Abstract
Objective
To identify the proportion and evaluate the content of eConsults (electronic consultations) in which the Champlain BASE (Building Access to Specialists through eConsultation) eConsult process prompted a referral to a specialist that was not originally contemplated by the primary care provider (PCP).
Design
Cross-sectional study of all eConsults submitted between April 15, 2011, and January 31, 2015.
Setting
Champlain Local Health Integration Network, a large health region in eastern Ontario.
Participants
Primary care providers registered to use the Champlain BASE eConsult service.
Main outcome measures
Answers from a close-out survey—completed by PCPs at the conclusion of each eConsult—stating that specialist referral was not originally contemplated but that the eConsult process had prompted referral. The logs containing the communication exchanged between the PCPs and the specialists were reviewed, and each prompted referral case was categorized by the type of question asked, if pharmaceutical advice was given, if the referral was redirected to a different specialty group, and if the referral was urgent.
Results
A total of 188 (3.4%) of 5601 eConsults completed during the study period were cases in which PCPs stated that they had originally not contemplated referring the patient to a specialist but that the Champlain BASE eConsult process had prompted referral. Prompted referrals were most often directed to cardiologists (10.6%), dermatologists (10.6%), infectious disease specialists (9.0%), hematologists (9.0%), and urologists (8.5%). The most common questions were about diagnosis (34.0%), drug treatment (18.0%), and management (15.0%). Pharmaceutical advice was given in 28.0% of prompted referral cases, and in 26.0% of cases, the face-to-face referral was redirected to another specialty group. In 5.0% of cases, the specialist stated the referral was urgent. The median specialist response time was 0.96 days (interquartile range 0.17 to 3.80 days).
Conclusion
By providing PCPs with increased access to specialists, the Champlain BASE eConsult service serves an important role in identifying and preventing the potential detrimental consequences of delayed medical referrals across specialty groups.
Résumé
Objectif
Vérifier le contenu des consultations électroniques (eConsult) et déterminer la proportion de ces consultations où l’utilisation du service eConsult Champlain BASE (Building Access to Specialists through eConsultation) a donné lieu à une demande de consultation à un spécialiste, laquelle n’avait pas été envisagée initialement par le soignant de première ligne (SPL).
Type d’étude
Étude transversale portant sur toutes les demandes effectuées par l’entremise du système eConsult entre le 15 avril 2011 et le 31 janvier 2015.
Contexte
Le réseau local d’intégration des services de santé de Champlain, une grande région sanitaire de l’est de l’Ontario.
Participants
Des soignants de première ligne autorisés à utiliser le service Champlain BASE eConsult.
Principaux paramètres à l’étude
Les réponses à une enquête – complétée par les SPL à la fin de chacune des eConsult – indiquant qu’une demande de consultation n’avait pas été envisagée initialement mais que ce processus avait entraîné une telle demande. On a révisé les registres contenant l’échange de renseignements entre les SPL et les spécialistes, et chaque cas ayant résulté en une demande de consultation a été catégorisé en fonction du type de question demandée, du fait que l’avis donné était d’ordre pharmaceutique, que la demande avait été redirigée vers une autre spécialité et que la demande était urgente.
Résultats
Sur 5601 eConsult effectuées durant l’étude, 188 (3,4 %) étaient des cas pour lesquels le SPL indiquait qu’il n’avait pas envisagé initialement de demander une consultation, mais que l’utilisation de ce service avait entraîné une telle demande. Le plus souvent, ces demandes étaient adressées à des cardiologues (10,6 %), des dermatologues (10,6 %), des infectiologues (9,0 %), des hématologues (9,0 %) et des urologues (8,5 %). Les questions les plus fréquemment posées portaient sur le diagnostic (34,0 %), la médication (18,0 %) et le traitement (15,0 %). Dans 28 % des cas qui avaient entraîné une demande de consultation, un avis d’ordre pharmaceutique avait été donné, et dans 26 % des cas, la demande avait été redirigée vers une autre spécialité. Dans 5 % des cas, le spécialiste avait indiqué que la consultation était urgente. Le temps de réponse médian des spécialistes était de 0.96 jours (écart interquartile: 0,17 à 3,80 jours).
Conclusion
Parce qu’il offre à des SPL un meilleur accès à des spécialistes, le service Champlain BASE eConsult joue un rôle important dans la détection et la prévention des conséquences éventuellement néfastes d’un retard dans la demande d’une consultation en spécialité.
