Abstract
Numerous partner and relationship characteristics are associated with sexual risk behavior among young men who have sex with men (YMSM), including being in a serious relationship and having older partners. However, most research in this area is limited by its reliance on variable-centered approaches. Using multilevel latent class analysis, this study identified subgroups of sexual partner types with a particular emphasis on examining if partner type moderated the association between drug use and condomless anal sex (CAS). Data were utilized from an ongoing cohort study of YMSM (ages 16–29) recruited from previous studies as well as peers and serious partners of existing cohort members. A total of 469 participants reported on 1,596 sexual partners in the past 6 months. We identified four distinct sexual partner typologies, which we refer to as: Casual, Older-Online, Much Older, and Serious. Results indicated that rates of CAS were highest for Older-Online and Serious partners. Additionally, there was a positive association between drug use and CAS among a predominantly marijuana using sample, but only for serious partners. While previous research has found that CAS is highest in serious relationships, findings suggest that there may be another type of partnership in which CAS is likely to occur (older partners met online). If confirmed, these results suggest interventions focused on the intersection of marijuana use and CAS may be particularly important among YMSM with serious partners.
Keywords: men who have sex with men, partner, relationship, sexual risk behavior, drug use
INTRODUCTION
HIV disproportionately affects men who have sex with men (MSM). In 2014, MSM accounted for 66% of estimated new HIV infections in the United States and 82% of estimated new infections among all males (CDC, 2015a). Further, young MSM (YMSM) are one of the only demographic groups for which rates of new HIV infections are increasing in the US. From 2010 to 2014, new infections increased 10% among MSM ages 13–24 and 27% among MSM ages 25–34 compared to a decrease of 10% among MSM ages 35–44 (CDC, 2015c). These statistics underscore the importance of identifying risk factors for HIV infection in this high-risk population. Doing so is a necessary first step toward refining evidence-based prevention programs to target the primary factors that drive HIV infection.
Condomless anal sex (CAS) is a robust risk factor for HIV (Meng et al., 2015) and research has identified numerous psychosocial correlates of engaging in CAS (Lacefield, Negy, Schrader, & Kuhlman, 2015; Mustanski, Newcomb, Du Bois, Garcia, & Grov, 2011). In early research on HIV, casual sex was thought to be the riskiest context for HIV infection among YMSM (Mustanski & Parsons, 2014). However, recent estimates indicate that steady or main partner relationships account for 79–84% of new HIV infections among YMSM ages 18–29 (Beck, Birkett, Armbruster, & Mustanski, 2015; Sullivan, Salazar, Buchbinder, & Sanchez, 2009). Given this shift in what the field defines as a high risk partnership, it is critical to understand how partner and relationship characteristics influence CAS among YMSM. One explanation for the context of serious relationships is that YMSM are more likely to have CAS with serious partners than with casual partners (Birkett, Kuhns, Latkin, Muth, & Mustanski, 2015; Crepaz et al., 2000; Dudley, Rostosky, Korfhage, & Zimmerman, 2004; Hays, Kegeles, & Coates, 1997; Mustanski, Newcomb, Du Bois, et al., 2011; Newcomb & Mustanski, 2015; Newcomb, Ryan, Garofalo, & Mustanski, 2014; Prejean et al., 2011; Sullivan et al., 2009). Qualitative evidence suggests that YMSM have CAS with serious partners to express trust and intimacy, and they stop using condoms because they perceive their relationship to be monogamous and thus low risk (Greene, Andrews, Kuper, & Mustanski, 2014; Perez-Figueroa, Kapadia, Barton, Eddy, & Halkitis, 2015). However, many YMSM could unknowingly put their serious partners at risk given that 49% of HIV-positive YMSM ages 18–24 do not know their HIV status (CDC, 2015b).
In addition to serious partnerships, research has demonstrated that several other partner and relationship characteristics are associated with sexual risk behavior. For example, MSM are more likely to engage in CAS with casual partners with whom they are more familiar, including those they have met before, have had sex with before, “know well,” and trust (Prestage, Jin, Grulich, de Wit, & Zablotska, 2012; Rouwenhorst, Mallitt, & Prestage, 2012). Additionally, perceiving one’s own HIV status to be the same as one’s partner’s HIV status is also associated with increased CAS among MSM (Bingham et al., 2003; Joseph et al., 2011; Mustanski, Newcomb, & Clerkin, 2011; Newcomb & Mustanski, 2013, 2015) and YMSM (Matser et al., 2014; Newcomb et al., 2014). Together, these studies suggest that YMSM tend to engage in CAS with partners who are perceived as lower risk. There is also evidence that having older partners is associated with increased CAS among MSM (Garofalo, Herrick, Mustanski, & Donenberg, 2007; Liau, Millett, & Marks, 2006) and YMSM (Bingham et al., 2003; Joseph et al., 2011; Mustanski, Newcomb, & Clerkin, 2011; Newcomb & Mustanski, 2015), suggesting that relationship power dynamics may influence HIV risk behavior. Finally, although there is evidence that meeting partners online is associated with higher levels of sexual risk behavior among MSM (Liau et al., 2006) and YMSM (Garofalo et al., 2007), when looking across partners, MSM are actually more likely to engage in safer sex with partners met online (Mustanski, 2007).
While drug use has been extensively studied as a risk factor for CAS among MSM (Drumright, Patterson, & Strathdee, 2006; Mustanski, Newcomb, Du Bois, et al., 2011; Vosburgh, Mansergh, Sullivan, & Purcell, 2012) and YMSM (Birkett et al., 2015; Celentano et al., 2006; Parsons, Lelutiu-Weinberger, Botsko, & Golub, 2012; Yeo & Ng, 2016), there is evidence that this association may depend on the type of relationship. For example, some studies have found that substance use is associated with increased CAS with casual partners, but not with main partners, among MSM (Starks, Millar, & Parsons, 2015; Vanable et al., 2004). Other studies have shown that the relationship between substance use and CAS across different partner types depends on the type of substances being used. For example, one study (Newcomb & Mustanski, 2014) found a stronger association between alcohol use before sex and sexual risk behavior among serious partners among YMSM. Similarly, another study found that only specific drugs acted as risk factors for CAS among YMSM and that the effect for each drug varied across partner types (Rusch, Lampinen, Schilder, & Hogg, 2004). For example, use of gamma-hydroxybutyrate (GHB) was only significantly associated with sexual risk behavior among regular partners, while ecstasy use was only associated with sexual risk behavior among casual partners.
While accumulating evidence supports the roles of specific partner and relationship characteristics in sexual risk behaviors, these characteristics do not function in isolation. For instance, while being in a serious relationship is associated with increased likelihood of CAS, this association is confounded by other relationship factors, such as relationship length and trust. Most research in this area is limited by its reliance on variable-centered approaches, which focus on the associations among individual variables. In contrast, person-centered approaches (e.g., latent class analysis [LCA]) can be used to simultaneously consider multiple variables in order to identify subgroups of individuals based on patterns of characteristics (Muthen & Muthen, 2000). As such, person-centered approaches may be better suited to capturing the multidimensional nature of sexual partnerships and the consequences of patterns of partner and relationship characteristics. In fact, it has been suggested that person-centered approaches may better illustrate the complexities of romantic relationships compared to variable-centered approaches (Moosmann & Roosa, 2015).
