Abstract
Purpose of review
The aim of this review is to summarize use of the FLIP for the evaluation and management of esophageal diseases.
Recent findings
The FLIP utilizes high-resolution impedance planimetry to evaluate the functional geometry and cross-sectional area/pressure relationship (i.e. distensibility) of the esophageal sphincters and body. Recent studies have reported the potential utility of FLIP to evaluate esophageal diseases, such as achalasia, gastroesophageal reflux disease, and eosinophilic esophagitis.
Summary
Esophageal distensibility measures provided by the FLIP will add to our understanding of the contribution of esophageal mechanical properties to esophageal symptoms and function. Application of the FLIP in clinical practice complements the diagnostic evaluation of esophageal function and may also be a valuable tool to help direct and target clinical management of esophageal diseases.
Keywords: functional lumen imaging probe, impedance planimetry, achalasia, gastroesophageal reflux disease, eosinophilic esophagitis
Introduction
The primary function of the esophagus is to serve as a transport conduit between the mouth and the stomach. Bolus flow is strongly related to esophageal opening dimensions, which are controlled by neuromuscular interactions involving active and passive contraction and relaxation to regulate distension of the esophageal sphincters and body in response to intra-luminal (i.e. intra-bolus) pressure.1, 2 Further, esophageal transport and esophageal sensation appear to be related to mechanical properties of the esophagus.3, 4 However, accurate assessments of esophageal distensibility are somewhat limited with traditional methods of esophageal disease evaluation (i.e. upper endoscopy, manometry, and barium-radiography).2
Devices employing impedance planimetry, which measures luminal cross-sectional area (CSA), combined with intra-luminal pressure sensors allow for evaluation of esophageal mechanical properties and distensibility. Initial studies applying impedance planimetry to the esophagus demonstrated the feasibility and utility in evaluating the esophagogastric junction (EGJ) and esophageal hypersensitivity.5, 6 Multiple impedance planimetry electrodes measuring serial, adjacent CSAs in a tubular lumen (essentially high-resolution impedance planimetry) allowed for anatomic and biomechanical characterization of the esophagus: a functional lumen imaging probe (FLIP).7
Research and clinical utilization of FLIP to assess esophageal function and disease has increased in recent years using the commercially-available device, the EndoFLIP (Crospon, Inc. Galway, Ireland). The FLIP has demonstrated the potential to become a valuable tool for functional evaluation in esophageal diseases associated with abnormalities of EGJ competence (e.g. achalasia and gastroesophgeal reflux disease, GERD) and mechanical properties of the esophageal body (e.g. eosinophilic esophagitis, EoE). Thus, this review aims to discuss the FLIP and its applications and implications for the evaluation and management of esophageal disease.
The EndoFLIP
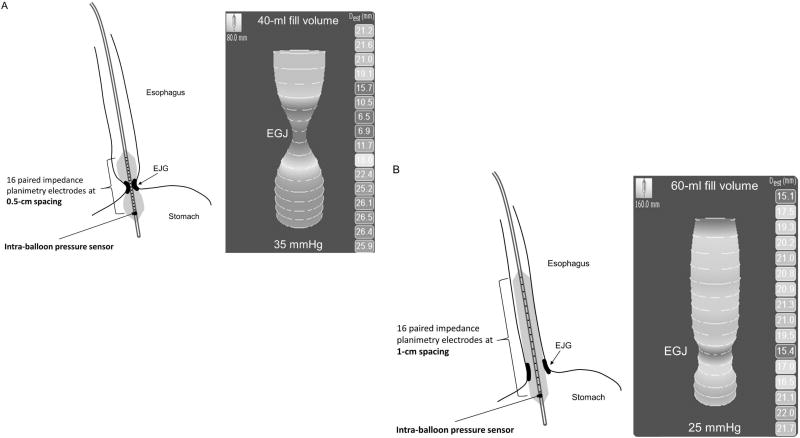
The FLIP consists of a 240-mm long, 3-mm outer diameter catheter with a balloon mounted on the distal end. The balloon houses 16 paired impedance planimetry electrodes spaced at regular intervals, and a solid-state pressure transducer located at the distal end (Figure 1). Excitation electrodes at either end of the balloon emit a continuous low electric current. The voltage is measured across the paired impedance planimetry electrodes when the balloon is filled with a conductive fluid (saline). With a known distance between electrodes and known fluid conductivity, the electrical resistance of the fluid (impedance) is proportional to the CSA; thus based on Ohm’s law (voltage = current × resistance) the CSA is determined from the voltage.8
Figure 1. The functional lumen imaging probe (FLIP).
Schematics (left) and real-time images (right) representing typical position of the two primary FLIP device sizes: A, left panel) An 8-cm cylindrical, measurement segment with impedance planimetry channels spaced at 5-mm intervals within a 10-cm length balloon (EF-325) and B, left panel) A 16-cm cylindrical, measurement segment with 1-cm channel spacing housed within an 18-cm length balloon (EF-322). The EGJ can be identified on the real time imaging by the waist in the hour-glass formation. A, right panel). An example of a patient with achalasia studied intra-operatively during a POEM using the 8-cm measurement length device. The EGJ distensibility index (EGJ-DI, the median narrowest CSA divided by median intra-balloon pressure) measured at a 40-ml fill volume was 0.9 mm2/mmHg. Dest=estimated luminal diameter at each impedance planimetry channel. B, right panel). An example of a patient with GERD studied during endoscopy using the 16-cm measurement length device. The EGJ-DI measured at a 60-ml fill volume was 8.0 mm2/mmHg. Figure used with permission from the Esophageal Center at Northwestern.
