Abstract
AIM
To estimate overall prevalence of retinopathy of prematurity (ROP) in Iran using a systematic review and Meta-analysis.
METHODS
A systematic review and Meta-analysis was performed of all published studies pertaining to prevalence of ROP using international and national electronic databases (ISI Web of Sciences, PubMed, Scopus, Google Scholar, SID, MagIran, and IranMedex) from their inception until May 2016 with standard keywords. Begg and Egger tests were used to examine the publication bias and Cochran test and I2 statistics were used to evaluate the statistical heterogeneity. Pooled estimate of the prevalence of ROP were calculated using random effects Meta-analysis.
RESULTS
The publication bias assumption was rejected by Egger tests with P-value equal to 0.024. The results of Cochran test and I2 statistics revealed substantial heterogeneity (Q=1099.02, df=25, I2=97.7%, P=0.001). The overall prevalence of ROP using the random effect model in Iran was 26.1% (95% CI: 20.3%-31.8%).
CONCLUSION
The prevalence of ROP is relatively high in Iran. Low birth weight and gestational age are significant risk factors for the disease. Improved care, including oxygen delivery and monitoring, for preterm babies in all facility settings would reduce the number of babies affected with ROP.
Keywords: retinopathy of prematurity, preterm birth, infant, Meta-analysis, systematic review, Iran
INTRODUCTION
Retinopathy of prematurity (ROP), previously known as retrolental fibroplasia, is a proliferative vascular disorder of the retina that can lead to poor visual acuity or blindness in preterm infants[1]. It affects a substantial number of preterm infants and is a leading cause of potentially preventable childhood blindness throughout the world[2]. Moreover, the increased survival of preterm infants in recent years, due to improvement in antenatal and neonatal care, has produced a population of infants at high risk of developing ROP[2]. The two most important risk factors for developing ROP are low birth weight (BW) and low gestational age (GA)[3]–[5]. Other risk factors include oxygen therapy, sex, sepsis, anemia, intraventricular hemorrhage and blood transfusion[3]–[4],[6]–[9].
Numerous studies have been conducted to determine the prevalence of ROP and its related factors in Iran. However, there is a remarkable diversity among the results. The prevalence of ROP in these studies was between 5.6% and 70.3%[10]–[35].
Due to the substantial heterogeneity among the reported prevalence and the importance of prevention and treating ROP, which constitutes a major burden for health care systems, the accurate determination of ROP prevalence is essential for strategic plan and health policy. Given the importance of the subject, we performed a systematic review and Meta-analysis of all published studies pertaining to prevalence of ROP in Iran.
MATERIALS AND METHODS
Search Strategy and Study Selection Criteria
To collect related articles, both international and national databases including ISI Web of Sciences, PubMed, Scopus, Google Scholar, SID, MagIran, and IranMedex were searched for MeSH terms “retinopathy of prematurity”, “ROP” and “Iran” and their Persian equivalents in titles or abstracts. A systematic review in the mentioned database was done without any time restriction. Duplications, Meta-analysis and case reports were excluded from analysis.
All Persian or English included studies were cross-sectional study (descriptive or analytical). All records were included in Endnote X6 for assessing and categorizing. At the first, title and abstract were systematically assessed for finding the relevant studies. Then, eligible studies were obtained for full text screening. All relevant publications were separately reviewed by two reviewers (Maroufizadeh S and Almasi-Hashiani A) for the eligibility criteria. Disagreement between reviewers was resolved by consensus.
Data Extraction and Study Quality
After review of the full texts, the following data were extracted from each study: study and participant characteristics including first author's name, date of study, sample size, province or city of the study, BW, GA, boy/girl (B/G) ratio, year of publication and ROP prevalence. The quality of the studies was evaluated using a modified STROBE checklist.
Data Analysis
All statistical analyses were performed using Stata version 13.0 (StataCorp, College Station, TX, USA). The prevalence of ROP was polled by the “metan” command and showed by a forest plot. The Cochrane Q test and I2 statistic were used to test heterogeneity across studies[36]. A P-value <0.1, rather than <0.05, was used as evidence of heterogeneity for the Cochrane Q test, as recommended by the Cochrane Collaboration. The I2 statistic expresses the percentage of total variation across studies due to heterogeneity. I2 values of 25%, 50% and 75% correspond to low, moderate and high heterogeneity, respectively[36]. Considering the substantial heterogeneity among studies, we used a random effects model for all analyses. Meta regression was used to explore the sources of between-study heterogeneity, including year of study, sample size, BW, GA and sex ratio. Moreover, the Galbraith plot was used to detect the potential sources of heterogeneity[37]. The Funnel plot and Begg's rank correlation and Egger's weighted regression tests were used to assess publication bias by “metabias” command[38]–[39]. To correct publication bias, the Trim and Filled method was used by the “metatrim” command in Stata. Sensitivity analysis was done by “metainf” command.
