Abstract
Background: Clostridium difficile infection (CDI) in patients with ileal pouch-anal anastomosis (IPAA) has been increasingly recognized. The aim of this study was to evaluate the outcome of fecal microbiota transplantation (FMT) in patients with pouch and CDI.
Methods: All consecutive patients that underwent FMT for CDI from 2012 to 2016 were extracted from our IRB-approved, prospectively maintained Registry of Pouch Disorders. The primary outcome was negative stool tests for Clostridium difficile after FMT and the secondary outcomes were symptomatic and endoscopic responses.
Results: A total of 13 patients were included in this study, with 10 being Caucasian males (76.9%). All patients had underlying ulcerative colitis for J pouch surgery. After a mean of 2.8±0.8 courses of antibiotic treatments was given and failed, 22 sessions of FMT were administered with an average of 1.7±1.1 sessions each. Within the 22 sessions, 16 were given via pouchoscopy, 4 via esophagogastroduodenoscopy and 2 via enemas. All patients tested negative on C. difficile polymerase chain reaction (PCR) after the initial FMT with a total of 7/12 (58.3%) documented patients showed symptomatic improvements and 3/11 (27.3%) patients showed endoscopic improvement according to the modified Pouchitis Disease Activity Index. During the follow-up of 1.2±1.1 years, there were a total of five patients (38.5%) that had recurrence after the successful initial treatment and four of them were successfully treated again with FMT.
Conclusions: FMT appeared to be effective in eradication of CDI in patients with ileal pouches. However, FMT had a modest impact on endoscopic inflammation and recurrence after FMT and recurrence was common.
Keywords: Clostridium difficile, fecal microbiota transplantation, ileal pouch, pouchitis
Introduction
Clostridium difficile (C. difficile) infection (CDI) is the leading cause of antibiotic-associated diarrhea and infectious colitis [1,2]. Management of CDI is challenging, as it is often associated with recurrence, with increasing morbidities and mortality rates in recent years [2]. Risk factors for CDI in general population include the use of antibiotics, hospitalization, advanced age and the comorbid diseases [3,4]. In addition, inflammatory bowel disease (IBD) was found to be a risk factor for CDI [5–7]. The incidence and prevalence of CDI have been increasing in IBD patients [8–11]. The impact of CDI and its treatment on IBD disease course are controversial [5].
Although CDI generally occurs in the colon, small intestine C. difficile enteritis has also been reported in several cases, especially with post-colectomy patients, and is often associated with poor outcome [12]. CDI in patients who underwent total proctocolectomy with the formation of an ileal pouch have been increasingly recognized over the past several years [12–17]. Restorative proctocolectomy with ileal pouch-anal anastomosis (IPAA) is commonly performed in patients with refractory ulcerative colitis (UC) or colitis-associated neoplasia [17]. The first reported case of refractory CDI in the pouch was from Mann et al. [13]. Our group has investigated the frequency, risk factors and treatment strategies for CDI and recurrent CDI in patients with IPAA [14]. While fecal microbiota transplantation (FMT) has been adopted as an effective approach for recurrent CDI in the general population [18,19], its use in patients with CDI of the pouch has not been reported beyond a case report [20]. We hypothesized that FMT may be a treatment option for refractory or recurrent CDI pouchitis patients. The aim of this study was to assess the efficacy of FMT in CDI.
Patients and methods
Patient identification
All consecutive patients that underwent IPAA were extracted from our institutional review board (IRB)-approved, prospectively maintained Registry of Pouch Disorders. Those who were treated with FMT for their recurrent CDI from 2012 to 2016 were identified. Demographic, clinical and endoscopic features together with the management and outcome were carefully reviewed and extracted from medical charts.
Inclusion and exclusion criteria
All patients with ileal pouches that were treated with FMT for their recurrent CDI were included in this study. The inclusion criteria were those with: (i) underlying UC and IPAA; (ii) CDI infections confirmed by presence of C. difficile toxin gene in stool sample by polymerase chain reaction (PCR) assay; (iii) at least one course of antibiotic treatment for 14 days prior to the first FMT; (iv) at least 2 months of follow-up after antibiotic treatment for the index CDI; (v) pouch endoscopy within 3–6 months of the index CDI; and (vi) refractory to antibiotic treatment for the index CDI or recurrence after successful antibiotic treatment confirmed by PCR. Refractory CDI was defined as continued symptoms following treatment of an index CDI with antibiotics for at least 14 days with a continued positive PCR for C. difficile toxin B. Recurrent CDI was defined as a period of symptom improvement or resolution after treatment for the index CDI associated with a negative C. difficile PCR, followed by a relapse or worsening of symptoms in the setting of repeatedly positive C. difficile PCR at any point during the follow-up period [21]. Recurrence corresponded to either relapse infection of the original strain or re-infection of new strains, since it is clinically difficult to distinguish these two. The presence of diarrhea could be caused by underlying IBD and/or CDI; therefore diarrhea alone was not used as a diagnostic criterion for both the index disease and refractory/recurrence. However, increased bowel frequency from postoperative baseline were described. IPAA patients with a history of familial adenomatous polyposis were excluded. A total of 13 patients were identified during this process.
