Abstract
Objectives
To date, there has been no evidence about objectively measured sleep characteristics from a representative national probability sample of adults in the United States. We used actigraphy to measure the sleep characteristics of older Americans.
Design
Cross-sectional study.
Setting
Sleep sub-study within Wave 2 (2010-2011) of the ongoing National Social Life, Health and Aging Project (NSHAP).
Participants
Seven hundred and thirty-nine NSHAP participants aged 62-90.
Intervention
Not applicable.
Measurements
Study participants wore a wrist actigraph for 72 hours and sleep properties were compared across demographic, socioeconomic, and health-behavior related lines.
Results
Actigraph-estimated sleep time averaged 7.2 hours (SE 0.06 hr) each night; the majority of the sample (80%) slept between 5.8 and 8.6 hours/night. Average time spent awake after sleep onset (WASO) was 39 minutes (SE 1.2 min). Women had significantly more total sleep time and lower sleep fragmentation compared to men. Total sleep time increased significantly with age although sleep percentage decreased with age. Compared with White participants, African American participants had significantly more WASO (9.2 minutes, p < 0.01) and greater sleep fragmentation (2.3 percentage points, p < 0.001). WASO was significantly higher and sleep percentage significantly lower among those with less education.
Conclusions
Both short sleepers and long sleepers – often conventionally defined as obtaining <6 and >9 hrs/night, respectively – are relatively rare among older Americans when sleep is estimated by actigraphy. Sleep quality is significantly poorer among men, African Americans, and those with less education.
Keywords: sleep, actigraphy, epidemiology, older adults
Introduction
Sleep characteristics including sleep duration and quality are of increasing interest to epidemiologists for their potential etiologic roles in a number of adverse health outcomes, including obesity, cardiovascular disease, and mortality.1-3 However, assessing sleep characteristics for community-based populations is complicated. The gold standard, polysomnography (PSG), is expensive and even home-based PSG is likely to disrupt routines, limiting its utility for understanding the sleep patterns of large numbers of individuals in natural settings. The most commonly used method for measuring sleep in large studies is through survey questions. However, a number of studies have demonstrated generally low correlations between self-reported and objective sleep measures of both duration and quality,4-8 suggesting that survey-based sleep measures may tap into different aspects of the experience or perception of sleep and do not simply reflect the sleep characteristic they appear to reference.
Wrist actigraphy is a practical method of estimating sleep objectively in large, free-living populations because it is does not disrupt routines and is reasonably low cost; estimates of sleep parameters from actigraphy have been shown to correspond reasonably well to those from PSG.9-11 The use of wrist actigraphy in large epidemiologic studies has yielded estimated sleep properties in several cohorts.11-14 However, previous cohorts with actigraphy have been geographically defined (both single site and multi-site studies) and not drawn from a national probability sample, and therefore the generalizability of sleep characteristics derived from these studies to the national population is unknown. Consequently, we do not have good answers to the following very basic question: How much and how well do Americans sleep?
Here we use nationally representative, actigraph-estimated sleep data in the U.S. to answer basic questions about sleep for older Americans aged 62 to 90 and to explore the relationship between sleep properties and sociodemographic factors and health behaviors.
Participants and Methods
Study Design and Subjects
This study employed a randomly-selected subsample of participants in the second wave of the National Social Life, Health, and Aging Project (NSHAP), a nationally representative longitudinal study of older Americans with in-home interviews.15,16 The first NSHAP data collection wave was in 2005-2006 and focused on individuals 57-85 years of age. Wave 2 of NSHAP data collection took place in 2010-11 and retained the excellent level of representativeness achieved in Wave 1.17
A randomly selected one-third of NSHAP participants in Wave 2 (2010-11) were invited to participate in the sleep sub-study.18 Of the 808 individuals in the Wave 2 sample and 309 spouses (or co-resident partners) invited, 80% (N=897) agreed to participate. The actigraphs were distributed from the central NSHAP office, and potential participants had to be re-contacted after the in-home interview to arrange device delivery. Ninety-five percent (N=849) of those who agreed to participate were successfully re-contacted and received the packet of materials for the sleep sub-study, including the wrist actigraph. Actiwatches were received back from 823 individuals. Of these, further exclusions occurred due to errors uploading data (N=4), blank data records indicating the watch was not worn (N=26), and, despite careful review, an absence of discernable rest intervals (N=13). We further restricted our analyses to participants aged 62-90 at the time of data collection (N=739) by excluding spouses outside the target age range.
Demographic and socioeconomic data, as well as data on health behaviors, were collected by trained interviewers during face-to-face interviews at study participants' homes using Computer-Assisted Personal Interviews (CAPI).15 Respondents who agreed to participate in the sleep sub-study were subsequently telephoned and then mailed wrist actiwatches and instructions on how to complete the actigraphy study, usually a few days following the in-home interview.18
These analyses used a de-identified dataset prepared for public release by the parent study. The University of Chicago IRB considers studies that use previously collected and de-identified data to be exempt from review.
Interview Data
Interviewers used structured questionnaires to identify study participants' gender, race/ethnicity, marital status, completed education, household income, household wealth, alcohol consumption, and tobacco use.
Race/ethnicity
Respondents were asked the following two questions to elicit race and ethnicity: (1) “Do you consider yourself primarily white or Caucasian, Black or African American, American Indian, Asian, or something else?” and (2) “Do you consider yourself Hispanic or Latino?” Using the answers to these questions, study participants were categorized into four race/ethnicity categories: White/Caucasian; Black/African American; Non-Black Hispanic; and Other.
Marital status
Respondents' current marital status was categorized for analysis as follows: married or living with a partner; divorced, separated, or never married; and widowed.
Socioeconomic status
We used three measures of socioeconomic status – educational attainment, household income, and household assets.
Educational attainment was categorized as less than high school degree; high school degree or some college; and bachelor's degree or more.
Household income was first queried with a global question asking respondents to approximate their household income prior to taxes or deductions. For those respondents who did not answer the global question, an unfolding bracket method of questions was employed. For example, respondents would be asked, “Would you say your household income was more than $50,000 or less than $50,000?” followed by more precise categories conditional on the first answer. Estimation of household income was then done using a multiple imputation technique that included the answers to the folding bracket questions and all predictors for each relevant regression model.
