Synopsis
Mycobacterium tuberculosis is the leading cause of death worldwide from a single bacterial pathogen. World Health Organization (WHO) estimates that annually, 1 million children have TB disease and many more harbor a latent form of infection. However, accurate estimates are hindered by under-recognition and challenges in diagnosis; to date, an accurate diagnostic test to confirm TB in children does not exist. TB treatment is lengthy, but outcomes are generally favorable with timely initiation. As we move toward the End TB Strategy, there is an urgent need for improved diagnostics and treatment to prevent the unnecessary morbidity and mortality from TB in children.
Keywords: Tuberculosis, global epidemiology, latent infection, diagnosis, management, prevention, advocacy
Introduction
Despite achieving great public health strides to control tuberculosis (TB) within the United States, it remains an enormous public health issue worldwide. Accurate statistics on pediatric TB cases are difficult to obtain for a multitude of reasons, including under-recognition, challenges in confirming the diagnosis, and under-reporting to national TB programs. The clinical and radiographic manifestations are less specific in children compared to adults, and are often confused with bacterial pneumonia. Microbiologic confirmation of disease is limited by the paucibacillary nature of TB in children; in general, TB cultures and newer rapid molecular tests are positive in the minority of children, generally <25–40% of children with TB disease.1,2 Additionally, there are often logistic challenges in obtaining adequate specimens from young children. However, in the era of multi drug-resistant TB (MDR-TB) in which the organism is resistant to isoniazid and rifampin (the two most potent first-line agents), there is an increasing need to attempt culture-confirmation on all children suspected of having TB in order to inform treatment decisions. Among children who are started on TB therapy, families struggle with proper dose administration due to the lack of pediatric drug formulations and there are programmatic gaps in notifying the national TB program, leading to under-reporting by the World Health Organization (WHO). Yet, with proper management, including timely treatment initiation with appropriate drug dosages, treatment outcomes are generally favorable.
Epidemiology
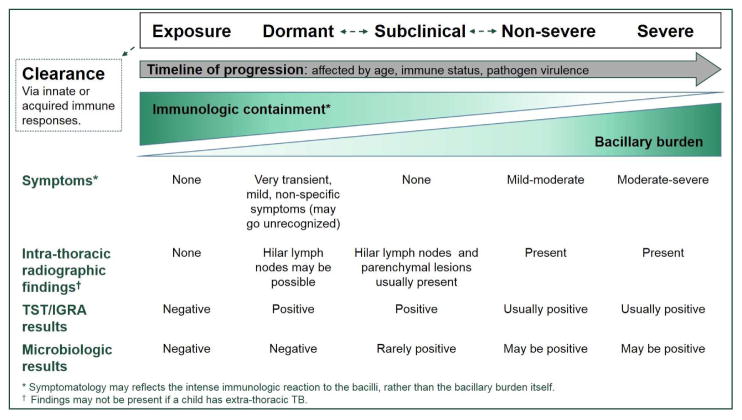
The global distribution of childhood TB mirrors that of adults (see Figure 1), with a heavy burden of disease in sub-Saharan Africa and Asia.3 The United States is considered a low-incidence country with <4 cases/100,000 population. Domestically, the majority of TB cases are associated with foreign birth;4 between 2008–2010, there were 2660 children and adolescents diagnosed with TB.5 Among them, 31% were foreign born youth; of the remaining US-born cases, 66% had at least one parent who was foreign-born. These trends suggest that the majority of domestic TB cases in children may be exposed in international settings or through foreign-born parents, thus highlighting an opportunity for increased prevention efforts.
Figure 1.
Estimated TB incidence rates in 2015.
From WHO Global Tuberculosis Report 2016; with permission.
Only recently have systematic attempts been made to quantify the disease burden of TB in children on a global scale. In response to increasing attention and demand, the WHO published pediatric-specific disease estimates for the first time in 2012, reporting approximately 500,000 cases of TB among children younger than 15 years of age.6 However, these were based on extrapolations from adult data, which were heavily weighted on sputum-smear positivity and did not incorporate sufficient adjustments to account for under-detection and under-reporting in pediatric populations.7 Subsequent modifications to the mathematical models have been incorporated, relying more on transmission dynamics, household demographics, and population-based age structures.8–10 As a result, the WHO estimates for pediatric TB in the ensuing years doubled: in 2015, the children comprised approximately 1 million (10%) of the 10.4 million incident cases.3 This immense variation in estimated disease burden highlights the challenges in detecting and reporting pediatric TB cases and stresses the importance in resolving these gaps to inform resource allocation and public health efforts.
Similarly, the estimated pediatric mortality burden from TB is poorly quantified. The WHO estimated 210,000 deaths from TB among children in 2015, 24% of whom were co-infected with HIV.3 In many high-burden regions, deaths from TB are often generalized as being due to pneumonia or meningitis. In a recent systematic review from the WHO’s and UNICEF’s Child Health Epidemiology Reference Group (CHERG) using vital registration and verbal autopsy data, TB was not included as a specific etiology of under-5 mortality.11 However, it has long been known that TB disproportionately affects young children:
mortality from TB is highest among the very young (0–4 years of age) compared to any other age group.12
infants and young children carry a higher risk of disseminated disease, including TB meningitis and miliary TB, each with associated mortality.13–15
The global TB community is working “toward zero TB deaths in children” 16 and meeting this goal relies on coordinated efforts to improve awareness, diagnosis, reporting and treatment outcomes.
Pathogenesis
Mycobacterium tuberculosis complex organisms, which include M. africanum, M. bovis, M. bovis BCG, M. canetti (and others which do not typically affect humans), are transmitted via the respiratory route when small (1–5 micrometer) infected droplet nuclei are aerosolized from people with pulmonary or laryngeal TB and inhaled into the alveoli by close contacts.17 There are many unknown details about the biological events that transpire during early stages of exposure and infection. Alveolar macrophages and dendritic cells are among the first cells to detect and ingest the mycobacteria. Along with additional innate antimicrobial mediators, they trigger a cascade of innate immunologic events to activate complement pathways, stimulate chemokine and pro-inflammatory cytokine production including interferon-gamma (IFN- γ) and tumor necrosis factor-alpha (TNF-α), and augment opsonization and phagocytosis in order to clear or control the infection.18 If this fails or is insufficient, the mycobacteria can invade the lung parenchyma. Adaptive immune responses are triggered when macrophages and dendritic cells present M. tuberculosis antigens to T-cells, including Th-1 type CD4+ T- cells, CD8+ cytotoxic T-cells, and gamma-delta (γδ) T-cells which further potentiate key cytokine secretion for M. tuberculosis control.19 Historically, B-cells were not considered to be an important component in TB immunopathogenesis, however there is growing evidence to suggest that B-cells mediate protection through antigen presentation, cytokine production, and antibody production via interactions with T-cells.20,21 Ultimately, we rely on measuring the T-cell mediated immune responses as an indication of TB infection, through the IFN-γ release assays (IGRAs) and the tuberculin skin test (TST).