The balloon is infinitely compliant (within allotted fill volumes) to allow conformation to the esophageal lumen and subsequent measurement of distensive properties of the tubular lumen. Two primary device sizes are commercially available with FLIP measurement segments of 8-cm (EF-325) or 16-cm (EF-322), Figure 1. Some studies report use of earlier models that consisted of a 10 –14 cm balloon that housed the 16-paired electrodes spaced at 4-mm intervals for a 6.4-cm measurement length.9–13
FLIP: Methods
Study protocol
During a FLIP study, measurements of 16-sequential CSAs and one intra-balloon pressure are simultaneously measured at a 10-Hz sampling rate during volume-controlled distension of the balloon. Luminal diameter measurements, which simplify use for clinical application, are generated from the CSA measures by assuming a circular lumen: CSA = π(diameter/2)2.
Variations in FLIP study methods and protocols exist (Table 1)14: The FLIP is placed into the esophagus either trans-orally or trans-nasally in a sedated or awake patient. Due to patient tolerance, our institutional practice is to place the catheter orally either during endoscopy with conscious sedation (typically using the 16-cm measurement device) or intra-operatively during general anesthesia (typically using the 8-cm measurement device). The FLIP is positioned within the esophagus by identifying the waist on the real-time, semi-3D display (Figure 1) at a low fill volume (typically 20–30ml). The esophageal body can be evaluated, such as in EoE, with the 8-cm FLIP by first identifying the EGJ then re-positioning proximally. With the 16-cm FLIP, the distal esophageal body can be evaluated simultaneously with the EGJ; the EGJ then serves as a reference point to control for catheter movement during the study. Marking the catheter with an endoscopically or manometrically measured distance to the EGJ can also assist with placement, though maintenance of stable FLIP positioning by visualizing landmarks on the real-time display during the course of the study remains paramount.
Table 1.
Summary of FLIP methods and results of studies evaluating EGJ-distensibility in asymptomatic controls.
| Author, year | N | FLIP length, cm |
IP channel spacing, mm |
Test setting, sedation |
Placement | Pressure zero |
Fill volume, ml |
EGJ-DI, mm2/mmHg* |
Comparator group |
|---|---|---|---|---|---|---|---|---|---|
|
| |||||||||
| Kwiatek, 20109 | 20 | 6.4 | 4 | Endoscopy, Conscious | Oral | Gastric | 10 | 3.2 (2.3 – 6.7) | GERD |
| 20 | 2.2 (1.2 – 6.5) | ||||||||
| 30 | 4.2 (1.7 – 10.4) | ||||||||
| 40 | 7.3 (3.8 – 11.4) | ||||||||
|
| |||||||||
| Kwiatek, 201115 | 15 | 8 | 5 | Endoscopy, Conscious | Oral | NR | 20 | 0.9 (0.3 – 1.4) | EoE |
| 30 | 0.8 (0.4 – 2.8) | ||||||||
|
| |||||||||
| Rohof, 201210 | 15 | 6.4 | 4 | Awake | Nasal | Atm | 50 | 6.3 +/− 0.7 | Achalasia |
|
| |||||||||
| Nathanson, 201216 | 50 | 8 | 5 | Intra-operative, General anesthesia | Oral | Gastric | 30 | 1.1 (0.7 – 1.6)† | -- |
| 40 | 1.2 (0.83 – 2.2)† | ||||||||
|
| |||||||||
| Tucker, 201312 | 22 | 6.4 | 4 | Endoscopy, Conscious | Oral | NR | 20 | 4.0 (2.4 – 7.5) | GERD |
| 30 | 6.1 (4.3 – 8.0) | ||||||||
|
| |||||||||
| Rieder, 201317 | 4 | 8 | 5 | Awake | Oral | NR | 30 | 2.5 (2.0 – 6.3) | Achalasia |
| 40 | 2.7 (2.4 – 8.3) | ||||||||
|
| |||||||||
| Fukazawa, 201418 | 9 | 8 | 5 | Awake | Nasal | Atm | 20 | 2.9 +/− (0.6) | Intra-subject following mosapride |
| 40 | 7.1 +/− (0.9) | ||||||||
| 50 | 8.2 +/− (0.8) | ||||||||
|
| |||||||||
| Lottrup, 201519 | 10 | 8 | 5 | Awake | Oral | Atm | 20 | 1.9 +/− 0.5 | GERD, hiatal hernia |
| 30 | 2.8 +/− 0.6 | ||||||||
| 40 | 3.8 +/− 0.9 | ||||||||
| 50 | 3.9 +/− 0.7 | ||||||||
|
| |||||||||
| Carlson, 201520 | 10 | 16 | 10 | Endoscopy, Conscious | Oral | Atm | 50 | 7.1 (3.8 – 8.9) | Achalasia |
| 60 | 6.2 (4.6 – 8.1) | ||||||||
|
| |||||||||
| Mikami, 201613 | 9 | 6.4 | 4 | Awake | Nasal | Atm | 20 | 1.8 +/− (0.2) | Intra-subject following metoclopramide |
| 30 | 3.5 +/− (0.6) | ||||||||
| 40 | 4.5 +/− (0.5) | ||||||||
Results are extrapolated from figures if not directly reported and represented as median (inter-quartile range) or mean +/− SD (SE).
