Abstract
Context
Patients with idiopathic interstitial pneumonia may display evidence of autoimmunity, without meeting criteria for a defined connective tissue disease. A recent European Respiratory Society/American Thoracic Society statement proposed research criteria for interstitial pneumonia with autoimmune features (IPAF), which includes findings from the clinical, serologic, and morphologic domains.
Objectives
To investigate the importance of histopathologic criteria within the morphologic domain and to report our methodology for identifying these features.
Design
Patients with idiopathic interstitial pneumonia at the University of Chicago, who underwent surgical lung biopsy or lung transplantation were assessed for IPAF histopathologic features, using the initial pathology interpretation in the electronic records. A focused rereview of available slides by a pulmonary pathologist was then performed for patients who failed to meet IPAF criteria on initial pathology assessment.
Results
Of 422 patients with idiopathic interstitial pneumonia, 176 (41.7%) underwent surgical lung biopsy or lung transplant. Forty-six of those 176 patients (26.1%) met IPAF criteria by initial pathology interpretation and a positive clinical or serologic feature. Of the remaining 130 patients, 73 (56.2%) met either the clinical or serologic domains without meeting the morphologic domain, whereas 36 (27.7%) had slides available for pathology rereview. This rereview demonstrated nonspecific interstitial pneumonia in 8 of 36 patients (22.2%) and lymphoplasmacytic infiltrates in 6 of 36 patients (16.7%), resulting in an additional 7 of 36 patients (19.4%) with idiopathic interstitial pneumonia that met the IPAF criteria. In IPAF, pulmonary vasculopathy was the most prevalent finding (45 of 84; 53.6%) and predicted increased mortality (hazard ratio, 2.5; P = .04).
Conclusions
Using a methodological approach to identifying IPAF pathology, we demonstrate a significant increase in the number of patients meeting IPAF criteria because of focused pathologic review and highlight the prognostic value of the IPAF pathologic findings.
Interstitial lung diseases (ILDs) often occur as a complication of connective tissue disease (CTD). It has been recognized that patients with ILD may demonstrate clinical or serologic features suggestive of an underlying autoimmune process but not fulfill diagnostic criteria for a defined CTD. The histopathologic features of an idiopathic, non-specific interstitial pneumonia (NSIP) pattern observed on surgical lung biopsy (SLB) have also been thought to be the pulmonary manifestation of this process.1,2 Demonstration of an NSIP pattern or a usual interstitial pneumonia (UIP) pattern has been shown to be of prognostic value in patients with idiopathic interstitial pneumonias (IIPs).3 In addition to these diverse histologic patterns, the association of IIP with the presence of clinical and serologic features suggestive of CTD, has led to nonuniform terminology in describing these patients: lung-dominant CTD, autoimmune-featured ILD, and undifferentiated CTD-associated ILD.4–6
Recently, the lack of consensus on the appropriate terminology and criteria for identifying this subset of patients resulted in the formation of an international, multidisciplinary European Respiratory Society (ERS, Lausanne, Switzerland)/American Thoracic Society (ATS, Washington, DC) task force that proposed new criteria for classifying these patients as having an interstitial pneumonia with autoimmune features (IPAF).5,7,8 Presently, the IPAF designation is implemented for research purposes only, and has yet to be regarded as a routine clinical diagnosis. The ERS/ATS task force recommends that individuals with IIP and features suggestive of CTD, who do not meet the diagnostic criteria for any defined CTD, should have their disease categorized into the IPAF research designation when those criteria are met.8 Those new criteria are built around 3 domains based on the presence of clinical, serologic, and morphologic features (Table 1).
Table 1.
| A. Clinical Domain | B. Serologic Domain | C. Morphologic Domain |
|---|---|---|
|
|
Radiology features
|
Histopathology features (SLB)
| ||
Multicompartment involvement
|
Abbreviations: ANA, antinuclear antibody; CADM, clinically amyopathic dermatomyositis; CCP, cyclic citrullinated peptide; CTD, connective tissue disease; dsDNA, double stranded deoxyribonucleic acid; GC, germinal center; HRCT, high-resolution computed tomography; LIP, lymphoid interstitial pneumonia; MDA, melanoma differentiation-associated; NSIP, nonspecific interstitial pneumonia; OP, organizing pneumonia; PFT, pulmonary function tests; PM-Scl, polymyositis/systemic scleroderma; RF, rheumatoid factor; SLB, surgical lung biopsy; SS-A, Sjögren syndrome–related antigen A; SS-B, Sjogren syndrome–related antigen B; tRNA, transfer RNA; ULN, upper limit of normal.
The criteria for IPAF are (1) the presence of an interstitial pneumonia (by HRCT or surgical lung biopsy) and (2) the exclusion of alternative etiologies and (3) incomplete features of a defined CTD and (4) at least one feature from at least 2 domains (columns A, B, or C).
This material has not been reviewed by European Respiratory Society before release; therefore, the European Respiratory Society is not responsible for any errors, omissions, or inaccuracies, or for any consequences arising therefrom, in the content. Reproduced with permission of the European Respiratory Society: ©European Respiratory Journal. 2015;46(4):976–987.
The clinical domain includes specific, extrathoracic, clinical features, such as Raynaud phenomenon, palmar telangiectasia, distal digital tip ulceration, digital fissuring (“mechanic hands”), and a rash on the extensor surfaces of the digits (Gottron sign), which may indicate an underlying autoimmune process. The serologic domain includes the presence of specific, circulating autoantibodies that frequently characterize CTDs, such as positive antinuclear antibody result with a nucleolar- or centromere-staining pattern, an antinuclear antibody titer of 1:320 or greater, a high-titer rheumatoid factor, and several other circulating autoantibodies. The morphologic domain comprises features from 3 categories: (1) high-resolution computed tomography imaging patterns commonly found in patients with CTD-ILD, such as those with NSIP, organizing pneumonia, NSIP with organizing pneumonia, and lymphoid interstitial pneumonia; (2) histopathologic findings in an SLB that are highly associated with the presence of CTD, such as an NSIP pattern, organizing pneumonia pattern, lymphoid interstitial pneumonia pattern, the presence of interstitial lymphoid aggregates with germinal centers, and diffuse lymphoplasmacytic infiltration with or without lymphoid follicles; and (3) multicompartment involvement, which includes additional features evident on diagnostic imaging, histopathology, cardiac catheterization, or pulmonary function testing. These features of multicompartment involvement, which often signal the presence of an underlying, systemic, autoimmune process, include unexplained intrinsic airways disease (including airflow obstruction, bronchiolitis, or bronchiectasis), unexplained pulmonary vasculopathy (such as precapillary pulmonary hypertension), and unexplained pleural or pericardial effusion or thickening resulting from inflammation of the serosal surfaces. Patients with IIP who demonstrate features of autoimmunity but who fail to meet diagnostic criteria for an established CTD can be categorized into the IPAF research designation based on the presence of at least one finding from at least 2 of the 3 required IPAF domains.
