Abstract
Background and aim:
Cervical cancer (CC) is the 7th most common cancer worldwide. It is the 4th most common cancer in females causing 7.5% of all female cancer deaths. Human Papilloma Virus (HPV) infection is the leading cause of CC and other diseases worldwide. Despite several measures taken to reduce the risk of infection with HPV, the most effective method remains the HPV vaccine. The aim of this study was to assess the knowledge and attitudes of parents in Sharjah towards HPV and whether or not they would vaccinate their daughters.
Methods and Material:
A quantitative, observational cross-sectional study of 400 subjects was conducted in public venues in Sharjah. Probability sampling method was used for selection of subjects (parents who have daughters). A self-administered 32-question questionnaire was distributed. SPSS 21 (Statistical Package for Social Sciences) was used for entry and analysis of data. Frequency was calculated, Chi square test was used to conduct bivariate analysis and bar charts and tables were used to present the results.
Results:
78.3% of the population had heard of CC, 41.3 % of HPV, and 36.5% of the HPV vaccine. Among them, the percentages of the correctly answered knowledge-related questions were found to be 66.2%, 50.9% and 52.1% for CC, HPV and HPV vaccine, respectively. 76.6% of parents were willing to vaccinate their daughters. The percentage increased to 92.9%, if the ministry of health (MOH) recommended the vaccine. A significant correlation was found between the spouse’s level of education, HPV (Pearson-chi square value: 5.049 and p: 0.025) and HPV vaccine (Pearson-chi square value: 4.057 and p:0.044).
Conclusions:
Despite the public’s lack of knowledge, the study showed a noticeable increase in parent’s willingness to vaccinate their daughters if the government recommends and provides the HPV vaccine. However, proper evaluation of the vaccine’s efficacy from a socioeconomic point of view is needed before recommending its implementation in the UAE immunization schedule.
Keywords: Human Papilloma Virus (HPV), cervical cancer, vaccine, knowledge, awareness
Introduction
Introduction of vaccines was a point of transition in medicine. They are one of the most effective public health interventions protecting against infectious diseases. Many infections have been found to be linked to certain types of cancer. Approximately 18% of cancer cases worldwide are attributed to infectious agents; particularly viruses (Perlman et al., 2014). In 2012, CC was the 7th most common cancer worldwide. It was the 4th most common cancer in females resulting in 7.5% of all female cancer deaths. It is also one of the leading causes of premature deaths in women at reproductive age. The majority of deaths (87%) occur in less developed regions (Globocan Cervical Cancer Fact Sheet, 2012). According to the “Human Papillomavirus and Related Diseases Report”, every year an estimated 93 new cervical cancer cases are diagnosed and approximately 28 cervical cancer deaths occur in the UAE (estimations for 2012). Cervical cancer ranks as the 3rd highest cause of female cancers and the 7th cause of female cancer deaths in the UAE (Human Papillomavirus and Related Diseases Report UAE Version, 2015).
HPV infection can be present without any detected abnormal cervical changes. This occurs in 11-12% of women worldwide with the highest rates in Sub Saharan Africa and Eastern Europe. There are many serotypes of HPV. The most common types causing infections are HPV 16 and 18 (Forman et al., 2012). According to the CDC, CC is highly preventable because of available screening tests (Pap smear) and the availability of a vaccine to protect against the HPV infection. When CC is detected early, it can have a good prognosis (HPV: Questions and Answers, 2015). HPV infection is the most leading cause of CC and other diseases worldwide. Despite several measures taken to reduce the risk of infection with HPV, the most effective method of prevention for women under 26 is the HPV vaccine, while for those above 26, Pap smear (screening) remains the best choice. This can be explained by the ability of the HPV vaccine to protect women below 26 before they get the HPV infection. For those above 26, the risk of being already infected with HPV is high, and thus benefits of the vaccine are restricted to the minority of women who have not been infected yet (HPV Vaccine Information for Young Women, 2015). The CDC suggests that HPV vaccination should be given for all males and females aged 11 or 12. There are two types of HPV vaccines: the quadrivalent vaccine (HPV 4-Gardasil) which protects against types 6, 11, 16, 18, and the bivalent vaccine (HPV 2-Cervarix) which protects against types 16 and 18 only. The HPV vaccine is given intramuscularly. It consists of three dose series of either type of vaccine given over six months, with a 2 months interval between the doses (Immunization Guidelines, Dubai).
