Abstract
The conservative management of upper tract urothelial carcinoma (UTUC) has historically been offered to patients with imperative indications. The recent International Consultation on Urologic Diseases publication on UTUC stratified treatment allocations based on high and low-risk groups. The risk-stratified approach allows selective patients who could benefit from kidney preserving procedures (KPP) with oncological outcomes similar to radical nephroureterectomy (RNU) with bladder cuff excision. There are no prospective randomized controlled studies to support management guidelines. Recent developments in imaging, minimally invasive techniques, multi-modality approaches, adjuvant topical and systemic chemotherapeutic regimens and bladder cancer prevention raise the hope for improved risk stratification and treatments with superior oncological outcomes.
Keywords: Urothelial cancer, upper tract, nephroureterectomy, ureteroscopy, renal pelvis, calyces
Introduction
Upper Tract Urothelial Carcinoma (UTUC) is a rare disease. Approximately two-thirds of UTUCs present as high-grade invasive disease at the time of diagnosis, and multifocal disease has been reported in about 25–30% of UTUCs [1, 2]. Radical nephroureterectomy (RNU) with excision of the bladder cuff is the gold standard surgical procedure for the treatment of UTUC in patients with a normal functional contralateral kidney with no evidence of metastatic disease [3]. The tumor characteristics can only be accurately determined by analysis of pathological specimens after RNU [4].
Low-risk cancers (defined for this section as pT0/pTa/pTis/pT1 low grade tumors) are reported in approximately 40–56% of UTUCs that undergo RNU, which may represent patients amenable to kidney preserving procedure (KPP) such as endoscopic management (ureteroscopic or percutaneous approach), partial nephrectomy and segmental ureterectomy [5, 6].
The management of UTUC should attempt to stratify patients in a pre-operative setting, allowing identification of individuals who may benefit from conservative kidney preserving procedures (KPP) without compromising oncological outcomes while preserving renal function [7]. Several studies have reported KPP for the treatment of low-risk UTUC in selected patients, suggesting similar oncological outcomes as the gold standard RNU [8]. This stratification can be performed using various prognostic factors that have been shown to be predictive of outcomes in multiple studies [9].
The KPP approach in the management of UTUC has been offered to patients with normal contralateral renal function, for low risk tumors as defined above, including selective cases of carcinoma in-situ (CIS) or high-grade presumed noninvasive tumors. Conservative approaches can also be considered in imperative cases in those with renal insufficiency, bilateral UTUC, solitary kidney and associated severe morbid conditions that preclude fitness for surgery [10]. Strict surveillance is a prerequisite for follow-up after KPP allowing detection of recurrence and disease progression. The focus of this review is to provide an overview of the current indications and modalities of KPP in the management of low-risk UTUC, and assessing the recommendations based on the level of evidence and grade of recommendations.
Endoscopic treatment of low-risk UTUC
The objectives of the endoscopic management of low-risk UTUC are to control local tumor growth, prevent local recurrence and disease progression while preserving the renal function in selected patients. The endoscopic management of low-risk UTUC needs meticulous and stringent close follow-up due to limitations of clinical staging with ureteroscopic biopsy, imaging studies and risk of high recurrence rates in these patients. There have been no prospective randomized studies comparing endoscopic management with RNU in support of the management guidelines. Most available published data to date is limited to retrospective or pooled retrospective data from selected institutes or case reports. These retrospective cohort studies would fall under the category of level 3-evidence. In a recent systematic review, a 52% recurrence of UTUC after endoscopic management and 37% recurrence was reported in percutaneous management [11]. Tumor grade, multifocality, tumor size, history of bladder cancer have been reported as predictors of UTUC recurrence [12]. Whether or not the addition of topical therapy can improve these recurrence rates remains a topic of some debate and is discussed further below.
Endoscopic management of UTUC is deemed a failure if clinical or radiological evidence of locally advanced or metastatic disease or pathological up staging or up grading is found on subsequent RNU specimen. Cutress et al. reported pooled data of failure rates for ureteroscopic treatment of around 24% and for the percutaneous approach around 32% [11]. A follow-up biopsy of the tumor base after ablation of the lesions might be helpful to determine if additional modalities of treatment are required (Table-1).
Table 1.
Recommendations for diagnosis and management of low risk tumors.
| Recommendations for endoscopic management | LEV | GOR |
|---|---|---|
| Unifocal | 3 | B |
| Small lesions (<2cm) | 3 | C |
| Low-grade tumor on biopsy | 3 | B |
| Negative cytology | 3 | C |
| Complete visualization | 3 | B |
| Papillary tumor | 3 | B |
| Good compliance | 3 | B |
| Understanding of invasive and close follow-up | 3 | B |
| All other tumor or patients features should be treated only in very selected patients with endoscopic treatment Recommendations for imaging | 3 | B |
| Imaging should be performed for exclusion of endoscopic treatment | 3 | B |
| CT-Urography should be performed for staging | 3 | B |
| Retrograde urography should be performed during endoscopic evaluation | 3 | C |
| Recommendations for diagnostic ureteroscopy | ||
| Ureteroscopic inspection of UTUC alone, without biopsy, has a very limited role, thus, biopsies are recommended | 3 | B |
| Tumor architecture, multifocality, number of lesions, size of lesions and their localizations should be documented | 3 | C |
| Localizations should also be evaluated for accessibility (need for flexible ureteroscopy, percutaneous approach) | 3 | C |
| Cystoscopy should be performed to exclude bladder cancer (up to 15%) | 3 | B |
| Recommendations for biopsy | ||
| Retrograde pyelography should be performed | 3 | C |
| Ureteroscopy should be performed | 3 | B |
| Flexible Ureteroscopy has technical advantages, especially for performing biopsies | 3 | C |
| The percutaneous approach is reserved for special indications | 3 | B |
| The biopsy can be performed using cup biopsies or using the basket | 3 | C |
| Ureteroscopic biopsy should be performed before endoscopic treatment | 3 | C |
| Number of biopsies should be more than 1 | 3 | C |
| Biopsy should distinguish between low and high-grade tumors | 3 | B |
| Grade is a surrogate marker. G1 correlates with low grade and low stage disease, whereas high grade correlates with high grade and high stage disease. | 3 | B |
| G2 alone is insufficient for the decision of endoscopic treatment, especially in elective cases. | 3 | B |
| The use of access sheets should be avoided during diagnostic approach | 4 | C |
| Recommendations for cytology and markers | ||
| Malignant tumor cells on urinary cytology suggest high grade / CIS disease | 3 | B |
| Cytology should be performed, because it can add information for decision making, however, voiding voided cytology is of little value. | 3 | C |
| Selective cytology from the upper tract should be considered to detect high grade and CIS | 3 | B |
| Urine markers like fluorescence in situ hybridization can increase sensitivity in experienced hands | 3 | C |
| Cytology should be done before using contrast agents and instrumentation because manipulation can lead to erroneous results | 3 | B |
LEV = Level of evidence; GOR = Grade of recommendation
1. Diagnosis
1.1. Imaging
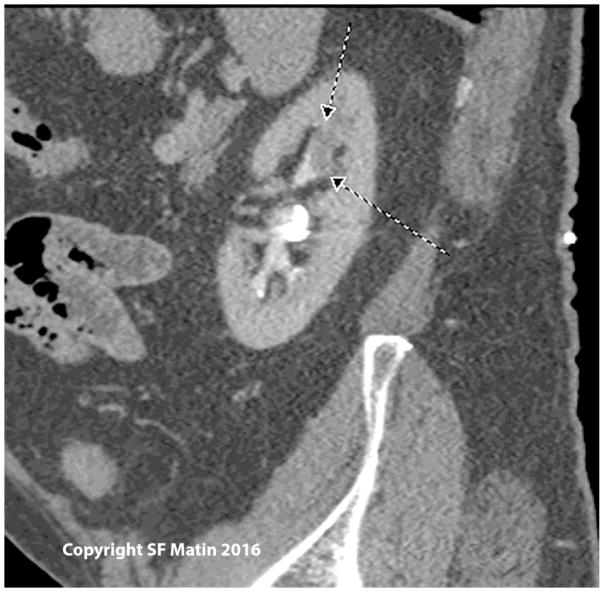
The Imaging modality identifying soft tissue density within the pelvicalyceal cavities and ureteral lumen has been most commonly used for the diagnosis of UTUC. CT urography (CTU) is a standard imaging study for the diagnosis of UTUC. Both nephrographic and excretory phases of CTU are complementary for the diagnosis of UTUC [13]. CTU using thin slices (<2mm) to visualize the entire urinary tract through multiplanar reformatted imaging (MPR) offers accuracy in diagnosing UTUC (Figure 1).
