Abstract
Background
In an attempt to resolve questions regarding the symptom classification of autism spectrum disorder (ASD), previous research generally aimed to demonstrate superiority of one model over another. Rather than adjudicating which model may be optimal, we propose an alternative approach that integrates competing models using Goldberg’s bass-ackwards method, providing a comprehensive understanding of the underlying symptom structure of ASD.
Methods
The study sample comprised 3,825 individuals, consecutive referrals to a university hospital developmental disabilities specialty clinic or a child psychiatry outpatient clinic. This study analyzed DSM-IV-referenced ASD symptom statements from parent and teacher versions of the Child and Adolescent Symptom Inventory-4R (CASI-4R). A series of exploratory structural equation models was conducted in order to produce interpretable latent factors that account for multivariate covariance.
Results
Results indicated that ASD symptoms were structured into an interpretable hierarchy across multiple informants. This hierarchy includes five levels; key features of ASD bifurcate into different constructs with increasing specificity.
Conclusions
This is the first study to examine an underlying structural hierarchy of ASD symptomatology using the bass-ackwards method. This hierarchy demonstrates how core features of ASD relate at differing levels of resolution, providing a model for conceptualizing ASD heterogeneity and a structure for integrating divergent theories of cognitive processes and behavioral features that define the disorder. These findings suggest that a more coherent and complete understanding of the structure of ASD symptoms may be reflected in a meta-structure rather than at one level of resolution.
Keywords: autism spectrum disorder, classification, structural hierarchy, Child and Adolescent Symptom Inventory, bass-ackwards
Introduction
Though its specific diagnostic criteria have evolved over the decades, autism spectrum disorder (ASD) remains a neurodevelopmental disorder characterized by a diverse range of atypical social, communication, and repetitive behaviors. Despite substantial and increasing clinical and research efforts focusing on ASD, fundamental questions regarding the classification of the disorder remain unresolved (Happé, 2011; Lecavalier, Gadow, DeVincent, Houts, & Edwards, 2009). Indeed, various classification and conceptual models of ASD have been proposed, resulting in a vast, piecemeal literature (Baron-Cohen, Leslie, & Frith, 1985; Chevallier, Kohls, Troiani, Brodkin, & Schultz, 2012; Mazefsky et al., 2013). To date, no study has integrated various models of ASD into a common framework; as such, a comprehensive overview of model utility cannot be adjudicated from the extant literature.
There is little consensus regarding the structure of ASD. Official nosologies, like the DSM-5 and ICD-10 (American Psychiatric Association, 2013; World Health Organization, 1992), have shifted ASD conceptualizations over time from a collection of interrelated syndromes characterized by a triad of symptoms (insistence on sameness, impaired ability to relate to others, and communication deficits) to a spectrum composed of two domains (social-communication deficits and restricted and repetitive behaviors; RRB) (American Psychiatric Association, 1980; Volkmar & McPartland, 2014). While some models identified in the research literature converged with these DSM-type classifications (e.g., Lecavalier et al., 2006; Mandy, Charman, & Skuse, 2012), others demonstrated that constructs not currently included in diagnostic classification systems (e.g., theory of mind, emotion regulation, emotion recognition, social avoidance, social intent, social motivation) represent key, even pathognomonic features of ASD (Baron-Cohen et al., 1985; Chevallier et al., 2012; Constantino et al., 2004; Duku et al., 2013; Mazefsky et al., 2013). However, research regarding these latter models tends to focus on how deficits associated with a single construct have effects on other deficit domains rather than modeling how deficits in multiple domains may interrelate. Meanwhile, data-driven modeling efforts have varied widely in the symptom structures they report (Constantino et al, 2004; Lecavalier et al., 2006; Mandy et al., 2012). However, no study to date has examined how various multifactorial models may interrelate, and whether more fine-grained classification systems may in fact reflect common symptom structures seen in broader construct-driven approaches.
Toward an Integrative Model of ASD
In an attempt to resolve these classification questions, ASD research generally aims to demonstrate superiority of one model over another (Duku et al., 2013; Mandy et al., 2012; Snow, Lecavalier, & Houts, 2009). Rather than adjudicating which model may be optimal, an alternative approach may prove beneficial: the development of a model that integrates competing models. Such an integration would highlight points of congruence and divergence and potentially synthesize the currently equivocal ASD nosological literature, providing a comprehensive understanding of the underlying structure of ASD. Moreover, this sort of integrative model could allow researchers to link findings that emerged from the different competing models of ASD.
In the current study, we applied Goldberg’s (2006) bass-ackwards method to investigate the structural hierarchy of ASD across various levels of resolution. This method produces a multi-level structure that links all plausible factor models, yielding an interpretable hierarchy of latent structures underlying observed data. Thus, applying this method to ASD data could help clarify what sort of symptom domains of ASD emerge as unique factors at each level and how a certain symptom domain is related to other domains within a single overarching structure of symptoms of ASD. This approach circumvents the necessity for choosing a single optimal solution, recognizing that the definition of optimality may differ across purposes (e.g., clinical application, research) and methods of adjudication (e.g., fit to data, predictive validity, substantive interpretability); rather, our approach reflects the possibility that, depending on the level of resolution, one may find differing underlying constructs. Therefore, this approach can illustrate how the current, seemingly disparate conceptualizations of ASD symptomatology may instead represent a coherent overarching multi-level meta-structure, providing the field with an integrative conceptual map for unlocking the complexities of ASD. Accordingly, the primary aims of this study were to understand better (1) the structure of ASD symptoms across different levels of resolution, and (2) how the resulting structures can be synthesized into an integrative hierarchy (from lowest to highest resolution), and (3) whether or not the resultant multi-level ASD structure would be stable across informants (i.e., parent- vs. teacher-report data).
Methods
Participants
The study sample comprised 3,825 individuals between 6 and 22 years old (M = 11.35, SD = 3.53) who were consecutive referrals to a university hospital developmental disabilities specialty clinic (DD referrals, n = 1,319) or a child psychiatry outpatient clinic (psychiatry referrals, n = 2,506). (The age range of the study sample is discussed in online supplementary Appendix S1 and the treatment of missing data is discussed in Appendix S2). Case records were screened for individuals who had the prerequisite assessment instruments (see Measures). About two thirds of DD clinic referrals (n = 899; 68%) met DSM-IV clinical criteria for ASD: 300 (23%) received a diagnosis of autistic disorder, 225 (17%) Asperger’s syndrome, and 374 (28%) pervasive developmental disorder, not otherwise specified (PDD-NOS). A subset of the ASD youth in the DD sample are described in prior publications (e.g., Gadow, DeVincent, & Schneider, 2008; Gadow, Perlman, Ramdhany, & de Ruiter, 2016; Lecavalier et al., 2009).