In this study, we identified patients with IIP who had an SLB or lung transplant (LTx) and applied the IPAF diagnostic criteria to those patients. This article outlines a methodology for identification of the IPAF histopathologic criteria and presents characteristic images of IPAF histopathologic features. We determined whether the application of the histopathologic criteria, including multicompartment involvement, influences the prevalence and prognosis of IPAF among those with IIP.
MATERIALS AND METHODS
Study Population
This study was conducted as part of a larger, recently published9 investigation at the University of Chicago (Chicago, Illinois) that was aimed at characterizing outcomes in patients with IPAF. We identified patients enrolled in our ILD registry (institutional review board protocol 14163-A), who had been followed from 2006 to 2015 (Figure 1). Patients meeting the ATS/ERS criteria for idiopathic pulmonary fibrosis (IPF), biopsy-proven idiopathic NSIP, and biopsy-proven cryptogenic organizing pneumonia, or previously proposed, narrow undifferentiated connective tissue disease criteria were evaluated,1,10,11 and all patients meeting these criteria with lung tissue available were included in this study. A retrospective review of the electronic medical record for extraction of pertinent data was performed. We identified the historical presence of histopathologic features within the IPAF criteria, as documented below, and patients were designated as having IPAF if they fulfilled the ERS/ATS classification criteria for IPAF.8
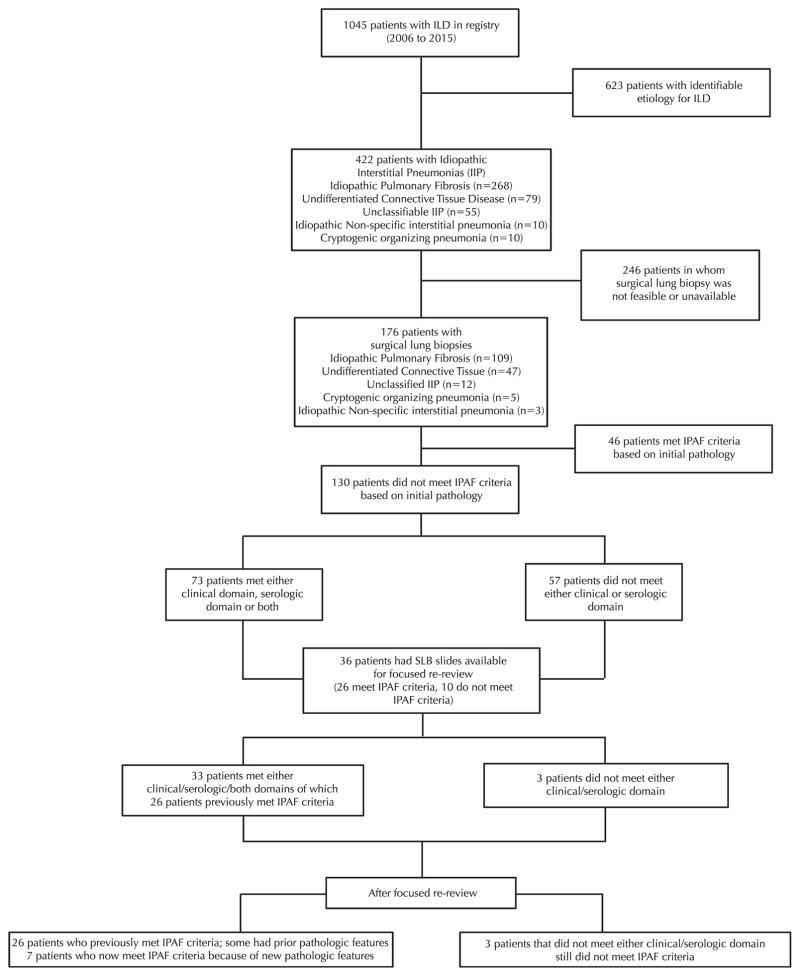
Figure 1.
Cohort diagram for a study aimed at characterizing outcomes in patients with interstitial pneumonia with autoimmune features (IPAF). Abbreviations: ILD, interstitial lung disease; SLB, surgical lung biopsy.
Histopathologic Review for IPAF Morphologic Criteria
For this study, we classified major histologic patterns according to the 2013 ATS/ERS multidisciplinary classification of IIPs.11 We retroactively applied the IPAF criteria in a systematic fashion to the initial electronic medical record report of tissue specimens in our IIP cohort. These tissue specimens had been initially reviewed as part of the usual, multidisciplinary care for patients with IIP (Figure 1). All tissue specimens were from a cohort containing diverse ILDs, including IPF, undifferentiated connective tissue disease, idiopathic NSIP, cryptogenic organizing pneumonia, and unclassifiable IIP. A hierarchical algorithm that included histopathologic features within the IPAF criteria was strictly followed and applied to each pathology report to determine whether it satisfied the IPAF histopathologic classification criteria (Table 1) (Figure 2). All available specimens that failed to meet IPAF criteria using the initial pathology assessment underwent a focused rereview.
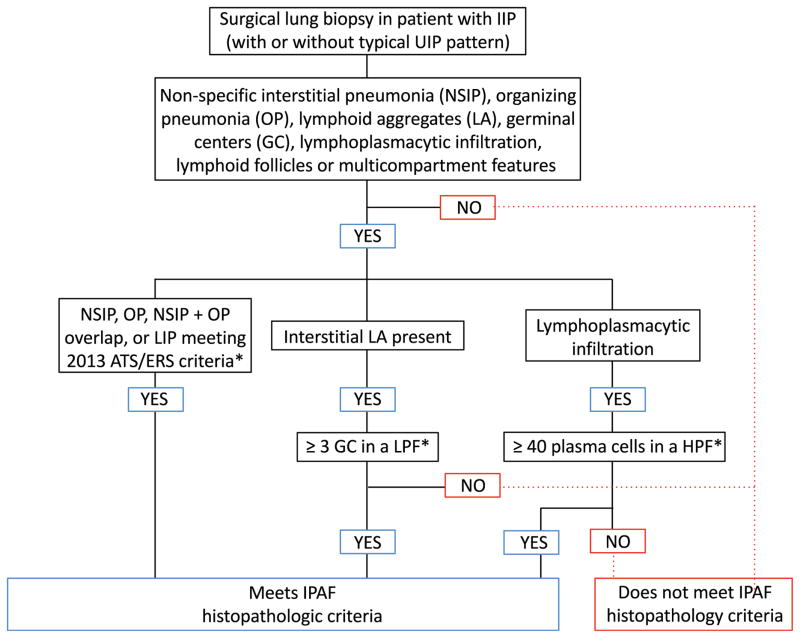
Figure 2.