Demographic and clinical variables
General background information, such as age, gender, ethnicity, height and weight, were extracted from the database. The body mass index (BMI) was calculated for each patient. Clinical histories included: current or past smoking history, concurrent significant comorbidities, autoimmune diseases and family history of IBD or colorectal cancer. Current smoker was defined as consuming more than seven cigarettes per week for at least 6 months and ex-smoker was defined as ceasing smoking at least 6 months prior to data entry. Significant comorbidities included congestive heart disease, coronary bypass surgery, chronic obstructive pulmonary disease, renal stone or renal insufficiency, non-gastrointestinal (GI) cancer, stroke and liver failure. Autoimmune disease included adult-onset asthma, type 1 diabetes, rheumatoid arthritis, autoimmune thyroid disease, psoriasis, systemic lupus erythematous, autoimmune hemolytic anemia, vitiligo, celiac disease, pernicious anemia, idiopathic thrombocytopenia purpura and multiple sclerosis. Family histories were recorded from those of the first-degree relatives to the patient.
IPAA-related variables included extent of UC, duration of UC, extra-intestinal manifestations, indication for proctocolectomy, pouch configuration and stage, duration of IPAA and postoperative complication. Postoperative complication was defined as a mechanical, infectious or thrombotic complication. Mechanical complication included the following based on a combination of consistent signs and symptoms, suggestive imaging studies and pouch endoscopy findings: intestinal obstruction, early or late (but surgery-related) fistula or sinus tract, wound dehiscence, stricture of the pouch inlet, pouch outlet, pouch body, anal transition zone or former ileostomy site, afferent limb syndrome (defined as a sharp angulation of the afferent limb at the junction with the ileal pouch) and twisted pouch body.
For the diagnosis and evaluation of pouchitis, the modified Pouchitis Disease Activity Index (mPDAI) clinical and endoscopic subscore (range 0–6 for each) was used [22]. Diagnosis of a normal pouch, acute pouchitis, chronic pouchitis, cuffitis, irritable pouch syndrome and Crohn’s disease (CD) of the pouch was based on the criteria that we previously reported [14,16].
Clinical practice pattern and FMT technique
The selection of antibiotics, antibiotic dosing, duration of antibiotic therapy and the use of FMT via pouch endoscopy, upper endoscopy or enema for the treatment of the first or subsequent CDI were based on the clinical discretion of the managing physician (B.S.). The commonly used agents included vancomycin, metronidazole, fidaxomicin and rifaximin. FMT was given to the patients with refractory or recurrent CDI.
Informed consent was obtained from both the recipient and the donor. The donor needed to be willing to share bio products with the patient and was preferably genetically related or genetically unrelated healthy family member. All donors were screened for hepatitis A, hepatitis B, hepatitis C, human immunodeficiency virus, human T-cell lymphotropic virus, syphilis, CDI, Helicobacter pylori, Vibrios, Listeria, Escherichia coli 0157:H7, Giardia, Cryptosporidium, Isospora and norovirus. The following donors were excluded: (i) those who have used antibiotics within 3 months; or (ii) those with conditions such as diarrhea, constipation, IBD, irritable bowel syndrome, colorectal cancer, anti-neoplastic drugs usage, immunocompromization, obesity, atopy, high risk behaviors or sexually transmitted diseases.
The stool samples were diluted and mixed in 500 ml normal saline using a blender. Filtering with a coffee filter/sterile gauze in a clean container yielded at least 350–450 ml of solution. The solution without fecal particles was stored in a clean container within a cooler before being transported to the endoscopy suite within 6 hours of the procedure. Prior to the procedure, antibiotics were discontinued in all recipients for 2–3 days. Polyethylene glycol-based bowel preparation was given the night before the procedure in the following morning.
The physician instilled a discrete volume of freshly prepared stool specimen into an afferent limb via a pouchoscopy or the distal duodenum via esophagogastroduodenoscopy (EGD) using a spray catheter. The volume given mostly depended on the patient’s response during the process of transplantation and the route of transplant. When FMT is performed via EGD, smaller volumes and slower rates should be used to reduce the risk of aspiration [23].
In our protocol, FMT via pouchoscopy was the first choice. FMT via EGD served as a backup, due to the concern of a theoretical high risk of aspiration in patients without a colon. For logistic reason, we did allow but did not encourage patients to have a self-enema with a screened donor at home as the third choice.
Outcome measurement
PCR was performed in all patients for a confirmed diagnosis of CDI and was also conducted after each course of antibiotics. PCR was also ordered when the patients came in for follow-ups after initial FMT and every subsequent treatment. All recurrence and refractory courses after the initial FMT were also confirmed by a positive PCR. The primary outcome was the eradication of C. difficile, which was defined as at least one negative PCR result after FMT. The secondary outcomes were improvements in symptom and endoscopic presentation. Symptomatic response was defined as a patient’s global subjective improvement as well as mPDAI symptom subscore improvement in the follow-up clinic visit after the initial FMT. Endoscopic improvement was assessed by comparing the mPDAI endoscopy subscores before and after the initial FMT.
Statistical analysis
Descriptive statistics were computed for all variables. Categorical variables were summarized as percentages. Quantitative variables with normal distribution were summarized as mean ± standard deviation (SD). Quantitative variables with paranormal distribution were summarized in median and interquartile range (IQR).
Results
A total of 13 consecutive patients with CDI of the ileal pouch were identified. None matched the exclusion criteria and therefore all were included in the study.
