Abstract
Objective
To explore and identify factors that influence physicians’ decisions while monitoring patients with prostate cancer on active surveillance (AS).
Subjects and methods
A purposive sampling strategy was used to identify physicians treating prostate cancer from diverse clinical backgrounds and geographic areas across the USA. We conducted 24 in-depth interviews from July to December 2015, until thematic saturation was reached. The Applied Thematic Analysis framework was used to guide data collection and analysis. Interview transcripts were reviewed and coded independently by two researchers. Matrix analysis and NVivo software were used for organization and further analysis.
Results
Eight key themes emerged to explain variation in AS monitoring: (i) physician comfort with AS; (ii) protocol selection; (iii) beliefs about the utility and quality of testing; (iv) years of experience and exposure to AS during training; (v) concerns about inflicting ‘harm’; (vi) patient characteristics; (vii) patient preferences; and (viii) financial incentives.
Conclusion
These qualitative data reveal which factors influence physicians who manage patients on AS. There is tension between providing standardized care while also considering individual patients' needs and health status. Additional education on AS is needed during urology training and continuing medical education. Future research is needed to empirically understand whether any specific protocol is superior to tailored, individualized care.
Keywords: prostate cancer, active surveillance, markers, qualitative, survey
Introduction
Many prostate cancers are unlikely to cause harm during a man's lifetime and can be safely managed conservatively, with active surveillance (AS) or watchful waiting (WW). AS involves serial testing (e.g. PSA, DRE, biopsy) to monitor for disease reclassification over time and offer selective curative intervention, whereas, WW is a less intensive observation approach without curative intent. Recent data from the US CaPSURE registry showed increasing use of AS/WW, with its use in 40.4% of low-risk cases and in 76.2% of men aged ≥75 years in 2010–2013 [1]. Despite similar increasing global trends [2, 3], there remains no consensus regarding patient selection and follow-up protocols, with multiple divergent published protocols and guidelines [4–8].
Several small quantitative surveys have examined this heterogeneity in AS practice [9]. Gorin et al. [10] reported a survey of 387 urologists primarily based in the USA. While 94% and 74% of respondents agreed that eligibility should be limited to men with PSA levels ≤10 ng/mL and Gleason scores ≤6, respectively, there was no consensus regarding the timing of follow-up biopsies and use of PSA kinetics.
A 2012–2013 survey of 35 British physicians found general consensus that patients with Gleason score 6, stage ≤T2 cancer, and PSA levels ≤10 ng/mL are suitable for AS [11]; however, there was less consensus about the suitability of intermediate-risk patients for AS, and regarding the use of age and MRI in candidate selection. There was also significant heterogeneity between respondents in the frequency of PSA testing, use of DRE, and timing of repeat biopsies.
The aim of the present study was to examine the motivations behind physician decision-making in relation to AS monitoring practices, given that there is no internationally accepted standard. Qualitative methods are particularly valuable for understanding phenomena from the perspective of study participants and to uncover the beliefs, values and motivations behind individual behaviour [12]. Identifying which factors influence physicians’ decisions during AS is an important first step to understanding how we can improve surveillance.
Subjects and Methods
From July to December 2015, we conducted semi-structured, in-depth interviews with prostate cancer physicians. First we purposively sampled urologists from the AUA to obtain detailed perspectives from experts in the field, including geographically diverse settings across the USA [13]. Purposive sampling is a non-probability sampling technique used to ascertain information about a specific population [13]. A snowball recruitment strategy was used, in which initial informants could then nominate other potential participants through connections in the field, including providers with different expertise involved in the care of patients on active surveillance [14].
Physicians were eligible if they reported currently caring for patients undergoing AS in the USA. We sent email invitations to a total of 48 physicians and conducted 24 interviews until we reached thematic saturation, wherein the research team reached consensus that no new themes were emerging from the interviews and therefore no further interviews were necessary [15, 16].
The study was approved by the institutional review board. Prior to the interview, all participants provided written informed consent and completed intake questionnaires with demographic information and criteria for patient selection and monitoring during AS.
Interviews
Qualitative interviews formed the primary data collection for our study. The research team developed an interview guide based on a literature review and previous research on AS [17–20]. We tested the guide with two pilot interviews and then modified it to improve clarity. Interview questions focused on specific protocols for monitoring during AS, how physicians chose the frequency of follow-up tests, opinions about testing options, and comfort with AS (Appendix 1). S.L. and E.S. conducted interviews in-person or by telephone, which lasted a mean (range) of 36 (22–51) min.
