Abstract
The last two decades have witnessed dramatic increases in obesity and family instability. To the extent that the social stigma of obesity is a risk factor and family instability represents the potential compromise of important protective factors, their convergence may disrupt socioemotional health, especially during periods of heightened social uncertainty. Drawing on data from the National Longitudinal Study of Adolescent Health, this study found that obese youth at the start of high school had higher levels of internalizing symptoms and lower levels of perceived social integration in school only when they had also experienced multiple family transitions since birth. This pattern, however, did not hold for boys, and it did not extend to overweight (as opposed to obese) adolescents of either gender.
Keywords: Emotional health, Family instability, Obesity, Schools, Social integration
1. Introduction
A central tenet of the life course paradigm is that macro-level trends are “lived” on the micro level. In other words, individual trajectories are shaped by and, collectively, contribute to population dynamics. Indeed, the experiences of children and adolescents in the daily settings of their lives offer a valuable window into the significance of dramatic changes in the American population (Hogan and Goldscheider, 2002; Elder, 1998). In recent decades, two striking population trends have generated a great deal of concern and, in response, major public health and social policy initiatives. These two trends—increasing rates of obesity and family instability—are rarely connected in public discussions or scientific research. Yet, the implications of both for the socioemotional health of young people in the U.S. suggest that their convergence could be particularly problematic for both individuals and society.
As background, rates of obesity among American youth have been rising over the last twenty years while, simultaneously, changes in adult marriage, divorce, and cohabitation patterns have resulted in an increase in the number of family arrangements that young people live in before entering adulthood (National Institute of Diabetes and Digestive and Kidney Diseases, 2009; McLanahan, 2004). Both trends have socioemotional implications for youth, which is notable given that navigating social relations, building networks of social support, and developing positive identities contribute to lifelong health and socioeconomic attainment (Giordano, 2003). Despite the rising prevalence of obesity, the long-standing stigma attached to obesity in American youth culture has not weakened, which means that obese youth are at heightened risk for social exclusion (Crosnoe et al., 2008; Crandall, 1994). At the same time, higher levels of family instability can disrupt young people’s development of relationship templates and senses of self in ways that put them at a disadvantage in social markets (Cavanagh and Huston, 2008). If the stigma of obesity reduces access to supportive and socializing peer relations on the “demand” side and family instability interferes with such access on the “supply” side, then the growing numbers of youth who are obese and come from unstable homes likely represent a segment of the American population in need of attention. In this way, family instability may be a family magnifier of the socioemotional risks of obesity. Such magnification likely plays out in school, a primary channel in socioeconomic attainment that doubles as a site of peer culture, and could indeed be more pronounced during periods of school in which young people are especially vulnerable socioemotionally (Crosnoe, 2011).
This study, therefore, draws on the National Longitudinal Study of Adolescent Health (Add Health) to examine whether body size and family structure histories interact to predict socioemotional health in the first years of high school. Results will illuminate the intersection of family and peer contexts in the socioemotional problems of overweight youth that, in turn, could magnify the social, public, and economic health costs of rising obesity rates.
2. Obesity and family structure trends
Today, about one-third of children and adolescents in the U.S. are obese or overweight. These numbers, which are higher among race/ethnic minorities, represent as much as a threefold increase from two decades ago, with the vast majority of increase occurring in the 1990s (Ogden et al., 2010, 2008). Such trends reflect multiple macro-level economic and social changes, including technological change (Lakdawalla and Philipson, 2009), and they are related to adolescent mortality, lifelong weight and health problems, and a range of socioeconomic and behavioral outcomes across the life course (Kalist and Siahaan, 2012; Koch, 2011; Cawley and Spiess, 2010; Freedman et al., 2007; Loh, 1993; Serdula et al., 1993).
During the same period, American youth were also undergoing dramatic changes in their family situations (Cherlin, 2009). The combination of increasing non-marital fertility, divorce, and cohabitation rates and declining marriage rates means that many children live in family structures other than those with two married parents at any given time. Moreover, the majority of children will spend some time prior to adulthood in these “alternative” family structures (Bumpass and Lu, 2000). Perhaps even more importantly, young people who have experienced one family structure transition in their lives are at significantly greater risk for experiencing subsequent transitions. For example, recent estimates indicate that as many as one-fifth of American adolescents have experienced two or more family structure transitions since birth (Cavanagh, 2008; Wu and Martinson, 1993). Again, all of this family change has led to often contentious public debates and major federal and state policy initiatives (Furstenberg, 2007).
2.1. Implications of obesity and family trends
Both of these population trends are meaningful for understanding multiple domains of youth wellbeing. One such domain is socioemotional development, particularly in the context of the schools that serve as primary sites of social relations in the early life course (Crosnoe, 2011). Socioemotional development—how young people gain awareness of social life and their place in it, how they negotiate tensions between self and other—is important in its own rite but also because it factors into health and educational attainment (Giordano, 2003; Hartup and Stevens, 1997). This role of socioemotional development in other life trajectories serves as one way that that body size and family instability in the short term can translate into long-term consequences for the life course.
Beginning with the socioemotional implications of body size, large bodies have long been stigmatized in American society, including American youth culture. In general, overweight youth are more likely to be seen as physically unattractive, undesirable as friends and romantic partners, and less competent, interesting, and likable (Brownell et al., 2005; Crandall, 1994). According to theoretical perspectives on social stigma, being stigmatized by aspects of physical appearance can lead to a “spoiling” of someone’s identity in social situations and, in the process, freeze her/him out of interpersonal relations (Link and Phelan, 2001; Goffman, 1963). Indeed, ample evidence suggests that overweight adolescents have fewer friends, are less integrated into the social networks of their schools, and date less often (Crosnoe et al., 2008; Halpern et al., 2005; Cawley, 2001). Partly as a result of this marginalization at school, they often rate lower on measures of psychological well-being (Needham and Crosnoe, 2005; Goodman and Whitaker, 2002). Importantly, although evidence does suggest that overweight children are often teased and bullied, emotional differences between youth of different body sizes are greater during high school than elementary school (Bradley et al., 2008; Janssen et al., 2004). The importance of the high school years is likely be related to the greater social orientation of adolescents and the more complex cross-sex networks of peer relations housed in secondary schools (Giordano, 2003).
