Abstract
Chronic obstructive pulmonary disease (COPD) is a progressive and debilitating respiratory condition that leads to significant burden, both medically and financially. It affects millions of people worldwide and causes significant morbidity and mortality. Most detailed information related to its prevalence, morbidity, and mortality comes from high-income countries, but 90% of COPD-related deaths occur in low- and middle-income countries. Cigarette smoking is the main risk factor for developing COPD, but other risk factors do exist and need to be recognized. A majority of morbidity and mortality as well as health care costs occur from acute exacerbations of COPD with a known phenotype of patients being “frequent exacerbators.” Health care costs for COPD are not only from treatment of exacerbations, such as hospitalization, but also medication costs for maintenance therapy and outpatient treatment. COPD has been linked with many comorbidities leading to significant burden of disease. The goal of this review is to evaluate the overall burden of disease including prevalence, morbidity, mortality, health care costs, and economic costs.
Keywords: Pulmonary disease, chronic obstructive, asthma, bronchitis, spirometry, smoking, tobacco, cost of illness, morbidity, mortality, prevalence
Chronic obstructive pulmonary disease (COPD) is a progressive, debilitating respiratory condition and is thought to be the most important respiratory disease globally.1–4 Previously, it was thought that COPD would be ranked fifth in overall burden of disease and third in mortality worldwide by 2020.3,5–7 However, COPD met this mark in the United States (U.S.) much earlier in 2008 and surpassed stroke becoming the third leading cause of mortality.3,6 Worldwide, 4.5 million people died from COPD in 2008,8 and in contrast to coronary heart disease and stroke, it is the only leading cause of death that is still increasing.3,9 In the U.S., COPD results in 15.4 million physician visits, 1.5 million emergency department (ED) visits, and 726,000 hospitalizations each year.10 The National Heart, Lung, and Blood Institute estimated that there were 14.8 million people in the U.S. with physician-diagnosed COPD and another 12 million with undiagnosed COPD.9 The worldwide unadjusted annual death rate for COPD in 2008 was 45.3 per 100,000 population.3,6 However, COPD mortality is hard to assess worldwide, due to nomenclature inconsistencies COPD is not being listed as the cause of death on death certificates; for this reason, COPD mortality is likely underestimated.
Cigarette use is the most common risk factor for developing COPD, with patients more likely to have COPD if they smoked one pack-per-day for 20 years or more.3,6 Another important and established aspect is that COPD is underdiagnosed in the general population. A recent study has shown even the most severe COPD patients are treated with medications only 50% of the time.4 Currently, there is no cure, but the overall management goal is to improve health status, prevent exacerbations, and prevent COPD-related complications and mortality.3 The aim of this review is to evaluate the overall burden of disease, including prevalence, morbidity, mortality, health care, and economic costs.
PREVALENCE
An estimated 64–210 million people worldwide are living with a diagnosis of COPD. This substantial population affected with COPD is expected to increase.1–4 Most detailed information about prevalence, morbidity, and mortality is from high-income countries, but 90% of COPD-related deaths occur in low- and middle-income countries.1 Different studies in the U.S. have determined COPD prevalence to be between 5%–10%.9,11 In 2011, the Behavior Risk Factor Surveillance System conducted a telephone survey of adults in the U.S. Of the responders, 6.3% stated that he or she had been diagnosed with COPD, which can be extrapolated to approximately 15 million people.12 This same study evaluated risk factors associated with COPD (Table 1).12 Additionally, a systematic review and metaanalysis was performed looking at articles from 1990 to 2004 and determined the overall pooled prevalence of COPD was 7.6% with similar risk factors (Table 1). Once again, most of this data is from Europe and North America and lacking data from other regions that may have higher mortality.13
Table 1.
Common risk factors for the development of COPD from two different studies

Common risk factors for the development of chronic obstructive pulmonary disease (COPD) from the Behavior Risk Factor Surveillance System (BFRSS) study done in the United States (U.S.)12 and from a systematic review that included 28 different countries.13 Common risk factors that were reported include older age, active smokers, but different in gender and location.
