Abstract
Background:
Intraoperative image guidance is a useful modality for transsphenoidal pituitary surgery. However, the outcomes associated with this technology have not been systematically evaluated.
Objective:
The purpose of the study was to quantify complication rates with and without the use of image guidance during transsphenoidal pituitary surgery using a nationwide database with broadly applicable results.
Methods:
A retrospective analysis of the Nationwide Inpatient Sample was performed from 2007 to 2011. Transsphenoidal pituitary resections for adenomas were identified by International Classification of Diseases-9th Revision, Clinical Modification code. The effect of image guidance on cerebrospinal fluid (CSF) leak complications and cost-benefit was analyzed.
Results:
A total of 48,848 transsphenoidal pituitary resections were identified, of which 77.5% were partial resections and 22.5% were complete. Pathologic indications included benign (89.3%), malignant primary (0.6%), and malignant secondary (0.4%). Complications included same-stay death (0.4%), CSF leak (8.8%), postoperative CSF rhinorrhea (1.9%), diabetes insipidus (12.4%), and meningitis (0.4%). Image guidance was employed in 7% (n = 3401) of all cases. When analyzed by modality, computed tomography (CT)-assisted procedures had lower CSF rhinorrhea rates (1.1%) compared with cases with no image guidance (1.9%), whereas magnetic resonance (MR)-assisted procedures had the highest rates (2.7%, χ2 p < 0.001). Rates of CSF leak demonstrated a similar pattern (CT 6.4%, no image guidance 8.9%, MR 9.2%, χ2 p < 0.001). CT-assisted surgery had significantly shorter length of stay (2.9 days) versus no image guidance (3.7 days, p < 0.001), lower total charges ($47,589 versus $62,629, p < 0.001), and lower total cost ($16,748 versus $20,530, p < 0.001).
Conclusions:
CT-assisted surgery is associated with a lower rate of CSF leak, shorter length of stay, and lower cost compared with patients without image guidance. Further studies that control for severity and extent of disease are warranted to confirm this finding.
Keywords: Image-guided surgery, image guidance, computed tomography-assisted surgery, magnetic resonance imaging-assisted surgery, cerebrospinal fluid leak, transsphenoidal pituitary surgery, nationwide inpatient sample cost and charge data, pituitary adenoma
Surgical management of pituitary pathology has largely transitioned from open craniotomies to transsphenoidal pituitary surgical approaches. For appropriate indications, the transsphenoidal approach has several theoretical advantages over open craniotomies including decreased cerebral edema, less risk of cerebrospinal fluid (CSF) leakage, and stroke, as well as fewer cosmetic complications that accompany external incisions.1 Furthermore, improvements in optics, powered instrumentation, and surgical expertise from widespread minimally invasive skull base surgical training have led to endoscopic approaches becoming the primary surgical approach of choice in many centers.1–6 Although the endoscopic technique has been widely adopted for its superb balance of exposure, minimal adjacent tissue trauma, and better visualization compared with traditional microscopic transsphenoidal approaches, complications including CSF leak, remain a significant morbidity of the procedure.7,8
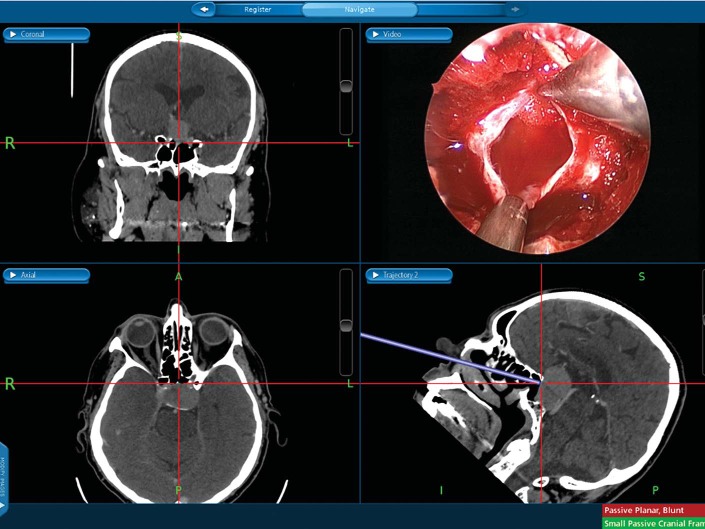
CSF leak is one of the most common complications after pituitary surgery with published rates between 1.8% and 13% since the adoption of endoscopic surgery.9–13 In an effort to further reduce pituitary surgery complications, image-guided surgical navigation systems developed for endoscopic sinus procedures have been used to improve the technical precision of pituitary surgery. Although this technology does not eliminate possible complications, additional information for surgical decision making may be provided, especially in the absence of normal anatomic landmarks.14 Image-guided systems monitor surgical instruments based upon preloaded computed tomography (CT) or magnetic resonance (MR) imaging scans that are registered to a fiduciary device or devices usually attached to the upper face. Instruments are calibrated relative to the device so that continuous information on instrument position and movement of instruments across coronal, axial, and sagittal planes can be provided during the surgical procedure. (Fig. 1). Although this technology has the potential to minimize adjacent tissue trauma and perioperative morbidity,15 its utility in pituitary surgery has not been quantified.