The decision for primary care providers (PCPs) to refer a patient to a specialist depends on many factors.1 Knowledge gaps, tolerance of uncertainty, time pressures, and patient characteristics have all been associated with PCPs’ decisions to refer.1–3 Failure to recognize the need for a referral can have a serious negative effect on patient outcomes. For example, among patients with chronic kidney disease, those who received late referrals to nephrologists exhibited higher mortality rates, had fewer treatment options, and incurred greater costs when compared with patients who were referred early.4–6
New models of accessing specialist care are being introduced. Electronic health platforms such as electronic consultations provide an opportunity to track referral decisions made by PCPs. In 2010, we implemented the Champlain BASE (Building Access to Specialists through eConsultation) eConsult service, a secure, Web-based application that allows PCPs to submit nonurgent, patient-specific questions to specialists.7,8 As of November 2015, more than 10 700 eConsults had been submitted to the Champlain BASE eConsult service, and specialists from 84 different specialty groups are available. The Champlain BASE eConsult service has improved access to specialist advice, reduced the number of face-to-face referrals required, provided educational value to PCPs, and been deemed an acceptable form of care by patients and providers.9–12
The Champlain BASE eConsult service provides rapid access to specialist advice for nonurgent cases. In some of these cases, PCPs have indicated that they were not intending to refer the patient, but as a result of the Champlain BASE eConsult process, a referral was prompted by the specialist who reviewed the patient case. The objectives of this study are 2-fold: to identify the proportion of eConsults that led to the PCP initiating a face-to-face specialist referral when one was not previously contemplated, and to evaluate the content of these eConsults that prompted referrals. The results will increase our understanding of how the Champlain BASE eConsult service might help avoid the negative consequences of delayed medical referrals.
METHODS
Design
We conducted a cross-sectional analysis of all eConsults submitted to the Champlain BASE service between April 15, 2011, and January 31, 2015.
Setting
The Champlain Local Health Integration Network is a large health region in eastern Ontario with a population of 1.2 million people spread out over a catchment area of approximately 16 000 km2. The region has comparable health outcomes and demographic characteristics to the rest of Canada.13
Champlain BASE eConsult service
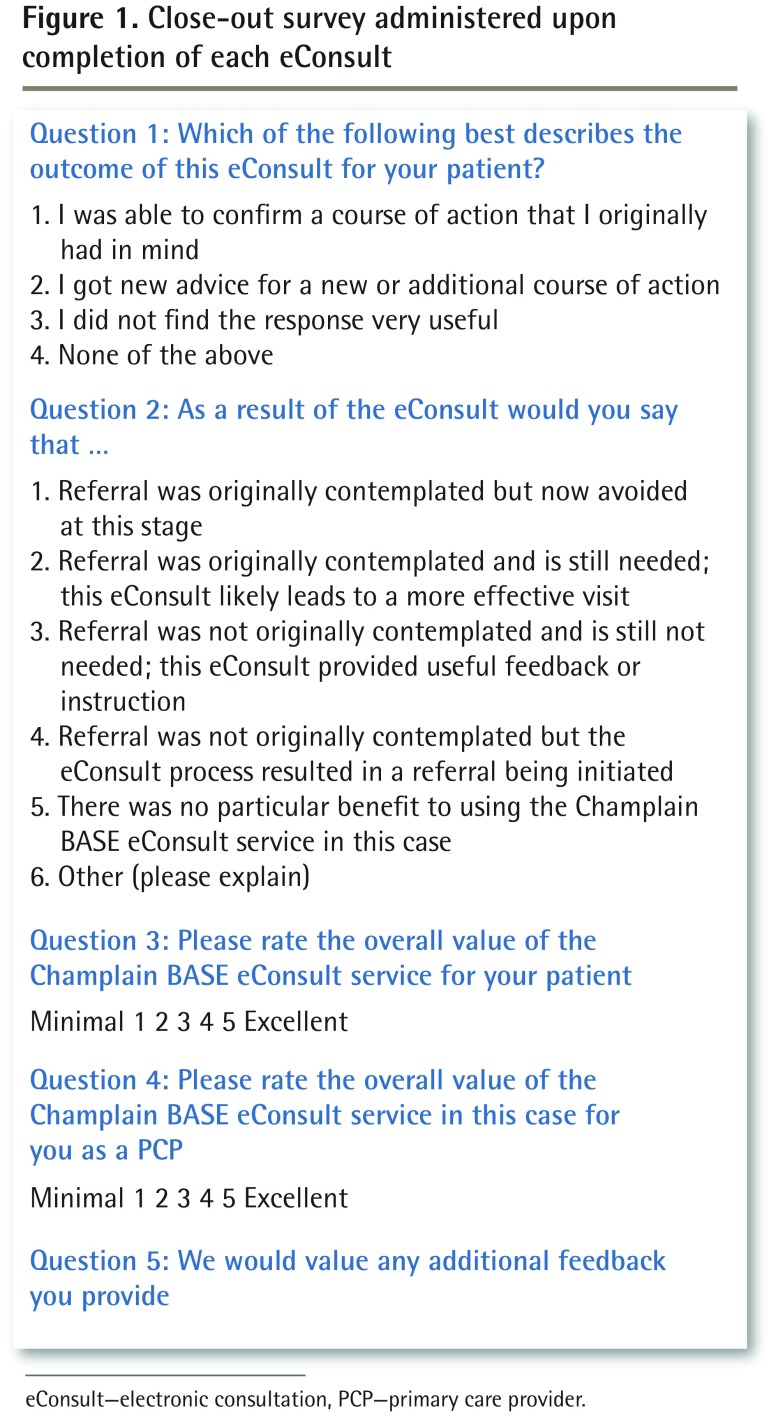