Figure 1.
Sagittal view of a computed tomography scan showing a filling defect representing a soft tissue mass in the upper pole of the left collecting system, in a patient with prior endoscopic therapy for low grade left ureteral tumors. Biopsy in this case showed high grade papillary tumor. Nephroureterectomy showed parenchymal invasion (stage pT3).
A filling defect or soft tissue density in the renal collecting system that enhances after the administration of contrast is highly suspicious for UTUC. CTU limitations leading to unclear findings might include flat lesions or focal wall thickening or sub-centimeter lesions for which attenuation measurements are difficult to characterize the lesion, or may be nonspecific findings [14]. A meta-analysis and systematic review of CTU for UTUC reported pooled sensitivity of 96% (95% CI, 88–100%) and specificity of 99% (95%CI, 98–100%) [15]. Another systematic review showed similar high sensitivity and specificity for CTU (96 and 99%) and retrograde urography (96 and 96%) in detecting the UTUC [16].
MR-Urography (MRU) had a high specificity of 97% with a rather low sensitivity of 69% [1]. Excretory urography had a low specificity of 81% and low sensitivity of 80%. It has been noted that sensitivities are lower with lower tumor burden for all imaging modalities [1].
1.2. Diagnostic Ureteroscopy (URS)
The development of high definition flexible fiber-optic and now digital URS has greatly improved visualizing the entire upper urinary tract and ureters. URS evaluation of UTUC should assess for tumor location, number, size, and architecture. URS assessment under direct vision of these parameters influences the treatment approach and outcomes. Ureteral access sheaths have been shown to increase the diagnostic efficacy of URS. Diagnostic URS should assess the ureter before the placement of ureteral access sheath. URS significantly missed concomitant CIS when compared to RNU specimens (9.7% vs. 43.3%) [17]. URS is invaluable in those cases where renal preservation may be paramount, such as individuals with renal insufficiency, solitary kidney, and multiple comorbidities. URS facilitates selective ureteral sampling for cytology from the renal pelvicalyceal system and ureters, which provides prognostic information. URS findings combining with biopsy grade, urinary/selective cytology, and imaging findings may help in determining if the patient would benefit from endoscopic management of UTUC (Table-1). The accuracy of URS biopsies for diagnosis and grading of UTUC is summarized in Table-2.
Table 2.
Accuracy of grading in ureteroscopic biopsies during diagnosis of UTUC
| Author | No. of UTUC cases (n) | No. of biopsies diagnostic (%) | No. Grading Correct (%) | No. of upgraded tumors |
|---|---|---|---|---|
| Gillan et al. 2015 [17] | 92 | 30 (32.6%) | 40 (43.4%) | 11 (11.9%) |
| Vashistha et al. 2013 [18] | 43 | 32 (74%) | 27/31 (87%) | 3/31 (9.7%) |
| Wang et al., 2012 [19] | 184 | 48 (26%) | 83 (45%) | 23 (96%) |
| Smith et al., 2011 [20] | 65 | NR | 41 (63%) | 24 (43%) |
| Williams et al., 2008 [21] | 30 | 30 (100%) | 17 (56.7%) | 3 (50%) |
| Shirashi et al., 2003 [22] | 40 | 35 (87.5%) | 18 (58%) | 0 (0%) |
| Skolarikos et al., 2003 [23] | 62 | 51 (82%) | 35 (69%) | NR |
| Guarnizo et al., 2000 [24] | 45 | 40 (89%) | 31(78%) | 5 (19%) |
| Keeley et al., 1997 [25] | 51 | 42 (82.4%) | 38 (90%) | 10% |
1.3. Biopsy
The difficulties in predicting accurate clinical staging result from limitations in biopsy specimen size and restriction of depth of resection. The tumor grade of UTUC is thus a primary driver in making treatment decisions, as grade is used to infer stage. Low-grade disease on biopsy specimen has a positive predictive value of 80–90% in predicting low stage disease, while high-grade disease has lower predictive value for invasiveness. It is often helpful for the pathologist to have more than one biopsy since non-diagnostic tissue materials are found in URS biopsy specimens up to 25% to 31.5% [17, 24, 26].
The primary objective of tumor biopsy is obtaining a proper grade rather than adequate staging. About 68–100% of G1 tumors on biopsy are non-invasive on final histology while 62–100% of G3 tumors are invasive. Results for G2 tumors vary significantly from 17–80%, again reflecting likely inclusion of both low and high-grade disease in this histological subgroup. Grade is one of the most important predictive factors for oncologic outcome of endoscopic treatment. High-grade UTUC has worse oncological outcomes. Gillan et al. in a retrospective multicenter study reported URS biopsy grade matched with final RNU histopathology on 43.4%, only 32.6% had concordance between URS biopsy and final pathology for both grade and stage of UTUC. Concomitant carcinoma in-situ (CIS) was found in 21.6% of cases in final RNU pathology, with finding of discordance between URS biopsy specimens and RNU specimens in the diagnosis of concomitant CIS in UTUC [17] (Table-1 and 3).
Table 3.