Figure 1.
CT-guided surgical navigation with triplanar imaging and endoscopic view during transsphenoidal pituitary surgery.
Given the low rate of complications and the limited use of surgical navigation systems, the ability to study the effect of image guidance is difficult without data from multiple surgical centers. National databases such as the Nationwide Inpatient Sample (NIS) provide a unique means of studying the effect of image guidance on complications and its potential impact on overall hospital expense. The objectives of the current study are to determine whether image-guided surgical navigation systems reduce the rate of CSF leaks after pituitary surgery and to quantify the relative cost of adding image guidance to these surgeries.
METHODS
The NIS is a national database funded by the United States Agency for Healthcare Research and Quality. It is the largest all-payer inpatient healthcare database in the United States and collects data from a 20% stratified sample of hospitals around the country. Weight coefficients for each hospital are provided to yield national estimates of inpatient stays. Data from admission to discharge are included for each patient in this database including charge and cost data. Financial information was inflation-adjusted to reflect 2013 equivalents.16
NIS data for the years 2007 to 2011 were obtained according to the Agency for Healthcare Research and Quality guidelines. Patients were selected by International Classification of Diseases-9th Revision, Clinical Modification (ICD-9-CM) codes for partial (07.62) or total (07.64) pituitary excisions by a transsphenoidal approach. Given the lack of specificity in ICD-9-CM codes differentiating microscopic and endoscopic techniques, a subanalysis was not possible. Although separate current procedural terminology codes exist for microscopic and endoscopic techniques, the NIS only includes ICD-9-CM codes that do not differentiate between these techniques.
Cases involving image guidance were identified by ICD-9-CM codes 00.31 (computer assisted surgery with CT/CT with angiography) and 00.32 (computer assisted surgery with MR/MR with angiography). It should be noted that these codes are distinct from intraoperative MR scan (88.96) and other tomography of the head (87.04). Our primary outcome measure was CSF leak (349.81 and 997.09). These codes unfortunately do not distinguish between intraoperative leaks and postoperative leaks. Indications for surgery were comprised of benign pituitary lesions (227.3), malignant primary (19.43), malignant secondary (198.89), and unknown behavior (237.0) or unspecified (253.9) pathologies. Symptoms relevant to pituitary conditions were identified including Cushing's syndrome (255.0), acromegaly (253.0), preoperative panhypopituitarism (253.2), and hypothyroidism (244.8, 244.9). The primary endpoints of our study included CSF leak, length of stay, and cost.
Statistical analysis was performed with IBM SPSS for Windows version 22 (IBM Corp., Armonk, NY). Descriptive statistics were performed to characterize our patient population. Pearson χ2 and analysis of variance test were used to compare dichotomized and continuous variables, respectively, between imaging subgroups. Fisher's exact t-test was used for univariate analysis, and p values were always two-tailed and statistically significant below 0.05.