Household assets were assessed similarly to income. Respondents were first asked a global question about their total household assets: ““Now I'd like you to think about all of the assets of your household. These are things like your house (if you own it), your cars, other rental properties and businesses you own, and financial assets like savings accounts, stocks, bonds, mutual funds, and pensions. Altogether, how much would you say that amounted to, approximately, after accounting for the loans you might have to pay off?” Again, those respondents who did not answer the question were then asked a set of questions to bracket their household assets. Multiple imputation was then used to estimate household assets using the answers to the bracketing questions and the predictors in the relevant regression models.
Models predicting the sleep properties were fit first with the three socioeconomic measures (education, income, and assets) separately and then together. In all of these models, only education was significantly associated with the sleep properties and thus this was the only socioeconomic measure retained in the final models, presented below.
Body mass index (BMI)
Height and weight were measured in the participants' homes by the trained interviewers.19 Participants were asked to stand against a wall and then the interviewer placed a clipboard on top of the participant's head followed by a post-it note to mark the clipboard's place on the wall. Height was then measured with a tape measure from the floor to the post-it note. Weight was measured with clothes on using a Health-o-Meter digital scale (Model: HDL111DQ-60).
Body mass index (BMI) was calculated as weight per height squared (kg/m2). Body mass index was divided into categories using the standard definitions for underweight (<18.5 kg/m2), normal (18.5 – 24.9 kg/m2), overweight (25.0-29.9 kg/m2), obese (30.0-34.9 kg/m2), and morbidly obese (≥ 35.0 kg/m2).20,21 Only two individuals were classified as underweight, one of whom had a BMI of 18.47 and the second a BMI of 18.0. Given the paucity of individuals in the underweight category and their BMIs, the two underweight individuals were included in the normal weight category for the main analyses.
Alcohol consumption
Alcohol consumption was queried using a set of questions that enabled the calculation of the average number of alcoholic drinks consumed per week by each of the study participants. First, participants were asked: “Do you drink alcohol?” Those participants answering yes were then asked how many days per week they drink alcohol and how many drinks of alcohol were consumed on those days. For the analyses, participants were categorized into: no drinks per week; 1-7 drinks per week; and > 7 drinks per week.
Tobacco use
Study participants were dichotomized into those who reported currently smoking cigarettes versus those who did not, reports that correlated highly with cotinine in Wave 1.22
Physical activity
Study participants were asked a single question about how often they participated in physical activities such as walking, dancing, gardening, physical exercise, or sports. Response categories included a set of weekly and monthly frequencies; these categories were dichotomized for analysis into “little physical activity (<1 time per week)” and “some physical activity (≥1 time per week).”
Actigraphy Data
Study participants were instructed to wear the wrist actigraphs (Actiwatch Spectrum Model, Phillips Respironics, Bend, OR) for 72 hours and to push the event marker (which recorded a time stamp but did not affect the activity recording) just before trying to fall asleep for the night and when fully awake for the day. Actigraphy data were collected using 15-second epochs. Upon return of the Actiwatches, data were downloaded and analyzed using the manufacturer-developed and tested software programs (Actiware 5.5). The main rest interval for each individual was initially set by the manufacturer's software based on the activity pattern. These rest intervals were then each manually re-examined, prioritizing the event marker data, which the software did not use, also considering the light data, and reset if the interval set by the software failed to fully include the longest sleep interval.18
After the main rest intervals were established, the manufacturer software was used to generate the following characteristics for each individual for each night of sleep: total sleep time; time spent awake after sleep onset (WASO); time in bed; sleep percentage; and sleep fragmentation. Each 15-second epoch is scored as “sleep” or wake” on the basis of the total activity count; here, we used the manufacturer's recommended default cutoff of 40 to score each epoch as sleep or wake.23 Total sleep time is defined as the total number of minutes counted as sleep in the main rest interval. WASO is defined as the number of minutes scored as awake between the first epoch scored as sleep and waking in the morning. Time in bed is defined as the time between when a participant pushed the event marker in the evening and then pushed it again in the morning. Time in bed is missing for some nights when participants forgot to push the event marker. Sleep percentage is an index defined as the total sleep time divided by the sum of the total sleep time and WASO. Fragmentation is an index of restlessness during the sleep period expressed as a percentage. It is defined by the manufacturer's software as the sum of two percentages: (1) the percentage of the sleep period epochs spent moving; and (2) the percentage of immobile periods (i.e., contiguous epochs with no movement) that are only one minute in duration. Fragmentation is a useful actigraphy metric because it is an indicator of sleep disruption or disturbance24,25 and because it most closely approximates the PSG measure of microarousals, demonstrated to be associated with poor health outcomes.26
Each of the sleep metrics was averaged across the three nights of data or, for the participants with fewer than three nights of analyzable data (n=50), across the number of nights available. No significant differences were observed in any of the sleep metrics for those individuals contributing fewer than three nights of actigraphy compared to those with three full nights of actigraphy (results not shown).
Short and long sleep were defined on the basis of the distribution of average sleep times obtained by individuals in the sample, with the bottom 10% defined as those with short sleep, the top 10% as those with long sleep, and those in the middle as those with “normal” sleep, with survey weights applied. Although there are somewhat accepted standards for short and long sleep in the literature (often <6 hours for short sleep and >9 hours for long sleep), these standards are based on survey measures, which do not necessarily correlate well with actigraphy sleep measures.4,5 There is also a statistical advantage to defining short and long sleep this way: the numbers of individuals are the same in both categories, so that the statistical significance tests in the mutinomial regressions are not based on different sample sizes.
Statistical analysis
Given the complex survey design employed by NSHAP, we used survey-weighted procedures to yield accurate point estimates and standard errors for all descriptive analyses and regression analyses.27 All analyses were run using Stata SE version 13.1 (StataCorp, College Station, TX). We used t-tests and chi-square tests to test for gender differences in the sleep outcomes and multiple regression models to test for associations between multiple predictors and the sleep properties of interest, modeled continuously. Multinomial logistic regression was used to test for associations between the predictors and either short or long (vs. normal) sleep time.
Because earlier studies have consistently reported differences in objective sleep properties by gender,12,28,29 we thought it possible that gender might modify relationships between the sleep properties and age. Therefore, all analyses initially included gender*age interaction terms, which were only retained in the final models when significant.
