To the Editor: Elastosis perforans serpiginosa (EPS) is part of different kinds of perforating diseases that are dependent on factors such as idiopathic, reactive, or drug induced. We report here a case of a patient who presented with multiple reddish-brown keratinized papules coalescing to form serpiginous plaques in the anterior and posterior of the neck, which was found to be typical D-penicillamine-induced EPS.
A 39-year-old man presented with rash on his neck for 2 years without any pruritus or pain. His medical history was significant for hepatolenticular degeneration, diagnosed 20 years ago, for which he took oral D-penicillamine. No trauma, medication changes, environmental triggers, significant family history, other systemic diseases, or fibrous tissue diseases were identified. The rash were described as multiple reddish-brown keratinized papules forming irregular serpiginous plaques with central scaling and horns in the anterior and posterior of cervical region [Figure 1a and 1b]. Central mild atrophy and depigmentations were also seen. Two annular lesions were observed on the anterior neck. Microscopic examination and culture for fungus were negative. A skin biopsy taken from the raised border of the plaque revealed a typical transepidermal tunnel containing destroyed elastic fibers through the acanthotic epidermis. Abundant, abnormal elastic fibers were observed in the reticular dermis. EPS was diagnosed with further confirmation of histopathological examination [Figure 1c]. Further Verhoeff-van Gieson staining confirmed collagen fibers positive, elastic fibers positive [Figure 1d–1f].
Figure 1.
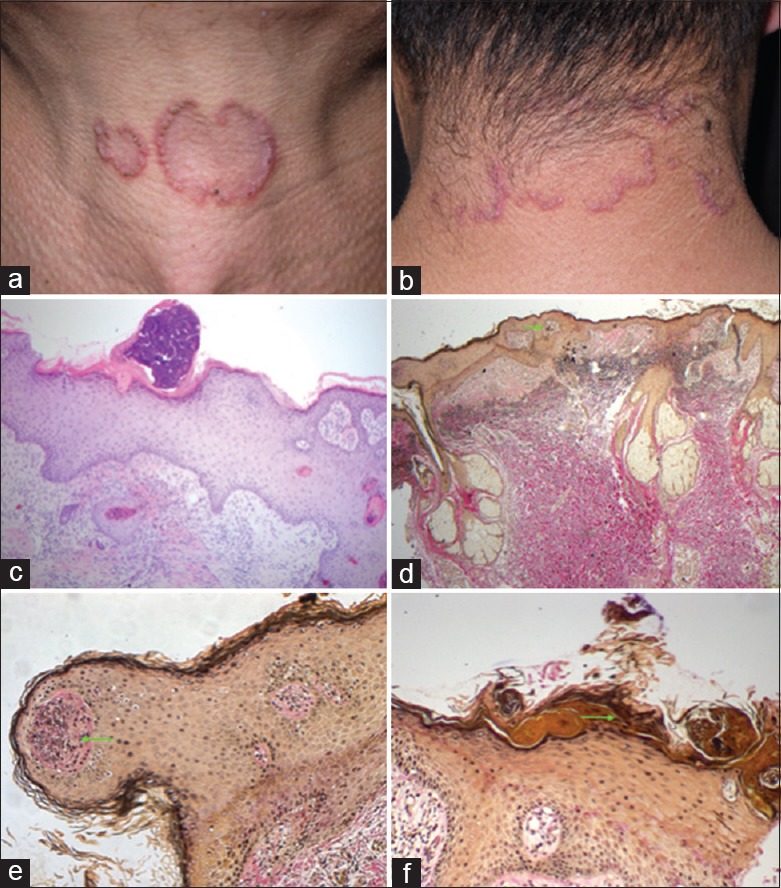
Representative images of the patient. D-penicillamine-induced elastosis perforans serpiginosa. (a and b) Physical examination showed multiple reddish-brown keratinized papules coalescing to form serpiginous plaques in the anterior and posterior of the neck. Scale and horny material can be observed in the center of the papules. (c) Epidermal hyperplasia with parakeratosis and dyskeratosis. Fiber necrosis can be observed in superficial dermis and especially in the stratum corneum. Lymphocyte, neutrophil infiltration is visible in focal location (Hematoxylin and Eeosin, ×100). (d) Elastic fibers mainly of the reticular dermis are coarser. Its perpendicular budding from the epidermis surface can be observed (arrow, Verhoeff-van Gieson staining, ×40). (e and f) Broken elastic fibers extruded through epidermis (arrow, Verhoeff-van Gieson staining, ×200).
