Scholar]
- 14.Lam H, et al. D-amino acids govern stationary phase cell wall remodeling in bacteria. Science. 2009;325:1552–1555. doi: 10.1126/science.1178123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hammes WP, Neuhaus FC. On the mechanism of action of vancomycin: inhibition of peptidoglycan synthesis in Gaffkya homari. Antimicrobial agents and chemotherapy. 1974;6:722–728. doi: 10.1128/AAC.6.6.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caparros M, Pisabarro AG, de Pedro MA. Effect of D-amino acids on structure and synthesis of peptidoglycan in Escherichia coli. Journal of bacteriology. 1992;174:5549–5559. doi: 10.1128/jb.174.17.5549-5559.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Siegrist MS, et al. (D)-Amino acid chemical reporters reveal peptidoglycan dynamics of an intracellular pathogen. ACS chemical biology. 2013;8:500–505. doi: 10.1021/cb3004995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuru E, Tekkam S, Hall E, Brun YV, Van Nieuwenhze MS. Synthesis of fluorescent D-amino acids and their use for probing peptidoglycan synthesis and bacterial growth in situ. Nature protocols. 2015;10:33–52. doi: 10.1038/nprot.2014.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mizuno KI, Yamazaki S, Iwata R, Pascali C, Ido T. Improved Preparation of L-[Methyl-C-11]Methionine by Online [C-11] Methylation. Appl Radiat Isotopes. 1993;44:788–790. doi: 10.1016/0969-8043(93)90152-Z. [DOI] [Google Scholar]
- 20.Kaper JB, Nataro JP, Mobley HL. Pathogenic Escherichia coli. Nature reviews. Microbiology. 2004;2:123–140. doi: 10.1038/nrmicro818. [DOI] [PubMed] [Google Scholar]
- 21.Tong SY, Davis JS, Eichenberger E, Holland TL, Fowler VG., Jr. Staphylococcus aureus infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev. 2015;28:603–661. doi: 10.1128/CMR.00134-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang D, et al. Synthesis of [18F]fluoroalanine and [18F]fluorotamoxifen for imaging breast tumors. Journal of drug targeting. 1993;1:259–267. doi: 10.3109/10611869308996084. [DOI] [PubMed] [Google Scholar]
- 23.Wang L, et al. Synthesis and evaluation of 18F labeled alanine derivatives as potential tumor imaging agents. Nuclear medicine and biology. 2012;39:933–943. doi: 10.1016/j.nucmedbio.2012.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fasth KJ, Antoni G, Langstrom B. Asymmetric-Synthesis of L-[3-C-11] Alanine and L-[3-C-11] Phenylalanine by a Phase-Transfer Alkylation Reaction. J Chem Soc Perk T. 1988;1:3081–3084. doi: 10.1039/P19880003081. [DOI] [Google Scholar]
- 25.Krasikova RN, et al. 4-[F-18]Fluoroglutamic Acid (BAY 85-8050), a New Amino Acid Radiotracer for PET Imaging of Tumors Synthesis and in Vitro Characterization. Journal of medicinal chemistry. 2011;54:406–410. doi: 10.1021/jm101068q. [DOI] [PubMed] [Google Scholar]
- 26.Koglin N, et al. Specific PET Imaging of x(C)(-) Transporter Activity Using a F-18-Labeled Glutamate Derivative Reveals a Dominant Pathway in Tumor Metabolism. Clinical Cancer Research. 2011;17:6000–6011. doi: 10.1158/1078-0432.CCR-11-0687. [DOI] [PubMed] [Google Scholar]
- 27.Langstrom B, et al. Synthesis of L- and D-[methyl-11C]methionine. Journal of nuclear medicine: official publication, Society of Nuclear Medicine. 1987;28:1037–1040. [PubMed] [Google Scholar]
- 28.Pascali C, et al. High efficiency preparation of L-[S-methyl-C-11]methionine by on-column [C-11]methylation on C18 Sep-Pak. J Labelled Compd Rad. 1999;42:715–724. doi: 10.1002/(SICI)1099-1344(199908)42:8<715::AID-JLCR224>3.0.CO;2-3. [DOI] [Google Scholar]
- 29.Gowrishankar G, et al. Investigation of 6-[(1)(8)F]-fluoromaltose as a novel PET tracer for imaging bacterial infection. PloS one. 2014;9:e107951. doi: 10.1371/journal.pone.0107951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Namavari M, Gowrishankar G, Hoehne A, Jouannot E, Gambhir SS. Synthesis of [(1)(8)F]-labelled maltose derivatives as PET tracers for imaging bacterial infection. Molecular imaging and biology: MIB: the official publication of the Academy of Molecular Imaging. 2015;17:168–176. doi: 10.1007/s11307-014-0793-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ning X, et al. PET imaging of bacterial infections with fluorine-18-labeled maltohexaose. Angewandte Chemie. 2014;53:14096–14101. doi: 10.1002/anie.201408533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pidgeon SE, et al. Metabolic Profiling of Bacteria by Unnatural C-terminated D-Amino Acids. Angewandte Chemie. 2015;54:6158–6162. doi: 10.1002/anie.201409927. [DOI] [PubMed] [Google Scholar]
- 33.Cho I, Blaser MJ. The human microbiome: at the interface of health and disease. Nat Rev Genet. 2012;13:260–270. doi: 10.1038/nrg3182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Comar D, Cartron J, Maziere M, Marazano C. Labelling and metabolism of methionine-methyl-11 C. Eur J Nucl Med. 1976;1:11–14. doi: 10.1007/BF00253260. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


