Abstract
Background:
Advances in anterior cruciate ligament (ACL) reconstruction procedures in pediatric and adolescent patients have resulted in an increase in recent clinical studies on this topic. However, the consistency with which outcome measures are reported in this demographic is unknown.
Purpose:
To document outcome reporting patterns of youth ACL reconstruction studies in high-impact journals.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
All articles published in 5 high-impact orthopaedic journals from 2010 to 2016 were reviewed to identify those reporting clinical outcomes of young patients who underwent ACL reconstruction. Studies that were nonclinical, reported on patients older than 18 years, or included fewer than 10 patients were excluded. Outcome measures used in all included studies were recorded.
Results:
Seventeen studies encompassing 772 subjects (mean age, 14.3 years; range, 6.3-18.0 years) were analyzed. Eight studies (47%) reported on Tanner stage of subjects, while 1 study reported skeletal age. Ten studies (59%) clearly documented the presence or absence of surgical complications. Range of motion was reported in 65% of studies. Leg-length discrepancy and angular deformity were each reported in 76% of studies, with 12% quantifying results through radiographic measurements. Ligament testing was variably defined by inclusion of instrumented testing (65%), Lachman test (53%), and pivot-shift test (53%). Fourteen studies (82%) explicitly reported on the rate of ACL rerupture, while 71% reported on the rate of revision surgery. Rate of return to preinjury activity was reported in 8 studies (47%), of which 2 defined criteria for return to sport and 3 defined the level of competitive sport. Patient-reported outcome measures (PROMs) were used variably. For the 3 most commonly reported PROMs (Lysholm, International Knee Documentation Committee, and Tegner), 24% of studies reported all 3 PROMs, 35% of studies reported 2 PROMs, and 6% of studies reported 1 PROM in isolation. A pediatric-specific PROM was reported in 1 of the 17 studies.
Conclusion:
Studies on pediatric ACL reconstruction published in high-impact journals unreliably defined subjects’ skeletal maturity, inconsistently reported on objective outcome measures, and used disparate adult-validated PROMs to assess subjective outcomes. These findings highlight the need for standardized, pediatric-specific outcome measures to be applied in future studies evaluating ACL reconstruction in children and adolescents.
Keywords: ACL reconstruction, outcomes, pediatric, adolescents, clinical assessment
Injuries to the anterior cruciate ligament (ACL) are increasingly prevalent among children and adolescents. An estimated 60 million Americans between 6 and 18 years of age participate in organized athletics.23,36 Participation in youth sports promotes physical and psychosocial well-being, reduces the risk of developing chronic medical conditions, and is believed to promote healthy behaviors.2,8,13,47 Increased participation in youth sports has led to a concomitant increase in musculoskeletal injuries in this population.11,37 The initiation of athletics at a younger age, single-sport specialization, and increased year-round play all contribute to an increased incidence of ACL injuries, and improvements in diagnostic modalities have increased the diagnosis of such injuries.3,18
Management of ACL injuries in skeletally immature patients is distinct from that in adults. Some surgical techniques traditionally used for adults are not performed in children and adolescents in order to prevent physeal violation and subsequent growth arrest. Alternative, physeal-respecting ACL reconstruction techniques have been developed to minimize the risk of this complication.19,25 Newer, milestone-based postoperative rehabilitation programs also account for the variable neuromuscular development in young athletes.49 Considerable debate regarding the optimal treatment strategies in this population persists and has resulted in heightened study of clinical outcomes among children and adolescents undergoing ACL reconstruction procedures. Ongoing clinical outcomes research is needed to delineate the indications for and outcomes associated with the treatment options currently in practice.
The extent to which these recent studies have used age-appropriate methods for evaluating clinical outcomes is unknown. This is important because standardized methods for evaluating and reporting surgical outcomes enable meaningful data pooling and the potential to draw powerful conclusions to guide clinical practice. The purpose of this study was to document outcome reporting patterns in high-impact studies of youth ACL reconstruction. In doing so, we aimed to provide a consistent framework for evaluation and/or highlight the need for future studies to employ the most commonly used and age-appropriate metrics, thereby enabling meaningful comparison of youth ACL outcomes studies.