RESULTS
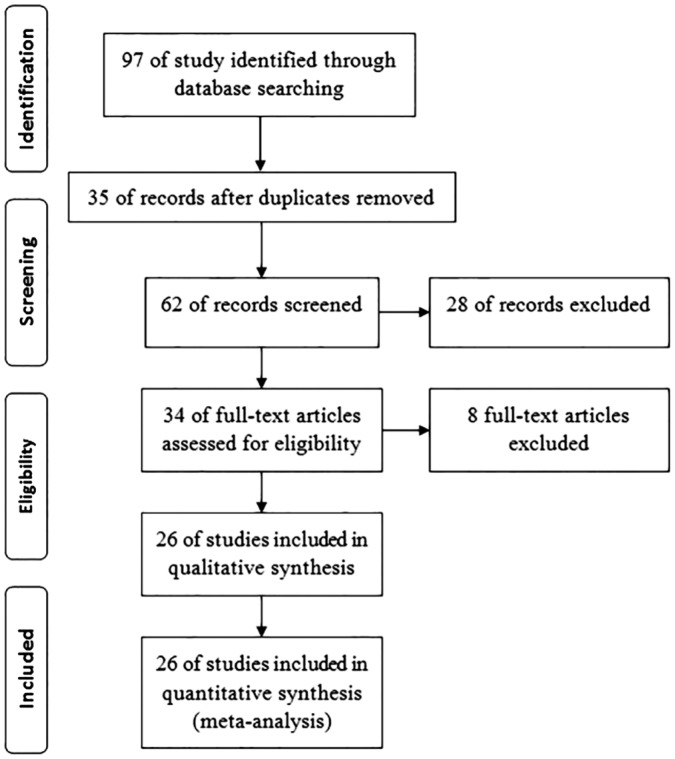
The findings of this review are summarized in Table 1. We include 26 individual studies from 10 provinces across the country (with 8786 cases). All included papers were cross-sectional studies. The sample size of the studies was between 50 and 1053 cases. The study flowchart was show in Figure 1.
Table 1. Description of the studies included in the Meta-analysis.
| Authors | Location | Year | n | Prevalence (%) | Inclusion criteria [GA (wk); BW (g)] | GA (wk) | BW (g) | B/G ratio |
| Riazi Esfahani et al[10] | Tehran | 1997-1999 | 150 | 6.0 | GA≤37 or BW≤2500 | 33.46 | 1814.5 | 0.97 |
| Nakshab et al[11] | Sari | 2001-2002 | 68 | 11.8 | BW≤2500 | 32.30 | 1695.9 | NR |
| Karkhaneh et al[12] | Tehran | 2000-2002 | 185 | 12.4 | GA≤37 or BW≤2500 | 31.64 | 1620.7 | 1.47 |
| Mansouri et al[13] | Tehran | 2004-2005 | 147 | 29.9 | GA≤32; BW≤1500 | 30.30 | 1385.8 | 1.01 |
| Karkhaneh et al[14] | Tehran | 2003-2007 | 953 | 34.5 | GA≤37 | 31.10 | 1542.0 | 1.19 |
| Fayyazi et al[15] | Tabriz | 2005-2006 | 399 | 7.3 | GA≤37 or BW≤2500, and infant with BW: 1500-2500 who had unstable condition | NR | NR | NR |
| Khatami et al[16] | Mashhad | 2000-2001 | 50 | 28.0 | GA≤34; BW≤2000 | 32.86 | 1586.0 | 0.92 |
| Mousavi et al[17] | Tehran | 2001-2006 | 191 | 39.3 | Premature infants with late retinal examination | 30.00 | 1404.0 | 1.15 |
| Riazi-Esfahani et al[18] | Tehran | 2002-2004 | 198 | 13.6 | GA≤30 or BW≤2500 | 32.04 | 1635.4 | 1.08 |
| Sadeghi et al[19] | Tabriz | NR | 150 | 17.3 | GA≤36; BW≤2000 | 29.12 | 1438.7 | 1.27 |
| Fouladinejad et al[20] | Gorgan | 2004-2005 | 89 | 5.6 | GA≤34 | NR | NR | 1.02 |
| Mousavi et al[21] | Tehran | 2001-2007 | 216 | 40.3 | Infants with late retinal examination | 29.90 | 1410.0 | 1.25 |
| Naderian et al[22] | Isfahan | 2002-2008 | 796 | 16.8 | 25≤GA≤34; 600≤BW≤1800 | 29.50 | 1300.0 | 1.04 |
| Saeidi et al[23] | Mashhad | 2005-2006 | 47 | 8.5 | GA≤32; BW≤1500 | NR | 1223.7 | 0.96 |