Results reflect measurements obtained at intubation, prior to pneumoperitoneum creation.
IP – impedance planimetry. NR – not reported. Atm – atmospheric.
During stable positioning of the catheter, volume-controlled distension of the balloon is performed. CSA and pressure (thus distensibility) measurements may vary depending on the degree of volume distension, thus measurements should be obtained at a stable distension volume and over a time sufficient to allow accounting for measurement fluctuation related to respiration and esophageal contractions/peristalsis. Additionally, measurements should be obtained at a volume that can generate sufficient intra-balloon pressure to distend the esophageal body to allow an evaluation of the luminal CSA/pressure relationship. Further, assessing the CSA/pressure response to varying distension volumes may be informative, such as to allow measurement of a distensibility plateau (see EoE below), thus step-wise volumetric distension at 5 – 10 ml increments may also be utilized. Our practice is to perform step-wise volumetric distension with the 16-cm FLIP during endoscopic evaluation; we focus on the EGJ distensibility measures at the 60-ml fill volume. For intra-operative use, we typically make EGJ measurements at the 40-ml fill volume with the 8-cm FLIP.
Data analysis
Though both CSA (diameter) and pressure are simultaneously measured (and often reported independently in studies), assessing the relationship between luminal CSA and distending (intra-balloon) pressure arguably reflects the greatest value provided by the FLIP for the esophageal evaluation. Thus distensibility will be the primary focus for the remainder of this review.
The distensibility index (DI) has been the typical measure of sphincter distensibility and is calculated by dividing the median narrowest CSA (within the sphincter of interest) divided by median intra-balloon pressure over a set timeframe (or distension volume). The FLIP measurements are dynamic with both CSA and pressure fluctuation occurring during a stable distension volume, thus various methods using the FLIP Analytics software (Crospon) or other external software methods (e.g. MATLAB, The Math Works, Natick, MA) have been reported to generate metrics.
The FLIP is indicated (and FDA approved for use in the United States) for clinical use as a pressure and dimension measurement device, as an adjunctive test in patients with symptoms consistent with esophageal hypersensitivity, and to estimate the size of a stoma produced by a gastric band. Thus, clinical applications for FLIP are varied.
Achalasia
A hallmark of achalasia is lower esophageal sphincter (LES) dysfunction, and achalasia treatments target relieving the resultant EGJ outflow obstruction; thus the FLIP appears well suited for evaluation of patients with achalasia.
Studies utilizing FLIP have consistently demonstrated an abnormally low EGJ-DI (i.e. more narrowed EGJ lumen at greater distending-pressure) in treatment naïve achalasia patients.10, 17, 20, 21 Further, studies assessing achalasia treatment response (e.g. after pneumatic dilation or LES myotomy) have reported lower EGJ-DI in patients with poor symptomatic outcomes (particularly below a threshold of 2.8 – 2.9 mm2/mmHg than in patients with good symptomatic outcomes10, 21; they also suggest that EGJ-DI may have a stronger association with symptoms and esophageal retention (per timed-barium esophagram) than manometric measures of LES pressures. Additionally, evaluation of esophageal contractility (described in more detail below) with achalasia may also provide some complementary clinical information to the standard achalasia assessment with esophageal manometry.20
Intra-operative use of FLIP during laparoscopic Heller myotomy or per-oral endoscopic myotomy (POEM) also offers the ability to assess the LES myotomy in real-time. Several studies have demonstrated an immediate increase in EGJ-DI following POEM or Heller myotomy (associated with a slight decrease following fundoplasty creation).22–26 Additionally, staged intra-operative FLIP during POEM demonstrated an increase in EGJ-DI during sub-mucosal tunnel creation (prior to LES myotomy).22, 26 While this finding raises questions regarding the role of the esophageal submucosa in achalasia, additional study is needed to clarify its clinical significance.
Further, intra-operative FLIP may provide a method to ‘tailor’ the myotomy +/− fundoplasty to help improve dysphagia (i.e. avoid too low EGJ distensibility), while limiting GERD (i.e. avoid overly-increasing EGJ-distensibility). A recent multi-center study assessed the association with early clinical outcomes (median follow-up 122 days) and retrospectively-evaluated final intra-operative FLIP measures of 63 patients with achalasia treated with POEM.24 They found a lower EGJ-CSA at a 30-ml fill volume of an 8-cm FLIP (but similar EGJ-CSA at 40-ml) in those with a poor symptomatic outcome (n = 13) than those with a good outcome (n = 50). EGJ-DI was numerically, but not statistically, lower among the poor outcome group at both 30 and 40-ml fill volumes. Further, they also found a greater EGJ-CSA (again at 30-ml, but not 40ml) associated with objective evidence of GERD (reflux esophagitis or abnormal esophageal acid exposure). Another recent study reported that a final intra-operative EGJ-DI (at 40-ml distension volume with an 8-cm FLIP) in the range of 4.5 – 8.5 mm2/mmHg was optimal in that it was high enough to relieve dysphagia, but low enough to result in minimal GERD symptoms at > 6 months follow-up after POEM (n = 21) or laparoscopic Heller myotomy (n = 11).25 Though additional study is needed to validate these findings in a prospective manner, FLIP offers significant promise to aid in the treatment of achalasia.