COPD was thought to affect men and women equally, but studies have noted COPD may be more prevalent in women and, perhaps, more difficult to treat.1,12,14 Data from the U.S. showed more women than men died from COPD in 2000 with previously more men dying than women.10 The diagnosis of COPD in females increased in the United Kingdom as well as Canada, whereas rates of diagnosis have plateaued in males.14,15
Recent studies have shown more severe disease than previously noted in both smokers and nonsmokers with a substantial prevalence (3%–11%) in life-long nonsmokers, most likely related to nontobacco environmental exposures or infectious etiologies.16
As noted, COPD is under diagnosed and may be related to patients failing to recognize early symptoms and restrict activities to avoid symptoms.17,18 Delays in diagnosis may result in quicker progression of COPD and inefficient or inappropriate consumption of health care services as diagnosis usually occurs when a patient has lost 50% or more of original lung capacity.19 A high-risk population study of smokers older than 39 previously not diagnosed with COPD found obstruction in 24.3% of these patients, and even more interesting, obstruction was found in 14.4% of life-long nonsmokers.20
RISK FACTORS
Tobacco is still the main risk factor for COPD. Daily cigarette consumption peaked in the 1970's for males and in the 1980's for females,21 but smoking prevalence has decreased in both groups recently, likely the result of large-scale antismoking activities.22 Unfortunately, 20.6% of the U.S. adult population still smokes,23 with more than 293 billion cigarettes purchased in the U.S. in 2011.24
Rate of death from COPD continues to increase among both female and male smokers,22 with the relative risk of death in both female and male smokers doubling from the 1980s to the 2000s (9.98 versus 25.61).22 It is important to note that females have more difficulty with quitting than men,22 but quitting smoking at any age dramatically lowers the mortality risk with the ability to nearly avoid all the excess-smoking-related deaths if cessation is achieved by age 40 (Fig. 1).22,25,26 This highlights the importance of tobacco cessation in the primary treatment of COPD. All at-risk patients need evaluation for COPD in the primary care setting with many diagnoses missed in this setting.27 Cigarettes are not the only causal factor. This is apparent especially in younger patients, females and people who reside in developing countries.11
Figure 1.
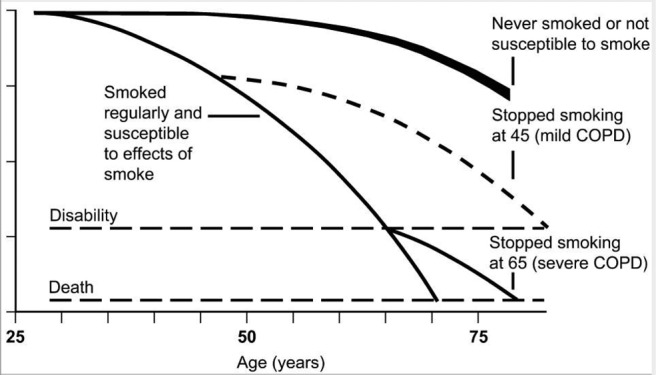
Cessation of smoking in patients with COPD reduces the mortality risk if achieved by age 40. This representation is one of multiple Fletcher-Peto curves that was reprinted by permission from Ref.25
The high prevalence of COPD in life-long nonsmokers may be related to in utero exposure to tobacco,28,29 but other possible etiologies include occupational exposures, traffic pollution, other outdoor pollution, and secondhand smoke exposure as well as risk factors associated with urbanization. These risk factors are underappreciated for the development of COPD.30–32 Indoor pollution from biomass cooking and heating is another risk with 3 billion people worldwide using this as their main energy source.33,34 In addition, rare inherited disorders such as α-1 antitrypsin deficiency are well-characterized risk factors for development of COPD.11
GLOBAL INITIATIVE FOR OBSTRUCTIVE LUNG DISEASE (GOLD)
GOLD is an organization that raises awareness about COPD that first published GOLD guidelines in 2001 and focused primarily on the severity of obstruction based on the patient's forced expiratory volume in one second (FEV1) (Fig. 2). However, since then, it has been noted that there are many different phenotypes within COPD and that FEV1 is not the only variable to evaluate. The updated GOLD guidelines in 2011 stratify COPD severity using FEV1, but also daily symptoms that impact quality of life and history of exacerbations (Fig. 3).4,5 The FEV1 severity alone is a limited predictor of disease status, including the burden of disease, symptoms, and activity limitations as well as future risk of exacerbations.5 With the new stratification, daily symptoms are assessed with validated tests, including the modified Medical Research Council dyspnea scale or COPD Assessment Test score. A study looked at the two versions printed in 2007 (Fig. 2) and 2011 (Fig. 3) and found that the 2011 version does predict exacerbations better, but the 2007 version predicts prognosis better.4
Figure 2.