RESULTS
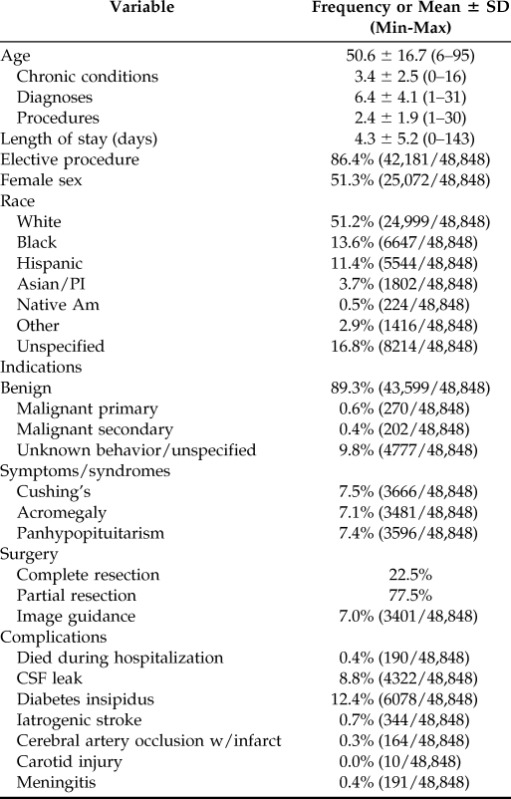
Patient characteristics are listed in Table 1. A total of 48,848 transsphenoidal pituitary resections were performed in the United States from 2007 to 2011, of which 77.5% were partial and 22.5% were complete. The majority of cases were performed for benign indications (89.3%). CSF leak occurred in 8.8% of cases. Carotid artery injury and vision loss rates were below 0.1% in this cohort.
Table 1.
Patient demographics
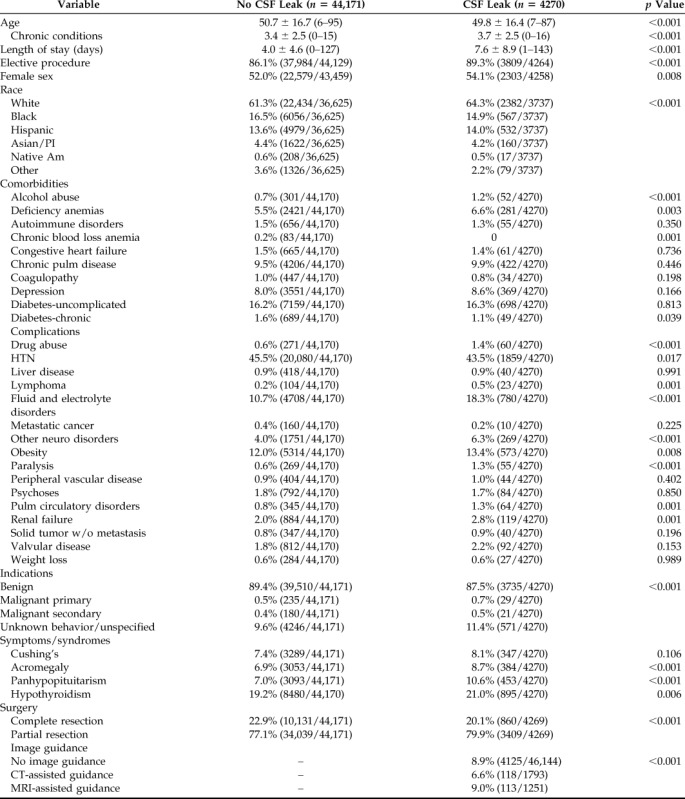
Analysis regarding the effect of image guidance on pituitary surgical patients is displayed in Table 2. CT or MR image guidance was used in 7% of all cases. Mean age was similar regardless of whether CT/MR image guidance or no image guidance was used. CT and MR-assisted categories generally had more symptoms or syndromes related to pituitary disease compared with the patients with no image guidance. Although the MR guidance subjects appeared to have slightly higher comorbidities before surgery, CT and unassisted surgeries were similar.
