To the Editor: A 35-year-old female was admitted with a 6-day history of fever and sore throat. On admission, she was feverish, with a temperature of 40.2°C by rectum. Her pulse was regular at 90 beats/min, and blood pressure was 93/69 mmHg. Other findings were vomiting, abdominal pain, and a macular rash across the upper trunk. She also had abdominal tenderness in the right upper quadrant and epigastrium without guarding.
Laboratory data revealed a total white blood cell count of 6.42 × 109/L with 37% lymphocytes and 16%“atypical” lymphocytes [Figure 1a and 1b] on the blood film. A heterophile antibody test yielded a positive result the day after admission, and a clinical diagnosis of infectious mononucleosis was confirmed 7 days later with positive Epstein–Barr virus (EBV) serology-positive viral capsid antigen immunoglobulin M, negative viral capsid antigen immunoglobulin G (IgG), and EBV nuclear antigen IgG. Liver dysfunction was observed the day after admission, with the aspartate aminotransferase level of 130 μmol/L, alanine aminotransferase level of 70 μmol/L, serum amylase level of 1300 U/L (normal range: 30–110 U/L), urine amylase level of 2110 U/L (normal range: 32–641 U/L), and lipase level of 1450 U/L (normal range: 30–140 U/L). An abdominal ultrasound eliminated the possibility of pancreatitis caused by gallstones. Computerized tomography (CT) scan of the chest and abdomen revealed findings consistent with pneumonia and acute pancreatitis, namely multiple patches in both zones of the lung [Figure 1e] and pancreatic edema [Figure 1c]. Blood culture and a sputum culture were taken. Empirical antibiotic and antiviral therapy consisting of amoxicillin, clavulanate potassium, and acyclovir was administered intravenously. After consultation with a gastroenterologist, the patient fasted. She developed gastrointestinal decompression and was given somatostatin and parenteral nutrition support basic therapy. The patient recovered uneventfully by day 10 at discharge. The CT scan of the chest and abdomen showed mostly absorption of inflammation [Figure 1d and 1f].
Figure 1.
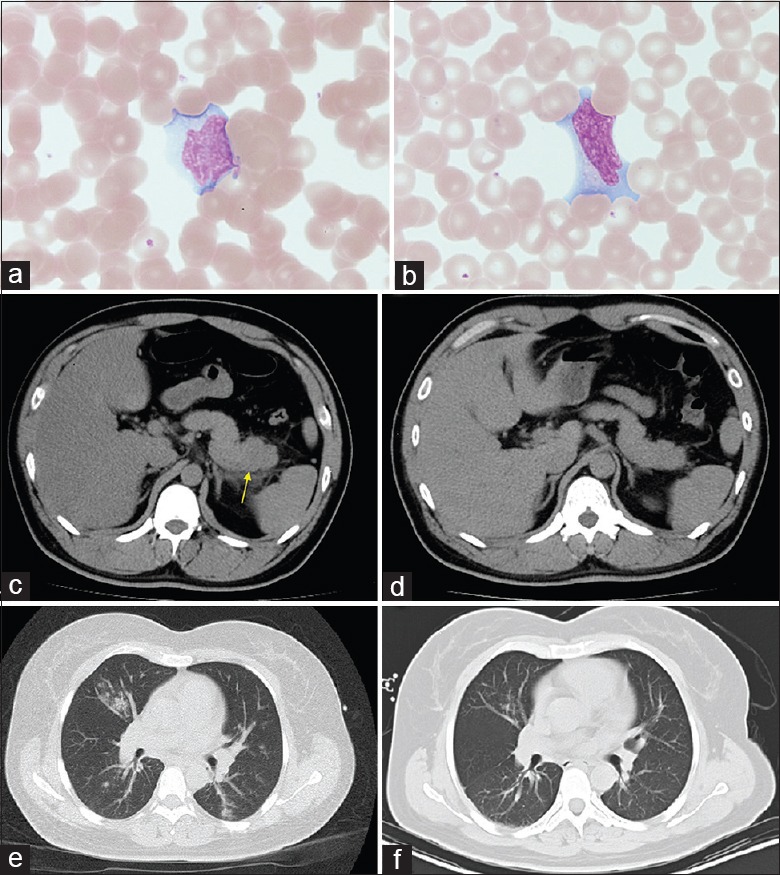
Blood film examination under microscopy and abdomen CT images of the patient. (a and b) Atypical lymphocytes (H and E, ×1000) in circulating blood. (c) CT images of abdomen showing edema of pancreatic tail (arrow) and increased peripheral fat density before treatment. (d) CT images of the abdomen after treatment showing mostly absorption of inflammation. (e) CT images showing patches in both zones of lung before treatment. (f) CT images showing mostly absorption of lung inflammation after treatment. CT: Computerized tomography.
