Abstract
The present study examined how interparental violence, neighborhood violence, behavioral regulation during parental conflict, and age predicted beliefs about the acceptability of aggression and the acceptance of retaliation against an aggressive peer among youths. Participants were 110 families (mothers, fathers, and children) in which one or both parents met criteria for substance use disorder. Results of a bootstrapped path model revealed higher exposure to neighborhood violence predicted greater acceptability of general aggression, whereas higher father-to-mother violence perpetration predicted lower acceptability of general aggression. Higher exposure to neighborhood violence, behavioral dysregulation during parental conflict, and older child age predicted greater approval of retaliation toward an aggressive peer. Findings are interpreted as related to the cognitive-contextual framework.
Keywords: Acceptability of aggression, children of substance-abusing parents, intimate partner violence, neighborhood violence
Introduction
Children of substance-abusers (COSAs), or youth who reside in the homes of parents who suffer from abuse or dependence for alcohol or drugs, are at considerable risk for exhibiting high levels of aggressive behavior (Edwards, Eiden, Colder, & Leonard, 2006; Hussong et al., 2007; Hussong, Huang, Curran, Chassin, & Zucker, 2010). Many factors influence children’s aggressive behavior, including disinhibited behavior (e.g., Eiden, Coles, Schuetze, & Colder, 2014), exposure to interparental violence (IPV), and witnessing neighborhood violence (Eiden et al., 2014). Because beliefs about aggression are associated with aggression toward peers (e.g., Chaux, Arboleda, & Rincon, 2012), understanding how home and neighborhood violence and individual characteristics such as behavioral dysregulation during parental conflict and age are associated with children’s beliefs about aggression, may help explain why some COSAs engage in peer aggression. This understanding may help guide clinical practice with these children. In this study, we examined associations between IPV, exposure to neighborhood violence, behavioral dysregulation during parental conflict, and child age as they relate to COSAs’ attitudes about the acceptability of aggression in general as well as beliefs about the acceptability of retaliation against peers in provocative situations. Identifying predictors of normative beliefs regarding how prevalent and socially acceptable aggression is among COSAs may help practitioners with efforts to curb aggressive behaviors among this high risk population.
Behavior Problems among COSAs
Children with a substance-abusing parent are at greater risk for aggressive and delinquent behaviors than their peers (Hussong et al., 2007; Hussong, Huang, Curran, Chassin, & Zucker, 2010; Stanger et al., 1999), findings consistent across type of substance abused (e.g., alcohol [Husson et al., 2007, 2010], cocaine, opioids [Stanger et al., 1999]). As compared to youth in families in which neither parent is dependent on alcohol or illicit drugs, Marmorstein, Iacono, and McGue (2009) found offspring of parents with alcohol or illicit drug dependence were at least three times more likely to have externalizing disorders (i.e., attention deficit hyperactivity disorder, oppositional defiant disorder, conduct disorder, or adult antisocial behavior). Furthermore, these early signs of aggression may lead to a myriad of problems later in life. Aggression is often stable across the lifespan and early conduct problems predict later antisocial problems, dating violence, and substance abuse (e.g., Bradshaw, Schaeffer, Petras, & Ialongo, 2010; Fergusson, Horwood, & Ridder, 2005). Importantly, normative beliefs regarding the acceptability of aggression is strongly associated with aggressive behaviors among youths; moreover, normative beliefs regarding aggression are highly predictive of aggressive behavior over time (Huesmann & Guerra, 1997). This indicates that normative beliefs regarding the acceptability of aggression may be an important indicator of future aggressive behavior.
Parental Substance Abuse and Intimate Partner Violence
One reason why COSAs may exhibit more behavioral problems is that children who reside with a substance-abusing parent are often exposed to high rates of IPV compared to peers whose parents are not substance abusers. The association between IPV among men and women seeking treatment for substance use disorders is alarmingly high. For instance, Chermack, Fuller, and Blow (2000) found that 57% of individuals entering substance abuse treatment engaged in partner violence in the past year, and that rates did not significantly differ by the gender of the substance abuser (with 53.6% and 59.5% for male and female substance abusers, respectively). Furthermore, this association between substance abuse and increased IPV has been demonstrated for alcohol (see Foran & O’Leary, 2008; Hines & Douglas, 2011; Shorey, Stuart, McNulty, & Moore, 2014), cocaine (Norlander & Eckhardt, 2005), alcohol and cocaine or marijuana (Crane, Oberleitner, Devine, & Easton, 2014), and opioids (Subodh et al., 2014).
In one of the few studies to examine IPV among fathers with substance abuse disorder as compared to neighborhood controls, fathers in methadone maintenance treatment reported more physical, sexual, and psychological aggression toward the mother of their youngest biological child over the course of their relationship (Moore, Easton, & McMahon, 2011). A limitation of the Moore et al. study, however, was that many fathers did not live with their children. Compared to couples without children, partners who share responsibility for the care of a minor child report higher rates of IPV (McDonald, Jouriles, Ramisetty-Mikler, Caetano, & Green, 2006). Thus, couples in which one or both partners have substance use disorder and who reside together may be expected to exhibit high levels of violence (Foran & O’Leary, 2008). These home environments of escalated violence may have a strong impact in COSAs’ normative beliefs about aggression.
Neighborhood Violence
Neighborhood violence may also influence normative beliefs about the acceptability of aggression among COSAs. Families in which one or both parents use illicit drugs, particularly opiates and cocaine, are likely to be living in disadvantaged neighborhoods (e.g., Hogan, 1998). Youth who live in disadvantaged neighborhoods are likely to witness neighborhood violence (Gorman-Smith, Henry & Tolan, 2004) and are more likely to engage in peer violence (Haynie, Silver, & Teasdale, 2006). For instance, Schwab-Stone et al. (1995) found that 40% of adolescents (i.e., 6th through 8th graders) living in an urban area had seen a shooting or a stabbing in the previous year, and that exposure to violence was associated with more externalizing symptoms two years later (Schwab-Stone et al., 1999). Neighborhood disadvantage is also associated with communities that contribute to children’s adopting streetwise beliefs that condone violence (Reid, Patterson, & Snyder, 2002), children’s beliefs that they could die at a young age which may contribute to risky behaviors (De Coster, Heimer, & Wittrock, 2006), and children’s externalizing problems (Scarpa, Jurley, Shumante, & Haden, 2006).
