Abstract
Purpose
To compare the efficacy and safety of open reduction and internal fixation through ilioinguinal approach and Stoppa approach for the treatment of displaced acetabular fractures.
Methods
Case-controlled trials (CCTs) published from January 2010 to August 2015 that compared the ilioinguinal approach and Stoppa approach in the management of displaced acetabular fractures were retrieved from the databases of Cochrane Library, Pubmed, CNKI, and so on. Methodological quality of the trials was critically assessed. Statistical software RevMan 5.0 was used for data analysis.
Results
Eight articles were included in the meta-analysis. Through comparing the efficacy and safety of ilioinguinal approach and Stoppa approach in the treatment of displaced acetabular fracture, statistical significance was found in the average operation time [WMD = 68.29, 95% CI (10.52, 126.05), p < 0.05] and the median intraoperative blood loss [WMD = 142.26, 95% CI (9.30, 275.23), p < 0.05]. However, there existed no statistical significance in the fracture end reset satisfaction rate [RR = 0.63, 95% CI (0.17, 2.37), p > 0.05], the early complications rate [RR = 0.89, 95% CI (0.33, 2.40), p > 0.05], the late complications rate [RR = 0.91, 95% CI (0.27, 3.01), p > 0.05], and Harris hip score good function rate [RR = 0.52, 95% CI (0.25, 1.10), p > 0.05].
Conclusion
Though both techniques can obtain satisfactory clinical functions in the treatment of displaced acetabular fractures, Stoppa approach is superior to the ilioinguinal approach in terms of operation time and intraoperative blood loss.
Keywords: Displaced acetabular fractures, Ilioinguinal approach, Stoppa approach, Meta-analysis
Introduction
It is widely accepted that the most important principle of displaced acetabular fracture treatment is anatomical restoration of the articular surface and stable fixation.1, 2, 3 Many studies demonstrated that anatomic reduction of shifting bone blocks leads to better clinical outcome for acetabular fractures, but reduction of displaced acetabular fractures remains a challenge,4, 5, 6 for even a small articular incongruence can result in joint degeneration in a short time.
Open reduction and internal fixation still is the best treatment for displaced acetabular fractures from the current research reports. The operative approaches to the displaced acetabular fractures can be classified into two categories: extrapelvic approaches and intrapelvic approaches. First described in 1961 by Letournel,7 the ilioinguinal approach is a typical extrapelvic approach which is used in anterior wall and column fractures. On the contrary, Stoppa approach belongs to the intrapelvic ones. It is named by Stoppa8 who described this approach for the treatment of intra-abdominal surgical diseases such as complicated groin and incisional hernias in 1989. Cole et al9 reported that the Stoppa approach could expose the quadrilateral surface, the pelvic medial wall and even extend to the sacroiliac joint. Thus it could safely and effectively be used for the treatment of displaced acetabular fractures. Given the specificity of reduction and fixation process, each approach bears different advantages and disadvantages in treating displaced acetabular fractures. Though abundant case-controlled trials (CCTs) have been undertaken to compare the outcomes and complications of the two approaches, their clinical merits and drawbacks remain in controversy. To choose the optimal treatment, a systematical review on the available evidence for those two methods is therefore needed.
The aim of the present study is to perform a meta-analysis of all the CCTs in the last five years to determine whether there were any significant differences in the average operation time, intraoperative blood loss, fracture end reset satisfaction rate, early/late complication rates, and the Harris hip score (HHS) good function rate.
Materials and methods
Search strategy
CCTs, both randomized controlled studies (RCTs) and retrospective case studies, which published from January 2010 to August 2015 and compared the ilioinguinal approach and Stoppa approach in the treatment of displaced acetabular fractures were searched from the Cochrane Library, PubMed, CNKI, Chinese Biomedical Database, and Wanfang Data manually. The searching key words were: acetabular fracture treatment, ilioinguinal approach and Stoppa approach.
Inclusion criteria
The inclusion criteria were: (1) adults with acetabular fractures; (2) CCTs; (3) comparison of ilioinguinal approach and Stoppa approach for the treatment of acetabular fractures; and (4) outcome measured in terms of average operation time, the median intraoperative blood loss, the fracture end reset satisfaction rate, the early/late complication rate, and the HHS good function rate.