Analysis
Responses to intake questionnaires were recorded in the secure Research Electronic Data Capture (REDCap) portal, and descriptive statistics were used to aggregate the results. We audio-recorded all interviews and focus groups, and a third-party service anonymously transcribed them. Transcripts were entered into NVivo10 qualitative software for data management and retrieval [21, 22].
We analyzed transcripts using Applied Thematic Analysis, an inductive set of procedures designed to identify and examine emerging themes from conceptual data [23]. Two researchers independently reviewed transcripts to develop an initial codebook and coded each transcript, modified the codebooks as themes emerged, and met to discuss and reconcile discrepancies until a final coded transcript was agreed upon. The team resolved disagreements around codes, themes, and subthemes by discussion or by going back to the original transcripts. Finally, themes from interviews and focus groups were organized using descriptive matrix analyses that visually displayed the range of responses related to each theme.
Results
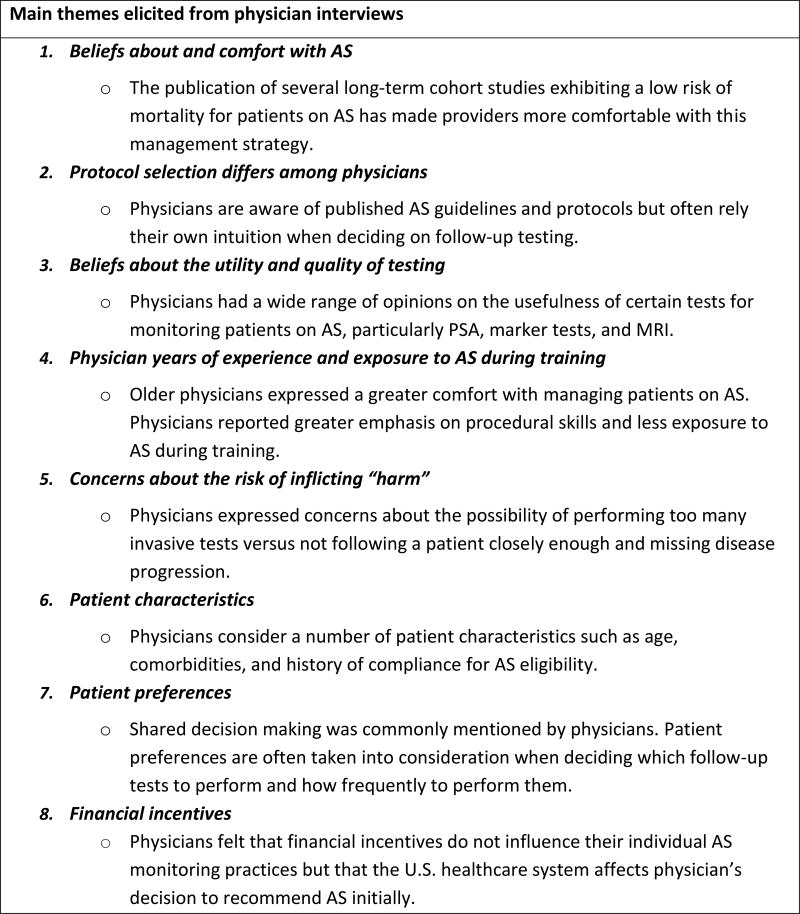
Table 1 shows the demographics of the study population. The majority of participants were urologists (83%), with a primary expertise of prostate cancer or urologic oncology (83%). The participants practiced in a variety of settings across 11 states. Physicians reported a variety of factors that affected how they monitored patients on AS and their comfort with current monitoring practices. Eight key themes were identified to explain the variability in AS protocols (Figure 1), which are further described with quotes.
Table 1.
Demographics table (n = 24).