Psychiatry referrals comprised two cohorts, an initial cohort (n = 1,276) for whom diagnostic data were available for most (72%) cases and a second subsequent cohort (n = 1,230) for whom diagnostic data were not available. Additional statistical analyses (i.e., independent groups t-tests and chi-squared tests) indicated that there were no significant differences between the two psychiatric cohorts in terms of age, gender, and ASD symptoms. Among those for whom diagnostic data were available (n = 917), the most common clinic diagnoses were attention-deficit/hyperactivity disorder (ADHD; 77%), learning disabilities (34%), language disorders (23%), oppositional defiant disorder (ODD; 17%), anxiety disorders (12%), major depressive disorder (12%), and social anxiety disorder (11%). Sixteen percent (n = 144) of psychiatry referrals whose diagnostic data were available met DSM-IV clinical criteria for ASD: autistic disorder (n=17, 12%), Asperger’s syndrome 39 (27%), or PDD-NOS (n=88, 61%). A subset of this sample is described in greater detail in prior publications (e.g., Drabick & Gadow, 2012; Gadow & Drabick, 2012; Gadow, Kaat, & Lecavalier, 2013).
Our study sample included both ASD and non-ASD individuals owing to the widespread distribution of ASD symptoms in non-ASD psychiatry referrals and general population samples (Constantino & Todd, 2003; Gadow & Sprafkin, 2002). This study was approved by a university Institutional Review Board.
Measures
The Child and Adolescent Symptom Inventory-4R (CASI-4R)
The CASI-4R (Gadow & Sprafkin, 2009) is a behavioral rating scale assessing various DSM-IV-TR (American Psychiatric Association, 2000) emotional and behavioral symptoms in youth aged 5 through 18 years (as well as up to 22 for those still in school). For each item, informants (parent or teacher) rate youth with a 4-point Likert-type scale ranging from 0 (never) to 3 (very often). This study analyzed the 12 items assessing ASD symptoms; four items for each of three core ASD symptom domain subscales (social deficits, communication deficits, perseverative behaviors). Numerous studies indicate CASI-4R subscales demonstrate satisfactory psychometric properties (Gadow, 2015; Gadow & Sprafkin, 2002, 2008; Gadow, Sprafkin, Salisbury, Schneider, & Loney, 2004; Sprafkin, Gadow, Salisbury, Schneider, & Loney, 2002). Specifically, individual symptom subscales evidence satisfactory internal consistency (Cronbach’s alpha), test-retest reliability, and convergent and divergent validity with respective measures from a range of relevant assessment instruments and diagnostic procedures in community-based normative and clinic-referred samples. The CASI-4R also demonstrates clinical utility with regard to identifying ASD in referred and non-referred youth (DeVincent, Gadow, Strong, Schwartz, & Cuva, 2008; DeVincent & Gadow, 2009). In the present study, CASI-4R ASD items demonstrated good internal consistency (i.e., Cronbach’s alpha ranged between .86 and .89) across different subsamples and reporters.
Procedure
Prior to their initial evaluation, parents of potential patients completed an intake assessment battery that included the CASI-4R and a background information questionnaire. Parents delivered a similar packet of materials to the school with instructions that requested teachers to complete the CASI-4R, and the school to provide copies of psycho-educational and intelligence evaluations. Schools mailed their information directly to the clinic. Parent ratings were completed primarily by the child’s mother (>90%). Intake evaluations included interviews with the children and their caregivers, informal observation of parent-child interaction, and review of the packet materials.
Analyses
Bass-ackwards analysis
Goldberg’s (2006) bass-ackwards method involves sequentially extracting increasing numbers of factors from the data, saving all factor scores, and correlating factor scores of immediately super- and sub-ordinate levels. Thus, we extracted one factor from the 12 ASD items and saved the factor scores; we then extracted two factors from the original data, saved the factor scores, and correlated these factor scores with those from the one-factor solution, and so on. This demonstrates how the first general ASD factor was associated with, and potentially bifurcated into two, separate sub-ordinate factors. We then proceeded by following this procedure for three-factor models and so on.
Although organized in a hierarchy, it is noteworthy that the resulting framework does not imply subordinate/superordinate relationships between latent variables, in the sense of a higher-order factor model; rather each level is a factor solution in itself at differing levels of resolution. Thus, the bass-ackwards method takes an atheoretical approach, rather than choosing any single optimal factor solution. In contrast, higher-order factor analysis takes the opposite approach: A single optimal structure is identified, and correlations among factors are then factor analyzed to produce higher-order factors, eventually yielding a multi-level structure. Thus, higher-order factor analysis is conceptually distinct from our bass-ackwards approach. To clarify ambiguous terminology across these methods, we use the term hierarchy throughout the manuscript to indicate the placement of separate, unique solutions into a single integrated structure that incorporates sequentially extracted ASD symptoms factors at multiple factor levels. For similar reasons, we use the term multi-level to indicate multiple factor solution levels that were sequentially extracted and integrated into an overarching framework, not to imply a multi-level model in the sense of nested random effects analyses.
Although Goldberg (2006) advocated principal components analysis (PCA) for the bass-ackwards method, PCA produces components rather than factors, given that it analyzes variance rather than a reduced correlation matrix of communalities (covariance). As such, following the method of Kim and Eaton (2015), we used exploratory structural equation modeling (ESEM; Asparouhov & Muthén, 2009), which, like factor analysis and unlike PCA, produces interpretable latent factors and allows Mplus to save factor scores. We used the orthogonal Crawford-Ferguson family Factor Parsimony (FACPARSIM) rotation (where κ = 1; for more information, see Browne, 2001; Crawford & Ferguson, 1970). Whereas oblique rotations are typically preferred for factor analytic solutions, the bass-ackwards method requires orthogonal rotation to produce interpretable between-level factor/component scores (Goldberg, 2006; Kim & Eaton, 2015) because factor scores produced by oblique rotations are not likely to produce interpretable between-level factor structural relations. Further, additional analyses using an oblique rotation (geomin) indicated that, although the oblique rotation produced highly similar factor solutions to our orthogonal rotations at the two- and three-factor levels, it produced weakly defined factors beyond the three-factor level, indicating interpretative superiority of our orthogonal rotations in these data.