EPS was a perforating disease that could be idiopathic, reactive, or drug induced. Idiopathic EPS, accounting for 65% of the total cases, might be related to genetics. Reactive EPS, accounting for approximately 25–30% of the total, was often associated with genetic diseases, systemic diseases, or other fibrous tissue degeneration diseases.[1] Reactive EPS could also be associated with other classic perforating diseases. A few could be secondary to endocrine or metabolic diseases. Drug-induced EPS was commonly associated with the use of penicillamine as previously observed by several reports.[2]
Clinically, EPS presented with serpiginous or annular patterned lesions up to several centimeters with or without pruritus. These lesions consisted of keratinized papules that were 2–5 mm in diameter and were typically located on the neck, face, arm, and other flexor surfaces. Some of these lesions resolved spontaneously, but most of them persisted for several years.
Two pathological mechanisms were proposed for D-penicillamine-induced EPS. First, the cross-linkage of elastic and collagen fibers in the derms by lysyl oxidase was copper dependent.[3] As D-penicillamine performed as a copper chelater, which indirectly inhibited the activity of lysyl oxidase, abnormal elastic fibers were formed and accumulated. Second, D-penicillamine might also lead to posttranslational inhibition of collagen synthesis that would result in defective cross-linking.[4]
Histopathologically, EPS was characterized by the increase in degenerated elastic fibers, predominately in the papillary layer of the dermis perforating through the epidermis. Small perforating tunnels on the epidermis were filled with keratotic plugs, which were composed of keratin material and degenerated basophilic material. Foreign body granulomatous composed by histiocytes and polykaryocyte could be observed. Moreover, elastic fiber staining showed increasing number of coarser elastic fibers in the dermis.
The treatment of EPS primarily consists of oral isotretinoin, intralesional injections of triamcinolone acetonide, topical application of tazarotene or allium cepa-allantoin-pentaglycan gel or cryotherapy. In addition, for our patient who requires penicillamine for his hepatolenticular degeneration, we suggest using zinc as a substitute.[5]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s)/patient's guardians has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients/patient's guardians understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
This work was supported by grants from the National Natural Science Foundation of China (No. 81402588), and the Beijing Municipal Natural Science Foundation (No. 7154247).
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Peng Lyu
REFERENCES
- 1.Lewis KG, Bercovitch L, Dill SW, Robinson-Bostom L. Acquired disorders of elastic tissue: Part I. Increased elastic tissue and solar elastotic syndromes. J Am Acad Dermatol. 2004;51:1–21. doi: 10.1016/j.jaad.2004.03.013. doi: 10.1016/j.jaad.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 2.Liang J, Wang D, Xu J, Chen L. Two cases of D-penicillamine-induced elastosis perforans serpiginosa. Indian J Dermatol Venereol Leprol. 2016;82:452–4. doi: 10.4103/0378-6323.178907. doi: 10.4103/0378-6323.178907. [DOI] [PubMed] [Google Scholar]
- 3.Matsuda I, Pearson T, Holtzman NA. Determination of apoceruloplasmin by radioimmunoassay in nutritional copper deficiency, Menkes’ kinky hair syndrome, Wilson's disease, and umbilical cord blood. Pediatr Res. 1974;8:821–4. doi: 10.1203/00006450-197410000-00001. doi: 10.1203/00006450-197410000-00001. [DOI] [PubMed] [Google Scholar]
- 4.Nimni ME. Penicillamine and collagen metabolism. Scand J Rheumatol. 1979;8(Suppl 28):71–7. doi: 10.3109/03009747909108241. doi: 10.3109/03009747909108241. [DOI] [PubMed] [Google Scholar]
- 5.Campanati A, Martina E, Giuliodori K, Ganzetti G, Marconi B, Conta I, et al. Elastosis perforans serpiginosa: A case successfully treated with intralesional steroids and topical allium cepa-allantoin-pentaglycan gel. Acta Dermatovenerol Alp Pannonica Adriat. 2014;23:39–41. doi: 10.15570/actaapa.2014.10. doi: 10.15570/actaapa.2014.10. [DOI] [PubMed] [Google Scholar]