The Champlain BASE service facilitates asynchronous communication between PCPs (ie, family physicians and nurse practitioners) and specialists. To use the service, PCPs submit patient-specific clinical questions to specialty groups, attaching any additional files they deem relevant to the case (eg, images, test results).8,9 The case is then assigned to our on-call specialist within the specialty group who can then log on and review the information provided. Specialists are asked to respond within 7 days and, for each eConsult, are able to do any of the following: provide a recommendation, request more information, or recommend a face-to-face referral. Users are specifically directed to use the Champlain BASE service for only nonurgent cases. The communication between PCPs and specialists is iterative and the discussion can occur back and forth until, ultimately, the PCP closes the case. At the conclusion of each eConsult, PCPs complete a mandatory close-out survey containing 5 questions; the first 4 are a mixture of multiple-choice and Likert-style answers, and the fifth question offers an optional free-text field (Figure 1).
Figure 1.
Close-out survey administered upon completion of each eConsult
eConsult—electronic consultation, PCP—primary care provider.
Data collection
Data collected from PCPs and specialists included provider type, sex, clinic postal code, and specialty type. Data regarding the use of the Champlain BASE service included specialists’ response time, length of time required by the specialist to answer the eConsult question, and PCPs’ responses to the close-out survey. Patient age and sex were also recorded. Primary care provider rurality was defined using the Rurality Index for Ontario in order to assess any differences in prompted referral patterns between PCPs practising in rural compared with urban regions.14 A log containing the complete exchange between PCPs and specialists was also captured.
Analysis
Cases were identified based on the answer from the close-out survey stating that a referral was not originally contemplated but that the eConsult process resulted in a referral being initiated (option 4 in question 2 [Figure 1]). We termed these eConsults prompted referrals for the purpose of this study. Descriptive statistics were used to obtain PCP, patient, and eConsult utilization characteristics for all eConsults submitted during the study period. One author (A.F.) independently reviewed the logs containing the complete exchanges between the PCPs and specialists, and then categorized each case by the type of question asked, if pharmaceutical advice was given, if the referral was redirected to a different specialty group, and if the referral was urgent. The type of question was classified based on a previously developed clinical taxonomy15,16 that was adapted for Champlain BASE.17 Each eConsult was assigned as being 1 of 5 question topics: diagnosis, prognosis, management, self-improvement, or request for direction. In the event the question had elements of more than 1 topic, the case was categorized as “more than 1 type of question.” Pharmaceutical advice was considered to have been given if the specialist provided either medication or vaccine advice. A referral was deemed urgent if the specialist’s response included the terms urgently, emergency, send right away, immediately, or as soon as possible.
Where appropriate,
 2 tests were used to examine any associations between the characteristics of the prompted referral cases and all other eConsults. Statistical analysis was completed using SAS software, version 9.4.