Table 2.
Analysis of cases by image-guidance modality for all patients
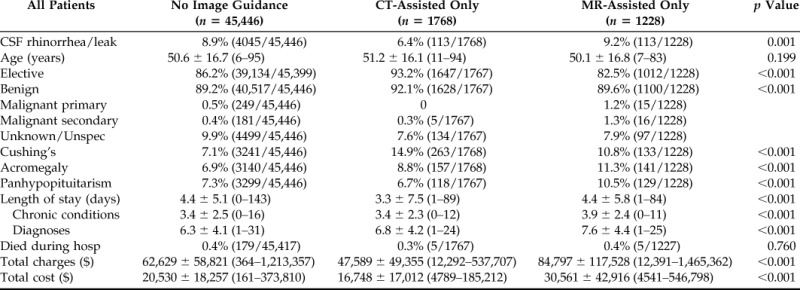
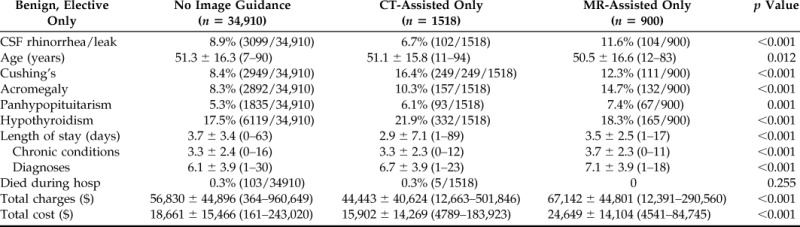
CSF leak rate was significantly higher in subjects who underwent surgery without image guidance when compared with the CT-guided cohort. Interestingly, MR guidance had the worst CSF leak rate of all groups (CT 6.4%, no image guidance 8.9%, MR 9.2%, χ2 p < 0.001). CT-guided surgery had significantly shorter length of stay (2.9 days) versus no image guidance (3.7 days, p < 0.001), lower total charges ($47,589 versus $62,629, p < 0.001), and lower total cost ($16,748 versus $20,530, p < 0.001). MR guidance had the longest length of stay, charge, and cost outcomes. Death during the hospitalization was similar across all three groups. To control for differences in indications for surgery, we performed a subanalysis restricted to benign, elective cases only (Table 3). Rates of CSF leak, length of stay, total charges, and total cost remained significantly lower with CT guidance when compared with no guidance. MR-assisted surgeries continued to have the highest CSF leaks, hospital days, and expense.
Table 3.
Analysis of cases by image guidance modality restricted to benign, elective cases only
Univariate analysis of preoperative risk factors for CSF leak are listed in Table 4. Patients who experienced CSF leak were younger with more chronic conditions, had a significantly longer hospital stay, were more symptomatic at the time of pituitary surgery, and underwent surgery for nonbenign indications. Comorbidities associated with leak were fluid and electrolyte imbalance, obesity, renal failure, pulmonary circulatory disorders, and substance abuse. Surprisingly, diabetes and hypertension were negative predictors of leak.
Table 4.
Univariate analysis of risk factors for cerebrospinal fluid leak
DISCUSSION
Data gleaned from the NIS database suggest that CT-guided transsphenoidal pituitary surgery has significantly lower rates of CSF leak compared with cases that do not employ image guidance. Although it is impossible to derive the reason for decreased CSF leak rate from this analysis, one likely explanation is the bony landmark information provided by CT guidance during pituitary surgery. Technical studies evaluating the accuracy of navigational systems have demonstrated that CT-guided systems are more accurate than MR-guided systems.17 Furthermore, knowledge of the location of nasal and parasellar bony structures facilitates the approach to the pituitary gland, particularly in cases where the mass has not invaded or eroded bone.18 These advantages may also benefit the resection and reconstruction phases of the procedure. It is important to note that cases using CT guidance are more likely to be endoscopic, whereas procedures without image guidance likely represent a mix of microscopic and endoscopic approaches. As such, some proportion of the advantages seen with CT-guided cases may be attributable to the surgical technique rather than the use of image guidance. The few studies that have compared with cost-effectiveness of microscopic and endoscopic approaches report both a decreased cost and better effectiveness using endoscopic surgery.19,20 Future studies that can isolate differences in surgical technique will improve upon established data.