GOLD grading of severity of airflow limitation in COPD based on 2007 guidelines. All patients had FEV1/FVC (forced vital capacity) less than 0.70.
Figure 3.
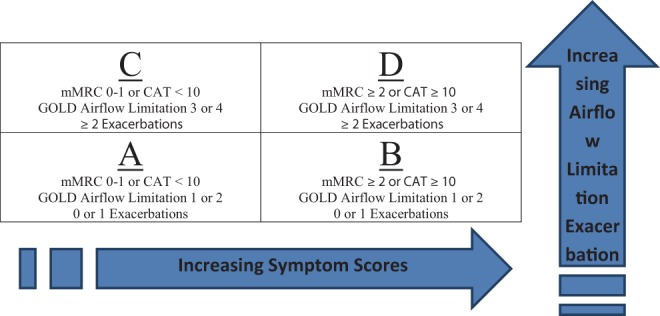
GOLD stratification of COPD guidelines for 2011 using symptoms scores, airflow limitation, and number of exacerbations. Symptom scores use either modified Medical Research Council (mMRC) or COPD Assessment Test (CAT).
MORBIDITY AND MORTALITY
Morbidity includes symptoms, health care visits, and quality of life related to COPD. Dyspnea is a poor prognostic sign based on survival being significantly less in patients with GOLD grades B and D (Fig. 3). This brings to light the need to evaluate for symptoms, as well as other comorbidities, that can lead to dyspnea.4 The Behavior Risk Factor Surveillance System survey collected more information related to morbidity. It found that of the people with COPD, 64.2% had shortness of breath that impaired their quality of life, 43.2% visited a provider for COPD-related symptoms in the last year, and 17.7% had been seen in the ED or admitted to the hospital for COPD.12 It has been well documented that quality of life is reduced in patients with COPD. This is more dramatic in patients with more severe disease and frequent exacerbations.35,36 Overall, morbidity increases with age in COPD patients and may be affected by other comorbid conditions.11,37,38
COPD has been associated with multiple comorbidities (Table 2).3,4,39–42 In a Canadian study, 95% of the patients had one or more comorbidities, with cardiovascular being the most common (75.1%).40 Mental health comorbidities are associated with and exacerbate COPD. For example, one study found only 1.5% of COPD patients suffered from substance abuse but had the largest association with increased hospital admission.41 In addition, COPD patients commonly experience psychological comorbidities,39 such as anxiety,42 with 10%–55% of patients having clinical anxiety disorders.43,44 Anxiety is known to affect functional status, health-related quality of life, and health care use.45 A study interviewed 14 patients with stable COPD and found that anxiety was both a symptom and a cause of breathlessness.45
Table 2.
Comorbidities that have been associated with COPD
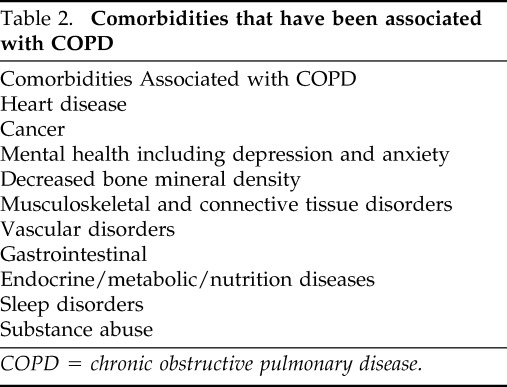
COPD = chronic obstructive pulmonary disease.