Methods
Five high-impact orthopaedic journals were selected for identification of source articles: The American Journal of Sports Medicine (AJSM), The Journal of Bone and Joint Surgery (American volume) (JBJS), Clinical Orthopaedics and Related Research (CORR), Arthroscopy, and The Journal of Pediatric Orthopaedics (JPO). Prior studies have similarly used these journals to identify high-quality clinical studies in sports medicine.21,32,34 All articles published in each of these journals from January 2010 to May 2016 were reviewed to identify those reporting clinical outcomes of young patients who underwent ACL reconstruction in recent years. Studies that were nonclinical, reported on patients older than 18 years, or entailed fewer than 10 patients were excluded.
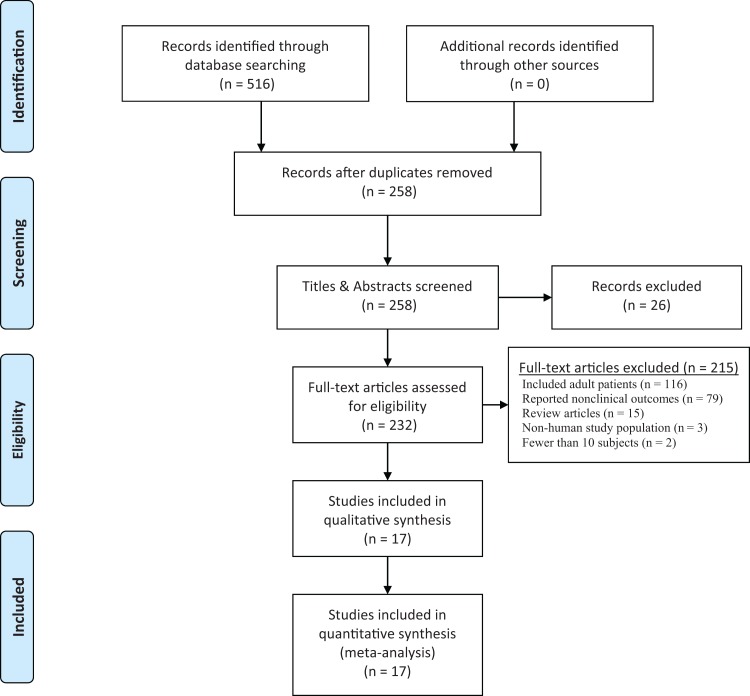
Two computerized databases (PubMed, EMBASE) with a comprehensive index of each of the 5 journals were searched to identify articles. “ACL” or “anterior cruciate ligament” was searched with the phrases [“pediatric” or “adolescent” or “immature”] and [“outcomes” or “complications” or “adverse events”] as well as all relevant iterations. Two researchers independently retrieved articles and reviewed studies to determine eligibility for inclusion. All articles were screened initially by title and abstract to exclude irrelevant studies. Remaining articles underwent full-text review. Discrepancies between reviewers were resolved through consensus with the senior author (P.D.F.). After an initial search yielded 258 unique articles, 17 articles met eligibility criteria (Figure 1).¶
Figure 1.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram for pediatric anterior cruciate ligament clinical outcomes literature.
Characteristics for each study article were recorded, including journal title, authors’ country of origin, publication year, level of evidence, and study type (retrospective vs prospective). All clinical outcomes identified through full-text review of included studies were recorded.
Results
General Characteristics
Seventeen articles that reported on ACL reconstruction in pediatric populations were analyzed (Table 1). Fifteen studies (88%) were retrospective in design and reported level 4 evidence (Table 2). No level 1 or 2 studies were identified. The median number of participants per study was 29, and the mean patient age was 14.3 years (range, 6.3-18.0 years). The study population consisted of 42% females. Mean duration of follow-up was 3.8 years. Five studies (29%) reported patient-level data. Eight studies (47%) reported on Tanner stage of subjects, while 1 study reported the skeletal age of subjects using the Greulich-Pyle method.