Outcomes of series using ureteroscopic treatment for UTUC
| Study | Number of patients | mean/median FU (months) | Recurrence (%) | OS (%) | CSS (%) | KPR (%) |
|---|---|---|---|---|---|---|
| LR / IVR | ||||||
| Hoffman et al 2014 [39] | 25 | 26 | 36/44 | 100 | 100 | 100 |
| Fajkovic et al., 2013 [5] | 20 | 20 | 25 / 15 | 45 | 95 | 100 |
| Cutress et al., 2012 [40] | 73 | 54 | 68 / 53 | 60 | 90 | 81 |
| Grasso et al., 2012 [41] | 66 | 51.5 | 77 / 61 | 74 | 87 | 83 |
| Gadzinski et al., 2010 [42] | 34 | 58 | 84 / NR | 75 | 100 | 89 |
| Cornu et al., 2010 [43] | 35 | 24 | 60 / 40 | 100 | 100 | 89 |
| Pak et al., 2009 [44] | 57 | 53 | 90 / NR | 93 | 95 | 81 |
| Lucas et al., 2008 [45] | 39 | 33 | 46 / NR | 62 | 82 | 72 |
| Painter et al., 2008 [46] | 45 | NR | NR / NR | NR | 89 | 91 |
| Krambeck et al., 2007 [47] | 37 | 32 | 62 / 37 | 35 | 70 | 70 |
| Reisiger et al., 2007 [48] | 10 | 73 | 50 / 70 | 100 | 100 | 90 |
| Roupret et al., 2006 [49] | 27 | 52 | 15 / 22 | 77 | 81 | 74 |
| Johnson et al., 2005 [50] | 35 | 32 | 68 / NR | NR | 100 | 97 |
| Iborra et al., 2003 [51] | 23 | NR | 35 / NR | NR | 96 | 91 |
| Matsuoka et al., 2003 [52] | 26 | 33 | 26 / 15 | NR | 89 | NR |
| Daneshmand et al., 2003 [53] | 30 | 31 | 90 / 23 | 77 | 97 | 87 |
| Chen et al., 2001 [54] | 23 | 30 | 64 / 12 | NR | NR | NR |
| Engelmyer et al., 1996 [55] | 10 | 43 | 70 / NR | 90 | 100 | 100 |
| Gaboardi et al., 1994 [56] | 18 | 15 | 50 / NR | 100 | 100 | 94 |
| Andersen et al., 1994 [2] | 10 | 25 | NR / NR | NR | NR | 80 |
| Schmeller et al., 1989 [57] | 16 | 14 | 19 / NR | 100 | 100 | 100 |
Abbreviations: CSS, cancer-specific survival; IVR, intravesical recurrence; NR, not reported; OS, overall survival; RNU, radical nephroureterectomy; LR, local recurrence; KPR, kidney preserving rate.
The multi-biopsy approach has been proposed to improve diagnosis. Biopsy grade was identical in 43.4% to 78% of cases to surgical pathology [17, 24]. The combined use of access sheath, cup biopsies, and baskets (particularly for papillary tumors) can yield substantially more tissue than has been historically possible (Figure 2).
Figure 2.

Photographs showing biopsy tools and potential specimen sizes. A) cup biopsy forceps and coaxial 3-way prong; B) steel-wire basket.
1.4. Cytology
Cytological examination is thought to play a significant role in diagnosis of high-grade urothelial cancer (UC) and CIS of the bladder, however, its role in the detection and management of UTUC is poorly investigated and controversy exists in the utility of routine cytology testing in the absence of radiographic or direct visual endoscopic evidence of a tumor. In cases where an upper tract source is suspected, selective ureteral samples (by catheterization or with brushing) are performed for lateralizing the source of the finding but should be confirmed endoscopically when possible. Recent interest in urinary biomarker studies for malignancies has developed [19]. The sensitivity of selective ureteral cytology for UTUC ranged from 43% to 78% [21, 27], with false-negative results as high as 50% for low-grade neoplasms [13].
Messer et al. evaluated patients who had undergone RNU or distal ureterectomy without previous history of bladder cancer and concluded the positive urine cytology was not predictive of either muscle invasive disease or high-grade urothelial lesions [29]. Selective upper tract cytology was more frequently positive than voiding urine cytology (60.3% vs. 33.6%, p<0.001). Sensitivity was 45.0% for low-grade UTUC, 66.3% for high-grade UTUC, and 78.6% for isolated CIS [15]. A multi-institutional retrospective study using Johns Hopkins Hospital template of cytopathology criteria reported sensitivity, specificity, PPV and NPV of UT urine cytology for high-grade UTUC were 71.4%, 91.9%, 66.7% and 93.4% respectively [31]. UT urine cytology has low sensitivity and specificity for low-grade UTUC [16–18].
The UroVysion test (Abbott Molecular, Des Plaines, IL, USA) is a multi-target multicolor fluorescent in situ hybridization (FISH) assay. This test has high occurrence of specific chromosomal abnormalities in urothelial cancers. UroVysion showed abnormalities in 91% of CIS and all invasive cancers and about 30% of nonneoplastic lesions in patients with concomitant urothelial carcinoma. The sensitivity of UroVysion ranges from 39 to 97% (average 74%) but is significantly lower for low-grade and low-stage tumors [19]. The UroVysion/fluorescent in-situ hybridization (FISH) combined with UT urine cytology may improve the sensitivity of detecting low grade-UTUC [35]. Table 1 shows the recommendations for cytology and markers.
2. Surgical Techniques
A Cochrane review of the surgical management of UTUC concluded that there is no high-quality evidence available to determine the best surgical management [21].
2.1. Endoscopic treatment of low-risk UTUC
2.1.1 Ureteroscopic management
Digital flexible URS is a most valuable instrument to evaluate the intrarenal collecting system and ureter under direct vision that enables complete ablation of the tumor. Advanced laser technology using holmium, holmium:yttrium aluminum garnet (YAG) and the neodymium:YAG lasers are efficient for treating neoplasms and can be delivered through a flexible ureteroscope.
The holmium:YAG laser energy tissue penetration is <0.5 mm, which enables excellent tumor ablation with a reduced risk of upper urinary tract perforation. The neodymium:YAG laser uses an alternative source of energy that has a tissue penetration of up to 5–6 mm and works by coagulative necrosis with eventual sloughing of the necrotic tumor. Laser technology for UTUC ablation through flexible URS has the advantage of lower morbidity compared to electrocautery. Other approaches include using a flat wire basket or tumor grasping forceps to debulk the tumor burden, with the tumor base treated with either electrocautery delivered through small Bugbee electrode (2 or 3 Fr) or laser ablation using flexible fibers (200 um or 365 um) that easily fit through the working channel of the URS [22, 23].
The outcomes of URS management of UTUC have been reported in various retrospective studies. The accuracy of URS grading is summarized in Table-2. URS management of UTUC can be associated with a high local recurrence (LR) and intravesical recurrence (IVR) rate. Table-3 shows these outcomes of URS management of UTUC.
2.1.2. Percutaneous management
The percutaneous antegrade approach can be considered for low-grade, large volume UTUCs that may not be anatomically accessible with flexible URS. After establishing percutaneous access, the tumor can be ablated using resectoscopes, cold cup biopsy forceps, or laser ablation. Percutaneous approach allows antegrade instillation of topical adjuvant agents if indicated after successful tumor ablation [45]. Retrospective studies have reported that the percutaneous approach had a lower local recurrence rates and lower IVR when compared to URS approach in the management of UTUC [46]. The oncological outcomes of the percutaneous approach in the management of UTUC are summarized in Table-4.