Theoretical Perspectives on Children’s Beliefs about Aggression
According to the cognitive-contextual framework (Grych & Fincham, 1990), when children witness a conflict, they attempt to comprehend how it will affect them (i.e., perceived threat level), why it is happening (i.e., attribution), and what they can do in response (i.e., coping). Consistent with Dodge and Crick (1990), violence inside and outside of the home is theorized to lead to hypervigilance and heightened sensitivity to conflict and parental anger. This heightened sensitivity may lead children to view situations as more serious and hostile than they really are. Perceiving situations as more hostile than they truly are may prime youth to react aggressively to provocation (Grych & Fincham, 1990).
Limited research has examined how home and neighborhood violence might be associated with COSAs’ beliefs about the appropriateness of aggression and suitability of retaliation against an aggressive peer. Nascent research revealed both adolescents (Clarey, Hokoda, & Ulloa, 2010) and college students (Luthra & Gidycz, 2006) exposed to interparental violence as children are more likely to view violence as a legitimate response to conflict and are more likely to respond aggressively toward relationship partners when provoked. The relationship between IPV and acceptability of violence, however, may be more nuanced than originally believed. For instance, if children perceive a disparity in power between parents, they may feel more threatened when the aggression is directed toward the less dominant parent. Thus, because men are often physically stronger and male-to-female violence is related to increased injury of their female relationship partners (e.g., Ansara & Hindin, 2010), father-to-mother violence may be perceived as more threatening than mother-to-father aggression.
Exposure to neighborhood violence has also been related to perceiving violence as more acceptable (Allwood & Bell, 2008). However, a distinction has been made between reactive aggression (e.g., hitting another child because the peer made fun of him/her) and proactive aggression (e.g., deliberately harming or provoking another child to achieve a desired goal) (Dodge & Coie, 1987). In a study of Columbian youth (i.e., 5th to 9th graders), normative beliefs about aggression partially mediated the association between neighborhood violence and both proactive and reactive aggression (Chaux et al., 2012). Thus, believing aggression in general as well as in response to provocation is more acceptable may mediate associations between exposure to violence and peer aggressive behaviors.
To adapt the cognitive-contextual framework to both parental violence as well as general conflict, Fosco, Grych, & DeBoard (2007) incorporate perception of the justifiability of aggression into children’s appraisals of parental conflict and IPV. In turn, exposure to neighborhood violence may positively impact children’s beliefs about the justifiability of aggression via normative associations (Fosco, Grych, & DeBoard, 2007). Violent individuals have more positive attitudes toward dating aggression and may use these beliefs to justify their violent behavior (Jouriles, Grych, Rosenfield, McDonald, & Dodson, 2011). Among child-mother dyads recruited from a domestic violence shelter who recently experienced severe IPV, children’s beliefs about the justifiability of aggression were positively associated with children’s self-reports of more externalizing problems (i.e., disruptive behavior) six months later (Jouriles, Vu, McDonald, & Rosenfield, 2014).
The adapted cognitive-contextual model (Fosco et al., 2007) also contends that children’s personal characteristics (e.g., age) shape their beliefs about aggression. Graham-Bermann and Brescoll (2000) found younger children viewed aggression as a more acceptable means of resolving disagreements as compared to older children. Among COSAs, however, older age may also mean more years of living in a home characterized by IPV and greater exposure to neighborhood violence. Prolonged exposure to this type of corrosive family environment may result in higher levels of acceptability of aggression. For instance, long-term exposure to risk factors such as paternal alcoholism (Moss, Mezzich, Yao, Gavaler, & Martin, 1995) and maternal drug use (Luthar, Cushing, Merikangas, & Roundsaville, 1998) have more detrimental effects on children’s behavior than short-term exposure.
Likewise, children with low behavioral regulation (e.g., difficulty inhibiting and overriding responses or urges) are more likely to engage in greater violence (e.g., Sullivan et al., 2007; Riccio, Hewitt, & Blake, 2011). Furthermore, poor self-regulation has been shown to mediate the association between reactive aggression and externalizing problems (White, Jarrett, & Ollendick, 2013). Because COSAs may be exposed to high levels of IPV, the ability to regulate behavior during interparental conflict may be especially important to examine. The escalated environment common in COSA households makes behavioral regulation particularly relevant.
The Present Study
Our understanding of youth who reside with substance-abusing parents is based largely on families of single mothers, where children tend to experience multiple father figures or transiently reside with extended family members (Chance & Scannapieco, 2002). To address calls for research on substance-abusing fathers (McMahon, Winkel, Luthar, & Rounsaville, 2005) and to prevent the overstatement of connections between mothers’ parenting and youth beliefs, we examined beliefs about general aggression and the suitability of retaliation toward an aggressive peer among youth in two-parent families in which one or both parents had SUD. Consistent with the cognitive-contextual model and prior research, we hypothesized that exposure to IPV, exposure to neighborhood violence, behavioral dysregulation during interparental conflict, and older youth age would predict higher acceptance of general aggression and greater acceptance of retaliation toward an aggressive peer. Whether exposure to violence has stronger associations for boys versus girls is not clear (e.g., Davies & Lindsey, 2001), therefore, we explored child gender as it related to children’s beliefs about the acceptability of aggression and degree to which peer retaliation was viewed as justified; however, no specific hypotheses were made with respect to child gender.
Method
Participants
Participants were 110 families (mothers, fathers, and the child with the closest birthdate to the phone screening) in which one or both parents met DSM-IV-TR criteria for a drug or alcohol disorder or both (in n = 37 couples [33.6%] both members of the couple met diagnostic criteria). Families were recruited from those seeking treatment at two outpatient clinics or from advertisements noting that couples meeting the study criteria could receive 12 weeks of free couples-based substance abuse treatment. Families were excluded if: (a) the child had cognitive, physical, or psychological limitations that would not allow their participation, (b) neither parent was the legal guardian of the child, (c) the child did not reside with the couple full-time (in a few instances the study parent maintained joint custody of the child and the child resided in the household on a regular, structured schedule), or (d) any family member was not fluent in English. The mean age of the children was 9.81 years (SD = 4.74 years). Approximately half of the children were boys (n = 56; 50.9%) and approximately half were girls (n = 52; 47.3%) with two families not disclosing the gender of the target child. See Table 1 for additional demographic information about the sample, including diagnosis status by parent type.
Table 1.