Analytic strategy
ASD items were treated as continuous variables, with standard errors corrected for non-normality by use of a robust maximum likelihood estimator (MLR). Three fit indices were used to evaluate models: the comparative fit index (CFI), Tucker-Lewis index (TLI), and the root mean square error of approximation (RMSEA). CFI and TLI values > .95, and RMSEA values < .06 indicate good model fit (Hu & Bentler, 1999). Analyses were conducted in Mplus (version 7.11; Muthén and Muthén, 2013).
Results
Structural Hierarchy of ASD Symptoms in Parent-Reports
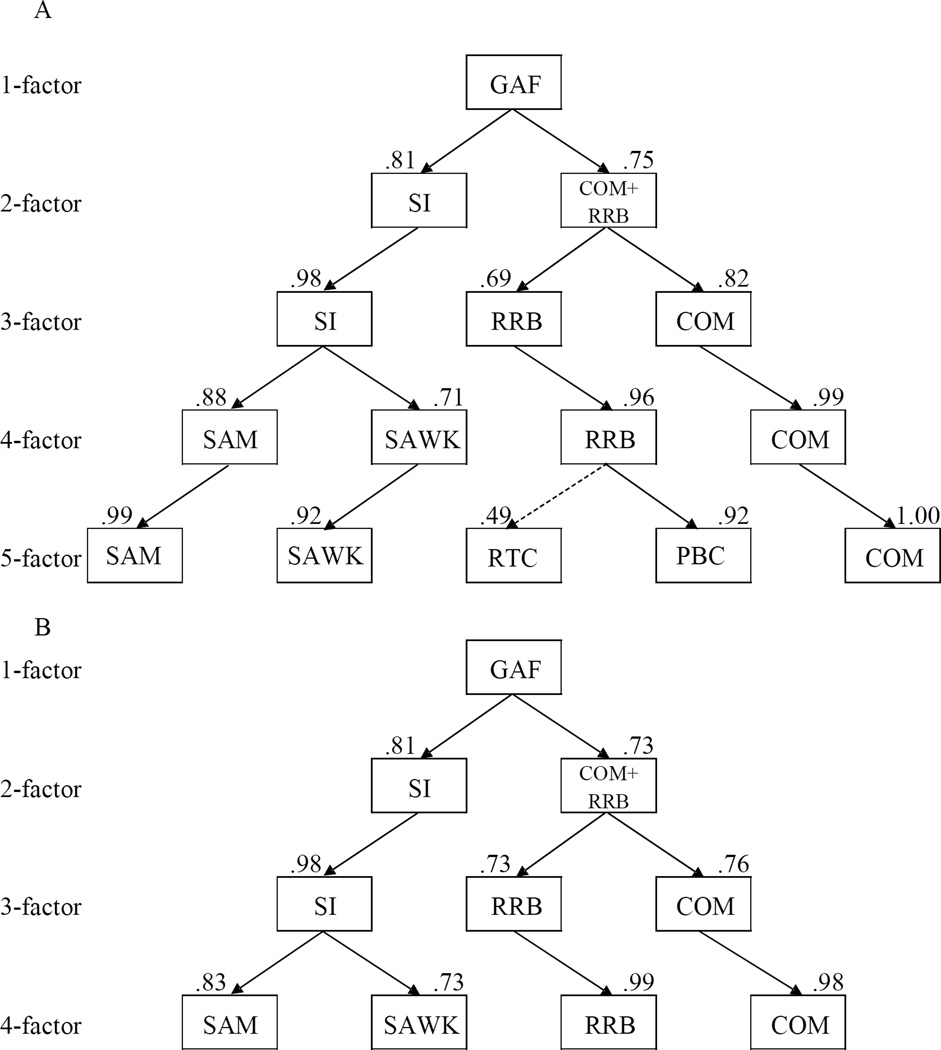
We initially conducted a bass-ackwards analysis of the 12 parent-report CASI-4R ASD items, extracting as many factors as possible. The six-factor solution did not converge successfully, suggesting over-extraction, and thus we used the five-factor solution as a reasonable stopping point. The one- and two-factor solutions showed poor to fair fit with the data, and the three- through five-factor solutions showed good fit (Table 1). The comprehensive bass-ackwards hierarchies of the autism spectrum from parent- and teacher-reports are depicted in Figure 1 and between-level factor correlations across levels of the hierarchy are shown in Table 3.
Table 1.
Model fit indices for one- through five-factor solutions in the parent- and teacher- report data
| Model Fit Indices |
Factor solutions | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Parent-reports |
Teacher-reports |
|||||||||
| 1-factor | 2-factor | 3-factor | 4-factor | 5-factor | 1-factor | 2-factor | 3-factor | 4-factor | 5-factor | |
| RMSEA | 0.086 | 0.067 | 0.047 | 0.029 | 0.020 | 0.111 | 0.092 | 0.061 | 0.041 | |
| CFI | 0.879 | 0.943 | 0.978 | 0.994 | 0.998 | 0.835 | 0.909 | 0.969 | 0.990 | N/A |
| TLI | 0.852 | 0.912 | 0.955 | 0.983 | 0.992 | 0.798 | 0.860 | 0.939 | 0.972 | |
Note. Exploratory structural equation modeling was conducted with a robust maximum likelihood estimator and Crawford-Ferguson family FACPARSIM rotation. RMSEA: root mean squared error of approximation; CFI: comparative fit index; TLI: Tucker-Lewis index; Five-factor solution in teacher-reports did not converge.
Figure 1.
The bass-ackwards hierarchy of autism spectrum disorder symptoms in (A) parent-reports and (B) teacher-reports data. The five-factor solution in teacher-reports failed to converge (See Appendix S3). Primary between-level factor correlations (r > .6) among factors are depicted with solid lines. Moderate associations between a factor and its primary super-ordinate factor (r < .6) are depicted in dashed lines. GAF, general autism spectrum disorder factor; SI, social interaction; COM, communication; RRB, restricted repetitive behavior; SAM, social amotivation; SAWK, social awkwardness; RTC, resistance to change; PBC, perseverative behaviors and cognitions.