Exclusion criteria
The exclusion criteria were: (1) case-based reports or reviews; (2) study objective or intervention measures failed to meet the inclusion criteria; (3) imprecise experimental design; and (4) with incomplete data.
Data extraction and quality assessment
Inclusion decisions were made independently by two reviewers according to the pre-stated eligible criteria. Disagreement between two reviewers was resolved by discussion or consultation with a third reviewer when necessary. The criteria included the following five items: (1) whether to adopt the random sequence generation; (2) whether to use the principle of allocation concealment; (3) whether to use the principle of blinding for the subjects, implementers and measurement; (4) whether to use incomplete data and selective reporting; and (5) whether there is any other bias. The relevant data recorded in this analysis included: on the one hand, the first author's name, published year, sample size, country of origin, duration of follow-up; on the other hand, the average operation time, the median intraoperatie blood loss, the fracture end reset satisfaction rate, the early complications rate, the late complications rate, the HHS good function rate, etc.
Statistical analysis
Data were independently entered into the RevMan 5.0 meta-analysis software program by two reviewers. Dichotomous outcomes were expressed in relative risk (RR) and the weighted mean difference (WMD) was used for continuous outcomes, both with 95% confidence intervals (95% CI). Heterogeneity was tested through both chi-square test and I2 test. A fixed-effects model was chosen when there was no statistical evidence of heterogeneity while random-effect model was adopted if significant heterogeneity was found. When heterogeneity occurred, the study population, treatment, outcome and methodologies were checked to determine where it came from. If the heterogeneity could not be quantitatively synthesized or its event rate was too low to be measured, qualitative evaluation was performed. A funnel plot was applied to assess the publication bias.
Results
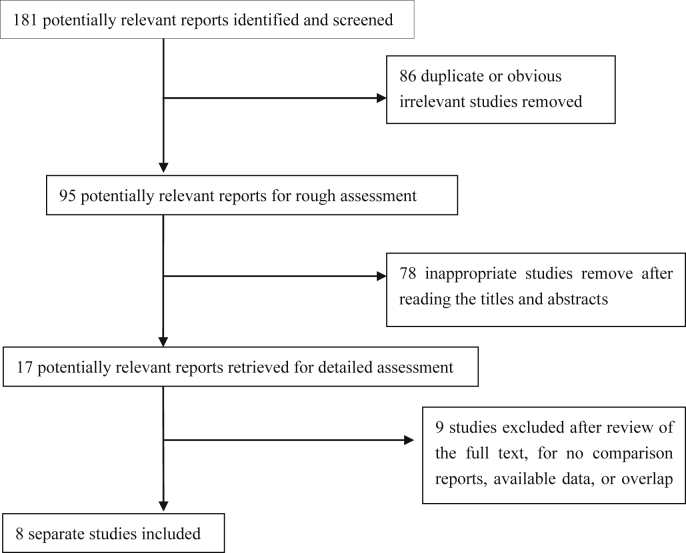
A total of 181 potentially relevant articles were identified. After screening the titles and abstracts, 164 studies were excluded. After reading the full-text of the remained 17 studies, we enrolled 8 studies on 637 patients that met all inclusion criteria,10, 11, 12, 13, 14, 15, 16, 17 including 2 English and 6 Chinese articles. Quality of the studies was evaluated by Jadad score.18 The total score is 7 points: ≤3 points defined as low quality study; ≥4 points as high quality paper. Therefore, 5 studies were regarded as high quality paper and 3 as medium quality paper11, 13, 17 (Fig. 1, Table 1).
Fig. 1.
Flow diagram of the study selection process.
Table 1.
General data of the included studies.