Demographics for Sample (N = 110 Families)
| Variable | Mother | Father | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Count (%) | Mean | SD | Count (%) | Mean | SD | |
| Age in years | – | 36.15 | 8.25 | – | 38.16 | 8.31 |
| Ethnicity | ||||||
| African-American | 25 (22.7) | – | – | 28 (25.5) | – | – |
| American Indian or Alaskan Native | 6 (5.5) | – | – | 8 (7.3) | – | – |
| Asian | 3 (2.7) | – | – | 0 (0.00) | – | – |
| White | 81 (73.6) | – | – | 68 (61.8) | – | – |
| Hispanic or Latino | 9 (8.2) | – | – | 9 (8.2) | – | – |
| Native Hawaiian or other Pacific Islander | 1 (0.9) | 0 (0.0) | ||||
| Multicultural/Other | 1 (0.9) | – | – | 1 (0.9) | – | – |
| Married | – | |||||
| Yes | 52 (47.3) | – | – | 53 (48.2) | – | – |
| No | 58 (52.7) | – | – | 57 (51.8) | – | – |
| Years cohabitating | – | 7.96 | 6.67 | – | 8.25 | 6.96 |
| Years of education | – | 13.45 | 2.46 | – | 12.55 | 2.33 |
| Income (past 6 months) | ||||||
| < $20,000 | 79 (71.8) | – | – | 62 (56.4) | – | – |
| $20,000 to < $40,000 | 18 (16.4) | – | – | 22 (20.0) | – | – |
| $40,000 to < $60,000 | 7 (6.4) | – | – | 14 (12.7) | – | – |
| > $60,000 | 3 (2.7) | – | – | 12 (10.9) | – | – |
| Missing | 3 (2.7) | – | – | 0 (0.00) | – | – |
| SUD diagnosis | ||||||
| None | 61 (55.5) | – | – | 18 (16.4) | – | – |
| Alcohol only | 13 (11.8) | – | – | 27 (24.5) | – | – |
| Drug only | 10 (9.1) | – | – | 15 (13.6) | – | – |
| Alcohol and drug | 26 (23.6) | – | – | 50 (45.5) | – | – |
Note. Ethnicity counts total more than n due to endorsement of multiple categories by some participants.
Procedure
The present study examined baseline data from a larger study designed to examine the secondary effects of couples treatment for parents with substance use disorder on children in their homes. Parents received information about the study at treatment entry or heard about the study via ads and flyers posted in local agencies. Interested adults completed a brief phone interview to determine potential study eligibility. If families met study eligibility and all members of the family expressed interest, an assessment meeting was scheduled. At the assessment, partners were given a detailed description of the study, all questions were answered, and each partner was consented individually. Parents also gave consent for their minor child to participate and children gave verbal assent.
After consent was provided, both parents were individually interviewed in separate rooms with the substance use modules of the Structured Clinical Interview for DSM-IV-TR (SCID; First, Spitzer, Gibbon, & Williams, 2002). The SCID was used to delineate parents’ substance use disorders and to identify potential participants who met one or more of the diagnostic exclusion criteria. The SCID interviews were conducted by licensed mental health counselors/psychologists with extensive experience working with clients with substance use disorders. In instances in which one of the licensed professionals was not able to conduct the SCID, a research assistant with SCID training and research experience with parents with substance use disorder conducted the interview. The counselor or clinical psychologist reviewed the SCID prior to determining substance use diagnosis. Mothers and fathers completed study questionnaires separately (in separate rooms), and children completed relevant questionnaires with a researcher present. Researchers provided assistance if children requested it or were too young to complete the questionnaire without assistance. The study was conducted in accordance with the code of ethics of the American Psychological Association and human subjects approval was granted by the participating research university prior to participation. Each family received $90.00 ($30.00 each) for their participation.
Measures
Children’s Beliefs about Aggression
Children’s beliefs were assessed via the Normative Believes about Aggression Scale (NOBAGS; Huesmann & Guerra, 1997). The NOBAGS is composed of 20 self-report items that address two subscales: general beliefs about aggression, and beliefs about retaliation after provocation. There are eight items concerning general beliefs about aggression (e.g., “In general, it is wrong to hit other people”) and 12 items address respondents’ beliefs about the acceptability of retaliating in each of the scenarios (e.g., “Suppose a girl hits another girl, Mary. Do you think it’s wrong for Mary to hit her back?”). Response options for both subscales are: 1 (It’s really wrong), 2 (It’s sort of wrong), 3 (It’s sort of ok), and 4 (It’s perfectly ok). Item scores were summed to create two overall scores that reflect an acceptability of general aggression score and an acceptability of retaliation score for each participant; higher scores indicate greater acceptability. Internal consistency was acceptable for general beliefs about aggression (α = .65) and retaliation (α = .89).
Child exposure to violence
Child exposure to violence outside the home was assessed via the Exposure to Violence scale (MyETV; Buka, Selner-O’Hagan, Kindlon, & Earls, 1997). MyETV is a 36-item self-report measure that asks children to report on past 3 months and lifetime exposure to violence. Although the ETV is comprised of 16 statements that describe violence in the home (e.g., “In the last 3 months, how often have you seen someone hit in your home?”), items that target violence in the home do not clarify the perpetrator/victim and may also overlap with the parental IPV assessment; therefore, only the 10 items that assessed past 3 months violence outside the home (e.g., “In the last 3 months, how often have you heard gunfire?”; In the last 3 months, how often have you seen someone attacked with a weapon?) were examined. Response options were 1 (never), 2 (once), 3 (2 or 3 times), 4 (4 to 10 times), 5 (11 to 50 times), and 6 (more than 50 times). Item scores were summed to reflect past three month exposure to violence in the neighborhood; higher scores reflect greater violence exposure (α = .73).
Child behavioral dysregulation
Child behavioral dysregulation was assessed via the Security in the Interparental Subsystem scale (SIS; Davies, Forman, Rasi, & Stevens, 2002). The SIS is comprised of 43 items to assess seven dimensions of different internal and external behaviors children may engage in during interparental conflict. For the purpose of the present study, however, only the three-item Behavioral Dysregulation dimension was used. A sample item is, “When my parents have an argument, I yell at or say unkind things to people in my family.” Using a Likert-type scale ranging from 1 (not at all true of me) to 4 (very true of me), children reported how true each behavior was for them in the past year. Items were summed to create a total score (α = .61).