Several studies have utilized person-centered approaches to characterize profiles of sexual behavior in samples of mostly heterosexual adolescents (Beadnell et al., 2005; Haydon, Herring, Prinstein, & Halpern, 2012; Hipwell, Stepp, Keenan, Chung, & Loeber, 2011). For instance, Vasilenko, Kugler, Butera, and Lanza (2015) identified latent classes of adolescents with particular profiles of sexual behavior measured by timing of oral and vaginal sex, condom use, number of sexual partners, and non-relationship partners. They identified five distinct classes of sexual behavior, finding that adolescents who reported any same-sex attraction were generally more likely to be in the riskier classes, which in turn were associated with increased sexually transmitted infection (STI) rates. These findings illustrate the usefulness of a person-centered approach in characterizing sexual behavior across various indicators and the ability of class membership to predict sexual health outcomes.
Finally, sexual health research typically assesses sexual behavior and partner characteristics for a single partnership (e.g., most recent sexual partner) or for general tendencies across partnerships (Mustanski, Starks, & Newcomb, 2014). While these approaches can inform our understanding of between-person differences in sexual risk behavior, they do not account for the fact that there is within-person variation in condom use across sexual partnerships (Cooper, 2010; Grov, Golub, Mustanski, & Parsons, 2010; Mustanski, Newcomb, & Clerkin, 2011). An alternative approach is to assess sexual behavior and partner characteristics for multiple partners (e.g., three most recent sexual partners or all sexual partners in the prior 6 months). This approach allows each individual to serve as their own control by comparing the same individual’s behavior across multiple relationships, thereby providing information about how an individual’s involvement in different types of sexual partnerships relates to their sexual risk behavior.
To address the reliance on variable-centered approaches in previous research, the current study utilized multilevel LCA to examine if distinct sexual partner typologies could be identified using multiple partner and relationship characteristics. In addition to the aforementioned benefits of LCA, multilevel LCA has the additional benefit of controlling for individual variation by examining data across multiple sexual partnerships. The specific goals of the current study were to: 1) examine if distinct sexual partner typologies could be identified using partner and relationship characteristics; 2) examine if the association between drug use and CAS varied across these typologies in a sample of predominately marijuana users; and 3) examine if individual characteristics were associated with the likelihood of reporting different sexual partner typologies.
METHODS
All data for this analysis came from the RADAR study. RADAR is a longitudinal cohort study aimed at identifying and understanding the multilevel connections among STIs, drug and alcohol use, and romantic and sexual relationship patterns over time among YMSM. Participants were asked to complete an initial baseline assessment with subsequent visits occurring every six months until the study ends. All data in the current analysis come from the first (baseline) interview.
Participants
To be enrolled in the RADAR cohort, all participants met the following criteria: they were between 16 and 29 years of age, born male, English-speaking, and had a sexual encounter with a man in the previous year or identified as gay or bisexual. Participants were recruited in three ways: 1) involvement in a cohort of YMSM and/or LGBT youth (Project Q2 (Mustanski, Garofalo, & Emerson, 2010), Crew 450 (Mustanski, Johnson, Garofalo, Ryan, & Birkett, 2013), and a new 2015 cohort) all of which enrolled individuals when they were 16–20 years of age; 2) through being a serious partner of an existing RADAR cohort member (i.e., being in a current serious relationship with a RADAR cohort member); or 3) through peer recruitment by an existing RADAR cohort member. Details about the previous cohorts can be found elsewhere (Mustanski et al., 2010; Mustanski et al., 2013), while the new 2015 cohort was recruited using venue-based, peer-referral, and online recruitment. Although all serious partners were eligible for a one-time interview visit, they were required to meet the criteria listed above to be enrolled in the cohort. Similarly, peer recruits were required to meet the same criteria except that age was restricted to 16–20 years of age. Age was restricted for peer recruits to match the recruitment design of the previous cohorts (i.e., Project Q2 and Crew 450), which at the time of the current study also had older participants (i.e., ages 20–29) and the overall RADAR sample needed to represent a full range of ages to achieve the multiple cohort, accelerated longitudinal design (Miyazaki & Raudenbush, 2000). To date, 540 participants have been enrolled in the cohort and completed the baseline network interview. Of these 540 cohort members, 469 named at least one sexual partner in the previous six months and were used in the current analysis. Data on a total of 1,596 partners were provided by these 469 participants.
Procedure
At each visit, participants completed a network interview, a self-report psychosocial survey, and biomedical specimen collection for testing (HIV, STI, and/or drug screening) and banking. The current analysis primarily uses data from the network interview, with some supplementary variables (e.g., demographics) from the psychosocial survey. An interviewer-assisted, touchscreen network interview (netCanvas-R) was used to elicit data about the social, drug, and sexual connections of the participant. Details on this network interview are discussed elsewhere (Hogan et al., 2016). In brief, the tool is structured so that social, drug, and sexual network members are first named by the study participant, and then the relationship role(s) of the individuals are identified. Next, important attributes of these individuals (e.g., age, race, HIV status) are captured, along with attributes of the connections between the participant and network members (e.g., estimated dates of first and most recent sex and sexual risk behavior). At each visit participants were compensated $50 for their time, and all study activities were approved by the Northwestern University Institutional Review Board. Data collection began in February 2015; this study utilizes data collected through mid-January 2016.
Measures
The following measures were used to capture information regarding sexual partners during the six months prior to the baseline interview.
Within-Person Variables
Variables at the within-person level represent characteristics and behaviors unique to each participant-partner dyad that vary within individuals across different partners. These variables include: partnership role, partnership length, whether they met online, CAS, perceived HIV concordance, age difference, relationship closeness, and drug use with that partner.
Partnership Role
When naming network members in the interview, participants are prompted with “roles” to select for each network member. These roles have been pre-populated from those that were identified as important by YMSM in a previous study (Kuhns et al., 2015). Participants can select multiple roles for each network member, and five roles are designated for romantic or sexual partners, including: “Boyfriend/Girlfriend”, “Ex-Boyfriend/Ex-Girlfriend”, “Booty Call/Fuck Buddy/Hook-Up”, “One Night Stand”, and “Other type of partner.” For the purpose of analysis, we created three mutually exclusive groups. The first group consisted of any partner that was designated as a current or former boyfriend/girlfriend, regardless of other potential roles selected. Current and former boyfriends/girlfriends were combined into a single group as it was impossible to ascertain the relationship status of former boyfriends/girlfriends at the time of the reported sexual behavior. The second group consisted of those identified as booty calls, fuck buddies, or hook-ups (hereafter referred to as hook-ups), but not as a current/former boyfriend/girlfriend. The third group consisted of those identified as one night stands or other sexual partners, but not as a current/former boyfriend/girlfriend or a hook-up. The third group also consisted of individuals who were not initially identified in a sexual relationship role, but were later designated as a sexual partner when asked to indicate all sexual partners in the last six months regardless of their previously identified role. For example, these could include someone only designated as a “Friend” in the role selection who also happened to be a sexual partner in the last six months.
Met Online
During the network interview, participants identified the category of location where they met each partner (i.e., Online/Mobile App: 52.2%, Bar: 6.8%, Work/School: 16.8%, or Somewhere else: 24.1%). This variable was dichotomized as either meeting the partner online/via mobile app or elsewhere given that this comparison has been the focus of much previous work and the difficulty computing estimates for variables with relatively small counts (e.g., partners met at a bar).
Partnership Length
Participants identified the first and last date they had sex with each sexual partner. However, exact date information is not obtained for partners whose first sexual encounter was earlier than six months prior to the interview. Accordingly, the following categories were created for partnership length: partners with the same first and last sex date (i.e., one-time sexual encounters); 2) those with partnership lengths between 1 day and less than six months; and 3) those with partnership lengths greater than or equal to six months.
Condomless Anal Sex (CAS)
CAS was measured by examining the number of insertive and receptive CAS acts the participant reported with each partner. Given that condoms were either used always or never in a large majority (i.e., 88.9%) of partnerships, this variable was dichotomized to indicate if the participant had ever engaged in CAS with each partner.