Additionally, esophageal dilatation balloons that incorporate FLIP (using a more rigid balloon material than the conventional measurement FLIP balloons) are available. Of note, no intra-balloon pressure sensor is included with the dilation balloons, though an external pressure monitor can be attached.27 A recent study demonstrated the feasibility and short-term clinical effectiveness of using the FLIP achalasia hydraulic dilation balloon (maximal diameter of 30-mm).27 As the EGJ can be identified with a waist on the real-time display to position the balloon, additional experience with this device may allow for achalasia dilation to be performed without the concurrent use of fluoroscopy.
Gastroesophageal reflux disease
As EGJ incompetence may contribute to GERD pathophysiology in some patients, it is reasonable to suspect that FLIP may help identify increased EGJ-distensibility (i.e. greater EGJ diameters at lower distending-pressures) in some patients with GERD. Results of studies, however, have been inconsistent. Initially, a study demonstrated greater EGJ-DIs among 20 symptomatic GERD patients than 20 asymptomatic volunteers.9 However, another study that compared patients who had typical GERD symptoms (n = 18) with asymptomatic controls (n = 18) found that GERD patients actually had lower EGJ-DI than controls.12 Furthermore, EGJ-DI did not differ between patients with normal (n = 9) or abnormal (n = 9) esophageal acid exposure time by 48-hour wireless esophageal pH monitoring. Recently, a study evaluating patients who had Barrett’s esophagus with hiatal hernias ≥ 2cm (n = 23) reported that FLIP could generally identify the hiatal hernia (measuring both distensibility of the LES and the crural diaphragm components of the EGJ), and that the distensibility of the LES in hiatal hernia patients was greater than in nasymptomatic controls.19 Although the diagnostic utility of FLIP in GERD may remain in question, further study may help evaluate physiologic components related to GERD pathophysiology.
As patients with fundoplication appear to have reduced EGJ distensibility compared with controls,28 FLIP may be a useful tool to tailor anti-reflux procedures (such as fundoplication).29 Several studies demonstrated the feasibility of intra-operative FLIP use during fundoplication, documenting a consistent reduction in EGJ-distensibility immediately following fundoplication.30, 31 Reduction in EGJ-distensibility following trans-oral incisionless fundoplication (TIF) has also been reported.32, 33 A report of pooled results of intra-operative FLIP during laparoscopic Nissen fundoplication from 4 high-volume centers reported a mean final EGJ-CSA of 6.1 mm2 (SD 1.4) and EGJ-DI of 1.6 mm2/mmHg (SD 1.1), suggesting these as targets for fundoplication based on historically good outcomes from their centers; however, directly-associated clinical outcomes were not reported.30
The role of FLIP for physiologic evaluation and management in GERD remains uncertain, but appears promising. Future outcome studies are needed to substantiate the clinical utility of FLIP in GERD.
Eosinophilic esophagitis
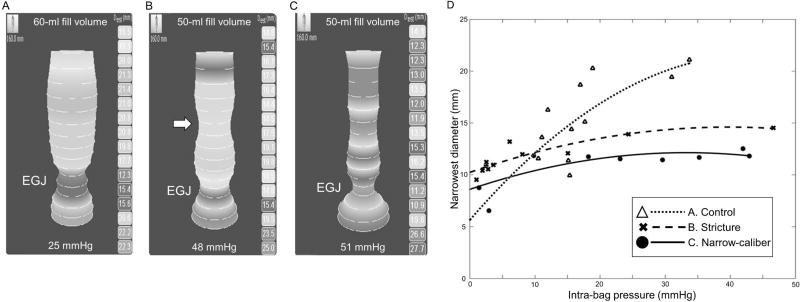
Eosinophilic esophagitis is a chronic, immune-mediated disease of the esophagus characterized by esophageal symptoms (predominantly dysphagia) and eosinophilic inflammation.34 Chronic inflammation is thought to progress to fibrosis and stenosis of the esophagus,35 which is typically evaluated with endoscopy. However there are limitations to endoscopic assessment of esophageal narrowing in EoE.36 FLIP assessment of the esophageal body in EoE allows objective measurement of esophageal narrowing and mechanical properties of the esophageal body.15 Measurement of a narrowest esophageal body CSA and corresponding intra-balloon pressure during step-wise volumetric distension with the FLIP positioned in the esophageal body allows plotting a CSA by pressure curve, which enables identification of the distensibility plateau (Figure 2). The distensibility plateau represents the luminal opening that may restrict passage of swallowed bolus, and reduced distensibility (a lower distensibility plateau) has been demonstrated in EoE patients compared with asymptomatic controls.15 Another study of EoE patients reported an association of reduced distensibility plateau with clinical outcomes including future food impaction and requirement for esophageal dilation. Additionally, a distensibility plateau < 225 mm2 (diameter ~17mm) was the only independent predictor (i.e. not treatment type or eosinophil count, among others) of future food impaction.
Figure 2. Distensibility plateau.
Real-time images from the maximum-achieved fill volume of A) an asymptomatic volunteer and patients with EoE and B) a focal stricture (identified with a white arrow) and C) diffuse narrow-caliber esophagus. D). The distensibility plateau was developed to represent the luminal CSA (or diameter) at which the pressure increases at a fixed luminal opening. Thus, the distensibility plateau is determined as the peak of the best-fit line generated from plotted data points of the narrowest esophageal body diameter and intra-balloon pressure for each distension volume during step-wise volumetric distension. The displayed distensibility plateaus are A) 22-mm, B) 14.6 mm, and C) 12.1 mm. Figure used with permission from the Esophageal Center at Northwestern.