Table 3.
Between-level correlations of factors in parent- and teacher-report data
| Level | Parent-reports | Teacher-report | |||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | GAF | GAF | |||||||
| 2 | SI | .81 | SI | .81 | |||||
| 2 | COM+RRB | .75 | COM+RRB | .73 | |||||
| 2 | SI | COM+RRB | SI | COM+RRB | |||||
| 3 | SI | .98 | .06 | SI | .98 | .02† | |||
| 3 | COM | .22 | .82 | COM | .23 | .76 | |||
| 3 | RRB | .35 | .69 | RRB | .26 | .73 | |||
| 3 | SI | COM | RRB | SI | COM | RRB | |||
| 4 | SAM | .88 | .17 | .15 | SAM | .83 | .13 | .17 | |
| 4 | COM | .03† | .99 | .15 | COM | .04 | .98 | .15 | |
| 4 | SAWK | .71 | .24 | .44 | SAWK | .73 | .30 | .26 | |
| 4 | RRB | .02† | .21 | .96 | RRB | .00† | .11 | .99 | |
| 4 | SAM | COM | SAWK | RRB | N/A | ||||
| 5 | SAM | .99 | .09 | .24 | .07 | ||||
| 5 | SAWK | .42 | .23 | .92 | .03* | ||||
| 5 | COM | .05 | 1.00 | .12 | .13 | ||||
| 5 | RTC | .11 | .03* | .46 | .49 | ||||
| 5 | PBC | .11 | .25 | .12 | .92 | ||||
Note. All correlations are significant at **p < .01, except
(significant at *p < .05) and
(nonsignificant).
Between-level factor correlations greater than .40 were bolded. GAF, general autism spectrum disorder factor; SI, social interaction; COM, communication; RRB, restricted repetitive behavior; SAM, social amotivation; SAWK, social awkwardness; RTC, resistance to change; PBC, perseverative behaviors and cognitions.
At the highest level of the hierarchy, all ASD items loaded well on the first factor, an undifferentiated general ASD factor, with standardized loadings ranging from .55 to .80 (Table 2). This general ASD factor then bifurcated into (1) a social interaction (SI) factor and (2) a factor that combined communication problems (COM) and social-communication deficits and restricted and repetitive behaviors (RRB) factor at the two-factor solution level. The SI factor and the combined COM+RRB factor were both significantly correlated with the super-ordinate general ASD factor.
Table 2.
Standardized factor loadings for one- through five-factor solutions in the parent- and teacher-report data
| aItems | Factor loadings | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Parent-reports | |||||||||||||||
| 1-factor | 2-factor | 3-factor | 4-factor | 5-factor | |||||||||||
| 1 | 1 | 2 | 1 | 2 | 3 | 1 | 2 | 3 | 4 | 1 | 2 | 3 | 4 | 5 | |
| Peculiar way of relating to others | .74 | .66 | .37 | .59 | .31 | .35 | .46 | .24 | .49 | .25 | .41 | .48 | .20 | .27 | .23 |
| Does not play well with others | .78 | .82 | .30 | .76 | .29 | .31 | .61 | .21 | .54 | .20 | .56 | .56 | .16 | .25 | .20 |
| Not interested in making friends | .65 | .62 | .29 | .57 | .30 | .25 | .66 | .23 | .20 | .22 | .65 | .22 | .21 | .19 | .20 |
| Unaware of other people’s feelings | .62 | .61 | .25 | .56 | .24 | .25 | .54 | .18 | .31 | .19 | .52 | .30 | .16 | .24 | .15 |
| Significant problem with language | .63 | .28 | .63 | .18 | .82 | .16 | .20 | .75 | .21 | .17 | .19 | .23 | .73 | .14 | .18 |
| Difficulty making socially appropriate conversation |
.80 | .59 | .54 | .52 | .52 | .34 | .32 | .47 | .61 | .20 | .25 | .63 | .42 | .26 | .21 |
| Talks in a strange way | .65 | .22 | .74 | .14 | .61 | .42 | .12 | .58 | .26 | .38 | .10 | .23 | .56 | .25 | .36 |
| Unable to pretend when playing | .59 | .29 | .57 | .20 | .46 | .38 | .27 | .44 | .14 | .37 | .26 | .14 | .42 | .18 | .37 |
| Excessive preocculation with one topic | .64 | .42 | .48 | .31 | .23 | .59 | .14 | .15 | .51 | .50 | .12 | .39 | .13 | .39 | .41 |
| Upset over small changes in routine | .57 | .40 | .41 | .30 | .20 | .50 | .19 | .14 | .40 | .42 | .14 | .15 | .12 | .87 | .16 |
| Makes strange repetitive movements | .58 | .30 | .54 | .17 | .30 | .58 | .20 | .26 | .21 | .55 | .16 | .20 | .22 | .23 | .56 |
| Strange fascination for parts of objects | .55 | .26 | .52 | .13 | .26 | .60 | .19 | .23 | .15 | .61 | .16 | .12 | .18 | .22 | .63 |
| Teacher-reports | |||||||||||||||
| 1-factor | 2-factor | 3-factor | 4-factor | 5-factor | |||||||||||
| 1 | 1 | 2 | 1 | 2 | 3 | 1 | 3 | 2 | 4 | 1 | 2 | 3 | 4 | 5 | |
| Peculiar way of relating to others | .78 | .64 | .44 | .57 | .32 | .42 | .42 | .23 | .52 | .33 | N/A | ||||
| Does not play well with others | .79 | .85 | .27 | .79 | .28 | .29 | .59 | .16 | .59 | .19 | |||||
| Not interested in making friends | .70 | .69 | .29 | .63 | .31 | .25 | .75 | .24 | .26 | .16 | |||||
| Unaware of other people’s feelings | .70 | .70 | .26 | .65 | .26 | .27 | .58 | .16 | .43 | .18 | |||||
| Significant problem with language | .61 | .28 | .61 | .14 | .84 | .14 | .14 | .76 | .27 | .12 | |||||
| Difficulty making socially appropriate conversation |
.82 | .64 | .51 | .56 | .55 | .29 | .32 | .46 | .66 | .17 | |||||
| Talks in a strange way | .67 | .28 | .71 | .19 | .57 | .44 | .18 | .54 | .28 | .39 | |||||
| Unable to pretend when playing | .60 | .28 | .61 | .19 | .59 | .30 | .30 | .61 | .11 | .26 | |||||
| Excessive preocculation with one topic | .61 | .36 | .51 | .26 | .20 | .62 | .12 | .13 | .43 | .59 | |||||
| Upset over small changes in routine | .60 | .37 | .48 | .27 | .22 | .58 | .21 | .16 | .33 | .54 | |||||
| Makes strange repetitive movements | .59 | .26 | .61 | .15 | .32 | .62 | .22 | .32 | .16 | .58 | |||||
| Strange fascination for parts of objects | .52 | .23 | .53 | .12 | .23 | .61 | .22 | .23 | .10 | .59 | |||||
Note. Exploratory structural equation modeling was conducted with a maximum likelihood estimator and Crawford-Ferguson family FACPARSIM rotation. Five-factor solution in teacher-reports did not converge.