COPD causes significant mortality worldwide, but it is hard to obtain accurate data worldwide.46,47 Statistics note that COPD is the fourth leading cause of death worldwide in 2004, leading to 3 million deaths. In 2008, this increased to 4.5 million deaths.8 This burden is expected to increase with some estimating 5.8 million deaths per year by 2030.1 In the U.S., COPD accounted for 56.7% of deaths related to lung diseases and deaths from COPD have increased, especially in females, over the last 20 years.9,11 As of 2008, COPD is the third leading cause of death and now more women than men die from COPD.48,49 The relative risk of mortality from COPD in current smokers compared with nonsmokers is 25.61 for men and 22.35 for women with mortality continuing to rise in both.22
Outside of the U.S., different regions have significantly higher mortality associated with COPD. Africa and Asia currently account for almost 90% of COPD deaths worldwide with China being affected the most.6,50–52
EXACERBATIONS
Exacerbations negatively affect patients' quality of life and increase their risk of death.35,53–56 After an exacerbation, symptoms and lung function take several weeks to recover,57 and exacerbations accelerate the rate of irreversible worsening pulmonary function.39,55,58 These not only lead to decline in lung function, but treatment of exacerbations in the hospital is costly. In Canada, COPD is the third leading cause of hospitalizations for men.55 A study published in 2010 described and characterized the costs of COPD in the hospital. It looked at 602 hospitals and calculated the costs for COPD-related visits based on rates for 2008 in the U.S. It determined the mean cost of an ED visit, simple admission, and complex admissions to be $6467, $7242, and $20,757, respectively. Intensive care unit admission with intubation was the most expensive at $44,909.59 A similar study out of Canada looked at moderate to severe COPD patients and determined the mean cost per exacerbation was $3036 Canadian dollars with hospitalization representing 80% of the total.40
There also seem to be two COPD populations: patients with frequent exacerbations and patients that do not have exacerbations. These phenotypes are highlighted in the new GOLD criteria (Fig. 3). Frequent exacerbators cohort had 2.5 exacerbations per person-years,39 and the likelihood of having another exacerbation increased with a history of two or more exacerbations in the previous year and/or increasing severity of disease.4,40 Exacerbations are treated with oral corticosteroids, which have shown to decrease the burden of exacerbations by shortening recovery time, improvement of lung function, and arterial hypoxemia. They also reduce the risk of relapse, treatment failure, and the length of hospital stay, all reducing the overall cost.5 Along with oral corticosteroids, antibiotics are used to treat exacerbations.60–63 Short-term mortality is reduced by 77% and treatment failure by 53%64,65 using antibiotics. Unfortunately, it has been found that patients are significantly undertreated for exacerbations with only 71% receiving oral corticosteroids if hospitalized and 43% if seen in an outpatient office, but 80% received antibiotics in both groups.39 This data suggest significant opportunity to improve both inpatient and outpatient management of COPD exacerbations.
HOSPITALIZATION
Hospitalizations are a major factor in the burden of disease in COPD as noted with acute exacerbations. Interestingly, hospitalization is higher in patients with GOLD grade B compared with C because of increased cardiac involvement and older age.4 In 2000, patients with physician-diagnosed COPD required 726,000 hospitalizations in the U.S.10 In 2009, the National Heart, Lung, and Blood Institute determined that the hospitalization rate per 10,000 population for COPD was 30.1 for 45–64 years old and 121.3 for people 65 years or older. A recent study performed in North Carolina found that there were 33,799 patients with diagnosed COPD and 97,511 COPD-related ED visits. This is equal to 13.8 ED visits per 1000 person years. In addition, 7% of these patients had a return ED visit within 30 days of their index visit, and 28% had a repeat visit within the same year.41 This study also found 51% of patients with COPD were admitted to the hospital from the original ED visit, which is two times more than all ED visits made by age-matched controls.41 Subsequent hospital admission risk increased with age, patients with congestive heart failure, substance-related disorders, or had respiratory failure and/or supplemental oxygen.41 The previously mentioned study looking at costs for treatment of exacerbations also found the mean length of stay ranged from 4.5 days (standard deviation 3.3) for simple admissions to 16.0 days (standard deviation 16.7) for intensive care unit stays.59 Death rates varied, which occurred in 0.9% of simple admission compared with 26.5%–39.1% for admissions with intubations.59 Conclusively, patients with COPD have frequent ED visits, higher rates of hospitalizations compared with controls, and readmission is common. In addition, length of stay and mortality increase in more severe exacerbations.