While FLIP appears to have significant value for patient evaluation in EoE, some complexity is involved to identify the narrowest portion of the esophageal body (to facilitate distensibility assessment) when esophageal contractions and peristalsis occur. Thus post-processing the FLIP data using software programs to filter out the contraction-associated changes in esophageal luminal diameter remains necessary.37, 38 Software advancements will hopefully be implemented to increase availability of these analysis techniques to broaden the application of FLIP to EoE evaluation and thus better determine its clinical value in future studies.
Other clinical uses
Esophageal motility
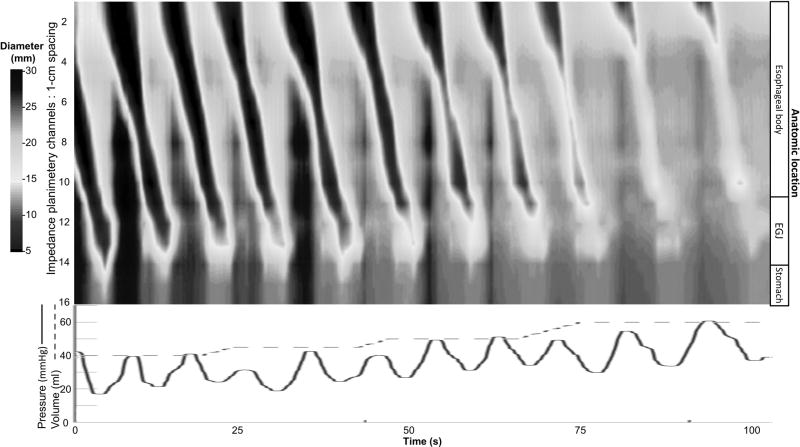
Although the contractility and peristalsis observed on FLIP may add complexity to distensibility analysis (as in EoE), it may also represent a method to evaluate the esophageal contractile response to distension (i.e. secondary peristalsis). Serially-spaced diameter changes measured with the FLIP can be interpolated by applying software algorithms to depict organized esophageal contractile patterns as FLIP topography (Figure 3), similar to representing serially-spaced pressures measured with high-resolution manometry as esophageal pressure topography. A study of asymptomatic volunteers observed that the majority demonstrated a stereotypical pattern of repetitive, antegrade contractions that likely represented secondary peristalsis in response to sustained volumetric dilation of the distal esophagus.39 Thresholds (volume, pressure, and esophageal diameter) to induce contractile activity as well as contractile properties (e.g. contractile velocity) were evaluated.
Figure 3. FLIP Topography.
Color-coded diameters (topography) generated by interpolation of data from the 16 impedance planimetry channels at 1-cm spacing (top), along with intra-balloon pressure (bottom) and distension volume (bottom) over a portion of a distension protocol in an asymptomatic, healthy volunteer. Repetitive, antegrade contraction (RACs) can be appreciated in the topographic plot. Figure used with permission from the Esophageal Center at Northwestern.
Additionally, evaluation of patients with newly diagnosed achalasia with FLIP topography demonstrated evidence of esophageal contractility in most cases, even among those without contractility observed on high-resolution manometry (37% of type I achalasia and 65% of type II achalasia).20 Some patients, especially those with spastic (type III) achalasia, demonstrated a novel pattern of repetitive, retrograde contractions, which was not observed in any of the controls. The contractility detected by FLIP in achalasia may represent contractions not detected on manometry due to lack of contact pressure on the manometry catheter or those masked by pressurization, and thus may provide supplemental prognostic information to the manometric assessment. While the clinical implications of motility findings appreciated with FLIP topography require further clinical study, FLIP may offer a well-tolerated method to complement the esophageal motility evaluation.
Upper esophageal sphincter
The FLIP has also been used to evaluate the distensibility and swallow associated opening dynamics of the upper esophageal sphincter (UES) in both asymptomatic, healthy volunteers and in patients following laryngectomy.40–42 Though further study is needed to demonstrate the clinical significance of FLIP findings of the UES, it appears to be a feasible and safe method to supplement the evaluation of the oropharyngeal swallow.42
Conclusions
The FLIP offers a novel method to enhance the evaluation of esophageal function, particularly in achalasia, GERD, and EoE. Future study is necessary to optimize study protocols and analysis techniques, which then need to be standardized for generalizable use. Further, translation of functional results to clinical outcomes remains needed to clarify clinical implications and enhance clinical use of the FLIP. Though research and experience with the FLIP remains in its relative infancy, the FLIP will help advance our understanding of the contribution of esophageal mechanical properties to esophageal symptoms and function, and may well emerge as a valuable tool to aid in clinical management of esophageal diseases.
Key Points.
Simultaneously measuring luminal cross sectional area (via impedance planimetry) and intra-balloon pressure, the functional lumen imaging probe (FLIP) provides a unique method to evaluate esophageal function by assessing the esophageal response to distension (i.e. distensibility).
Various FLIP study protocol and analysis methods have been reported, thus optimization and standardization of FLIP methods are needed.
In achalasia, reduced EGJ distensibility is associated with dysphagia while elevated EGJ distensibility (following therapy) is associated with reflux. Thus, FLIP can provide both symptomatic evaluation and intra-interventional (e.g. during operative LES myotomy) guidance to aid achalasia management.