Perceived HIV Concordance
HIV concordance was based on the participant’s perception of their own HIV status and that of each partner. This variable was coded as: 1) concordant, if they perceived themselves and their partner to be the same HIV serostatus (either negative or positive); 2) discordant, if they perceived differing serostatuses; and 3) unknown, if either they were unsure of their own or their partner’s HIV status.
Drug Use
Participants were asked to identify any network member they used “marijuana or other drugs” within the past six months and were instructed by the interviewer that this included “marijuana or other drugs such as poppers or ecstasy.” The participant later indicated which drug they used in the last six months from a list of the following dugs: Marijuana, Cocaine or Crack, Heroin, Methamphetamines, Painkillers or Opiates, Poppers, Stimulants or Amphetamines (not prescribed), Depressants or Tranquilizers (not prescribed), Ecstasy, or ‘some other drug.’ For each of the types of drugs used in the prior six months, participants then indicated the frequency of use with each partner. Of 375 partners who used drugs with a participant, marijuana was the most frequently shared drug (80.3%) with only a small number of partners who either did not specify the drug used (10.7%) or who exclusively used drugs other than marijuana (9.1%). Of those who exclusively used drugs other than marijuana, poppers were the most frequently used drug (70.5%), while the other drugs used were roughly equally split with a smaller percentage of partners (i.e., ~17–20%) using each cocaine, methamphetamines, amphetamines, and ecstasy. Drug use was coded dichotomously for analysis (i.e., used drugs in the past six months with this partner or did not use drugs in the past six months with this partner).
Age Difference
Age difference was calculated by subtracting the age of the partner from the age of the participant so that positive values indicated partners that were older than the participant, while negative values indicated the partner was younger than the participant.
Relationship closeness
Relationship closeness was measured on a three-point ordinal scale from 0 to 2 (0 = not close at all, 2 = very close).
Between-Person Variables
Variables at the between-person level represent individual-level variables, such as demographics of the participant and the total number of sexual partners. Variables used in the current analysis are: race/ethnicity, age, and number of sexual partners, and HIV status of the participant. Race/ethnicity was coded as: White, non-Hispanic; Black, non-Hispanic; Hispanic; and Other. Number of sexual partners represents the participant’s total number of sexual partners in the previous six months. Finally, known HIV positive status indicated if the participant had been tested prior to the interview and knew that they were HIV positive.
Latent Class Analysis
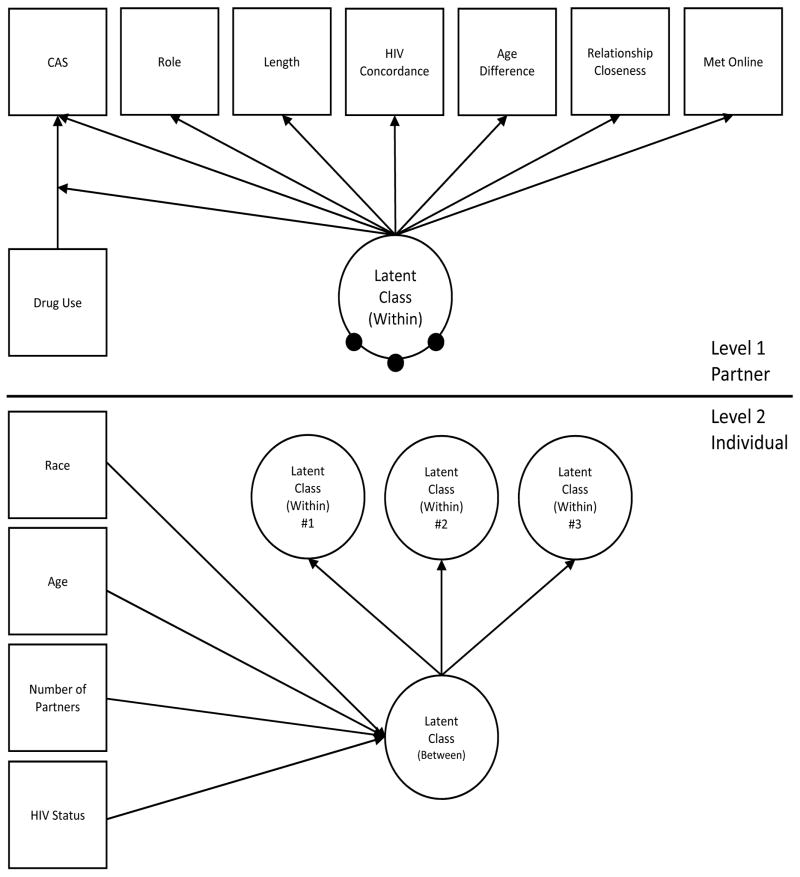
Multilevel latent class analysis was used to examine typologies of sexual partners among YMSM. In the current analysis, this involves attempting to classify partners into categorical groups based on the participant’s report of each partner’s characteristics, the characteristics of the relationship between the participant and the partner, and the difference/similarity between the participant’s and the partner’s characteristics. Given that participants were instructed to report all sexual partners during the last six months, multiple partners could be reported by the same participant. Multilevel latent class analysis controls for the repeated observations (i.e., multiple partners) within each participant. The lower level latent class (i.e., level 1 – partner) models distinct clusters of partner typologies, while the higher level model (i.e., level 2 – participant) models the variability in likelihood that participants will have partners of specific typologies. More specifically (see Figure 1), a non-parametric approach (Henry & Muthen, 2010) was taken with the means of the within-level latent class being modeled by a between-person latent class. This approach is non-parametric because variability in the lower level latent classes are modeled through a higher level discrete latent variable (i.e., latent class) instead of a traditional continuous random-effect (Vermunt, 2008). Therefore, latent classes at the within level are not assumed to be random latent variables at the between level, but instead are modeled as discrete means, with m – 1 (where m equals the number of level 1 classes) means modeled at the between level, and one latent class serving as the reference group. This approach also allows for the variability of the likelihood of partner types (i.e., level 1 latent classes) to be associated with level 2 characteristics. Significant differences across latent class indicators were examined using a Wald χ2 test. Furthermore, drug use (in the past six months) with the partner was also used as a covariate of CAS to examine if this association differed across partner typologies (see Figure 1). At level 1, drug use was the sole covariate of the latent classes. At level 2, the likelihood for the within level classes had three covariates: race/ethnicity, age, and number of sexual partners. All analyses were performed using Mplus 7.3 (Muthén & Muthén, 1998–2011).
Figure 1.
Theoretical Path Model for 4-Class Model
Note. Random intercepts for level-1 latent class categories are modeled as latent variables at Level 2 with Latent Class 4 as the reference category.
Number of Level 1 Classes
Determining the number of latent classes is a vital step to any latent class analysis. Ideally, the smallest number of classes that adequately fits the data is selected (Muthen & Muthen, 2000). For the current analysis, we used the Akaike’s information criterion (AIC) (Bozdogan, 1987), Bayesian information criteria (BIC) (Nylund, Asparoutiov, & Muthen, 2007), and entropy (Celeux & Soromenho, 1996) to select the best-fitting number of within-level classes with attention to previous research and theory regarding partner types among YMSM. BIC and AIC are two log-likelihood based statistical information criteria fit indices that allow the comparison of fit across different models with lower values indicating better fit. Entropy represents the degree of separation between classes and ranges from 0 to 1, with higher values indicating better separation (distinct latent classes) and lower values representing less separation between classes.