Demographic and clinical data
Demographic and clinical characteristics are listed in Table 1. CDI in pouch patients were male-dominated (76.9%). All of them were UC patients with pancolitis who underwent IPAA with a J configuration. A total of 11 (84.6%) patients underwent IPAA for refractory UC and 2 (15.4%) for colitis-associated neoplasia. Two patients (15.4%) underwent one-stage surgery, while 2 (15.4%) underwent two-stage surgery, 8 (61.5%) underwent a three-stage surgery and 1 (7.7%) had a redo pouch. Eight (61.5%) patients presented with postoperative complications including seven (53.8%) with pouch strictures and five (38.5%) with pouch leak/abscess. The mean duration from the pouch construction to the diagnosis of CDI was 11.5 ± 6.9 years. The predominant symptoms of the patients were the increase in bowel movements from the postoperative baseline, followed by abdominal pain, nausea and vomiting and blood in stool.
Table 1.
Patient’s clinical characteristics
| Characteristics | Total case (N=13) |
|---|---|
| Male gender, n (%) | 10 (76.9%) |
| Caucasian, n (%) | 13 (100.0%) |
| Weight at the time of FMT, kg | 72.2 ± 10.9 |
| BMI at the time of FMT, kg/m2 | 24.0 ± 3.6 |
| Ever smoked, n (%) | |
| Current | 1 (7.7%) |
| Quit | 3 (23.1%) |
| Significant comorbidities, n (%) | 2 (15.4%) |
| Concurrent autoimmune disorders, n (%) | 1 (7.1%) |
| Family history of IBD, n (%) | 4 (30.8%) |
| Family history of colorectal cancer, n (%) | 2 (15.4%) |
| Age at IBD diagnosis, years | 21.7 ± 12.5 |
| Precolectomy diagnosis of UC, n (%) | 13 (100.0%) |
| Extensive colitis, n (%) | 13 (100.0%) |
| Primary sclerosing cholangitis, n (%) | 1 (7.7 %) |
| Other extra-intestinal manifestation, n (%) | 2 (15.4%) |
| Preoperative use of biologics, n (%) | 4 (30.8%) |
| Age at colectomy, years | 32.7 ± 12.6 |
| Duration from IBD diagnosis to colectomy, years | 11.0 ± 11.9 |
| Indication for colectomy, n (%) | |
| Refractory disease | 11 (84.6%) |
| Neoplasia | 2 (15.4%) |
| Stage of pouch construction, n (%) | |
| 1 | 2 (15.4%) |
| 2 | 2 (15.4%) |
| 3 | 8 (61.5%) |
| Redo pouch | 1 (7.7%) |
| J configuration of the pouch, n (%) | 13 (100.0%) |
| Postoperative leak/abscess, n (%) | 5 (38.5%) |
| Concurrent stricture, n (%) | 7 (53.8%) |
| Concurrent cuffitis, n (%) | 5 (38.5%) |
| Concurrent CD of pouch, n (%) | 4 (30.8%) |
| Age at the diagnosis of CDI, years | 44.5 ± 13.8 |
| Duration from colectomy to diagnosis of CDI, years | 11.5 ± 6.9 |
| Presenting symptoms, n (%) | |
| Increase bowel movements | 8 (61.6%) |
| Urgency | 10 (76.9%) |
| Abdominal pain | 8 (61.5%) |
| Nausea and vomiting | 3 (23.1%) |
| Bleeding, n (%) | 2 (15.4%) |
| Mean session of FMT, n (%) | 1.7 ± 1.1 |
| Route of FMT, n (%) | |
| Pouchoscopy | 16 (72.7%) |
| Esophagogastroduodenoscopy | 4 (18.2%) |
| Self-enema | 2 (9.1%) |
| Volume of stool administered, ml | 186.9 ± 70.6 |
| Pouchoscopy | |
| Upper endoscopy | 30.0 ± 0.0 |
| Duration of follow-up, years | 1.2 ± 1.1 |
| Hospitalization after FMT treatment, n (%) | 2 (15.4%) |
| Cause of diverted pouch, n (%) | |
| Nausea and abdominal pain | 2 (15.4%) |
| Bowel obstruction | 1 (7.7%) |
| Ischemic pouchitis | 1 (7.7%) |
CDI, Clostridium difficile infection; FTM, fecal microbiota transplant; IBD, inflammatory bowel disease.