Interparental violence (IPV)
IPV was assessed via the Revised Conflict Tactics Scale-2 (CTS2; Straus, Hamby, Boney-McCoy, & Sugarman, 1996). Fathers and mothers independently completed the Physical Assault subscale of the CTS2. Sample items include “I threw something at my partner that could hurt” and “I pushed or shoved my partner.” Parents reported how frequently they perpetrated various acts of partner violence in the past year using response choices 0 (never), 1 (once), 2 (twice), 3 (3–5 times), 4 (6–10 times), 5 (11–20 times), 6 (more than 20 times), and 7 (not in the past year, but it did happen before). Midpoint estimates were used for response ranges (e.g., 6–10 times = 8) consistent with Straus et al (1996). Items were summed to create two partner violence perpetration scores; father-to-mother perpetration (α = .83) and mother-to-father perpetration (α = .83); higher scores reflect more frequent past-year violence perpetration. The square root of the total score was used to reduce skewness for the current sample.
Analysis Approach
To determine the effect of children’s exposure to violence outside the home, children’s behavioral dysregulation, and parental IPV on children’s acceptability of aggression, a single path model incorporating multivariate regressions was estimated. The dependent variables were the two subscale scores from the NOBAGS: (1) general beliefs about aggression, and (2) retaliation. Predictor variables were children’s exposure (in past three months) to violence outside the home, children’s behavioral dysregulation during interparental conflict, children’s age, mother’s (past year) perpetration of IPV against father, and father’s (past year) perpetration of IPV against mother (see Figure 1). Child gender was not associated with the dependent variables (p > .05) and not explored further. All predictors were allowed to correlate within the model.
Figure 1.
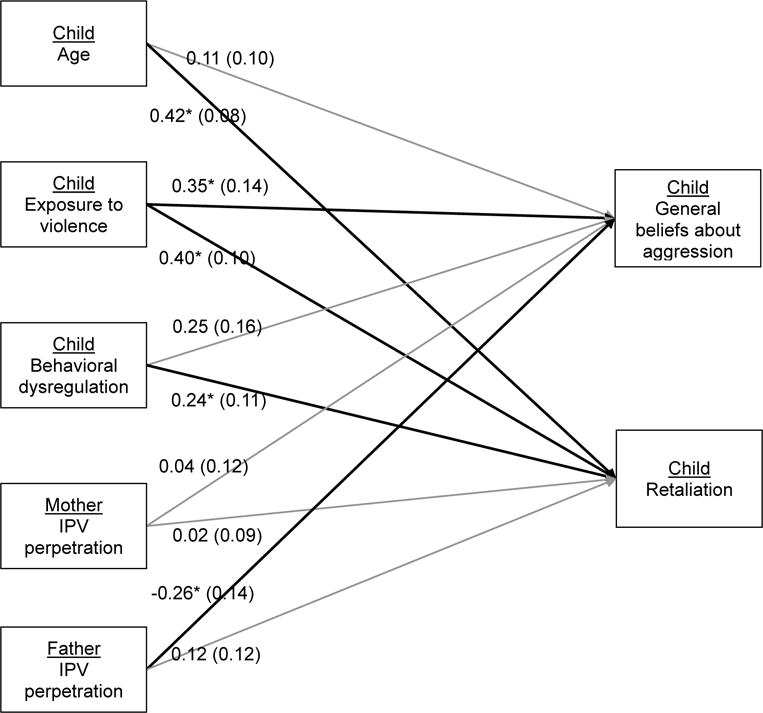
Multivariate regression model. IPV = interparental violence. Standardized regression coefficients are presented with associated standard errors in parentheses. Significant coefficients at the p < .05 level are represented with asterisks, and corresponding paths are bold. Note that predictors were allowed to correlate, but this is omitted from the figure for clarity.
The model was fitted in Mplus 7.4 using full-information maximum likelihood estimation (FIML). Bootstrapping with 5,000 replications was used to account for small departures from normality, thus 95% bootstrap empirical confidence intervals were used to identify estimates statistically significant at α = .05 (i.e., confidence intervals not containing zero indicated p < .05). Pearson correlations and descriptive statistics among study variables are presented in Table 2.
Table 2.
Pearson Correlations and Descriptive Statistics for Study Variables
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|
| 1. Child: General Beliefs | (.65) | ||||||
| 2. Child: Retaliation | .52 | (.89) | |||||
| 3. Child: Exposure to Violence | .32 | .38 | (.73) | ||||
| 4. Child: Behavioral Dysregulation | .25 | .22 | −.16 | (.61) | |||
| 5. Child: Age | .16 | .47 | .14 | .09 | – | ||
| 6. Mother: IPV perpetration | −.08 | −.00 | −.19 | .20 | −.20 | (.83) | |
| 7. Father: IPV perpetration | −.20 | .12 | −.04 | .03 | −.11 | .42 | (.83) |
|
| |||||||
| Mean | 10.39 | 19.50 | 4.13 | 3.60 | 9.81 | 2.45 | 1.33 |
| Standard deviation | 3.10 | 6.99 | 4.66 | 0.25 | 4.74 | 2.60 | 1.78 |
| Skewness | 1.96 | 0.74 | 2.29 | 2.31 | −0.11 | 1.40 | 2.00 |
| Kurtosis | 4.18 | −0.34 | 6.50 | 4.53 | −0.82 | 1.68 | 5.12 |
Note. All estimates are maximum likelihood estimates obtaining using full-information maximum likelihood except skewness and kurtosis; these estimates are the standard moment estimates ignoring missing data. Bold font indicates statistical significance at α = .05. Cronbach’s alphas are presented in parentheses along the diagonal.
Results
Three univariate outliers for behavioral dysregulation were identified using boxplots. To prevent spurious effects due to outliers, the influential data were adjusted to a score one higher than the next most extreme score. Outliers were not detected in the other study variables. Missing data ranged from none on child’s age to 19.1% on children’s exposure to violence. Missing data were handled via FIML estimation. To determine the potential effects of missing data on results, models were re-estimated using listwise deletion. The results were identical in terms of magnitude of regression coefficients and statistical significance of effects. Given that we had common amounts of missing data (e.g., Schlomer, Bauman, & Card, 2010) and results with FIML paralleled those with listwise deletion, we report results with FIML below.
Multivariate Regression Model
As seen in Table 3, results indicated that after controlling for other variables, children’s exposure to neighborhood violence was positively related to children’s general beliefs about aggression, whereas, and father’s perpetration of violence toward mothers was negatively related to children’s general beliefs about aggression. That is, when other variables are held constant, more exposure to violence outside the home is associated with more acceptance regarding general aggression (e.g., acceptability about hitting people) among COSAs, but higher IPV perpetration by fathers is associated with less acceptance regarding general aggression.
Table 3.