Table 1.
Overview of Studies on Youth ACL Injuries
| % (n) | |
|---|---|
| Journal | |
| American Journal of Sports Medicine | 52.9 (9) |
| Arthroscopy | 23.5 (4) |
| Journal of Pediatric Orthopaedics | 11.8 (2) |
| Journal of Bone and Joint Surgery (American volume) | 5.9 (1) |
| Clinical Orthopaedics and Related Research | 5.9 (1) |
| Level of evidence | |
| 1 or 2 | 0 (0) |
| 3 | 12 (2) |
| 4 | 88 (15) |
| Study type | |
| Prospective randomized controlled trial | 0 (0) |
| Prospective, nonrandomized | 12 (2) |
| Retrospective | 88 (15) |
Table 2.
Characteristics of Included Studies (Chronological Order)a
| Study | Year | Journal | Level of Evidence | No. of Patients | Mean Patient Age at Surgery, yb |
|---|---|---|---|---|---|
| Krych et al27 | 2010 | AJSM | 4 | 99 | 16 (13-18) |
| Ellis et al14 | 2012 | Arthroscopy | 3 | 79 | 16 (14-18) |
| Hui et al22 | 2012 | AJSM | 4 | 16 | 12 (8-14) |
| Redler et al41 | 2012 | Arthroscopy | 4 | 18 | 14 (±0.9) |
| Goddard et al20 | 2013 | AJSM | 4 | 31 | 13 (8-16) |
| Kumar et al28 | 2013 | JBJS | 4 | 32 | 11 (9-14) |
| Cassard et al6 | 2014 | JPO | 4 | 28 | 13 (9-15) |
| Demange and Camanho10 | 2014 | AJSM | 4 | 12 | 11 (8-12) |
| Engelman et al15 | 2014 | AJSM | 3 | 73 | 15 (11-18) |
| Schmale et al42 | 2014 | CORR | 4 | 29 | 14 (±1) |
| Calvo et al5 | 2015 | AJSM | 4 | 27 | 13 (12-16) |
| Luo et al31 | 2015 | AJSM | 4 | 124 | 16 (±1.5) |
| Mansson et al33 | 2015 | AJSM | 4 | 29 | 15 (±1.1) |
| Willimon et al48 | 2015 | AJSM | 4 | 21 | 12 (9-14) |
| Domzalski et al12 | 2016 | Arthroscopy | 4 | 22 | 12 (10-13) |
| Larson et al30 | 2016 | Arthroscopy | 4 | 29 | 14 (9-16) |
| Cruz et al9 | 2017 | JPO | 4 | 103 | 12 (±1.8) |
aAJSM, American Journal of Sports Medicine; CORR, Clinical Orthopaedics and Related Research; JBJS, Journal of Bone and Joint Surgery (American volume); JPO, Journal of Pediatric Orthopaedics.
bStandard deviation is reported in parentheses when available. Otherwise, age range is reported.
Objective Outcome Measures
Ten studies (59%) clearly documented the presence or absence of surgical complications. Rate of infection was reported in 29% of studies, rate of nerve injury was reported in 24%, and rate of deep vein thrombosis was reported in 12%.
Twelve studies (71%) reported on postoperative radiographic imaging. Two studies reported radiographic measurements to assess for lower limb deformity, while 1 study obtained postoperative magnetic resonance imaging (MRI) in all subjects. One study reported on MRI imaging for a subset of patients.
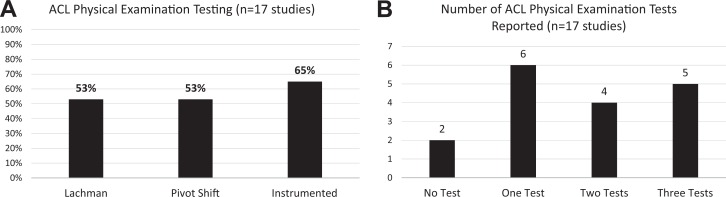
Range of motion was reported in 65% of studies. Leg length discrepancy and angular deformity were each reported in 76% of studies, with 12% providing radiographic measurements. Fifteen studies (88%) documented at least 1 form of laxity testing (Figure 2). Ligament testing was variably defined by inclusion of instrumented testing (65%), Lachman test (53%), and pivot-shift test (53%). Of 11 studies reporting instrumented laxity testing, 73% used KT arthrometer instruments (Medmetric), 18% used Aircast (Rolimeter), and 1 study reported measurements from Genourob (GNRB). All studies reporting KT-instrumented laxity testing used the KT-1000 arthrometer. In 82% of studies reporting instrumented laxity testing, no precise force settings were reported.