Turning to the socioemotional implications of family instability, stress theory argues that changes in a parent’s marital or romantic relationships are significant stressors for young people, especially when they accumulate over time into long-term patterns of family upheaval (McLanahan, 2004; Teachman, 2003). Such stress is manifested in socioemotional problems, with each family transition adding to the risk above and beyond family structure at any given time. For example, youth tend to have more behavioral problems, greater difficulties connecting to their peers, greater engagement in risky behavior, more observable signs of emotional distress, and other symptoms of maladjustment with each family transition they undergo after birth (Cavanagh et al., 2008; Fomby and Cherlin, 2007; Osborne and McLanahan, 2007; Cavanagh and Huston, 2006; Wu and Martinson, 1993). Importantly, although family change very early in life may be critical, later changes—including in adolescence—do matter to socioemotional adjustment (Cavanagh, 2008; Cavanagh and Huston, 2008).
Thus, body size and family instability can be seen as risk factors for socioemotional health in elementary school and high school. Of course, these risks may differ by gender. Some evidence suggests that, because body norms are stricter and the stigma of weight is stronger among girls than boys, obesity poses greater socioemotional risks to girls (Puhl and Brownell, 2008; Halpern et al., 2005; Needham and Crosnoe, 2005). At the same time, emerging evidence suggests that, for a variety of reasons, family instability may pose more socioemotional risks for boys than girls (Cavanagh and Huston, 2008; Capaldi and Patterson, 1991).
2.2. The potential significance of converging obesity and family trends
Although much attention as been paid to rising rates of obesity and family instability, the possible connections between the two are rarely discussed. Certainly, obesity and family instability may be linked on the individual level. At the very least, they share some common root causes, including socioeconomic disadvantage (McLanahan, 2004; Berkowitz and Stunkard, 2002). Moreover, as both obesity and family instability become more common in the U.S., the number of young people who are overweight and have unstable family lives is likely to grow.
For this study, the conceptual model is grounded in the life course perspective (Elder, 1998), which views the life course as a set of interwoven developmental trajectories (i.e., physical, cognitive, and psychological change), social convoys (i.e., continuity and change in interpersonal relations), and social pathways (i.e., navigation of institutions and contexts). First, the conceptual model of this study considers how one aspect of developmental trajectories (body size) comes together with one aspect of social convoys (the configuration of family members at home) to shape the socioemotional health of young people. Second, as for social pathways, the model focuses on a particular point of vulnerability in the school career, highlighting the early years of high school.
To further break down the first part of this conceptual model, I am working—with a twist—from a well-documented pattern by which potential threats to socioemotional health are buffered by resources in the family domain. For example, numerous factors inside and outside the home are related to poorer socioemotional functioning among young people, including negative peer influences and maternal depression. Yet, youth tend to function better even in the face of such risks when they have other social supports and resources at home, such as a well-organized family environment, a mother with high levels of education, and parents who are sensitive and involved (Augustine and Crosnoe, 2010; Burchinal et al., 2008; Change et al., 2007; Steinberg, 2001). Importantly, the same pattern is relevant to the issues of adolescent obesity and family instability, as evidence suggests that obese youth are better adjusted when they have strong ties to parents and that youth with two present and involved parents function better even in the context of family and neighborhood disadvantage (Crosnoe, 2011; Vanderbilt-Adriance and Shaw, 2008; Change et al., 2007).
This risk × protection framework applies to the current study with a significant conceptual modification. Here, body size is the risk factor for socioemotional health, in that overweight youth are a category of young people with greater probabilities of negative socioemotional outcomes than non-overweight youth. Family instability is, of course, not a protective factor. Instead, it can be viewed as a compromised protective factor. Instead of a protective factor that reduces the translation of risk into negative outcome, a compromised risk factor amplifies this translation. Ample evidence suggests that children and adolescents have healthier socioemotional development when their families serve as a secure base from which they can navigate the world, when safety, order, and stability at home counterbalances the potential chaos that they might encounter outside the home. As such, families that enact this secure base role can counteract other developmental, social, or structural forces that might put young people at socioemotional risk (Steinberg, 2001; Cox and Paley, 1997). Regular changes in family composition (i.e., family members moving in and out) are likely to undermine that secure base, reducing the buffers that children have against any risks they face. Family instability, therefore, may leave young people unprotected against a stigma that threatens their socioemotional health, thereby amplifying the impact of that stigma.
As for the second part of the model, Crosnoe’s (2011) work on social marginalization has demonstrated that risks to socioemotional functioning increase during the early years of high school. At the start of high school, new people are mixed together, social networks (and hierarchies) are gradually constructed over time, and young people often feel momentarily untethered (Benner and Graham, 2009; Eccles et al., 1993). In such contexts, first impressions and external status markers tend to matter a great deal, and lacking a strong sense of security (e.g., from family support) may lead to heightened vulnerability (Crosnoe, 2011). Going back to the interplay of risk and compromised protection described above, these early years in high school may allow the stigma of obesity to stratify social relations while also serving as a period of chaos or uncertainty that magnifies any absence of stability at home. Thus, the first years of high school likely represent a period in which the interplay of body size and family instability will matter to socioemotional health.
Yet, recall the aforementioned stage-related patterns—being overweight may be riskier for girls than boys, but family instability may be more problematic for boys than girls. Whether girls or boys in early high school demonstrate maximum problems related to the interplay of risk (body size) and compromised protection (family instability), therefore, needs to be determined.