| Study | Country | Published year | Study design | Age (year) | Sample size Ili/Sto |
Follow-up time (month) |
|---|---|---|---|---|---|---|
| Mardian et al10 | Germany | 2015 | Retrospective | 57 | 56/44 | 12 |
| Shazar et al11 | Israel | 2013 | Retrospective | 41.5 ± 15.4 | 122/103 | 12 |
| Qiu et al13 | China | 2013 | Retrospective | 16–65 | 18/16 | 12 |
| Shen et al16 | China | 2014 | Retrospective | 45.2/46.5 | 21/19 | 12 |
| Xiong et al14 | China | 2015 | RCT | 41.2 ± 10.1 | 25/40 | 12 |
| Xu et al15 | China | 2014 | RCT | 46.7 ± 12.4 | 20/18 | 12 |
| Yuan et al17 | China | 2015 | Retrospective | 20–65 | 33/22 | 12 |
| Zhang et al12 | China | 2015 | RCT | 30.27 ± 6.02 | 40/40 | – |
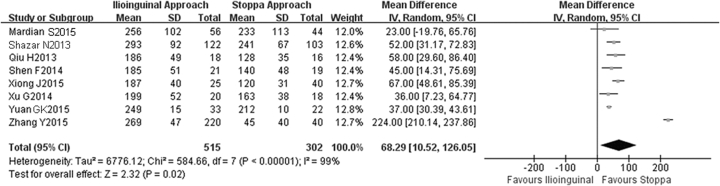
The average operation time
All of the 8 trials10, 11, 12, 13, 14, 15, 16, 17 compared the average operation time. Results showed much heterogeneity among the studies (I2 = 99%, p < 0.05), and the random model was performed. There was statistical difference between the two groups [WMD = 68.29, 95% CI (10.52, 126.05), p < 0.05, Fig. 2], suggesting that ilioinguinal approach requires a longer operation time than Stoppa approach in the treatment of displaced acetabular fractures.
Fig. 2.
The forest plot of the average operation time between two groups.
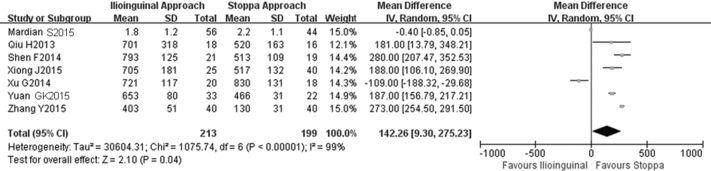
The median intraoperative blood loss
Seven trials10, 12, 13, 14, 15, 16, 17 reported the median intraoperative blood loss, showing obvious heterogeneity among the studies (I2 = 99%, p < 0.05), and the random model was performed. Results showed that ilioinguinal approach had much more blood loss than Stoppa approach [WMD = 142.26, 95% CI (9.30, 275.23), p < 0.05, Fig. 3].
Fig. 3.
The forest plot of the median intraoperative blood loss between two groups.
The fracture end reset satisfaction rate
Six trials10, 11, 14, 15, 16, 17 reported the fracture end reset satisfaction rate. Heterogeneity among the studies (I2 = 61%, p < 0.05) was found and the random model was performed. However, there was no statistical difference between the two groups [RR = 0.63, 95% CI (0.17, 2.37), p > 0.05, Fig. 4].
Fig. 4.
The forest plot of the rate of fracture end reset satisfaction between two groups.
The early complication rate
Six trials10, 11, 13, 15, 16, 17 studying the early complication rate showed much evidence of heterogeneity across the studies (I2 = 58%, p < 0.05). Though the random model was performed, no statistical difference between the two groups was found [RR = 0.89, 95% CI (0.33, 2.40), p > 0.05, Fig. 5].
Fig. 5.
The forest plot of the early complications rate between two groups.
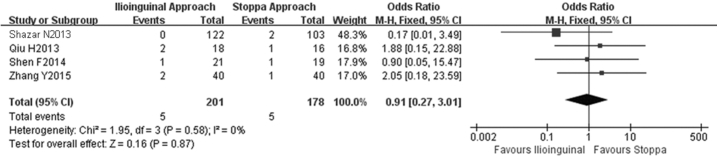
The late complication rate
Four trials11, 12, 13, 16 applied the late complication rate, showing little evidence of heterogeneity across the studies (I2 = 0%, p > 0.05), and thus the fixed model was performed, suggesting no statistical difference between the two groups [RR = 0.91, 95% CI (0.27, 3.01), p > 0.05, Fig. 6].
Fig. 6.
The forest plot of the late complications rate between two groups.