Evaluation of esophageal body distensibility in EoE offers a method to objectively measure fibrostenotic disease effects, and potentially aid prediction of clinical outcomes (e.g. food impaction).
Use of FLIP for evaluation of GERD, upper esophageal sphincter function, and esophageal motility is promising, though requires further research to establish its clinical utility and implications.
Acknowledgments
None
Funding:
This work was supported by T32 DK101363 (PI: Pandolfino).
Abbreviations
- CSA
cross-sectional area
- DI
distensibility index
- EoE
eosinophilic esophagitis
- EGJ
esophagogastric junction
- FLIP
functional lumen imaging probe
- GERD
gastroesophgeal reflux disease
- LES
lower esophageal sphincter
- POEM
per-oral endoscopic myotomy
- TIF
transoral incisionless fundoplication
- UES
upper esophageal sphincter
Footnotes
Conflicts of interest:
None
References
- 1.Goyal RK, Chaudhury A. Physiology of normal esophageal motility. J Clin Gastroenterol. 2008;42(5):610–9. doi: 10.1097/MCG.0b013e31816b444d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pandolfino JE, Shi G, Trueworthy B, et al. Esophagogastric junction opening during relaxation distinguishes nonhernia reflux patients, hernia patients, and normal subjects. Gastroenterology. 2003;125(4):1018–24. doi: 10.1016/s0016-5085(03)01210-1. [DOI] [PubMed] [Google Scholar]
- 3.Nasr I, Attaluri A, Hashmi S, et al. Investigation of esophageal sensation and biomechanical properties in functional chest pain. Neurogastroenterol Motil. 2010;22(5):520–6. e116. doi: 10.1111/j.1365-2982.2009.01451.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lin Z, Yim B, Gawron A, et al. The four phases of esophageal bolus transit defined using high resolution impedance manometry and fluoroscopy. Am J Physiol Gastrointest Liver Physiol. 2014 doi: 10.1152/ajpgi.00148.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rao SS, Hayek B, Summers RW. Impedance planimetry: an integrated approach for assessing sensory, active, and passive biomechanical properties of the human esophagus. Am J Gastroenterol. 1995;90(3):431–8. [PubMed] [Google Scholar]
- 6.McMahon BP, Frokjaer JB, Drewes AM, et al. A new measurement of oesophago-gastric junction competence. Neurogastroenterol Motil. 2004;16(5):543–6. doi: 10.1111/j.1365-2982.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- 7.McMahon BP, Frokjaer JB, Liao D, et al. A new technique for evaluating sphincter function in visceral organs: application of the functional lumen imaging probe (FLIP) for the evaluation of the oesophago-gastric junction. Physiol Meas. 2005;26(5):823–36. doi: 10.1088/0967-3334/26/5/019. [DOI] [PubMed] [Google Scholar]
- 8.Gregersen H, Djurhuus JC. Impedance planimetry: a new approach to biomechanical intestinal wall properties. Dig Dis. 1991;9(6):332–40. doi: 10.1159/000171320. [DOI] [PubMed] [Google Scholar]
- 9.Kwiatek MA, Pandolfino JE, Hirano I, et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP) Gastrointest Endosc. 2010;72(2):272–8. doi: 10.1016/j.gie.2010.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rohof WO, Hirsch DP, Kessing BF, et al. Efficacy of treatment for patients with achalasia depends on the distensibility of the esophagogastric junction. Gastroenterology. 2012;143(2):328–35. doi: 10.1053/j.gastro.2012.04.048. [DOI] [PubMed] [Google Scholar]
- 11.Verlaan T, Rohof WO, Bredenoord AJ, et al. Effect of peroral endoscopic myotomy on esophagogastric junction physiology in patients with achalasia. Gastrointest Endosc. 2013;78(1):39–44. doi: 10.1016/j.gie.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 12.Tucker E, Sweis R, Anggiansah A, et al. Measurement of esophago-gastric junction cross-sectional area and distensibility by an endolumenal functional lumen imaging probe for the diagnosis of gastro-esophageal reflux disease. Neurogastroenterol Motil. 2013;25(11):904–10. doi: 10.1111/nmo.12218. [DOI] [PubMed] [Google Scholar]
- *13.Mikami H, Ishimura N, Fukazawa K, et al. Effects of Metoclopramide on Esophageal Motor Activity and Esophagogastric Junction Compliance in Healthy Volunteers. J Neurogastroenterol Motil. 2016;22(1):112–7. doi: 10.5056/jnm15130. This study evaluated the effect of metoclopromide on EGJ distensibility in 9 asymptomatic controls. No difference in EGJ-DI measured with FLIP was detected following a dose of intraveneous metoclopramide. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen J, Rubenstein J. Reference Values of Esophagogastric Junction Distensibility Assessed Using the Endolumenal Functional Lumen Imaging Probe (EndoFLIP) - A Systematic Review. Gastroenterol. 2015;148(4):S817–18. [Google Scholar]
- 15.Kwiatek MA, Hirano I, Kahrilas PJ, et al. Mechanical properties of the esophagus in eosinophilic esophagitis. Gastroenterology. 2011;140(1):82–90. doi: 10.1053/j.gastro.2010.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nathanson LK, Brunott N, Cavallucci D. Adult esophagogastric junction distensibility during general anesthesia assessed with an endoscopic functional luminal imaging probe (EndoFLIP(R)) Surg Endosc. 2012;26(4):1051–5. doi: 10.1007/s00464-011-1996-3. [DOI] [PubMed] [Google Scholar]