Table 4.
Outcomes of series using percutaneous approach for UTUC
| Study | Number of patients | mean FU (months) | Recurrence (%) | OS (%) | CSS (%) | KPR (%) |
|---|---|---|---|---|---|---|
| LR /IVR | ||||||
| Motamedinia et al. 2015 [60] | 141 | 66 | 37 LG, 63 HG/NR |
NR | NR | 87 |
| Rastinehad et al., 2009 [58] | 89 | 61 | 33 / NR | 68 | Nr | 87 |
| Roupret et al., 2007 [61] | 24 | 62 | 13 / 17 | 79 | 83 | 79 |
| median | ||||||
| Palou et el., 2004 [59] | 34 | 51 | 44 / NR | 74 | 94 | 74 |
| Goel et al., 2003 [62] | 20 | 64 | 65 / 15 | NR | 75 | 50 |
| Clark et al., 1999 [63] | 17 | 24 | 33 / NR | 75 | 82 | 88 |
| Patel et al., 1996 [64] | 26 | 45 | 35 / 42 | 75 | 91 | 94 |
| Plancke et al., 1995 [65] | 10 | 28 | 10/NR | 90 | 100 | 90 |
| Fuglsig et al., 1995 [66] | 26 | 21 | 31 / NR | 96 | 100 | 65 |
| Tasca et al., 1992 [67] | 10 | 19 | 50 / NR | 90 | 100 | 70 |
Abbreviations: CSS, cancer-specific survival; IVR, intravesical recurrence; NR, not reported; OS, overall survival; RNU, radical nephroureterectomy; LR, local recurrence; KPR, kidney preserving rate.
2.1.3. Adjuvant Topical Therapies
Recurrence rates in the upper tract following endoscopic treatment of UTUC have been reported in 30–70% of patients [68, 69]. Topical adjuvant agents might decrease the risk of local recurrence as suggested by several reported case series [57]. In theory, there should be a role of topical adjuvant therapies based on what is observed in patients with bladder cancer [9].
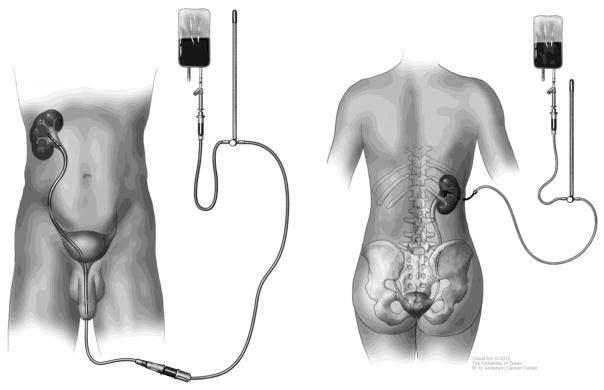
Adjuvant topical installation can be accomplished in either antegrade instillation through nephrostomy tube or retrograde instillation through an open-ended, multiple side hole ureteral catheter (Figure 3). Use of double-J stents promoting reflux is not a reliable delivery method and its use is discouraged.
Figure 3.
Figures showing our institutional technique for reliably instilling topical therapy to the upper tract by either nephrostomy tube or cystoscopically placed Beacon tip ureteral catheter. Patients are given the option of technique employed in the absence of data for the better technique.
Topical treatment of UTUC is made more complicated by the need for reliable approach of accessing the upper tract, mode of delivery, and lack of dwell time for the therapeutic agent. A single-institution retrospective study of 28 cases was recently presented, showing improved results of adjuvant topical chemotherapy to the upper tract when given as induction and maintenance therapy [60]. Lifshitz et al. recently reported a novel hydrogel polymer with reverse thermal gelation properties, solid at body temperature and liquid at cold temperature, which might promote high-dose delivery of Mitomycin C into the upper urinary tract [61]. This product is expected to enter a phase 2/3 trial in the United States by 2016 for intended use as chemoablation of low-grade UTUC.
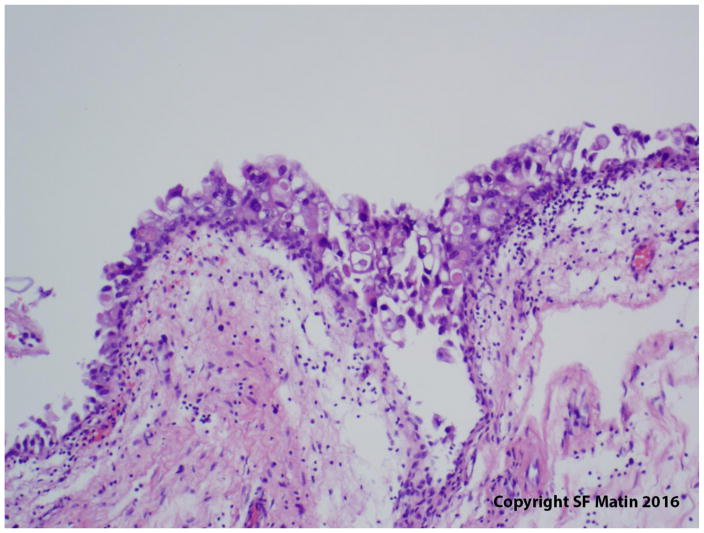
Patients with high-grade non-invasive UTUC considered for conservative management should be offered adjuvant installation of BCG. For isolated CIS (Figure 4), in the absence of any papillary tumors, topical therapy should be considered the primary mode of treatment, given the field-effect nature of the disease. The available data pertaining to BCG instillation in patients with CIS is limited to small series of retrospective studies.
Figure 4.
Photomicrograph showing upper tract carcinoma in-situ. Original magnification 200x.
Patients with UTUC treated with RNU subsequently developed IVR in approximately 30% [9]. The risk of IVR is even greater in patients managed with KPP, and such patients might logically benefit from the adjuvant intravesical instillation of chemotherapy. Two randomized clinical trials have demonstrated a decreased risk of IVR after radical nephroureterectomy when using a single dose of early intravesical instillation of chemotherapy [71, 72]. Future studies are needed to evaluate the benefit of single dose intravesical chemotherapy after KPP.