Summary of Multivariate Regression Predicting Children’s Acceptability about Aggression
| 95% CI for β
|
|||||
|---|---|---|---|---|---|
| Outcome: General beliefs (R2 = .297) | b | β | SE (β) | LL | UL |
| Child: Age | 0.075 | 0.111 | 0.098 | −0.094 | 0.303 |
| Child: Exposure to violence | 0.233 | 0.353 | 0.142 | 0.071 | 0.616 |
| Child: Behavioral dysregulation | 0.617 | 0.245 | 0.157 | −0.077 | 0.544 |
| Mother: IPV perpetration | 0.047 | 0.038 | 0.123 | −0.176 | 0.327 |
| Father: IPV perpetration | −0.471 | −0.264 | 0.136 | −0.549 | −0.02 |
|
| |||||
| 95% CI for β
|
|||||
| Outcome: Retaliation (R2 = .443) | b | β | SE (β) | LL | UL |
|
| |||||
| Child: Age | 0.644 | 0.424 | 0.080 | 0.258 | 0.578 |
| Child: Exposure to violence | 0.59 | 0.397 | 0.100 | 0.201 | 0.587 |
| Child: Behavioral dysregulation | 1.373 | 0.242 | 0.105 | 0.039 | 0.454 |
| Mother: IPV perpetration | 0.061 | 0.022 | 0.091 | −0.154 | 0.202 |
| Father: IPV perpetration | 0.498 | 0.124 | 0.124 | −0.102 | 0.388 |
Note. N = 110. b = unstandardized parameter estimates, β = standardized parameter estimates, SE = standard error. LL = lower limit, UL = upper limit for 95% bootstrap empirical confidence intervals (n = 5,000), used to identify estimates statistically significant at α = .05 (identified via bold typeface).
Results also indicated that, while controlling for other variables, children’s exposure to violence outside the home, children’s behavioral dysregulation during interparental conflict, and children’s age were all positively related to children’s beliefs about retaliation (see Table 3). For children, more exposure to violence outside the home, higher behavioral dysregulation (i.e., poorer behavioral regulation), and older age were associated with more accepting attitudes about retaliation toward an aggressive peer among COSAs. See Figure 1 for a pictorial representation of these relationships, with bold lines indicating significant relationships among variables.
Discussion
Although COSAs are more likely to experience behavioral problems (e.g., Marmorstein et al., 2009) and high levels of aggressive behavior (e.g., Hussong et al., 2007; Hussong, Huang, Curran, Chassin, & Zucker, 2010), understanding why some COSAs develop externalizing problems and others do not is unclear. The present study examined variables that may contribute to COSAs’ beliefs about the acceptability of general aggression and retaliation against a peer. Study hypotheses were fully confirmed for exposure to neighborhood violence, and partially confirmed for child age and behavioral dysregulation (i.e., for retaliation against peers, but not general aggression). An interesting finding also emerged where the hypothesis regarding IPV was partially confirmed, with father perpetration of violence against mothers being linked to beliefs about general aggression, though negatively so.
Although considerable research has shown that exposure to IPV provides a model for children to imitate or tolerate these behaviors in later life (O’Keefe, 1998), our findings suggest father-to-mother aggression was actually associated with less acceptance of general aggression. This finding reflects the gendered nature of domestic violence. That is, women are more likely to be injured by IPV, “not necessarily because men strike more often, but because men strike harder” (Morse, 1995, p. 269). Furthermore, even when men and women engage in what appears to be the same act (e.g., slapping or shoving a partner), owing to differences in size and strength, there is greater potential for men to harm women than vice versa (Straus, 1990). Thus, consistent with the cognitive-contextual framework (Fosco et al., 2007), partner violence by fathers (often the more physically dominant parent) that is directed toward mothers may intensify children’s perceived threat and have stronger associations with children’s beliefs about aggression. Related to this point, women typically have more fear of a violent partner than do men (Ross, 2012). It is possible that children may sense some of their mothers’ fear, which may also heighten children’s perceptions of threat and contribute to children’s recognition that interparental violence is not acceptable. In addition, it is important to recognize that we assessed children’s beliefs about the acceptability of aggression, which may differ from actual acts of aggression. That is, a child could believe that violence is wrong, yet still act in a violent way towards peers.
As expected, greater exposure to neighborhood violence was consistently associated with greater acceptance of general aggression. This finding supports the cognitive-contextual framework (Fosco et al., 2007) in that greater exposure to neighborhood violence may create a set of beliefs that it is acceptable to use violence in social situations (Topalli et al., 2014). Individuals who use illegal drugs often live in neighborhoods characterized by poverty and violence (e.g., Hogan, 1998). This was the case in the present study as 50% of children reported having heard gunfire and 8% of children had seen a shooting in the three months prior to study participation.
As a second component of aggression beliefs, children’s reports of exposure to neighborhood violence, behavioral dysregulation in response to interparental conflict, and older age were associated with greater approval of the retaliation against an aggressive peer. In line with the cognitive-contextual framework, violence outside the home was associated with children’s beliefs that retaliation toward an aggressive peer was acceptable. Grych and Fincham (1990) contend that exposure to neighborhood violence may lead children to mis-perceive other children as more hostile than they actually are and thus prime youth to react aggressively to provocation. Our findings extend the literature by demonstrating that exposure to neighborhood violence among COSAs is associated with the degree to which retaliation against an aggressive peer is perceived as acceptable.
Although behavioral dysregulation was not associated with children’s reports of the acceptability of general aggression, children who reported less behavioral control during interparental conflict were more likely to approve of violence when provoked. This finding supports previous research that has shown links between poorer behavioral regulation and reactive, but not proactive, aggression (White et al., 2013). A number of investigators (e.g., Blais, Solodukhin, & Forth, 2014) have documented differences between children who engage in proactive (i.e., aggression that is not provoked) versus reactive aggression (i.e., aggression that is in response to provocation). It is possible that other characteristics not examined, such as callous-unemotional tendencies (Leeuwen, Rodgers, Gibbs, & Chabrol, 2013), may account for COSAs’ beliefs regarding proactive peer aggression (non-provoked aggression).
Older COSAs were more likely to endorse retaliation against an aggressive peer as acceptable. As shown in Table 2, older youth reported more exposure to neighborhood violence. Prolonged exposure to neighborhoods in which violence is common may explain this finding. This finding also supports studies that have shown that prolonged exposure to paternal alcoholism (Moss et al., 1995) and maternal drug use (Luthar et al., 1998) have more detrimental effects on children’s behavior than short-term exposure. This finding may also support the peer contagion hypothesis (e.g., Dishion, McCord, & Poulin, 1999). That is, as children age, they spend more time with peers. Association with aggressive peers may have negative effects on youth. In addition, children who reside in poor or dangerous neighborhoods may learn that avoiding confrontation may lead to children’s elevated risk for peer victimization. Although we did not examine children’s behavior, importantly, retaliatory attitudes appear to increase youth violence in other samples (e.g., Copeland-Linder et al., 2012).