Histopathologic algorithm used for classifying surgical lung biopsies in idiopathic interstitial pneumonia (IIP) as meeting criteria for interstitial pneumonia with autoimmune features (IPAF). Multicompartment features are unexplained pulmonary vasculopathy, unexplained pleural or pericardial thickening, or effusion. *IPAF histopathologic criteria requires presence of at least one of these features. Abbreviations: ATS, American Thoracic Society; ERS, European Respiratory Society; HPF, high-power field; LIP, lymphoid interstitial pneumonia; LPF, low-power field; UIP, usual interstitial pneumonia.
Qualitative Assessment for NSIP Pattern
The NSIP pattern on tissue specimens consisted of widened alveolar septae with interstitial inflammatory infiltrates, which were identified at low-power field throughout large areas.11,12 These infiltrates were characterized as cellular NSIP; dense, fibrosing NSIP; or both (mixed NSIP).11,12
Qualitative Assessment for Organizing Pneumonia Pattern
A pathologic pattern of organizing pneumonia was identified when biopsy specimens showed widespread foci of organizing pneumonia in the presence of preserved, background lung architecture.11,13,14 These specimens were characterized by a patchy distribution of intraluminal, organizing fibrosis in the distal airspaces; mild, interstitial chronic inflammation; and preserved lung architecture. These tissue specimens lacked prominent infiltration with eosinophils or neutrophils, granulomas, airspace fibrin deposition, or apical fibrosis.11
Qualitative Assessment for NSIP With an Organizing Pneumonia Overlap Pattern
An NSIP with an organizing pneumonia overlap, as indicated in the IPAF criteria,8 was identified on tissue specimens by widespread organizing pneumonia foci with preserved background lung architecture and a concurrent demonstration of diffuse interstitial inflammatory infiltrates or dense fibrosis in regions that were spatially distinct from the organizing pneumonia foci.11,12,14,15
Quantitative Assessment for Interstitial Lymphoid Aggregates and Germinal Centers
Tissue specimens were evaluated for the presence of interstitial lymphoid aggregates and germinal centers.2 Because the number of germinal centers is not specified in the IPAF criteria, on rereview, we designated germinal centers as being present if at least 3 germinal centers were observed in any one low-power field.
Quantitative Assessment for Lymphoplasmacytic Infiltrates
The presence of lymphoplasmacytic infiltration within the pulmonary interstitium was assessed. Because a variable number of infiltrating plasma cells may accompany lymphoid follicles,16 on rereview, we designated the presence of diffuse lymphoplasmacytic infiltrates by lymphocytes and 40 or more plasma cells in a high-power field. Diffuse lymphoplasmacytic infiltrates meeting that threshold were counted as present, with or without lymphoid follicles.8
Qualitative Assessment for Multicompartment Involvement
We assessed tissue specimens for other concurrent manifestations of autoimmunity outside the pulmonary interstitium but within the thoracic compartment, termed multicompartment involvement (Table 1).8 These IPAF features of multicompartment involvement included unexplained intrinsic airway disease, unexplained pulmonary vasculopathy, and unexplained pleural or pericardial effusion or thickening.8 Intrinsic airway disease was categorized as present if histopathologic obliterative bronchiolitis was noted on tissue specimens. Pulmonary vasculopathy was categorized as present when histopathologic arterial changes consistent with precapillary pulmonary hypertension were noted on tissue specimens. The histopathologic criteria used to determine pulmonary vasculopathy were the presence of intimal fibrosis, medial hypertrophy, and muscular hyperplasia on tissue specimens. When the presence of intrinsic airway disease, unexplained pulmonary vasculopathy, or unexplained pleural or pericardial effusion or thickening was noted, the tissue specimen was classified as meeting criteria for the IPAF morphologic domain.
Qualitative Assessment for UIP Pattern
Where applicable, features consistent with pathologic fibrosis were identified, and if consistent with UIP, the tissue was categorized as a typical UIP pattern.2,11 Tissue specimens with a UIP pattern demonstrated the presence of patchy parenchymal involvement with evidence of temporal and spatial heterogeneity. Coexistence of NSIP and UIP was not consistently reported in the diagnostic line of the initial tissue specimen reports.
Focused Rereviews of IIP Tissue Specimens
Focused rereviews were performed for all available specimens that failed to meet IPAF criteria using the initial pathology assessment. Specimens were obtained from both wedge biopsies and explanted lungs. The number of slides per specimen varied (≥2). Thus, to standardize analysis across all patients whose specimens were rereviewed (n = 36), all available slides for those with SLB/LTx were rereviewed (n = 311) and examined microscopically by the same thoracic pathologist with expertise in ILD (A.N.H.) in a blinded fashion for applying IPAF criteria. Histopathologic patterns were classified according to the ATS/ERS 2013 guidelines. All features consistent with IPAF were identified and described when present (Figure 3). After rereview, the number of patients who met IPAF based on histopathology was determined.
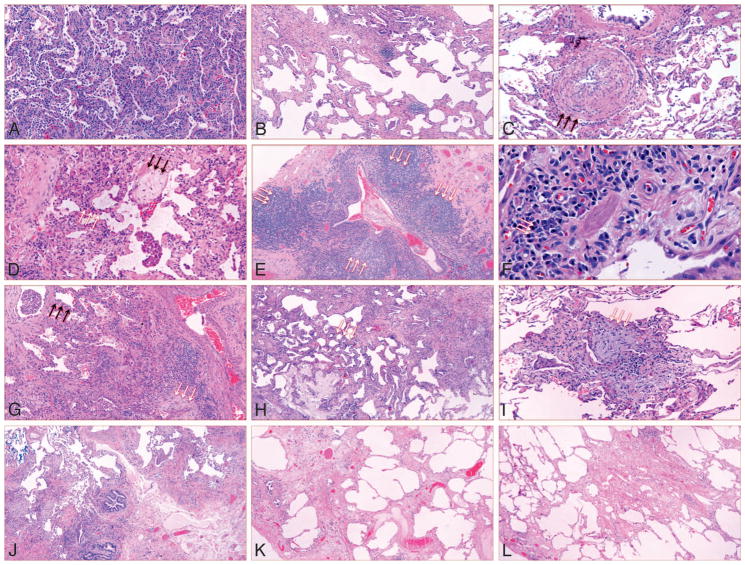
Figure 3.