Treatment
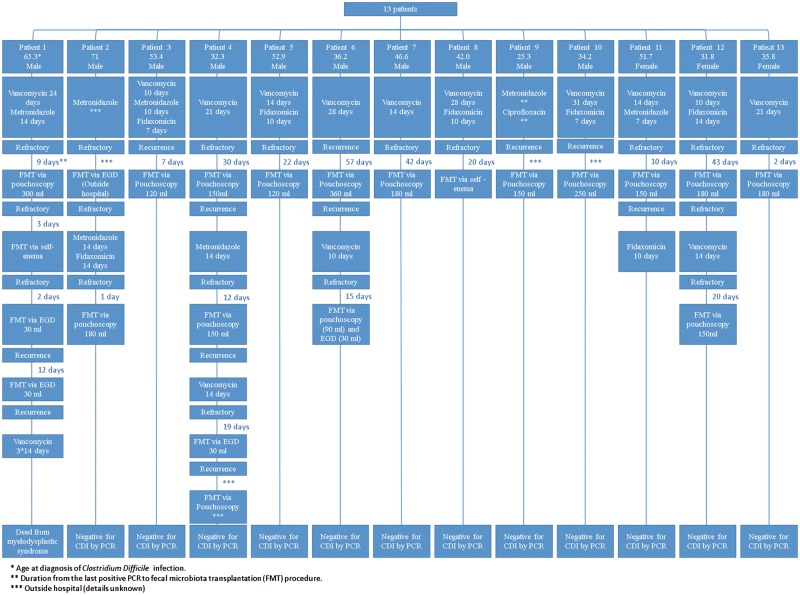
CDI patients were previously treated with an average of 22.8 ± 7.6 days of antibiotics upon diagnosis. The antibiotics used in each patient are listed in Figure 1. Vancomycin was given to 11 patients, metronidazole to 5 patients and fidaxomicin to 5 patients. After failing the antibiotic treatments, patients were recommended to have FMT. The first course of FMT was given in our institution via pouchoscopy in 10 patients. An average of 189.0 ± 78.8 ml of liquid fecal material was administered into the afferent limb and pouch body. Two patients received their first course in an outside hospital, with one via EGD and the other via pouchoscopy. The last patient conducted a self-enema.
Figure 1.
Flowchart of the treatment that each patient received.
After the initial FMT, three patients remained positive for CDI and three patients had a recurrence after a negative PCR result. Of the six patients, antibiotics were given to five for an average of 12.4 ± 2.2 days and FMT via self-enema was performed in one. One patient was treated successfully with fidaxomicin and the remaining five developed refractory course. These five patients were all given additional FMT with three via pouchoscopy, one via EGD and one with both pouchoscopy and EGD. However, two patients had recurrence after a short C. difficile-free period of 12 days and 46 days, respectively. One patient received a fourth course of FMT via EGD and the other patient had another 14 days of vancomycin before receiving his third FMT, which was also via EGD. These two patients had another recurrence after 16.8 and 2.3 months, respectively. The first patient had a refractory course and was treated with three courses of vancomycin with 14 days each, within a year, while the second patient was treated successfully with his fourth course of FMT in an outside hospital.
Outcomes
During a follow-up of 1.2 ± 1.1 years, 11 patients (84.6%) remained negative for CDI after the last course of FMT and 2 (15.4%) had a flare 1 month and 6 months, respectively, after the last FMT. The first patient was treated with 10 days of fidaxomicin and remained cleared of CDI since. The latter patient was previously treated with a total of four courses of FMT successfully and, during the last flare, FMT was suggested but, due to the patient’s overall health status (under chemotherapy for malignancy), vancomycin was given instead. The patient died 6 months later because of myelodysplastic syndrome.
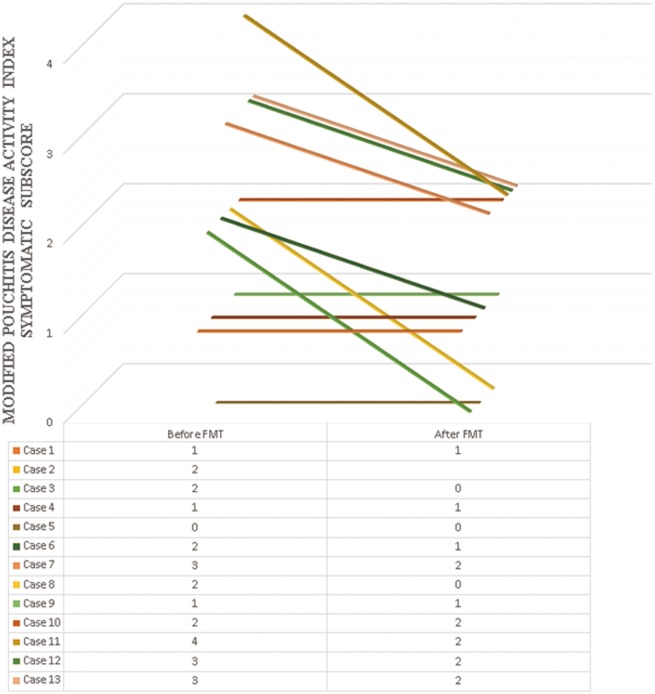
Out of 13 patients, 1 was lost to clinic follow-up after the initial FMT therapy and therefore records regarding symptomatic improvements were not available. In the remaining 12 patients, global symptomatic improvement was claimed in 9 (75.0%) patients. The mPDAI symptom and endoscopy subscores of each individual patient before and after the initial FMT were compared. Improvement of the mPDAI symptom subscore was only noted in 7 (58.3%) of the 12 patients with clinic follow-ups available (Figure 2). However, the results were not unanimous with patients’ subjective feelings.
Figure 2.
Modified Pouchitis Disease Activity Index clinical subscores before and after FMT.