| Median (range) age, years | 43 (33–70) |
|---|---|
|
| |
| Gender, n (%) | |
| Men | 22 (91.7) |
| Women | 2 (8.3) |
|
| |
| Race/ethnicity, n (%) | |
| White | 15 (62.5) |
| Black | 1 (4.2) |
| Other | 8 (33.3) |
|
| |
| Type of provider, n (%) | |
| Urologist | 20 (83.3) |
| Radiation oncologist | 3 (12.5) |
| Naturopathic doctor | 1 (4.2) |
|
| |
| Years in practice | |
| Median (range) | 10 (1–40) |
| Mean (SD) | 14.3 (11.8) |
|
| |
| Practice location (multiple affiliations possible), n (%) | |
| Academic | 18 (75.0) |
| VA Medical Center | 5 (20.8) |
| Military Hospital | 1 (4.2) |
| Private practice | 2 (8.3) |
| Private hospital | 1 (4.2) |
| Public hospital | 1 (4.2) |
|
| |
| Geographical location, n (%) | |
| New England | 4 (16.7) |
| Middle Atlantic | 9 (37.5) |
| Midwest | 2 (8.3) |
| South | 8 (33.3) |
| West | 1 (4.2) |
|
| |
| Practice at multiple institutions: yes, n (%) | 9 (37.5) |
|
| |
| Primary expertise, n (%) | |
| Prostate cancer | 12 (50.0) |
| Urological oncology | 8 (33.3) |
| Naturopathic doctor | 1 (4.2) |
| Other | 3 (12.5) |
|
| |
| Proportion of practice managing prostate cancer, n (%) | |
| 0–25% | 5 (20.8) |
| 25–50% | 7 (29.2) |
| 50–75% | 8 (33.3) |
| 75–100% | 4 (16.7) |
|
| |
| Approximate number of surveillance patients, median (range) | 20 (0–700) |
Figure 1.
Main themes elicited from physician interviews to explain decision-making in active surveillance (AS)
Physician Comfort with Active Surveillance
All participants stated that among the biggest advances in AS was the availability of long-term outcomes data, which made them more comfortable recommending AS. All physicians agreed that AS is now a standard management approach and not experimental.
“Because we have a reasonably long follow-up now with the Klotz series, patients going on active surveillance no longer feel like pioneers. They no longer feel like they’re stepping out on a limb. ” [Physician 18]
“I think there’s this general acceptance, as we see more literature coming out from different groups showing that it’s safe.” [Physician 11]
Protocol Selection
Despite agreement that AS is now a standard option, we found wide variability in methods used to monitor patients on AS in the pre-interview questionnaires (Table 2). For patient selection, there was 100% agreement on grade, and nearly all participants also used PSA and clinical stage. There was less agreement on the use of age, imaging and other tests for patient selection or monitoring.
Table 2.
Percent of participants who use each variable or test for selection and/or monitoring during active surveillance (n = 23).
| # (%) Using for selection | # (%) Using for monitoring | |
|---|---|---|
| Age | 13 (56.5) | 11 (47.8) |
| PSA or PSA derivative | 21 (91.3) | 22 (95.7) |
| Clinical stage | 21 (91.3) | 19 (82.6) |
| Grade | 23 (100) | 21 (91.3) |
| Other biopsy features | 19 (82.6) | 15 (65.2) |
| Imaging | 14 (60.9) | 12 (52.2) |
| Other test | 8 (34.8) | 4 (17.4) |
Variation in AS practices was also reflected during interviews. For example, several physicians reported following one published protocol strictly; whereas, other participants felt that since there is no empiric data showing the superiority of any one strategy, follow-up should be tailored to individual patient preferences, physician discretion and experience.
“I use mainly the Johns Hopkins criteria: PSA <10, <3 cores, Gleason 6, ideally a T1c.” [Physician 7]
“If you look at the major series that have been published there are variable approaches to AS. I don’t think any are validated and so I feel my assessment is just as good as any other expert in the field.” [Physician 8]
“If you ask 10 urologists ‘what is your criteria for AS’ I’m curious to see what everyone says but I bet you it’s all over the place.” [Physician 9]
Beliefs about the Utility and Quality of Testing
There were a wide range of responses about the utility and quality of specific tests (Table 3). Some physicians believed a particular test was the “gold standard” while others felt it was “useless.” All physicians stated that they rely heavily on biopsy results and most felt PSA was less important.
“Most of the studies show that PSA is not a reliable trigger for intervention. And so we get it but then we don’t know what to do with it, and it just ends up scaring patients.” [Physician 3]
Table 3.