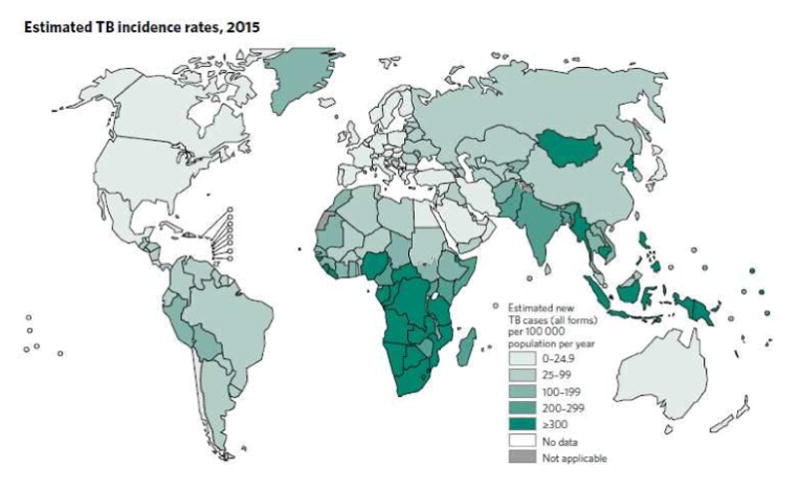
Effective immune responses may lead to complete clearance of the pathogen, or containment in a quiescent state. Inadequate or inappropriate immune responses lead to continued replication of the pathogen with progression to pulmonary disease and possible dissemination to extra-pulmonary sites. Age and immunologic function are the biggest drivers of progressive disease. Infants and young children have the highest propensity to progress to active, disseminated disease due to the age-related deficiencies and/or down-regulation of key immunologic factors (see Figure 2).22,23 However, it is important to note that the risk of TB disease follows a bimodal pattern. While children between the ages of 5–10 years are at the lowest risk of progressing to disease, adolescents carry higher risks including reactivation of M. tuberculosis manifesting as active disease after years of successful containment.5,23
Figure 2.
Age related risks of TB disease after primary infection in the pre-chemotherapy era.
Additional factors that affect progression of disease include:
time since exposure, with greatest risk in the first 2 years after exposure
mycobacterial burden of exposure,
the virulence of the mycobacterial strain.
Host and environmental risk factors associated with progression include:
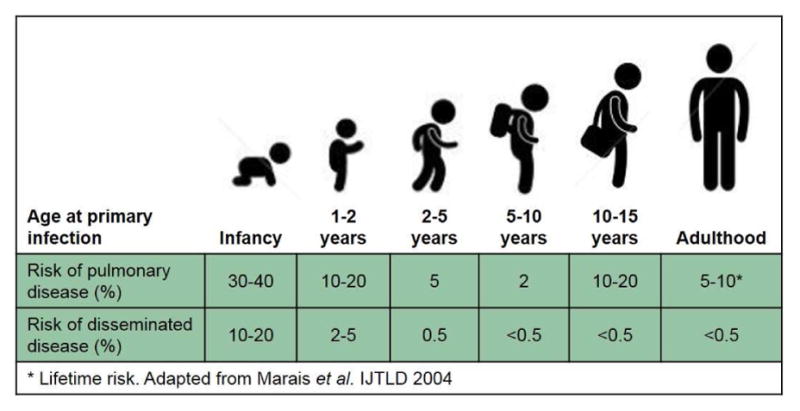
Natural history of disease
TB is often oversimplified as having two possible clinical states: latent TB infection (LTBI) or active disease. However, as we move toward global targets to end the TB epidemic by 2030,30 there is a renewed appreciation for the historically described spectrum of manifestations which include pathogen clearance, dormant states of infection, subclinical disease, non-severe disease and severe TB disease.31,32 (see Figure 3) A better understanding of the spectrum of TB may improve resource allocation by focusing treatment and prevention efforts on susceptible individuals, thereby moving us closer toward TB control.
Figure 3.
Spectrum of TB in children.
Immediately after exposure and primary infection from an infectious TB case, there are generally no clinical or radiologic manifestations. It may be possible for humans to clear the pathogen after close contact with infectious sources.31 Clearance of the pathogen may be attributed to genetic “resistance” to infection, or other innate immune responses.33–36 If clearance occurs through T-cell independent mechanisms, IGRA and TST results should be negative. However, clearance may also occur through T-cell mediated immunity, which would manifest with positive IGRA/TST results. This latter phenomenon may explain why some people who are diagnosed as having latent TB infection (LTBI) ultimately have a low likelihood of ever developing active TB disease.31 However, how often this truly occurs in young children is not well documented.
As per pediatrician Arvid Wallgren’s historical description of the timetable of primary tuberculosis in children, it takes approximately 4–12 weeks after exposure for the adaptive immune responses to reflect evidence of TB infection, as measured by the IGRA/TST.37 During this period, there is local extension of the infection into the lung parenchyma, termed a Ghon focus, which can manifest clinically with mild, self-limiting and non-specific respiratory symptoms, including hypersensitivity reactions such as fevers, erythema nodosum, or phlyctenular conjunctivitis.23 As demonstrated in contact tracing reports, chest radiographs at this time may also demonstrate transient lymphadenopathy in the hilar and/or mediastinal regions; together with the Ghon focus this is termed a Ghon complex.38,39 From the regional lymph nodes, the mycobacteria are capable of traversing through the lymphatics into the systemic circulation, allowing for occult hematogenous spread and seeding of distant sites which may serve as a nidus for future disease. Yet, in the absence of effective immunologic control, this stage confers great risk of developing miliary TB and TB meningitis, although the exact pathogenesis of the latter is still under debate.40,41 In the ensuing ~6 months, intrathoracic lymph node enlargement and/or parenchymal disease may develop; older children may develop pleural effusions. These manifestations can be associated with respiratory and systemic symptoms. In some children, calcifications may develop approximately 1–2 years after primary infection; this is associated with a reduced risk of further disease progression.37,38 However, late manifestations of TB, including reactivation of TB within the lungs or at extrapulmonary sites, do occur.42
Clinical manifestations of disease
M. tuberculosis is capable of infecting nearly any organ (Table 1), however the most common clinical manifestations of disease are found within the thoracic cavity and peripheral lymph nodes.
Table 1.
Extrathoracic manifestation of TB disease
| Organ System | Potential disease manifestations |
|---|---|
| Central nervous system | Meningitis; tuberculoma; stroke |
| Ocular | Uveitis; phlyctenular conjunctivitis* |
| Otic/nasopharyngeal | Chronic suppurative otitis media; mastoiditis; tonsillitis; laryngeal involvement |
| Cardiac | Pericardial effusion; secondary right sided heart failure from extensive pulmonary disease and bronchiectasis. |
| Abdominal | Peritonitis; enteritis; involvement of lymph nodes; visceral involvement (especially liver and spleen) |
| Genitourinary† | Genital involvement possible for females>males; Interstitial nephritis; glomerulonephritis |
| Osteoarticular | Vertebral osteomyelitis; other skeletal involvement possible, especially tubular and flat bones; dactylitis; joint effusions/arthritis (less common); reactive arthritis (Poncet’s Disease). |
| Lymphatic | Peripheral (cervical > axillary > inguinal region) or central adenopathy |
| Cutaneous | Numerous manifestations from exogenous infection (chancres, warts) or endogenous spread (lupus vulgaris,pustulonodular lesions); Erythema induratum of Bazin |
hypersensitivity reaction;
uncommonly seen in young children due to long latency for reactivation in these organs
Common intrathoracic manifestations include mediastinal or hilar lymphadenopathy and pulmonary parenchymal lesions. Less commonly, the pleura or pericardium become involved. Isolated intrathoracic lymphadenopathy may be detected early after infection and is often not associated with symptoms. However, as these inflammatory reactions progress and lymph nodes enlarge, complications can ensue:
Small airways may become obstructed or compressed which may manifest with cough, wheezing or dyspnea.
Lymph nodes may caseate or necrose, erupting into the airway leading to bronchopneumonia and manifesting with cough, dyspnea, malaise and fever.
Hypersensitivity reactions may also occur, including pleural effusions which may provoke symptoms of chest pain, fever and reduced endurance.