Clinical Implications
COSAs represent a hard-to-reach population. Given the reluctance of many parents seeking substance abuse treatment to allow their children to receive individual or family mental health treatment (Kelley, D’Lima, Henson, & Cotton, 2014), the current findings indicate that programs for parents should include information on how interparental conflict and neighborhood violence may impact their children. In addition, online parenting programs could be developed to aide these parents, particularly those who are not able or willing to attend face-to-face treatment. Given their risk for behavioral problems (e.g., Marmorstein et al., 2009), programs are needed that target children who perceive aggression as more acceptable prior to the development of behavioral disorders. Identifying youth early (i.e., while normative beliefs regarding aggression are emerging but aggressive behavior has not yet manifested) may be key as moderate to severe aggression in youth is characterized by poor treatment outcomes and the need for more extensive treatment (see Werry, 1997 for a review).
Study Limitations
Although this study extends our knowledge of COSAs’ attitudes about beliefs about general aggression as well as retaliation against a peer, there are several limitations. Of note, the study was cross-sectional. Future research should examine these associations in a longitudinal design. Importantly, we focused on beliefs regarding aggression rather than aggressive behaviors themselves. While there strong associations have been observed between aggressive beliefs and behaviors (Huesmann & Guerra, 1997), aggressive behaviors should be directly studies in future studies. In addition, parents indicated they were willing to attend treatment for substance abuse with their partner. Parents were also willing to take part in the study and allow their children to take part. Thurs, we must use caution in generalizing findings to other populations (e.g., where parents are unwilling to seek treatment for themselves or their children). Further, we did not ask parents or children about behaviors that constitute child maltreatment. Therefore, we were not able to examine whether child maltreatment was associated with children’s beliefs about aggression.
In addition, the sample was comprised of married or cohabitating two-parent families who were living with a child. In all but 18 families, fathers met criteria for substance use disorders. Men are more likely to use all substances other than nonmedical use of psychotherapeutic drugs and pain relievers than women (Substance Abuse and Mental Health Services Administration, 2013). Thus, this family dynamic may be the most common way that children are exposed to parental substance abuse. Nevertheless, these results may not generalize single-parent families. Finally, parents were recruited to the study that met substance abuse criteria for any number of drugs or alcohol use combinations. The sample size prohibited fine-grained analysis of different forms of alcohol or drug use as related to child beliefs regarding aggression.
Conclusions
Among COSAs, those who witness neighborhood violence are more likely to believe aggression in general is acceptable and are more likely to approve of retaliation against a provocative peer. Furthermore, older age and less behavioral regulation in response to interparental conflict was associated with greater approval of retaliation against an aggressive peer. These findings suggest the importance of intervening with these children prior to the development of serious behavioral problems. Father-to-mother aggression in the last year, however, was associated with less acceptability of peer aggression suggesting that children who live in homes in which fathers’ exhibit aggression against their mothers understand the seriousness of these behaviors. While this finding is important, because children who witness family violence are more likely to engage in dating violence (e.g., Clarey et al., 2010), late childhood or early adolescence may be a critical period to reinforce COSAs’ beliefs about the acceptability of aggression.
Acknowledgments
Funding
This research was supported by The National Institute of Drug Abuse.
References
- Allwood MA, Bell DJ. A preliminary examination of emotional and cognitive mediators in the relations between violence exposure and violent behaviors in youth. Journal of Neighborhood Psychology. 2008;36:989–1007. [Google Scholar]
- Ansara DL, Hindin MJ. Exploring gender differences in the patterns of intimate partner violence in Canada: A latent class approach. Journal of Epidemiology and Neighborhood Health. 2010;64:849–854. doi: 10.1136/jech.2009.095208. [DOI] [PubMed] [Google Scholar]
- Blais J, Solodukhin E, Forth AE. A meta-analysis exploring the relationship between psychopathy and instrumental versus reactive violence. Criminal Justice and Behavior. 2014;41:797–821. [Google Scholar]
- Bradshaw CP, Schaeffer CM, Petras H, Ialongo N. Predicting negative life outcomes from early aggressive-disruptive behavior trajectories: Gender differences in maladaptation across life domains. Journal of Youth and Adolescence. 2010;39:953–966. doi: 10.1007/s10964-009-9442-8. [DOI] [PubMed] [Google Scholar]
- Buka SL, Selner-O’Hagan MB, Kindlon DJ, Earls FJ. The “My Exposure to Violence Interviews”; Administration and Scoring Manual, Version 3. Boston, MA: Harvard School of Public Health; 1997. [Google Scholar]
- Chance T, Scannapieco M. Ecological correlates of child maltreatment: Similarities and differences between child fatality and nonfatality cases. Child & Adolescent Social Work Journal. 2002;19:139–161. [Google Scholar]
- Chaux E, Arboleda J, Rincon C. Neighborhood violence and reactive and proactive aggression: The mediating role of cognitive and emotional variables. Revista Colombiana de Psicologia. 2012;21:233–251. [Google Scholar]
- Chermack ST, Fuller BE, Blow FC. Predictors of expressed partner and non-partner violence among patients in substance abuse treatment. Drug and Alcohol Dependence. 2000;58(1–2):43–54. doi: 10.1016/s0376-8716(99)00067-8. [DOI] [PubMed] [Google Scholar]
- Clarey A, Hokoda A, Ulloa EC. Anger control and acceptance of violence as mediators in the relationship between exposure to interparental conflict and dating violence perpetration in Mexican adolescents. Journal of Family Violence. 2010;25:619–625. [Google Scholar]