- 17.Rieder E, Swanstrom LL, Perretta S, et al. Intraoperative assessment of esophagogastric junction distensibility during per oral endoscopic myotomy (POEM) for esophageal motility disorders. Surg Endosc. 2013;27(2):400–5. doi: 10.1007/s00464-012-2484-0. [DOI] [PubMed] [Google Scholar]
- *18.Fukazawa K, Furuta K, Adachi K, et al. Effects of mosapride on esophageal motor activity and esophagogastric junction compliance in healthy volunteers. J Gastroenterol. 2014;49(9):1307–13. doi: 10.1007/s00535-013-0876-0. This study evaluated the effect of mosapride on EGJ distensibility in 9 asymptomatic controls. A reduction in EGJ-DI measured with FLIP was detected following a dose of oral mosapride. [DOI] [PubMed] [Google Scholar]
- **19.Lottrup C, McMahon BP, Ejstrud P, et al. Esophagogastric junction distensibility in hiatus hernia. Dis Esophagus. 2015 doi: 10.1111/dote.12344. This study reported that hiatal hernia was able to be reliably identified using the FLIP; additionally, the distensibility parameters at both the LES and crural diaphram were able to be measured. [DOI] [PubMed] [Google Scholar]
- *20.Carlson DA, Lin Z, Kahrilas PJ, et al. The Functional Lumen Imaging Probe Detects Esophageal Contractility Not Observed With Manometry in Patients With Achalasia. Gastroenterology. 2015;149(7):1742–51. doi: 10.1053/j.gastro.2015.08.005. Using FLIP topography in patients with treatment naïve achalasia, esophageal contractility (lumen occluding and non-occluding contractions and specific, distension-related contractile patterns) was observed that was not identified on high-resolution resultion manometry. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pandolfino JE, de Ruigh A, Nicodeme F, et al. Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP) in achalasia patients. Neurogastroenterol Motil. 2013;25(6):496–501. doi: 10.1111/nmo.12097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Teitelbaum EN, Boris L, Arafat FO, et al. Comparison of esophagogastric junction distensibility changes during POEM and Heller myotomy using intraoperative FLIP. Surg Endosc. 2013;27(12):4547–55. doi: 10.1007/s00464-013-3121-2. [DOI] [PubMed] [Google Scholar]
- **23.Teitelbaum EN, Soper NJ, Pandolfino JE, et al. An extended proximal esophageal myotomy is necessary to normalize EGJ distensibility during Heller myotomy for achalasia, but not POEM. Surg Endosc. 2014;28(10):2840–7. doi: 10.1007/s00464-014-3563-1. This study evaluating EGJ-distensibility using intra-operative FLIP during stages of laparoscopic Heller myotomy and POEM in patients with achalasia demonstrated a greater increase in EGJ-DI with POEM than Heller mytomy. This study supports tailoring the achalasia myotomy by demonstrating that the increase in EGJ-DI with POEM occurs with only the EGJ-mytomy (with little gain from proximal extension), while proximal extinsion was required for Heller myotomy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **24.Ngamruengphong S, von Rahden BH, Filser J, et al. Intraoperative measurement of esophagogastric junction cross-sectional area by impedance planimetry correlates with clinical outcomes of peroral endoscopic myotomy for achalasia: a multicenter study. Surg Endosc. 2015 doi: 10.1007/s00464-015-4574-2. This retrospective, multi-center study demonstrated that intra-operative EGJ-CSA (but not EGJ-DI) following POEM was lower in achalasia patients with poor symptomatic outcomes than those with good symptomatic outcomes at a median follow-up interval of 122 days; thus suggesting that intra-operative FLIP may be a useful tool to predict clinical outcomes. [DOI] [PubMed] [Google Scholar]
- **25.Teitelbaum EN, Soper NJ, Pandolfino JE, et al. Esophagogastric junction distensibility measurements during Heller myotomy and POEM for achalasia predict postoperative symptomatic outcomes. Surg Endosc. 2015;29(3):522–8. doi: 10.1007/s00464-014-3733-1. This study suggested that intra-operative FLIP may allow tailoring of achalasia LES myotomy to a target EGJ distensibility. They reported that a final intra-operative EGJ-DI of 4.5 – 8.5 mm2/mmHg following POEM or laparoscopic Heller myotomy was associated with lack of dysphagia or reflux symptoms in achalasia patients at follow-up of >6 months. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *26.Teitelbaum EN, Sternbach JM, El Khoury R, et al. The effect of incremental distal gastric myotomy lengths on EGJ distensibility during POEM for achalasia. Surg Endosc. 2015 doi: 10.1007/s00464-015-4269-8. Further supporting that intra-operative FLIP may be valuable as a tool to tailor the myotomy in POEM, this study demonstrated that EGJ-distensibility increased during creation of the submucosal tunnel and following extension of the EGJ myotomy 2-cm along the gastric wall; minimal gain in EGJ-distensibility was achieved with additional extension. [DOI] [PMC free article] [PubMed] [Google Scholar]