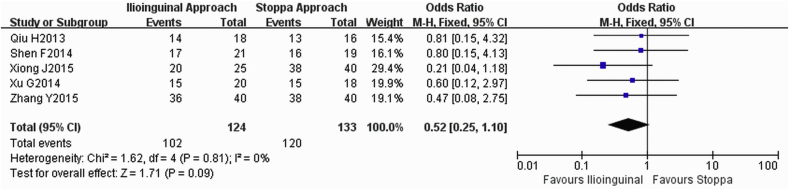
The HHS good function rate
Five trials12, 13, 14, 15, 16 included the HHS good function of operational hip rate, whose results demonstrated little evidence of heterogeneity across the studies (I2 = 0%, p > 0.05), and the fixed model was performed. There was no statistical difference between the two groups [RR = 0.52, 95% CI (0.25, 1.10), p > 0.05, Fig. 7].
Fig. 7.
The forest plot of the rate of HHS good function rate between two groups.
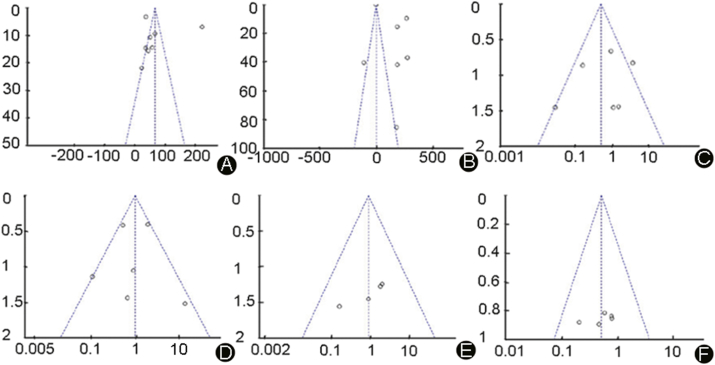
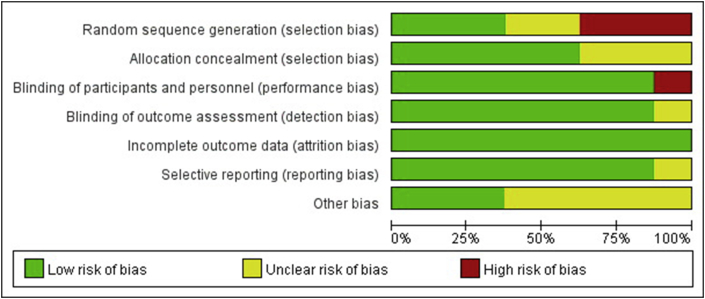
Publication bias
All the 8 studies included in this meta-analysis have gone through a strict quality assessment. All of them were CCTs with a low possibility of a bias. Nevertheless, the funnel figure showed that there was a small bias, which may be associated with the incomplete collection of relevant literature, insufficient sample size and the different proficiency of clinical physicians. Sensitivity analysis however showed a good overall result (Fig. 8, Fig. 9, Fig. 10).
Fig. 8.
The funnel figures of the evaluation projects. A: average operation time, B: the median intraoperatie blood loss, C: fracture end reset satisfaction, D: the early complications rate, E: the late complications rate, F: HHS good function rate.
Fig. 9.
Risk of bias. Each risk of bias item is presented as a percentage across all included studies and indicates the proportional level for each risk of bias item.
Fig. 10.
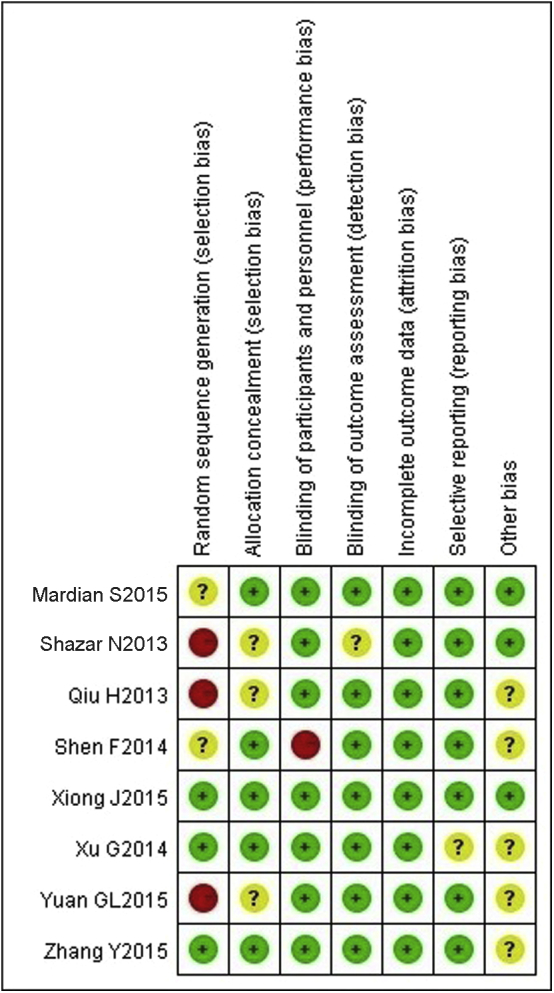
Methodological quality of the included studies. This risk of bias tool incorporates assessment of randomization (sequence generation and allocation concealment), blinding (participants, personnel and outcome assessors), completeness of outcome data, selection of outcomes reported and other sources of bias. The items were scored with ‘‘yes’’, ‘‘no’’, or ‘‘unsure’’.