Variability in physician quotes about the utility and quality of various testing options during active surveillance, ranging from favorable on the left to unfavorable on the right.
|
|
|
|
|
|
|---|---|---|---|---|
| PSA | “I still think PSA is the sort of gold standard that many of us still follow.” | “I mean I usually get PSA, you know, every 6 months or so and I have a couple patients where that has sort of been a trigger for treatment when other things looked okay. More often biopsy changes or patient preference has been a trigger for treatment but I don’t totally dismiss the PSA.” | “The advantages are if it’s stable, it gives the patients some assurance that what they’re doing is correct. The downside is that PSA is not particularly accurate in checking the extent of the disease or grade of disease.” | “So I would say that [PSA tests] that’s mostly to satisfy the patients. I think the value of doing those things is pretty limited.” |
| Marker tests | “Mainly I tend to use Oncotype DX, you know, Genomic Health. I haven’t really done a lot of Prolaris but I am excited about that. They’re hopefully going to be coming out soon for surveillance.” | “Although all the genomic tests are first generation tools I think all the decision analytics have shown that they make us make better decisions than if we don’t use them and therefore we should use them. I like genomics because they’re objective and so you can have instead of relying on a local pathologist who may or may not be an expert in prostate cancer.” | “But you know these genomic tests I’m sure they have value. I actually think they do but they’ve been rolled out so quickly and so broadly that we’re not really able to figure out what that value is.” | “I don’t think they’re that useful and I’ve had a couple of patients who have had them. You know, who have requested them because they just were aware of them and we got it and I didn’t feel like it was helpful.” |
| MRI | “There is not a single patient that I will put on active surveillance unless they’ve had an MRI.” | “Imaging, we use -- obviously, they can’t have evidence of metastatic disease, but we know have started to incorporate MRI’s into our algorithms for following these patients so MRI’s would make a difference.” | “I think in some cases, the MRI could replace the second confirmatory biopsy and select people earlier who might have ended up failing a year or two down the road.” | “The problem with MRI is I don’t think we know enough about it yet. If you look at the data MRI misses about 15% of high grade tumors grade 7 or above. And MRI makes it more likely for you to find a high grade tumor but it doesn’t tell you whether that high grade tumor needs to be treated.” |
| Biopsy | “Probably the biopsy results are the most important. The surveillance biopsy results.” | “I was, kind of having everyone get biopsies every year and really looking at biopsy changes as a major thing. And then in the last couple of years I started to loosen a little bit, you know, how often people get biopsies, particularly when everything is pretty reassuring.” | “Obviously most guys want to stay away from biopsies if they can and if I find that the MRI is negative or it doesn’t show a concerning lesion then I don’t feel bad about, you know, going a little longer before we do a confirmative biopsy, you know, up to about a year even.” | “I like to do as few biopsies as possible…I like to space them out every couple of years, 2, 3, even 4 years.” |
Responses about marker tests varied considerably; most physicians stated that they were still novel and expressed uncertainty if the benefit justified the cost.
“I don't have access to any of those [marker tests], so I don't have any experience in using them." [Physician 23]
“I haven’t really started to use any of the more sophisticated genetic markers yet. I think the jury is still out on some of those like OncotypeDX and Prolaris, etc. I did use PCA3 for a while but I haven’t found it to be tremendously helpful in most cases.” [Physician 3]
Most physicians felt that MRI was useful to reduce the number of biopsies, but that high-quality results were not available in all settings.
“I think MRI has been very helpful in determining who might be a candidate for AS if either prior to the first biopsy in some cases or subsequent to the biopsy to ensure that there is not a large tumor that was missed.” [Physician 3]
“I think MRI is very user-dependent.” [Physician 9]
Years of Experience and Exposure to Active Surveillance During Training
Physicians’ feelings regarding AS varied depending on how long ago they trained. Physicians who completed training recently tended to follow specific protocols more strictly (e.g. Klotz or Johns Hopkins), and several reported being uncomfortable with the lack of national guidelines.
“I feel like I’m all loosey goosey with how I do AS like I should be more like protocolized.” [Physician 5]
Several other physicians who had been employing AS for many years felt comfortable following their own protocol.
“For me I consider myself an expert … I’m aware of what others do, so I don’t practice in a vacuum but I rely on 30 years of basically treating nothing but prostate cancer.” [Physician 8]
Lastly, a few physicians mentioned that AS was not as prioritized as “treatment” during residency, so they did not feel properly trained to care for men on AS. Several participants mentioned emulating former mentors' AS protocols in lieu of formal training.
“We train people to do something, we pay to do something. We are by nature doers and AS is not really part of what a surgeon is wired to do. So that’s another barrier.” [Physician 12]
“I started out doing a lot of what my mentor did when I was in fellowship.” [Physician 13]
Concerns about Inflicting “Harm”
Nearly all participants mentioned the tension between “over-“ or “under-” testing patients and the desire to reduce “harm” whether through repeat biopsies versus the risk of “missing” aggressive disease.