| Bayat-Mokhtari et al[24] | Shiraz | 2006-2007 | 199 | 42.2 | BW<1500 or infants with BW between 1500-2000 who had unstable clinical condition | 30.80 | 1393.1 | 1.14 |
| Mousavi et al[25] | Tehran | 2003-2007 | 1053 | 36.1 | Premature infants | NR | NR | NR |
| Naderian et al[26] | Isfahan | 2003-2008 | 604 | 17.5 | GA≤37; BW≤2500 | 31.00 | 1375.3 | 1.16 |
| Ebrahim et al[27] | Babol | 2004-2008 | 173 | 19.1 | GA≤37 | 32.24 | 1680.6 | 1.06 |
| Ghaseminejad and Niknafs[28] | Kerman | 2006-2008 | 83 | 28.9 | GA≤36; BW≤2500 | 31.76 | 1543.4 | 1.44 |
| Naderian et al[29] | Isfahan | NR | 200 | 35.5 | GA≤34; BW≤1800 | 30.72 | 1325.5 | 1.00 |
| Afarid et al[30] | Shiraz | 2006-2010 | 787 | 37.2 | GA≤32 or BW≤2000 | 30.87 | 1397.0 | 0.98 |
| Feghhi et al[31] | Ahvaz | 2006-2010 | 576 | 31.8 | GA≤32 and/or BW≤2500 | 31.64 | 1204.0 | 1.09 |
| Abrishami et al[32] | Mashhad | 2006-2010 | 122 | 26.2 | GA≤32 | 30.54 | 1249.0 | 0.88 |
| Sabzehei et al[33] | Tehran | 2007-2010 | 414 | 17.1 | BW≤1500 | 30.45 | 1268.6 | 1.01 |
| Ahmadpour-kacho et al[34] | Babol | 2009-2012 | 256 | 70.3 | GA≤28; BW≤1500; infant with GA: 29-34 and BW:1500-2000 with an unstable clinical condition | 31.08 | 1489.6 | 0.98 |
| Rasoulinejad and Montazeri[35] | Babol | 2007-2013 | 680 | 45.0 | GA≤37 or BW≤2500 | 31.45 | 1713.9 | 1.66 |
GA: Gestational age; BW: Birth weight; B/G ratio: Boy/girl ratio; NR: Not reported.
Figure 1. Study flowchart.
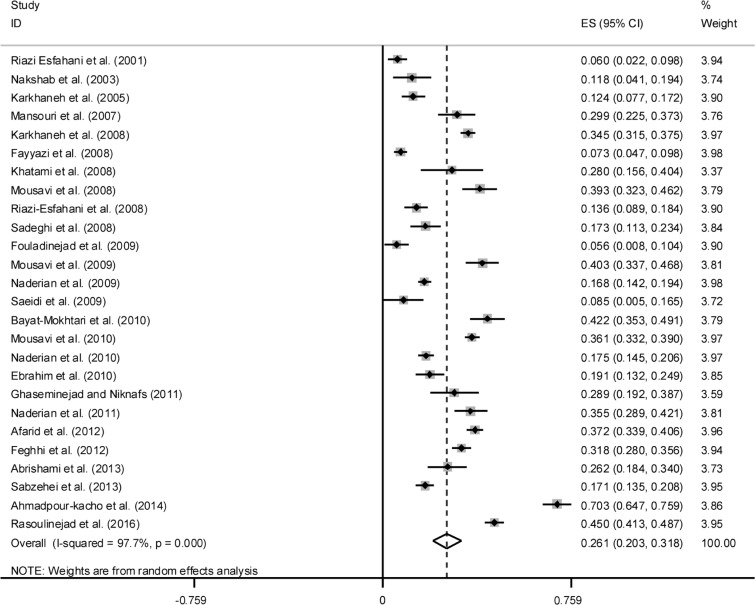
The results of Cochran's Q test and I2 statistics showed high heterogeneity among the included studies. Due to evidence of heterogeneity in studies (Q=1099.02, df=25, I2=97.7%, P=0.001), random model was used to poll the studies. The overall estimates of the prevalence of ROP based on the individual studies were 26.1% (95% CI: 20.3%-31.8%) (Figure 2). The highest prevalence of ROP (70.3%, 95% CI: 64.7%-75.9%) was reported from Babolcity, and the lowest prevalence of ROP (5.6%, 95% CI: 0.8%-10.4%) was reported in Golestan Province.
Figure 2. Prevalence of ROP in Iranian neonatal.