The symptomatology is largely non-specific and thus can easily be confused with bacterial or viral etiologies of pneumonia. The classic description of a chronic cough may apply, but it is also important to recognize that young children have a propensity to progress rapidly to disease after exposure. Indeed, TB as an etiology of acute pneumonia among young, immunocompromised children is under-recognized.43 Systematic reviews report M. tuberculosis as a culture-confirmed pathogen in 7.5–12% of children under 5 years of age with pneumonia from TB-endemic areas.43,44 This is a notable finding given the paucibacillary nature of pediatric TB disease.
Extra-thoracic manifestations comprise ~20–40% of TB cases, although concomitant overlap with pulmonary disease can occur. The most commonly involved extra-thoracic sites are the peripheral lymph nodes or the central nervous system. Lymphadenitis often manifests in the cervical regions with enlarged, painless lymph nodes. Examination typically reveals a solitary rubbery node that lacks erythema or warmth. Over time, adjacent nodes may become palpable and the lesion grows matted and fixed; sinus fistulas may also form. In low-TB-incidence countries, other non-tuberculous mycobacteria (NTM) are capable of manifesting with lymphadenitis.
Disease within the central nervous system represents the most serious complication of TB, with significant morbidity or mortality occurring in approximately 50% of cases.45,46 Contributing to the devastating consequences of disease are the sub-acute onset and non-specific systemic symptoms during the early stages, such as irritability, fever, anorexia, and occasionally, focal respiratory or gastrointestinal symptoms. As disease progresses, findings of meningitis become apparent including vomiting, altered consciousness, convulsions, meningismus, cranial nerve palsies, or signs of raised intracranial pressure. Complications include hydrocephalus, cerebrovascular disease such as stroke and vasculitis, tuberculoma, and coma.47 Early diagnosis is the key to improved outcomes, but in the absence of reliable diagnostic tools, a high index of clinical suspicion is required, not only in TB-endemic regions but also in low-TB-burden countries with migrant populations.48
Disease in special populations
Perinatal infection from M. tuberculosis is thought to be a rare but serious event. It can occur from hematogenous spread of the bacilli from an infected mother through the placenta which typically results in primary infection of the fetal liver, or directly into the amniotic fluid with subsequent aspiration and infection of the lungs or gastrointestinal tract.49 TB of the reproductive organs was historically associated with infertility, however direct extension of TB to the uterus is increasingly being described as a mechanism for congenital TB in the era of improved assistive reproductive technology.50 Additionally, respiratory transmission may occur post-natally. Symptoms of disease are non-specific and are indistinguishable from bacterial sepsis or congenital viral infections, and may manifest as early as 2–3 weeks of age. A high clinical index of suspicion is required for this relatively uncommon event.
Adolescence represents another uniquely susceptible time for TB progression (Figure 2). Disease presentation can digress from typical childhood manifestations to include aspects of adult-type TB, including cavitary pulmonary TB or extra-thoracic manifestations that are associated with longer incubation periods, such as genitourinary TB.51 Healthcare providers should inquire about concurrent substance abuse, as this may call for additional counseling or monitoring that is not routinely conducted for younger children. Anxiety and depression may be common, exacerbated by infection control and contact investigation procedures as well as stigma associated with the diagnosis.52 These factors, combined with behavioral aspects, add to the vulnerabilities in this population and may lead to poor outcomes including challenges related to adherence and follow up.53,54
Across the world, HIV infection is the strongest risk factor for TB. Children experience indirect as well as direct effects of HIV: children who are HIV-uninfected but exposed to others who are HIV-positive also bear an increased risk of TB infection and disease.55,56 Those who are infected with HIV have impaired cell mediated immunity to control TB infection, conferring a higher risk of progression to active TB disease after exposure, of reactivation of latent infection, and of severe disease manifestations.57 Timely recognition of HIV and initiation of anti-retroviral therapy (ART) is essential for immune restoration and improved TB control; also important are repeated screening for TB in the early months of ART, as well as provision of isoniazid preventive therapy (in all children who have been ruled out for active TB) and co-trimoxazole therapy.58–61
Diagnosis
There are various challenges in confirming the diagnosis of TB in children which stem from the subtle or non-specific radiographic findings and the paucibacillary nature of disease.16,62,63 To date, an accurate diagnostic test for pediatric TB does not exist. Thus, it is essential for clinicians to note that TB is often a clinical diagnosis and given the poor sensitivity of our current diagnostic tools, a negative test does not rule out disease in children.
Confirmatory tests
A confirmatory diagnosis relies on detecting the pathogen directly; alternative approaches include detecting the histopathologic or host immune response to the pathogen. Direct pathogen-based tests include TB culture, nucleic acid amplification tests (NAAT), and smear microscopy:
-
Mycobacterial culture is the gold-standard test for TB, with a limit of detection (LOD) of ~10–100 colony forming units per milliliter (CFU/mL) in solid or liquid culture media.
The sensitivity is generally only 7–40% in children due to the paucibacillary nature of disease in this sub-population.1,64–66
The time required (up to 6 weeks for positive growth) is sometimes too lengthy to be clinically useful; but this is a necessary step in order to conduct phenotypic drug susceptibility testing.
When M. tuberculosis is isolated, it is important to perform drug-sensitivity testing against first-line TB drugs as a start, and against second-line TB drugs as needed.
-
Although smear microscopy and NAATs are much faster than culture, these assays are also contingent upon the bacillary burden and the sensitivity is even further reduced.67–71
Smear microscopy has a LOD of ~10,000 CFU/mL, conferring limited utility in pediatric TB cases.
The newer GeneXpert MTB/RIF (Cepheid, Sunnyvale, California USA) assay is a NAAT that detects M. tuberculosis DNA and concomitant resistance to Rifampicin with a LOD of 131 CFU/mL.72 The hands-free and automated nature of this rapid cartridge-based test has contributed to its wide spread implementation throughout high-TB burden settings.73
GeneXpert only has a pooled sensitivity of ~66% compared to TB culture in pediatric populations.2
Of course, collecting a deep respiratory specimen for TB culture from a young child brings added challenges. Most children <7 years do not have the tussive force and/or the oromotor coordination to produce a good-quality expectorated sputum specimen on command. Semi-invasive techniques such as gastric aspiration/lavage or sputum induction with or without nasopharyngeal aspiration may be required. With procedural training, sputum induction provides at least similar microbiologic yield compared to gastric aspiration.64,65,74 An alternative method of obtaining respiratory specimens includes the use of the string test in which a gelatin capsule containing a nylon string is swallowed and later retrieved for TB culture. The procedure is tolerable for children who can swallow and culture yield seems comparable to sputum induction in preliminary studies.75,76 Detecting the organism in stool may be an option where GeneXpert MTB/RIF testing is available.77,78
In extrapulmonary TB, site-specific specimens for TB culture are often collected, such as cerebrospinal fluid (CSF), lymph node aspirates and other tissue specimens. However, the yield is variable. Mycobacterial blood cultures seem to be of limited yield in children compared to adults.64,79–81 Histopathologic diagnosis is more commonly pursued in extra-pulmonary TB. The overall yield is not well characterized, and is somewhat dependent upon the experience of the proceduralist and pathologist; sensitivity and specificity may be hindered by other granulomatous processes.82
Screening tests
Host immune responses can be harnessed to determine immunologic evidence of exposure to M. tuberculosis. However, the currently available immunodiagnostics are not able to distinguish between latent infection and active disease. The TST is the oldest screening test for TB and works by measuring a delayed-type hypersensitivity reaction to various mycobacterial antigens within the purified protein derivative (PPD). It is well recognized that this test suffers from lack of sensitivity and specificity.83 In order to minimize the false-negative and false-positive rates, different cutoffs are used to interpret the findings based on epidemiologic (i.e. recent exposure) and individual (i.e. host immune response, age) factors.