RESULTS
Descriptive Statistics
Descriptive statistics at the participant- and partner-level are displayed in Table 1. As indicated, there were slightly fewer current/former boyfriends/girlfriends (28.4%) compared to hook-ups (35.2%) or other partner roles (36.5%). Partnership length was more frequently one time only (35.9%) or six months or more (35.9%) relative to less than six months (27.6%). Most partnerships were perceived to have the same (57.7%) or unknown (34.5%) HIV status. Finally, a substantial minority of participants engaged in CAS (34.5%) or drug use (23.5%) with partners.
Table 1.
Descriptive Statistics on Partner and Participant Characteristics
| n (%) | M (SD) | |
|---|---|---|
| Level 1 - Partner (n = 1596) | ||
| Partnership Role | ||
| Current/Former Boyfriend/Girlfriend | 453 (28.4) | |
| Hook-up | 561 (35.2) | |
| Other | 582 (36.5) | |
| Met Online/Mobile App | 833 (52.2) | |
| Partnership Length | ||
| One time only | 573 (35.9) | |
| Less than six months | 440 (27.6) | |
| Six months or more | 573 (35.9) | |
| CAS | 551 (34.5) | |
| Perceived HIV Seroconcordance | ||
| Unknown | 550 (34.5) | |
| Concordant | 921 (57.7) | |
| Discordant | 122 (7.6) | |
| Drug Use with Partner | 375 (23.5) | |
| Age Difference (years) | 3.4 (6.9) | |
| Relationship Closeness | 1.0 (0.9) | |
| Level 2 - Participant (n = 469) | ||
| Race/ethnicity | ||
| Black | 162 (34.5) | |
| White | 99 (21.1) | |
| Hispanic | 152 (32.4) | |
| Other | 55 (11.7) | |
| Age (years) | 21.5 (3.1) | |
| Number of Partners | 3.4 (3.3) | |
| Known HIV Positive | 62 (13.2) | |
Note. Partnership role “Other” indicates either “one night stand” or “other partner”. Closeness scale was from 0 = Not Close At All, 2 = Very Close.
Number of Classes
Table 2 displays the model fit statistics for models with 1 through 5 level-1 latent classes. While the 5-class solution had the best model fit for the AIC and BIC, the 4-class solution had the most distinct latent classes as indicated by entropy. In addition, the 5-class solution could not replicate the best log-likelihood even after substantial increases in the number of random starts, suggesting that the model was likely too complex for the current data. Accordingly, we chose the 4-class model for all subsequent analysis.
Table 2.
Model Fit Statistics
| Number of Classes | Log-likelihood (# of parameters) | AIC | BIC | Entropy |
|---|---|---|---|---|
| 1 | −17465.543 (25) | 34981.09 | 35115.47 | |
| 2 | −13456.058 (31) | 26974.12 | 27140.75 | 0.836 |
| 3 | −13214.354 (49) | 26526.71 | 26790.10 | 0.858 |
| 4 | −13082.850 (67) | 26299.70 | 26659.84 | 0.864 |
| 5 | −12990.674 (85) | 26151.35 | 26608.25 | 0.799 |
Latent Classes
Table 3 displays estimated probability and means for each indicator variable across the four classes for all variables and, as indicated, all variables significantly varied across classes. Using these results, we characterized the four classes as follows: Casual (Class 1: 54.7%), Older-Online (Class 2: 11.4%), Much Older (Class 3: 2.7%), and Serious (Class 4: 31.1%). Casual partners tended to be identified as hook-ups (0.40 probability) or “other” partner types (0.48); many were met online (0.57), were only slightly older than the participant (mean age difference = 1.66 years), and had low rates of CAS (0.21) relative to other latent classes. Older-online partners were most likely to be identified as hook-ups (0.61), have met online (0.81), and engaged in CAS (0.54). Older-online partners were also estimated to be 13.00 years older than the participant. Much older partners were characterized by an even larger estimated age difference of 28.50 years older than the participant. Much older partners were also unlikely to be one-time partners (0.33), tended to be identified in an “other” partner role (0.43) and had lower CAS (0.30) relative to other classes. Finally, serious partners were most likely to be identified as a current/former boyfriend/girlfriend (0.66), least likely to have been met online (0.33), tended to have been partners for at least 6 months (0.63), and engaged in relatively higher levels of CAS (0.51).
Table 3.
Estimated Probability and Means of Latent Class Indicators
| Variable | Casual (55.2%) | Older-Online (11.0%) | Much Older (2.6%) | Serious (31.1%) | Wald χ2 | p-value |
|---|---|---|---|---|---|---|
| Partnership Role | ||||||
| Current/Former Boyfriend/Girlfriend | 0.12 | 0.05 | 0.18 | 0.66 | ||
| Hook-up | 0.40 | 0.61 | 0.29 | 0.18 | ||
| Other | 0.48 | 0.34 | 0.54 | 0.16 | 228.24 | < 0.001 |
| Met Online/Mobile app | 0.57 | 0.81 | 0.54 | 0.33 | 64.39 | < 0.001 |
| Partnership Length | ||||||
| One time | 0.53 | 0.37 | 0.33 | 0.07 | ||
| Less than six months | 0.24 | 0.37 | 0.44 | 0.30 | ||
| Six months or more | 0.23 | 0.26 | 0.23 | 0.63 | 182.87 | < 0.001 |
| CAS | 0.21 | 0.55 | 0.31 | 0.50 | 23.48 | < 0.001 |
| Perceived HIV Seroconcordance | ||||||
| Unknown | 0.43 | 0.29 | 0.41 | 0.22 | ||
| Concordant | 0.53 | 0.56 | 0.47 | 0.68 | ||
| Discordant | 0.05 | 0.14 | 0.12 | 0.10 | 29.18 | < 0.001 |
| Age Difference | 1.67 | 12.97 | 28.71 | 0.82 | 107.75 | < 0.001 |
| Relationship Closeness | 0.24 | 0.35 | 0.67 | 1.66 | 1380.51 | < 0.001 |
Note. Estimated mean scores reported for continuous variables.
Moderation of Drug Use and CAS
There was no significant association between drug use with a partner and engaging in CAS with that partner in the past six months for casual partners (odds ratio [OR] = 1.09; 95% Confidence Interval [CI]: 0.55, 2.18; p = 0.803), older-online partners (OR = 0.80; 95% CI: 0.22, 2.92; p = 0.740), or much older partners (OR = 2.60; 95% CI: 0.34, 19.88; p = 0.356). However, among serious partners, there was a significant positive association between drug use and CAS (OR = 1.83; 95% CI: 1.20, 2.80; p = 0.005), indicating that participants were more likely to have engaged in CAS with serious partners if they also used drugs with them in the past six months.
Class Membership Covariates
Both Level 1 and Level 2 covariates were used to predict the likelihood of reporting partners in each latent class with serious partners serving as the reference category (Table 4). For the sole partner level covariate (drug use), results indicated that drug use was less common among casual (OR = 0.12; 95% CI: 0.08, 0.18 p < 0.001), older-online (OR = 0.19; 95% CI: 0.09, 0.39; p < 0.001), and much older (OR = 0.14; 95% CI: 0.05, 0.45; p = 0.001) partners, relative to serious partners.
Table 4.