In 2008, Abu Dhabi became the first city in the Middle East to start giving free HPV vaccinations for all grade 11 school girls, both Emiratis and expatriates (Ortashi et al., 2013). This resulted in a dramatic increase in uptake of the vaccine from less than 60% to more than 95% in 2013 (Ortashi et al., 2013). Since the UAE lacks a national cervical screening program, the Health Authority of Abu Dhabi (HAAD) started Abu Dhabi’s Cervical Screening Program in 2013, the most comprehensive and the first of its kind in the region (Ortashi et al., 2013). The Ministry of Health (MOH) is yet to impose the HPV vaccine as a compulsory vaccine in the UAE’s immunization program.
Many researches have been recently conducted on the HPV vaccine. There are many aspects about this vaccine that remain unknown. For example, the long-term safety and long lasting immunity provided by the vaccine was studied in researches only up to 10 years post vaccination, but what happens after the 10 years remains unknown. (Vincenzo, 2014). The cost effectiveness of the HPV vaccine implementation is still questionable in many countries as this depends on many factors such as the incidence of the disease in the country, which varies between different areas. The willingness of the public to take the vaccine and their knowledge about it and its’ importance is also not known in many countries.
This study was conducted to assess the knowledge and attitudes of parents in Sharjah towards HPV and whether they would vaccinate their daughters or not, and if this will have an impact on the MOH’s decision to make the vaccine compulsory as part of their vaccination schedule.
Materials and Methods
A quantitative, observational, cross-sectional study of 400 randomly selected subjects (parents of any age, any nationality and who have daughters of any age) was conducted in the city of Sharjah in the UAE over a two months period, from February to April 2015. Parents living in Sharjah and available in public places at the time of data collection were eligible to participate in the study while those working in the medical field and those who do not speak English or Arabic were excluded. The sample was calculated based on 5% marginal error and 50% prevalence. A probability sampling method was used in the recruitment of participants.
This study was approved by the Research Ethics Committee, of the Medical Colleges, at the University of Sharjah. Participants’ consents were obtained. A self-directed questionnaire was developed initially and later a pilot study was conducted to check the reliability. The questionnaire was then modified after feedback from the pilot study. Face validity was checked by subject matter experts. Other references were reviewed to assess content validity. The questionnaire had 32 questions and was divided into 5 sections: 1) Demographics, including: age, nationality, level of education and spouse’s level of education. 2) Cervical cancer knowledge, where we asked questions about who gets CC, what is its cause and whether CC is preventable or not. 3) HPV knowledge by asking questions about HPV, how common it is, consequences of getting infected with it, routes of transmission and cure. 4) HPV vaccine knowledge by asking about the starting age of getting the vaccine, how it is given and what are its side effects. 5) People’s attitude towards the vaccine by asking about the willingness of mothers to get themselves vaccinated and whether they are willing to vaccinate their daughters if the MOH recommends the vaccine. Questions varied between multiple-choice questions, closed and open-ended questions, as well as Likert scale questions. Participants’ responses were entered and analyzed using SPSS 21 (Statistical Package for Social Sciences). Frequency was calculated for each variable. Chi square test was used to conduct bivariate analysis. Bar charts and tables were used to present the results.
Results
The demographic data of the sample is shown in Table 1. There were 296 Arab participants (non-UAE nationals). They were the majority forming 77% of the sample. Only 38 (9.5%) were UAE citizens while the 66 non-Arab participants formed 16.5% of the sample. As shown, the mean age was 40.56 years old with a standard deviation of 10.35. 308 (77%) of the participants and 310 (78.5%) of the spouses had a university degree.
Table 1.