Histopathologic features of samples from patients with idiopathic interstitial pneumonia. A, Cellular nonspecific interstitial pneumonia (NSIP). B, Fibrotic nonspecific interstitial pneumonia NSIP. C, Pulmonary vasculopathy in specimen with NSIP. Pulmonary vasculopathy (black arrows). D, Overlap of NSIP with organizing pneumonia (OP): NSIP, white arrows; OP, black arrows. Multiple foci of OP were present in the tissue specimen. E, Interstitial lymphoid aggregates with germinal centers (white arrows). F, Lymphoplasmacytic infiltration with lymphoid follicles (white arrows). G, Usual interstitial pneumonia with NSIP; NSIP in upper left (black arrows); fibroblastic focus in bottom right (white arrows). H, Usual interstitial pneumonia with fibrosing NSIP (fibrosing NSIP, white arrows). I, Usual interstitial pneumonia with OP (white arrows). Multiple foci of OP were present in tissue specimen. J, Usual interstitial pneumonia only. K and L, Unclassifiable interstitial pneumonia. A through I, The idiopathic interstitial pneumonia meets interstitial pneumonia with autoimmune features criteria. J through L, The IIP does not meet IPAF criteria (hematoxylineosin, original magnifications ×100 [A, C, D, and G], ×40 [B, E, H, and J–L], × 600 [F], and × 200 [I]).
Statistical Methods
Continuous variables were reported as means (standard deviation). and comparisons were made using a 2-tailed Student t test. Categorical variables were reported as counts and percentages; comparisons were made using χ2 or the Fisher exact test, as appropriate. McNemar test was used to compare the proportions of SLB features meeting IPAF histopathologic criteria before and after the rereview process. A P < .05 was considered statistically significance. Associations between survival and individual histopathologic features were assessed using the log-rank test. The significance of any prognostic factors was further investigated using univariate and multivariable Cox proportional hazards regression. Multivariable adjustment was performed using variables previously linked to survival in ILD, such as components of the gender–age–physiology ILD score17 and the presence of IPAF clinical domain findings.9 The Kaplan-Meier survival estimator was used to plot survival curves. In patients unable to perform the diffusing capacity of the lung for carbon monoxide maneuver, imputation of the lowest quartile mean (27.3%) was used, as previously described.9 Survival time was defined as time from diagnostic test (SLB/LTx or high-resolution computed tomography) to death, transplant, loss to follow-up, or the end of study period. Survival time was censored on December 31, 2015, or at the time a patient underwent LTx or was lost to follow-up. All statistical analyses were performed using Stata (StataCorp 2015; release 14, StataCorp, College Station, Texas).
RESULTS
Of the 1045 patients with ILD, 422 (40.4%) had IIP. Of those 422 patients, 176 (41.7%) with IIP had histopathologic reports available for inclusion in this study. Before publication of the IPAF criteria, those 176 patients carried the following diagnoses: IPF (n = 109; 61.9%), undifferentiated connective tissue disease (n = 47; 26.7%), unclassifiable IIP (n = 12; 6.8%), cryptogenic organizing pneumonia (n = 5; 2.8%), and idiopathic NSIP (n = 3; 1.7%) (Figure 1). Eighty-four patients had features from at least 2 of the 3 required IPAF domains and, thus, satisfied IPAF criteria. Forty-six of those 84 patients (54.8%) met IPAF pathologic criteria.
Histopathologic Characteristics
Although patients classified as IPAF had tissue specimens demonstrating NSIP, organizing pneumonia, interstitial lymphoid aggregates with germinal centers, or diffuse lymphoplasmacytic infiltrates, those features were also present in patients who did not have IPAF. A lymphoid interstitial pneumonia pattern was not seen in either subgroup.
Assessment of specimens for features of multicompartment involvement demonstrated the presence of unexplained intrinsic airway disease (3 of 84; 3.6%) and unexplained pleural or pericardial effusion/thickening (4 of 84; 4.8%), only in those patients classified as IPAF (Table 2).
Table 2.
Demographic and Clinical Characteristics of Patients With Idiopathic Interstitial Pneumonia (IIP), N = 176a
| Characteristics | IPAF, n = 84 | Non-IPAF IIP, n = 92 | P valueb |
|---|---|---|---|
| Age, y, mean (SD) | 60.1 (10.0) | 65.2 (7.4) | <.001 |
| Sex, No. (%) | 43 F (51.2); 41 M (48.8) | 24 (26.1) | .001 |
| Non-Hispanic white, No. (%) | 61 (72.6) | 76 (82.6) | .11 |
| Ever smoker, No. (%) | 47 (56.0) | 65 (70.7) | .03 |
| BMI, mean (SD) | 31.5 (7.1) | 30.9 (5.5) | .52 |
| TLC, %, mean (SD)c | 65.4 (15.9) | 64.2 (14.1) | .62 |
| FVC, %, mean (SD)c | 60.7 (17.5) | 61.5 (15.6) | .74 |
| DLCO, %, mean (SD)c | 46.4 (22.2) | 48.1 (15.7) | .56 |
| Walking distance in 6 min,d mean (SD)c | 1100.8 (401.9) | 1140.2 (395.2) | .55 |
| IPAF domain criteria met, No. (%) | |||
| Clinicale | 36 (44.4) | 2 (2.2) | <.001 |
| Serologic | 79 (94.0) | 33 (35.9) | <.001 |
| Morphologic | |||
| Radiographicf | 34 (42.5) | 6 (6.7) | <.001 |
| Pathologicg | 46 (54.8) | 11 (12.0) | <.001 |
| NSIP | 22 (26.2) | 4 (4.3) | <.001 |
| OP | 15 (17.9) | 2 (2.2) | <.001 |
| NSIP/OP overlap | 3 (3.6) | 0 (0.0 | .07 |
| Interstitial lymphoid aggregates with GCs | 11 (13.1) | 3 (3.3) | .02 |
| Diffuse lymphoplasmacytic infiltrates | 11 (13.1) | 2 (2.2) | .006 |
| Multicompartment involvementh | 48 (57.1) | 42 (45.7) | .14 |
| Intrinsic airway disease | 3 (3.6) | 0 (0.0) | .12 |
| Pleural or pericardial effusion or thickening | 4 (4.8) | 0 (0.0) | .05 |
| Pulmonary vasculopathy | 45 (53.6) | 42 (45.7) | .29 |
| UIP pattern | 62 (73.8) | 90 (97.8) | <.001 |
Abbreviations: BMI, body mass index; DLCO, diffusing capacity of the lungs for carbon monoxide; FVC, forced vital capacity; GC, germinal center; IPAF, interstitial pneumonia with autoimmune features; NSIP, nonspecific interstitial pneumonia; OP, organizing pneumonia; TLC, total lung capacity; UIP, usual interstitial pneumonia.