2 tests were used to examine any associations between the characteristics of the prompted referral cases and all other eConsults. Statistical analysis was completed using SAS software, version 9.4.
RESULTS
Of the 5601 eConsults processed between April 15, 2011, and January 31, 2015, 188 (3.4%) resulted in prompted referrals to 26 different specialty groups. Prompted referrals tended to be submitted more often by male PCPs (P = .006) and for male patients (P = .03). Table 1 shows the differences between patient and PCP characteristics among eConsults that prompted referrals compared with all other eConsults.
Table 1.
Characteristics of PCPs and patients for the eConsults submitted between April 15, 2011, and January 31, 2015, that prompted referrals compared with those that did not prompt referrals
| CHARACTERISTICS | eCONSULTS THAT PROMPTED REFERRALS (N = 188), N (%)*† | eCONSULTS THAT DID NOT PROMPT REFERRALS (N = 5413), N (%)*‡ | P VALUE§ |
|---|---|---|---|
| PCPs | |||
| Type of PCP | .39 | ||
| • Family physician | 160 (85.1) | 4722 (87.2) | |
| • Nurse practitioner | 28 (14.9) | 691 (12.8) | |
| Sex | .006 | ||
| • Male | 56 (29.8) | 1160 (21.4) | |
| • Female | 132 (70.2) | 4253 (78.6) | |
| Practice location | .48 | ||
| • Urban | 161 (85.6) | 4731 (87.4) | |
| • Rural | 27 (14.4) | 682 (12.6) | |
| Patients | |||
| Sex | .03 | ||
| • Male | 84 (44.7) | 2007 (37.1) | |
| • Female | 104 (55.3) | 3406 (62.9) | |
| Age, y | .90 | ||
| • 0–17 | 26 (13.8) | 793 (14.6) | |
| • 18–64 | 123 (65.4) | 3454 (63.8) | |
| • ≥ 65 | 39 (20.7) | 1166 (21.5) |
eConsults—electronic consultations, PCP—primary care provider.
Percentages might not add to 100 owing to rounding.
Refers to close-out survey responses to question 2 in which PCPs selected the option-4 answer: Referral was not originally contemplated but the eConsult process resulted in a referral being initiated (Figure 1).
Refers to close-out survey responses to question 2 in which PCPs selected any other answer but option 4 (Figure 1).
 2 test.
2 test.
The eConsults that prompted referrals were directed to cardiologists (10.6%), dermatologists (10.6%), infectious disease specialists (9.0%), hematologists (9.0%), urologists (8.5%), and neurologists (7.5%). Compared with cases that did not prompt referrals, prompted referrals were directed most often to cardiologists, infectious disease specialists, and urologists (P < .001).
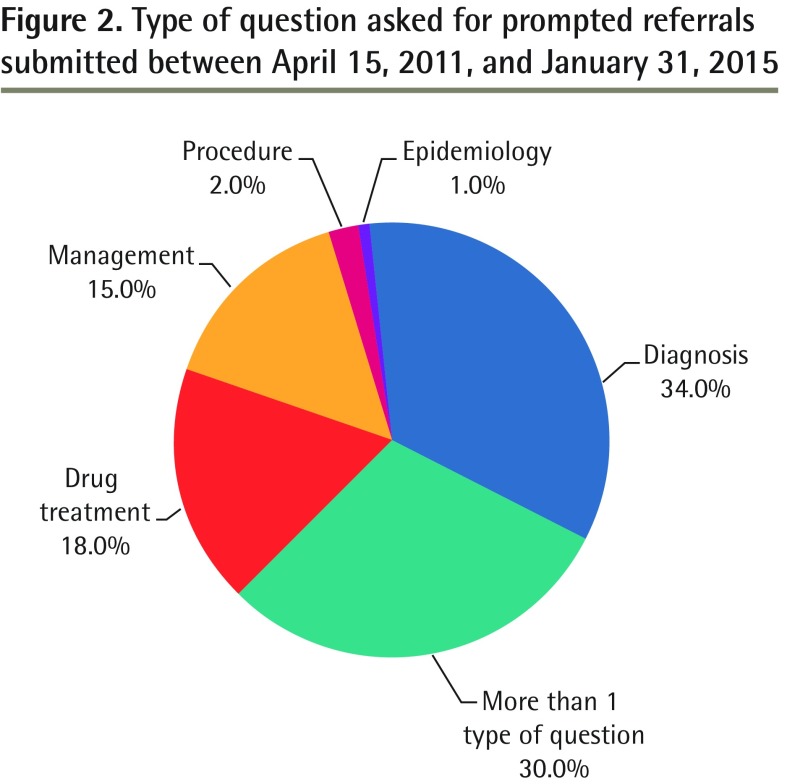
Among the prompted referrals, the most common types of questions were about diagnosis (34.0%), drug treatment (18.0%), and management (15.0%). For 30.0% of cases, there was more than 1 type of question (Figure 2). Pharmaceutical advice was given in 28.0% of prompted referrals; and in 26.0% of cases, the face-to-face referral was redirected to another specialty group.