Remarkably, MR-guided surgery had significantly higher rates of CSF leak compared with no image guidance and CT-guided procedures. One possible explanation for this is that MR-assisted patients had more extensive or invasive pituitary disease, thereby necessitating MR imaging to identify soft tissue boundaries. Thus, the MR-guidance cohort could represent patients undergoing extended endoscopic approaches that more often transgress the arachnoid membrane or involve larger tumors requiring more extensive resection and consequently have a higher risk for CSF leak. Furthermore, the presence of significantly higher chronic comorbidities could also factor into worse outcomes. If neither of these factors contribute substantially to the increased rate of CSF leak in MR-assisted cases, then the presence of bony landmark data may indeed improve surgical outcomes. Preoperative CT imaging has demonstrated a greater ability to identify the lateral tumor margins, sellar floor invasion, and clival invasion when compared directly with MR imaging of pituitary adenomas, which may translate into improved surgical navigation.21,22 Unfortunately, this database does not include information on the size of lesion, zones of involvement, or revision surgeries, factors that would aid in isolating a more specific correlation to explain this difference in outcomes.
Although the overall CSF leak rate for this study is consistent with published reports, it is higher than average.9,13,23 This database is likely to underestimate postoperative CSF leak rates because it is restricted to complications that occur during the index hospital stay. In the only other study of transsphenoidal pituitary surgeries using the NIS, their measured end point was limited to CSF rhinorrhea (ICD-9-CM 349.81) and did not include codes for postoperative CSF leak.24 Beyond administrative databases, precise estimates of CSF leak rates are challenging given the relatively low rate of occurrence and the complexities involved in coordinating multicenter studies. Those individual centers that perform transsphenoidal pituitary surgery with sufficient volume may experience lower complication rates than are broadly generalizable across the country.24 Mortality rates seen in this study are in line with most large series at less than 1%.11,24,25
With the adoption of any new technology, a thorough analysis of its impact on overall cost must be carried out, as has been discussed in an article by Jane et al.26 in addition to associated commentaries. In the current study, the addition of CT guidance was associated with lower overall charge and cost. At the operative level, this may include cost savings from shorter operative time.27,28 However, operative time could not be analyzed with the NIS. On a population level, cost savings may have been attributable to lower complication rates and subsequently shorter mean hospital stays. The notion that an investment in surgical efficiency can improve overall costs is counterintuitive but has been shown in other arenas of surgical quality improvement.29–31 These examples highlight the importance of empirically evaluating investments in surgical innovation.
There are important limitations to this study using the NIS. As noted, the NIS is an administrative database that uses ICD-9-CM as its primary medical vocabulary. As such, the ability to differentiate microscopic versus endoscopic cases, determine the size and extent of the lesion, identify revision cases, or distinguish intraoperative CSF leaks from postoperative leaks is not possible. Additionally, this study was a retrospective study and therefore is subject to selection bias. Although the MR guidance group was associated with the worst outcomes, they also had the worst preoperative risk factors. Knowing the extent of disease and the true rate of preventable CSF leaks in addition to the methodology of repair would further refine our analysis. Finally, CSF leak rate may not be the best measure of the efficacy of image-guided surgery. Other endpoints such as completeness of resection, functional improvement in symptoms, time in surgery, and long-term outcomes also factor into the utility of this technology. With these limitations in mind, this study represents the first national analysis of the effect of image-guided surgery for transsphenoidal pituitary adenoma and demonstrates evidence that CT-guided surgery is associated with reduced CSF leak rates, shortened hospital stay, and reduced cost.