Figure 2.
(A) Type of anterior cruciate ligament (ACL) physical examination reported. Anterior drawer test was not reported in any included study. (B) Number of different ACL physical examination tests reported per study.
Four studies (24%) reported hop-testing results for assessment of knee function. Each study reported single-hop testing results, while 1 study additionally reported triple-hop testing results.
Fourteen studies (82%) explicitly reported on the rate of ACL reruptures, while 12 studies (71%) reported on the rate of revision surgery. Three studies (18%) reported the rate of contralateral ACL rupture.
Subjective Outcome Measures
Rate of return to preinjury activity was reported in 8 studies (47%). Of these studies, 2 defined criteria for determining eligible return to sport, and 3 defined the level of competitive sport.
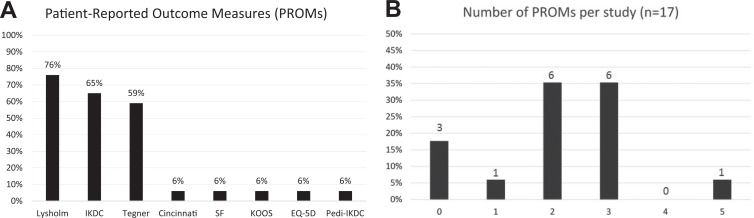
Fifteen (88%) studies reported a total of 8 patient-reported outcome measures (PROMs). The remaining 2 studies reported on general patient satisfaction. Specific PROMs were used variably (Figure 3). Of the 3 most commonly reported PROMs (Lysholm, International Knee Documentation Committee [IKDC], and Tegner), 24% studies reported all 3 PROMs, 35% reported 2 PROMs, and 6% reported 1 PROM in isolation. Although the Tegner score was designed to complement the Lysholm score,4,46 the Lysholm score was used independently in 4 studies (24%). A pediatric-specific PROM, the Pediatric International Knee Documentation Committee (Pedi-IKDC) subjective knee form,26 was reported in 1 of the 17 studies.48
Figure 3.
(A) A variety of patient-reported outcome measures (PROMs) were reported. One study used a PROM that is tailored to a young population. (B) Studies varied in the number of PROMs used. EQ-5D, EuroQol Group-5 Dimensions; IKDC, International Knee Documentation Committee questionnaire; KOOS, Knee injury and Osteoarthritis Outcome Score; Pedi-IKDC, Pediatric IKDC; SF, short form.
Discussion
The findings of the present research demonstrate that the level of evidence of published studies examining treatment of ACL injuries in pediatric and adolescent populations remains low. In a systematic review of all articles published through 2011, Moksnes et al35 identified no randomized controlled trials and a dearth of prospective studies in the youth ACL literature. Our review of data from 2010 to 2016 reveals no measurable improvements in the quality of studies published in the field. Makhni et al32 recently performed a similar study specifically of the adult ACL reconstruction literature. Whereas 50% of the articles identified by Makhni et al were level 1 or 2 studies, all articles identified in the present analysis of youth ACL literature were level 3 or 4 studies.
The low quality and retrospective nature of available studies may contribute to the inconsistencies observed among study parameters and outcome measures. Widespread variability was noted in defining pediatric patients, including different chronologic ages and, in 2 instances, radiographic estimates of skeletal age. Particularly relevant to pediatric patient groups, the presence of limb length discrepancy or angular deformity was widely reported (76%); however, just 12% of studies reported quantitative radiographic measurements to objectively determine these outcomes. The widespread variability noted in clinical outcome measures may in part reflect the retrospective cohort study design most commonly used. Researchers relying on retrospective studies are limited to data that are readily available at their institutions. In clinical settings where surgeons care jointly for adult and pediatric ACL injuries, limited sample sizes among youth ACL injuries may preclude dedicated analysis of this subgroup.