Level 2 Covariates of Partner Typologies
| Class | Variable | OR [95% CI] | p-value |
|---|---|---|---|
| Casual | |||
| Race/ethnicity | |||
| African-American (Ref) | - | - | |
| White | 1.30 [0.83, 2.05] | 0.247 | |
| Hispanic | 1.23 [0.80, 1.90] | 0.337 | |
| Other | 1.96 [1.16, 3.32] | 0.013 | |
| Age | 0.93 [0.88, 0.98] | 0.010 | |
| Number of Sexual Partners | 1.18 [1.12, 1.24] | < 0.001 | |
| Known HIV Positive | 1.33 [0.74, 2.39] | 0.343 | |
| Older-Online | |||
| Race/ethnicity | |||
| African-American (Ref) | - | - | |
| White | 1.68 [0.41, 6.95] | 0.475 | |
| Hispanic | 1.66 [0.54, 5.04] | 0.374 | |
| Other | 4.03 [0.87, 18.70] | 0.075 | |
| Age | 0.89 [0.77, 1.02] | 0.103 | |
| Number of Sexual Partners | 1.39 [1.23, 1.58] | < 0.001 | |
| Known HIV Positive | 2.74 [0.71, 10.63] | 0.144 | |
| Much Older | |||
| Race/ethnicity | |||
| African-American (Ref) | - | - | |
| White | 1.83 [0.54, 6.23] | 0.331 | |
| Hispanic | 1.09 [0.22, 5.38] | 0.919 | |
| Other | 0.63 [0.09, 4.47] | 0.645 | |
| Age | 0.95 [0.86, 1.05] | 0.304 | |
| Number of Sexual Partners | 1.18 [1.07, 1.30] | 0.001 | |
| Known HIV Positive | 3.65 [1.06, 12.60] | 0.040 | |
Note. Reference group for analysis is “Serious”
For participant level covariates, results indicated age was inversely related to Class 1 (OR = 0.94; 95% CI: 0.89, 0.99; p = 0.044), indicating that older participants were less likely to have casual partners relative to serious partners. Further, “other” race/ethnicity was positively associated with Class 1 (OR = 1.82; 95% CI: 1.03, 3.20; p = 0.038), indicating that participants who identified as “other” race/ethnicity were more likely to have casual partners compared to Black participants. Participants with a larger number of sexual partners were more likely to have casual partners (OR = 1.17; 95% CI: 1.12, 1.22; p < 0.001), older-online partners (OR = 1.38; 95% CI: 1.23, 1.54; p < 0.001), and much older partners (OR = 1.16; 95% CI: 1.06, 1.27; p = 0.001), relative to serious partners. Finally, participants that knew they were HIV positive were significantly more likely to have much older partners (OR = 3.71; 95% CI: 1.24, 11.12; p = 0.019) relative to serious partners.
DISCUSSION
Given the growing burden of HIV among YMSM in the US, prevention strategies must be optimized to reduce the spread of HIV in this population. This study assessed sexual partner typologies across a range of partner and relationship characteristics and behaviors. In addition to identifying distinct partner typologies, we found that these typologies were associated with CAS and moderated the association between drug use and CAS among a predominantly marijuana using sample. Importantly, of the four partner typologies identified (Casual, Older-Online, Much Older, and Serious), we found that CAS was highest among older-online and serious partners. Our finding that CAS was high among serious partners is consistent with several previous studies that have found that MSM engage in sexual risk behavior at much higher rates with serious partners compared to casual partners (Dudley et al., 2004; Newcomb & Mustanski, 2015; Newcomb et al., 2014; Sullivan et al., 2009). This may be due to higher intimacy and trust with romantic partners and lower perceived risk among romantic partners, which may lead to elevated levels of risk behavior with these partners (Greene et al., 2014; Karney et al., 2010).
However, we also found that older-online partners reported similar rates of CAS as serious partners. As noted, previous studies found having older partners (Bingham et al., 2003; Joseph et al., 2011) or larger age differences between partners among YMSM (Mustanski, Newcomb, & Clerkin, 2011) was associated with higher rates of sexual risk behavior. Other research that examined the impact of meeting sexual partners online found mixed results. For example, while a meta-analysis found that MSM who seek sexual partners online reported higher rates of sexual risk behavior (Liau et al., 2006), more nuanced analysis suggests that individuals who report higher risk behavior may be more likely to utilize the internet to seek sexual partners, but also more likely to use condoms with partners met online (Grov, Breslow, Newcomb, Rosenberger, & Bauermeister, 2014; Mustanski, 2007). Our findings concur with a more nuanced interpretation of the association between meeting sexual partners online and likelihood of CAS. For example, while older-online partners reported the highest likelihood of CAS, the two other partner types that were also likely to have met online (i.e., much older and casual) displayed the lowest levels of CAS. Although speculative, it is possible that meeting older partners online creates a relationship power dynamic in which the older partner has a particularly strong influence on condom use decision making due to his age and unfamiliarity. While meeting in-person may provide a level of interpersonal comfort to assert oneself during sex with an older partner, meeting online may contribute to being passive with older partners. Thus, our findings suggest that simultaneous consideration of how these characteristics are associated with risk for CAS may be beneficial compared to examining either factor in isolation.
It is also possible that the older sexual partners who were predominantly met online also served roles that were not directly measured in the analysis. For example, previous work suggests that African American YMSM may seek older partners due to restricted access to or un-welcomeness in LGBTQ venues, and these partners may serve as a “broker” to that community (Arrington-Sanders, Leonard, Brooks, Celentano, & Ellen, 2013; Mustanski & Newcomb, 2013). While race/ethnicity was not associated with the likelihood of having an older-online partner, older-online partners in the current sample could play a similar bridging role to provide unique resources and connection. Alternatively, partners in this class could be exchange partners (i.e., partners involved with trading sex for money or drugs), a possibility that cannot be examined in the current dataset but merits further investigation. Nonetheless, given the elevated rates of CAS reported with these partners, older-online partners represent an important and potentially overlooked partner type for targeting interventions. However, the results of the current study suggest that merely targeting age-discordant relationships alone may be imprecise given that the partner type with the largest age discrepancy (i.e., much older partners) showed lower levels of CAS relative to the other partner types. Accordingly, future studies and interventions should further explore this intersection of age discrepancy and how YMSM meet their sexual partners.
Controlling for differential rates of drug use across partner types, we also found that drug use with a sexual partner was associated with CAS, but only for serious partners. This suggests that YMSM are more likely to engage in CAS with serious partners with whom they have used drugs (i.e., mostly marijuana use) compared to serious partners with whom they have not used drugs, and this association is not present within other partner types. While this is consistent with two previous studies (Newcomb & Mustanski, 2014; Rusch et al., 2004), other studies have found individuals using drugs reporting increased risk with casual partners but not regular partners (Starks et al., 2015; Vanable et al., 2004). However, important differences between the current study and previous research such as the focus on YMSM, the predominance of marijuana use, and not examining event specific associations, limit the inference that can be drawn by this finding. Given the inconsistencies across prior studies, future research should explore if sample characteristics (e.g., age of sample, types of substances, definitions of relationships) may explain why some studies find greater risks of drug use in serious or casual relationships. If our findings are confirmed, it suggests that HIV prevention interventions among YMSM might benefit from a greater focus on these serious long-term partnerships and other related factors (e.g., trust, intimacy, drug use) that may lead to greater levels of CAS among these partners. This finding also suggests that interventions specifically targeting drug use as a risk factor may yield greater benefit to those with serious partners relative to individuals with other partner types. While couple-based HIV prevention programs have been developed and tested for heterosexuals, similar dyadic interventions for MSM are scarce (for reviews, see Burton, Darbes, & Operario, 2010; Jiwatram-Negron & El-Bassel, 2014). In an exception, Wu et al. (2011) tested a couple-based HIV/STI prevention program for methamphetamine-using Black MSM, finding that the intervention reduced sexual risk behavior and drug use from pre- to post-test. The success of this intervention provides preliminary support for the possibility of reducing drug use and sexual risk behavior using a dyadic approach.