The newer IGRAs address the issue of specificity cross reactivity by using particular antigens that are absent from M. bovis BCG and many other NTM species; this confers a performance advantage among BCG-vaccinated children. Both of the two commonly used commercial assays, the T-Spot.TB (Oxford Immunotec, Abingdon, UK) and the QuantiFERON-TB Gold (Qiagen, Hilden, Germany), require a whole blood sample to measure IFN-γ secretion from CD4+ T-cells in response to ex-vivo stimulation with RD1 antigens; neither is preferred over the other.84 They rely upon intact cell mediated immunity, which may hinder performance in very young children and/or children co-infected with HIV, two populations who would benefit most from an accurate diagnostic assay.85 Advisory bodies have recommended caution when using IGRAs in children <5 years of age due to a lack of data and favor the use of the TST.86,87 However, increasing experience suggests potential utility in young children, particularly those between 2–5 years of age.84,88
Overall, when using these screening tests it is helpful to note that:
Each test has inherent limitations leading to false-positives or false-negatives.
Routine screening should be avoided in favor of targeted testing among children with at least one risk factor for TB.
Neither test can discriminate between latent infection and active disease
Among symptomatic children, a negative test (TST or IGRA) never rules out TB disease.89
Clearly, improved diagnostics are urgently needed for children.63 Newer methods that have been evaluated in limited pediatric studies have focused on non-respiratory specimens including blood based assays, such as the T-cell activation marker (TAM) assay which harnesses host immune responses as a diagnostic biomarker,90 and transcriptomic studies which hold promise as a diagnostic and prognostic marker.91–93 Other biomarkers which have shown promise in adult populations, such as the Antibodies in Lymphocyte Supernatant Assay (ALS) and the urinary lipoarabinomannan (LAM) assay, have not shown consistent results in pediatric populations.94–98 Using feasibly obtained specimens, such as urine, would confer a notable advantage as a point-of-care diagnostic test, and further work in this area is warranted.
Imaging
Given the lack of accurate diagnostic assays, imaging studies serve an important role in the diagnosis of intra-thoracic TB. Chest radiographs are the most commonly used method. However, the findings can be relatively non-specific and inter-observer variation may exist, even among experienced clinicians.99,100 Suggestive findings include:
intra-thoracic lymphadenopathy, for which a lateral film may have additive yield101
complications such as airway compression
air-space disease, which may be indistinguishable from other causes of pneumonia
and less commonly, miliary nodules or cavitation.
Computer aided detection for pulmonary TB has shown initial promise among adults, although performance is reduced in smear-negative (i.e. paucibacillary) disease;102 this technology has not yet been validated among children. Other modalities such as dose-reduced CT scans, FDG-PET imaging, and MRI may provide additional detail, but are not routinely used in children.
Management
Treatment regimens for pediatric TB have been largely adapted from adults. Because of the slow growth of mycobacteria and the dormant state of many bacilli, the duration of treatment is quite lengthy. Additional considerations include:
treatment of latent TB requires 3–9 months, depending on whether a mono-therapy or combination therapy approach is used.
the “short course” regimen for active TB requires 6 months
more severe forms of TB including TB meningitis and drug-resistant TB require 12+ months of therapy.
Traditional treatment of LTBI typically includes 9-months of isoniazid daily with pyridoxine (for breastfeeding infants, adolescents, and others with low pyridoxine intake). The newer regimen of isoniazid and rifapentine weekly for 12 doses is safe and effective in children aged 2–17 years of age and may improve adherence rates.103 However, it is currently only available through directly observed therapy (DOT) programs, which may not be routinely available. In attempts to improve completion rates, some experts have increasingly used the 4-month regimen of rifampin, which had typically been recommended for LTBI treatment among those exposed to isoniazid-resistant strains.104,105
The standard approach to drug-susceptible TB relies on combination drug therapy with isoniazid, rifampin, pyrazinamide and ethambutol for the first two months, followed by four months of isoniazid and rifampin. Directly observed therapy (DOT), typically through a public health department, is recommended in order to assist with delivery of medications which may be un-palatable, improve adherence, monitor for toxicity, and provide additional support. However, this brings added costs and may not be routinely available.
If drug resistance is confirmed or presumed through an epidemiologic link, treatment should be based upon drug susceptibility results (using the index case’s results when appropriate). A minimum of four active drugs should be used, including an injectable agent. Because of variable efficacy of some second-line drugs, and increased risks of toxicities, treatment decisions should be made in conjunction with a specialist. 86 Close monitoring is required to ensure culture conversion, clinical resolution, and minimize side effects and long-term sequelae.106
For the first time in decades, there are newer anti-TB drugs available and in the pipelines. Including children in pre-clinical and clinical pharmacokinetic studies and efficacy trials is imperative to meeting the goals for global TB control.107,108 Equally urgent is the need for child-friendly first- and second-line drugs which are palatable and easily administered.
Prevention
TB is a preventable condition that requires coordinated systematic efforts. A child with active TB represents a sentinel event, typically reflecting ongoing transmission in the community. Infection control measures conferring great strides in TB control include household contact investigation of index cases and treatment for LTBI, and these strategies are increasingly being adopted in high-TB-burden settings.30,109 In addition to these public health efforts, primary care providers have an important role in TB control by conducting annual targeted LTBI screening.86,110
For decades, the BCG vaccine has been widely used to protect against childhood TB. Although the vaccine is not perfect, it is estimated that one year of BCG vaccination prevents over 117,000 deaths per pediatric (<15 years of age) birth cohort.111,112 However production issues have led to sizeable shortfalls in supply since 2013, which have not completely been resolved. Modelling studies have estimated that the recent shortages may contribute to nearly 20,000 excess childhood deaths from TB.112
The development of new and improved TB vaccines is hindered by insufficient understanding of the correlates of protection. As was realized after the MVA85A TB vaccine trial among human infants, experimental animal models have been unreliable in predicting responses in humans.113 However, various TB vaccine strategies are under study, including modifications to replace the current BCG, novel vaccines designed to boost responses among BCG recipients, and therapeutic vaccines designed to aid those undergoing TB treatment.114
Summary
TB remains a major threat to child health worldwide. Global migration requires that clinicians in low-incidence countries maintain awareness for TB, since timely recognition is key, especially in young children. We are at a turning point in which increased advocacy has stimulated major efforts toward recognition and control of TB in children. However, there is much to be done in order to meet the ambitious programmatic targets, including widespread uptake of proven prevention efforts, and development of newer strategies including effective vaccines. Dedicated research and development are need for accurate, child-friendly, and fieldable diagnostics. Pediatric-specific studies are necessary in order to define the best approach to childhood TB using tolerable drugs, especially for drug-resistant TB. All of this requires coordinated efforts, and adequate funding. The momentum must continue to end the neglect of childhood TB.
Key Points.
Although TB is a preventable condition, it remains a major cause of childhood morbidity and mortality worldwide.
Young children are at especially high risk of progressing to active TB after exposure.
Because an accurate diagnostic test for TB in children does not exist, making a confirmatory diagnosis is challenging and requires clinical acumen.
TB treatment is lengthy, and child-friendly drug formulations are urgently needed.
Footnotes
Disclosure statement: TAT reports no financial conflicts of interest. TAT is supported by K23 AI097197
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Starke JR. Pediatric tuberculosis: time for a new approach. Tuberculosis (Edinb) 2003;83(1– 3):208–212. doi: 10.1016/s1472-9792(02)00088-4. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: Xpert MTB/RIF assay for the diagnosis of pulmonary and extrapulmonary TB in adults and children. Policy update. Geneva: World Health Organization; 2013. [PubMed] [Google Scholar]
- 3.World Health Organization. Global tuberculosis report 2016. Geneva: World Health Organization; 2016. [Google Scholar]
- 4.CDC. [Accessed November 30, 2016];Reported Tuberculosis in the United States, 2014. 2015 http://www.cdc.gov/tb/statistics/reports/2014.