“I think we still don’t understand the impact of repetitive biopsies with inflammation and infection risks. Especially for the ones that we start surveillance young." [Physician 2]
“It’s been placed in your hands to treat their prostate cancer, and it’s possible that you miss the window of curability on your watch. They could be hurt by that choice. That’s a lot of responsibility.” [Physician 1]
Several participants mentioned medico-legal concerns. Some mentioned that AS places liability on the physician, and felt the need to “cover” themselves.
“There’s obviously some degree of liability because you’re at some point fundamentally telling the patient not to seek treatment because of our experience and understanding.” [Physician 1]
Patient Characteristics
Most physicians consider patient characteristics such as age, comorbidities, and history of compliance when deciding who is an appropriate candidate for AS and when it should be discontinued.
“You know, you look at age and comorbidities. I don’t think any of us put guys under 50 on surveillance and some of my colleagues are a little reluctant to put anybody under 60 on surveillance.” [Physician 12]
“I follow people pretty carefully because I also think that them seeing me frequently decreases the likelihood that they're going to be lost to follow-up.” [Physician 23]
Physicians also reported considering patients' financial and insurance status before recommending certain tests.
“I think one of the limitations of using something like the 4KScore is that it’s so expensive and it’s not reimbursed. So there is a lot of patient resistance and I’m not sure what the risk reward is, you know, the cost benefit.” [Physician 8]
“I think a lot of times people think that anything medical is going to be covered especially for their cancer. I mean the potential costs are significant. I saw a guy who is retired on a fixed income who had I can’t remember what stupid test and he had a bill for like over $2000.” [Physician 5]
Finally, some physicians reported a lack of guidance regarding decisions to transition from AS to WW, and that this decision was individualized based on patient characteristics.
“That [switching from AS to WW] depends on the patient because I have to tell you I think there is a little bit of a continuum.” [Physician 7]
Patient Preferences
Several participants mentioned that the “type” of patients choosing AS tend to be more comfortable with “uncertainty” and regular follow-up testing.
“The ones that choose it [AS], it’s a little bit self-selective. The super nervous types don’t tend to choose it." [Physician 1]
Some physicians try to provide “patient-centered care” by considering patients' preferences regarding the type and frequency of testing.
“I’ve started to [use marker tests]. A couple of patients have requested it.” [Physician 4]
“I try to adhere to the principles of shared decision-making when I’m talking to the patients. I try to inform them as much as I can. I try to elicit their preferences.” [Physician 1]
Financial Incentives
Physicians did not believe that financial incentives directly affected their individual practice or their decisions while monitoring men on AS, but many acknowledged that it is a part of the healthcare industry in the USA and may influence a physician’s decision to recommend AS upfront. Some physicians felt that financial incentives were a reason why the uptake of AS in the US has been slower than in other countries.
“Guys in practice make their money doing things. They don’t make nearly as much money doing surveillance and I think that that plays a lot into it. I think there is this attitude that I have heard expressed many times which is, you know, I believe in surveillance, you watch the tumor all the way to the time you wheel the patient in the operating room.” [Physician 12]
“We as an industry, as a large corporation, we have to meet certain benchmarks. And certainly on our side if we don’t do radiation we’re not really doing things, you know, that’s what they pay me to do, to put it mildly. And so I think there is probably a bias in any health system national or otherwise. There is always an incentive.” [Physician 16]
“In Europe where there is no fee for service system the uptake of surveillance is exponentially higher than it is in the US.” [Physician 14]
Discussion
There is significant heterogeneity in the real-world practice of AS, consistent with previous quantitative studies [10, 11, 24]. Using qualitative methods, we explored the reasons for variability in AS and factors influencing the physician decision-making process. Eight key themes emerged: (i) physician comfort with AS; (ii) protocol selection; (iii) beliefs about the utility and quality of testing; (iv) years of experience and exposure to AS during training; (v) concerns about inflicting “harm”; (vi) patient characteristics; (vii) patient preferences; and (viii) financial incentives.
Although physician comfort with AS has increased and it is now considered a standard management option, there are substantial differences in protocol selection. In particular, our results illustrate the conflict between guideline-based vs personalized medicine [25]. While standardized, evidence-based care is generally considered "best practice," it is important to note that there are multiple published protocols for monitoring during AS. For example, the frequency of follow-up biopsy varies between programs and new tests such as MRI are starting to become integrated, but there is a lack of prospective data comparing the long-term outcomes among these differing approaches [26].