3. Data and methods
Add Health is a representative study of American adolescents in grades 7–12 in 1994 (see http://www.cpc.unc.edu/projects/addhealth). With a multi-stage, stratified design, Add Health selected 80 high schools based on region, urbanicity, sector, racial composition, and size. Each school was matched to one of its feeder schools, typically a middle school, with the probability of the feeder school being selected proportional to its contribution to the high school’s student body. Because some high schools were comprehensive schools (e.g., they included 7th or 8th grades too), they served as their own feeder schools. The final school sample included 80 high schools and 52 middle/junior high schools. Nearly all students in each school (approximately 90,000) completed the In-School Survey in the 1994–5 school year. A representative subsample of this student universe, selected evenly across school pairs, participated in the more extensive In-Home Interview at Wave I in 1995 (n = 20,475). Finally, the Wave I sample, minus the Wave I seniors, was followed-up in the Wave II In-Home Interview in 1996 (n = 14,736). The In-Home Interview was repeated in 2001–2002 (Wave IIII) and 2007–2008 (Wave IV), but these data will not be used here. Unfortunately, the Add Health time frame predated the recession of the late 2000s, which would have been an interesting historical period to study.
The focus of this study is on the start of high school. Because Add Health had a multi-cohort design, only one segment of its full sample was studied here. This segment included ninth graders in Wave I attending high schools in which ninth grade was the lowest grade. Some of these students dropped out of Add Health by Wave II. Importantly, Add Health created longitudinal sampling weights to correct for the differential attrition of youth over time. Thus, the Add Health analytical sample included 1751 Wave I ninth graders who remained in the study through Wave II, with special techniques (described below) used to estimate item- and instrument-level missingness in this analytical sample.
3.1. Measures
The Centers for Disease Control and Prevention sets thresholds for overweight and obesity based on body mass index (BMI), a ratio of weight to height calculated with the formula: [weight (kg)/[height (m)]2. Overweight and obesity are defined as having a BMI at or above the 85th and 95th percentiles, respectively, for age and gender. In Wave I, Add Health only included self-reports of height and weight, which is not ideal. Interviewer measures of height and weight were included at Wave II, and they were correlated at .95 with the adolescent self-reports for Wave II (Goodman et al., 2000).
Table 1 includes descriptive statistics for these variables as well as for the other independent and dependent variables. In the 9th grade subsample of Add Health, 27% of youth had BMI categorizing them as overweight, 13% as obese.
Table 1.
Descriptive statistics for all variables.
| M | SD | |
|---|---|---|
| Socioemotional adjustment | ||
| 9th grade internalizing symptoms | 7.26 | 6.04 |
| 10th grade internalizing symptoms | 7.52 | 6.00 |
| 9th grade feelings of not fitting in | 1.02 | 1.22 |
| 10th grade feelings of not fitting in | 1.00 | 1.12 |
| Body size | ||
| Overweight | .27 | .44 |
| Obesity | .13 | .32 |
| Family structure | ||
| Current family structure | ||
| Two-parent family | .52 | .50 |
| Single parent family | .26 | .44 |
| Stepparent family | .17 | .38 |
| Other family type | .05 | .22 |
| Family structure instability (count) | .72 | 1.09 |
| Youth, family, and school controls | ||
| Gender (female) | .51 | .50 |
| White | .57 | .50 |
| African American | .20 | .41 |
| Latino/a | .17 | .37 |
| Asian American | .03 | .18 |
| Other race/ethnicity | .03 | .18 |
| 1st generation immigrant | .07 | .26 |
| 2nd generation immigrant | .12 | .33 |
| 3rd generation immigrant | .80 | .40 |
| Parent a high school dropout | .12 | .32 |
| Parent a high school graduate | .23 | .42 |
| Parent had some college | .26 | .44 |
| Parent a college graduate | .16 | .37 |
| Parent had graduate education | .13 | .33 |
| Family income to needs | 3.16 | 2.16 |
| School sector (private) | .04 | .18 |
| School size | 1444.59 | 867.53 |
| School minority representation | .43 | .31 |
| School SES | .32 | .12 |
Source: National Longitudinal Study of Adolescent Health (http://www.cpc.unc.edu/projects/addhealth).
n = 1751.
A strategy employed by Cavanagh (Cavanagh et al., 2008; Cavanagh, 2008) for Add Health was followed to measure family structure at particular time points as well as cumulative family structure histories. Measurement of current family structure was straightforward. Parent reports of household composition in Wave I household composition were collapsed into dummy variables representing families with two biological parents, single parent families, stepparent families, and other family types. A majority of youth (52%) lived with both biological parents.
Measurement of family structure histories drew on Wave I parent reports of marriages and marriage-like relationships and youth reports of current household composition, the duration of life spent with current household members, and duration of life spent with any non-resident biological parent. For each year of the adolescent’s life, family structure was coded into eight categories (the stepparent and single parent family categories mentioned above were broken down by gender composition, and additional categories, such as adoptive and surrogate parents, were included). Cumulative family instability was measured as a count that increased by one for each transition from one family structure to another from birth through Wave I. As seen in Table 1, the modal amount of family instability was less than one family transition over time.
The two dimensions of socioemotional adjustment considered here were internalizing symptoms and social connections in school. Measures were created across grades/waves for use as both outcomes and controls. Add Health included a modified Center for Epidemiological Studies-Depression scale (Radloff and Locke, 1986), which I used to measure ninth and tenth grade internalizing symptoms. Adolescents reported how often they experienced 15 symptoms of depression, including loneliness and anxiety. Responses, which ranged from 0 (never or rarely) to 3 (most or all of the time), were summed. The not fitting in scale (Crosnoe, 2011) was created for both grades to tap social connections in school. Adolescents reported whether they felt rejected, felt unwanted, had trouble with other students, did not feel close to others at school, and did not feel part of things at school (1 = strongly disagree, 2 = somewhat disagree, 3 = neither disagree or agree, 4 = somewhat disagree, 5 = strongly disagree). The final scale for each grade represented the number of items with which the adolescent somewhat or strongly agreed.