Implementation of PROMs as a means to assess therapeutic interventions has been a transformative development in medical research.7,43 The current study confirms the widespread use of PROMs in the youth ACL literature. However, no consensus is available regarding which measures are to be used uniformly. This issue, which has been identified in the adult ACL reconstruction literature as well,32 precludes efficient translation of outcomes data across studies.
A unique consideration for pediatric-focused research is that many PROMs developed and validated for adult patients may lack specificity for children and adolescents. To our knowledge, for this demographic the IKDC is the only known adult PROM that has been secondarily shown to be translatable to the pediatric version in adolescent athletes.45 In a study by Oak et al,38 the adult and pediatric forms of the IKDC were shown to be significantly different by 1.5 points, although this difference was not clinically significant. The authors concluded that the adult version of the IKDC could be used in adolescents aged 13 to 17 years. Conversely, a study of the IKDC by Iversen et al24 established that children experienced difficulty in comprehending several aspects of the adult form of the IKDC. While an argument may exist in favor of continuing to use the adult form longitudinally in this demographic for investigations that are already underway, it stands to reason that new research in children and adolescents should preferentially use the pediatric version, which was specifically validated for that age group.39 That said, only 1 study from our sample incorporated a pediatric-specific, validated instrument.48 Recently developed pediatric-focused knee and activity PROMs may have a widespread impact if appropriately used for future clinical outcomes assessments in this demographic.16,17,26
This study must be considered in the context of its limitations. Only articles published in the 5 aforementioned peer-reviewed journals were analyzed. Moreover, the study focused on the most recent 6-year period. Together, these inclusion criteria intentionally emphasize studies with the greatest potential to influence future research. However, they do not offer a comprehensive review of the entire youth ACL literature, nor do they offer sufficient historical context to identify trends in outcome measures used. It is also possible that focusing on articles from high-impact journals may not reveal the true variability in reporting of clinical outcome measures, which may be even more widespread than we have identified.
The present study reveals a need for more research on standardized, validated outcome measures tailored to pediatric patients with ACL injuries. Furthermore, ongoing clinical research should be performed prospectively or, at a minimum, should entail the retrospective analysis of prospectively collected registry data, as such research is less subject to selection bias than retrospective case series.40 This recommendation is consistent with large-scale initiatives to promote both multicenter collaborative studies and more widespread use of patient registries.1,44 Establishing procedure-specific patient registries is a best-practice approach to maximizing the informational yield in clinical outcomes assessment. Although patient registries require resources and infrastructure, new technologies are already allowing the effective implementation of such registries.29 These recommendations should guide future directions of clinical outcomes research, and research should be undertaken to identify the most relevant outcome metrics for ACL reconstruction in children and adolescents.
Conclusion
Studies on pediatric ACL reconstruction published in high-impact journals unreliably defined subjects’ skeletal maturity, inconsistently reported on objective outcome measures, and used disparate adult-validated PROMs to assess subjective outcomes. These findings highlight the need for standardized, pediatric-specific outcome measures to be applied in future studies evaluating ACL reconstruction in children and adolescents; further, the development of patient registries and multicenter collaboration should be considered.
Footnotes
One or more of the authors has declared the following potential conflict of interest or source of funding: K.J.J. has received a research grant from the Musculoskeletal Transplant Foundation and education support from Arthrex. D.W.G. is a consultant for Arthrex and Pega Medical.