Indeed, the question of whether it is appropriate to use the same protocol for vastly different patient populations has not been answered. For example, some factors that emerged in the present study as key themes for decision-making (age and comorbidity) also significantly impact the risk-to-benefit ratio of intense monitoring (biopsy risks, risk-to-benefit of undergoing definitive treatment for localized disease), and therefore heterogeneity based on these factors may be justifiable or even preferred [27, 28]. Furthermore, the risk of disease reclassification is a conditional probability, whereby the risk is reduced with each negative surveillance biopsy [29]. Tailoring AS protocols over time, therefore, based on updated results may be optimal. Although many new tests are available that could be used to tailor AS, such as MRI and genomic tests, the uptake and perceptions of these tests remained variable among participants.
Table 4 summarizes key actionable recommendations and research gaps identified through our study. First is the lack of randomized data comparing different AS protocols or alternative testing strategies. This was previously identified as an important research gap by a 2011 National Institutes of Health (NIH) consensus conference [30], and our findings confirm the ongoing need for additional data to help inform and standardize clinical practice. Notably, an ongoing prospective study in Sweden is comparing two different AS approaches [31]. Furthermore, in the absence of randomized comparison studies, modeling studies would be useful to compare benefits, harms and costs of different protocols.
Table 4.
Recommendations based on themes from qualitative interviews with prostate cancer providers about active surveillance.
| Recommendations | Ways to implement |
|---|---|
| 1. Future research comparing AS protocols | Studies are needed to compare the effectiveness of various AS protocols vs individualized care for patients on AS. More data are needed on the optimum type and frequency of testing during AS, and how this may vary based on patient characteristics |
| 2. Training for residents | AS should be a topic covered during residency. Newly trained urologists should be aware that AS is a viable option for patients with low-risk prostate cancer. Training should include an overview of current protocols and guidelines, how to discuss active surveillance with patients and which testing options are available |
| 3. CME | CME courses can enhance comfort with AS for those with limited exposure during training and can provide evidence updates for those already employing AS. This training should include how to incorporate shared decision-making and follow-up testing options |
AS, active surveillance; CME, continuing medical education.
Another novel finding of our study is the lack of emphasis on AS during urology training, with greater emphasis placed on procedural skills. This is an important and actionable finding, suggesting the need to make AS a core part of urology training and continuing medical education.
A limitation of this study is that physicians who chose to participate may differ from other physicians, which could produce a selection bias. Although our gender distribution was in line with national estimates (∼8% of US urologists are women [32]) and we included providers from a variety of practice settings, our study population was younger (mean age 43 years) than the national average (more than half of practicing urologists aged >53 years) [33]. Although purposive sampling was used to increase diversity across geographic areas and specialties, only US physicians were included and AS practices may differ in other healthcare systems and cultures, and our study did not include any primary care providers. Lastly, although physicians were asked about concerns expressed by their patients, actual patient perspectives were not included in the present analysis and will be the subject of future study. As is the goal of qualitative research, this study was designed to engender deeper knowledge in a specific context, rather than generalizable findings.
In conclusion, physician, patient and healthcare system factors all contribute to the underlying heterogeneity in AS practices in the USA. More data are needed comparing the benefits, harms and costs of alternative protocols to inform a more standardized approach, and greater emphasis is needed on managing patients who are undergoing AS during urology training and continuing education.
Acknowledgments
This study was supported by The Edward Blank and Sharon Cosloy-Blank Family Foundation, the Gertrude and Louis Feil Family, the New York State Department of Health (DOH01-C30697GG-3450000), The Laura and Isaac Perlmutter Cancer Center at NYU Langone Medical Center (P30CA016087), and the NIH (Award Number K07CA178258) to Stacy Loeb. The content is solely the responsibility of the authors and does not represent the official views of the NIH.
Abbreviations
- AS
active surveillance
- WW
watchful waiting
- PSA
prostate specific antigen
- MRI
magnetic resonance imaging
- NCCN
National Comprehensive Cancer Network
Appendix 1. Interview guide
What do you think are the biggest advances in our knowledge of active surveillance?
What are the biggest challenges in our knowledge of active surveillance?
How do you think we can better support patients on active surveillance?
How do you decide which patients are good candidates for active surveillance?
Once your patients have chosen active surveillance, what is your protocol to monitor them?
What are the advantages and disadvantages of PSA measurements during active surveillance?
Do you think any other new markers are useful during active surveillance – which ones and why?
How often do you repeat prostate biopsies during active surveillance?
What kinds of imaging do you use for men on active surveillance?