Meta-regression for Heterogeneity
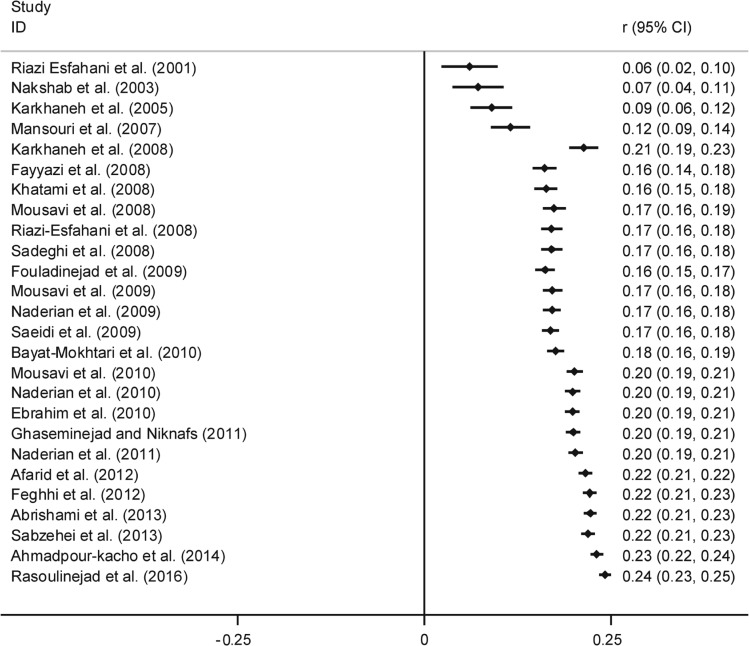
Meta regression was used to explore the sources of between-study heterogeneity, including year of publication, sample size, BW, GA and B/G ratio. This analysis revealed that the year of publication is responsible for heterogeneity. Therefore, a cumulative Meta-analysis and subgroup analysis based on the year of publication were performed. In the subgroup analysis, the individual studies were divided into two time periods of publication, before and after 2010. The polled estimated prevalence of ROP before and after 2010 were different, 19.2 (95% CI: 12.8-25.5) and 33.9 (95% CI: 26.1-41.8), respectively. After running cumulative Meta-analysis with “metacum” command in Stata, the prevalence of ROP showed an increase from 6.0% in 2001 to 24.1% in 2016 (Figure 3). Also we perform sensitivity analysis to identify the effect of the each study on polled estimate and the results showed that Ahmadpour-kacho et al[34] study has more effect on polled estimate so that after removing it the polled estimate decreases to 24.2% (Table 2).
Figure 3. Cumulative prevalence of ROP according to year of publication.
Table 2. Sensitivity analysis to identify the effect of each study on polled estimate.
| Authors | Prevalence (95% CI) |
| Riazi Esfahani et al[10] | 0.269 (0.211-0.326) |
| Nakshab et al[11] | 0.266 (0.208-0.324) |
| Karkhaneh et al[12] | 0.266 (0.207-0.325) |
| Mansouri et al[13] | 0.259 (0.200-0.318) |
| Karkhaneh et al[14] | 0.257 (0.198-0.316) |
| Fayyazi et al[15] | 0.268 (0.212-0.325) |
| Khatami et al[16] | 0.260 (0.201-0.318) |
| Mousavi et al[17] | 0.255 (0.197-0.314) |
| Riazi-Esfahani et al[18] | 0.266 (0.207-0.324) |
| Sadeghi et al[19] | 0.264 (0.205-0.323) |
| Fouladinejad et al[20] | 0.269 (0.211-0.327) |
| Mousavi et al[21] | 0.255 (0.197-0.313) |
| Naderian et al[22] | 0.264 (0.204-0.325) |
| Saeidi et al[23] | 0.267 (0.209-0.326) |
| Bayat-Mokhtari et al[24] | 0.254 (0.196-0.312) |
| Mousavi et al[25] | 0.256 (0.197-0.315) |
| Naderian et al[26] | 0.264 (0.204-0.324) |
| Ebrahim et al[27] | 0.263 (0.204-0.322) |
| Ghaseminejad and Niknafs[28] | 0.259 (0.201-0.318) |
| Naderian et al[29] | 0.257 (0.198-0.315) |
| Afarid et al[30] | 0.256 (0.197-0.315) |
| Feghhi et al[31] | 0.258 (0.199-0.318) |
| Abrishami et al[32] | 0.260 (0.202-0.319) |
| Sabzehei et al[33] | 0.264 (0.204-0.324) |
| Ahmadpour-kacho et al[34] | 0.243 (0.191-0.294) |
| Rasoulinejad and Montazeri[35] | 0.253 (0.196-0.309) |
| Combined | 0.261 (0.203-0.318) |
CI: Confidence interval.