- 5.Winston CA, Menzies HJ. Pediatric and adolescent tuberculosis in the United States, 2008–2010. Pediatrics. 2012;130(6):e1425–1432. doi: 10.1542/peds.2012-1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. Global tuberculosis report 2012 (in IRIS) Geneva: World Health Organization; 2012. [Google Scholar]
- 7.Seddon JA, Jenkins HE, Liu L, et al. Counting children with tuberculosis: why numbers matter. Int J Tuberc Lung Dis. 2015;19(Suppl 1):9–16. doi: 10.5588/ijtld.15.0471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dodd PJ, Gardiner E, Coghlan R, Seddon JA. Burden of childhood tuberculosis in 22 high-burden countries: a mathematical modelling study. Lancet Glob Health. 2014;2(8):e453–459. doi: 10.1016/S2214-109X(14)70245-1. [DOI] [PubMed] [Google Scholar]
- 9.Jenkins HE, Tolman AW, Yuen CM, et al. Incidence of multidrug-resistant tuberculosis disease in children: systematic review and global estimates. Lancet. 2014;383(9928):1572–1579. doi: 10.1016/S0140-6736(14)60195-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Bank. [Accessed November 30, 2016];Population ages 0–14. 2015 http://data.worldbank.org/indicator/SP.POP.0014.TO.ZS.
- 11.Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of child mortality in 2000–13, with projections to inform post-2015 priorities: an updated systematic analysis. Lancet. 2015;385(9966):430–440. doi: 10.1016/S0140-6736(14)61698-6. [DOI] [PubMed] [Google Scholar]
- 12.Frost WH. The age selection of mortality from tuberculosis in successive decades. 1939. Am J Epidemiol. 1995;141(1):4–9. doi: 10.1093/oxfordjournals.aje.a117343. discussion 3. [DOI] [PubMed] [Google Scholar]
- 13.Karande S, Gupta V, Kulkarni M, Joshi A. Prognostic clinical variables in childhood tuberculous meningitis: an experience from Mumbai, India. Neurol India. 2005;53(2):191–195. doi: 10.4103/0028-3886.16407. discussion 195–196. [DOI] [PubMed] [Google Scholar]
- 14.van Toorn R, Springer P, Laubscher JA, Schoeman JF. Value of different staging systems for predicting neurological outcome in childhood tuberculous meningitis. Int J Tuberc Lung Dis. 2012;16(5):628–632. doi: 10.5588/ijtld.11.0648. [DOI] [PubMed] [Google Scholar]
- 15.Sharma SK, Mohan A, Sharma A, Mitra DK. Miliary tuberculosis: new insights into an old disease. Lancet Infect Dis. 2005;5(7):415–430. doi: 10.1016/S1473-3099(05)70163-8. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. Roadmap for childhood tuberculosis: towards zero deaths. Geneva, Switzerland: 2013. [Google Scholar]
- 17.Fennelly KP, Martyny JW, Fulton KE, Orme IM, Cave DM, Heifets LB. Cough-generated aerosols of Mycobacterium tuberculosis: a new method to study infectiousness. Am J Respir Crit Care Med. 2004;169(5):604–609. doi: 10.1164/rccm.200308-1101OC. [DOI] [PubMed] [Google Scholar]
- 18.Basu Roy R, Whittaker E, Kampmann B. Current understanding of the immune response to tuberculosis in children. Curr Opin Infect Dis. 2012;25(3):250–257. doi: 10.1097/QCO.0b013e3283529af9. [DOI] [PubMed] [Google Scholar]
- 19.Lewinsohn DA, Gennaro ML, Scholvinck L, Lewinsohn DM. Tuberculosis immunology in children: diagnostic and therapeutic challenges and opportunities. Int J Tuberc Lung Dis. 2004;8(5):658– 674. [PubMed] [Google Scholar]
- 20.Chan J, Mehta S, Bharrhan S, et al. The role of B cells and humoral immunity in Mycobacterium tuberculosis infection. Semin Immunol. 2014;26(6):588–600. doi: 10.1016/j.smim.2014.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rao M, Valentini D, Poiret T, et al. B in TB: B Cells as Mediators of Clinically Relevant Immune Responses in Tuberculosis. Clin Infect Dis. 2015;61(Suppl 3):S225–234. doi: 10.1093/cid/civ614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Vanden Driessche K, Persson A, Marais BJ, Fink PJ, Urdahl KB. Immune vulnerability of infants to tuberculosis. Clin Dev Immunol. 2013;2013:781320. doi: 10.1155/2013/781320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marais BJ, Gie RP, Schaaf HS, et al. The clinical epidemiology of childhood pulmonary tuberculosis: a critical review of literature from the pre-chemotherapy era. Int J Tuberc Lung Dis. 2004;8(3):278–285. [PubMed] [Google Scholar]
- 24.Ekim M, Tumer N, Bakkaloglu S. Tuberculosis in children undergoing continuous ambulatory peritoneal dialysis. Pediatr Nephrol. 1999;13(7):577–579. doi: 10.1007/s004670050660. [DOI] [PubMed] [Google Scholar]
- 25.Munteanu M, Cucer F, Halitchi C, Muller R, Brumariu O. The TB infection in children with chronic renal diseases [abstract only] Rev Med Chir Soc Med Nat Iasi. 2006;110(2):309–313. [PubMed] [Google Scholar]
- 26.Jaganath D, Mupere E. Childhood tuberculosis and malnutrition. J Infect Dis. 2012;206(12):1809– 1815. doi: 10.1093/infdis/jis608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chisti MJ, Ahmed T, Shahid AS, et al. Sociodemographic, Epidemiological, and Clinical Risk Factors for Childhood Pulmonary Tuberculosis in Severely Malnourished Children Presenting With Pneumonia: Observation in an Urban Hospital in Bangladesh. Glob Pediatr Health. 2015;2 doi: 10.1177/2333794X15594183. 2333794x15594183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Patra S, Sharma S, Behera D. Passive smoking, indoor air pollution and childhood tuberculosis: a case control study. Indian J Tuberc. 2012;59(3):151–155. [PubMed] [Google Scholar]
- 29.Jafta N, Jeena PM, Barregard L, Naidoo RN. Childhood tuberculosis and exposure to indoor air pollution: a systematic review and meta-analysis. Int J Tuberc Lung Dis. 2015;19(5):596–602. doi: 10.5588/ijtld.14.0686. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization. The End TB Strategy. Geneva, Switzerland: 2015. [Google Scholar]
- 31.Dheda K, Schwander SK, Zhu B, van Zyl-Smit RN, Zhang Y. The immunology of tuberculosis: from bench to bedside. Respirology. 2010;15(3):433–450. doi: 10.1111/j.1440-1843.2010.01739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Barry CE, 3rd, Boshoff HI, Dartois V, et al. The spectrum of latent tuberculosis: rethinking the biology and intervention strategies. Nat Rev Microbiol. 2009;7(12):845–855. doi: 10.1038/nrmicro2236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cobat A, Gallant CJ, Simkin L, et al. Two loci control tuberculin skin test reactivity in an area hyperendemic for tuberculosis. J Exp Med. 2009;206(12):2583–2591. doi: 10.1084/jem.20090892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thye T, Owusu-Dabo E, Vannberg FO, et al. Common variants at 11p13 are associated with susceptibility to tuberculosis. Nat Genet. 2012;44(3):257–259. doi: 10.1038/ng.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cobat A, Poirier C, Hoal E, et al. Tuberculin skin test negativity is under tight genetic control of chromosomal region 11p14–15 in settings with different tuberculosis endemicities. J Infect Dis. 2015;211(2):317–321. doi: 10.1093/infdis/jiu446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fox GJ, Orlova M, Schurr E. Tuberculosis in Newborns: The Lessons of the "Lubeck Disaster" (1929–1933) PLoS Pathog. 2016;12(1):e1005271. doi: 10.1371/journal.ppat.1005271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wallgren A. The time-table of tuberculosis. Tubercle. 1948;29(11):245–251. doi: 10.1016/s0041-3879(48)80033-4. [DOI] [PubMed] [Google Scholar]