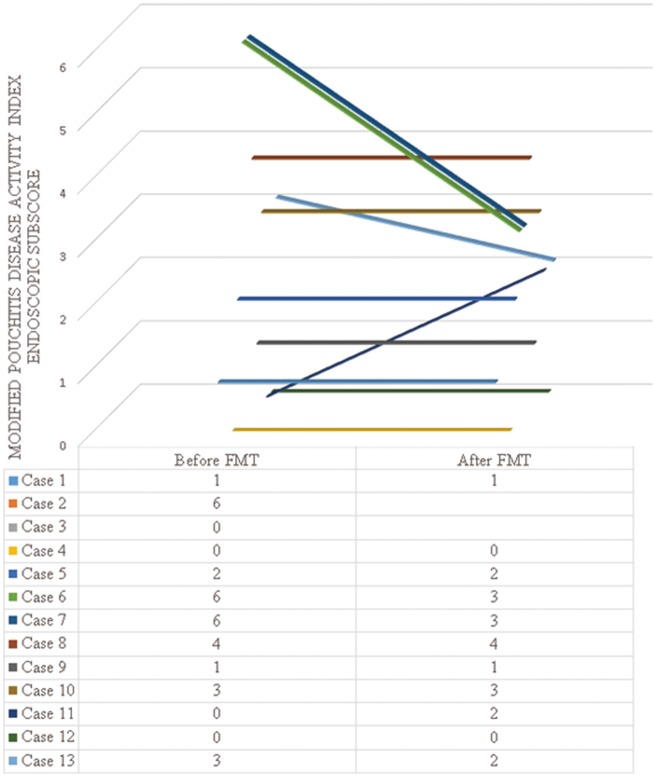
The comparison of mPDAI endoscopic subscore was conducted within the 11 patients that had endoscopic follow-ups available (Figure 3). Out of the 11 patients, severe pouchitis with a 6/6 mPDAI endoscopic subscore was seen in two patients. Both showed a significant improvement after FMT with the mPDAI endoscopic subscore decreased to 3/6. Another patient also showed slight improvement, with mPDAI endoscopic subscore decreasing from 3/6 to 2/6. However, these were the only three patients who showed endoscopic improvements. Apart from that, there was one patient that had an increase in mPDAI subscore from 0/6 to 2/6. No obvious endoscopic change was observed in the remaining seven patients.
Figure 3.
Modified Pouchitis Disease Activity Index endoscopic subscores before and after FMT.
Safety
Hospitalization after the procedure was documented in two patients. The first patient complained of abdominal pain and nausea when having lunch about 15 minutes after the procedure and was admitted to the emergence room. He was diagnosed with small bowel obstruction on CT scan. The second patient presented with severe abdominal pain, nausea and non-bloody diarrhea later in the evening after the procedure. Barium enema and anopouch manometry showed a dilated pouch and paradoxical contractions. Both patients were managed conservatively. The association between the presenting symptoms and the FMT procedure was not definite.
There were two patients who eventually developed pouch failure and underwent ileostomy, with one for bowel obstruction and the other from having ischemic pouchitis. The causes of pouch failure were considered as non-FMT-related.
Discussion
In the current study, a total of 13 patients underwent FMT for CDI. Approximately 40% of the patients had a recurrence of CDI after the initial FMT, requiring one or more additional FMT therapies. After an average of approximately two courses of FMT, all but one patient remained negative for C. difficile during a mean follow-up of 1.2 years. Seven of 12 patients (58.3%) experienced symptomatic responses and only three patients (27.3%) had endoscopic improvement according to the mPDAI score. Two patients (15.4%) developed abdominal pain and nausea that required hospitalization. However, whether or not the symptoms were related to FMT remained unclear.
The prevalence and incidence of CDI appear to have been increasing in recent years [24–26]. The true incidence of CDI in pouch patients remains uncertain due to possible referral bias. Two studies from our institution showed that, within the symptomatic patients with IPAA and underlying UC who presented for pouchoscopy, 21/115 (18%) patients tested positive for C. difficile toxin A or B as measured by enzyme immunoassay [15] and 21/196 (11%) patients tested positive by PCR [16]. In the general population, the most commonly known risk factors for CDI are antibiotic use, recent hospitalization, older age, patients with multiple comorbidities and malnutrition [3,4,27–30]. IBD has been shown to be a risk factor for CDI. In the IBD population, the use of corticosteroids or immunomodulators and the presence of colonic disease were shown to be risk factors for CDI [7,31–33]. In contrast to the general population, prior usage of antibiotics was not a risk factor in patients with IBD [5]. In patients with ileal pouches, our previous studies consistently showed that male gender was a risk factor for CDI [15,16].
Currently, the standard therapy for mild-to-moderate CDI includes the use of metronidazole or vancomycin [25,34]. There are conflicting data on the conventional therapy for recurrent CDI. Recent literature suggests that FMT is a feasible, effective and safe procedure for patients with antibiotic-refractory CDI, with a reported curative rate >90% in the general population [19,35–39]. Adverse events are rare but, in a meta-analysis of 317 patients in 27 studies, the following side effects were reported: upper GI bleeding (n = 1), symptoms of irritable bowel syndrome (IBS) (n = 5) and constipation (n = 1) [19]. The effectiveness of FMT in the treatment of IBD is still controversial. A meta-analysis that included 18 studies and 122 patients showed clinical remission in 45% of patients for IBD in general, including 22% for UC [40]. Individual studies showed a clinical remission rate of 70–80% in CD patients [41–43]. Alteration of the bacteria spectrum was found in almost all related studies [44,45]. The use of probiotics (especially VHL#3) in treating chronic pouchitis had been studied and was found to be effective in the maintenance of remission [46]. Despite the favorable clinical response of FMT in treating IBD in some studies, most also reported no significant changes in bacterial richness or diversity [40,45]. Some investigators also believed that FMT was less effective when treating CDI patients with concurrent IBD than for those without underlying IBD [47].