Tissue specimens were obtained from a single lobe in 48 patients, whereas 128 patients had slides obtained from 2 or more lobes.
Bolded values were significant.
Number of patients differed, N = 169.
Distance in feet, to convert to meters, multiply by 0.3048.
Number of patients differed, N = 173.
Number of patients differed, N = 170.
No patient had lymphoid interstitial pneumonia, several patients had multiple pathologic features.
No patient had unexplained pleural or pericardial effusion or thickening, several patients had multiple multicompartment features.
Of the 176 patients in this cohort, pulmonary vasculopathy was prevalent (n = 87; 49.4%) and was associated with a UIP pattern (83 of 87; 95.4%), an NSIP pattern (14 of 87; 16.1%), an organizing pneumonia pattern (7 of 87; 8.0%), or an NSIP with organizing pneumonia overlap pattern (1 of 87; 1.1%); several patients had multiple pathologic patterns. The prevalence of pulmonary vasculopathy did not differ between the IPAF and non-IPAF subgroups (53.6% versus 45.7%).
Focused Rereview With Application of IPAF Criteria
In this IIP cohort, 36 patients had available tissue specimens for rereview. Specimens evaluated included lung wedge biopsies (n = 33; 91.7%) and explanted lungs (n = 3; 8.3%). The tissue specimens included in the rereview were obtained from patients initially classified as IPF (n = 17; 47.2%), undifferentiated connective tissue disease (n = 17; 47.2%), cryptogenic organizing pneumonia (n = 1; 2.8%), and unclassifiable IIP (n = 1; 2.8%). Compared with initial pathologic diagnosis, focused rereviews resulted in a significant increase in the number of tissue specimens demonstrating IPAF histopathologic features (n = 26 [72.2%] versus n = 16 [44.4%]; P = .002). Those features were NSIP (12 [33.3%] versus 4 [11.1%]; P = .008], diffuse lymphoplasmacytic infiltrates (12 [33.3%] versus 6 [16.7%]; P = .03] (Table 3). Specimens with organizing pneumonia, NSIP with organizing pneumonia overlap and lymphoid aggregates with germinal centers were also increased but not to a statistically significant level (Table 3). Combining these pathologic findings with features from other IPAF domains resulted in an additional 7 patients being reclassified as having IPAF. All 7 patients reclassified as having IPAF were previously diagnosed with IPF.
Table 3.
Results of Focused Rereview of Surgical Lung Biopsies in Patients With Idiopathic Interstitial Pneumonia
| Characteristics | Initial Review Before IPAF Criteria, No. (%), n = 36 | Focused Rereview for Features of IPAF Criteria, No. (%), n = 36 | P valuea |
|---|---|---|---|
| Classified as IPAF | 26 (72.2) | 33 (91.7) | .02 |
| Met histopathologic IPAF criteria | 16 (44.4) | 26 (72.0) | .002 |
| NSIP | 4 (11.1) | 12 (33.3) | .008 |
| OP | 3 (8.3) | 4 (11.1) | >.99 |
| NSIP/OP overlap | 0 (0.0) | 1 (2.8) | >.99 |
| ILA and GCs | 3 (8.3) | 8 (22.2) | .06 |
| Diffuse LPI | 6 (16.7) | 12 (33.3) | .03 |
| Multicompartment involvementb | |||
| Intrinsic airway disease | 1 (2.8) | 1 (2.8) | >.99 |
| Pulmonary vasculopathy | 20 (55.6) | 20 (55.6) | >.99 |
| Pleural or pericardial thickening or effusion | 2 (5.6) | 4 (11.1) | .50 |
| UIP pattern | 32 (88.9) | 32 (88.9) | >.99 |
| Mixed UIP-NSIP pattern | 3 (9.4) | 11 (34.4) | .009 |
Abbreviations: GC, germinal center; ILA, interstitial lymphoid aggregates; IPAF, interstitial pneumonia with autoimmune features; LPI, lymphoplasmacytic infiltrates; NSIP, nonspecific interstitial pneumonia; OP, organizing pneumonia; UIP, usual interstitial pneumonia.
Bolded font denotes significant P-values at a .05 level of significance.
No patient had unexplained pleural or pericardial effusion or thickening.