- 38.Davies PD. The natural history of tuberculosis in children. A study of child contacts in the Brompton Hospital Child Contact Clinic from 1930 to 1952. Tubercle. 1961;42(Suppl):1–40. [PubMed] [Google Scholar]
- 39.Marais BJ, Gie RP, Schaaf HS, et al. A proposed radiological classification of childhood intra-thoracic tuberculosis. Pediatr Radiol. 2004;34(11):886–894. doi: 10.1007/s00247-004-1238-0. [DOI] [PubMed] [Google Scholar]
- 40.Donald PR, Schaaf HS, Schoeman JF. Tuberculous meningitis and miliary tuberculosis: the Rich focus revisited. J Infect. 2005;50(3):193–195. doi: 10.1016/j.jinf.2004.02.010. [DOI] [PubMed] [Google Scholar]
- 41.Janse van Rensburg P, Andronikou S, van Toorn R, Pienaar M. Magnetic resonance imaging of miliary tuberculosis of the central nervous system in children with tuberculous meningitis. Pediatr Radiol. 2008;38(12):1306–1313. doi: 10.1007/s00247-008-1028-1. [DOI] [PubMed] [Google Scholar]
- 42.Perez-Velez CM, Marais BJ. Tuberculosis in children. N Engl J Med. 2012;367(4):348–361. doi: 10.1056/NEJMra1008049. [DOI] [PubMed] [Google Scholar]
- 43.Chisti MJ, Ahmed T, Pietroni MA, et al. Pulmonary tuberculosis in severely-malnourished or HIV-infected children with pneumonia: a review. J Health Popul Nutr. 2013;31(3):308–313. doi: 10.3329/jhpn.v31i3.16516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Oliwa JN, Karumbi JM, Marais BJ, Madhi SA, Graham SM. Tuberculosis as a cause or comorbidity of childhood pneumonia in tuberculosis-endemic areas: a systematic review. Lancet Respir Med. 2015;3(3):235–243. doi: 10.1016/S2213-2600(15)00028-4. [DOI] [PubMed] [Google Scholar]
- 45.Chiang SS, Khan FA, Milstein MB, et al. Treatment outcomes of childhood tuberculous meningitis: a systematic review and meta-analysis. Lancet Infect Dis. 2014;14(10):947–957. doi: 10.1016/S1473-3099(14)70852-7. [DOI] [PubMed] [Google Scholar]
- 46.Bang ND, Caws M, Truc TT, et al. Clinical presentations, diagnosis, mortality and prognostic markers of tuberculous meningitis in Vietnamese children: a prospective descriptive study. BMC Infect Dis. 2016;16(1):573. doi: 10.1186/s12879-016-1923-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.van Toorn R, Solomons R. Update on the diagnosis and management of tuberculous meningitis in children. Semin Pediatr Neurol. 2014;21(1):12–18. doi: 10.1016/j.spen.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 48.van Well GT, Paes BF, Terwee CB, et al. Twenty years of pediatric tuberculous meningitis: a retrospective cohort study in the western cape of South Africa. Pediatrics. 2009;123(1):e1–8. doi: 10.1542/peds.2008-1353. [DOI] [PubMed] [Google Scholar]
- 49.Peng W, Yang J, Liu E. Analysis of 170 cases of congenital TB reported in the literature between 1946 and 2009. Pediatr Pulmonol. 2011;46(12):1215–1224. doi: 10.1002/ppul.21490. [DOI] [PubMed] [Google Scholar]
- 50.Flibotte JJ, Lee GE, Buser GL, et al. Infertility, in vitro fertilization and congenital tuberculosis. J Perinatol. 2013;33(7):565–568. doi: 10.1038/jp.2012.146. [DOI] [PubMed] [Google Scholar]
- 51.Cruz AT, Hwang KM, Birnbaum GD, Starke JR. Adolescents with tuberculosis: a review of 145 cases. Pediatr Infect Dis J. 2013;32(9):937–941. doi: 10.1097/INF.0b013e3182933214. [DOI] [PubMed] [Google Scholar]
- 52.Franck C, Seddon JA, Hesseling AC, Schaaf HS, Skinner D, Reynolds L. Assessing the impact of multidrug-resistant tuberculosis in children: an exploratory qualitative study. BMC Infect Dis. 2014;14:426. doi: 10.1186/1471-2334-14-426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Blok N, van den Boom M, Erkens C, Dara M, van den Hof S. Eur Respir J. Vol. 48. England: 2016. Variation in policy and practice of adolescent tuberculosis management in the WHO European Region; pp. 943–946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Enane LA, Lowenthal ED, Arscott-Mills T, et al. Loss to follow-up among adolescents with tuberculosis in Gaborone, Botswana. Int J Tuberc Lung Dis. 2016;20(10):1320–1325. doi: 10.5588/ijtld.16.0060. [DOI] [PubMed] [Google Scholar]
- 55.Marquez C, Chamie G, Achan J, et al. Tuberculosis Infection in Early Childhood and the Association with HIV-exposure in HIV-uninfected Children in Rural Uganda. Pediatr Infect Dis J. 2016;35(5):524–529. doi: 10.1097/INF.0000000000001062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cotton MF, Slogrove A, Rabie H. Infections in HIV-exposed uninfected children with focus on sub-Saharan Africa. Pediatr Infect Dis J. 2014;33(10):1085–1086. doi: 10.1097/INF.0000000000000489. [DOI] [PubMed] [Google Scholar]
- 57.Verhagen LM, Warris A, van Soolingen D, de Groot R, Hermans PW. Human immunodeficiency virus and tuberculosis coinfection in children: challenges in diagnosis and treatment. Pediatr Infect Dis J. 2010;29(10):e63–70. doi: 10.1097/INF.0b013e3181ee23ae. [DOI] [PubMed] [Google Scholar]
- 58.Anigilaje EA, Aderibigbe SA, Adeoti AO, Nweke NO. Tuberculosis, before and after Antiretroviral Therapy among HIV-Infected Children in Nigeria: What Are the Risk Factors? PLoS One. 2016;11(5):e0156177. doi: 10.1371/journal.pone.0156177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zar HJ, Cotton MF, Strauss S, et al. Effect of isoniazid prophylaxis on mortality and incidence of tuberculosis in children with HIV: randomised controlled trial. Bmj. 2007;334(7585):136. doi: 10.1136/bmj.39000.486400.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bwakura-Dangarembizi M, Kendall L, Bakeera-Kitaka S, et al. A randomized trial of prolonged co-trimoxazole in HIV-infected children in Africa. N Engl J Med. 2014;370(1):41–53. doi: 10.1056/NEJMoa1214901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Crook AM, Turkova A, Musiime V, et al. Tuberculosis incidence is high in HIV-infected African children but is reduced by co-trimoxazole and time on antiretroviral therapy. BMC Med. 2016;14:50. doi: 10.1186/s12916-016-0593-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cuevas LE, Petrucci R, Swaminathan S. Tuberculosis diagnostics for children in high-burden countries: what is available and what is needed. Paediatr Int Child Health. 2012;32(Suppl 2):S30– 37. doi: 10.1179/2046904712Z.00000000076. [DOI] [PubMed] [Google Scholar]