CONCLUSION
CT-guided surgery is associated with a lower rate of CSF leak, shorter length of stay, and lower cost compared with patients without image guidance. Although MR-guided surgery demonstrated worse results compared with no image guidance, it is unclear whether this is due to more severe or extensive disease or attributable to the lack of bony landmarks that may bring value to surgical navigation. Further studies that control for severity of disease are warranted to confirm these findings.
Footnotes
Presented at the 60th Annual Meeting of the American Rhinologic Society, September 20, 2014, Orlando, Florida
This work was funded by National Institutes of Health Grant T32CA091078
BA Woodworth is a consultant for Cook Medical, Smith and Nephew, and Olympus. The remaining authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. Chaaban MR, Woodworth BA, Vattoth S, et al. Surgical approaches to central skull base and postsurgical imaging. Semin Ultrasound CT MR 34:476–489, 2013. [DOI] [PubMed] [Google Scholar]
- 2. Daniels DL, Yu S, Pech P, Haughton VM. Computed tomography and magnetic resonance imaging of the orbital apex. Radiol Clin North Am 25:803–817, 1987. [PubMed] [Google Scholar]
- 3. Demirci HSC, Shields JA, Honavar SG, et al. Orbital tumors in the older adult population. Ophthalmology 109:51–56, 2002. [DOI] [PubMed] [Google Scholar]
- 4. Rootman J. Diseases of the Orbit: A Multidisciplinary Approach. Philadelphia, PA: Lippincott Williams & Wilkins, 2003. [Google Scholar]
- 5. Illing E, Chaaban MR, Riley KO, Woodworth BA. Porcine small intestine submucosal graft for endoscopic skull base reconstruction. Int Forum Allergy Rhinol 3:928–932, 2013. [DOI] [PubMed] [Google Scholar]
- 6. Virgin FW, Bleier BS, Woodworth BA. Evolving materials and techniques for endoscopic sinus surgery. Otolaryngol Clin North Am 43:653–672, xi, 2010. [DOI] [PubMed] [Google Scholar]
- 7. Chaaban MR, Woodworth BA. Complications of skull base reconstruction. Adv Otorhinolaryngol 74:148–162, 2013. [DOI] [PubMed] [Google Scholar]
- 8. Alexander NS, Chaaban MR, Riley KO, Woodworth BA. Treatment strategies for lateral sphenoid sinus recess cerebrospinal fluid leaks. Arch Otolaryngol Head Neck Surg 138:471–478, 2012. [DOI] [PubMed] [Google Scholar]
- 9. Fatemi N, Dusick JR, De Paiva Neto MA, Kelly DF. The endonasal microscopic approach for pituitary adenomas and other parasellar tumors: A 10-year experience. Neurosurgery 63:ONS244–ONS256, 2008. [DOI] [PubMed] [Google Scholar]
- 10. Casler JD, Doolittle AM, Mair EA. Endoscopic surgery of the anterior skull base. Laryngoscope 115:16–24, 2005. [DOI] [PubMed] [Google Scholar]
- 11. Kassam AB, Prevedello DM, Carrau RL, et al. Endoscopic endonasal skull base surgery: Analysis of complications in the authors' initial 800 patients. J Neurosurg 114:1544–1568, 2011. [DOI] [PubMed] [Google Scholar]
- 12. Sudhakar N, Ray A, Vafidis JA. Complications after trans-sphenoidal surgery: Our experience and a review of the literature. Br J Neurosurg 18:507–512, 2004. [DOI] [PubMed] [Google Scholar]
- 13. Gondim JA, Schops M, de Almeida JP, et al. Endoscopic endonasal transsphenoidal surgery: Surgical results of 228 pituitary adenomas treated in a pituitary center. Pituitary 13:68–77, 2010. [DOI] [PubMed] [Google Scholar]
- 14. Woodworth BA, Davis GW, Schlosser RJ. Comparison of laser versus surface-touch registration for image-guided sinus surgery. Am J Rhinol 19:623–626, 2005. [PubMed] [Google Scholar]
- 15. Dalgorf DM, Sacks R, Wormald PJ, et al. Image-guided surgery influences perioperative morbidity from endoscopic sinus surgery: A systematic review and meta-analysis. Otolaryngol Head Neck Surg 149:17–29, 2013. [DOI] [PubMed] [Google Scholar]
- 16. Bureau of Labor Statistics. Consumer price index. Available at http://www.bls.gov/cpi Accessed January 18, 2014.