Results
There were 739 participants aged 62-90 with sufficient actigraphy data for calculating the sleep duration and fragmentation measures (Tables 1 & 2). Of those 739 individuals, 736 had non-missing values for all of the covariates and thus comprised the analytic set for the multivariable models (Tables 3 – 5). Per the survey's intention, the sample had a broad representation of older Americans across race/ethnicity and socioeconomic groups (Table 1). Among the 739 individuals in the analytic sample, 600 used their event markers in the evening and morning, thus allowing for calculation of time in bed (Table 2).
Table 1.
Description of the study population from the NSHAP actigraphy sample, 2010-2011 (N=739), with survey weights applied.
| Characteristic | Men (N=348) | Women (N=391) |
|---|---|---|
| Age (years) (Mean (SD)) | 72.4 (7.4) | 71.2 (7.2) |
| Race/ethnicity (N=736) (%) | ||
| White | 83.2 | 83.3 |
| Black | 6.2 | 7.9 |
| Hispanic, non-Black | 7.4 | 4.7 |
| Other | 3.2 | 4.1 |
| Marital status (%) | ||
| Married or living with partner | 76.6 | 60.1 |
| Divorced, separated, or never married | 8.7 | 12.8 |
| Widowed | 14.7 | 27.1 |
| Education (%) | ||
| < High school | 13.6 | 13.1 |
| High school degree or some college | 56.7 | 71.0 |
| College degree or more | 29.7 | 15.9 |
| Household income (US $) (%) (N=577) | ||
| <15,000 | 7.9 | 11.5 |
| 15,000-24,000 | 10.8 | 16.9 |
| 25,000-49,000 | 30.5 | 30.5 |
| 50,000-99,000 | 32.5 | 33.4 |
| ≥100,000 | 18.3 | 7.7 |
| Household assets (US $) (%) (N=502) | ||
| <10,000 | 5.0 | 6.3 |
| 10,000-99,000 | 15.5 | 24.5 |
| 100,000-249,000 | 20.3 | 23.6 |
| 250,000-499,000 | 24.2 | 20.3 |
| ≥500,000 | 35.0 | 25.3 |
| BMI (%) | ||
| Normal (18.5-24.9 kg/m2) | 22.5 | 26.1 |
| Underweight (<18.5 kg/m2) | 0.14 | 1.6 |
| Overweight (25-29.9 kg/m2) | 37.8 | 35.1 |
| Obese (30-35 kg/m2) | 27.9 | 20.9 |
| Morbidly obese (>35 kg/m2) | 11.6 | 16.4 |
| Current smoker (%) | 16.4 | 11.9 |
| Alcohol consumption (N=729) (%) | 3.6 (7.9) | 1.7 (4.0) |
| None | 54.6 | 69 |
| 1-7 drinks/week | 32 | 25 |
| > 7 drinks/week | 13.4 | 6 |
| Frequency of physical activity (%) | ||
| Little physical activity (<1/wk) | 38 | 40 |
| Some physical activity (≥1/wk) | 62 | 60 |
Table 2.
Sleep properties of older Americans, aged 62-90, participating in the NSHAP study, 2010-11 (N=739), with survey weights applied.
| All participants (N=739) | Men (N=348) | Women (N=391) | P-value for gender differencea | |
|---|---|---|---|---|
| Total sleep time (hrs) (Mean (SE)) | 7.21 (0.055) | 7.03 (0.073) | 7.38 (0.078) | 0.003 |
| Wake after sleep onset (minutes) (Mean (SE)) | 38.7 (1.2) | 38.5 (1.4) | 38.8 (1.4) | 0.824 |
| Time in bed (hours) (N=600) (Mean (SE)) | 8.4 (0.07) | 8.3 (0.07) | 8.5 (0.099) | 0.018 |
| Sleep percentage (%) (Mean (SE)) | 82.4 (0.53) | 82.6 (0.72) | 82.2 (0.75) | 0.69 |
| Fragmentation (%, (Mean (SE)) | 14.4 (0.33) | 15.0 (0.44) | 13.9 (0.35) | 0.008 |
| Short sleepers (≤5.7 hours) Proportion (SE)) | 0.10 (0.01) | 0.12 (0.02) | 0.08 (0.02) | 0.04 |
| Long sleepers (≥8.7 hours) (Proportion (SE)) | 0.10 (0.02) | 0.07 (0.01) | 0.13 (0.02) |
Gender differences tested with t-tests and chi-square tests.
Table 3.
Results of multiple linear regression models testing for associations between objective sleep properties and demographic and socioeconomic variables among NSHAP study participants (2010-11); models also controlled for BMI category, alcohol consumption, current smoking, and physical activity level (N = 726).
| Predictors | Total sleep time (minutes) | WASO (minutes) | Time in bed (hours) (N=591) | Sleep percentage (%) | Sleep fragmentation (%) |
|---|---|---|---|---|---|
|
| |||||
| β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | |
| Female gender (males = reference) a | 25.8 (7.3)** | 4.1 (2.4) | 0.79 (0.19)*** | 0.17 (1.1) | -1.6 (0.45)** |
| Age (decades) | 11.9 (5.2)* | --- | -3.1 (0.81)*** | 0.60 (0.40) | |
| Age effect for men (decades)b (N=342) | --- | 3.3 (2.0) | 0.32 (0.13) * | --- | --- |
| Age effect for women (decades)b (N=384) | --- | -1.0 (1.5) | -0.22 (0.16) | --- | --- |
| pgender*age interaction term | --- | 0.013 | 0.001 | --- | --- |
| Race/ethnicity | |||||
| Non-Hispanic white | Ref | Ref | Ref | Ref | Ref |
| Black | -9.8 (9.6) | 9.2 (2.8)** | -0.10 (0.31) | -2.9 (1.6) | 2.3 (0.62)*** |
| Hispanic | -4.9 (10.6) | -1.1 (3.7) | -0.38 (0.22) | 1.6 (2.3) | -0.2 (0.68) |
| Other | -73.2 (20.1)** | -3.8 (3.9) | 0.10 (0.44) | 2.4 (3.2) | 1.9 (2.0) |
| Marital status | |||||
| Married/living with a partner | Ref | Ref | Ref | Ref | Ref |
| Divorced/separated/never married | -26.2 (10.5)* | 0.8 (3.3) | -0.24 (0.18) | -1.0 (1.9) | 0.58 (0.95) |
| Widowed | -7.8 (10.4) | 8.6 (2.6)** | -0.2 (0.2) | -4.2 (1.7)* | 1.28 (0.60)* |
| Educational attainment | |||||
| < High school degree | Ref | Ref | Ref | Ref | Ref |
| High school degree/some college | -14.3 (9.5) | -10.0 (4.0)* | -0.73 (0.2)*** | 5.8 (2.3)* | -1.3 (0.88) |
| Bachelor's degree or more | -12.6 (10.4) | -11.6 (3.4)** | -1.0 (0.23)*** | 6.1 (2.0)** | -1.55 (0.82) |
P<=0.05;
P <0.01;
P<0.001
Note that for those models including a gender × age interaction term, the female gender effect refers to those individuals at the youngest ages.