2.2. Conservative Surgery
2.2.1. Partial pyelectomy or partial nephrectomy
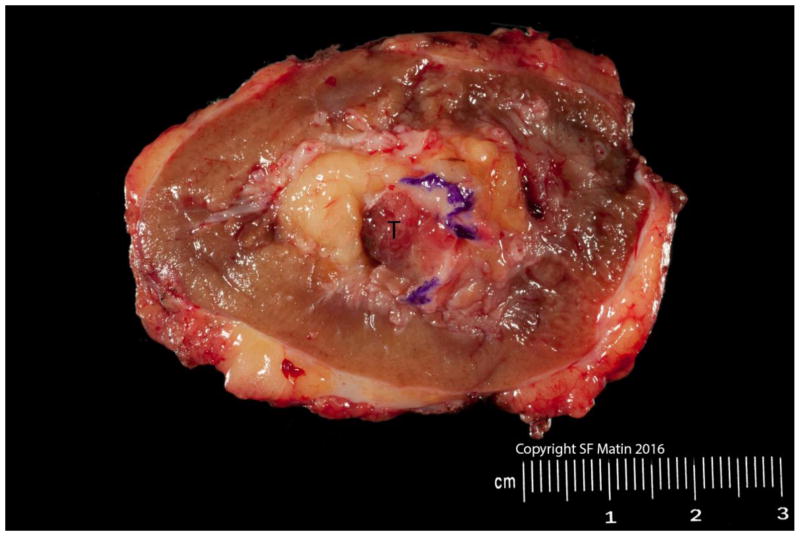
Partial pyelectomy or partial nephrectomy is rarely performed for renal pelvic tumors, in particular with advent of newer digital URS technologies. Partial nephrectomy has a very narrow indication for treatment of UTUC and is rarely undertaken due to the uncommon nature of the disease as well as the much higher technical complexity than partial nephrectomy for parenchymal tumors (Figure 5). Generally it is reserved for low-grade, unifocal polar tumors in the setting of solitary kidneys, and has had variably successful results [62].
Figure 5.
A partial nephrectomy specimen performed in a patient with a solitary kidney and polar tumor (T). Blue ink indicates the urothelial margin. As opposed to partial nephrectomy for parenchymal tumors, the urothelial margin needs to be planned and examined in addition when performing a partial nephrectomy for UTUC. Indications for partial nephrectomy are very narrow, and include an endoscopically unmanageable tumor, no multifocality, polar location, and imperative indications for kidney preservation.
2.2.2. Segmental ureterectomy
Ureteral cancers occur in the distal ureter about two-thirds of the time, and these may be managed with endoscopic ablation or segmental resection with ureteroneocystostomy in highly selected patients. High risk proximal or mid ureteral tumors are managed with RNU with bladder cuff excision. For low risk tumors, these can invariably be managed endoscopically in most cases.
3. Follow-up
The European Association of Urology (EAU) guidelines recommend close oncological follow-up for ≥5 years [63]. After conservative management, cystoscopy, ureteroscopy and cytology at 3 and 6 months, and then every 6 months for 2 years, then yearly. Urinary cytology and CTU at 3 and 6 months, and then yearly.
Low-risk UC have a low risk of progression to invasion (<3%), metastasis and death, but often recur as non-invasive lesions elsewhere within the urinary tract [77, 78]. Five-year disease specific survival for pT0/pTa/pTis is 100% and pT1 92% respectively [4]. Noting that the majority of UTUC cases are high-grade [4], the greatest potential lies in improving clinical risk stratification, which is highly limited in this disease.
3.1. Cystoscopy
IVR has been reported in 20–50% of patients after RNU for UTUC [10]. Recurrence is common within the first 2 years after the management of UTUC, thus strict follow-up with scheduled cystoscopic evaluation is prudent in detecting IVR [9].
3.2. Urinary cytology
Urine cytology preferably collected with selective washings might be helpful in assessing tumor recurrence after conservative treatment of low-risk UTUC.
3.3. Imaging
CTU is a standard imaging study for surveillance for early detection of potential recurrence following KPP approach for low-grade, low-stage UTUC. MRU is indicated in patients with renal insufficiency or allergic to iodinated based IV contrast media. However, gadolinium is contraindicated in patients with severe renal insufficiency (GFR <30 ml/min), although in these cases T2 weighted imaging without gadolinium may still be performed.
3.4. Ureteroscopy
Patients treated with KPP require close monitoring owing to the high risk of recurrence [1]. URS has become most valuable to evaluate these patients while assessing ipsilateral as well contralateral renal units for recurrence and selective collection of urine cytology.
Conclusions
The management of UTUC requires a risk-adopted approach, which determines who would benefit from KPP. This strategy has demonstrated oncological outcomes in selected patients, which appear to be comparable with gold standard RNU with bladder cuff excision in patients with low-risk UTUC, albeit only within the context of retrospective, single institutional data. Adjuvant topical therapies, particularly with novel agents, raise the hope of decreasing the risk of tumor recurrence and disease progression in those undergoing KPP. Recent developments in genomics, tumor biology, and molecular profiling of UTUCs hold promise in providing a better risk-adopted approach and development for future therapies.
Acknowledgments
the senior author would like to recognize the Monteleone Family Foundation for Research in Kidney and Bladder Cancer.
Footnotes
Statements:
Ethical standards: This review does not involve human subjects and meets Helsinki declaration for protection of human subjects.
Conflict of interest: No conflicts of interest by any author directly related to the topic.
Authors’f Contribution:
Mandalapu: Protocol/project development, Data collection or management, Data analysis, Manuscript writing/editing
Remzi: Data collection or management, Data analysis, Manuscript writing/editing
De Reijke: Data collection or management, Data analysis, Manuscript writing/editing
Margulis: Data collection or management, Data analysis, Manuscript writing/editing
Palou: Data collection or management, Data analysis, Manuscript writing/editing
Kapoor: Data collection or management, Data analysis, Manuscript writing/editing
Yossepowitch: Data collection or management, Data analysis, Manuscript writing/editing
Coleman: Data collection or management, Data analysis, Manuscript writing/editing
Traxer: Data collection or management, Data analysis, Manuscript writing/editing
Anderson: Data collection or management, Data analysis, Manuscript writing/editing
Catto: Data collection or management, Data analysis, Manuscript writing/editing
de la Rosette: Data collection or management, Data analysis, Manuscript writing/editing
O’Brien: Data collection or management, Data analysis, Manuscript writing/editing
Zlotta: Data collection or management, Data analysis, Manuscript writing/editing
Matin: Protocol/project development, Data collection or management, Data analysis, Manuscript writing/editing
References
- 1.Roupret M, et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Cell Carcinoma: 2015 Update. Eur Urol. 2015;68(5):868–79. doi: 10.1016/j.eururo.2015.06.044. [DOI] [PubMed] [Google Scholar]