Discussion
ORIF remains the gold standard for the treatment of most displaced acetabular fractures.19, 20, 21, 22, 23, 24 For the acetabular fracture when anterior access is needed, be it in anterior column, transverse, T-type fractures, etc, both the ilioinguinal approach and Stoppa approach can be used.18 However, the purpose of this review is to provide further insight into the options of the two approaches for treating displaced acetabular fractures by focusing on the efficacy and safety. From this meta-analysis, the average operation time and the median intraoperative blood loss bear statistical difference between two approaches. In other words, the average operation time was significantly shorter and the median intraoperative blood loss was obviously less for Stoppa approach. However in terms of the fracture end reset satisfaction rate and early/late complication rates, no statistical difference was found. The early complications evaluated included secondary surgery and wound infection; the late ones involved fracture nonunion and progression of hip arthritis. The merits of the HHS good function rate after surgery have a great impact on the quality of the patient's life. In present meta-analysis, there was no difference between the two groups in that regard.
The choice of surgical approaches to treat displaced acetabular fractures has beset the surgeons with uncertainty for a long time; we believe that this study now provides evidence to guide clinical practice. But our meta-analysis has some limitations. First, only 8 CCTs were included. Second, the follow-up periods of most studies were not long enough to confirm the results. Third, most of the retrieved documents were in Chinese and there may be language bias.
In conclusion, this study confirms that there were no significant differences in functional outcome between using ilioinguinal approach and Stoppa approach in the treatment of displaced acetabular fractures, but the former has longer operation time and more intraoperative blood loss. We hope there will be more multicentre, large-scale and high quality CCTs to further prove the conclusion.
Fund
This study was funded by the National Natural Science Foundation of China (No.81572098) and Natural Science Foundation of Shanxi Province of China (No. 2008012011-3).
Footnotes
Peer review under responsibility of Daping Hospital and the Research Institute of Surgery of the Third Military Medical University.
References
- 1.Salama W., Mousa S., Khalefa A. Simultaneous open reduction and internal fixation and total hip arthroplasty for the treatment of steoporotic acetabular fractures. Int Orthop. 2017;41:181–189. doi: 10.1007/s00264-016-3175-6. [DOI] [PubMed] [Google Scholar]
- 2.Peng Y., Zhang L., Min W. Comparison of anterograde versus retrograde percutaneous screw fixation of anterior column acetabular fractures. Int J Comput Assist Radiol Surg. 2016;11:635–639. doi: 10.1007/s11548-015-1308-9. [DOI] [PubMed] [Google Scholar]
- 3.Anizar-Faizi A., Hisam A., Sudhagar K.P. Outcome of surgical treatment for displaced acetabular fractures. Malays Orthop J. 2014;8:1–6. doi: 10.5704/MOJ.1411.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giannoudis P.V., Grotz M.R., Papakostidis C. Operative treatment of displaced fractures of the acetabulum. A meta-analysis. J Bone Jt Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 5.Chaus G.W., Heng M., Smith R.M. Occult internal iliac arterial injury identified during open reduction internal fixation of an acetabular fracture: a report of two cases. Injury. 2015;46:1417–1422. doi: 10.1016/j.injury.2015.04.030. [DOI] [PubMed] [Google Scholar]