ECONOMIC COSTS
Health Care Costs
Higher health care costs are associated with COPD maintenance treatment and even more so with the treatment of acute exacerbations. In Canada, patients with COPD were enrolled in a study for three months to assess health care costs. It found the mean annual total COPD-related cost per patient to be $4147 (±$6255). Both the costs for maintenance therapy and acute treatment increased as severity level increased.40 An interesting retrospective case-control study looked at the cost of health care 36 months before the diagnosis of COPD. COPD patients used 1.5–1.6 times more ED services and inpatient services and had more outpatient visits.66 There was a marked increase use of these services the month before diagnosis, suggesting that patients are not diagnosed until they experience acute exacerbations or a sudden change in respiratory status. Even when adjusting for higher incidence of comorbidities in these patients, having a COPD diagnosis was associated with significantly higher resource use and treatment cost.66 Economic burden from COPD is expected to increase secondary to the aging population, tobacco use, and air pollution.67 A recent review looked at studies that evaluated economic costs in elderly patients specifically and found a trend of direct cost growth in this population.67
In 2010, the estimated total cost of COPD in the U.S. was $36 billion with $32.1 billion related to health care costs directly.68 Along with the burden of disease and treatment costs, research funding directed at COPD is also costly. In 2013, the National Institute of Health funded $102 million for COPD research. However, this is significantly less than the $1.9 billion for cardiovascular disease and $282 million for stroke, even though the rate of death from these diseases is decreasing unlike COPD.69
Medication Costs
Medication costs contribute to the overall health care costs associated with COPD. It is important to note that medication costs related to smoking cessation are cost effective, especially when paired with counseling.70 Electronic cigarettes have become a very popular smoking cessation aid in the general population and now a billion-dollar industry. This was recently reviewed in detail by Nickels et al.71
Medication costs also increase with severity. When evaluated according to GOLD severity, the percentage of patients taking inhaled corticosteroid/long-acting β-agonist (LABA) combination, LABA and long-acting anticholinergic medications was greater in patients with more severe COPD.40 In the Canadian study, 70% of the $2475 per patient was from medication for maintenance treatment in moderate to severe COPD patients.40 In the U.S., prescription costs for COPD in 2008 were $20.4 billion.9 Costs for maintenance medication can be elevated due to incorrect medication use. This same study found that under one-third of patients with either GOLD stage, one or two had more than two acute exacerbations in the previous year. However, over two-thirds of these same patients were on a combination inhaled corticosteroid with LABA inhaler, interventions recommended for more severe disease.40 Overall, mild to moderate COPD is more common than severe COPD, but if providers are using medicine incorrectly in this group, there will be increased cost for the treatment of this population.40
CONCLUSION
Overall, COPD is associated with significant morbidity, mortality, health-care use and reduced quality of life. With this comes increased health care cost and burden on the health care system. It is a serious public health burden that needs to be addressed in the U.S. and worldwide with the goal to prevent COPD, reduce costs associated with the disease, and in the end, improve the patient's quality of life.
Footnotes
Presented at the Eastern Allergy Conference, May 31, 2014, Palm Beach, Florida
The authors have no conflicts of interest to declare pertaining to this article
REFERENCES
- 1. World Health Organization. The global burden of disease: 2004 update. 2008. Available at www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf Accessed June 11, 2014.
- 2. Chronic Obstructive Pulmonary Disease (COPD). Available at http://www.cdc.gov/copd/data.htm Accessed June 11, 2014.
- 3. Michalski JM. Prostaglandin E2 signaling in human lung fibroblasts: mechanisms of signal attenuation and implications in chronic lung diseases. ProQuest, UMI Dissertation Publishing, 2011. [Google Scholar]
- 4. Lange P, Marott JL, Vestbo J, et al. Prediction of the clinical course of chronic obstructive pulmonary disease, using the new GOLD classification: a study of the general population. Am J Respir Crit Care Med 186:975–981, 2012. [DOI] [PubMed] [Google Scholar]
- 5. Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 187:347–365, 2013. [DOI] [PubMed] [Google Scholar]
- 6. Rabe KF, Hurd S, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med 176:532–555, 2007. [DOI] [PubMed] [Google Scholar]
- 7. Calverley PM, Walker P. Chronic obstructive pulmonary disease. Lancet 362:1053–1061, 2003. [DOI] [PubMed] [Google Scholar]
- 8. World Helath Organization. Global status report on noncommunicable diseases 2010. Geneva, 2011. Available at http://www.who.int/nmh/publications/ncd_report2010/en/ Accessed June 23, 2014. [Google Scholar]
- 9. National Heart, Lung and Blood Institute. Morbidity and Mortality: 2012 chartbook on Cardiovascular, lung, and blood diseases. 2012. Available at http://www.nhlbi.nih.gov/resources/docs/2012_ChartBook_508.pdf Accessed June 23, 2014.