Demographic Characteristics of Study Participants
| Demographics | UAE | Arabs (Non- UAE nationals) | Non –Arabs | Total | ||||
|---|---|---|---|---|---|---|---|---|
| Age | N | % | N | % | N | % | N | % |
| <36 | 11 | 28.9 | 104 | 53.1 | 29 | 43.9 | 144 | 36.0 |
| 36-50 | 18 | 47.4 | 137 | 46.3 | 31 | 47.0 | 186 | 46.5 |
| >50 | 9 | 23.7 | 55 | 18.6 | 6 | 9.1 | 70 | 17.5 |
| Mean + SD | 42.71 +/- 9.2 | 40.95 +/- 10.6 | 37.54 +/- 9.5 | 40.56 +/- 10.3 | ||||
| Education | N | % | N | % | N | % | N | % |
| Below university | 10 | 26.0 | 73 | 42.7 | 9 | 13.6 | 92 | 23.0 |
| University | 28 | 73.7 | 223 | 75.3 | 57 | 86.4 | 308 | 77.0 |
| Spouse education | N | % | N | % | N | % | N | % |
| Below university | 16 | 42.1 | 60 | 20.3 | 9 | 14.8 | 85 | 21.5 |
| University | 22 | 57.9 | 236 | 79.7 | 52 | 85.2 | 310 | 78.5 |
Figure 1 represents participants who heard about CC, HPV and the HPV vaccine. Out of those who had heard of the three topics, only 66.2%, 50.9% and 52.1% were considered to be knowledgeable at the end of the study. Those who did not hear of the disease or the vaccine were asked to skip the knowledge questions. Thus, the total knowledge of the sample was only 24%, 21.3% and 19% for CC, HPV and the HPV vaccine respectively.
Figure 1.
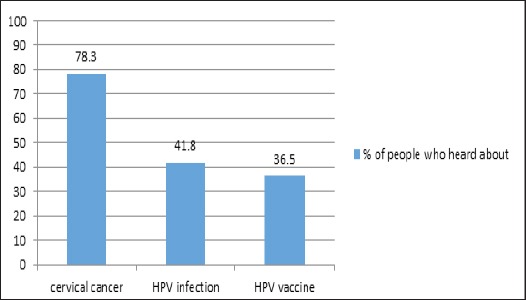
Percentage of People Who Heard about CC, HPV and HPV Vaccine
Table 2 shows participants’ sources of knowledge. The television is the main source of information for CC and HPV vaccine, while schools, universities and work were the providers of knowledge on HPV infection.
Table 2.
Sources of Obtaining Knowledge among the Participants
| UAE | Arab (Non UAE nationals) | Non- Arab | Total | |||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | % | ||
| Knowledge of CC | TV | 13 | 34.2 | 135 | 53.6 | 32 | 54.2 | 51.6 |
| News | 10 | 26.3 | 78 | 31.0 | 28 | 47.5 | 33.2 | |
| Radio | 1 | 2.6 | 26 | 10.3 | 15 | 25.4 | 12.0 | |
| Internet | 8 | 21.1 | 75 | 29.8 | 28 | 47.5 | 31.8 | |
| School\university\ work | 7 | 18.4 | 66 | 26.2 | 25 | 42.4 | 28.1 | |
| Someone | 6 | 15.8 | 53 | 21.0 | 12 | 20.3 | 20.3 | |
| Others | 12 | 31.6 | 26 | 10.3 | 10 | 16.9 | 30.8 | |
| Knowledge of HPV | TV | 3 | 15.8 | 41 | 36.6 | 13 | 40.6 | 35.0 |
| News | 3 | 15.8 | 27 | 24.1 | 7 | 21.9 | 22.7 | |
| Radio | 0 | 0.0 | 8 | 7.1 | 3 | 9.4 | 6.7 | |
| Internet | 4 | 21.1 | 34 | 30.4 | 12 | 37.5 | 30.7 | |
| School\university\ work | 11 | 57.9 | 33 | 29.5 | 14 | 43.8 | 35.6 | |
| Someone | 3 | 15.8 | 17 | 15.2 | 8 | 25.0 | 17.2 | |
| Others | 1 | 5.3 | 6 | 5.4 | 3 | 9.4 | 6.1 | |
| Knowledge of HPV vaccine | TV | 3 | 25.0 | 38 | 35.8 | 9 | 33.3 | 34.5 |
| News | 3 | 25.0 | 20 | 18.9 | 11 | 40.7 | 23.4 | |
| Radio | 1 | 8.3 | 3 | 2.8 | 4 | 14.8 | 5.5 | |
| Internet | 2 | 16.7 | 25 | 23.6 | 11 | 40.7 | 26.2 | |
| School\university\ work | 2 | 16.7 | 27 | 25.5 | 12 | 44.4 | 28.3 | |
| Someone | 4 | 33.3 | 18 | 17.0 | 5 | 18.5 | 18.6 | |
| Others | 3 | 25.0 | 15 | 14.2 | 4 | 15.8 | 15.3 | |
Figure 2 demonstrates knowledge about CC and HPV that was measured by asking questions on each topic. It can be observed that knowledge about CC, HPV and the link between the two is poor. 41.8% of population knew that CC can be preventable but only 14.5% of the sample knew that HPV is the leading cause of CC.