Publication Bias
Begg's test, Egger's test and also Funnel plot were used to determine the present of publication bias and there was a controversy between Begg's and Egger's tests (P=0.582, 0.024, respectively), and based on Begg's test there was no evidence of publication bias but Egger's test shows some evidence of publication bias in the studies. Since the Egger's test has more power, therefore, the Trim and Filled method was used to estimate the prevalence of ROP. By Trim and Filled analysis, ROP prevalence in Iran was estimated as 20.9% (95% CI: 14.8%-27.1%).
DISCUSSION
The major goal of the present study was to estimate the prevalence of ROP in Iran. Based on the results of the Meta-analysis, the prevalence of ROP in Iran was estimated to be 26.1% (95% CI: 20.3%-31.8%). In the Meta-analysis, the larger sample size will be reviewed and estimation would be more accurate for researchers and policy makers[40]. In Iran, the prevalence of ROP in published papers was reported between 5.6% and 70.3%[10]–[35], after weighting for each study we polled these studies.
ROP is a potentially blinding disease of the retina. In spite of in progress screening and different treatment guidelines, ROP is still a main cause of blindness in children in the both developing and developed world[41]. Gilbert et al[42] between 1991 and 1996, examined 4121 children in 23 middle-income countries and their results showed that the prevalence of severe visual impairment or blindness due to ROP ranged from 0 in most African countries to more than 38% in Cuba.
The prevalence of ROP has diversity across the countries and states. The existing data suggest that blindness due ROP varies extremely from country to country, and globally, over 50 000 children are blind due to ROP[2]. Graziano et al[43] conducted a prospective examination on 102 neonates with very low BW in Brazil and in their study, prevalence of ROP was reported 29.09% which is slightly higher than estimated prevalence in our study (26.1%). Several studies have emphasized that a significant proportion of blindness due to ROP can be prevented in the presence of a regular screening program and promote awareness of physicians as well as the parents[44]–[45]. Another way to reduce blindness due to ROP is examination of high-risk newborns in the neonatal intensive care unit (NICU)[46].
In the present study, after running cumulative Meta-analysis, the prevalence of ROP showed an increase from 6.0% in 2001 to 24.1% in 2016. This rise may be explained by improvements in neonatal care in our NICUs, which leads to increased survival of premature infants. Similar our results, in the Karkhaneh et al[14] study that performed in Farabi Hospital as a referral hospital for eyes disease in Iran (the Tertiary Eye Hospital), a significant increase was observed in the incidence of ROP. In the Farabi Hospital the incidence of ROP increases from 6% in 1997-1999 to 12.4% in 2000-2002, and 34.5% in 2007[14]. In the subgroup analysis in our study, the polled estimated prevalence of ROP before 2010 were 19.2% and after 2010 were increases to 33.9%.
In compare to the prevalence of ROP reported from other countries, ROP incidence in Iran is higher than some countries. For instance, the incidence of ROP in infants with GA<31wk or BW<1500 g in France in 2007 was 15%[47] and also the incidence of ROP in infants with BW <2000 g or GA <34wk was 10.8% in China in 2008[48]. Incidence of ROP in more developed countries was reported between 10% to 27% and it is depend on degree of prematurity and BW[49]–[50].
Increase trend in the incidence of ROP represents the better care of the infants in premature infants in the NICU but on the other hand it should be keep in mind that these infants needed more attention to problems such as retinopathy. We conduct a wide search strategy in different databases to include as many studies as possible. We screened 97 retrieved published papers and finally included 26 individual studies in the Meta-analysis with 8786 cases. Egger and Begg tests show some evidence of the possibility of publication bias and in this case we used Trim and Filled method and also Chi-square and I2 tests show heterogeneity between studies, therefore we used random effect model in the Meta-analysis and perform subgroups analysis based on year of publication which is recognized as a heterogeneity factor in the Meta regression.
In summary, the overall prevalence of ROP is relatively high in Iran. This disorder can lead to visual impairment or blindness in premature infants. Much of this burden is avoidable with improved quality of antenatal and neonatal care, notably oxygen monitoring, and with both screening and treatment of ROP. Urgent action is required to improve awareness of ROP among all healthcare professionals involved in the care of premature infants, coupled with commitments to improve neonatal care, and to develop and implement protocol and guidelines for the prevention, screening, and treatment of ROP.
Acknowledgments
Conflicts of Interest: Maroufizadeh S, None; Almasi-Hashiani A, None; Omani Samani R, None; Sepidarkish M, None.