The sex-specific age effects were extracted from sex-stratified models, for ease of interpretation, when there was evidence of sex differences.
Table 5.
Relative risk ratios (RRRs) from multinomial logistic regression models testing associations between demographic, socioeconomic, and health behavior related variables and likelihood of being a short or long sleeper among NSHAP study participants (2010-11). Short and long sleepers were defined as the bottom and top 10th percentiles of the sample (≤5.7 hours and ≥8.7 hours, respectively). All predictors were included in each model (N = 726).
| Predictors | Short sleep (≤5.7 hours) | Long sleep (≥8.7 hours) |
|---|---|---|
|
| ||
| RRR (95% CI) | RRR (95% CI) | |
| Female gender (males = reference) | 0.5 (0.2, 1.1) | 1.9 (0.99, 3.8) |
| Age (in decades) | 0.57 (0.3, 0.96)* | 1.1 (0.7, 1.8) |
| Race/ethnicity | ||
| Non-Hispanic white | Ref | Ref |
| Black | 1.4 (0.6, 3.1) | 0.7 (0.3, 1.8) |
| Hispanic | 1.3 (0.54, 3.2) | 0.97 (0.3, 3.2) |
| Other | 9.2 (2.6, 32.2)** | 0.3 (0.02, 4.0) |
| Marital status | ||
| Married/living with a partner | Ref | Ref |
| Divorced/separated/never married | 1.7 (0.9, 3.2) | 0.6 (0.2, 1.8) |
| Widowed | 1.3 (0.5, 3.4) | 1.4 (0.7, 3.2) |
| Educational attainment | ||
| < High school degree | Ref | Ref |
| High school degree/some college | 0.97 (0.5, 1.9) | 0.5 (0.2, 1.2) |
| Bachelor's degree or more | 0.74 (0.41, 1.36) | 0.5 (0.1, 1.5) |
| BMI category | ||
| Normal (18.5-24.9 kg/m2)b | Ref | Ref |
| Overweight (25-29.9 kg/m2) | 0.6 (0.2, 1.5) | 1.4 (0.6, 3.4) |
| Obese (30-35 kg/m2) | 0.6 (0.2, 1.5) | 0.3 (0.1, 0.9)* |
| Morbidly obese (>35 kg/m2) | 0.8 (0.3, 2.4) | 0.6 (0.2, 1.6) |
| Health behaviors | ||
| Alcohol consumption | ||
| None | Ref | Ref |
| 1 – 7 drinks/week | 0.5 (0.3, 1.0)* | 0.8 (0.4, 1.8) |
| > 7 drinks/week | 1.0 (0.4, 2.8) | 1.2 (0.4, 3.4) |
| Current smoker | 2.3 (1.1, 4.7)* | 1.6 (0.8, 3.1) |
| Frequency of physical activity | ||
| Little physical activity (<1/wk) | Ref | Ref |
| Some physical activity (≥1/week) | 0.7 (0.4, 1.3) | 0.9 (0.4, 1.8) |
p<=0.05;
p<0.01
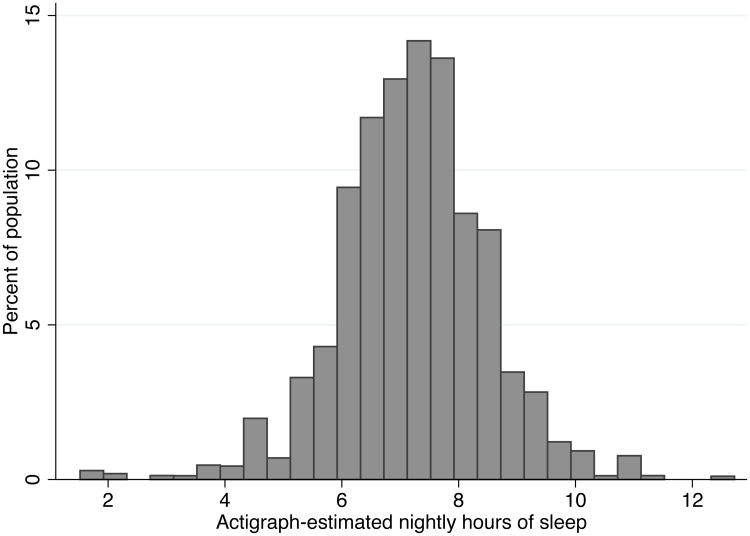
Average sleep duration was 7.2 hours each night (Table 2) and the distribution of total average sleep time across the population is shown in Figure 1. Wake after sleep onset, or WASO, averaged 39 minutes per night. Once sleep was initiated, 82% of the interval was spent sleeping (sleep percentage). A total of 8.4 hours were spent in bed, with time in bed measured as the time between respondents pushing the event marker in the evening and then pushing it again in the morning. The bottom decile of sleep duration, those we defined as short sleepers, slept ≤ 5.7 hours per night and the top decile, those we defined as long sleepers, slept ≥ 8.7 hours (Figure 1).
Figure 1.
Distribution of actigraph-estimated nightly total sleep time among older Americans, aged 62-90, participating in the NHSAP study (2010-11), with survey weights applied (N=739).
The results of our simplest models indicate that older women sleep significantly more than older men do each night – approximately 21 minutes more on average (Table 2). Consistent with this, women in this age group are less likely than men to be short sleepers and more likely to be long sleepers. We also observed that women had significantly reduced sleep fragmentation, as compared to men (Table 2).