Survival Patterns
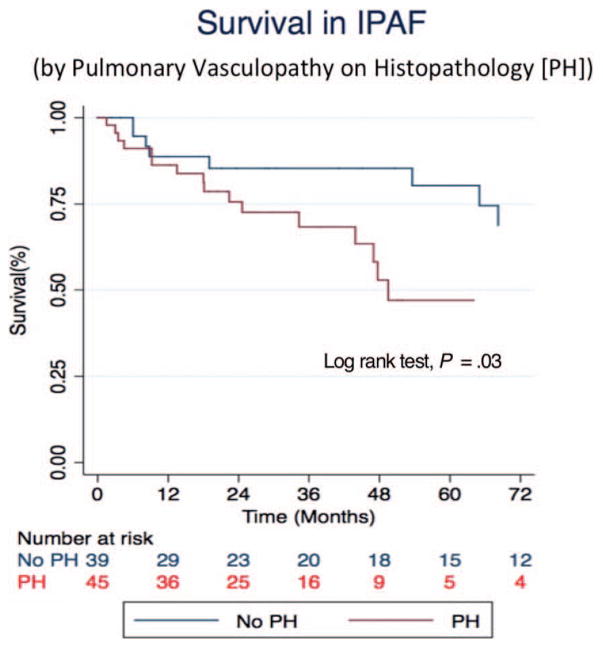
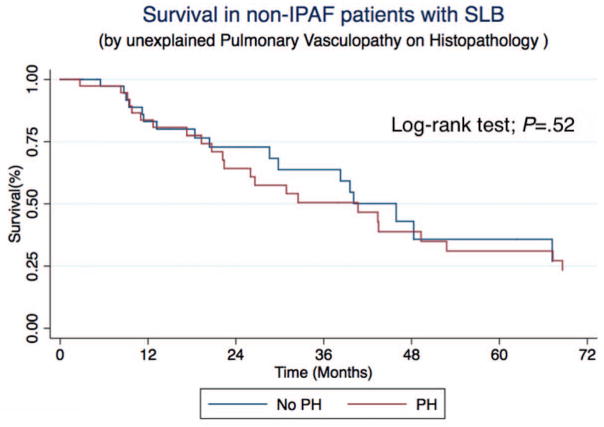
In an outcome analysis of our IIP cohort with SLB/LTx, 61 of 176 patients (34.7%) died during the follow-up period, and 25 (14.2%) underwent LTx. Stratification of the IPAF cohort by patients with pulmonary vasculopathy, the most prevalent, pathologic, multicompartment involvement (45 of 84; 53.6%) demonstrated significantly worse survival (P = .03) (Figure 4), whereas pulmonary vasculopathy was not associated with a worse outcome in patients without IPAF (P = .52) (Figure 5). In IIP, regardless of IPAF status, the presence of a UIP pattern (152 of 176; 86.4%) significantly predicted an increased mortality risk (hazard ratio [HR], 7.31; 95% CI, 1.77–30.13; P = .006) (Table 4). After multivariable adjustment for age, gender, forced vital capacity, diffusing capacity of the lung for carbon monoxide, and the presence of clinical domain features, only the presence of a UIP pattern remained significantly predictive of increased mortality risk in the entire IIP cohort (HR, 4.64; 95% CI, 1.08–20.00; P = .04) and within the IPAF cohort (HR, 5.35; 95% CI, 1.21–23.67; P = .03).
Figure 4.
Survival in patients with interstitial pneumonia and autoimmune features (IPAF) who met the criteria for classified by surgical lung biopsy, with or without the presence of unexplained pulmonary vasculopathy on histopathology.
Figure 5.
Survival of patients with noninterstitial pneumonia with autoimmune features (IPAF) classified by surgical lung biopsy (SLB), with or without the presence of pulmonary vasculopathy on histopathology (PH).
Table 4.
Prognostic Value of Pathologic Featuresa
| Variables | IIP
|
IPAF
|
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted, n = 169
|
Adjusted,b n = 166
|
Unadjusted, n = 84
|
Adjusted,b n = 81
|
|||||||||
| HR | P value | 95% CI | HR | P value | 95% CI | HR | P value | 95% CI | HR | P value | 95% CI | |
| IPAF histopathologic criteria | 0.55 | .05 | 0.31–1.00 | 0.77 | .41 | 0.41–1.44 | 0.82 | .63 | 0.37–1.81 | 1.07 | .87 | 0.47–2.46 |
| UIP Pattern | 7.31 | .006 | 1.77–30.13 | 4.64 | .04 | 1.08–20.00 | 6.11 | .01 | 1.43–26.08 | 5.35 | .03 | 1.21–23.67 |
| NSIP | 0.48 | .12 | 0.19–1.22 | 0.71 | .50 | 0.26–1.90 | ||||||
| OP | 0.59 | .31 | 0.21–1.64 | 0.99 | .98 | 0.34–2.90 | ||||||
| Interstitial lymphoid aggregates with GCs | 0.9 | .83 | 0.36–2.72 | 1.12 | .84 | 0.38–3.29 | ||||||
| Diffuse lymphoplasmacytic infiltrates | 1.13 | .79 | 0.48–2.64 | 1.58 | .37 | 0.58–4.26 | ||||||
| Pulmonary vasculopathy | 1.65 | .07 | 0.96–2.83 | 2.50 | .04 | 1.05–5.92 | ||||||
Abbreviations: DLCO, diffusing capacity of the lungs for carbon monoxide; FVC, forced vital capacity; GC, germinal center; HR, hazard ratio; IIP, idiopathic interstitial pneumonia; IPAF, interstitial pneumonia with autoimmune features; OP, organizing pneumonia; NSIP, nonspecific interstitial pneumonia; UIP, usual interstitial pneumonia.
Bolded data denote significant values at a .05 level of significance.
Adjusted for age, gender, FVC, DLCO, and the presence of clinical domain features.
DISCUSSION
In this article, we report our methodological approach for identifying histopathologic IPAF criteria, demonstrate a significant increase in the number of patients meeting IPAF criteria because of focused pathologic review, and highlight the prognostic value of the IPAF pathologic criteria. The demographic characteristics of this cohort were not significantly different from our previously described IPAF cohort, which included patients without histopathology.9 Patients meeting IPAF criteria tended to be younger and female. Although autoimmune features may present at any age, the pattern of female predominance aligns with the expected gender distribution in individuals with underlying features of CTD.3,4
Retroactive application of the IPAF histopathologic criteria identified an additional 10 patients with these findings, 7 of whom then met criteria for IPAF. The remaining 3 patients did not fulfill criteria from clinical and/or serologic domains. Similar to our previous findings,9 a UIP pattern of fibrosis was prevalent among patients with IIP at our institution, irrespective of IPAF classification; however, most patients with IIP, who were classified as having IPAF, demonstrated concurrent, histologic evidence of NSIP or organizing pneumonia on tissue specimens. This highlights the observation that, although UIP is not a feature listed on the IPAF morphologic criteria, pathologic evaluation of tissue specimens often demonstrated the coexistence of a UIP pattern with NSIP or organizing pneumonia in those specimens reclassified as IPAF (Figure 3).18–21
Our findings are consistent with those of other investigators who have demonstrated the coexistence of UIP and NSIP patterns.22,23 Katzenstein et al23 showed extensive areas of NSIP pattern in several UIP biopsy and explant specimens. The increasing recognition that both pathologic patterns of UIP and NSIP may coexist in a single biopsy specimen11,22,23 may be an important factor in distinguishing CTD-associated UIP from idiopathic UIP. With that recognition, assessing patients for NSIP should be performed in regions that are distant from the densely fibrotic areas with significant architectural distortion.2 The presence of a UIP pattern of fibrosis does not preclude the occurrence of organizing pneumonia; however, the simultaneous presence of UIP and organizing pneumonia in a specimen was not common among SLB/LTx specimens in our cohort. Furthermore, we did not observe a lymphoid interstitial pneumonia pattern in any tissue specimens from our IIP cohort.