- 63.Nicol MP, Gnanashanmugam D, Browning R, et al. A Blueprint to Address Research Gaps in the Development of Biomarkers for Pediatric Tuberculosis. Clin Infect Dis. 2015;61(Suppl 3):S164–172. doi: 10.1093/cid/civ613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Thomas TA, Heysell SK, Moodley P, et al. Intensified specimen collection to improve tuberculosis diagnosis in children from Rural South Africa, an observational study. BMC Infect Dis. 2014;14:11. doi: 10.1186/1471-2334-14-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zar H, Hanslo D, Apolles P, Swingler G, Hussey G. Induced sputum versus gastric lavage for microbiological confirmation of pulmonary tuberculosis in infants and young children: a prospective study. Lancet. 2005;365(9454):130–134. doi: 10.1016/S0140-6736(05)17702-2. [DOI] [PubMed] [Google Scholar]
- 66.Nicol MP, Zar HJ. New specimens and laboratory diagnostics for childhood pulmonary TB: progress and prospects. Paediatr Respir Rev. 2011;12(1):16–21. doi: 10.1016/j.prrv.2010.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nicol MP, Workman L, Isaacs W, et al. Accuracy of the Xpert MTB/RIF test for the diagnosis of pulmonary tuberculosis in children admitted to hospital in Cape Town, South Africa: a descriptive study. Lancet Infect Dis. 2011 doi: 10.1016/S1473-3099(11)70167-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zar HJ, Workman L, Isaacs W, et al. Rapid Molecular Diagnosis of Pulmonary Tuberculosis in Children Using Nasopharyngeal Specimens. Clin Infect Dis. 2012 doi: 10.1093/cid/cis598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rachow A, Clowes P, Saathoff E, et al. Increased and Expedited Case Detection by Xpert MTB/RIF Assay in Childhood Tuberculosis: A Prospective Cohort Study. Clin Infect Dis. 2012;54(10):1388– 1396. doi: 10.1093/cid/cis190. [DOI] [PubMed] [Google Scholar]
- 70.Zar HJ, Workman L, Isaacs W, Dheda K, Zemanay W, Nicol MP. Rapid diagnosis of pulmonary tuberculosis in African children in a primary care setting by use of Xpert MTB/RIF on respiratory specimens: a prospective study. Lancet Glob Health. 2013;1(2):e97–e104. doi: 10.1016/S2214-109X(13)70036-6. [DOI] [PubMed] [Google Scholar]
- 71.Detjen AK, DiNardo AR, Leyden J, et al. Xpert MTB/RIF assay for the diagnosis of pulmonary tuberculosis in children: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(6):451–461. doi: 10.1016/S2213-2600(15)00095-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Helb D, Jones M, Story E, et al. Rapid detection of Mycobacterium tuberculosis and rifampin resistance by use of on-demand, near-patient technology. J Clin Microbiol. 2010;48(1):229–237. doi: 10.1128/JCM.01463-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Lawn SD, Nicol MP. Xpert(R) MTB/RIF assay: development, evaluation and implementation of a new rapid molecular diagnostic for tuberculosis and rifampicin resistance. Future Microbiol. 2011;6(9):1067–1082. doi: 10.2217/fmb.11.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hatherill M, Hawkridge T, Zar HJ, et al. Induced sputum or gastric lavage for community-based diagnosis of childhood pulmonary tuberculosis? Arch Dis Child. 2009;94(3):195–201. doi: 10.1136/adc.2007.136929. [DOI] [PubMed] [Google Scholar]
- 75.Chow F, Espiritu N, Gilman RH, et al. La cuerda dulce--a tolerability and acceptability study of a novel approach to specimen collection for diagnosis of paediatric pulmonary tuberculosis. BMC Infect Dis. 2006;6:67. doi: 10.1186/1471-2334-6-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Nansumba M, Kumbakumba E, Orikiriza P, et al. Detection Yield and Tolerability of String Test for Diagnosis of Childhood Intrathoracic Tuberculosis. Pediatr Infect Dis J. 2016;35(2):146–151. doi: 10.1097/INF.0000000000000956. [DOI] [PubMed] [Google Scholar]
- 77.Marcy O, Ung V, Goyet S, et al. Performance of Xpert MTB/RIF and Alternative Specimen Collection Methods for the Diagnosis of Tuberculosis in HIV-Infected Children. Clin Infect Dis. 2016;62(9):1161–1168. doi: 10.1093/cid/ciw036. [DOI] [PubMed] [Google Scholar]
- 78.Banada PP, Naidoo U, Deshpande S, et al. A Novel Sample Processing Method for Rapid Detection of Tuberculosis in the Stool of Pediatric Patients Using the Xpert MTB/RIF Assay. PLoS One. 2016;11(3):e0151980. doi: 10.1371/journal.pone.0151980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pavlinac PB, Lokken EM, Walson JL, Richardson BA, Crump JA, John-Stewart GC. Mycobacterium tuberculosis bacteremia in adults and children: a systematic review and meta-analysis. Int J Tuberc Lung Dis. 2016;20(7):895–902. doi: 10.5588/ijtld.15.0773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Heysell SK, Thomas TA, Gandhi NR, et al. Blood cultures for the diagnosis of multidrug-resistant and extensively drug-resistant tuberculosis among HIV-infected patients from rural South Africa: a cross-sectional study. BMC Infectious Diseases. 2010;10:344. doi: 10.1186/1471-2334-10-344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gray KD, Cunningham CK, Clifton DC, et al. Prevalence of mycobacteremia among HIV-infected infants and children in northern Tanzania. Pediatr Infect Dis J. 2013;32(7):754–756. doi: 10.1097/INF.0b013e318286957f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fukunaga H, Murakami T, Gondo T, Sugi K, Ishihara T. Sensitivity of acid-fast staining for Mycobacterium tuberculosis in formalin-fixed tissue. Am J Respir Crit Care Med. 2002;166(7):994–997. doi: 10.1164/rccm.2111028. [DOI] [PubMed] [Google Scholar]
- 83.Dunn JJ, Starke JR, Revell PA. Laboratory Diagnosis of Mycobacterium tuberculosis Infection and Disease in Children. J Clin Microbiol. 2016;54(6):1434–1441. doi: 10.1128/JCM.03043-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Starke JR, Byington CL, Maldonado YA, et al. Interferon-γ release assays for diagnosis of tuberculosis infection and disease in children. Pediatrics. 2014;134(6):e1763–e1773. doi: 10.1542/peds.2014-2983. [DOI] [PubMed] [Google Scholar]
- 85.Mandalakas AM, Detjen AK, Hesseling AC, Benedetti A, Menzies D. Interferon-gamma release assays and childhood tuberculosis: systematic review and meta-analysis. Int J Tuberc Lung Dis. 2011;15(8):1018–1032. doi: 10.5588/ijtld.10.0631. [DOI] [PubMed] [Google Scholar]
- 86.Kimberlin D, Brady M, Jackson M, Long S, editors. American Academy of Pediatrics. Tuberculosis. Pediatrics. 2015. Vol. 30. Elk Grove Village, IL: American Academy of Pediatrics; 2015. pp. 805–831. [Google Scholar]