Truncated versions of CASI-4R items.
In the three-factor solution, the SI factor remained the same (i.e. correlated with the two-factor solution’s SI factor at r = .98), and the two-factor level’s COM+RRB factor split into separate COM and RRB factors.
In the four-factor solution, the three-factor level’s SI factor split into a social amotivation (SAM) factor and a social awkwardness (SAWK) factor. The SAM and SAWK factors were highly correlated with their super-ordinate SI factor. The four-factor level’s SAWK factor was also moderately correlated with the three-factor level’s RRB factor, whereas the separate COM and RRB factors were correlated almost at unity across three- and four-factor levels.
In the five-factor solution, the four-factor level’s RRB factor bifurcated into a resistance to change (RTC) factor and a perseverative behaviors and cognitions (PBC) factor, defined by strange repetitive movements and fascination with parts of objects. This PBC factor was almost perfectly correlated with its super-ordinate RRB factor. The RTC showed only moderate correlation with the four-factor level’s RRB factor, and it was also moderately correlated with four-factor solution SAWK factor. The five-factor level’s SAWK factor was strongly correlated with the four-factor level’s SAWK factor and also moderately correlated with the four-factor level’s SAM factor. The SAM and COM factors were almost perfectly correlated across four-and five-factor levels.
Structural Hierarchy of ASD Symptoms in Teacher-Reports
We conducted another bass-ackwards analysis of the teacher-reports to examine whether the structural hierarchy of the parent-report data was comparable. We report results up through the four-factor solution, because the five-factor solution failed to converge (see Appendix S3 for more information). The factor loadings for all teacher-report items are given in Table 2. (Model fit index values for one- through four-factor solutions are shown in Table 1.) The comprehensive bass-ackwards hierarchy of the autism spectrum from teacher-reports is depicted in Figure 1.
Results indicated that the bass-ackwards analysis for teacher-reports yielded comparable findings to those from parent-reports in that (1) the factors with the same interpretations emerged at each level; (2) patterns associations among factors between levels were highly similar (Figure 1); and (3) the magnitude of these between-level factor correlations in the ASD hierarchy was also highly similar. Considering our large sample size and resulting statistical power, even trivial differences between correlations (e.g., a difference of .02 between correlations) would be statistically significant using Fisher’s r-to-z test. Thus, to compare correlations among factors between parent- and teacher-report data, we adopted a conservative benchmark of a difference of < .1 between correlations (i.e., a difference of r2 of 1%) as indicating a meaningful difference between the correlations. Result indicated that all correlations between factors compared between parent- and teacher-report data differed by < .1.
Discussion
This is the first study to examine an underlying structural hierarchy of ASD symptomatology using the bass-ackwards method. Overall, results indicate that the symptom structure of ASD may be meaningfully interpreted across different levels of resolution and can be integrated into a single, overarching hierarchy (Figure 1). Further, findings suggest that this hierarchy of ASD symptomatology is generalizable across contexts (i.e., consistent for both parent- and teacher-report data).
Interpreting the Structure of ASD Symptom Hierarchy
Our findings suggest an interpretable hierarchy that emerges in both parent- and teacher-report data. The parent-report data yielded five levels of factor solutions with levels 1–4 substantively replicated using teacher-report data. This hierarchy produced key features of many existing models of ASD. At the first level of the hierarchy, the overall ASD spectrum may be understood with a single general ASD factor, congruent with previous finding of a single underlying factor that is continuously distributed and even extends into the non-ASD population (i.e., a so-called broader autism phenotype) (Constantino et al., 2004; Dawson et al., 2002). This view has practical implications. For instance, many interventions identify reduction in general ASD symptomatology as their primary target (e.g., Dawson et al., 2010). However, because subsequent factor solutions fit the data more optimally, a single cluster of symptoms may not be the best way to represent the underlying structure of ASD symptoms for all purposes —it can be empirically deconstructed in ways coherent with other interpretations. Further, delineating sub-constructs may provide individualized and more specific treatment targets for future intervention research.
At the second level of the hierarchy, the general ASD factor bifurcates into an SI factor and combined COM+RRB factor. This solution differs from the two-factor solution reflective of the DSM-5 criteria, which incorporates communication and social interaction deficits into a single factor (American Psychiatric Association, 2013; Mandy et al., 2012; Snow et al., 2009). Our findings suggest that the social production of language (e.g., engaging in socially appropriate conversation) cross-loaded onto both the SI and combined COM+RRB factors, whereas other symptoms associated with communication deficits (e.g., language difficulties and speaking in an odd way) primarily loaded onto the combined COM+RRB factor. This subtle distinction converges with previous literature indicating that different types of communication deficits may be differentially related to restricted and repetitive behavior versus social interaction symptoms (Tager-Flusberg, 2006). Additionally, whereas some of the items included in the COM+RRB factor suggests the construct represents communication broadly, many of these items in fact represent language-specific features characteristic of ASD. Future studies considering replication of these factors should therefore examine the relationship between this factor and spoken language ability. Thus, the DSM-5 two-factor solution for ASD may in fact obfuscate this subtlety by grouping all communication deficit symptoms under the rubric of social deficits.