To account for demographic variation, several control variables were measured: gender, parent education (dummy variables for high school dropout, high school graduate, some college, college graduate, postgraduate degree), and family income to needs (annual income reported by parents at ninth grade divided by the federal poverty threshold for that family’s household size). Immigration status (dummy variables for first, second, and third-plus generation) was also measured, as was race/ethnicity (dummy variables for White, African American, Latino/a, Asian American, and other race/ethnicity). Unfortunately, small sample sizes disallowed the examination of race/ethnic differences in results, but doing so is certainly a future need.
Also available were measures of the characteristics of the schools in which youths’ socioemotional experiences were embedded. School administrators completed a survey about schools in Wave I. With these data, I measured school sector (private vs. public), size, minority representation (proportion of students in school who were not White), and socioeconomic composition. School size was measured as the number of students in the student body as reported by school administrators, and school socioeconomic composition was measured by aggregating adolescent reports of parent education on the In-School Survey, a census of each school, to count the proportion of students in each school with a college-educated parent. Corresponding measures of neighborhood characteristics (e.g., minority representation, poverty rate) were created based on Census block data linked to Add Health, but these measures were dropped because they added no explanatory power and did not affect the focal results.
3.2. Plan of analyses
The analytical plan included three steps. In the first, the tenth grade outcomes were regressed on the focal predictors (body size, family structure, family instability) as well as the prior (ninth grade) measures of the outcomes to determine the degree to which the body size and family factors were associated with changes in socioemotional health over time. In the second step, the full set of youth, family, and school controls were added to the model to determine the degree to which observed associations of the body size and family factors with the socioemotional outcomes were accounted for by other characteristics of young people or their social contexts. In the third step, interactions between body size and the focal family variables were estimated to determine the extent to which the socioemotional implications of the body size and family factors were connected. These models were estimated separately by gender.
All models were estimated in Mplus (Muthen and Muthen, 2007), which employed full information maximum likelihood to estimate missing data. It also corrected the study design effects (e.g., the clustering of students within schools) and allowed the use of the aforementioned sampling weights. The final models employed linear regression after comparisons of linear and poisson techniques for the more count-like outcomes revealed little difference between the two.
4. Results
The focus of this study is on the interplay of body size and family instability at different stages of school. As a first step in understanding this interplay, Table 2 presents the breakdown of the various family structure measures by overweight status.
Table 2.
Family status by body size.
| M (SD) | ||
|---|---|---|
|
| ||
| Not overweight | Overweight | |
| Current family structure | ||
| Two-parent family | .54* | .47 |
| (.50) | (.50) | |
| Single parent family | .25+ | .29 |
| (.43) | (.45) | |
| Stepparent family | .17 | .18 |
| (.38) | (.39) | |
| Other family type | .04 | .06 |
| (.21) | (.24) | |
| Family structure instability (count) | .70 | .78 |
| (1.09) | (1.08) | |
| n | 1278 | 473 |
Source: National Longitudinal Study of Adolescent Health (http://www.cpc.unc.edu/projects/addhealth).
Note: Overweight defined as 85% of BMI for age and gender or higher.
Significantly different between groups (p < .05).
Significantly different between groups (p < .10).
Young people who were overweight (at 85th percentile of BMI for age and gender or higher) were slightly more likely than their non-overweight peers to live in households that did not include both of their biological parents, and they had experienced slightly more family instability since birth up to that point in their lives than these peers. These differences, however, were only statistically significant for whether or not youth lived with both parents. Thus, being overweight and experiencing family change were not completely independent of each other during this period windows, although the connection between them was not substantial.
4.1. Overweight high school students
To explore the relations among body size, family instability, and socioemotional health among adolescents in the early years of high school, I estimated a series of models. Table 3 presents partial results of these analyses.
Table 3.
Results of regression models for socioemotional outcomes by overweight status.
| 10th grade internalizing symptoms | 10th grade feelings of not fitting | |||
|---|---|---|---|---|
|
|
|
|||
| Girls | Boys | Girls | Boys | |
| 9th grade version of outcome | .53*** | .56** | .47*** | .43*** |
| (.04) | (.05) | (.03) | (.04) | |
| Overweight | .59 | −.13 | .14 | −.04 |
| (.64) | (.37) | (.11) | (.15) | |
| Current family structure | ||||
| Single parent familya | .57 | 1.60+ | .32* | .39* |
| (.70) | (.96) | (.14) | (.16) | |
| Stepparent family | .70 | −.27 | .03 | −.25 |
| (.85) | (1.16) | (.17) | (.22) | |
| Other family type | .63 | 1.09 | −.05 | −.58+ |
| (1.40) | (2.66) | (.21) | (.34) | |
| Family structure instabilityb | .13 | .14 | .01 | −.02 |
| (.45) | (.65) | (.02) | (.13) | |
| Intercept | 3.76*** | 4.26*** | .55** | .71*** |
| (.97) | (.93) | (.19) | (.13) | |
| R2 | 34 | .32 | .28 | .22 |
| n | 898 | 853 | 898 | 853 |
Source: National Longitudinal Study of Adolescent Health (http://www.cpc.unc.edu/projects/addhealth).
Note: B coefficients presented with standard errors in parentheses. All models also controlled for race/ethnicity, immigration status, parent education, family income to needs, school sector, school size, school minority representation, and school socioeconomic composition. Model 2 also included interactions of obesity with the family structure dummy variables.
Reference category for family structure dummy variables is two-parent.
Family instability is a count of family structure transitions.
p < .05.
p < .01.
p < .001.
Once ninth grade internalizing symptoms and family socioeconomic circumstances were controlled, being overweight was not associated with girls’ or boys’ internalizing symptoms in tenth grade. The same basic pattern held when the outcome was tenth grade measure of feelings of not fitting in at school. Both outcomes did vary somewhat by family structure, but primarily for the single parent structure and more consistently for boys. For example, the association between living single parent homes and feelings of not fitting in (net of such feelings a year earlier) among boys equaled about a third of a standard deviation in the not fitting in distribution.