Finally, there were several individual characteristics that were associated with sexual partner typologies. Younger MSM were more likely to have casual partners than serious partners. Participants who reported more sexual partners were also less likely to have serious partners relative to all other partner types. Given that serious partners were one of the typologies associated with increased CAS, YMSM who report fewer sexual partners can be considered high-risk if their partners are of a particular type (i.e., serious). This suggests that there are multiple pathways to risk, such as having more sexual partners or having fewer serious sexual partners. Finally, MSM who identified their race/ethnicity as “other” were more likely to have casual partners compared to those who identified as Black. However, no other significant differences in partner types were found across different race/ethnicity groups. Importantly, participants that knew they were HIV-positive were more likely to have much older partners. While it is unclear why HIV-positive YMSM are more likely to have these partners, it does not appear that these partners were selected for their HIV seroconcordance given that the pattern of concordance among much older partner is close to those of other partner types. Despite these uncertainties, given that known HIV-positive participants were more likely to have these partners, this partner category certainly warrants attention in future studies. In addition, research is needed to explore additional individual-level correlates, as they will provide information regarding the scope of targeting interventions such as exploring whether partner types are relatively evenly distributed across YMSM or if there are certain individuals that are most likely to have partners with the highest level of risk behavior (e.g., older-online).
Limitations
There are several limitations to consider when interpreting the current findings. First, due to advances in biomedical prevention strategies for HIV (i.e., pre-exposure prophylaxis [PrEP] and antiretroviral treatment as prevention), CAS is an increasingly less precise indicator of HIV transmission risk, as it may not accurately reflect true seroconversion risk. For example, some individuals may be engaging in risk reduction strategies such as “biomed-matching,” which involves making calculated decisions about condom use based on one’s own and one’s partner’s use of biomedical prevention (Newcomb, Mongrella, Weis, McMillen, & Mustanski, 2016). Biomedical prevention was not included in the current analyses given that perceived PrEP status was only available for a subset of all sexual partners. However, it will be important for future studies to consider how it may impact partner typologies and associated sexual risk behavior. Second, the association between drug use and CAS was not assessed at the level of specific drugs (e.g., marijuana versus poppers) given the small number of individuals who only used drugs other than marijuana with their partners. Accordingly, these results may be limited to marijuana use given that previous research (Heath, Lanoye, & Maisto, 2012) suggests the specific type of drug likely impacts the association between that drug and risk behavior. Furthermore, sexual risk behavior and drug use were not measured at the event-level, so we were unable to link drug use with partners to specific sexual encounters with those partners. Fourth, although our latent classes were based on numerous partner and relationship characteristics, it is likely that there are additional individual and partner/relationship characteristics that influence sexual risk behavior and drug use. Fifth, we utilized a large, but not representative, sample of YMSM, so it remains unclear to what extent findings generalize to the broader population of YMSM. Accordingly, the results are not intended to generalize to all YMSM. Sixth, LCA is an inductive and exploratory approach to modeling categorical latent variables. As such, future research may benefit from utilizing confirmatory approaches to LCA (Finch & Bronk, 2011) to examine if these categories are consistent across other samples of YMSM. Seventh, given that a small number of participants (i.e., 10.9%) were recruited into the study through their serious partners, the data likely contain some un-modeled dependency across participants (i.e., participants reporting sex with other participants) which could underestimate the standard errors. However, given the complexity of modeling this dependency for a small subset of participants, we could not account for it in the current analysis. Finally, as with all studies, not all relevant variables could be included in the current analysis. In particular, research has implicated a mental health and other psychological correlates of CAS that may have important impact on the spread of HIV among MSM (Lacefield et al., 2015).
Conclusions
Despite limitations, the current study demonstrated the utility of simultaneously considering multiple partner and relationship characteristics as a way to identify distinct sexual partner typologies. These typologies have important implications for sexual risk behavior, as we found evidence that CAS was highest with serious partners and older partners who were met online, and that drug use was only a risk factor for CAS with serious partners among individuals who mostly used marijuana. Additional research using similar statistical approaches has the potential to better capture the multidimensional nature of sexual partnerships, in turn providing a more complete understanding of what puts YMSM at risk for HIV.
Acknowledgments
Funding: This work was supported by the National Institute on Drug Abuse of the National Institutes of Health (U01DA036939, PI: Mustanski; K08DA037825, PI: Birkett)
Footnotes
Compliance with Ethical Standards
Conflict of Interest: Patrick Janulis has no conflict of interest to declare. Brian A. Feinstein has no conflict of interest to declare. Gregory Phillips II has no conflict of interest to declare. Michael E. Newcomb has no conflict of interest to declare. Michelle Birkett has no conflict of interest to declare. Brian Mustanski has no conflict of interest to declare.
Ethical approval: All procedures performed in this study were in accordance with the ethical standards and approved by our institutional review board.
Informed consent: Informed consent for participants 18 years or older and informed assent for participants ages 16–17 years old was obtained from all individuals included in the study. A waiver of parental consent was obtained from the institutional review board for participants 16 to 17 years old.
References
- Arrington-Sanders R, Leonard L, Brooks D, Celentano D, Ellen J. Older partner selection in young african-american men who have sex with men. Journal of Adolescent Health. 2013;52(6):682–688. doi: 10.1016/j.jadohealth.2012.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beadnell B, Morrison DM, Wilsdon A, Wells EA, Murowchick E, Hoppe M, … Nahom D. Condom use, frequency of sex, and number of partners: Multidimensional characterization of adolescent sexual risk-taking. Journal of Sex Research. 2005;42(3):192–202. doi: 10.1080/00224490509552274. [DOI] [PubMed] [Google Scholar]
- Beck EC, Birkett M, Armbruster B, Mustanski B. A data-driven simulation of hiv spread among young men who have sex with men: Role of age and race mixing and stis. Journal of Acquired Immune Deficiency Syndromes. 2015;70(2):186–194. doi: 10.1097/QAI.0000000000000733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bingham TA, Harawa NT, Johnson DF, Secura GM, MacKellar DA, Valleroy LA. The effect of partner characteristics on hiv infection among african american men who have sex with men in the young men’s survey, los angeles, 1999–2000. AIDS Education and Prevention. 2003;15(1 Suppl A):39–52. doi: 10.1521/aeap.15.1.5.39.23613. [DOI] [PubMed] [Google Scholar]
- Birkett M, Kuhns LM, Latkin C, Muth S, Mustanski B. The sexual networks of racially diverse young men who have sex with men. Archives of Sexual Behavior. 2015;44(7):1787–1797. doi: 10.1007/s10508-015-0485-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bozdogan H. Model selection and akaike information criterion (aic) - the general-theory and its analytical extensions. Psychometrika. 1987;52(3):345–370. doi: 10.1007/Bf02294361. [DOI] [Google Scholar]
- Burton J, Darbes LA, Operario D. Couples-focused behavioral interventions for prevention of hiv: Systematic review of the state of evidence. AIDS and Behavior. 2010;14(1):1–10. doi: 10.1007/s10461-008-9471-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Diagnoses of hiv infection in the united states and dependent areas, 2014. HIV Surveillance Report. 2015a;26:1–123. Retrieved from http://www.cdc.gov/hiv/pdf/library/reports/surveillance/ [Google Scholar]
- CDC. Hiv among gay and bisexual men. 2015b Retrieved from http://www.cdc.gov/hiv/risk/gender/msm/facts/
- CDC. Hiv surveillance - men who have sex with men (msm) 2015c http://www.cdc.gov/hiv/library/slideSets/index.html Retrieved from http://www.cdc.gov/hiv/library/slideSets/index.html.