At the three-factor level, the SI factor remains the same, whereas the combined COM+RRB factor split into separate COM and RRB factors. This result is not only consistent with DSM-IV criteria for ASD (American Psychiatric Association, 2000), but it is also in agreement with our prior findings using a more conventional factor-analytic strategy (Lecavalier et al., 2009). The emergence of separate COM and RRB factors is also important clinically as it underscores the long recognized significance of atypical communication characteristics in the earliest formulations of what we now refer to as the ASD clinical phenotype (Hippler, Viding, Klicpera, & Happé, 2010; Kanner, 1944) and highlights the ongoing importance of studying communication in ASD research.
At the four-factor level of the hierarchy, the separate COM and RRB factors remained the same, whereas the SI factor bifurcated into a SAM and a SAWK factor. The characteristics of the SAWK factor (e.g. difficulty engaging in socially appropriate conversation and preoccupation with certain topics) are consistent with extant literature emphasizing the role of reciprocal communication difficulties in ASD (Losh & Piven, 2007; Wing, 1997). The symptoms that load primarily onto the SAM factor are characterized by a lack of interest in making friends and lack of interest in or awareness of other people’s feelings. These symptoms are also characteristic of schizoid and schizotypal personality disorders (American Psychiatric Association, 2013), which have previously been found to be important phenotypic characteristics of a subgroup of youth with ASD (Gadow, 2013). Though some recent research highlights social motivation deficits as an important feature of ASD (Chevallier et al., 2012; Kohls, Chevallier, Troiani, & Schultz, 2012), it is worth noting that our findings not only reveal the presence of separate SAM and SAWK factors, but also place them into a comprehensive hierarchy, thus providing valuable understanding of how the factors are associated with other core features of ASD. Further, the distinction between social skills (SAWK) and social amotivation (SAM informs how social functioning deficits at lower levels of functioning in ASD might be stratified. This distinction is particularly meaningful in the context of interventions that aim to target either social skills via didactic training or SAM through more naturalistic methods (Lerner, White, & McPartland, 2012; McMahon, Lerner, & Britton, 2013).
Finally, at the five-factor level, the RRB factor split into a RTC and a PBC factor. The RTC factor was represented by distress at small changes in routine or environment, whereas the PBC factor was characterized by conventional restricted and repetitive behaviors such as preoccupation with certain topics, odd repetitive movements, and intense interest in parts of objects. The PBC factor almost perfectly correlated with the four-factor level RRB, whereas the RTC factor only moderately correlated with the separate RRB and SAWK factors. The moderate correlations among those three factors demonstrates that RTC features are not only associated with the presence of RRB, but are also related to difficulties engaging in skilled SI. The emergence of two sub-factors related to the broader RRB factor is consistent with recent research indicating subtypes of RRBs, particularly those that distinguish insistence on sameness and circumscribed interests (Bishop et al., 2013; Lam, Bodfish, & Piven, 2008; Leekam, Prior, & Uljarevic, 2011). In fact, certain subtypes of RRBs appear to be more familial than others (Lam et al., 2008). Researchers have also found evidence suggesting there are different genetic association patterns for the insistence on sameness subtype (similar to RTC) as compared to other subtypes of RRBs (Tao et al., 2016). Indeed, previous research using a traditional factor analytic approach has shown differential associations between ASD symptom factors and genetic loci (Liu et al., 2011). Building on that approach by linking genetic loci to the structural hierarchy derived via the bass-ackwards method could potentially yield a richer picture of the associations between genotypic and phenotypic aspects of ASD. Taken together these findings support the importance of distinguishing between subtypes of RRBs.
Strengths, Limitations, and Future Directions
The present study has a number of strengths: use of a large sample of clinically referred youth, a well-validated measure of ASD symptoms, and a heterogeneous sample of school-eligible, clinic-referred youth. Furthermore, the inclusion of a balanced sample of individuals with and without ASD represents a truly (multi-)dimensional approach to understanding how ASD symptomatology is distributed across psychiatric diagnoses. Therefore, the ASD symptom hierarchy identified here reflects how symptoms are grouped and bifurcate across levels of severity. Nonetheless, the current study possesses some limitations. Symptom data were collected from a single questionnaire, although for both parent- and teacher-report. Collecting data from multiple methods and sources (e.g., semi-structured interviews, behavioral observations from trained observers) would provide a more comprehensive symptom picture of each participant. Further, data were obtained for ASD symptoms defined in DSM-IV; future research should consider whether a similar hierarchy emerges when examining a broader range of ASD behavioral characteristics, which have proven useful in studies differentiating ASD and non-ASD samples (Kohls et al., 2012; Tager-Flusberg, 2006). Also, caution is needed when interpreting the results of one- and two-factor solutions, given the relatively poor model fits of those solutions; they should not be interpreted individually as wholly adequate representations of the data but instead considered in the context of an ASD symptom hierarchy. Lastly, we included only 12 ASD subscale items from the CASI-4R in our analyses. The inclusion of more ASD symptom items, particularly those composing the RTC factor, may yield additional symptom factors and thus provide a more comprehensive picture of ASD symptomatology.
Supplementary Material
Key points.
Fundamental questions regarding the symptom structure and true heterogeneity of the ASD clinical phenotype remain unresolved.
Our results from bass-ackwards analyses indicate that the latent structure of ASD symptoms produces an interpretable hierarchy at various levels of resolution and across multiple informants.
The core symptom dimensions of ASD are composed of various subdomains of cognitive and behavioral dysfunctions.
Our findings suggest a model for integrating the divergent theories of cognitive processes and behavioral features that define the disorder.
The reported hierarchy of ASD symptoms suggests a strategy for clinical assessment that includes aspects of both formal nosologies as well as more precise evaluation of component deficits that can be used to formulate personalized intervention.
Acknowledgments
This study was supported, in part, by the Matt and Debra Cody Center for Autism and Developmental Disabilities. M. D. L. received support from NIMH grant R01MH110585 and the Simons Foundation Autism Research Initiative (SFARI# 381283), during the course of this project. K.D.G. is shareholder in Checkmate Plus, publisher of the Child and Adolescent Symptom Inventory-4R. All the other authors have declared they have no potential or competing conflicts of interest in relation to this paper. The authors would like to thank the study participants and their families.