- 2.Andersen JR, Kristensen JK. Ureteroscopic management of transitional cell tumors. Scand J Urol Nephrol. 1994;28(2):153–7. doi: 10.3109/00365599409180492. [DOI] [PubMed] [Google Scholar]
- 3.Roupret M, et al. European guidelines on upper tract urothelial carcinomas: 2013 update. Eur Urol. 2013;63(6):1059–71. doi: 10.1016/j.eururo.2013.03.032. [DOI] [PubMed] [Google Scholar]
- 4.Margulis V, et al. Outcomes of radical nephroureterectomy: a series from the Upper Tract Urothelial Carcinoma Collaboration. Cancer. 2009;115(6):1224–33. doi: 10.1002/cncr.24135. [DOI] [PubMed] [Google Scholar]
- 5.Fajkovic H, et al. Results and outcomes after endoscopic treatment of upper urinary tract carcinoma: the Austrian experience. World J Urol. 2013;31(1):37–44. doi: 10.1007/s00345-012-0948-4. [DOI] [PubMed] [Google Scholar]
- 6.Sverrisson EF, et al. The merits of cytology in the workup for upper tract urothelial carcinoma - a contemporary review of a perplexing issue. Int Braz J Urol. 2014;40(4):493–8. doi: 10.1590/S1677-5538.IBJU.2014.04.07. [DOI] [PubMed] [Google Scholar]
- 7.Roupret M, Colin P, Yates DR. A new proposal to risk stratify urothelial carcinomas of the upper urinary tract (UTUCs) in a predefinitive treatment setting: low-risk versus high-risk UTUCs. Eur Urol. 2014;66(2):181–3. doi: 10.1016/j.eururo.2013.12.007. [DOI] [PubMed] [Google Scholar]
- 8.Yakoubi R, et al. Radical nephroureterectomy versus endoscopic procedures for the treatment of localised upper tract urothelial carcinoma: a meta-analysis and a systematic review of current evidence from comparative studies. Eur J Surg Oncol. 2014;40(12):1629–34. doi: 10.1016/j.ejso.2014.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Seisen T, et al. A Systematic Review and Meta-analysis of Clinicopathologic Factors Linked to Intravesical Recurrence After Radical Nephroureterectomy to Treat Upper Tract Urothelial Carcinoma. Eur Urol. 2015;67(6):1122–33. doi: 10.1016/j.eururo.2014.11.035. [DOI] [PubMed] [Google Scholar]
- 10.Roupret M, et al. European Association of Urology Guidelines on Upper Urinary Tract Urothelial Cell Carcinoma: 2015 Update. Eur Urol. 2015 doi: 10.1016/j.eururo.2015.06.044. [DOI] [PubMed] [Google Scholar]
- 11.Cutress ML, et al. Ureteroscopic and percutaneous management of upper tract urothelial carcinoma (UTUC): systematic review. BJU Int. 2012;110(5):614–28. doi: 10.1111/j.1464-410X.2012.11068.x. [DOI] [PubMed] [Google Scholar]
- 12.Thompson RH, et al. Elective endoscopic management of transitional cell carcinoma first diagnosed in the upper urinary tract. BJU Int. 2008;102(9):1107–10. doi: 10.1111/j.1464-410X.2008.07766.x. [DOI] [PubMed] [Google Scholar]
- 13.Takeuchi M, et al. CT Urography for Diagnosis of Upper Urinary Tract Urothelial Carcinoma: Are Both Nephrographic and Excretory Phases Necessary? AJR Am J Roentgenol. 2015;205(3):W320–7. doi: 10.2214/AJR.14.14075. [DOI] [PubMed] [Google Scholar]
- 14.Potretzke AM, et al. Urology. 2015. Is Ureteroscopy Needed Prior to Nephroureterectomy? an Evidence-Based Algorithmic Approach. Published online: November 3 2015. [DOI] [PubMed] [Google Scholar]
- 15.Chlapoutakis K, et al. Performance of computed tomographic urography in diagnosis of upper urinary tract urothelial carcinoma, in patients presenting with hematuria: Systematic review and meta-analysis. Eur J Radiol. 2010;73(2):334–8. doi: 10.1016/j.ejrad.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 16.Razavi SA, et al. Comparative effectiveness of imaging modalities for the diagnosis of upper and lower urinary tract malignancy: a critically appraised topic. Acad Radiol. 2012;19(9):1134–40. doi: 10.1016/j.acra.2012.05.004. [DOI] [PubMed] [Google Scholar]
- 17.Gillan A, et al. Carcinoma in situ is significantly underdetected by prenephroureterectomy ureteroscopy in the management of upper tract urothelial cancers. Biomed Res Int. 2015;2015:547586. doi: 10.1155/2015/547586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Vashistha V, Shabsigh A, Zynger DL. Utility and diagnostic accuracy of ureteroscopic biopsy in upper tract urothelial carcinoma. Arch Pathol Lab Med. 2013;137(3):400–7. doi: 10.5858/arpa.2012-0136-OA. [DOI] [PubMed] [Google Scholar]
- 19.Wang J, et al. Distinguishing urothelial carcinoma in the upper urinary tract from benign diseases with hematuria using FISH. Acta Cytol. 2012;56(5):533–8. doi: 10.1159/000341622. [DOI] [PubMed] [Google Scholar]
- 20.Smith AK, et al. Inadequacy of biopsy for diagnosis of upper tract urothelial carcinoma: implications for conservative management. Urology. 2011;78(1):82–6. doi: 10.1016/j.urology.2011.02.038. [DOI] [PubMed] [Google Scholar]
- 21.Williams SK, et al. Correlation of upper-tract cytology, retrograde pyelography, ureteroscopic appearance, and ureteroscopic biopsy with histologic examination of upper-tract transitional cell carcinoma. J Endourol. 2008;22(1):71–6. doi: 10.1089/end.2007.9853. [DOI] [PubMed] [Google Scholar]
- 22.Shiraishi K, et al. Role of ureteroscopic biopsy in the management of upper urinary tract malignancy. Int J Urol. 2003;10(12):627–30. doi: 10.1046/j.1442-2042.2003.00721.x. [DOI] [PubMed] [Google Scholar]
- 23.Skolarikos A, et al. Cytologic analysis of ureteral washings is informative in patients with grade 2 upper tract TCC considering endoscopic treatment. Urology. 2003;61(6):1146–50. doi: 10.1016/s0090-4295(03)00026-8. [DOI] [PubMed] [Google Scholar]
- 24.Guarnizo E, et al. Ureteroscopic biopsy of upper tract urothelial carcinoma: improved diagnostic accuracy and histopathological considerations using a multi-biopsy approach. J Urol. 2000;163(1):52–5. doi: 10.1016/s0022-5347(05)67970-0. [DOI] [PubMed] [Google Scholar]
- 25.Keeley FX, et al. Diagnostic accuracy of ureteroscopic biopsy in upper tract transitional cell carcinoma. J Urol. 1997;157(1):33–7. [PubMed] [Google Scholar]
- 26.Tavora F, et al. Small endoscopic biopsies of the ureter and renal pelvis: pathologic pitfalls. Am J Surg Pathol. 2009;33(10):1540–6. doi: 10.1097/PAS.0b013e3181aec42a. [DOI] [PubMed] [Google Scholar]