Additional iterations of each model were estimated with interactions between overweight status and all family structure variables (not shown in Table 3). None reached statistical significance, indicating that the relations between being overweight and indicators of socioemotional adjustment—or lack thereof—did not appear to vary as a function of their current or past family structures, and vice versa. Even though being overweight and experiencing family instability may have co-occurred among some adolescents, this co-occurrence did not seem to have implications for socioemotional health during this particular period.
4.2. Obese high school students
As a final step, I explored the same set of relations in a comparison of high school students who were and were not obese (i.e., at or above the 95th percentile of BMI for age and gender), as opposed to the prior comparisons by overweight status. In doing so, I had to adjust the measurement of family instability due to sparse cell sizes among obese boys and girls in the upper ranges of family instability. The scale was truncated, with those having experienced more than two transitions coded as 2. These additional models revealed no new findings among boys, but they did reveal evidence of a significant interplay between obesity and family instability for girls. Table 4 presents the partial results of these models for the high school girls.
Table 4.
Results of regression models for socioemotional outcomes among girls.
| 10th grade not fitting | 10th grade feelings of internalizing symptoms | |||
|---|---|---|---|---|
|
|
|
|||
| Model 1 | Model 2 | Model 1 | Model 2 | |
| 9th grade version of outcome | .53*** | .53*** | .46*** | .46*** |
| (.04) | (.04) | (.04) | (.04) | |
| Obesity | .55 | −.88 | .04 | .12 |
| (.73) | (.92) | (.13) | (.14) | |
| Current family structure | ||||
| Single parent familya | .58 | .66 | .32* | .39* |
| (.71) | (.73) | (.15) | (.16) | |
| Stepparent family | .68 | 1.24 | .02 | .11 |
| (.85) | (.95) | (.17) | (.19) | |
| Other family type | .64 | 1.41 | −.05 | .04 |
| (1.40) | (1.53) | (.21) | (.23) | |
| Family structure instabilityb | .15 | .15 | .01 | −.05 |
| (.55) | (.55) | (.08) | (.09) | |
| Obesity × family interaction | ||||
| Obesity × instability | 3.46** | .54* | ||
| (1.21) | (.25) | |||
| Intercept | 3.64*** | 3.74*** | .51** | .50 |
| (1.00) | (.98) | (.19) | (.18) | |
| R2 | .34 | .35 | .29 | .29 |
| n | 898 | 898 | 898 | 898 |
Source: National Longitudinal Study of Adolescent Health (http://www.cpc.unc.edu/projects/addhealth).
Note: B coefficients presented with standard errors in parentheses. All models also controlled for race/ethnicity, immigration status, parent education, family income to needs, school sector, school size, school minority representation, and school socioeconomic composition. Model 2 also included interactions of obesity with the family structure dummy variables.
Reference category for family structure dummy variables is two-parent.
Family instability is a count of family structure transitions.
p < .05.
p < .01.
p < .001.
p < .001.
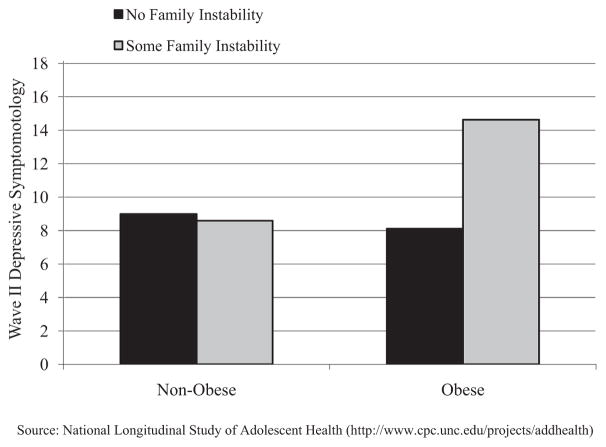
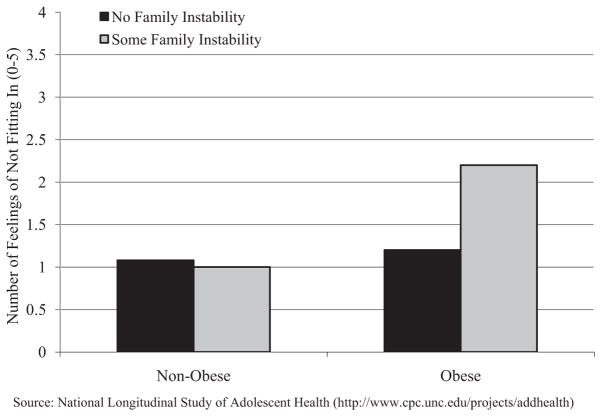
In terms of main effects, obesity was unrelated to the two tenth grade socioemotional outcomes once the ninth grade versions of these outcomes and other important controls were included in the model. Yet, it also interacted significantly with family instability in the fully controlled models. To interpret these two interactions, I calculated predicted values for the two tenth grade outcomes for four focal groups of girls—non-obese and no history of family instability, non-obese and two or more past family structure transitions, obese and no history of family instability, obese and two or more past family structure transitions—while holding all other variables in the model to their sample means/modes among girls. Figs. 1 and 2 present graphs of these predicted values.
Fig. 1.
High school girls’ internalizing symptoms, by obesity and family instability.
Source: National Longitudinal Study of Adolescent Health (http://www.cpc.unc.edu/projects/addhealth).
Fig. 2.
High school girls’ feelings of not fitting in at school, by obesity and family instability.
Source: National Longitudinal Study of Adolescent Health (http://www.cpc.unc.edu/projects/addhealth).