Figure 2.
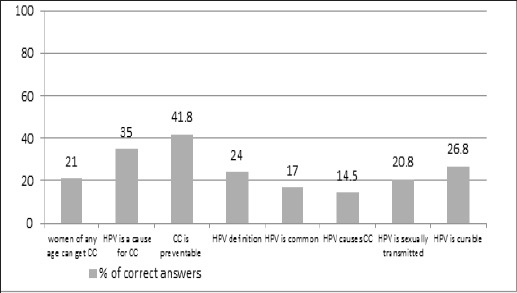
Knowledge about CC and HPV
72.5% of the participating mothers agreed they would take the vaccine. Those who refused to be vaccinated justified their choice by claiming they were too old (43.2%) or had doubts about the vaccine’s safety (23.4%), in terms of potential side effects or long term complications.
76.6% of participants are willing to give their daughters HPV vaccine. The main reasons for refusal were the side effects of the vaccine (45.3%) and the lack of knowledge about it (40%). The increase in willingness to vaccinate the daughters if the MOH had recommended the vaccine can be noticed in Figure 4.
Figure 3.
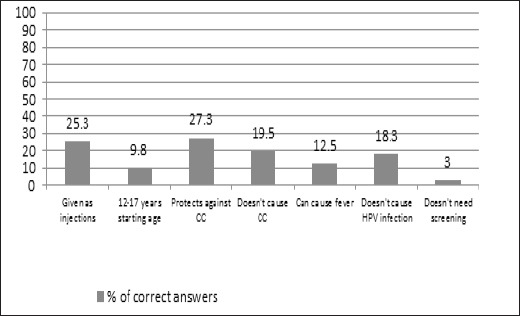
Knowledge about HPV Vaccine
Figure 4.
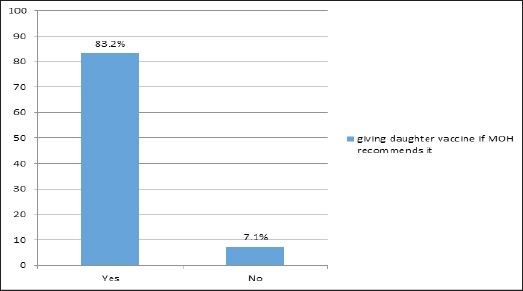
Giving Daughter Vaccine if MOH Recommends it
A significant correlation was found between the spouse’s education and knowledge about HPV (X2: 5.049 and p: 0.025) and its vaccine (X2: 4.057 and p:0.044). Other correlations are shown in Table 3.
Table 3.
Correlations
| Correlation | Pearson chi square value | P value |
|---|---|---|
| Age and knowledge about CC | 0.141 | 0.932 |
| Nationality and knowledge about CC | 4.443 | 0.108 |
| Education and knowledge about CC | 0.129 | 0.719 |
| Spouse education and knowledge about CC | 1.208 | 0.272 |
| Age and knowledge about HPV | 4.268 | 0.118 |
| Nationality and knowledge about HPV | 2.073 | 0.355 |
| Education and knowledge about HPV | 0.219 | 0.64 |
| Spouse education and knowledge about HPV | 5.049 | 0.025 |
| Age and HPV vaccine | 0.904 | 0.636 |
| Nationality and HPV vaccine | 3.005 | 0.223 |
| Education and HPV vaccine | 0.755 | 0.385 |
| Spouse education and HPV vaccine | 4.057 | 0.044 |
| Age and willingness to get the vaccine | 2.611 | 0.271 |
| Nationality and willingness to get the vaccine | 7.088 | 0.029 |
| Education and willingness to get the vaccine | 1.075 | 0.3 |
| Spouse education and willingness to get the vaccine | 0.06 | 0.807 |
| Age and willingness to vaccinate the daughter | 0.911 | 0.634 |
| Nationality and willingness to vaccinate the daughter | 7.867 | 0.02 |
| Education and willingness to vaccinate the daughter | 0.84 | 0.359 |
| Spouse education and willingness to vaccinate the daughter | 0.562 | 0.453 |
Discussion
This study assessed the knowledge and attitudes of parents in Sharjah towards CC, HPV and its vaccine. The study showed the increase in the willingness of parents to vaccinate their daughters if the MOH recommends the HPV vaccine.