- 27.Renshaw AA. Comparison of ureteral washing and biopsy specimens in the community setting. Cancer. 2006;108(1):45–8. doi: 10.1002/cncr.21456. [DOI] [PubMed] [Google Scholar]
- 28.Sedlock DJ, MacLennan GT. Urine cytology in the evaluation of upper tract urothelial lesions. J Urol. 2004;172(6 Pt 1):2406. doi: 10.1097/01.ju.0000145261.49281.bb. [DOI] [PubMed] [Google Scholar]
- 29.Messer J, et al. Urinary cytology has a poor performance for predicting invasive or high-grade upper-tract urothelial carcinoma. BJU Int. 2011;108(5):701–5. doi: 10.1111/j.1464-410X.2010.09899.x. [DOI] [PubMed] [Google Scholar]
- 30.Comploj EBM, Capitanio U, Cha E, Colin P, Fritsche HM, Herrmann T, Hübner W, Klatte T, Merseburger A, Montorsi F, Pycha A, Roscigno M, Rouprêt M, Shariat S, Zigeuner R, Remzi M. Role of conventional cytology in the treatment of upper tract urothelial carcinoma (OSS-UTUC): Results from the multi-institutional organ-sparing-UTUC collaboration. Eur Urol. 2013 [Google Scholar]; Eur Urol Suppl. 2013;(12):e601–2. [Google Scholar]
- 31.Chen L, et al. Upper tract urinary cytology to detect upper tract urothelial carcinoma: Using the Johns Hopkins Hospital template and evaluation of its feasibility. Cytojournal. 2015;12:17. doi: 10.4103/1742-6413.161608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tanaka N, et al. The predictive value of positive urine cytology for outcomes following radical nephroureterectomy in patients with primary upper tract urothelial carcinoma: a multi-institutional study. Urol Oncol. 2014;32(1):48e19–26. doi: 10.1016/j.urolonc.2013.07.003. [DOI] [PubMed] [Google Scholar]
- 33.Wang L. Diagnsosis of upper tract urothelial carcinoma-A comparative study of urine cytology and surgical biopsy. J Am Soc Cytopathol. 2015;(4):3–9. doi: 10.1016/j.jasc.2014.09.203. [DOI] [PubMed] [Google Scholar]
- 34.Daniely M, et al. Combined morphologic and fluorescence in situ hybridization analysis of voided urine samples for the detection and follow-up of bladder cancer in patients with benign urine cytology. Cancer. 2007;111(6):517–24. doi: 10.1002/cncr.23119. [DOI] [PubMed] [Google Scholar]
- 35.Reynolds JP, et al. Comparison of urine cytology and fluorescence in situ hybridization in upper urothelial tract samples. Cancer Cytopathol. 2014;122(6):459–67. doi: 10.1002/cncy.21414. [DOI] [PubMed] [Google Scholar]
- 36.Rai BP, et al. Surgical management for upper urinary tract transitional cell carcinoma. Cochrane Database Syst Rev. 2011;(4):CD007349. doi: 10.1002/14651858.CD007349.pub2. [DOI] [PubMed] [Google Scholar]
- 37.Seisen T, Colin P, Roupret M. Risk-adapted strategy for the kidney-sparing management of upper tract tumours. Nat Rev Urol. 2015;12(3):155–66. doi: 10.1038/nrurol.2015.24. [DOI] [PubMed] [Google Scholar]
- 38.Kalaitzis C, et al. Ureteroscopic laser treatment of upper urinary tract urothelial cell carcinomas: can a tumour free status be achieved? Adv Urol. 2013;2013:429585. doi: 10.1155/2013/429585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hoffman A, et al. Oncologic results of nephron sparing endoscopic approach for upper tract low grade transitional cell carcinoma in comparison to nephroureterectomy - a case control study. BMC Urol. 2014;14:97. doi: 10.1186/1471-2490-14-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cutress ML, et al. Long-term endoscopic management of upper tract urothelial carcinoma: 20-year single-centre experience. BJU Int. 2012;110(11):1608–17. doi: 10.1111/j.1464-410X.2012.11169.x. [DOI] [PubMed] [Google Scholar]
- 41.Grasso M, et al. Ureteroscopic and extirpative treatment of upper urinary tract urothelial carcinoma: a 15-year comprehensive review of 160 consecutive patients. BJU Int. 2012;110(11):1618–26. doi: 10.1111/j.1464-410X.2012.11066.x. [DOI] [PubMed] [Google Scholar]
- 42.Gadzinski AJ, et al. Long-term outcomes of nephroureterectomy versus endoscopic management for upper tract urothelial carcinoma. J Urol. 2010;183(6):2148–53. doi: 10.1016/j.juro.2010.02.005. [DOI] [PubMed] [Google Scholar]
- 43.Cornu JN, et al. Oncologic control obtained after exclusive flexible ureteroscopic management of upper urinary tract urothelial cell carcinoma. World J Urol. 2010;28(2):151–6. doi: 10.1007/s00345-009-0494-x. [DOI] [PubMed] [Google Scholar]
- 44.Pak RW, Moskowitz EJ, Bagley DH. What is the cost of maintaining a kidney in upper-tract transitional-cell carcinoma? An objective analysis of cost and survival. J Endourol. 2009;23(3):341–6. doi: 10.1089/end.2008.0251. [DOI] [PubMed] [Google Scholar]
- 45.Lucas SM, et al. Conservative management in selected patients with upper tract urothelial carcinoma compares favourably with early radical surgery. BJU Int. 2008;102(2):172–6. doi: 10.1111/j.1464-410X.2008.07535.x. [DOI] [PubMed] [Google Scholar]
- 46.Painter DJ, et al. Ureteroscopic management of upper-tract urothelial cancer: an exciting nephron-sparing option or an unacceptable risk? J Endourol. 2008;22(6):1237–9. doi: 10.1089/end.2008.0187. [DOI] [PubMed] [Google Scholar]
- 47.Krambeck AE, et al. Endoscopic management of upper tract urothelial carcinoma in patients with a history of bladder urothelial carcinoma. J Urol. 2007;177(5):1721–6. doi: 10.1016/j.juro.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 48.Reisiger K, et al. Office-based surveillance ureteroscopy after endoscopic treatment of transitional cell carcinoma: technique and clinical outcome. Urology. 2007;70(2):263–6. doi: 10.1016/j.urology.2007.03.065. [DOI] [PubMed] [Google Scholar]
- 49.Roupret M, et al. Comparison of open nephroureterectomy and ureteroscopic and percutaneous management of upper urinary tract transitional cell carcinoma. Urology. 2006;67(6):1181–7. doi: 10.1016/j.urology.2005.12.034. [DOI] [PubMed] [Google Scholar]
- 50.Johnson GB, Grasso M. Ureteroscopic management of upper urinary tract transitional cell carcinoma. Curr Opin Urol. 2005;15(2):89–93. doi: 10.1097/01.mou.0000160622.13366.a1. [DOI] [PubMed] [Google Scholar]
- 51.Iborra I, et al. Conservative elective treatment of upper urinary tract tumors: a multivariate analysis of prognostic factors for recurrence and progression. J Urol. 2003;169(1):82–5. doi: 10.1016/S0022-5347(05)64041-4. [DOI] [PubMed] [Google Scholar]