Footnotes
Conflicts of interest statement: See Acknowledgements for disclosures.
Supporting information
Additional supporting information may be found in the online version of this article:
Table S1. Study sample characteristics
Appendix S1. Age range of the study sample
Appendix S2. Missing data, sensitivity analysis, and analytic sample
Appendix S3. Convergence failure of five-factor model in teacher-report data
References
- Asparouhov T, Muthén B. Exploratory structural equation modeling. Structural equation modeling: a multidisciplinary journal. 2009;16(3):397–438. [Google Scholar]
- American Psychiatric Association. DSM-III-R: Diagnostic and statistical manual of mental disorders. American Psychiatric Association; 1980. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual-text revision (DSM-IV-TRim, 2000) American Psychiatric Association; 2000. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. Arlington: American Psychiatric Publishing; 2013. [Google Scholar]
- Baron-Cohen S, Leslie AM, Frith U. Does the autistic child have a “theory of mind”? Cognition. 1985;21(1):37–46. doi: 10.1016/0010-0277(85)90022-8. [DOI] [PubMed] [Google Scholar]
- Bishop SL, Hus V, Duncan A, Huerta M, Gotham K, Pickles A, Lord C. Subcategories of restricted and repetitive behaviors in children with autism spectrum disorders. Journal of autism and developmental disorders. 2013;43(6):1287–1297. doi: 10.1007/s10803-012-1671-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW. An overview of analytic rotation in exploratory factor analysis. Multivariate Behavioral Research. 2001;36(1):111–150. [Google Scholar]
- Chevallier C, Kohls G, Troiani V, Brodkin ES, Schultz RT. The social motivation theory of autism. Trends in cognitive sciences. 2012;16(4):231–239. doi: 10.1016/j.tics.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino JN, Gruber CP, Davis S, Hayes S, Passanante N, Przybeck T. The factor structure of autistic traits. Journal of Child Psychology and Psychiatry. 2004;45(4):719–726. doi: 10.1111/j.1469-7610.2004.00266.x. [DOI] [PubMed] [Google Scholar]
- Constantino JN, Todd RD. Autistic traits in the general population: a twin study. Archives of general psychiatry. 2003;60(5):524–530. doi: 10.1001/archpsyc.60.5.524. [DOI] [PubMed] [Google Scholar]
- Crawford CB, Ferguson GA. A general rotation criterion and its use in orthogonal rotation. Psychometrika. 1970;35(3):321–332. [Google Scholar]
- Dawson G, Rogers S, Munson J, Smith M, Winter J, Greenson J, Varley J. Randomized, controlled trial of an intervention for toddlers with autism: the Early Start Denver Model. Pediatrics. 2010;125(1):e17–e23. doi: 10.1542/peds.2009-0958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson G, Webb S, Schellenberg GD, Dager S, Friedman S, Aylward E, Richards T. Defining the broader phenotype of autism: Genetic, brain, and behavioral perspectives. Development and psychopathology. 2002;14(03):581–611. doi: 10.1017/s0954579402003103. [DOI] [PubMed] [Google Scholar]
- DeVincent C, Gadow KD, Strong G, Schwartz J, Cuva S. Screening for autism spectrum disorder with the Early Childhood Inventory-4. Journal of Developmental & Behavioral Pediatrics. 2008;29(1):1–10. doi: 10.1097/DBP.0b013e3181468c32. [DOI] [PubMed] [Google Scholar]
- DeVincent CJ, Gadow KD. Relative clinical utility of three child symptom inventory-4 scoring algorithms for differentiating children with autism spectrum disorder vs. attention-deficit hyperactivity disorder. Autism Research. 2009;2(6):312–321. doi: 10.1002/aur.106. [DOI] [PubMed] [Google Scholar]
- Drabick DA, Gadow KD. Deconstructing oppositional defiant disorder: clinic-based evidence for an anger/irritability phenotype. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(4):384–393. doi: 10.1016/j.jaac.2012.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duku E, Szatmari P, Vaillancourt T, Georgiades S, Thompson A, Liu XQ, Bennett T. Measurement equivalence of the autism symptom phenotype in children and youth. Journal of Child Psychology and Psychiatry. 2013;54(12):1346–1355. doi: 10.1111/jcpp.12103. [DOI] [PubMed] [Google Scholar]
- Gadow KD. Association of schizophrenia spectrum and autism spectrum disorder (ASD) symptoms in children with ASD and clinic controls. Research in developmental disabilities. 2013;34(4):1289–1299. doi: 10.1016/j.ridd.2013.01.011. [DOI] [PubMed] [Google Scholar]
- Gadow KD. The Symptom Inventories: An annotated bibliography. Stony Brook, NY: Checkmate Plus; 2015. Available from www.checkmateplus.com. [Google Scholar]
- Gadow KD, DeVincent C, Schneider J. Predictors of psychiatric symptoms in children with an autism spectrum disorder. Journal of autism and developmental Disorders. 2008;38(9):1710–1720. doi: 10.1007/s10803-008-0556-8. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Drabick DA. Anger and irritability symptoms among youth with ODD: Cross-informant versus source-exclusive syndromes. Journal of abnormal child psychology. 2012;40(7):1073–1085. doi: 10.1007/s10802-012-9637-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gadow KD, Kaat AJ, Lecavalier L. Relation of symptom-induced impairment with other illness parameters in clinic-referred youth. Journal of Child Psychology and Psychiatry. 2013;54(11):1198–1207. doi: 10.1111/jcpp.12077. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Perlman G, Ramdhany L, de Ruiter J. Clinical Correlates of Co-occurring Psychiatric and Autism Spectrum Disorder (ASD) Symptom-Induced Impairment in Children with ASD. Journal of abnormal child psychology. 2016;44(1):129–139. doi: 10.1007/s10802-015-9979-9. [DOI] [PubMed] [Google Scholar]
- Gadow KD, Sprafkin J. Child Symptom Inventory-4 screening and norms manual. Stony Brook, NY: Checkmate Plus; 2002. [Google Scholar]
- Gadow KD, Sprafkin J. Adolescent Symptom Inventory-4 screening and norms manual. Stony Brook, NY: Checkmate Plus; 2008. [Google Scholar]