As seen in Fig. 1, non-obese girls did not differ significantly in their tenth grade level of internalizing symptoms (net of ninth grade symptoms) as a function of the level of family instability they had experienced since birth, although non-obese girls with no history of family instability did have slightly fewer symptoms. Among obese girls, however, those who had some experience of family instability in the past demonstrated higher levels of tenth grade internalizing symptoms (net of ninth grade) than their otherwise similar peers with no such histories. In fact, the predicted effect size for family instability among obese girls was nearly a full standard deviation on the tenth grade internalizing scale. The same pattern was observed for girls’ tenth grade feelings of not fitting in (Fig. 2), although the effect size was slightly smaller (about three-fourths of a standard deviation on the tenth grade not fitting in scale).
Among girls at the start of high school, therefore, obesity and family instability appeared to be risks to socioemotional health over time when they were coupled together. This pattern was not true of high school boys or of high school girls who were overweight but not obese.
4.3. Additional considerations
Of great concern in analyses like these is the potential for observed obesity and family stability effects to be endogenous, which would be doubly problematic when studying the interaction between the two (Morris, 2007; McLanahan, 2004). Lagged (or residual change) models, which estimate effects on an outcome at one point net of scores on the outcome at some prior point, are a method for partially reducing the possibility of unobserved confounds (Glazerman et al., 2003). At the same time, by looking at the smaller sample of youth who participated in Wave I in ninth grade and the In-School Survey in 8th grade, I was able to assess whether results were sensitive to more limited pre-high school measures of some aspects of socioemotional functioning. Results appeared consistent. Still, these strategies alone are insufficient. Other sensitivity tests included models weighted by propensity scores indexing the factors predicting obesity or family change (see Frank et al., 2008), which yielded similar results as those presented here. These tests provided some boost in confidence in the results but essentially represented only an alternate way of assessing the impact of observable confounds. Unfortunately, other strategies for assessing or reducing the impact of unobservable confounds were precluded by data limitations. For example, an instrumental variable analysis would be ideal (Cawley, 2000), but no suitable instruments could be found in the two data sets. As another example, the calculation of post hoc robustness indices, such as the Impact Threshold for Confounding Variables (Frank et al., 2008), was made difficult by the small cell sizes and the centrality of interactions to the models.
5. Discussion
The general purpose of this study was to connect two contemporary trends—one dealing with health, one with families—that independently receive a great a deal of attention from researchers and policymakers but are not often considered in tandem. Following the general life course paradigm as well as more specific theories, the argument was that the well-documented social stigma of obesity would put young people at risk for negative self and social evaluations that would hurt their socioemotional health and that family instability would compromise the kinds of family security and attachments that could protect against these risks. In exploring this possible interplay between risk and potentially compromised protection, I focused on the early years of high school, given the potential for heightened socioemotional vulnerability during these years as well evidence that socioemotional problems during this period can factor into truncated rates of educational attainment.
Analyses of Add Health, which had data appropriate data for measuring the focal theoretical concepts, did provide support for the risk × compromised protection framework central to the conceptual model, but only for girls at the highest end of the BMI distribution Specifically, among girls in the first two years of high school, obesity was only associated with socioemotional problems (e.g., internalizing symptoms, feelings of not fitting in at school) when it was coupled with some history of family structure instability. In other words, family instability appeared to magnify the socioemotional risks of obesity for girls during this stage of school to the point that they differed significantly from other girls. Boys did not demonstrate this pattern at the start of high school.
The theoretical interpretation for the isolated evidence for the conceptual model is both developmental and ecological, and it emphasizes the gendered nature of adolescent socioemotional development. Recently pubescent girls tend to be very concerned about (and judged by) their bodies in a school context that facilitates the use of outward appearance and other superficial characteristics as a sorting mechanism and at a point of development in which self-perceptions are often dependent on social feedback (Crosnoe, 2011; Ge et al., 2001). Girls’ bodies are highly sexualized and, as such, are held to a much more stringent standard of appearance. At the same time, they are socialized to be more concerned with others’ feelings toward them, which amplifies the highly social tendencies of adolescents more generally (Rudolph and Conley, 2005; Martin, 1996; Eder et al., 1995). As a result, girls might be more negatively sanctioned for obesity, more likely to internalize these feelings or let them color their perceptions of themselves, and more in need of other social resources (e.g., support and stability at home) to be resilient in the face of such risks. This confluence of issues, then, makes obese girls with unstable family histories especially vulnerable at the start of high school.
Drawing this conclusion is difficult, however, because of many methodological factors, including the reliance on self-reported BMI data as opposed to more sophisticated measures of body fat. Also, the weak family instability main effects were unexpected given past work with Add Health. Some of the discrepancy might have reflected the focus on the start of high school rather than high school or secondary school more generally, but methodological issues (e.g., small sample size, multiple imputation) could also be at work. Furthermore, as already discussed in Section 4.3, causal inference is somewhat shaky. The likelihood is high that obese and non-obese youth are different in ways that might also factor into their socioemotional health. Moreover, socioemotional problems could lead to weight gain (Crosnoe et al., 2008; Goodman and Whitaker, 2002). Similarly, the forces selecting parents into unstable romantic and marital trajectories could also affect their children’s socioemotional health (McLanahan, 2004). A similar pattern of selection could also relate to adolescents’ body size, perhaps even through genetic pathways. Analyzing the data in a longitudinal framework with lagged outcomes helped to address these threats to causal inference, as did the control for a host of individual, family, school, and neighborhood characteristics and some additional sensitivity tests that were performed. Still, these threats cannot be solved with the fairly routine modeling techniques used here. Too many confounds cannot be adequately observed or are as of yet unknown.