REFERENCES
- 1.Good WV, Hardy RJ, Dobson V, Palmer EA, Phelps DL, Quintos M, Tung B, Early Treatment for Retinopathy of Prematurity Cooperative Group The incidence and course of retinopathy of prematurity: findings from the early treatment for retinopathy of prematurity study. Pediatrics. 2005;116(1):15–23. doi: 10.1542/peds.2004-1413. [DOI] [PubMed] [Google Scholar]
- 2.Gilbert C, Fielder A, Gordillo L, Quinn G, Semiglia R, Visintin P, Zin A, International NO-ROP Group Characteristics of infants with severe retinopathy of prematurity in countries with low, moderate, and high levels of development: implications for screening programs. Pediatrics. 2005;115(5):518–525. doi: 10.1542/peds.2004-1180. [DOI] [PubMed] [Google Scholar]
- 3.Darlow BA, Hutchinson JL, Henderson-Smart DJ, Donoghue DA, Simpson JM, Evans NJ. Prenatal risk factors for severe retinopathy of prematurity among very preterm infants of the Australian and New Zealand neonatal network. Pediatrics. 2005;115(4):990–996. doi: 10.1542/peds.2004-1309. [DOI] [PubMed] [Google Scholar]
- 4.Kim TI, Sohn J, Pi SY, Yoon YH. Postnatal risk factors of retinopathy of prematurity. Paediatr Perinat Epidemiol. 2004;18(2):130–134. doi: 10.1111/j.1365-3016.2003.00545.x. [DOI] [PubMed] [Google Scholar]
- 5.Aclimandos W. Seventy years of retinopathy of prematurity. Br J Ophthalmol. 2011;95(7):899–900. doi: 10.1136/bjo.2010.201079. [DOI] [PubMed] [Google Scholar]
- 6.Cooke RW, Clark D, Hickey-Dwyer M, Weindling AM. The apparent role of blood transfusions in the development of retinopathy of prematurity. Eur J Pediatr. 1993;152(10):833–836. doi: 10.1007/BF02073381. [DOI] [PubMed] [Google Scholar]
- 7.Brooks SE, Marcus DM, Gillis D, Pirie E, Johnson MH, Bhatia J. The effect of blood transfusion protocol on retinopathy of prematurity: a prospective, randomized study. Pediatrics. 1999;104(3):514–518. doi: 10.1542/peds.104.3.514. [DOI] [PubMed] [Google Scholar]
- 8.Englert JA, Saunders RA, Purohit D, Hulsey TC, Ebeling M. The effect of anemia on retinopathy of prematurity in extremely low birth weight infants. J Perinatol. 2001;21(1):21–26. doi: 10.1038/sj.jp.7200511. [DOI] [PubMed] [Google Scholar]
- 9.Gupta VP, Dhaliwal U, Sharma R, Gupta P, Rohatgi J. Retinopathy of prematurity--risk factors. Indian J Pediatr. 2004;71(10):887–892. doi: 10.1007/BF02830827. [DOI] [PubMed] [Google Scholar]
- 10.Riazi Esfahani M, Karkhaneh R, Shokravi N. Assessment of retinopathy of prematurity among 150 premature neonates in Farabi Eye Hospital. Acta Med Iran. 2001;39(1):35–38. [Google Scholar]
- 11.Nakshab M, Bayani G, Ahmadzadeh Amiri A, Eshaghi M. Prevalence of retinopathy in premature neonates in neonatal intensive care unit of Boali sina hospital in 2001. J Mazandaran Univ Med Sci. 2003;13(39):63–70. [Google Scholar]
- 12.Karkhaneh R, Riazi Esfahani M, Ghojehzadeh L, Kadivar M, Nayeri F, Chams H, Nili Ahmadabadi M. Incidence and risk factors of retinopathy of prematurity. Bina J Ophthalmol. 2005;11(1):81–90. [Google Scholar]
- 13.Mansouri M, Kadivar M, Karkhaneh R, Riazi Esfahani M, Nili Ahmadabadi M, Faghihi H, Mirshahi A, Sadat-Nayeri F, Farahvash M, Tabatabaei A, Adelpour A, Abdollahi M. Prevalence and risk factors of retinopathy of prematurity in very low birth weight or low gestational age infants. Bina J Ophthalmol. 2007;12(4):428–434. [Google Scholar]
- 14.Karkhaneh R, Mousavi SZ, Riazi-Esfahani M, Ebrahimzadeh SA, Roohipoor R, Kadivar M, Ghalichi L, Mohammadi SF, Mansouri MR. Incidence and risk factors of retinopathy of prematurity in a tertiary eye hospital in Tehran. Br J Ophthalmol. 2008;92(11):1446–1449. doi: 10.1136/bjo.2008.145136. [DOI] [PubMed] [Google Scholar]
- 15.Fayyazi A, Heidarzadeh M, Fayzalahzadeh H, Golzar A, Sadegi K. Prevalence of retinopathy of prematurity in preterm infant hospitalized in Tabriz Alzahra Hospital's NICU. Med J Tabriz Uni Med Sci. 2008;30(4):63–66. [Google Scholar]