How do you decide if/when to do biopsies or imaging for patients on active surveillance? How comfortable are you with these standards?
Are you familiar with any guidelines that state how often it’s recommended to give these tests?
What are your triggers to start treatment? What are your triggers to stop active surveillance and convert to watchful waiting?
What information is important for you to make decisions during active surveillance?
What are your main concerns about active surveillance? What are the concerns expressed by your patients about active surveillance?
Is there anything that we have not covered that you would like to add? Do you have any questions for us?
References
- 1.Cooperberg MR, Carroll PR. Trends in Management for Patients With Localized Prostate Cancer, 1990–2013. Jama. 2015 Jul 7;314:80–2. doi: 10.1001/jama.2015.6036. [DOI] [PubMed] [Google Scholar]
- 2.Loeb S, Berglund A, Stattin P. Population Based Study of Use and Determinants of Active Surveillance and Watchful Waiting for Low and Intermediate Risk Prostate Cancer. The Journal of urology. 2013 May 30; doi: 10.1016/j.juro.2013.05.054. [DOI] [PubMed] [Google Scholar]
- 3.Weerakoon M, Papa N, Lawrentschuk N, et al. The current use of active surveillance in an Australian cohort of men: a pattern of care analysis from the Victorian Prostate Cancer Registry. BJU Int. 2015 Apr;115(Suppl 5):50–6. doi: 10.1111/bju.13049. [DOI] [PubMed] [Google Scholar]
- 4.Klotz L, Zhang L, Lam A, Nam R, Mamedov A, Loblaw A. Clinical results of long-term follow-up of a large, active surveillance cohort with localized prostate cancer. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2010 Jan 1;28:126–31. doi: 10.1200/JCO.2009.24.2180. [DOI] [PubMed] [Google Scholar]
- 5.Tosoian JJ, Trock BJ, Landis P, et al. Active surveillance program for prostate cancer: an update of the Johns Hopkins experience. Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2011 Jun 1;29:2185–90. doi: 10.1200/JCO.2010.32.8112. [DOI] [PubMed] [Google Scholar]
- 6.Heidenreich A, Bellmunt J, Bolla M, et al. EAU Guidelines on Prostate Cancer. Part 1: Screening, Diagnosis, and Treatment of Clinically Localised Disease. European urology. 2011 Jan;59:61–71. doi: 10.1016/j.eururo.2010.10.039. [DOI] [PubMed] [Google Scholar]
- 7.Thompson I, Thrasher JB, Aus G, et al. Guideline for the management of clinically localized prostate cancer: 2007 update. The Journal of urology. 2007 Jun;177:2106–31. doi: 10.1016/j.juro.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 8.National Comprehensive Cancer Network Clinical Practice Guidelines in Oncology. [cited; Available from: http://www.nccn.org/professionals/physician_gls/pdf/prostate.pdf.
- 9.Loeb S, Carter HB, Schwartz M, Fagerlin A, Braithwaite RS, Lepor H. Heterogeneity in active surveillance protocols worldwide. Reviews in urology. 2014;16:202–3. [PMC free article] [PubMed] [Google Scholar]
- 10.Gorin MA, Eldefrawy A, Ekwenna O, Soloway MS. Active surveillance for low-risk prostate cancer: knowledge, acceptance and practice among urologists. Prostate cancer and prostatic diseases. 2012 Jun;15:177–81. doi: 10.1038/pcan.2011.57. [DOI] [PubMed] [Google Scholar]
- 11.Philippou Y, Raja H, Gnanapragasam VJ. Active surveillance of prostate cancer: a questionnaire survey of urologists, clinical oncologists and urology nurse specialists across three cancer networks in the United Kingdom. BMC urology. 2015;15:52. doi: 10.1186/s12894-015-0049-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Curry LA, Nembhard IM, Bradley EH. Qualitative and mixed methods provide unique contributions to outcomes research. Circulation. 2009 Mar 17;119:1442–52. doi: 10.1161/CIRCULATIONAHA.107.742775. [DOI] [PubMed] [Google Scholar]
- 13.Patton M. Qualitative evaluation and research methods. Beverly Hills, CA: Sage; 1990. [Google Scholar]
- 14.Palinkas LA, Horwitz SM, Green CA, Wisdom JP, Duan N, Hoagwood K. Purposeful Sampling for Qualitative Data Collection and Analysis in Mixed Method Implementation Research. Adm Policy Ment Health. 2015 Sep;42:533–44. doi: 10.1007/s10488-013-0528-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kreuger RC. MA. Focus Groups: A Practical Guide for Applied Research. 4. Thousand Oaks, California: Sage; 2009. [Google Scholar]