Given these methodological limitations, this study must be viewed as a preliminary one. Much more rigorous tests are required in the future. If future studies replicate the patterns of this preliminary study, then the evidence will indicate a need to focus on high school girls experiencing the “double disadvantage” of obesity and family instability. One strategy for better serving these girls is to reduce obesity rates and make family structures more stable. Efforts to do both are now widespread, although with mixed results (Furstenberg, 2007; Wechsler et al., 2004). Another strategy, is to reduce the impact of both on the developmental outcomes of young people through, for example, school mental health services, the expansion of the extracurriculum (given that such activities can provide a concrete way for at-risk youth to meet others and gain senses of achievement and belonging), and even the incorporation of curricular tools to reduce prejudice through educational activities akin to multicultural programs (Pfiefer et al., 2007; Mahoney et al., 2005; Millstein, 1988).
Triangulating such services as a part of extant efforts to ease youth through the early years in a school might be appropriate. Of course, the expected evidence for widespread vulnerability of youth during the two focal school stages studied here did not materialize. Indeed, even the main effects of body size and family instability on socioemotional outcomes reported in past studies of both samples (e.g., Bradley et al., 2008; Cavanagh, 2008; Cavanagh and Huston, 2006; Needham and Crosnoe, 2005) did not hold when looking at these specific time periods or, in the case of Add Health, this specific subset of the sample. As already noted, these discrepancies could reflect measurement or cell size. They could also reflect, however, the possibility that the stages of schooling in question are themselves so socioemotionally troublesome or unsettling for young people that risk factors at other stages might not have as marginally large effects during these periods.
Building on this preliminary study and others like it is important because obesity and family life in the U.S. are intricately related. For young people, obesity is something that develops in the context of families, and so we need to do more to understand what families do or do not do that put children and adolescents at risk for becoming obese and for experiencing the many physical, psychological, and social consequences of being an unhealthy weight.
Acknowledgments
The author acknowledges the support of a faculty scholar award from the William T. Grant Foundation as well as grants from the National Institute of Child Health and Human Development (R01 HD055359, PI: Robert Crosnoe; R24 HD042849, PI: Mark Hayward).
References
- Augustine J, Crosnoe R. Mothers’ depression and educational attainment and their children’s academic trajectories. Journal of Health and Social Behavior. 2010;51:274–290. doi: 10.1177/0022146510377757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benner AD, Graham S. The transition to high school as a developmental process among multi-ethnic urban youth. Child Development. 2009;80:356–376. doi: 10.1111/j.1467-8624.2009.01265.x. [DOI] [PubMed] [Google Scholar]
- Berkowitz RI, Stunkard AJ. Development of childhood obesity. In: Wadden T, Stunkar AJ, editors. Handbook of Obesity Treatment. Guilford; New York: 2002. pp. 515–531. [Google Scholar]
- Bradley RH, Houts R, Nader P, O’Brien M, Belsky J, Crosnoe R the NICHD Early Child Care Research Network. The relationship between body mass index and behavior in children. Journal of Pediatrics. 2008;153:629–634. doi: 10.1016/j.jpeds.2008.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownell KD, Puhl R, Schwartz M, Rudd L. Weight Bias: Nature, Consequences, and Remedies. Guilford; New York: 2005. [Google Scholar]
- Bumpass L, Lu HH. Trends in cohabitation and implications for children’s family contexts in the United States. Population Studies. 2000;54:29–41. doi: 10.1080/713779060. [DOI] [PubMed] [Google Scholar]
- Burchinal M, Roberts J, Zeisel S, Rowley S. Social risk and protective factors for African American children’s academic achievement and adjustment during the transition to middle school. Developmental Psychology. 2008;44:286–292. doi: 10.1037/0012-1649.44.1.286. [DOI] [PubMed] [Google Scholar]
- Capaldi DM, Patterson GR. The relation of parental transitions to boys’ adjustment problems: I. A linear hypothesis, and II. Mothers at risk for transitions and unskilled parenting. Developmental Psychology. 1991;27:489–504. [Google Scholar]
- Cavanagh SE. Family structure history and adolescent adjustment. Journal of Family Issues. 2008;29:944–980. [Google Scholar]
- Cavanagh SE, Crissey SR, Raley RK. Family structure history and adolescent romance. Journal of Marriage and Family. 2008;70:698–714. [Google Scholar]
- Cavanagh SE, Huston AC. Family instability and child well-being. Social Forces. 2006;85:551–581. [Google Scholar]
- Cavanagh SE, Huston AC. The timing of family instability and children’s social adjustment. Journal of Marriage and Family. 2008;70:1258–1270. [Google Scholar]
- Cawley J, Spiess K. Obesity and skill attainment in early childhood. Economics and Human Biology. 2010;6:388–397. doi: 10.1016/j.ehb.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Cawley J. An instrumental variables approach to measuring the effect of body weight on employment disability. Health Services Review. 2000;35:1159–1179. [PMC free article] [PubMed] [Google Scholar]
- Cawley J. Body weight and the dating behaviors of young adolescents. In: Michael RT, editor. Social Awakening: Adolescent Behavior as Adulthood Approaches. Russell Sage; New York: 2001. pp. 174–198. [Google Scholar]
- Change J, Halpern C, Kaufman J. Maternal depressive symptoms, father’s involvement, and the trajectories of child problem behaviors in a U.S. national sample. Archives of Pediatric Adolescent Medicine. 2007;161:697–703. doi: 10.1001/archpedi.161.7.697. [DOI] [PubMed] [Google Scholar]