- 10. Mannino DM, Homa DM, Akinbami LJ, et al. Chronic obstructive pulmonary disease surveillance–United States, 1971–2000. MMWR Surveill Summ 51:1–16, 2002. [PubMed] [Google Scholar]
- 11. Eisner MD, Anthonisen N, Coultas D, et al. An official American Thoracic Society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 182:693–718, 2010. [DOI] [PubMed] [Google Scholar]
- 12. Centers for Disease Control and Prevention. Chronic obstructive pulmonary disease among adults — United States, 2011. 2012. Available at http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6146a2.htm Accessed June 11, 2014.
- 13. Halbert RJ, Natoli JL, Gano A, et al. Global burden of COPD: systematic review and meta-analysis. Eur Respir J 28:523–532, 2006. [DOI] [PubMed] [Google Scholar]
- 14. Soriano JB, Maier WC, Egger P, et al. Recent trends in physician diagnosed COPD in women and men in the UK. Thorax 55:789–794, 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sørheim IC, Johannessen A, Gulsvik A, et al. Gender differences in COPD: are women more susceptible to smoking effects than men? Thorax 65:480–485, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Buist AS, McBurnie MA, Vollmer WM, et al. , BOLD Collaborative Research Group. International variation in the prevalence of COPD (the BOLD Study): a population-based prevalence study. Lancet 370:741–750, 2007. [DOI] [PubMed] [Google Scholar]
- 17. Rennard SI, Farmer SG. COPD in 2001: a major challenge for medicine, the pharmaceutical industry, and society. Chest 121:113S–115S, 2002. [DOI] [PubMed] [Google Scholar]
- 18. Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects' perspective of Confronting COPD International Survey. Eur Respir J 20:799–805, 2002. [DOI] [PubMed] [Google Scholar]
- 19. Ferguson GT, Petty TL. Screening and early intervention for COPD. Hosp Pract 1998;33:67–72, 9,–80, 3; discussion 3–4, 1995. [DOI] [PubMed] [Google Scholar]
- 20. Zieliñski J, Bednarek M, and Know the Age of Your Lung Study Group. Early detection of COPD in a high-risk population using spirometric screening. Chest 119:731–736, 2001. [DOI] [PubMed] [Google Scholar]
- 21. National Cancer Institute. Changes in number of cigarettes smoked per day: cross-sectional and birth cohort analyses using NHIS. 2003. Available at http://cancercontrol.cancer.gov/brp/tcrb/monographs/15/monograph15-chapter7.pdf Accessed June 23, 2014.
- 22. Thun MJ, Carter BD, Feskanich D, et al. 50-year trends in smoking-related mortality in the United States. N Engl J Med 368:351–364, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Pleis JR, Lucas JW, Ward BW. Summary health statistics for U.S. adults: National Health Interview Survey, 2008. Vital Health Stat 10:1–157, 2009. [PubMed] [Google Scholar]
- 24. Economic Facts About U.S. Tobacco Production and Use. 2014. Available at http://www.cdc.gov/tobacco/data_statistics/fact_sheets/economics/econ_facts/ Accessed August 20, 2014.
- 25. Fletcher C, Peto R. The natural history of chronic airflow obstruction. Br Med J 1:1645–1648, 1977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rennard SI, Vestbo J. Natural histories of chronic obstructive pulmonary disease. Proc Am Thorac Soc 5:878–883, 2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Hill K, Goldstein RS, Guyatt GH, et al. Prevalence and underdiagnosis of chronic obstructive pulmonary disease among patients at risk in primary care. CMAJ 182:673–678, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Holt PG. Immune and inflammatory function in cigarette smokers. Thorax 42:241–249, 1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Tager IB, Ngo L, Hanrahan JP. Maternal smoking during pregnancy. Effects on lung function during the first 18 months of life. Am J Respir Crit Care Med 152:977–983, 1995. [DOI] [PubMed] [Google Scholar]
- 30. Hnizdo E, Sullivan PA, Bang KM, Wagner G. Airflow obstruction attributable to work in industry and occupation among U.S. race/ethnic groups: a study of NHANES III data. Am J Ind Med 46:126–135, 2004. [DOI] [PubMed] [Google Scholar]