There were scant data regarding the treatment of C. difficile-associated pouchitis. The pathogenesis of pouchitis is not clear. Due to the unclear relationship between CDI, pouchitis and patient symptoms, refractory and recurrence of CDI are common [15]. There has been no consensus on the timing and number of repeat stool tests for the definition of refractory or recurrent CDI in the general population, much less so in IBD patients or pouch patients. We speculate that the pathogenesis, risk factors and disease course of CDI in the general population and CDI in the IBD or pouch population are different. The presence of C. difficile, an anaerobe, may be a consequence of tissue ischemia or tissue hypoxia in the setting of IPAA [48]. Therefore, the authors have used different definitions for refractory and recurrent CDI in pouchitis [21].
The standard therapy for CDI in non-IBD and non-pouch patients has been metronidazole as the first line, followed by vancomycin, and fidaxomicin was approved recently, although its cost-effectiveness is unclear. The paradigm has changed since FMT became widely adopted for the treatment of CDI, especially recurrent CDI. The natural history for CDI in pouch patients warrants further investigation. In our anecdotal experience, metronidazole has not been effective in treating CDI in patients with IPAA and the treatment with vancomycin or fidaxomicin has often been followed by recurrent CDI. Therefore, FMT in those patients is justified. This was also supported by our previous report of refractory CDI pouchitis in which a patient was successfully treated with FMT [20].
The current study was conducted to systematically evaluate the efficacy and safety of FMT. While, in the general population, a greater proportion of patients with refractory CDI are women [7,31], male dominance was observed in this cohort, similarly to our previous cohorts [16,22]. The mechanism of the male predominance of CDI in the pouch population is not clear. It is possible that the etiopathogenesis of CDI is related to underlying diseases. We have hypothesized that male patients had a high risk for the development of ischemia-type pouchitis with tissue hypoxia, which may make the patient susceptible to infection of anaerobes, including C. difficile [45]. In this study, only seven (58.3%) of the patients experienced a symptomatic improvement and only three (27.3%) showed endoscopic improvements. The lack of efficacy in objective endoscopy score improvement after FMT for CDI of the pouch suggests that the infection may be only an epiphenomenon and the underlying etiology of the infection was not treated, which in this case might be pouch ischemia.
The findings of this study have several clinical implications. As CDI is becoming increasingly recognized among patients post IPAA, C. difficile should be routinely checked in patients presenting with exacerbation of symptoms. In the case of refractory CDI, FMT is feasible, safe and maybe effective. Though the eventual eradication of C. difficile can be achieved by FMT in a majority of patients, there was a limited response in mPDAI endoscopy subscores. It is possible that the patients might also have other co-existing pathogens, other underlying diseases (such as chronic pouchitis and CD of the pouch) or mechanical issues (such as ischemia), which could have contributed to the patient’s symptoms and endoscopic inflammation. It is also important to understand that FMT might not be an ultimate cure for all causes of pouchitis and the treatment of the primary, underlying causes is necessary.
Our study has several limitations. This is not a controlled study, despite its being the largest case series of FMT for refractory or recurrent CDI in pouches. Second, this study was conducted in a tertiary care and subspecialized facility, which might have been subject to selection and referral bias. Therefore, the findings of this study may not be generalizable in the general population. In addition, this was a retrospective study that showed difficulty in obtaining some important data, such as the bacterial profile of the patients before and after FMT as well as the bacterial profile of the donors. Data on the treatment outcome were not available for all. Lastly, PCR-based assay has become the standard practice in our tertiary care center but there are several limitations to PCR assay, as it does not tell the difference between colonization and infection, since it only detects the DNA of the toxin A or B but not the actual toxin peptide. The similarity of the symptoms between CDI and underlying IBD made it even more difficult to differentiate between carrier state and infection. In addition, it is difficult to distinguish among different strains of C. difficile.
In conclusion, FMT is a feasible and safe way of treating patients with pouch and CDI. However, FMT had a modest impact on the endoscopic inflammation and recurrence of CDI after the initial FMT.
Acknowledgements
Dr Bo Shen is supported by the Ed and Joey Story Endowed Chair. This study was presented as a poster at the digestive disease week, May 2016, San Diego, California.
Conflict of interest statement: none declared.