Table 3 displays the results of adjusted models showing how each of the sleep properties of interest is patterned with regard to demographic and socioeconomic variables, controlling for health behaviors. For both total sleep time and sleep fragmentation, the gender pattern observed in the simpler model persisted, with women sleeping significantly more than men – approximately 26 minutes more per night, on average – and women having significantly less fragmented sleep as compared to men in the fully-adjusted model (Table 3).
Total sleep time increased with age, approximately 12 minutes per decade. Conversely, sleep percentage decreased significantly with age, approximately 3 percentage points per decade. Gender differences in how sleep was patterned with age were apparent for wake after sleep onset and time in bed, with both metrics increasing significantly with age in men, but not in women (Table 3).
Compared with White participants, African American participants had significantly more WASO (9.2 minutes more) and significantly greater sleep fragmentation (2.3 percentage points) compared with Whites (Table 3). Those in the “Other” race category had dramatically less sleep time (75.3 minutes) compared to Whites. This effect, however, was limited to women (data not shown) of whom there were only a very small number (N=12) in the “Other” race category.
Individuals who were divorced, separated, or never married had substantially less total sleep time compared with those participants who were married or currently living with a partner (26 fewer minutes) (Table 3). Widowed individuals had significantly more WASO (8 minutes), a significantly lower sleep percentage, and significantly greater sleep fragmentation (1.3 percentage points) than did partnered participants.
Educational attainment was associated with WASO and sleep percentage in a gradient like effect; those with more education spent less time awake after sleep onset and thus had a higher sleep percentage (Table 3).
Only two significant associations were observed between the health behaviors under study (BMI, alcohol consumption, smoking, or physical activity) and the sleep properties when these properties were modeled continuously (Table 4). Individuals consuming 1-7 alcoholic drinks per week had significantly less WASO (6.4 minutes) and lower sleep fragmentation (2.4 percentage points) compared to participants reporting no alcohol consumption.
Table 4.
Results of multiple linear regression models testing for associations between objective sleep properties and health-related factors among NSHAP study participants (2010-11); models also controlled for age, gender, race/ethnicity, marital status, and education (N = 726).
| Predictors | Total sleep time (minutes) | WASO (minutes) | Time in bed (hours) (N=591) | Sleep percentage (%) | Sleep fragmentation (%) |
|---|---|---|---|---|---|
|
| |||||
| β (SE) | β (SE) | β (SE) | β (SE) | β (SE) | |
| BMI category (Reference = 18.5-24.9 kg/m2)a | |||||
| Overweight (25-29.9 kg/m2) | 9.3 (8.7) | -0.66 (2.7) | 0.18 (0.17) | -0.21 (1.4) | 0.44 (0.8) |
| Obese (30-35 kg/m2) | -10.3 (9.2) | 2.3 (2.7) | 0.14 (0.16) | -2.0 (1.8) | 1.03 (0.81) |
| Morbidly obese (>35 kg/m2) | -5.1 (11.0) | 1.6 (3.4) | 0.12 (0.19) | -2.9 (2.0) | 1.4 (0.88) |
| Alcohol consumption (Reference = no drinks/wk) | |||||
| 1-7 drinks/week | 3.7 (9.4) | -6.4 (1.9)** | -0.03 (0.12) | 1.6 (1.1) | -2.4 (0.45)*** |
| >7 drinks/week | 0.87 (12.0) | 3.5 (2.9) | 0.24 (0.17) | -3.7 (1.8)* | 0.72 (0.87) |
| Current smoker (Reference = non-smoker) | -17.2 (10.8) | 3.8 (2.8) | -0.03 (0.24) | -1.1 (1.3) | 0.75 (0.69) |
| Physical activity (≥1/week) (Reference = <1/week) | 0.75 (6.7) | -1.8 (2.4) | -0.16 (0.13) | 1.9 (1.1) | -0.66 (0.69) |
P<=0.05;
P <0.01;
P<0.001
Note that the normal weight category also includes the two underweight individuals (see Methods).
Table 5 shows the results of multinomial logistic regression models testing for associations between demographic, socioeconomic, and health-behavior related variables and the likelihood of being in the short (≤5.7 hours) or long (≥8.7 hours) sleep categories. Each decade increase in age was associated with a decreased likelihood of being in the short sleep category (RRR = 0.57, 95% CI (0.3, 0.96)). Those in the “Other” race/ethnicity category and current smokers were significantly more likely to be in the short sleep category. Relative to participants reporting no alcohol consumption, participants reporting consuming 1-7 drinks per week were significantly less like to be in the short sleep category. Finally, compared to normal weight individuals, those in the obese category were significantly less likely to be in the long sleep category, but not more likely to be in the short sleep category.
Discussion
In this paper, we present the first nationally representative actigraphy estimates of nighttime sleep duration and quality for older Americans. Our findings indicate that community dwelling older Americans (aged 62-90 years) sleep, on average, just over 7 hours each night. They spend a total of 8.4 hours in bed with, on average, 39 minutes awake during the sleep period (WASO). The bottom and top deciles of the study population sleep ≤5.7 hours and ≥8.7 hours each night, respectively. We also observed a high sleep percentage despite common complaints about sleep among older individuals;30 once sleep had been initiated, 82% of the rest interval was spent sleeping.
Our results highlighted gender differences in the experience of sleep among older Americans. We found that women in this age range sleep more and have lower sleep fragmentation levels than do men; these findings are consistent with those in past cohort studies 12,28,29 and with a meta-analysis over a wider age range of sleep properties assessed with PSG or actigraphy conducted by Ohayon and colleagues.31 Further, we also observed significant gender-by-age interactions with regard to both WASO and time in bed. Our results suggest considering men and women separately when analyzing sleep in this age range.
We observed a significant increase in sleep time with age, in contrast to the meta-analysis by Ohayon et al., which found that for those aged 60 and above there was no significant age-related trend in total sleep. In the same meta-analysis, increases in WASO with age were reported, but the combined data indicate substantial variability in results among studies focused on participants 60 years of age and older.31
Our observations that sleep is patterned by social structural variables including race/ethnicity, socioeconomic status, and marital status also confirm associations reported in past studies, which have generally reported shorter and/or lower quality sleep for African Americans as compared to Whites,12,32,33 for those with lower vs. higher SES,12,32,33 and for non-partnered individuals compared to married individuals.34 The observed differences in actigraphy sleep measures suggest that sleep may mediate the effects of these fundamental socio-demographic characteristics on health. Our study's findings also highlight the potential role of sleep quality in the path from social factors to health outcomes, as WASO, sleep percentage, and sleep fragmentation were variously associated with the social structural factors that are themselves markers for higher health risk.