Figure 2.
Type of question asked for prompted referrals submitted between April 15, 2011, and January 31, 2015
In 5.0% (n = 9) of cases, the referral was deemed urgent. The median initial specialist response time for prompted referrals was 0.96 days (interquartile range 0.17 to 3.80 days). The self-reported time it took specialists to complete the eConsult was less than 10 minutes in 54.3% of cases, 10 to 15 minutes in 22.9%, and 15 to 20 minutes in 16.5% of cases (Table 2). There was a greater proportion of specialists taking more than 15 minutes to respond to prompted referral cases compared with other eConsults (P = .002).
Table 2.
Self-reported time it took non–family physician specialists to complete eConsults submitted between April 15, 2011, and January 31, 2015, that prompted referrals compared with those that did not prompt referrals
| TIME TO COMPLETE eCONSULT | eCONSULTS THAT PROMPTED REFERRALS (N = 188), N (%)* | eCONSULTS THAT DID NOT PROMPT REFERRALS (N = 5413), N (%) | P VALUE† |
|---|---|---|---|
| Time, min | .002 | ||
| • < 10 | 102 (54.3) | 2915 (53.9) | |
| • 10–15 | 43 (22.9) | 1653 (30.5) | |
| • 15–20 | 31 (16.5) | 708 (13.1) | |
| • > 20 | 12 (6.4) | 137 (2.5) |
eConsults—electronic consultations.
Percentages might not add to 100 owing to rounding.
 2 test.
2 test.
DISCUSSION
In this study, we identified 188 cases in which the PCPs had not originally contemplated a referral but initiated one as a result of the advice they received through the eConsult process. Most of these prompted referrals were originally directed to cardiologists and dermatologists, and most of these eConsults consisted of questions related to diagnosis, drug treatment, or management. In 5.0% of these prompted referrals, the specialist expressed a sense of urgency in the timeliness of when a referral should be scheduled.
There is only one other eConsult service to our knowledge that routinely collects similar data. In 2014, Thijssing and colleagues described a telepulmonology service in which GPs digitally consulted pulmonologists to help them interpret spirometry results; the authors reported that in 18% of cases, GPs stated that they had not originally considered a referral but completed one based on the advice they had received.18 The Champlain BASE eConsult service shows a much lower rate of prompted referrals. This might be owing to differences in the types of specialties available, PCPs’ experience, or differing patient populations.
A possible benefit to prompted referrals could be the avoidance of delayed medical referral, as specialists recommended face-to-face consultations for cases in which the PCPs had not originally considered referral. The consequences of a delayed medical referral can be severe.19 In a recent study of patients diagnosed with end-stage renal disease, those who were referred early (defined as meeting with a nephrologist at least 1 year before dialysis) had higher survival rates when compared with those who were referred late.4 Compared with those patients who were referred early, patients who were diagnosed late with rheumatoid arthritis, who were thereby delayed in seeing a rheumatologist, were found to have higher rates of orthopedic surgery.20 Similarly, those with rheumatoid arthritis who were diagnosed late have also been found to have greater joint destruction compared with those who were diagnosed early.21 By providing PCPs with increased access to specialists, the Champlain BASE service serves an important role in identifying and preventing the potential detrimental consequences of delayed medical referrals across specialty groups.
Limitations
This study has some limitations. Although we were able to identify and categorize the eConsults in which a referral was prompted, we were unable to link to other health information and thus cannot determine if patients did indeed visit specialists. The relatively uncommon nature of prompted referrals (3.4% of eConsults) resulted in a fairly small data set, which limits our study’s generalizability.