- 87.Lewinsohn DM, Leonard MK, LoBue PA, et al. Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention Clinical Practice Guidelines: Diagnosis of Tuberculosis in Adults and Children. Clin Infect Dis. 2016 doi: 10.1093/cid/ciw778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Grinsdale JA, Islam S, Tran OC, Ho CS, Kawamura LM, Higashi JM. Interferon-Gamma Release Assays and Pediatric Public Health Tuberculosis Screening: The San Francisco Program Experience 2005 to 2008. J Pediatric Infect Dis Soc. 2016;5(2):122–130. doi: 10.1093/jpids/piu119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Starke JR. Interferon-gamma release assays for the diagnosis of tuberculosis infection in children. J Pediatr. 2012;161(4):581–582. doi: 10.1016/j.jpeds.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 90.Portevin D, Moukambi F, Clowes P, et al. Assessment of the novel T-cell activation marker-tuberculosis assay for diagnosis of active tuberculosis in children: a prospective proof-of-concept study. Lancet Infect Dis. 2014;14(10):931–938. doi: 10.1016/S1473-3099(14)70884-9. [DOI] [PubMed] [Google Scholar]
- 91.Anderson ST, Kaforou M, Brent AJ, et al. Diagnosis of childhood tuberculosis and host RNA expression in Africa. N Engl J Med. 2014;370(18):1712–1723. doi: 10.1056/NEJMoa1303657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zak DE, Penn-Nicholson A, Scriba TJ, et al. A blood RNA signature for tuberculosis disease risk: a prospective cohort study. Lancet. 2016;387(10035):2312–2322. doi: 10.1016/S0140-6736(15)01316-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhou M, Yu G, Yang X, Zhu C, Zhang Z, Zhan X. Circulating microRNAs as biomarkers for the early diagnosis of childhood tuberculosis infection. Mol Med Rep. 2016;13:4620–4626. doi: 10.3892/mmr.2016.5097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rekha RS, Kamal SM, Andersen P, et al. Validation of the ALS assay in adult patients with culture confirmed pulmonary tuberculosis. PLoS One. 2011;6(1):e16425. doi: 10.1371/journal.pone.0016425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Thomas T, Brighenti S, Andersson J, Sack D, Raqib R. A new potential biomarker for childhood tuberculosis. Thorax. 2011;66(8):727–729. doi: 10.1136/thx.2010.147363. [DOI] [PubMed] [Google Scholar]
- 96.Chisti MJ, Salam MA, Raqib R, et al. Validity of antibodies in lymphocyte supernatant in diagnosing tuberculosis in severely malnourished children presenting with pneumonia. PLoS One. 2015;10(5):e0126863. doi: 10.1371/journal.pone.0126863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Blok N, Visser DH, Solomons R, Van Elsland SL, den Hertog AL, van Furth AM. Lipoarabinomannan enzyme-linked immunosorbent assay for early diagnosis of childhood tuberculous meningitis. Int J Tuberc Lung Dis. 2014;18(2):205–210. doi: 10.5588/ijtld.13.0526. [DOI] [PubMed] [Google Scholar]
- 98.Nicol MP, Allen V, Workman L, et al. Urine lipoarabinomannan testing for diagnosis of pulmonary tuberculosis in children: a prospective study. Lancet Glob Health. 2014;2(5):e278– e284. doi: 10.1016/S2214-109X(14)70195-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Du Toit G, Swingler G, Iloni K. Observer variation in detecting lymphadenopathy on chest radiography. Int J Tuberc Lung Dis. 2002;6(9):814–817. [PubMed] [Google Scholar]
- 100.Swingler GH, du Toit G, Andronikou S, van der Merwe L, Zar HJ. Diagnostic accuracy of chest radiography in detecting mediastinal lymphadenopathy in suspected pulmonary tuberculosis. Arch Dis Child. 2005;90(11):1153–1156. doi: 10.1136/adc.2004.062315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Smuts NA, Beyers N, Gie RP, et al. Value of the lateral chest radiograph in tuberculosis in children. Pediatr Radiol. 1994;24(7):478–480. doi: 10.1007/BF02015003. [DOI] [PubMed] [Google Scholar]
- 102.Breuninger M, van Ginneken B, Philipsen RH, et al. Diagnostic accuracy of computer-aided detection of pulmonary tuberculosis in chest radiographs: a validation study from sub-Saharan Africa. PLoS One. 2014;9(9):e106381. doi: 10.1371/journal.pone.0106381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Villarino ME, Scott NA, Weis SE, et al. Treatment for preventing tuberculosis in children and adolescents: a randomized clinical trial of a 3-month, 12-dose regimen of a combination of rifapentine and isoniazid. JAMA Pediatr. 2015;169(3):247–255. doi: 10.1001/jamapediatrics.2014.3158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cruz AT, Starke JR. Safety and completion of a 4-month course of rifampicin for latent tuberculous infection in children. Int J Tuberc Lung Dis. 2014;18(9):1057–1061. doi: 10.5588/ijtld.14.0286. [DOI] [PubMed] [Google Scholar]
- 105.Cruz AT, Martinez BJ. Childhood tuberculosis in the United States: shifting the focus to prevention. Int J Tuberc Lung Dis. 2015;19(Suppl 1):50–53. doi: 10.5588/ijtld.15.0418. [DOI] [PubMed] [Google Scholar]
- 106.Seddon JA, Furin JJ, Gale M, et al. Caring for children with drug-resistant tuberculosis: practice-based recommendations. Am J Respir Crit Care Med. 2012;186(10):953–964. doi: 10.1164/rccm.201206-1001CI. [DOI] [PubMed] [Google Scholar]
- 107.Nachman S, Ahmed A, Amanullah F, et al. Towards early inclusion of children in tuberculosis drugs trials: a consensus statement. Lancet Infect Dis. 2015;15(6):711–720. doi: 10.1016/S1473-3099(15)00007-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Srivastava S, Deshpande D, Pasipanodya JG, et al. A Combination Regimen Design Program Based on Pharmacodynamic Target Setting for Childhood Tuberculosis: Design Rules for the Playground. Clin Infect Dis. 2016;63(suppl 3):S75–s79. doi: 10.1093/cid/ciw472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Morrison J, Pai M, Hopewell PC. Tuberculosis and latent tuberculosis infection in close contacts of people with pulmonary tuberculosis in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Infect Dis. 2008;8(6):359–368. doi: 10.1016/S1473-3099(08)70071-9. [DOI] [PubMed] [Google Scholar]
- 110.van der Heijden YF, Heerman WJ, McFadden S, Zhu Y, Patterson BL. Missed opportunities for tuberculosis screening in primary care. J Pediatr. 2015;166(5):1240–1245. e1241. doi: 10.1016/j.jpeds.2015.01.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Mangtani P, Abubakar I, Ariti C, et al. Protection by BCG vaccine against tuberculosis: a systematic review of randomized controlled trials. Clin Infect Dis. 2014;58(4):470–480. doi: 10.1093/cid/cit790. [DOI] [PubMed] [Google Scholar]
- 112.Harris RC, Dodd PJ, White RG. The potential impact of BCG vaccine supply shortages on global paediatric tuberculosis mortality. BMC Med. 2016;14(1):138. doi: 10.1186/s12916-016-0685-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Tameris MD, Hatherill M, Landry BS, et al. Safety and efficacy of MVA85A, a new tuberculosis vaccine, in infants previously vaccinated with BCG: a randomised, placebo-controlled phase 2b trial. Lancet. 2013;381(9871):1021–1028. doi: 10.1016/S0140-6736(13)60177-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Principi N, Esposito S. The present and future of tuberculosis vaccinations. Tuberculosis (Edinb) 2015;95(1):6–13. doi: 10.1016/j.tube.2014.10.004. [DOI] [PubMed] [Google Scholar]