References
- 1. Andrawis JP, Chenok KE, Bozic KJ. Health policy implications of outcomes measurement in orthopaedics. Clin Orthop Relat Res. 2013;471(11):3475–3481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Booth FW, Roberts CK, Laye MJ. Lack of exercise is a major cause of chronic diseases. Compr Physiol. 2012;2(2):1143–1211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brenner JS; Council on Sports Medicine and Fitness. Sports specialization and intensive training in young athletes. Pediatrics. 2016;138(3). [DOI] [PubMed] [Google Scholar]
- 4. Briggs KK, Lysholm J, Tegner Y, Rodkey WG, Kocher MS, Steadman JR. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37(5):890–897. [DOI] [PubMed] [Google Scholar]
- 5. Calvo R, Figueroa D, Gili F, et al. Transphyseal anterior cruciate ligament reconstruction in patients with open physes: 10-year follow-up study. Am J Sports Med. 2015;43(2):289–294. [DOI] [PubMed] [Google Scholar]
- 6. Cassard X, Cavaignac E, Maubisson L, Bowen M. Anterior cruciate ligament reconstruction in children with a quadrupled semitendinosus graft: preliminary results with minimum 2 years of follow-up. J Pediatr Orthop. 2014;34(1):70–77. [DOI] [PubMed] [Google Scholar]
- 7. Cella D, Gershon R, Lai JS, Choi S. The future of outcomes measurement: item banking, tailored short-forms, and computerized adaptive assessment. Qual Life Res. 2007;16(suppl 1):133–141. [DOI] [PubMed] [Google Scholar]
- 8. Centers for Disease Control and Prevention (CDC). School health guidelines to promote healthy eating and physical activity. MMWR Recomm Rep. 2011;60(RR-5):1–76. [PubMed] [Google Scholar]
- 9. Cruz AI, Jr, Fabricant PD, McGraw M, Rozell JC, Ganley TJ, Wells L. All-epiphyseal ACL reconstruction in children: review of safety and early complications. J Pediatr Orthop. 2017;37(3):204–209. [DOI] [PubMed] [Google Scholar]
- 10. Demange MK, Camanho GL. Nonanatomic anterior cruciate ligament reconstruction with double-stranded semitendinosus grafts in children with open physes: minimum 15-year follow-up. Am J Sports Med. 2014;42(12):2926–2932. [DOI] [PubMed] [Google Scholar]
- 11. Dodwell ER, Lamont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med. 2014;42(3):675–680. [DOI] [PubMed] [Google Scholar]
- 12. Domzalski M, Karauda A, Grzegorzewski A, Lebiedzinski R, Zabierek S, Synder M. Anterior cruciate ligament reconstruction using the transphyseal technique in prepubescent athletes: midterm, prospective evaluation of results. Arthroscopy. 2016;32(6):1141–1146. [DOI] [PubMed] [Google Scholar]
- 13. Eime RM, Young JA, Harvey JT, Charity MJ, Payne WR. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Act. 2013;10:98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ellis HB, Matheny LM, Briggs KK, Pennock AT, Steadman JR. Outcomes and revision rate after bone-patellar tendon-bone allograft versus autograft anterior cruciate ligament reconstruction in patients aged 18 years or younger with closed physes. Arthroscopy. 2012;28(12):1819–1825. [DOI] [PubMed] [Google Scholar]
- 15. Engelman GH, Carry PM, Hitt KG, Polousky JD, Vidal AF. Comparison of allograft versus autograft anterior cruciate ligament reconstruction graft survival in an active adolescent cohort. Am J Sports Med. 2014;42(10):2311–2318. [DOI] [PubMed] [Google Scholar]
- 16. Fabricant PD, Robles A, Downey-Zayas T, et al. Development and validation of a pediatric sports activity rating scale: the Hospital for Special Surgery Pediatric Functional Activity Brief Scale (HSS pedi-FABS). Am J Sports Med. 2013;41(10):2421–2429. [DOI] [PubMed] [Google Scholar]
- 17. Fabricant PD, Robles A, McLaren SH, Marx RG, Widmann RF, Green DW. Hospital for Special Surgery Pediatric Functional Activity Brief Scale predicts physical fitness testing performance. Clin Orthop Relat Res. 2014;472(5):1610–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Frank JS, Gambacorta PL. Anterior cruciate ligament injuries in the skeletally immature athlete: diagnosis and management. J Am Acad Orthop Surg. 2013;21(2):78–87. [DOI] [PubMed] [Google Scholar]
- 19. Gausden EB, Calcei JG, Fabricant PD, Green DW. Surgical options for anterior cruciate ligament reconstruction in the young child. Curr Opin Pediatr. 2015;27(1):82–91. [DOI] [PubMed] [Google Scholar]