- 17. Dorward NL, Alberti O, Palmer JD, et al. Accuracy of true frameless stereotaxy: In vivo measurement and laboratory phantom studies. J Neurosurg 90:160–168, 1999. [DOI] [PubMed] [Google Scholar]
- 18. Wang YY, Thiryayi WA, Ramaswamy R, Gnanalingham KK. Accuracy of surgeon's estimation of sella margins during endoscopic surgery for pituitary adenomas: Verification using neuronavigation. Skull Base 21:193–200, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Rudmik L, Starreveld YP, Vandergrift WA, et al. Cost-effectiveness of the endoscopic versus microscopic approach for pituitary adenoma resection. Laryngoscope 125:16–24, 2015. [DOI] [PubMed] [Google Scholar]
- 20. Ament JD, Yang Z, Tertulien P, Shahlaie K. Comparing the cost-effectiveness of endoscopic and microscopic approaches to transphenoidal pituitary surgery. J Neurol Surg B 75:A044, 2014. [Google Scholar]
- 21. Chen X, Dai J, Ai L, et al. Clival invasion on multi-detector CT in 390 pituitary macroadenomas: Correlation with sex, subtype and rates of operative complication and recurrence. Am J Neuroradiol 32:785–789, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Miki Y, Kanagaki M, Takahashi JA, et al. Evaluation of pituitary macroadenomas with multidetector-row CT (MDCT): Comparison with MR imaging. Neuroradiology 49:327–333, 2007. [DOI] [PubMed] [Google Scholar]
- 23. Shiley SG, Limonadi F, Delashaw JB, et al. Incidence, etiology, and management of cerebrospinal fluid leaks following trans-sphenoidal surgery. Laryngoscope 113:1283–1288, 2003. [DOI] [PubMed] [Google Scholar]
- 24. Barker FG, 2nd, Klibanski A, Swearingen B. Transsphenoidal surgery for pituitary tumors in the United States, 1996–2000: Mortality, morbidity, and the effects of hospital and surgeon volume. J Clin Endocrinol Metab 88:4709–4719, 2003. [DOI] [PubMed] [Google Scholar]
- 25. Tabaee A, Anand VK, Barrón Y, et al. Endoscopic pituitary surgery: A systematic review and meta-analysis. J Neurosurg 111:545–554, 2009. [DOI] [PubMed] [Google Scholar]
- 26. Jane JA, Jr, Thapar K, Alden TD, Laws ER., Jr Fluoroscopic frameless stereotaxy for transsphenoidal surgery. Neurosurgery 48:1302–1307, discussion 1307–1308, 2001. [DOI] [PubMed] [Google Scholar]
- 27. Lasio G, Ferroli P, Felisati G, Broggi G. Image-guided endoscopic transnasal removal of recurrent pituitary adenomas. Neurosurgery 51:132–137; discussion 136–137, 2002. [DOI] [PubMed] [Google Scholar]
- 28. Gong J, Mohr G, Vezina JL. Endoscopic pituitary surgery with and without image guidance: An experimental comparison. Surg Neurol 67:572–578, discussion 578, 2007. [DOI] [PubMed] [Google Scholar]
- 29. Scalea TM, Carco D, Reece M, et al. Effect of a novel financial incentive program on operating room efficiency. JAMA Surg 149:920–924, 2014. [DOI] [PubMed] [Google Scholar]
- 30. Stockert EW, Langerman A. Assessing the magnitude and costs of intraoperative inefficiencies attributable to surgical instrument trays. J Am Coll Surg 219:646–655, 2014. [DOI] [PubMed] [Google Scholar]
- 31. Chung TK, Rosenthal EL, Magnuson JS, Carroll WR. Transoral robotic surgery for oropharyngeal and tongue cancer in the United States. Laryngoscope 125:140–145, 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]