Future research should examine PCPs who reported a prompted referral to better understand their underlying reasons for what might have caused them to complete a specialist referral when one was not originally contemplated. An exploration of possible PCP and specialist drivers of prompted referrals should also be completed. Finally, an examination of the type of patient questions contained in these referrals and reasons the PCP did not originally contemplate a referral could also be used to inform continuing professional development planning.
Conclusion
This study identified the proportion of eConsults that prompted PCPs to refer patients to specialists—although they had not originally considered doing so—owing to the advice they received through the eConsult process. With the Champlain BASE eConsult service, delayed medical referral is avoided, and patients are provided with access to specialist care they otherwise might not receive.
EDITOR’S KEY POINTS
The Champlain BASE (Building Access to Specialists through eConsultation) eConsult service is a secure, Web-based application that allows primary care providers (PCPs) to submit nonurgent, patient-specific questions to specialists. The advice PCPs receive through the eConsult (electronic consultation) process can help them decide whether specialist referral is needed.
In 3.4% of eConsults completed during the study period, PCPs stated that they had originally not contemplated referring the patient to a specialist but that the eConsult process had prompted referral. The most common questions PCPs had for specialists were about diagnosis, drug treatment, and management.
Delayed medical referrals can have serious adverse consequences for patients. With the Champlain BASE eConsult service, PCPs’ access to specialists is increased and patients are provided with specialist care that they otherwise might not receive.
POINTS DE REPÈRE DU RÉDACTEUR
Le service eConsult Champlain BASE (Building Access to Specialists through eConsultation) est une application sécuritaire du Web qui permet à un soignant de première ligne (SPL) de soumettre à un spécialiste une question non urgente à propos d’un patient. La réponse obtenue grâce à ce système de consultation électronique peut éclairer le SPL qui se demande si une consultation est nécessaire.
Dans 3,4 % des eConsult complétées au cours de la période de l’étude, le SPL disait ne pas avoir envisagé de demander une consultation initialement, mais que la réponse obtenue grâce à ce service l’avait convaincu de le faire. Les questions des SPL les plus fréquentes portaient sur le diagnostic, la médication et le traitement.
Un retard dans une demande de consultation peut avoir des conséquences néfastes pour le patient. Grâce au service eConsult, les SPL ont un meilleur accès aux spécialistes, et les patients bénéficient de soins spécialisés qu’ils auraient pu ne pas recevoir autrement.
Footnotes
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
Contributors
Drs Liddy and Keely conceived of and designed the study, and contributed to the data analysis and drafting of the publication. Mr Drosinis and Mr Fogel contributed to the data analysis and drafting of the manuscript. All authors have read and approved the final submitted version of the manuscript.
Competing interests
None declared
References
- 1.Forrest CB, Nutting PA, von Schrader S, Rohde C, Starfield B. Primary care physician specialty referral decision making: patient, physician, and health care system determinants. Med Decis Making. 2006;26(1):76–85. doi: 10.1177/0272989X05284110. [DOI] [PubMed] [Google Scholar]