A large percentage of the Sharjah population had heard of CC, but less than 50% had heard of HPV and its vaccine. Among them, the percentages of the correctly answered knowledge-related questions were found to be on the low side. These results are concordant with a cross sectional study conducted in 2013 in China where knowledge about HPV and it’s vaccine was found to be poor among women with teenage daughters (Yu et al., 2016).
Our findings also suggest that the public consider the media (TV, internet, advertisements) to be their greatest source of information. This is useful as it can help guide the government to target its efforts in promoting awareness on social media rather than public campaigns.
A good percentage of mothers were willing to take the vaccine but 27.5% refused the vaccine and one of the main reasons was the vaccine’s safety. Similarly, a cross sectional study in Mali conducted in 2013 found that 76.6% of the mothers were willing to give the vaccine to their daughters but not themselves. The main reasons for this refusal in that study were the side effects of the vaccine and lack of knowledge (Poole et al., 2013). The safety of the vaccine has been well-documented by the CDC (Slade et al., 2009) consequently, it is only a matter of raising awareness.
The government needs to constantly engage and educate the public. Community-based interventions are vital and must be implemented so as to address concerns about vaccine safety and curb misconceptions the public may have acquired online or from the media. Health care providers also play a vital role in providing scientifically sound information, as people will seek their medical advice (Perlman et al., 2014).
The significant correlation found, between the male spouse’s education and knowledge about HPV and its vaccine, suggests that husbands can influence their wife / daughter’s decision on whether or not to take the vaccine. Better immunization outcomes may be expected if emerging immunization programs targeted men as well as women. This is similar to the findings of a recent cross sectional study conducted in the Emirate of Abu-Dhabi (Ortashi et al., 2013).
The increase in the public’s willingness to take the vaccine if the MOH recommends it is due to the fact that the majority of people in the UAE community accept their health care provider’s advice. Contrary to other countries, where the public may question advice from healthcare professionals, most people in the UAE consider such recommendations to be for their sake and therefore comply with instructions or suggestions given to them by their healthcare provider (Ortashi et al., 2013). This is an important finding of the study, and demonstrates the need for MOH approval of the HPV vaccine as part of the UAE vaccination schedule.
There may be concerns regarding the cost-effectiveness of implementing the HPV vaccine in the UAE immunization schedule. This is mainly because the prevalence of HPV infections is generally low in Islamic countries. However, the latest data published in the “UAE: Human Papilloma Virus & Related Diseases” report shows that the UAE ranks 3rd in terms of CC incidence and 4th in CC mortality across Western Asia. (Human Papillomavirus and Related Diseases Report UAE Version, 2015) Thus, despite the variability in the cost-effectiveness criteria across different countries, a preliminary evaluation is needed to determine whether implementing a national vaccination program would sensibly decrease the incidence of CC at the population level. Moreover, there may be added individual benefits that screening and vaccination can provide, especially to those who are more at-risk due to their lifestyle, behaviors and practices (Alsbeih, 2014).
The low number of UAE nationals in our sample size was not surprising given the demographic constitution of the society where more than half of the population is expatriate (Ortashi et al., 2013).
Having male collaborators collecting data proved problematic when approaching parents, especially mothers, since the topic is a relatively sensitive one. This is due to the UAE community being quite conservative.
The limitation in the study was the convenient sampling method used. This decreased the ability to generalize the results. However, this could not have been avoided due to the fact that the UAE community is a conservative one and thus home visits for the purpose of research would not have been welcomed. The study was also conducted in an economically well-developed city in the UAE and was not a multi-center study. Thus, our results cannot be generalized to underdeveloped areas in the region with similar statistical data. There might also be a response bias in the study as parents filled the questionnaires themselves, and thus may have answered with sociably desirable responses (Yu et al., 2016).