References
- 1. Chen X, Lamont JT.. Overview of Clostridium difficile infection: implications for China. Gastroenterol Rep (Oxf) 2013;1:153–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. DuPont HL. Diagnosis and management of Clostridium difficile infection. Clin Gastroenterol Hepatol 2013;11:1216–23. [DOI] [PubMed] [Google Scholar]
- 3. McFarland LV, Surawicz CM, Stamm WE.. Risk factors for Clostridium difficile carriage and C. difficile-associated diarrhea in a cohort of hospitalized patients. J Infect Dis 1990;162:678–84. [DOI] [PubMed] [Google Scholar]
- 4. Loo VG, Bourgault A, Poirier L. et al. Host and pathogen factors for Clostridium difficile infection and colonization. N Engl J Med 2011;365:1693–1703. [DOI] [PubMed] [Google Scholar]
- 5. Berg AM, Kelly CP, Farraye FA.. Clostridium difficile infection in the inflammatory bowel disease patient. Inflamm Bowel Dis 2013;19:194–204. [DOI] [PubMed] [Google Scholar]
- 6. Bossuyt P, Verhaegen J, Van Assche G. et al. Increasing incidence of Clostridium difficile-associated diarrhea in inflammatory bowel disease. J Crohns Colitis 2009;3:4–7. [DOI] [PubMed] [Google Scholar]
- 7. Issa M, Vijayapal A, Graham MB. et al. Impact of Clostridium difficile on inflammatory bowel disease. Clin Gastroenterol Hepatol 2007;5:345–51. [DOI] [PubMed] [Google Scholar]
- 8. Ananthakrishnan AN, McGinley EL, Binion DG.. Excess hospitalisation burden associated with Clostridium difficile in patients with inflammatory bowel disease. Gut 2008;57:205–10. [DOI] [PubMed] [Google Scholar]
- 9. Ananthakrishnan AN, McGinley EL, Saeian K. et al. Temporal trends in disease outcomes related to Clostridium difficile infection in patients with inflammatory bowel disease. Inflamm Bowel Dis 2011;17:976–83. [DOI] [PubMed] [Google Scholar]
- 10. Nguyen GC, Kaplan GG, Harris ML. et al. A national survey of the prevalence and impact of Clostridium difficile infection among hospitalized inflammatory bowel disease patients. Am J Gastroenterol 2008;103:1443–50. [DOI] [PubMed] [Google Scholar]
- 11. Ricciardi R, Ogilvie JW Jr, Roberts PL. et al. Epidemiology of Clostridium difficile colitis in hospitalized patients with inflammatory bowel diseases. Dis Colon Rectum 2009;52:40–5. [DOI] [PubMed] [Google Scholar]
- 12. Kim J, Muder R.. Clostridium difficile enteritis: a review and pooled analysis of the cases. Anaerobe 2011;17:52–5. [DOI] [PubMed] [Google Scholar]
- 13. Mann SD, Pitt J, Springall RG. et al. Clostridium difficile infection—an unusual cause of refractory pouchitis: report of a case. Dis Colon Rectum 2003;46:267–70. [DOI] [PubMed] [Google Scholar]
- 14. Shen B, Goldblum JR, Hull TL. et al. Clostridium difficile-associated pouchitis. Dig Dis Sci 2006;51:2361–4. [DOI] [PubMed] [Google Scholar]
- 15. Shen B, Jiang Z, Fazio VW. et al. Clostridium difficile infection in patients with ileal pouch–anal anastomosis. Clin Gastroenterol Hepatol 2008;6:782–8. [DOI] [PubMed] [Google Scholar]
- 16. Li Y, Qian J, Queener E. et al. Risk factors and outcome of PCR-detected Clostridium difficile infection in ileal pouch patients. Inflamm Bowel Dis 2013;19:397–403. [DOI] [PubMed] [Google Scholar]
- 17. Wu H, Shen B.. Pouchitis: lessons for inflammatory bowel disease. Curr Opin Gastroenterol 2009;25:314–22. [DOI] [PubMed] [Google Scholar]
- 18. Surawicz CM, Brandt LJ, Binion DG. et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol 2013;108:478–98. [DOI] [PubMed] [Google Scholar]
- 19. Gough E, Shaikh H, Manges AR.. Systematic review of intestinal microbiota transplantation (fecal bacteriotherapy) for recurrent Clostridium difficile infection. Clin Infect Dis 2011;53:994–1002. [DOI] [PubMed] [Google Scholar]
- 20. Patel LN, Schairer J, Shen B.. Fecal transplantation therapy for Clostridium difficile-associated pouchitis. Int J Colorectal Dis 2014;29:263–4. [DOI] [PubMed] [Google Scholar]
- 21. Seril DN, Ashburn JH, Lian L. et al. Risk factors and management of refractory or recurrent clostridium difficile infection in ileal pouch patients. Inflamm Bowel Dis 2014;20:2226–33. [DOI] [PubMed] [Google Scholar]
- 22. Shen B, Achkar J, Connor JT. et al. Modified pouchitis disease activity index. Dis Colon Rectum 2003;46:748–53. [DOI] [PubMed] [Google Scholar]
- 23. Brandt LJ, Aroniadis OC.. An overview of fecal microbiota transplantation: techniques, indications, and outcomes. Gastrointest Endosc 2013;78:240–9. [DOI] [PubMed] [Google Scholar]
- 24. Bartlett JG. Narrative review: the new epidemic of Clostridium difficile-associated enteric disease. Ann Intern Med 2006;145:758–64. [DOI] [PubMed] [Google Scholar]
- 25. McDonald LC, Killgore GE, Thompson A. et al. An epidemic, toxin gene-variant strain of Clostridium difficile. N Engl J Med 2005;353:2433–41. [DOI] [PubMed] [Google Scholar]