- Copeland-Linder N, Johnson SB, Haynie DL, Chung S, Cheng TL. Retaliatory attitudes and violent behaviors among assault-injured youth. Journal of Adolescent Health. 2012;50:215–220. doi: 10.1016/j.jadohealth.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crane CA, Oberleitner LMS, Devine S, Easton CJ. Substance use disorders and intimate partner violence perpetration among male and female offenders. Psychology of Violence. 2014;4:322–333. doi: 10.1037/a0034338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davies PT, Forman EM, Rasi JA, Stevens KI. Assessing children’s emotional security in the interparental relationship: The security in the interparental subsystem scales. Child Development. 2002;73:544–562. doi: 10.1111/1467-8624.00423. [DOI] [PubMed] [Google Scholar]
- Davies PT, Lindsay L. Does gender moderate the effects of conflict on children? In: Grych J, Fincham F, editors. Child Development and Interparental Conflict. New York: Cambridge University Press; 2001. pp. 64–97. [Google Scholar]
- De Coster S, Heimer K, Wtitrock S. The Neighborhood Disadvantage, Social Capital, Street Context, and Youth Violence. The Sociological Quarterly. 2006;47:723–753. [Google Scholar]
- Dishion TJ, McCord J, Poulin F. When interventions harm: Peer groups and problem behavior. American Psychologist. 1999;54:755–764. doi: 10.1037//0003-066x.54.9.755. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Coie JD. Social-information-processing factors in reactive and proactive aggression in children’s peer groups. Journal of Personality and Social Psychology. 1987;53:1146–1158. doi: 10.1037//0022-3514.53.6.1146. [DOI] [PubMed] [Google Scholar]
- Dodge KA, Crick NR. Social information-processing bases of aggressive behavior in children. Personality and Social Psychology Bulletin. 1990;16:8–22. [Google Scholar]
- Eiden RD, Coles CD, Schuetze P, Colder CR. Externalizing behavior problems among polydrug cocaine-exposed children: Indirect pathways via maternal harshness and self-regulation in early childhood. Psychology of Addictive Behaviors. 2014;28:139–153. doi: 10.1037/a0032632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards EP, Eiden RD, Colder C, Leonard KE. The development of aggression in 18 to 48 month old children of alcoholic parents. Journal of Abnormal Child Psychology. 2006;34:409–423. doi: 10.1007/s10802-006-9021-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson DM, Horwood LJ, Ridder EM. Show me the child at seven: The consequences of conduct problems in childhood for psychosocial functioning in adulthood. Journal of Child Psychology and Psychiatry. 2005;46:837–849. doi: 10.1111/j.1469-7610.2004.00387.x. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version. Patient. New York: Biometrics Research, New York State Psychiatric Institute; 2002. Nov, (SCID-I/P). 2002. [Google Scholar]
- Foran HM, O’Leary KD. Alcohol and intimate partner violence: A meta-analytic review. Clinical Psychology Review. 2008;28:1222–1234. doi: 10.1016/j.cpr.2008.05.001. [DOI] [PubMed] [Google Scholar]
- Fosco GM, Grych JH, DeBoard RL. Making sense of family violence: Implications of children’s appraisals of interparental aggression for their short- and long-term functioning. European Psychologist. 2007;12:6–16. [Google Scholar]
- Gorman-Smith D, Henry DB, Tolan PH. Exposure to neighborhood violence and violence perpetration: The protective effects of family functioning. Journal of Clinical Child and Adolescent Psychology. 2004;33:439–449. doi: 10.1207/s15374424jccp3303_2. [DOI] [PubMed] [Google Scholar]
- Graham-Bermann SA, Brescoll V. Gender, power, and violence: Assessing the family stereotypes of the children of batterers. Journal of Family Psychology. 2000;14:600–612. doi: 10.1037//0893-3200.14.4.600. [DOI] [PubMed] [Google Scholar]
- Grych JH, Fincham FD. Marital conflict and children’s adjustment: A cognitive-contextual framework. Psychological Bulletin. 1990;108:267–290. doi: 10.1037/0033-2909.108.2.267. [DOI] [PubMed] [Google Scholar]
- Haynie D, Silver E, Teasdale B. Neighborhood characteristics, peer networks, and adolescent violence. Journal of Quantitative Criminology. 2006;22:147–169. [Google Scholar]
- Hines DA, Douglas EM. Alcohol and drug abuse in men who sustain intimate partner violence. Aggressive Behavior. 2011;38:31–46. doi: 10.1002/ab.20418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogan DM. Annotation: The psychological development and welfare of children of opiate and cocaine users. Review and research needs. Journal of Child Psychology and Psychiatry. 1998;39:609–619. [PubMed] [Google Scholar]
- Huesmann LR, Guerra NG. Children’s normative beliefs about aggression and aggressive behavior. Journal of Personality and Social Psychology. 1997;72:408–419. doi: 10.1037//0022-3514.72.2.408. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Huang W, Curran PJ, Chassin L, Zucker RA. Parent alcoholism impacts the severity and timing of children’s externalizing symptoms. Journal of Abnormal Child Psychology. 2010;38:367–380. doi: 10.1007/s10802-009-9374-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Wirth RJ, Edwards MC, Curran PJ, Chassin LA, Zucker RA. Externalizing symptoms among children of alcoholic parents: entry points for an antisocial pathway to alcoholism. Journal of Abnormal Psychology. 2007;116:529–542. doi: 10.1037/0021-843X.116.3.529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jouriles EN, Vu NL, McDonald R, Rosenfield D. Children’s appraisals of conflict, beliefs about aggression, and externalizing problems in families characterized by severe intimate partner violence. Journal of Family Psychology. 2014;28:915–924. doi: 10.1037/a0037921. [DOI] [PubMed] [Google Scholar]
- Jouriles EN, Grych JH, Rosenfield D. Automatic cognitions and teen dating violence. Psychology of Violence. 2011;1:302–314. [Google Scholar]
- Kelley ML, D’Lima GM, Henson JM, Cotton C. Substance-abusing mothers and fathers’ willingness to allow their children to receive mental health treatment. Journal of Substance Abuse Treatment. 2014;47:106–111. doi: 10.1016/j.jsat.2014.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leeuwen N, Rodgers RF, Gibbs JC, Chabrol H. Callous-unemotional traits and antisocial behavioral among adolescents: The roles of self-serving cognitions. Journal of Abnormal Child Psychology. 2013;42:229–237. doi: 10.1007/s10802-013-9779-z. [DOI] [PubMed] [Google Scholar]
- Luthar SS, Cushing G, Merikangas KR, Roundsaville BJ. Multiple jeopardy: Risk/protective factors among addicted mothers’ offspring. Development and Psychopathology. 1998;11:117–136. doi: 10.1017/s0954579498001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luthra R, Gidycz CA. Dating violence among college men and women. Journal of Interpersonal Violence. 2006;21:717–731. doi: 10.1177/0886260506287312. [DOI] [PubMed] [Google Scholar]