The link between gender or medical history verses knowledge, awareness and willingness to vaccinate would also be interesting to consider investigating in the future. It would also be interesting to explore the levels of knowledge and willingness to vaccinate daughters in low-income un-insured people.
In conclusion, this study showed that the knowledge of CC, HPV and HPV vaccine among the general public in Sharjah was lacking. Furthermore, the study showed a noticeable increase in parent’s willingness to vaccinate their daughters if the government recommends the HPV vaccine. Current practice guidelines advocate giving the HPV vaccine to minors, thus, parents’ involvement is important, as they are the primary decision makers in such cases. However, the vaccines efficacy from a socioeconomic point of view is yet to be evaluated before recommending its implementation in the UAE immunization schedule.
Conflict of interest
None.
References
- Alsbeih G. HPV infection in cervical and other cancers in Saudi Arabia:Implication for prevention and vaccination. Front Oncol. 2014;4:1–6. doi: 10.3389/fonc.2014.00065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- cForman D, De Martel C, Lacey C, et al. Global burden of human papillomavirus and related diseases. Vaccine. 2012;30:12–23. doi: 10.1016/j.vaccine.2012.07.055. [DOI] [PubMed] [Google Scholar]
- GLOBOCAN. Cervical cancer fact sheet:Cervical cancer estimated incidence, Mortality and prevalence worldwide in 2012. France: International agency for research on cancer; 2012. Available from: http://globocan.iarc.fr/old/FactSheets/cancers/cervix-new.asp . [Google Scholar]
- HPV. Questions and answers. USA: CDC; 2015. Available from: http://www.cdc.gov/hpv/parents/questions-answers.html . [Google Scholar]
- HPV. Vaccine information for young women. USA: CDC; 2015. Available from: http://www.cdc.gov/std/hpv/stdfact-hpv-vaccine-young-women.htm . [Google Scholar]
- Human papillomavirus and related diseases report UAE Version. Spain: HPV centre; 2015. Available from: http://www.hpvcentre.net/statistics/reports/ARE.pdf . [Google Scholar]
- Immunization guidelines. Dubai: Dubai health authority, Public health & safety department, health policy & strategy sector. Report No. HPSS/PHSDM001; 2012. [Google Scholar]
- Ortashi O, Raheel H, Khamis J. Acceptability of human papillomavirus vaccination among male university students in the United Arab Emirates. Vaccine. 2013;31:5141–4. doi: 10.1016/j.vaccine.2013.08.016. [DOI] [PubMed] [Google Scholar]
- Ortashi O, Raheel H, Shalal M, Osman N. Awareness and knowledge about human papillomavirus infection and vaccination among women in UAE. Asian Pac J Cancer Prev. 2013;14:6077–80. doi: 10.7314/apjcp.2013.14.10.6077. [DOI] [PubMed] [Google Scholar]
- Perlman S, Wamai R, Bain P, et al. Knowledge and awareness of HPV vaccine and acceptability to vaccinate in sub-Saharan Africa:A systematic review. PLoS One. 2014;9:1–14. doi: 10.1371/journal.pone.0090912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poole D, Tracy J, Levitz L, et al. A cross-sectional study to assess HPV knowledge and HPV vaccine acceptability in Mali. PLoS One. 2013;8:1–7. doi: 10.1371/journal.pone.0056402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade B, Leidel L, Vellozzi C, et al. Postlicensure safety surveillance for quadrivalent human papillomavirus recombinant vaccine. JAMA. 2009;302:750–7. doi: 10.1001/jama.2009.1201. [DOI] [PubMed] [Google Scholar]
- Vincenzo R, Conte C, Ricci C, et al. Long-term effecacy and safety of human papillomavirus vaccination. Int J Womens Health. 2014;6:999–1010. doi: 10.2147/IJWH.S50365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu Y, Xu M, Sun J, et al. Human papillomavirus infection and vaccination:Awareness and knowledge of HPV and acceptability of HPV vaccine among mothers of teenage daughters in Weihai, Shandong, China. PLoS One. 2016;11:1–14. doi: 10.1371/journal.pone.0146741. [DOI] [PMC free article] [PubMed] [Google Scholar]