The relationship between sleep and body mass index is of substantial interest.3,13,35-37 While some prior studies have reported either longer and/or shorter sleep, on average, in association with increasing BMI,3,13,37 we observed no differences of note in any of the five sleep parameters across BMI groups. The only significant association identified was a reduced likelihood of obese individuals to be in the long sleep category versus the normal sleep category, as compared with normal weight individuals. However, obese individuals were not more likely to be in the short sleep category. While several reviews have found strong evidence of an association between sleep duration and BMI,38-40 two critical reviews on the topic have noted that the existing evidence is too variable and methodologically challenged to support a definitive or causal relationship between sleep duration and obesity.41,42 The general absence of BMI/sleep associations in our study may also be related to the older age range of the study population.
Our estimate of total sleep time among 62-90 year old Americans is higher than those reported by other studies employing actigraphy. Among cohorts of older individuals, arguably those most comparable with the NSHAP sample, average total nightly sleep time estimates have included 6.7 hours among women in the Study of Osteoporotic Fractures,14 6.4 hours among men in the MrOS Sleep Study,43 and 6.5 hours among the elderly community-dwelling participants in the Rotterdam study.13 The CARDIA study reported an average sleep duration one hour shorter than what we observed in the NSHAP sample – 6.2 hours – although the CARDIA study population was much younger, comprised of adults in early middle age (38-50 year olds).12
Sleep properties assessed through objective means have also been reported by studies employing in-home PSG, although these study populations had generally younger or broader age distributions than that in NSHAP. The largest of these – the Sleep Heart Health Study – included more than 2,000 individuals 40 years of age and older, with an average age of 67, and reported an average total sleep time of 6.05 hours.28 The SWAN study of women going through menopause (average age of 50) reported an average sleep duration of 6.4 hours.32 Another, smaller, study employing in-home PSG, the Pittsburgh Sleep SCORE project, reported average sleep times between 5 and 6 hours/night in its 187 middle-aged and older adult participants.33
Notably, all of these estimates, including ours, are substantially lower than values typically derived from self-report. For example, Gangwisch et al.44 reported sleep duration (self-reported) stratified by age in the 1982-1992 waves of the National Health and Nutrition Examinatin Surey (NHANES). Among the 60-86 year olds in the NHANES sample, 34%, and 14% of the sample reported typically sleeping 8 and 9 hours of sleep per night, respectively.44 By contrast, in the NSHAP sample, the actigraphy data indicate that only 17% and 7% of the participants slept 8 and 9 hours, respectively (data not shown). Correspondingly higher percentages of the NSHAP sample compared to the NHANES sample slept ≤ 5, 6, and 7 hours per night.
In contrast to total sleep time, time spent awake after sleep onset, or WASO, was substantially shorter among the NSHAP study participants in contrast to some past reports among older adults utilizing actigraphy. While our study participants spent approximately 39 minutes awake after sleep onset, previous cohorts have reported WASO values roughly double this – 78.4 minutes in the MrOS study,43 77.2 minutes in the Study of Osteoporotic Fractures,14 and 69.5 minutes in the Rotterdam study.45 Our WASO value looks much more similar to the 46 minutes reported for non-diabetic middle-aged adults in the CARDIA study46 and to the 52 minutes reported for the women in the SWAN Study.32 The reported WASO value in the Pittsburgh Sleep SCORE project was 77-87 minutes.33
The differences between the sleep time and WASO estimates from NSHAP and those of prior cohort studies are interesting and deserve consideration. One explanation could be differences in the populations being studied. The NSHAP population is nationally representative, which was not a sampling aim of prior studies. It is therefore possible that differences in the age structure and/or health properties of the populations being compared resulted in differences in sleep characteristics as well. For example, in the report cited from the Study of Osteoporotic Fractures,14 the average age of the women in the study was 83.5, more than a decade older than the NSHAP participants. The average age of men in the MrOS study43 was more similar to the NSHAP sample, but MrOS participants were recruited at clinical centers and screened for the use of mechanical devices during sleep. The Rotterdam Study is a population-based cohort study, but focuses solely on residents of a single district in Rotterdam.13
A second explanation could be differences across studies in actigraphy technology employed, although in general similar methods and instruments were used across studies. We used the standard manufacturer-supplied software to extract the sleep properties of interest, which is generally consistent with practices of other studies as well. 12-14 It should be noted, however, that inter-device reliability can be quite low,47 and thus could contribute to observed variability in estimates across studies. We used the manufacturer's recommended activity count threshold of 40 to differentiate sleep from wake; different activity count thresholds can yield different total sleep time values, with more sensitive thresholds yielding lower total sleep time.23 Finally, perhaps the scientific and popular attention devoted to the health consequences of short sleep in recent years has actually resulted in older adults sleeping more.
Although our study had a number of strengths, including measuring sleep with actigraphy in a nationally representative sample, there are also a number of limitations to consider. First, given that not all of the invited individuals agreed to participate in the sleep sub-study, the question of whether the sample remains representative arises. Relative to those in the total Wave 2 sample, we observed a slight over-representation of whites, females, and younger individuals.
Second, because we had small numbers of individuals in some of the analytic categories, we were unable to test for specific effects of, for example, being underweight on sleep or to fully examine differences across marital status types. Further, in the present study, we did not consider the relationship between sleep and either physical comorbidities or forms of psychological distress such as depression or anxiety among those in the NSHAP sample; this is a topic for future research.
An additional limitation is that we had just three nights of actigraphy, when more would be preferable. Although older adults would likely experience fewer work-related sleep schedule fluctuations relative to younger adults, substantial variability in their sleep patterns night to night has been observed.48 More nights of actigraphy would be required to estimate that variability properly and our estimates of the mean values are likely noisier than would be the case with more days, however they should not be systematically biased relative to estimates derived from more nights.49 When comparing our findings to those of others, however, it is unknown whether and to what extent different instruments across studies could play a role in the different estimates.