- 52.Matsuoka K, et al. Transurethral endoscopic treatment of upper urinary tract tumors using a holmium:YAG laser. Lasers Surg Med. 2003;32(5):336–40. doi: 10.1002/lsm.10184. [DOI] [PubMed] [Google Scholar]
- 53.Daneshmand S, Quek ML, Huffman JL. Endoscopic management of upper urinary tract transitional cell carcinoma: long-term experience. Cancer. 2003;98(1):55–60. doi: 10.1002/cncr.11446. [DOI] [PubMed] [Google Scholar]
- 54.Chen GL, Bagley DH. Ureteroscopic surgery for upper tract transitional-cell carcinoma: complications and management. J Endourol. 2001;15(4):399–404. doi: 10.1089/089277901300189420. discussion 409. [DOI] [PubMed] [Google Scholar]
- 55.Engelmyer EI, Belis JA. Long-term ureteroscopic management of low-grade transitional cell carcinoma of the upper urinary tract. Tech Urol. 1996;2(2):113–6. [PubMed] [Google Scholar]
- 56.Gaboardi F, et al. Conservative treatment of upper urinary tract tumors with Nd:YAG laser. J Endourol. 1994;8(1):37–41. doi: 10.1089/end.1994.8.37. [DOI] [PubMed] [Google Scholar]
- 57.Schmeller NT, Hofstetter AG. Laser treatment of ureteral tumors. J Urol. 1989;141(4):840–3. doi: 10.1016/s0022-5347(17)41027-5. [DOI] [PubMed] [Google Scholar]
- 58.Rastinehad AR, et al. A 20-year experience with percutaneous resection of upper tract transitional carcinoma: is there an oncologic benefit with adjuvant bacillus Calmette Guerin therapy? Urology. 2009;73(1):27–31. doi: 10.1016/j.urology.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 59.Palou J, et al. Percutaneous nephroscopic management of upper urinary tract transitional cell carcinoma: recurrence and long-term followup. J Urol. 2004;172(1):66–9. doi: 10.1097/01.ju.0000132128.79974.db. [DOI] [PubMed] [Google Scholar]
- 60.Motamedinia P, et al. The Expanded Use of Percutaneous Resection for Upper Tract Urothelial Carcinoma: A 30-Year Comprehensive Experience. J Endourol. 2015 doi: 10.1089/end.2015.0248. Published online: December 2, 2015. [DOI] [PubMed] [Google Scholar]
- 61.Roupret M, et al. Upper urinary tract transitional cell carcinoma: recurrence rate after percutaneous endoscopic resection. Eur Urol. 2007;51(3):709–13. doi: 10.1016/j.eururo.2006.07.019. discussion 714. [DOI] [PubMed] [Google Scholar]
- 62.Goel MC, Mahendra V, Roberts JG. Percutaneous management of renal pelvic urothelial tumors: long-term followup. J Urol. 2003;169(3):925–9. doi: 10.1097/01.ju.0000050242.68745.4d. discussion 929–30. [DOI] [PubMed] [Google Scholar]
- 63.Clark PE, Streem SB, Geisinger MA. 13-year experience with percutaneous management of upper tract transitional cell carcinoma. J Urol. 1999;161(3):772–5. discussion 775–6. [PubMed] [Google Scholar]
- 64.Patel A, et al. Long-term outcome after percutaneous treatment of transitional cell carcinoma of the renal pelvis. J Urol. 1996;155(3):868–74. [PubMed] [Google Scholar]
- 65.Plancke HR, Strijbos WE, Delaere KP. Percutaneous endoscopic treatment of urothelial tumours of the renal pelvis. Br J Urol. 1995;75(6):736–9. doi: 10.1111/j.1464-410x.1995.tb07382.x. [DOI] [PubMed] [Google Scholar]
- 66.Fuglsig S, Krarup T. Percutaneous nephroscopic resection of renal pelvic tumors. Scand J Urol Nephrol Suppl. 1995;172:15–7. [PubMed] [Google Scholar]
- 67.Tasca A, ZF, Garbeglio A, Villi G, Bassi P, Meneghini A. Endourologic treatment of transitional cell carcinoma of the upper urinary tract. J Endourol. 1992;6(3):253–6. [Google Scholar]
- 68.Johnson GB, Fraiman M, Grasso M. Broadening experience with the retrograde endoscopic management of upper urinary tract urothelial malignancies. BJU Int. 2005;95(Suppl 2):110–3. doi: 10.1111/j.1464-410x.2005.05210.x. [DOI] [PubMed] [Google Scholar]
- 69.Keeley FX, Jr, Bibbo M, Bagley DH. Ureteroscopic treatment and surveillance of upper urinary tract transitional cell carcinoma. J Urol. 1997;157(5):1560–5. [PubMed] [Google Scholar]
- 70.Aboumarzouk OM, et al. Mitomycin C instillation following ureterorenoscopic laser ablation of upper urinary tract carcinoma. Urol Ann. 2013;5(3):184–9. doi: 10.4103/0974-7796.115746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.O'Brien T, et al. Prevention of bladder tumours after nephroureterectomy for primary upper urinary tract urothelial carcinoma: a prospective, multicentre, randomised clinical trial of a single postoperative intravesical dose of mitomycin C (the ODMIT-C Trial) Eur Urol. 2011;60(4):703–10. doi: 10.1016/j.eururo.2011.05.064. [DOI] [PubMed] [Google Scholar]
- 72.Ito A, et al. Prospective randomized phase II trial of a single early intravesical instillation of pirarubicin (THP) in the prevention of bladder recurrence after nephroureterectomy for upper urinary tract urothelial carcinoma: the THP Monotherapy Study Group Trial. J Clin Oncol. 2013;31(11):1422–7. doi: 10.1200/JCO.2012.45.2128. [DOI] [PubMed] [Google Scholar]
- 73.Wagenheim GN, Papadopoulos J, Navai N, Davis JW, Karam JA, Kamat AM, Wood CG, Dinney CP, Matin SF. Mitomycin c induction and maintenance topical therapy for upper tract urothelial carcinoma. Presented at GU Symposium; San Francisco, CA. January 8, 2016. [Google Scholar]
- 74.Lifshitz D. Hydrogel based drug retention system for the treatment of upper tract urothelial carcinoma. Eur Urol Suppl, EAU. 2014;13:e26. [Google Scholar]
- 75.Goel MC, et al. Partial nephrectomy for renal urothelial tumors: clinical update. Urology. 2006;67(3):490–5. doi: 10.1016/j.urology.2005.09.016. [DOI] [PubMed] [Google Scholar]
- 76.Roupret M, et al. European guidelines on upper tract urothelial carcinomas: 2013 update. Eur Urol. 63(6):1059–71. doi: 10.1016/j.eururo.2013.03.032. [DOI] [PubMed] [Google Scholar]
- 77.Roupret M, et al. European Guidelines on Upper Tract Urothelial Carcinomas: 2013 Update. Eur Urol. 2013;63(6):1059–1071. doi: 10.1016/j.eururo.2013.03.032. [DOI] [PubMed] [Google Scholar]
- 78.Linton KD, et al. Disease specific mortality in patients with low risk bladder cancer and the impact of cystoscopic surveillance. J Urol. 2013;189(3):828–83. doi: 10.1016/j.juro.2012.09.084. [DOI] [PubMed] [Google Scholar]