- 16.Khatami SF, Yousefi A, Fathi Bayat G, Mamuri G. Retinopathy of prematurity among 1000-2000 gram birth weight newborn infants. Iran J Pediatr. 2008;18(2):137–142. [Google Scholar]
- 17.Mousavi S, Karkhaneh R, Riazi-Esfahani M, Mansouri M, Roohipoor R, Ghalichi L, Kadivar M, Nili-AhmadAbadi M, Naieri F. Incidence, severity and risk factors of retinopathy of prematurity in premature infants with late retinal examination. Bina J Ophthalmol. 2008;13(4):412–417. [Google Scholar]
- 18.Riazi-Esfahani M, Alizadeh Y, Karkhaneh R, Mansouri MR, Kadivar M, Nili Ahmadabadi M, Nayeri F. Retinopathy of prematurity: single versus multiple-birth pregnancies. J Ophthalmic Vis Res. 2008;3(1):47–51. [PMC free article] [PubMed] [Google Scholar]
- 19.Sadeghi K, Heidary E, Hashemi F, Heydarzadeh M. Incidence and risk factors of retinopathy of prematurity. Med J Tabriz Uni Med Sci. 2008;30(2):73–77. [Google Scholar]
- 20.Fouladinejad M, Motahari MM, Gharib MH, Sheishari F, Soltani M. The prevalence, intensity and some risk factors of retinopathy of premature newborns in Taleghani Hospital, Gorgan, Iran. J Gorgan Uni Med Sci. 2009;11(2):51–54. [Google Scholar]
- 21.Mousavi SZ, Karkhaneh R, Riazi-Esfahani M, Mansouri MR, Roohipoor R, Ghalichi L, Kadivar M, Nili-Ahmadabadi M, Naieri F. Retinopathy of prematurity in infants with late retinal examination. J Ophthalmic Vis Res. 2009;4(1):24–28. [PMC free article] [PubMed] [Google Scholar]
- 22.Naderian G, Parvaresh M, Rismanchiyan A, Sajadi V. Refractive errors after laser therapy for retinopathy of prematurity. Bina J Ophthalmol. 2009;15(1):13–18. [Google Scholar]
- 23.Saeidi R, Hashemzadeh A, Ahmadi S, Rahmani S. Prevalence and predisposing factors of retinopathy of prematurity in very low-birth-weight infants discharged from NICU. Iran J Pediatr. 2009;19(1):59–63. [Google Scholar]
- 24.Bayat-Mokhtari M, Pishva N, Attarzadeh A, Hosseini H, Pourarian S. Incidence and risk factors of retinopathy of prematurity among preterm infants in Shiraz/Iran. Iran J Pediatr. 2010;20(3):303–307. [PMC free article] [PubMed] [Google Scholar]
- 25.Mousavi S, Riazi Esfahani M, Roohipoor R, Jabbarvand M, Ghalichi L, Nili Ahmadabadi M, Ghassemi F, Aalami Harandi Z, Karkhaneh R. Characteristics of advanced stages of retinopathy of prematurity. Iran J Ophthalmol. 2010;22(2):19–24. [Google Scholar]
- 26.Naderian G, Molavi-Vardanjani H, Hadipour M, Sajjadi V. Prevalence and risk factors for retinopathy of prematurity in Isfahan. Bina J Ophthalmol. 2010;15(3):208–213. [Google Scholar]
- 27.Ebrahim M, Ahmad RS, Mohammad M. Incidence and risk factors of retinopathy of prematurity in Babol, North of Iran. Ophthalmic Epidemiol. 2010;17(3):166–170. doi: 10.3109/09286581003734860. [DOI] [PubMed] [Google Scholar]
- 28.Ghaseminejad A, Niknafs P. Distribution of retinopathy of prematurity and its risk factors. Iran J Pediatr. 2011;21(2):209–214. [PMC free article] [PubMed] [Google Scholar]
- 29.Naderian G, Iranpour R, Mohammadizadeh M, Fazel Najafabadi F, Badiei Z, Naseri F, Naderian M, Sajadi V. The frequency of retinopathy of prematurity in premature infants referred to an ophthalmology clinic in Isfahan. J Isfahan Med Sch. 2011;29(128):126–130. [Google Scholar]
- 30.Afarid M, Hosseini H, Abtahi B. Screening for retinopathy of prematurity in south of Iran. Middle East Afr J Ophthalmol. 2012;19(3):277–281. doi: 10.4103/0974-9233.97922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Feghhi M, Altayeb SM, Haghi F, Kasiri A, Farahi F, Dehdashtyan M, Movasaghi M, Rahim F. Incidence of retinopathy of prematurity and risk factors in the south-western region of Iran. Middle East Afr J Ophthalmol. 2012;19(1):101–106. doi: 10.4103/0974-9233.92124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abrishami M, Maemori GA, Boskabadi H, Yaeghobi Z, Mafi-Nejad S, Abrishami M. Incidence and risk factors of retinopathy of prematurity in Mashhad, Northeast Iran. Iran Red Crescent Med J. 2013;15(3):229–233. doi: 10.5812/ircmj.4513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sabzehei MK, Afjeh SA, Dastijani Farahani A, Shamshiri AR, Esmaili F. Retinopathy of prematurity: incidence, risk factors, and outcome. Arch Iran Med. 2013;16(9):507–512. [PubMed] [Google Scholar]