- 31. Matheson MC, Benke G, Raven J, et al. Biological dust exposure in the workplace is a risk factor for chronic obstructive pulmonary disease. Thorax 60:645–651, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Trupin L, Earnest G, San Pedro M, et al. The occupational burden of chronic obstructive pulmonary disease. Eur Respir J 22:462–469, 2003. [DOI] [PubMed] [Google Scholar]
- 33. Torres-Duque C, Maldonado D, Pérez-Padilla R, et al. , Forum of International Respiratory Studies (FIRS) Task Force on Health Effects of Biomass Exposure. Biomass fuels and respiratory diseases: a review of the evidence. Proc Am Thorac Soc 5:577–590, 2008. [DOI] [PubMed] [Google Scholar]
- 34. Orozco-Levi M, Garcia-Aymerich J, Villar J, et al. Wood smoke exposure and risk of chronic obstructive pulmonary disease. Eur Respir J 27:542–546, 2006. [DOI] [PubMed] [Google Scholar]
- 35. Seemungal TA, Donaldson GC, Paul EA, et al. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 157:1418–1422, 1998. [DOI] [PubMed] [Google Scholar]
- 36. Gore JM, Brophy CJ, Greenstone MA. How well do we care for patients with end stage chronic obstructive pulmonary disease (COPD)? A comparison of palliative care and quality of life in COPD and lung cancer. Thorax 55:1000–1006, 2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Celli BR, Halbert RJ, Nordyke RJ, Schau B. Airway obstruction in never smokers: results from the Third National Health and Nutrition Examination Survey. Am J Med 118:1364–1372, 2005. [DOI] [PubMed] [Google Scholar]
- 38. Lamprecht B, McBurnie MA, Vollmer WM, et al. COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest 139:752–763, 2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. FitzGerald JM, Haddon JM, Bradly-Kennedy C, et al. , RUSIC Study Group. Resource use study in COPD (RUSIC): a prospective study to quantify the effects of COPD exacerbations on health care resource use among COPD patients. Can Respir J 14:145–152, 2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Maleki-Yazdi MR, Kelly SM, Lam SY, et al. The burden of illness in patients with moderate to severe chronic obstructive pulmonary disease in Canada. Can Respir J 19:319–324, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Yeatts KB, Lippmann SJ, Waller AE, et al. Population-based burden of COPD-related visits in the ED: return ED visits, hospital admissions, and comorbidity risks. Chest 144:784–793, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Yohannes AM, Willgoss TG, Baldwin RC, Connolly MJ. Depression and anxiety in chronic heart failure and chronic obstructive pulmonary disease: prevalence, relevance, clinical implications and management principles. Int J Geriatr Psychiatry 25:1209–1221, 2010. [DOI] [PubMed] [Google Scholar]
- 43. Aghanwa HS, Erhabor GE. Specific psychiatric morbidity among patients with chronic obstructive pulmonary disease in a Nigerian general hospital. J Psychosom Res 50:179–183, 2001. [DOI] [PubMed] [Google Scholar]
- 44. Vögele C, von Leupoldt A. Mental disorders in chronic obstructive pulmonary disease (COPD). Respir Med 102:764–773, 2008. [DOI] [PubMed] [Google Scholar]
- 45. Willgoss TG, Yohannes AM, Goldbart J, Fatoye F. “Everything was spiraling out of control”: experiences of anxiety in people with chronic obstructive pulmonary disease. Heart Lung 41:562–571, 2012. [DOI] [PubMed] [Google Scholar]
- 46. Tálamo C, de Oca MM, Halbert R, et al. Diagnostic labeling of COPD in five Latin American cities. Chest 131:60–67, 2007. [DOI] [PubMed] [Google Scholar]
- 47. Peña VS, Miravitlles M, Gabriel R, et al. Geographic variations in prevalence and underdiagnosis of COPD: results of the IBERPOC multicentre epidemiological study. Chest 118:981–989, 2000. [DOI] [PubMed] [Google Scholar]
- 48. Kochanek KD, XJ, Murphy SL, Miniño AM, Kung H. Deaths: final data for 2009. Natl Vital Stat Rep 60:1–116, 2011. [PubMed] [Google Scholar]
- 49. Mannino DM. COPD: epidemiology, prevalence, morbidity and mortality, and disease heterogeneity. Chest 121:121S–126S, 2002. [DOI] [PubMed] [Google Scholar]
- 50. Chan-Yeung M, Aït-Khaled N, White N, et al. The burden and impact of COPD in Asia and Africa. Int J Tuberc Lung Dis 8:2–14, 2004. [PubMed] [Google Scholar]
- 51. Gonzalez-Pier E, Gutierrez-Delgado C, Stevens G, et al. [Priority setting for health interventions in Mexico's System of Social Protection in Health]. Salud Publica Mex 49(Suppl. 1):S37–S52, 2007. [PubMed] [Google Scholar]