- 16.Marshall M. Sampling for qualitative research. Family Practice. 1996;13:522–5. doi: 10.1093/fampra/13.6.522. [DOI] [PubMed] [Google Scholar]
- 17.Davison BJ, Oliffe JL, Pickles T, Mroz L. Factors influencing men undertaking active surveillance for the management of low-risk prostate cancer. Oncology nursing forum. 2009 Jan;36:89–96. doi: 10.1188/09.ONF.89-96. [DOI] [PubMed] [Google Scholar]
- 18.O'Callaghan C, Dryden T, Hyatt A, et al. ‘What is this active surveillance thing?' Men's and partners' reactions to treatment decision making for prostate cancer when active surveillance is the recommended treatment option. PsychoOncology. 2014 Dec;23:1391–8. doi: 10.1002/pon.3576. [DOI] [PubMed] [Google Scholar]
- 19.Kazer MW, Bailey DE, Jr, Colberg J, Kelly WK, Carroll P. The needs for men undergoing active surveillance (AS) for prostate cancer: results of a focus group study. Journal of clinical nursing. 2011 Feb;20:581–6. doi: 10.1111/j.1365-2702.2010.03489.x. [DOI] [PubMed] [Google Scholar]
- 20.Mishra MV, Bennett M, Vincent A, et al. Identifying barriers to patient acceptance of active surveillance: content analysis of online patient communications. PloS one. 2013;8:e68563. doi: 10.1371/journal.pone.0068563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qualitative health research. 2002 Jul;12:855–66. doi: 10.1177/104973230201200611. [DOI] [PubMed] [Google Scholar]
- 22.NVivo qualitative data analysis software. QSR International Pty Ltd. 2012 Version 10. [Google Scholar]
- 23.Guest GMK, Namey EE. Applied Thematic Analysis SAGE Publications, Inc. 2012 [Google Scholar]
- 24.Hoffman KE, Niu J, Shen Y, et al. Physician variation in management of low-risk prostate cancer: a population-based cohort study. JAMA internal medicine. 2014 Sep;174:1450–9. doi: 10.1001/jamainternmed.2014.3021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Goldberger JJ, Buxton AE. PErsonalized medicine vs guideline-based medicine. Jama. 2013;309:2559–60. doi: 10.1001/jama.2013.6629. [DOI] [PubMed] [Google Scholar]
- 26.Tosoian JJ, Carter HB, Lepor A, Loeb S. Active surveillance for prostate cancer: current evidence and contemporary state of practice. Nat Rev Urol. 2016 Apr;13:205–15. doi: 10.1038/nrurol.2016.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Loeb S, Vellekoop A, Ahmed HU, et al. Systematic review of complications of prostate biopsy. European urology. 2013 Dec;64:876–92. doi: 10.1016/j.eururo.2013.05.049. [DOI] [PubMed] [Google Scholar]
- 28.Bill-Axelson A, Holmberg L, Garmo H, et al. Radical prostatectomy or watchful waiting in early prostate cancer. The New England journal of medicine. 2014 Mar 6;370:932–42. doi: 10.1056/NEJMoa1311593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alam R, Carter HB, Landis P, Epstein JI, Mamawala M. Conditional probability of reclassification in an active surveillance program for prostate cancer. The Journal of urology. 2015 Jun;193:1950–5. doi: 10.1016/j.juro.2014.12.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ganz PA, Barry JM, Burke W, et al. National Institutes of Health State-of-the-Science Conference: role of active surveillance in the management of men with localized prostate cancer. Annals of internal medicine. 2012 Apr 17;156:591–5. doi: 10.7326/0003-4819-156-8-201204170-00401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bratt O, Carlsson S, Holmberg E, et al. The Study of Active Monitoring in Sweden (SAMS): a randomized study comparing two different follow-up schedules for active surveillance of low-risk prostate cancer. Scandinavian journal of urology. 2013 Oct;47:347–55. doi: 10.3109/21681805.2013.813962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Medscape. [cited January 3, 2016];Medscape Physician Compensation Report 2015. 2015 Available from: http://www.medscape.com/features/slideshow/compensation/2015/public/overview#page=14.
- 33.Association AU. AUA Census Highlights State of Urology Workforce. 2015 [cited; Press Release ]. Available from: https://www.auanet.org/advnews/press_releases/article.cfm?articleNo=405.