- 34.Ahmadpour-kacho M, Zahed Pasha Y, Rasoulinejad SA, Hajiahmadi M, Pourdad P. Correlation between retinopathy of prematurity and clinical risk index for babies score. Tehran Univ Med J. 2014;72(6):404–411. [Google Scholar]
- 35.Rasoulinejad SA, Montazeri M. Retinopathy of prematurity in neonates and its risk factors: a seven year study in Northern Iran. Open Ophthalmol J. 2016;10(1):17–21. doi: 10.2174/1874364101610010017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 37.Galbraith RF. A note on graphical presentation of estimated odds ratios from several clinical trials. Stat Med. 1988;7(8):889–894. doi: 10.1002/sim.4780070807. [DOI] [PubMed] [Google Scholar]
- 38.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50(4):1088–1101. [PubMed] [Google Scholar]
- 39.Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Noble JH., Jr Meta-analysis: Methods, strengths, weaknesses, and political uses. J Lab Clin Med. 2006;147(1):7–20. doi: 10.1016/j.lab.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 41.Chen J, Stahl A, Hellstrom A, Smith LE. Current update on retinopathy of prematurity: screening and treatment. Curr Opin Pediatr. 2011;23(2):173–178. doi: 10.1097/MOP.0b013e3283423f35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gilbert C, Rahi J, Eckstein M, O'Sullivan J, Foster A. Retinopathy of prematurity in middle-income countries. Lancet. 1997;350(9070):12–14. doi: 10.1016/S0140-6736(97)01107-0. [DOI] [PubMed] [Google Scholar]
- 43.Graziano RM, Leone CR, Cunha SL, Pinheiro AC. Prevalence of retinopathy of prematurity in very low birth weight infants. J Pediatr (Rio J) 1997;73(6):377–382. doi: 10.2223/jped.564. [DOI] [PubMed] [Google Scholar]
- 44.Modrzejewska M. Retinopathy of prematurity: clinical findings and current opinions on diagnosis and treatment. Ann Acad Med Stetin. 2006;52(1):73–78. [PubMed] [Google Scholar]
- 45.Gilbert C. Retinopathy of prematurity: a global perspective of the epidemics, population of babies at risk and implications for control. Early Hum Dev. 2008;84(2):77–82. doi: 10.1016/j.earlhumdev.2007.11.009. [DOI] [PubMed] [Google Scholar]
- 46.Attar MA, Gates MR, Iatrow AM, Lang SW, Bratton SL. Barriers to screening infants for retinopathy of prematurity after discharge or transfer from a neonatal intensive care unit. J Perinatol. 2005;25(1):36–40. doi: 10.1038/sj.jp.7211203. [DOI] [PubMed] [Google Scholar]
- 47.Lala-Gitteau E, Majzoub S, Saliba E, Pisella PJ. Epidemiology for retinopathy of prematurity: risk factors in the Tours hospital (France) J Fr Ophtalmol. 2007;30(4):366–373. doi: 10.1016/s0181-5512(07)89606-9. [DOI] [PubMed] [Google Scholar]
- 48.Chen Y, Li XX, Yin H, Gilbert C, Liang JH, Jiang YR, Zhao MW, Beijing ROP Survey Group Risk factors for retinopathy of prematurity in six neonatal intensive care units in Beijing, China. Br J Ophthalmol. 2008;92(3):326–330. doi: 10.1136/bjo.2007.131813. [DOI] [PubMed] [Google Scholar]
- 49.Darlow BA, Horwood LJ, Clemett RS. Retinopathy of prematurity: risk factors in a prospective population-based study. Paediatr Perinat Epidemiol. 1992;6(1):62–80. doi: 10.1111/j.1365-3016.1992.tb00747.x. [DOI] [PubMed] [Google Scholar]
- 50.Early Treatment For Retinopathy Of Prematurity Cooperative Group Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial. Arch Ophthalmol. 2003;121(12):1684–1694. doi: 10.1001/archopht.121.12.1684. [DOI] [PubMed] [Google Scholar]