Conclusions
In summary, our data provide the first actigraphy-based evidence regarding sleep in a nationally representative sample of older Americans. These data can be used as reference data for smaller clinic-based populations. Our data suggest better population sleep of older adults in the U.S. in terms of both duration and consolidation than have previous cohort studies with similar measurements.
Acknowledgments
We thank Phil Schumm for his excellent technical assistance with the NSHAP data.
This work was supported by R01AG042164 from the National Institute of Aging and the Basic Behavioral and Social Sciences Research Opportunity Network (OppNet) at the National Institutes of Health. The core data collection in the National Social Life and Aging Project (NSHAP) was supported by R01 AG021487 and R01 AG033903 from the National Institute of Aging at the National Institutes of Health.
Footnotes
The work for this paper was performed at the University of Chicago and at Stanford University.
Conflicts of interest: None declared.
References
- 1.King CR, Knutson KL, Rathouz PJ, Sidney S, Liu K, Lauderdale DS. Short sleep duration and incident coronary artery calcification. Jama. 2008;300(24):2859–2866. doi: 10.1001/jama.2008.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kurina LM, McClintock MK, Chen JH, Waite LJ, Thisted RA, Lauderdale DS. Sleep duration and all-cause mortality: a critical review of measurement and associations. Annals of epidemiology. 2013;23(6):361–370. doi: 10.1016/j.annepidem.2013.03.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lauderdale DS, Knutson KL, Rathouz PJ, Yan LL, Hulley SB, Liu K. Cross-sectional and longitudinal associations between objectively measured sleep duration and body mass index: the CARDIA Sleep Study. American journal of epidemiology. 2009;170(7):805–813. doi: 10.1093/aje/kwp230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;19(6):838–845. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Den Berg JF, Van Rooij FJ, Vos H, et al. Disagreement between subjective and actigraphic measures of sleep duration in a population-based study of elderly persons. Journal of sleep research. 2008;17(3):295–302. doi: 10.1111/j.1365-2869.2008.00638.x. [DOI] [PubMed] [Google Scholar]
- 6.Chen JH, Waite L, Kurina LM, Thisted RA, McClintock M, Lauderdale DS. Insomnia Symptoms and Actigraph-Estimated Sleep Characteristics in a Nationally Representative Sample of Older Adults. The journals of gerontology Series A, Biological sciences and medical sciences. 2014 doi: 10.1093/gerona/glu144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Unruh ML, Redline S, An MW, et al. Subjective and objective sleep quality and aging in the sleep heart health study. Journal of the American Geriatrics Society. 2008;56(7):1218–1227. doi: 10.1111/j.1532-5415.2008.01755.x. [DOI] [PubMed] [Google Scholar]
- 8.Krystal AD, Edinger JD. Measuring sleep quality. Sleep medicine. 2008;9(1):S10–17. doi: 10.1016/S1389-9457(08)70011-X. [DOI] [PubMed] [Google Scholar]
- 9.Marino M, Li Y, Rueschman MN, et al. Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013;36(11):1747–1755. doi: 10.5665/sleep.3142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Blackwell T, Redline S, Ancoli-Israel S, et al. Comparison of sleep parameters from actigraphy and polysomnography in older women: the SOF study. Sleep. 2008;31(2):283–291. doi: 10.1093/sleep/31.2.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Blackwell T, Ancoli-Israel S, Redline S, Stone KL Osteoporotic Fractures in Men Study G. Factors that may influence the classification of sleep-wake by wrist actigraphy: the MrOS Sleep Study. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2011;7(4):357–367. doi: 10.5664/JCSM.1190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lauderdale DS, Knutson KL, Yan LL, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. American journal of epidemiology. 2006;164(1):5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 13.van den Berg JF, Knvistingh Neven A, Tulen JH, et al. Actigraphic sleep duration and fragmentation are related to obesity in the elderly: the Rotterdam Study. International journal of obesity. 2008;32(7):1083–1090. doi: 10.1038/ijo.2008.57. [DOI] [PubMed] [Google Scholar]
- 14.Blackwell T, Yaffe K, Ancoli-Israel S, et al. Poor sleep is associated with impaired cognitive function in older women: the study of osteoporotic fractures. The journals of gerontology. Series A, Biological sciences and medical sciences. 2006;61(4):405–410. doi: 10.1093/gerona/61.4.405. [DOI] [PubMed] [Google Scholar]
- 15.Jaszczak A, O'Doherty K, Colicchia M, et al. Continuity and Innovation in the Data Collection Protocols of the Second Wave of the National Social Life, Health, and Aging Project. The journals of gerontology Series B, Psychological sciences and social sciences. 2014 doi: 10.1093/geronb/gbu031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith S, Jaszczak A, Graber J, et al. Instrument development, study design implementation, and survey conduct for the national social life, health, and aging project. The journals of gerontology Series B, Psychological sciences and social sciences. 2009;64(1):i20–29. doi: 10.1093/geronb/gbn013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.O'Muircheartaigh C, English N, Pedlow S, Kwok PK. Sample design, sample augmentation, and estimation for Wave 2 of the NSHAP. The journals of gerontology Series B, Psychological sciences and social sciences. 2014;69(2):S15–26. doi: 10.1093/geronb/gbu053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lauderdale DS, Schumm LP, Kurina LM, et al. Assessment of sleep in the national social life, health, and aging project. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2014 doi: 10.1093/geronb/gbu092. Forthcoming. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams SR, Pham-Kanter G, Leitsch SA. Measures of chronic conditions and diseases associated with aging in the national social life, health, and aging project. The journals of gerontology Series B, Psychological sciences and social sciences. 2009;64(1):i67–75. doi: 10.1093/geronb/gbn015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults--The Evidence Report. National Institutes of Health. Obesity research. 1998;6(2):51S–209S. [PubMed] [Google Scholar]
- 21.Obesity: preventing and managing the global epidemic Report of a WHO consultation. World Health Organization technical report series. 2000;894:i–xii. 1–253. [PubMed] [Google Scholar]