- Gadow KD, Sprafkin J, Salisbury H, Schneider J, Loney J. Further validity evidence for the teacher version of the Child Symptom Inventory-4. School Psychology Quarterly. 2004;19:50–71. [Google Scholar]
- Goldberg LR. Doing it all bass-ackwards: The development of hierarchical factor structures from the top down. Journal of Research in Personality. 2006;40(4):347–358. [Google Scholar]
- Happé F. Criteria, categories, and continua: autism and related disorders in DSM-5. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(6):540–542. doi: 10.1016/j.jaac.2011.03.015. [DOI] [PubMed] [Google Scholar]
- Hippler K, Viding E, Klicpera C, Happé F. Brief report: No increase in criminal convictions in Hans Asperger’s original cohort. Journal of autism and developmental disorders. 2010;40(6):774–780. doi: 10.1007/s10803-009-0917-y. [DOI] [PubMed] [Google Scholar]
- Hu Lt, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural equation modeling: a multidisciplinary journal. 1999;6(1):1–55. [Google Scholar]
- Kanner L. Early infantile autism. The Journal of Pediatrics. 1944;25(3):211–217. [Google Scholar]
- Kim H, Eaton NR. The hierarchical structure of common mental disorders: Connecting multiple levels of comorbidity, bifactor models, and predictive validity. Journal of abnormal psychology. 2015;124(4):1064. doi: 10.1037/abn0000113. [DOI] [PubMed] [Google Scholar]
- Kohls G, Chevallier C, Troiani V, Schultz RT. Social ‘wanting’dysfunction in autism: neurobiological underpinnings and treatment implications. Journal of Neurodevelopmental Disorders. 2012;4(1):1. doi: 10.1186/1866-1955-4-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lam KS, Bodfish JW, Piven J. Evidence for three subtypes of repetitive behavior in autism that differ in familiality and association with other symptoms. Journal of Child Psychology and Psychiatry. 2008;49(11):1193–1200. doi: 10.1111/j.1469-7610.2008.01944.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecavalier L, Aman MG, Scahill L, McDougle CJ, McCracken JT, Vitiello B, Loftin RL. Validity of the autism diagnostic interview-revised. American Journal on Mental Retardation. 2006;111(3):199–215. doi: 10.1352/0895-8017(2006)111[199:VOTADI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Gadow KD, DeVincent CJ, Houts C, Edwards MC. Deconstructing the PDD clinical phenotype: internal validity of the DSM-IV. Journal of Child Psychology and Psychiatry. 2009;50(10):1246–1254. doi: 10.1111/j.1469-7610.2009.02104.x. [DOI] [PubMed] [Google Scholar]
- Leekam SR, Prior MR, Uljarevic M. Restricted and repetitive behaviors in autism spectrum disorders: a review of research in the last decade. Psychological bulletin. 2011;137(4):562. doi: 10.1037/a0023341. [DOI] [PubMed] [Google Scholar]
- Lerner M, White S, McPartland J. Mechanisms of change in psychosocial interventions for autism spectrum disorders. Dialogues in clinical neuroscience. 2012;14(3):307. doi: 10.31887/DCNS.2012.14.3/mlerner. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu XQ, Georgiades S, Duku E, Thompson A, Devlin B, Cook EH, Szatmari P. Identification of genetic loci underlying the phenotypic constructs of autism spectrum disorders. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(7):687–696. doi: 10.1016/j.jaac.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losh M, Piven J. Social-cognition and the broad autism phenotype: identifying genetically meaningful phenotypes. Journal of Child Psychology and Psychiatry. 2007;48(1):105–112. doi: 10.1111/j.1469-7610.2006.01594.x. [DOI] [PubMed] [Google Scholar]
- Mandy WP, Charman T, Skuse DH. Testing the construct validity of proposed criteria for DSM-5 autism spectrum disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2012;51(1):41–50. doi: 10.1016/j.jaac.2011.10.013. [DOI] [PubMed] [Google Scholar]
- Mazefsky CA, Herrington J, Siegel M, Scarpa A, Maddox BB, Scahill L, White SW. The role of emotion regulation in autism spectrum disorder. Journal of the American Academy of Child & Adolescent Psychiatry. 2013;52(7):679–688. doi: 10.1016/j.jaac.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon CM, Lerner MD, Britton N. Group-based social skills interventions for adolescents with higher-functioning autism spectrum disorder: a review and looking to the future. Adolescent health, medicine and therapeutics. 2013;4(23):9. doi: 10.2147/AHMT.S25402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L, Muthén B. Mplus: Statistical analysis with latent variables (Version 7.11)[Software] Muthén & Muthén; Los Angeles: 2013. [Google Scholar]
- Snow AV, Lecavalier L, Houts C. The structure of the Autism Diagnostic Interview-Revised: diagnostic and phenotypic implications. Journal of Child Psychology and Psychiatry. 2009;50(6):734–742. doi: 10.1111/j.1469-7610.2008.02018.x. [DOI] [PubMed] [Google Scholar]
- Sprafkin J, Gadow KD, Salisbury H, Schneider J, Loney J. Further evidence of reliability and validity of the Child Symptom Inventory-4: Parent Checklist in clinically referred boys. Journal of Clinical Child and Adolescent Psychology. 2002;31:513–524. doi: 10.1207/S15374424JCCP3104_10. [DOI] [PubMed] [Google Scholar]
- Tager-Flusberg H. Defining language phenotypes in autism. Clinical Neuroscience Research. 2006;6(3):219–224. [Google Scholar]
- Tao Y, Gao H, Ackerman B, Guo W, Saffen D, Shugart YY. Evidence for contribution of common genetic variants within chromosome 8p21. 2-8p21. 1 to restricted and repetitive behaviors in autism spectrum disorders. BMC genomics. 2016;17(1):1. doi: 10.1186/s12864-016-2475-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkmar FR, McPartland JC. From Kanner to DSM-5: autism as an evolving diagnostic concept. Annual review of clinical psychology. 2014;10:193–212. doi: 10.1146/annurev-clinpsy-032813-153710. [DOI] [PubMed] [Google Scholar]
- Wing L. The autistic spectrum. The lancet. 1997;350(9093):1761–1766. doi: 10.1016/S0140-6736(97)09218-0. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines. Geneva: 1992. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.