- 20. Goddard M, Bowman N, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Endoscopic anterior cruciate ligament reconstruction in children using living donor hamstring tendon allografts. Am J Sports Med. 2013;41(3):567–574. [DOI] [PubMed] [Google Scholar]
- 21. Harvie P, Pollard TC, Chennagiri RJ, Carr AJ. The use of outcome scores in surgery of the shoulder. J Bone Joint Surg Br. 2005;87(2):151–154. [DOI] [PubMed] [Google Scholar]
- 22. Hui C, Roe J, Ferguson D, Waller A, Salmon L, Pinczewski L. Outcome of anatomic transphyseal anterior cruciate ligament reconstruction in Tanner stage 1 and 2 patients with open physes. Am J Sports Med. 2012;40(5):1093–1098. [DOI] [PubMed] [Google Scholar]
- 23. Hulteen RM, Smith JJ, Morgan PJ, et al. Global participation in sport and leisure-time physical activities: a systematic review and meta-analysis. Prev Med. 2016;95:14–25. [DOI] [PubMed] [Google Scholar]
- 24. Iversen MD, Lee B, Connell P, Andersen J, Anderson AF, Kocher MS. Validity and comprehensibility of the International Knee Documentation Committee subjective knee evaluation form in children. Scand J Med Sci Sports. 2010;20(1):e87–e95. [DOI] [PubMed] [Google Scholar]
- 25. Kaeding CC, Flanigan D, Donaldson C. Surgical techniques and outcomes after anterior cruciate ligament reconstruction in preadolescent patients. Arthroscopy. 2010;26(11):1530–1538. [DOI] [PubMed] [Google Scholar]
- 26. Kocher MS, Smith JT, Iversen MD, et al. Reliability, validity, and responsiveness of a modified International Knee Documentation Committee subjective knee form (pedi-IKDC) in children with knee disorders. Am J Sports Med. 2011;39(5):933–939. [DOI] [PubMed] [Google Scholar]
- 27. Krych AJ, Pitts RT, Dajani KA, Stuart MJ, Levy BA, Dahm DL. Surgical repair of meniscal tears with concomitant anterior cruciate ligament reconstruction in patients 18 years and younger. Am J Sports Med. 2010;38(5):976–982. [DOI] [PubMed] [Google Scholar]
- 28. Kumar S, Ahearne D, Hunt DM. Transphyseal anterior cruciate ligament reconstruction in the skeletally immature: follow-up to a minimum of sixteen years of age. J Bone Joint Surg Am. 2013;95(1):e1. [DOI] [PubMed] [Google Scholar]
- 29. Labek G, Janda W, Agreiter M, Schuh R, Bohler N. Organisation, data evaluation, interpretation and effect of arthroplasty register data on the outcome in terms of revision rate in total hip arthroplasty. Int Orthop. 2011;35(2):157–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Larson CM, Heikes CS, Ellingson CI, et al. Allograft and autograft transphyseal anterior cruciate ligament reconstruction in skeletally immature patients: outcomes and complications. Arthroscopy. 2016;32(5):860–867. [DOI] [PubMed] [Google Scholar]
- 31. Luo TD, Ashraf A, Dahm DL, Stuart MJ, McIntosh AL. Femoral nerve block is associated with persistent strength deficits at 6 months after anterior cruciate ligament reconstruction in pediatric and adolescent patients. Am J Sports Med. 2015;43(2):331–336. [DOI] [PubMed] [Google Scholar]
- 32. Makhni EC, Padaki AS, Petridis PD, et al. High variability in outcome reporting patterns in high-impact ACL literature. J Bone Joint Surg Am. 2015;97(18):1529–1542. [DOI] [PubMed] [Google Scholar]
- 33. Mansson O, Sernert N, Rostgard-Christensen L, Kartus J. Long-term clinical and radiographic results after delayed anterior cruciate ligament reconstruction in adolescents. Am J Sports Med. 2015;43(1):138–145. [DOI] [PubMed] [Google Scholar]
- 34. McCormick F, Cvetanovich GL, Kim JM, et al. An assessment of the quality of rotator cuff randomized controlled trials: utilizing the Jadad score and CONSORT criteria. J Shoulder Elbow Surg. 2013;22(9):1180–1185. [DOI] [PubMed] [Google Scholar]
- 35. Moksnes H, Engebretsen L, Risberg MA. The current evidence for treatment of ACL injuries in children is low: a systematic review. J Bone Joint Surg Am. 2012;94(12):1112–1119. [DOI] [PubMed] [Google Scholar]
- 36. National Council of Youth Sports. Report on trends and participation in organized youth sports. www.ncys.org/pdfs/2008/2008-ncys-market-research-report.pdf. Accessed January 24, 2017.