- 2.Song Z, Sequist TD, Barnett ML. Patient referrals: a linchpin for increasing the value of care. JAMA. 2014;312(6):597–8. doi: 10.1001/jama.2014.7878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mehrotra A, Forrest CB, Lin CY. Dropping the baton: specialty referrals in the United States. Milbank Q. 2011;89(1):39–68. doi: 10.1111/j.1468-0009.2011.00619.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kim DH, Kim M, Kim H, Kim YL, Kang SW, Yang CW, et al. Early referral to a nephrologist improved patient survival: prospective cohort study for end-stage renal disease in Korea. PLoS One. 2013;8(1):e55323. doi: 10.1371/journal.pone.0055323. Epub 2013 Jan 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee J, Lee JP, Park JI, Hwang JH, Jang HM, Choi JY, et al. Early nephrology referral reduces the economic costs among patients who start renal replacement therapy: a prospective cohort study in Korea. PLoS One. 2014;9(6):e99460. doi: 10.1371/journal.pone.0099460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roderick P, Jones C, Drey N, Blakeley S, Webster P, Goddard J, et al. Late referral for end-stage renal disease: a region-wide survey in the south west of England. Nephrol Dial Transplant. 2002;17(7):1252–9. doi: 10.1093/ndt/17.7.1252. [DOI] [PubMed] [Google Scholar]
- 7.Liddy C, Maranger J, Afkham A, Keely E. Ten steps to establishing an e-consultation service to improve access to specialist care. Telemed J E Health. 2013;19(12):982–90. doi: 10.1089/tmj.2013.0056. Epub 2013 Sep 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liddy C, Rowan MS, Afkham A, Maranger J, Keely E. Building access to specialist care through e-consultation. Open Med. 2013;7(1):e1–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Keely E, Liddy C, Afkham A. Utilization, benefits, and impact of an e-consultation service across diverse specialties and primary care providers. Telemed J E Health. 2013;19(10):733–8. doi: 10.1089/tmj.2013.0007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liddy C, Afkham A, Drosinis P, Joschko J, Keely E. Impact and satisfaction with a new eConsult service: a mixed methods study of primary care providers. J Am Board Fam Med. 2015;28(3):394–403. doi: 10.3122/jabfm.2015.03.140255. [DOI] [PubMed] [Google Scholar]
- 11.Keely E, Drosinis P, Afkham A, Liddy C. Perspectives of Champlain BASE specialist physicians: their motivation, experiences and recommendations for providing eConsultations to primary care providers. Stud Health Technol Inform. 2015;209:38–45. [PubMed] [Google Scholar]
- 12.Keely E, Traczyk L, Liddy C. Patient perspectives on wait times and the referral-consultation process while attending a tertiary diabetes and endocrinology centre: is eConsultation an acceptable option? Can J Diabetes. 2015;39(4):325–9. doi: 10.1016/j.jcjd.2014.12.010. Epub 2015 Mar 19. [DOI] [PubMed] [Google Scholar]
- 13.Bains N, Dall K, Hay C. Population health profile: Champlain LHIN. Toronto, ON: Ministry of Health and Long-Term Care; 2008. [Google Scholar]
- 14.Kralj B. Measuring “rurality” for purposes of health care planning: an empirical measure for Ontario. Toronto, ON: Ontario Medical Association; 2005. [Google Scholar]
- 15.Sackett DL, Richardson WS, Rosenberg W, Haynes RB. Evidence-based medicine: how to practice and teach EBM. New York, NY: Churchill Livingstone; 1997. [Google Scholar]
- 16.Bergus GR, Randall CS, Sinift SD, Rosenthal DM. Does the structure of clinical questions affect the outcome of curbside consultations with specialty colleagues? Arch Fam Med. 2000;9(6):541–7. doi: 10.1001/archfami.9.6.541. [DOI] [PubMed] [Google Scholar]
- 17.Tran C, Liddy C, Pinto N, Keely E. Impact of question content on e-consultation outcomes. Telemed J E Health. 2016;22(3):216–22. doi: 10.1089/tmj.2015.0081. Epub 2015 Aug 17. [DOI] [PubMed] [Google Scholar]
- 18.Thijssing L, van der Heijden JP, Chavannes NH, Melissant CF, Jaspers MW, Witkamp L. Telepulmonology: effect on quality and efficiency of care. Respir Med. 2014;108(2):314–8. doi: 10.1016/j.rmed.2013.10.017. Epub 2013 Oct 31. [DOI] [PubMed] [Google Scholar]
- 19.Levin A. Consequences of late referral on patient outcomes. Nephrol Dial Transplant. 2000;15(Suppl 3):8–13. doi: 10.1093/oxfordjournals.ndt.a027977. [DOI] [PubMed] [Google Scholar]
- 20.Feldman DE, Bernatsky S, Houde M, Beauchamp ME, Abrahamowicz M. Early consultation with a rheumatologist for RA: does it reduce subsequent use of orthopaedic surgery? Rheumatology (Oxford) 2013;52(3):452–9. doi: 10.1093/rheumatology/kes231. Epub 2012 Sep 3. [DOI] [PubMed] [Google Scholar]
- 21.Van der Linden MP, le Cessie S, Raza K, van der Woude D, Knevel R, Huizinga TW, et al. Long-term impact of delay in assessment of patients with early arthritis. Arthritis Rheum. 2010;62(12):3537–46. doi: 10.1002/art.27692. [DOI] [PubMed] [Google Scholar]