- Celentano DD, Valleroy LA, Sifakis F, MacKellar DA, Hylton J, Thiede H, … Grp YMSS. Associations between substance use and sexual risk among very young men who have sex with men. Sexually Transmitted Diseases. 2006;33(4):265–271. doi: 10.1097/01.olq.0000187207.10992.4e. [DOI] [PubMed] [Google Scholar]
- Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. Journal of Classification. 1996;13(2):195–212. doi: 10.1007/Bf01246098. [DOI] [Google Scholar]
- Cooper ML. Toward a person x situation model of sexual risk-taking behaviors: Illuminating the conditional effects of traits across sexual situations and relationship contexts. Journal of Personality and Social Psychology. 2010;98(2):319–341. doi: 10.1037/a0017785. [DOI] [PubMed] [Google Scholar]
- Crepaz N, Marks G, Mansergh G, Murphy S, Miller LC, Appleby PR. Age-related risk for hiv infection in men who have sex with men: Examination of behavioral, relationship, and serostatus variables. AIDS Education and Prevention. 2000;12(5):405–415. [PubMed] [Google Scholar]
- Drumright LN, Patterson TL, Strathdee SA. Club drugs as causal risk factors for hiv acquisition among men who have sex with men: A review. Substance Use and Misuse. 2006;41(10–12):1551–1601. doi: 10.1080/10826080600847894. [DOI] [PubMed] [Google Scholar]
- Dudley MG, Rostosky SS, Korfhage BA, Zimmerman RS. Correlates of high-risk sexual behavior among young men who have sex with men. AIDS Education and Prevention. 2004;16(4):328–340. doi: 10.1521/aeap.16.4.328.40397. [DOI] [PubMed] [Google Scholar]
- Finch WH, Bronk KC. Conducting confirmatory latent class analysis using mplus. Structural Equation Modeling-a Multidisciplinary Journal. 2011;18(1):132–151. doi: 10.1080/10705511.2011.532732. [DOI] [Google Scholar]
- Garofalo R, Herrick A, Mustanski BS, Donenberg GR. Tip of the iceberg: Young men who have sex with men, the internet, and hiv risk. American Journal of Public Health. 2007;97(6):1113–1117. doi: 10.2105/AJPH.2005.075630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greene GJ, Andrews R, Kuper L, Mustanski B. Intimacy, monogamy, and condom problems drive unprotected sex among young men in serious relationships with other men: A mixed methods dyadic study. Archives of Sexual Behavior. 2014;43:73–87. doi: 10.1007/s10508-013-0210-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Breslow AS, Newcomb ME, Rosenberger JG, Bauermeister JA. Gay and bisexual men’s use of the internet: Research from the 1990s through 2013. Journal of Sex Research. 2014;51(4):390–409. doi: 10.1080/00224499.2013.871626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grov C, Golub SA, Mustanski B, Parsons JT. Sexual compulsivity, state affect, and sexual risk behavior in a daily diary study of gay and bisexual men. Psychology of Addictive Behaviors. 2010;24(3):487–497. doi: 10.1037/a0020527. [DOI] [PubMed] [Google Scholar]
- Haydon AA, Herring AH, Prinstein MJ, Halpern CT. Beyond age at first sex: Patterns of emerging sexual behavior in adolescence and young adulthood. Journal of Adolescent Health. 2012;50(5):456–463. doi: 10.1016/j.jadohealth.2011.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RB, Kegeles SM, Coates TJ. Unprotected sex and hiv risk taking among young gay men within boyfriend relationships. AIDS Education and Prevention. 1997;9(4):314–329. [PubMed] [Google Scholar]
- Heath J, Lanoye A, Maisto SA. The role of alcohol and substance use in risky sexual behavior among older men who have sex with men: A review and critique of the current literature. AIDS and Behavior. 2012;16(3):578–589. doi: 10.1007/s10461-011-9921-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henry KL, Muthen B. Multilevel latent class analysis: An application of adolescent smoking typologies with individual and contextual predictors. Structural Equation Modeling-a Multidisciplinary Journal. 2010;17(2):193–215. doi: 10.1080/10705511003659342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hipwell AE, Stepp SD, Keenan K, Chung T, Loeber R. Brief report: Parsing the heterogeneity of adolescent girls’ sexual behavior: Relationships to individual and interpersonal factors. Journal of Adolescence. 2011;34(3):589–592. doi: 10.1016/j.adolescence.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan B, Melville J, Phillips G, II, Janulis P, Contractor N, Mustanski B, Birkett M. Evaluating the paper-to-screen translation of participant-aided sociograms with high-risk participants. Paper presented at the ACM CHI; San Jose, CA, USA. 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiwatram-Negron T, El-Bassel N. Systematic review of couple-based hiv intervention and prevention studies: Advantages, gaps, and future directions. AIDS and Behavior. 2014;18(10):1864–1887. doi: 10.1007/s10461-014-0827-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joseph HA, Marks G, Belcher L, Millett GA, Stueve A, Bingham TA, Lauby J. Older partner selection, sexual risk behaviour and unrecognised hiv infection among black and latino men who have sex with men. Sexually Transmitted Infections. 2011;87(5):442–447. doi: 10.1136/sextrans-2011-050010. [DOI] [PubMed] [Google Scholar]
- Karney BR, Hops H, Redding CA, Reis HT, Rothman AJ, Simpson JA. A framework for incorporating dyads in models of hiv-prevention. AIDS and Behavior. 2010;14(Suppl 2):189–203. doi: 10.1007/s10461-010-9802-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhns LM, Birkett M, Muth SQ, Latkin C, Ortiz-Estes I, Garofalo R, Mustanski B. Methods for collection of participant-aided sociograms for the study of social, sexual and substance-using networks among young men who have sex with men. Connect (Tor) 2015;35(1) doi: 10.17266/35.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacefield K, Negy C, Schrader RM, Kuhlman C. Comparing psychosocial correlates of condomless anal sex in hiv-diagnosed and hiv-nondiagnosed men who have sex with men: A series of meta-analyses of studies from 1993–2013. LGBT Health. 2015;2(3):200–220. doi: 10.1089/lgbt.2014.0069. [DOI] [PubMed] [Google Scholar]
- Liau A, Millett G, Marks G. Meta-analytic examination of online sex-seeking and sexual risk behavior among men who have sex with men. Sexually Transmitted Diseases. 2006;33(9):576–584. doi: 10.1097/01.olq.0000204710.35332.c5. [DOI] [PubMed] [Google Scholar]
- Matser A, Heijman T, Geskus R, de Vries H, Kretzschmar M, Speksnijder A, … van der Loeff MS. Perceived hiv status is a key determinant of unprotected anal intercourse within partnerships of men who have sex with men in amsterdam. AIDS and Behavior. 2014;18(12):2442–2456. doi: 10.1007/s10461-014-0819-7. [DOI] [PubMed] [Google Scholar]
- Meng XJ, Zou HC, Fan S, Zheng BF, Zhang L, Dai X, … Lu B. Relative risk for hiv infection among men who have sex with men engaging in different roles in anal sex: A systematic review and meta-analysis on global data. AIDS and Behavior. 2015;19(5):882–889. doi: 10.1007/s10461-014-0921-x. [DOI] [PubMed] [Google Scholar]
- Miyazaki Y, Raudenbush SW. Tests for linkage of multiple cohorts in an accelerated longitudinal design. Psychological Methods. 2000;5(1):44–63. doi: 10.1037/1082-989x.5.1.44. [DOI] [PubMed] [Google Scholar]