- 22.Drum ML, Shiovitz-Ezra S, Gaumer E, Lindau ST. Assessment of smoking behaviors and alcohol use in the national social life, health, and aging project. The journals of gerontology Series B, Psychological sciences and social sciences. 2009;64(1):i119–130. doi: 10.1093/geronb/gbn017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lauderdale DS, Schumm LP. Response to Dr. Kawada. The journals of gerontology Series B, Psychological sciences and social sciences. 2015 doi: 10.1093/geronb/gbu221. [DOI] [PubMed] [Google Scholar]
- 24.Loewen A, Siemens A, Hanly P. Sleep disruption in patients with sleep apnea and end-stage renal disease. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2009;5(4):324–329. [PMC free article] [PubMed] [Google Scholar]
- 25.Rimmer J, Downie S, Bartlett DJ, Gralton J, Salome C. Sleep disturbance in persistent allergic rhinitis measured using actigraphy. Ann Allergy Asthma Immunol. 2009;103(3):190–194. doi: 10.1016/S1081-1206(10)60180-9. [DOI] [PubMed] [Google Scholar]
- 26.Thomas RJ. Sleep fragmentation and arousals from sleep-time scales, associations, and implications. Clin Neurophysiol. 2006;117(4):707–711. doi: 10.1016/j.clinph.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 27.O'Muircheartaigh C, Eckman S, Smith S. Statistical design and estimation for the national social life, health, and aging project. The journals of gerontology Series B, Psychological sciences and social sciences. 2009;64(1):i12–19. doi: 10.1093/geronb/gbp045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Silva GE, Goodwin JL, Sherrill DL, et al. Relationship between reported and measured sleep times: the sleep heart health study (SHHS) Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine. 2007;3(6):622–630. [PMC free article] [PubMed] [Google Scholar]
- 29.van den Berg JF, Miedema HM, Tulen JH, Hofman A, Neven AK, Tiemeier H. Sex differences in subjective and actigraphic sleep measures: a population-based study of elderly persons. Sleep. 2009;32(10):1367–1375. doi: 10.1093/sleep/32.10.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ancoli-Israel S, Ayalon L, Salzman C. Sleep in the elderly: normal variations and common sleep disorders. Harvard review of psychiatry. 2008;16(5):279–286. doi: 10.1080/10673220802432210. [DOI] [PubMed] [Google Scholar]
- 31.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27(7):1255–1273. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 32.Hall MH, Matthews KA, Kravitz HM, et al. Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep. 2009;32(1):73–82. [PMC free article] [PubMed] [Google Scholar]
- 33.Mezick EJ, Matthews KA, Hall M, et al. Influence of race and socioeconomic status on sleep: Pittsburgh SleepSCORE project. Psychosomatic medicine. 2008;70(4):410–416. doi: 10.1097/PSY.0b013e31816fdf21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Troxel WM, Buysse DJ, Matthews KA, et al. Marital/cohabitation status and history in relation to sleep in midlife women. Sleep. 2010;33(7):973–981. doi: 10.1093/sleep/33.7.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Taheri S, Lin L, Austin D, Young T, Mignot E. Short sleep duration is associated with reduced leptin, elevated ghrelin, and increased body mass index. PLoS medicine. 2004;1(3):e62. doi: 10.1371/journal.pmed.0010062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hasler G, Buysse DJ, Klaghofer R, et al. The association between short sleep duration and obesity in young adults: a 13-year prospective study. Sleep. 2004;27(4):661–666. doi: 10.1093/sleep/27.4.661. [DOI] [PubMed] [Google Scholar]
- 37.Patel SR, Blackwell T, Redline S, et al. The association between sleep duration and obesity in older adults. International journal of obesity. 2008;32(12):1825–1834. doi: 10.1038/ijo.2008.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity. 2008;16(3):643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Van Cauter E, Knutson KL. Sleep and the epidemic of obesity in children and adults. European journal of endocrinology / European Federation of Endocrine Societies. 2008;159(1):S59–66. doi: 10.1530/EJE-08-0298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marshall NS, Glozier N, Grunstein RR. Is sleep duration related to obesity? A critical review of the epidemiological evidence. Sleep medicine reviews. 2008;12(4):289–298. doi: 10.1016/j.smrv.2008.03.001. [DOI] [PubMed] [Google Scholar]
- 42.Nielsen LS, Danielsen KV, Sorensen TI. Short sleep duration as a possible cause of obesity: critical analysis of the epidemiological evidence. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2011;12(2):78–92. doi: 10.1111/j.1467-789X.2010.00724.x. [DOI] [PubMed] [Google Scholar]
- 43.Blackwell T, Yaffe K, Ancoli-Israel S, et al. Association of sleep characteristics and cognition in older community-dwelling men: the MrOS sleep study. Sleep. 2011;34(10):1347–1356. doi: 10.5665/SLEEP.1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Sleep duration associated with mortality in elderly, but not middle-aged, adults in a large US sample. Sleep. 2008;31(8):1087–1096. [PMC free article] [PubMed] [Google Scholar]
- 45.Luik AI, Zuurbier LA, Hofman A, Van Someren EJ, Tiemeier H. Stability and fragmentation of the activity rhythm across the sleep-wake cycle: the importance of age, lifestyle, and mental health. Chronobiology international. 2013;30(10):1223–1230. doi: 10.3109/07420528.2013.813528. [DOI] [PubMed] [Google Scholar]
- 46.Carnethon MR, De Chavez PJ, Lauderdale DS, Carson AP, Liu K, Knutson KL. Abstract MP90: Association of sleep duration and quality with incident diabetes: Coronary Artery Risk Development in Young Adults Sleep Study. Circulation. 2013;127(AMP) [Google Scholar]
- 47.Meltzer LJ, Walsh CM, Traylor J, Westin AM. Direct comparison of two new actigraphs and polysomnography in children and adolescents. Sleep. 2012;35(1):159–166. doi: 10.5665/sleep.1608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mezick EJ, Matthews KA, Hall M, et al. Intra-individual variability in sleep duration and fragmentation: associations with stress. Psychoneuroendocrinology. 2009;34(9):1346–1354. doi: 10.1016/j.psyneuen.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rowe M, McCrae C, Campbell J, et al. Actigraphy in older adults: comparison of means and variability of three different aggregates of measurement. Behavioral sleep medicine. 2008;6(2):127–145. doi: 10.1080/15402000801952872. [DOI] [PubMed] [Google Scholar]