Infectious mononucleosis is caused by EBV in 90% of cases.[1] It may account for about 1% of patients who present with a sore throat to their doctor. Nonspecific prodromal symptoms of fever and malaise may be seen in infectious mononucleosis. The likelihood of infectious mononucleosis is increased with the presence of posterior cervical adenopathy, inguinal or axillary adenopathy, palatine petechiae, and splenomegaly, whereas the likelihood reduces with the absence of any lymphadenopathy. The combination of a patient having greater than 50% lymphocytes and greater than 10% atypical lymphocytes is also useful.[2] However, the Hoagland criteria state that in patients presenting with clinically suspected infectious mononucleosis, the diagnosis should be confirmed using the heterophile antibody (monospot) test. A recent report showed that high-throughput sequencing served as a useful tool for the early detection and identification of EBV infection.[3]
Acute pancreatitis is an atypical complication of primary acute symptomatic EBV infection. A recent study integrated information on acute pancreatitis from 14 patients with primary acute EBV infection and suggested that the complication deserved attention, especially in cases with severe abdominal pain. Testing for pancreatic enzymes and CT scan of the abdomen are the most appropriate diagnostic tools. The review also concluded that the atypical complication was rather mild and recovered with no sequelae.[4] The pancreatitis was considered to be due to the involvement of pancreas in the inflammatory process of infectious mononucleosis; the underlying mechanism needs further exploration.
This study presented a rare case of a Chinese female who suffered from pancreatitis combined with EBV infection. The diagnosis of infectious mononucleosis was based on the patient's history, physical examination, laboratory findings, serological detection, and heterophile antibody test. Combined with increased serum lipase level and radiological evidence, the diagnosis of acute pancreatitis is not difficult. Treatment with gastrointestinal decompression, somatostatin, antibiotic, and acyclovir resulted in the complete recovery.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Qiang Shi
REFERENCES
- 1.Lennon P, Crotty M, Fenton JE. Infectious mononucleosis. BMJ. 2015;350:h1825. doi: 10.1136/bmj.h1825. doi: 10.1136/bmj. [DOI] [PubMed] [Google Scholar]
- 2.Ebell MH, Call M, Shinholser J, Gardner J. Does this patient have infectious mononucleosis? The rational clinical examination systematic review. JAMA. 2016;315:1502–9. doi: 10.1001/jama.2016.2111. doi: 10.1001/jama.2016.2111. [DOI] [PubMed] [Google Scholar]
- 3.Ni PX, Ding X, Zhang YX, Yao X, Sun RX, Wang P, et al. Rapid detection and identification of infectious pathogens based on high-throughput sequencing. Chin Med J. 2015;128:877–83. doi: 10.4103/0366-6999.154281. doi: 10.4103/0366-6999.154281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kottanattu L, Lava SA, Helbling R, Simonetti GD, Bianchetti MG, Milani GP. Pancreatitis and cholecystitis in primary acute symptomatic Epstein-Barr virus infection – Systematic review of the literature. J Clin Virol. 2016;82:51–5. doi: 10.1016/j.jcv.2016.06.017. doi: 10.1016/j.jcv.2016.06.017. [DOI] [PubMed] [Google Scholar]