We also found that interstitial lymphoid aggregates with germinal centers on tissue specimens did not universally reclassify those specimens as IPAF. We elected to use a threshold of 3 germinal centers in any one low-power field to score germinal centers as being present. That threshold was selected because of its increased specificity and easy applicability in routine practice. Although germinal centers may be observed in IPF, CTD-ILD, and hypersensitivity pneumonitis,19,24–26 patients with CTD-ILD are described as having higher germinal center scores than do patients with IPF.24 Furthermore, patients with hypersensitivity pneumonitis may have up to 2 germinal centers in one high-power field.25 The low prevalence of germinal centers and the limited size of our sample precluded the use of a germinal center score for further comparisons. Similarly, no standard approach exists for quantifying plasma cell extent that defines the presence of a significant lymphoplasmacytic infiltrate.27,28 In our evaluation, we used lymphocytes and 40 or more plasma cells in a high-power field as the threshold for determining the presence of a lymphoplasmacytic infiltrate.9 That threshold was also selected for its increased specificity and easy applicability in routine practice.
Patients who met IPAF histopathologic criteria demonstrated a trend toward improved survival when compared with other patients without IPAF IIP.9 However, the presence of multicompartment involvement in all patients with IIP substantially increased the mortality risk. Our study demonstrates that the increased risk appeared to be driven by the presence of pulmonary vasculopathy, which was associated with a UIP pattern in most cases. The increased mortality risk associated with the presence of pulmonary vasculopathy or UIP pattern was similar to that observed in IPF and certain CTD-ILDs.29–31
This study has several limitations. First, as we are a referral center, many SLBs were performed at outside institutions and were subsequently returned. Thus, a focused rereview could only be performed in a subset of individuals with IIP. Second, the low prevalence of each pathologic criterion limited our ability to determine their individual prognostic significance in both IPAF and IIP. Third, all specimens included in the focused rereview process were examined by one thoracic pathologist; however, that examination was performed in a blinded fashion for applying IPAF criteria. Fourth, the documentation in initial pathology reports was obtained as part of routine clinical care; therefore, there is a potential for interobserver variability because not all tissue specimens were read by the same thoracic pathologist. However, most tissue specimens were read by the thoracic pathologist with expertise in ILD, and less than 5% of reported slides were signed out by a covering surgical pathologist. Fifth, our study was performed at a single, tertiary referral center with expertise in ILD; thus, our findings require external validation.
In conclusion, our findings underscore the challenges encountered with accurate disease classification in the evaluation of patients with idiopathic ILDs. Individual IPAF histopathologic features should be routinely assessed as part of the clinical pathologic interpretation because our results indicate that this is important in identifying patients who meet IPAF criteria. Because the IPAF designation inherently requires multidisciplinary evaluation, it is critical that patients whose biopsies demonstrate features of IPAF also undergo thorough clinical and serologic evaluation. In routine clinical practice, we suggest that features of IPAF be included in the comment section of pathology reports, and, when the IPAF morphologic criteria are met, a recommendation be made for comprehensive serologic studies. A focused rereview of pathology slides is necessary for the retrospective application of IPAF histopathologic criteria given the high frequency with which those features were identified. Thus, in patients with idiopathic ILD, familiarity with the IPAF histopathologic criteria increases the recognition of patients who meet IPAF criteria, which may, in turn, alter management. In the future, larger, multicenter studies investigating the differences in outcomes among patients based on IPAF histopathologic criteria may further determine the clinical significance of these morphologic features.
Acknowledgments
This investigation was supported by a US National Institutes of Health T32 training grant (T32-HL007605).
Footnotes
The authors have no relevant financial interest in the products or companies described in this article.
References
- 1.Corte TJ, Copley SJ, Desai SR, et al. Significance of connective tissue disease features in idiopathic interstitial pneumonia. Eur Respir J. 2012;39(3):661–668. doi: 10.1183/09031936.00174910. [DOI] [PubMed] [Google Scholar]
- 2.Cipriani NA, Strek M, Noth I, et al. Pathologic quantification of connective tissue disease-associated versus idiopathic usual interstitial pneumonia. Arch Pathol Lab Med. 2012;136(10):1253–1258. doi: 10.5858/arpa.2012-0102-OA. [DOI] [PubMed] [Google Scholar]
- 3.Kim HC, Ji W, Kim MY, et al. Interstitial pneumonia related to undifferentiated connective tissue disease: pathologic pattern and prognosis. Chest. 2015;147(1):165–172. doi: 10.1378/chest.14-0272. [DOI] [PubMed] [Google Scholar]
- 4.Vij R, Noth I, Strek ME. Autoimmune-featured interstitial lung disease: a distinct entity. Chest. 2011;140(5):1292–1299. doi: 10.1378/chest.10-2662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fischer A, West SG, Swigris JJ, Brown KK, du Bois RM. Connective tissue disease-associated interstitial lung disease: a call for clarification. Chest. 2010;138(2):251–256. doi: 10.1378/chest.10-0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kinder BW, Collard HR, Koth L, et al. Idiopathic nonspecific interstitial pneumonia: lung manifestation of undifferentiated connective tissue disease? Am J Respir Crit Care Med. 2007;176(7):691–697. doi: 10.1164/rccm.200702-220OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vij R, Strek ME. Diagnosis and treatment of connective tissue disease-associated interstitial lung disease. Chest. 2013;143(3):814–824. doi: 10.1378/chest.12-0741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fischer A, Antoniou KM, Brown KK, et al. ERS/ATS Task Force on Undifferentiated Forms of CTD-ILD. An official European Respiratory Society/American Thoracic Society research statement: interstitial pneumonia with autoimmune features. Eur Respir J. 2015;46(4):976–987. doi: 10.1183/13993003.00150-2015. [DOI] [PubMed] [Google Scholar]