- Moosmann DA, Roosa MW. Exploring mexican american adolescent romantic relationship profiles and adjustment. Journal of Adolescence. 2015;43:181–192. doi: 10.1016/j.adolescence.2015.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B. Are sexual partners met online associated with hiv/sti risk behaviours? Retrospective and daily diary data in conflict. AIDS Care. 2007;19(6):822–827. doi: 10.1080/09540120701237244. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Garofalo R, Emerson EM. Mental health disorders, psychological distress, and suicidality in a diverse sample of lesbian, gay, bisexual, and transgender youths. American Journal of Public Health. 2010;100(12):2426–2432. doi: 10.2105/AJPH.2009.178319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Johnson AK, Garofalo R, Ryan D, Birkett M. Perceived likelihood of using hiv pre-exposure prophylaxis medications among young men who have sex with men. AIDS and Behavior. 2013;17(6):2173–2179. doi: 10.1007/s10461-012-0359-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Newcomb M, Du Bois SN, Garcia SC, Grov C. Hiv in young men who have sex with men: A review of epidemiology, risk and protective factors, and interventions. Journal of Sex Research. 2011;48(2–3):218–253. doi: 10.1080/00224499.2011.558645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Newcomb ME. Older sexual partners may contribute to racial disparities in hiv among young men who have sex with men. Journal of Adolescent Health. 2013;52(6):666–667. doi: 10.1016/j.jadohealth.2013.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Newcomb ME, Clerkin EM. Relationship characteristics and sexual risk-taking in young men who have sex with men. Health Psychology. 2011;30(5):597–605. doi: 10.1037/a0023858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mustanski B, Parsons JT. Introduction to the special section on sexual health in gay and bisexual male couples. Archives of Sexual Behavior. 2014;43(1):17–19. doi: 10.1007/s10508-013-0228-4. [DOI] [PubMed] [Google Scholar]
- Mustanski B, Starks T, Newcomb ME. Methods for the design and analysis of relationship and partner effects on sexual health. Archives of Sexual Behavior. 2014;43(1):21–33. doi: 10.1007/s10508-013-0215-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen B, Muthen LK. Integrating person-centered and variable-centered analyses: Growth mixture modeling with latent trajectory classes. Alcoholism, Clinical and Experimental Research. 2000;24(6):882–891. [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 6. Los Angeles, CA: Muthén & Muthén; 1998–2011. [Google Scholar]
- Newcomb ME, Mongrella MC, Weis B, McMillen SJ, Mustanski B. Partner disclosure of prep use and undetectable viral load on geosocial networking apps: Frequency of disclosure and decisions about condomless sex. Journal of Acquired Immune Deficiency Syndromes. 2016;71(2):200–206. doi: 10.1097/QAI.0000000000000819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Mustanski B. Racial differences in same-race partnering and the effects of sexual partnership characteristics on hiv risk in msm: A prospective sexual diary study. Journal of Acquired Immune Deficiency Syndromes. 2013;62(3):329–333. doi: 10.1097/QAI.0b013e31827e5f8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Mustanski B. Developmental change in the relationship between alcohol and drug use before sex and sexual risk behavior in young men who have sex with men. AIDS and Behavior. 2014;18(10):1981–1990. doi: 10.1007/s10461-014-0766-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Mustanski B. Developmental change in the effects of sexual partner and relationship characteristics on sexual risk behavior in young men who have sex with men. AIDS and Behavior. 2015 doi: 10.1007/s10461-015-1046-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newcomb ME, Ryan DT, Garofalo R, Mustanski B. The effects of sexual partnership and relationship characteristics on three sexual risk variables in young men who have sex with men. Archives of Sexual Behavior. 2014;43(1):61–72. doi: 10.1007/s10508-013-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nylund KL, Asparoutiov T, Muthen BO. Deciding on the number of classes in latent class analysis and growth mixture modeling: A monte carlo simulation study. Structural Equation Modeling-a Multidisciplinary Journal. 2007;14(4):535–569. [Google Scholar]
- Parsons JT, Lelutiu-Weinberger C, Botsko M, Golub SA. Predictors of day-level sexual risk for young gay and bisexual men. AIDS and Behavior. 2012 doi: 10.1007/s10461-012-0206-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez-Figueroa RE, Kapadia F, Barton SC, Eddy JA, Halkitis PN. Acceptability of prep uptake among racially/ethnically diverse young men who have sex with men: The p18 study. AIDS Education and Prevention. 2015;27(2):112–125. doi: 10.1521/aeap.2015.27.2.112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prejean J, Song R, Hernandez A, Ziebell R, Green T, Walker F … Group HIVIS. Estimated hiv incidence in the united states, 2006–2009. PloS One. 2011;6(8):e17502. doi: 10.1371/journal.pone.0017502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prestage G, Jin FY, Grulich A, de Wit J, Zablotska I. Gay men are less likely to use condoms with casual sex partners they know ‘well’. AIDS and Behavior. 2012;16(3):664–668. doi: 10.1007/s10461-011-9952-8. [DOI] [PubMed] [Google Scholar]
- Rouwenhorst E, Mallitt KA, Prestage G. Gay men’s use of condoms with casual partners depends on the extent of their prior acquaintance. AIDS and Behavior. 2012;16(6):1589–1596. doi: 10.1007/s10461-011-0092-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusch M, Lampinen TM, Schilder A, Hogg RS. Unprotected anal intercourse associated with recreational drug use among young men who have sex with men depends on partner type and intercourse role. Sexually Transmitted Diseases. 2004;31(8):492–498. doi: 10.1097/01.olq.0000135991.21755.18. [DOI] [PubMed] [Google Scholar]
- Starks TJ, Millar BM, Parsons JT. Predictors of condom use with main and casual partners among hiv-positive men over 50. Health Psychology. 2015;34(11):1116–1122. doi: 10.1037/hea0000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of hiv transmissions from main sex partners among men who have sex with men in five us cities. AIDS. 2009;23(9):1153–1162. doi: 10.1097/QAD.0b013e32832baa34. [DOI] [PubMed] [Google Scholar]
- Vanable PA, McKirnan DJ, Buchbinder SP, Bartholow BN, Douglas JM, Jr, Judson FN, MacQueen KM. Alcohol use and high-risk sexual behavior among men who have sex with men: The effects of consumption level and partner type. Health Psychology. 2004;23(5):525–532. doi: 10.1037/0278-6133.23.5.525. [DOI] [PubMed] [Google Scholar]
- Vasilenko SA, Kugler KC, Butera NM, Lanza ST. Patterns of adolescent sexual behavior predicting young adult sexually transmitted infections: A latent class analysis approach. Archives of Sexual Behavior. 2015;44(3):705–715. doi: 10.1007/s10508-014-0258-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermunt JK. Latent class and finite mixture models for multilevel data sets. Statistical Methods in Medical Research. 2008;17(1):33–51. doi: 10.1177/0962280207081238. [DOI] [PubMed] [Google Scholar]
- Vosburgh HW, Mansergh G, Sullivan PS, Purcell DW. A review of the literature on event-level substance use and sexual risk behavior among men who have sex with men. AIDS and Behavior. 2012;16(6):1394–1410. doi: 10.1007/s10461-011-0131-8. [DOI] [PubMed] [Google Scholar]
- Wu E, El-Bassel N, McVinney LD, Hess L, Remien RH, Charania M, Mansergh G. Feasibility and promise of a couple-based hiv/sti preventive intervention for methamphetamine-using, black men who have sex with men. AIDS and Behavior. 2011;15(8):1745–1754. doi: 10.1007/s10461-011-9997-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeo TED, Ng YL. Sexual risk behaviors among apps-using young men who have sex with men in hong kong. Aids Care-Psychological and Socio-Medical Aspects of Aids/Hiv. 2016;28(3):314–318. doi: 10.1080/09540121.2015.1093597. [DOI] [PubMed] [Google Scholar]