- 6.Sagi H.C., Afsari A., Dziadosz D. The anterior intra-pelvic (modified rives- Stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010;24:263–270. doi: 10.1097/BOT.0b013e3181dd0b84. [DOI] [PubMed] [Google Scholar]
- 7.Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993;292:62–76. [PubMed] [Google Scholar]
- 8.Stoppa R.E. The treatment of complicated groin and incisional hernias. World J Surg. 1989;13:545–554. doi: 10.1007/BF01658869. [DOI] [PubMed] [Google Scholar]
- 9.Cole J.D., Bolhofner B.R. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994;305:112–123. [PubMed] [Google Scholar]
- 10.Mardian S., Schaser K.D., Hinz P. Fixation of acetabular fractures via the ilioinguinal versus pararectus approach: a direct comparison. Bone Jt J. 2015;97-B:1271–1278. doi: 10.1302/0301-620X.97B9.35403. [DOI] [PubMed] [Google Scholar]
- 11.Shazar N., Eshed I., Ackshota N. Comparison of acetabular fracture reduction quality by the ilioinguinal or the anterior intrapelvic (modified rives–Stoppa) surgical approaches. J Orthop Trauma. 2014;28:313–319. doi: 10.1097/01.bot.0000435627.56658.53. [DOI] [PubMed] [Google Scholar]
- 12.Zhang Y. The effect of ilioinguinal approach versus Stoppa approach for fixation of acetabular and pelvic fractures. Contemp Med. 2015;21:75–76. [Google Scholar]
- 13.Qiu H. Nanchang University; Nan Chang China: 2013. Effectiveness Comparison of Modified-Stoppa Approach and Ilioinguinal Approach in Treatment of Acetabular Fractures. [Google Scholar]
- 14.Xiong J. Contrast and analysis the curative effect of treatment on pelvic fracture and acetabular fracture by modified Stoppa approach and ilioinguinal approach. Med Innov China. 2015;12:81–83. [Google Scholar]
- 15.Xu G., Tang X.Z., Wang J. Modified Stoppa approach versus ilioinguinal approach for fixation of acetabular and pelvic fractures. Chin J Bone Jt Inj. 2014;29:521–523. [Google Scholar]
- 16.Shen F. Soochow University; Su Zhou China: 2014. Application and Comparison of Modified Rives-stoppa Approach in Acetabular Fracture Surgery. [Google Scholar]
- 17.Yuan G.K., Wei L.X., Zhang Y.D. Comparison study on modified Rives-Stoppa approach and ilioinguinal approach in treatment of acetabular fractures. China Mod Dr. 2015;53:123–125. [Google Scholar]
- 18.Jadad A.R., Moore R.A., Carroll D. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 19.Gänsslen A., Grechenig S.T., Nerlich M. Standard approaches to the acetabulum part 2: ilioinguinal approach. Acta Chir Orthop Traumatol Cech. 2016;83:217–222. [PubMed] [Google Scholar]
- 20.Wang P., Zhu X., Xu P. Modified ilioinguinal approach in combined surgical exposures for displaced acetabular fractures involving two columns. Springerplus. 2016;5:1602. doi: 10.1186/s40064-016-3316-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hartung M.P., Tutton S.M., Hohenwalter E.J. Safety and efficacy of minimally invasive acetabular stabilization for periacetabular metastatic disease with thermal ablation and augmented screw fixation. J Vasc Interv Radiol. 2016;27:682–688. doi: 10.1016/j.jvir.2016.01.142. [DOI] [PubMed] [Google Scholar]
- 22.Sen M.K., Warner S.J., Sama N. Treatment of acetabular fractures in adolescents. Am J Orthop (Belle Mead NJ) 2015;44:465–470. [PubMed] [Google Scholar]
- 23.Li Y.L., Tang Y.Y. Displaced acetabular fractures in the elderly: results after open reduction and internal fixation. Injury. 2014;45:1908–1913. doi: 10.1016/j.injury.2014.09.004. [DOI] [PubMed] [Google Scholar]
- 24.Mears D.C., Velyvis J.H., Chang C.P. Displaced acetabular fractures managed operatively: indicators of outcome. Clin Orthop Relat Res. 2003;407:173–186. doi: 10.1097/00003086-200302000-00026. [DOI] [PubMed] [Google Scholar]