- Marmorstein NR, Iacono WG, McGue M. Alcohol and illicit drug dependence among parents: Associations with offspring externalizing disorders. Psychological Medicine. 2009;39:149–155. doi: 10.1017/S0033291708003085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDonald R, Jouriles EN, Ramisetty-Mikler S, Caetano R, Green CE. Estimating the number of American children living in partner-violence families. Journal of Family Psychology. 2006;20:137–142. doi: 10.1037/0893-3200.20.1.137. [DOI] [PubMed] [Google Scholar]
- McMahon TJ, Winkel JD, Luthar SS. Looking for poppa: Parenting status of men versus women seeking drug abuse treatment. American Journal of Drug and Alcohol Abuse. 2005;31:79–91. [PubMed] [Google Scholar]
- Milletich RJ, Kelley ML, Doane AN, Pearson MP. Exposure to interparental violence and childhood physical and emotional abuse as related to physical aggression in undergraduate dating relationships. Journal of Family Violence. 2010;25:627–637. [Google Scholar]
- Moore BC, Easton CJ, McMahon TJ. Drug abuse and intimate partner violence: A comparative study of opioid-dependent fathers. American Journal of Orthopsychiatry. 2011;81:218–227. doi: 10.1111/j.1939-0025.2011.01091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morse BJ. Beyond the conflict tactics scale: Assessing gender differences in partner violence. Violence and Victims. 1995;10:251–272. [PubMed] [Google Scholar]
- Moss HB, Mezzich A, Yao JK, Gavaler J, Martin CS. Aggressivity among sons of substance-abusing fathers: Association with psychiatric disorder in the father and son, paternal personality, pubertal development, and socioeconomic status. American Journal of Drug and Alcohol Abuse. 1995;21:195–208. doi: 10.3109/00952999509002688. [DOI] [PubMed] [Google Scholar]
- Norlander B, Eckhardt C. Anger, hostility, and male perpetrators of intimate partner violence: A meta-analytic review. Clinical Psychology Review. 2005;25:119–152. doi: 10.1016/j.cpr.2004.10.001. [DOI] [PubMed] [Google Scholar]
- O’Keefe M. Factor mediating the link between witnessing interparental violence and dating violence. Journal of Family Violence. 1998;13:39–57. [Google Scholar]
- Reid JB, Patterson GR, Snyder J. Antisocial behavior in children and adolescents: A developmental analysis and model for intervention. Washington, DC, US: American Psychological Association; 2002. [Google Scholar]
- Riccio CA, Hewitt LL, Blake JJ. Relation of measures of executive function to aggressive behavior in children. Applied Neuropsychology. 2011;18(1):1–10. doi: 10.1080/09084282.2010.525143. [DOI] [PubMed] [Google Scholar]
- Ross JM. Self-reported fear in partner violent relationships: Findings on gender differences from two samples. Psychology of Violence. 2012;2:58–75. [Google Scholar]
- Scarpa A, Hurley JD, Shumante HW, Haden SC. Lifetime prevalence and socioemotional effects of hearing about neighborhood violence. Journal of Interpersonal Violence. 2006;21:5–23. doi: 10.1177/0886260505281661. [DOI] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, Card NA. Best practices for missing data management in counseling psychology. Journal of Counseling Psychology. 2010;57:1–10. doi: 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone ME, Ayers TS, Kasprow W, Voyce C, et al. No safe haven: A study of violence exposure in an urban community. Journal of the American Academy of Child & Adolescent Psychiatry. 1995;34(10):1343–1352. doi: 10.1097/00004583-199510000-00020. [DOI] [PubMed] [Google Scholar]
- Schwab-Stone ME, Chen C, Greenberger E, Silver D, Lichtmas J, Voyce C. No safe haven II: The effect of violence exposure on urban youth. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38(4):359–367. doi: 10.1097/00004583-199904000-00007. [DOI] [PubMed] [Google Scholar]
- Selner-O’Hagan, Kindlon DJ, Buka SL, Raudenbush SW, Earls FJ. Assessing exposure to violence in urban youth. Journal of Child Psychology and Psychiatry. 1998;39:215–224. [PubMed] [Google Scholar]
- Shorey RC, Stuart GL, McNulty JK, Moore TM. Acute alcohol use temporally increases the odds of male perpetrated dating violence: A 90-day diary analysis. Addictive Behaviors. 2014;39:365–368. doi: 10.1016/j.addbeh.2013.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanger C, Higgins ST, Bickel WK, Elk R, Grabowski J, Schmitz J, et al. Behavioral and emotional problems among children of cocaine- and opiate-dependent parents. Journal of the American Academy of Child & Adolescent Psychiatry. 1999;38:421–428. doi: 10.1097/00004583-199904000-00015. [DOI] [PubMed] [Google Scholar]
- Strauss MA. The conflict tactic scales and its critics: An evaluation and new data on validity and reliability. In: Strauss MA, Gelles RJ, editors. Physical violence in American families: Risk factors and adaptations to violence in 8,145 families. New Brunswick, NJ: Transaction Books; 1990. pp. 49–73. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The Revised Conflict Tactics Scales (CTS2). Development and preliminary psychometric data. Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Subodh NB, Grover M, Grewal M, Grewal S, Basu D, Mattoo SK. Interpersonal violence against wives by substance dependent men. Drug and Alcohol Dependence. 2014;138:124–129. doi: 10.1016/j.drugalcdep.2014.02.017. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. pp. 13–4795. (NSDUH Series H-46, HHS Publication No. (SMA)). [Google Scholar]
- Sullivan TN, Farrell AD, Kliewer W, Vulin-Reynolds M, Valois RF. Exposure to violence in early adolescence: The impact of self-restraint, witnessing violence, and victimization on aggression and drug use. The Journal of Early Adolescence. 2007;27:296–323. [Google Scholar]
- Topalli V, Giancola PR, Tarter RE, Swahn M, Martel MM, Godlaski AJ, McCoun KT. The persistence of neighborhood disadvantage: An experimental investigation of alcohol and later physical aggression. Criminal Justice and Behavior. 2014;41:400–416. [Google Scholar]
- Werry JS. Severe conduct disorder: Some key issue. Canadian Journal of Psychiatry. 1997;42:577–583. doi: 10.1177/070674379704200603. [DOI] [PubMed] [Google Scholar]
- White BA, Jarrett MA, Ollendick TH. Self-regulation deficits explain the link between reactive aggression and internalizing and externalizing behavior problems in children. Journal of Psychopathology and Behavioral Assessment. 2013;35:1–9. [Google Scholar]