- 9.Oldham JM, Adegunsoye A, Valenzi E, et al. Characterisation of patients with interstitial pneumonia with autoimmune features. Eur Respir J. 2016;47(6):1767–1775. doi: 10.1183/13993003.01565-2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raghu G, Collard HR, Egan JJ, et al. ATS/ERS/JRS/ALAT Committee on Idiopathic Pulmonary Fibrosis. An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med. 2011;183(6):788–824. doi: 10.1164/rccm.2009-040GL. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Travis WD, Costabel U, Hansell DM, et al. ATS/ERS Committee on Idiopathic Interstitial Pneumonias. An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013;188(6):733–748. doi: 10.1164/rccm.201308-1483ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Travis WD, Hunninghake G, King TE, Jr, et al. Idiopathic nonspecific interstitial pneumonia: report of an American Thoracic Society project [published correction appears in Am J Respir Crit Care Med. 2008;178(2):211] Am J Respir Crit Care Med. 2008;177(12):1338–1347. doi: 10.1164/rccm.200611-1685OC. [DOI] [PubMed] [Google Scholar]
- 13.Maldonado F, Daniels CE, Hoffman EA, Yi ES, Ryu JH. Focal organizing pneumonia on surgical lung biopsy: causes, clinicoradiologic features, and outcomes. Chest. 2007;132(5):1579–1583. doi: 10.1378/chest.07-1148. [DOI] [PubMed] [Google Scholar]
- 14.American Thoracic Society; European Respiratory Society. American Thoracic Society/European Respiratory Society international multidisciplinary consensus classification of the idiopathic interstitial pneumonias: this joint statement of the American Thoracic Society (ATS), and the European Respiratory Society (ERS) was adopted by the ATS board of directors, June 2001 and by the ERS Executive Committee, June 2001 [published correction appears in Am J Respir Crit Care Med. 2002:166(3):426] Am J Respir Crit Care Med. 2002;165(2):277–304. doi: 10.1164/ajrccm.165.2.ats01. [DOI] [PubMed] [Google Scholar]
- 15.Todd NW, Marciniak ET, Sachdeva A, et al. Organizing pneumonia/non-specific interstitial pneumonia overlap is associated with unfavorable lung disease progression. Respir Med. 2015;109(11):1460–1468. doi: 10.1016/j.rmed.2015.09.015. [DOI] [PubMed] [Google Scholar]
- 16.Ryu JH, Sekiguchi H, Yi ES. Pulmonary manifestations of immunoglobulin G4-related sclerosing disease. Eur Respir J. 2012;39(1):180–186. doi: 10.1183/09031936.00025211. [DOI] [PubMed] [Google Scholar]
- 17.Ryerson CJ, Vittinghoff E, Ley B, et al. Predicting survival across chronic interstitial lung disease: the ILD-GAP model. Chest. 2014;145(4):723–728. doi: 10.1378/chest.13-1474. [DOI] [PubMed] [Google Scholar]
- 18.Wuyts WA, Cavazza A, Rossi G, Bonella F, Sverzellati N, Spagnolo P. Differential diagnosis of usual interstitial pneumonia: when is it truly idiopathic [published correction appears in Eur Respir Rev 2014;23(134):537]? Eur Respir Rev. 2014;23(133):308–319. doi: 10.1183/09059180.00004914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Enomoto Y, Takemura T, Hagiwara E, et al. Features of usual interstitial pneumonia in patients with primary Sjögren’s syndrome compared with idiopathic pulmonary fibrosis. Respir Investig. 2014;52(4):227–235. doi: 10.1016/j.resinv.2014.02.003. [DOI] [PubMed] [Google Scholar]
- 20.Fang X, Luo B, Yi X, et al. Usual interstitial pneumonia coexisted with nonspecific interstitial pneumonia, what’s the diagnosis? Diagn Pathol. 2012;7:167. doi: 10.1186/1746-1596-7-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Collins B, Raghu G. Interstitial pneumonia with autoimmune features: the new consensus-based definition for this cohort of patients should be broadened [comment] Eur Respir J. 2016;47(4):1293–1295. doi: 10.1183/13993003.02084-2015. [DOI] [PubMed] [Google Scholar]
- 22.Rabeyrin M, Thivolet F, Ferretti GR, et al. Usual interstitial pneumonia end-stage features from explants with radiologic and pathological correlations. Ann Diagn Pathol. 2015;19(4):269–276. doi: 10.1016/j.anndiagpath.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 23.Katzenstein AL, Zisman DA, Litzky LA, Nguyen BT, Kotloff RM. Usual interstitial pneumonia: histologic study of biopsy and explant specimens. Am J Surg Pathol. 2002;26(12):1567–1577. doi: 10.1097/00000478-200212000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Song JW, Do KH, Kim MY, Jang SJ, Colby TV, Kim DS. Pathologic and radiologic differences between idiopathic and collagen vascular disease-related usual interstitial pneumonia. Chest. 2009;136(1):23–30. doi: 10.1378/chest.08-2572. [DOI] [PubMed] [Google Scholar]
- 25.Myers JL. Hypersensitivity pneumonia: the role of lung biopsy in diagnosis and management. Mod Pathol. 2012;25(suppl 1):S58–S67. doi: 10.1038/modpathol.2011.152. [DOI] [PubMed] [Google Scholar]
- 26.Adegunsoye A, Oldham JM, Demchuk C, Montner S, Vij R, Strek ME. Predictors of survival in coexistent hypersensitivity pneumonitis with autoimmune features. Respir Med. 2016;114:53–60. doi: 10.1016/j.rmed.2016.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yi ES, Sekiguchi H, Peikert T, Ryu JH, Colby TV. Pathologic manifestations of Immunoglobulin(Ig)G4-related lung disease. Semin Diagn Pathol. 2012;29(4):219–225. doi: 10.1053/j.semdp.2012.07.002. [DOI] [PubMed] [Google Scholar]
- 28.Yamashita K, Haga H, Kobashi Y, Miyagawa-Hayashino A, Yoshizawa A, Manabe T. Lung involvement in IgG4-related lymphoplasmacytic vasculitis and interstitial fibrosis: report of 3 cases and review of the literature. Am J Surg Pathol. 2008;32(11):1620–1626. doi: 10.1097/PAS.0b013e318172622f. [DOI] [PubMed] [Google Scholar]
- 29.Nadrous HF, Pellikka PA, Krowka MJ, et al. Pulmonary hypertension in patients with idiopathic pulmonary fibrosis. Chest. 2005;128(4):2393–2399. doi: 10.1378/chest.128.4.2393. [DOI] [PubMed] [Google Scholar]
- 30.Takahashi K, Taniguchi H, Ando M, et al. Mean pulmonary arterial pressure as a prognostic indicator in connective tissue disease associated with interstitial lung disease: a retrospective cohort study. BMC Pulm Med. 2016;16(1):55. doi: 10.1186/s12890-016-0207-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chung L, Domsic RT, Lingala B, et al. Survival and predictors of mortality in systemic sclerosis-associated pulmonary arterial hypertension: outcomes from the pulmonary hypertension assessment and recognition of outcomes in scleroderma registry. Arthritis Care Res (Hoboken) 2014;66(3):489–495. doi: 10.1002/acr.22121. [DOI] [PMC free article] [PubMed] [Google Scholar]