- **27.Kappelle WF, Bogte A, Siersema PD. Hydraulic dilation with a shape-measuring balloon in idiopathic achalasia: a feasibility study. Endoscopy. 2015;47(11):1028–34. doi: 10.1055/s-0034-1392481. This study demostrated the feasibility, safety, and short-term (up to 3-months) clinical effectiveness of the FLIP achalasia dilation balloon (dilation diameter of 30-mm) in 10 patients with achalasia. Using an external pressure sensor with the dilation balloon, they reported an increase in EGJ-distensibility immediately following dilation. [DOI] [PubMed] [Google Scholar]
- 28.Kwiatek MA, Kahrilas K, Soper NJ, et al. Esophagogastric junction distensibility after fundoplication assessed with a novel functional luminal imaging probe. J Gastrointest Surg. 2010;14(2):268–76. doi: 10.1007/s11605-009-1086-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Perretta S, Dallemagne B, McMahon BP, et al. Video. Improving functional esophageal surgery with a "smart" bougie: Endoflip. Surg Endosc. 2011;25(9) doi: 10.1007/s00464-011-1611-7. [DOI] [PubMed] [Google Scholar]
- 30.Perretta S, McAnena O, Botha A, et al. Acta from the EndoFLIP(R) Symposium. Surg Innov. 2013;20(6):545–52. doi: 10.1177/1553350613513515. [DOI] [PubMed] [Google Scholar]
- 31.Ilczyszyn A, Botha AJ. Feasibility of esophagogastric junction distensibility measurement during Nissen fundoplication. Dis Esophagus. 2013 doi: 10.1111/dote.12130. [DOI] [PubMed] [Google Scholar]
- 32.Hoppo T, McMahon BP, Witteman BP, et al. Functional lumen imaging probe to assess geometric changes in the esophagogastric junction following endolumenal fundoplication. J Gastrointest Surg. 2011;15(7):1112–20. doi: 10.1007/s11605-011-1562-2. [DOI] [PubMed] [Google Scholar]
- 33.Rinsma NF, Smeets FG, Bruls DW, et al. Effect of transoral incisionless fundoplication on reflux mechanisms. Surg Endosc. 2014;28(3):941–9. doi: 10.1007/s00464-013-3250-7. [DOI] [PubMed] [Google Scholar]
- 34.Dellon ES, Gonsalves N, Hirano I, et al. ACG clinical guideline: Evidenced based approach to the diagnosis and management of esophageal eosinophilia and eosinophilic esophagitis (EoE) Am J Gastroenterol. 2013;108(5):679–92. doi: 10.1038/ajg.2013.71. quiz 93. [DOI] [PubMed] [Google Scholar]
- 35.Schoepfer AM, Safroneeva E, Bussmann C, et al. Delay in diagnosis of eosinophilic esophagitis increases risk for stricture formation in a time-dependent manner. Gastroenterology. 2013;145(6):1230–6. e1–2. doi: 10.1053/j.gastro.2013.08.015. [DOI] [PubMed] [Google Scholar]
- 36.Gentile N, Katzka D, Ravi K, et al. Oesophageal narrowing is common and frequently under-appreciated at endoscopy in patients with oesophageal eosinophilia. Aliment Pharmacol Ther. 2014;40(11–12):1333–40. doi: 10.1111/apt.12977. [DOI] [PubMed] [Google Scholar]
- 37.Lin Z, Kahrilas PJ, Xiao Y, et al. Functional luminal imaging probe topography: an improved method for characterizing esophageal distensibility in eosinophilic esophagitis. Therap Adv Gastroenterol. 2013;6(2):97–107. doi: 10.1177/1756283X12470017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nicodeme F, Hirano I, Chen J, et al. Esophageal distensibility as a measure of disease severity in patients with eosinophilic esophagitis. Clin Gastroenterol Hepatol. 2013;11(9):1101–7. e1. doi: 10.1016/j.cgh.2013.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *39.Carlson DA, Lin Z, Rogers MC, et al. Utilizing functional lumen imaging probe topography to evaluate esophageal contractility during volumetric distention: a pilot study. Neurogastroenterol Motil. 2015;27(7):981–9. doi: 10.1111/nmo.12572. This study demonstrated a novel technique (FLIP topography) for evaluating distension-related esophageal contractions (i.e. secondary peristalsis) in asymptomatic volunteers. Thresholds for triggering contractility and contraction-associated parameters were also reported. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Regan J, Walshe M, Rommel N, et al. New measures of upper esophageal sphincter distensibility and opening patterns during swallowing in healthy subjects using EndoFLIP(R) Neurogastroenterol Motil. 2013;25(1):e25–34. doi: 10.1111/nmo.12041. [DOI] [PubMed] [Google Scholar]
- 41.Regan J, Walshe M, Rommel N, et al. A new evaluation of the upper esophageal sphincter using the functional lumen imaging probe: a preliminary report. Dis Esophagus. 2013;26(2):117–23. doi: 10.1111/j.1442-2050.2012.01331.x. [DOI] [PubMed] [Google Scholar]
- *42.Regan J, Walshe M, Timon C, et al. 'Endoflip(R) evaluation of pharyngo-oesophageal segment tone and swallowing in a clinical population: a total laryngectomy case series'. Clin Otolaryngol. 2015;40(2):121–9. doi: 10.1111/coa.12337. This study demonstrated the feasibility and safety of evaluating the distensibility and swallow-associated dynamics of the upper esophageal sphincter with FLIP in a clinical popultion: following laryngectomy. [DOI] [PubMed] [Google Scholar]