- 52. Jamison DT. Investing in Health. In Disease Control Priorities in Developing Countries. Jamison DT, Breman JG, Measham AR, et al. (Eds) 2nd ed Washington, DC, 2006. [PubMed] [Google Scholar]
- 53. Kessler R, Ståhl E, Vogelmeier C, et al. Patient understanding, detection, and experience of COPD exacerbations: an observational, interview-based study. Chest 130:133–142, 2006. [DOI] [PubMed] [Google Scholar]
- 54. Spencer S, Calverley PM, Burge PS, Jones PW. Impact of preventing exacerbations on deterioration of health status in COPD. Eur Respir J 23:698–702, 2004. [DOI] [PubMed] [Google Scholar]
- 55. Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax 57:847–852, 2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, et al. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax 60:925–931, 2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Seemungal TA, Donaldson GC, Bhowmik A, et al. Time course and recovery of exacerbations in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 161:1608–1613, 2000. [DOI] [PubMed] [Google Scholar]
- 58. Kanner RE, Anthonisen NR, Connett JE. Lower respiratory illnesses promote FEV(1) decline in current smokers but not ex-smokers with mild chronic obstructive pulmonary disease: results from the lung health study. Am J Respir Crit Care Med 164:358–364, 2001. [DOI] [PubMed] [Google Scholar]
- 59. Dalal AA, Shah M, D'Souza AO, Rane P. Costs of COPD exacerbations in the emergency department and inpatient setting. Respir Med 105:454–460, 2011. [DOI] [PubMed] [Google Scholar]
- 60. Aaron SD, Vandemheen KL, Hebert P, et al. Outpatient oral prednisone after emergency treatment of chronic obstructive pulmonary disease. N Engl J Med 348:2618–2625, 2003. [DOI] [PubMed] [Google Scholar]
- 61. Anthonisen NR, Manfreda J, Warren CP, et al. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 106:196–204, 1987. [DOI] [PubMed] [Google Scholar]
- 62. Davies L, Angus RM, Calverley PM. Oral corticosteroids in patients admitted to hospital with exacerbations of chronic obstructive pulmonary disease: a prospective randomised controlled trial. Lancet 354:456–460, 1999. [DOI] [PubMed] [Google Scholar]
- 63. Wood-Baker RR, Gibson PG, Hannay M, et al. Systemic corticosteroids for acute exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2005:CD001288. [DOI] [PubMed] [Google Scholar]
- 64. Quon BS, Gan WQ, Sin DD. Contemporary management of acute exacerbations of COPD: a systematic review and metaanalysis. Chest 133:756–766, 2008. [DOI] [PubMed] [Google Scholar]
- 65. Ram FS, Rodriguez-Roisin R, Granados-Navarrete A, et al. Antibiotics for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2006:CD004403. [DOI] [PubMed] [Google Scholar]
- 66. Akazawa M, Halpern R, Riedel AA, et al. Economic burden prior to COPD diagnosis: a matched case-control study in the United States. Respir Med 102:1744–1752, 2008. [DOI] [PubMed] [Google Scholar]
- 67. Bustacchini S, Chiatti C, Furneri G, et al. The economic burden of chronic obstructive pulmonary disease in the elderly: results from a systematic review of the literature. Curr Opin Pulm Med 17(Suppl. 1):S35–S41, 2011. [DOI] [PubMed] [Google Scholar]
- 68. Ford ES, Murphy LB, Khavjou O, et al. Total and state-specific medical and absenteeism costs of chronic obstructive pulmonary disease among adults aged ≥18 years in the United States for 2010 and projections through 2020. Chest 2014. doi: 10.1378/chest.14–0972. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 69. National Institute of Health. Estimates of Funding for Various Research, Condition, and Disease Categories (RCDC). 2014. Available at http://report.nih.gov/categorical_spending.aspx Accessed June 30, 2014.
- 70. Feenstra TL, Hamberg-van Reenen HH, Hoogenveen RT, Rutten-van Mölken MP. Cost-effectiveness of face-to-face smoking cessation interventions: a dynamic modeling study. Value Health 8:178–190, 2005. [DOI] [PubMed] [Google Scholar]
- 71. Nickels AS, Joshi AY, Dinakar C. Electronic cigarettes: navigating the vapor. Ann Allergy Asthma Im 112:481–483, 2014. [DOI] [PubMed] [Google Scholar]