- 26. Pepin J, Valiquette L, Cossette B.. Mortality attributable to nosocomial Clostridium difficile-associated disease during an epidemic caused by a hypervirulent strain in Quebec. Can Med Assoc J 2005;173:1037–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Heard S, Wren B, Barnett M. et al. Clostridium difficile infection in patients with haematological malignant disease. Epidemiol Infect 1988;100:63–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cudmore MA, Silva J, Fekety R. et al. Clostridium difficile colitis associated with cancer chemotherapy. Arch Intern Med 1982;142:333–5. [PubMed] [Google Scholar]
- 29. Collini PJ, Bauer M, Kuijper E. et al. Clostridium difficile infection in HIV-seropositive individuals and transplant recipients. J Infect 2012;64:131–47. [DOI] [PubMed] [Google Scholar]
- 30. Peled N, Pitlik S, Samra Z. et al. Predicting Clostridium difficile toxin in hospitalized patients with antibiotic-associated diarrhea. Infect Control Hosp Epidemiol 2007;28:377–81. [DOI] [PubMed] [Google Scholar]
- 31. Rodemann JF, Dubberke ER, Reske KA. et al. Incidence of Clostridium difficile infection in inflammatory bowel disease. Clin Gastroenterol Hepatol 2007;5:339–44. [DOI] [PubMed] [Google Scholar]
- 32. Das R, Feuerstadt P, Brandt LJ.. Glucocorticoids are associated with increased risk of short-term mortality in hospitalized patients with Clostridium difficile-associated disease. Am J Gastroenterol 2010;105:2040–9. [DOI] [PubMed] [Google Scholar]
- 33. Schneeweiss S, Korzenik J, Solomon D. et al. Infliximab and other immunomodulating drugs in patients with inflammatory bowel disease and the risk of serious bacterial infections. Aliment Pharmacol Ther 2009;30:253–64. [DOI] [PubMed] [Google Scholar]
- 34. Zar FA, Bakkanagari SR, Moorthi KM. et al. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis 2007;45:302–7. [DOI] [PubMed] [Google Scholar]
- 35. Girotra M, Bartlett J, Koerner K. et al. Combined jejunal and colonic fecal bacteriotherapy in patients with recurrent Clostridium difficile infection (RCDI). Am J Gastroenterol 2011;106:S162–3. [Google Scholar]
- 36. Hellemans R, Naegels S, Holvoet J.. Fecal transplantation for recurrent Clostridium difficile colitis, an underused treatment modality. Acta Gastroenterol Belg 2009;72:269–70. [PubMed] [Google Scholar]
- 37. Khoruts A, Dicksved J, Jansson JK. et al. Changes in the composition of the human fecal microbiome after bacteriotherapy for recurrent Clostridium difficile-associated diarrhea. J Clin Gastroenterol 2010;44:354–60. [DOI] [PubMed] [Google Scholar]
- 38. Rohlke F, Surawicz CM, Stollman N.. Fecal flora reconstitution for recurrent Clostridium difficile infection: results and methodology. J Clin Gastroenterol 2010;44:567–70. [DOI] [PubMed] [Google Scholar]
- 39. Yoon SS, Brandt LJ.. Treatment of refractory/recurrent C. difficile-associated disease by donated stool transplanted via colonoscopy: a case series of 12 patients. J Clin Gastroenterol 2010;44:562–6. [DOI] [PubMed] [Google Scholar]
- 40. Colman RJ, Rubin DT.. Fecal microbiota transplantation as therapy for inflammatory bowel disease: a systematic review and meta-analysis. J Crohns Colitis 2014;8:1569–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Suskind DL, Brittnacher MJ, Wahbeh G. et al. Fecal microbial transplant effect on clinical outcomes and fecal microbiome in active Crohn’s disease. Inflamm Bowel Dis 2015;21:556–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Cui B, Feng Q, Wang H. et al. Fecal microbiota transplantation through mid-gut for refractory Crohn’s disease: Safety, feasibility, and efficacy trial results. J Gastroenterol Hepatol 2015;30:51–8. [DOI] [PubMed] [Google Scholar]
- 43. Zhang F, Wang H, Wang M. et al. Standard fecal microbiota transplantation through mid-gut is an effective therapy of refractory Crohn’s disease. J Gastroenterol Hepatol 2013;28:9. [DOI] [PubMed] [Google Scholar]
- 44. Damman CJ, Miller SI, Surawicz CM. et al. The microbiome and inflammatory bowel disease: is there a therapeutic role for fecal microbiota transplantation? Am J Gastroenterol 2012;107:1452–9. [DOI] [PubMed] [Google Scholar]
- 45. Landy J, Walker AW, Li JV. et al. Variable alterations of the microbiota, without metabolic or immunological change, following faecal microbiota transplantation in patients with chronic pouchitis. Sci Rep 2015;5:12955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Singh S, Stroud AM, Holubar SD. et al. Treatment and prevention of pouchitis after ileal pouch-anal anastomosis for chronic ulcerative colitis. Cochrane Database Syst Rev 2015;11:CD001176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Khoruts A, Rank KM, Newman KM. et al. Inflammatory bowel disease affects the outcome of fecal microbiota transplantation for recurrent clostridium difficile infection. Clin Gastroenterol Hepatol 2016;14:1433–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Shen B. Problems after restorative proctocolectomy: assessment and therapy. Curr Opin Gastroenterol 2016;32:49–54. [DOI] [PubMed] [Google Scholar]