- 37. National Federation of State High School Associations. High school sports participation increases for 20th consecutive year. http://old.nfhs.org/content.aspx?id=3505. Published September 15, 2009. Accessed January 24, 2017.
- 38. Oak SR, O’Rourke C, Strnad G, et al. Statistical comparison of the pediatric versus adult IKDC subjective knee evaluation form in adolescents. Am J Sports Med. 2015;43(9):2216–2221. [DOI] [PubMed] [Google Scholar]
- 39. Phillips L, Carsen S, Vasireddi A, Mulpuri K. Use of patient-reported outcome measures in pediatric orthopaedic literature [published online September 3, 2016]. J Pediatr Orthop. [DOI] [PubMed] [Google Scholar]
- 40. Pugely AJ, Martin CT, Harwood J, Ong KL, Bozic KJ, Callaghan JJ. Database and registry research in orthopaedic surgery, part 2: clinical registry data. J Bone Joint Surg Am. 2015;97(21):1799–1808. [DOI] [PubMed] [Google Scholar]
- 41. Redler LH, Brafman RT, Trentacosta N, Ahmad CS. Anterior cruciate ligament reconstruction in skeletally immature patients with transphyseal tunnels. Arthroscopy. 2012;28(11):1710–1717. [DOI] [PubMed] [Google Scholar]
- 42. Schmale GA, Kweon C, Larson RV, Bompadre V. High satisfaction yet decreased activity 4 years after transphyseal ACL reconstruction. Clin Orthop Relat Res. 2014;472(7):2168–2174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Schmidt CW. NIH roadmap for medical research. Environ Health Perspect. 2004;112(3):A165–A166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Shaha SH, Sayeed Z, Anoushiravani AA, El-Othmani MM, Saleh KJ. Big data, big problems: incorporating mission, values, and culture in provider affiliations. Orthop Clin North Am. 2016;47(4):725–732. [DOI] [PubMed] [Google Scholar]
- 45. Stegmeier N, Oak S, O’Rourke C, et al. No clinically significant difference between adult and pediatric IKDC subjective knee evaluation scores in adults. Sports Health. 2017:1941738116685299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]
- 47. US Department of Health and Human Services, Public Health Service, Office of the Surgeon General. The Surgeon General’s Vision for a Healthy and Fit Nation. Washington, DC: US Department of Health and Human Services; 2010. [PubMed] [Google Scholar]
- 48. Willimon SC, Jones CR, Herzog MM, May KH, Leake MJ, Busch MT. Micheli anterior cruciate ligament reconstruction in skeletally immature youths: a retrospective case series with a mean 3-year follow-up. Am J Sports Med. 2015;43(12):2974–2981. [DOI] [PubMed] [Google Scholar]
- 49. Yellin JL, Fabricant PD, Gornitzky A, et al. Rehabilitation following anterior cruciate ligament tears in children: a systematic review. JBJS Rev. 2016;4(1). [DOI] [PubMed] [Google Scholar]