- Cherlin A. The Marriage-Go-Round: The State of Marriage and Family in America Today. Random House; New York: 2009. [Google Scholar]
- Cox M, Paley B. Families as systems. Annual Review of Psychology. 1997;48:243–267. doi: 10.1146/annurev.psych.48.1.243. [DOI] [PubMed] [Google Scholar]
- Crandall C. Prejudice against fat people: ideology and self-interest. Journal of Personality and Social Psychology. 1994;66:882–894. doi: 10.1037//0022-3514.66.5.882. [DOI] [PubMed] [Google Scholar]
- Crosnoe R. Fitting In, Standing Out: Navigating the Social Challenges of High School to Get an Education. Cambridge University Press; New York: 2011. [Google Scholar]
- Crosnoe R, Frank K, Mueller AS. Gender, body size, and social relations in American high schools. Social Forces. 2008;86:1189–1216. [Google Scholar]
- Eccles JS, Midgley C, Wigfield A, Buchanan C. Development during adolescence: the impact of stage-environment fit on young adolescents’ experiences in schools and in families. American Psychologist. 1993;48:90–101. doi: 10.1037//0003-066x.48.2.90. [DOI] [PubMed] [Google Scholar]
- Eder D, Evans C, Parker S. School Talk: Gender and Adolescent Culture. Rutgers University Press; New Brunswick, New Jersey: 1995. [Google Scholar]
- Elder GH. The life course as developmental theory. Child Development. 1998;69:1–12. [PubMed] [Google Scholar]
- Fomby P, Cherlin A. Family instability and child well-being. American Sociological Review. 2007;72:181–204. doi: 10.1177/000312240707200203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank K, Sykes G, Anagnostopoulos D, Cannata M, Chard L, Krouse A, McCrory R. Does NBPTS certification affect the number of colleagues a teacher helps with instructional matters? Educational Evaluation and Policy Analysis. 2008;30:3–30. [Google Scholar]
- Freedman D, Mei Z, Srinivasan S, Berenson G, Dietz W. Cardiovascular risk factors and excess adiposity among overweight children and adolescents: the Bogalusa Heart Study. Journal of Pediatrics. 2007;150:12–1700. doi: 10.1016/j.jpeds.2006.08.042. [DOI] [PubMed] [Google Scholar]
- Furstenberg F. Should government promote marriage? Journal of Policy Analysis and Management. 2007;26:956–960. [Google Scholar]
- Ge X, Elder GH, Jr, Regnerus M, Cox C. Pubertal transitions, overweight self perceptions, and adolescent psychosomatic adjustment: gender and ethnic differences. Social Psychology Quarterly. 2001;64:363–375. [Google Scholar]
- Giordano PC. Relationships in adolescence. Annual Review of Sociology. 2003;29:257–281. [Google Scholar]
- Glazerman S, Levy D, Myers D. Nonexperimental versus experimental estimates of earnings impacts. Annals of the American Academy of Political and Social Science. 2003;589:63–85. [Google Scholar]
- Goffman E. Stigma: Notes on the Management of Spoiled Identity. Prentice-Hall; Englewood Cliffs, NJ: 1963. [Google Scholar]
- Goodman E, Hinden B, Khandelwal S. Accuracy of teen and parental reports of obesity and body mass index. Pediatrics. 2000;106:52–58. doi: 10.1542/peds.106.1.52. [DOI] [PubMed] [Google Scholar]
- Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;109:497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- Halpern C, King R, Oslak S, Udry JR. Body mass index, dieting, romance, and sexual activity in adolescent girls: relationships over time. Journal of Research on Adolescence. 2005;15:535–559. [Google Scholar]
- Hartup W, Stevens N. Friendships and adaptation in the life course. Psychological Bulletin. 1997;121:355–370. [Google Scholar]
- Hogan DP, Goldscheider FK. Success and challenge in demographic studies of the life course. In: Mortimer J, Shanahan M, editors. Handbook of the Life Course. Plenum; New York: 2002. pp. 681–702. [Google Scholar]
- Janssen I, Craig W, Boyce W, Pickett W. Associations between overweight and obesity with bullying behaviors in school-age children. Pediatrics. 2004;113:1187–1193. doi: 10.1542/peds.113.5.1187. [DOI] [PubMed] [Google Scholar]
- Kalist DE, Siahaan F. The association of obesity with the likelihood of arrest for young adults. Economics and Human Biology. 2012 doi: 10.1016/j.ehb.2012.02.001. [DOI] [PubMed] [Google Scholar]
- Koch D. Waaler revisited: the anthropometrics of mortality. Economics and Human Biology. 2011;9:106–117. doi: 10.1016/j.ehb.2010.04.001. [DOI] [PubMed] [Google Scholar]
- Lakdawalla D, Philipson T. The growth of obesity and technological change. Economics and Human Biology. 2009;7:283–293. doi: 10.1016/j.ehb.2009.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Link BG, Phelan JC. Conceptualizing stigma. Annual Review of Sociology. 2001;27:363–385. [Google Scholar]
- Loh ES. The economic effects of physical appearance. Social Science Quarterly. 1993;74:420–438. [Google Scholar]
- Mahoney JL, Larson RW, Eccles JS, editors. Organized Activities as Contexts of Development: Extracurricular Activities, After-School and Community Programs. Routledge; New York: 2005. [Google Scholar]
- Martin KA. Puberty, Sexuality, and the Self: Boys and Girls at Adolescence. Routledge; New York: 1996. [Google Scholar]
- McLanahan S. Children and the second demographic transition. Demography. 2004;41:607–628. doi: 10.1353/dem.2004.0033. [DOI] [PubMed] [Google Scholar]
- Millstein SG. The Potential of School-Linked Centers to Promote Adolescent Health and Development. Carnegie; Washington, DC: 1988. [Google Scholar]
- Morris S. The impact of obesity on employment. Labour Economics. 2007;14:413–433. [Google Scholar]
- Muthen LK, Muthen BO. Mplus User’s Guide. Authors; Los Angeles: 2007. [Google Scholar]
- National Institute of Diabetes and Digestive and Kidney Diseases. [accessed 01.05.09];Weight Control Information Network. 2009 http://win.niddk.nih.gov/index.htm.
- Needham BL, Crosnoe R. Overweight status and depressive symptoms during adolescence. Journal of Adolescent Health. 2005;36:48–55. doi: 10.1016/j.jadohealth.2003.12.015. [DOI] [PubMed] [Google Scholar]
- Ogden C, Carroll M, Curtin L, Lamb L, Flegal K. Prevalence of high body mass index in U.S. children and adolescents, 2007–2008. Journal of the American Medical Association. 2010;303:242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- Ogden C, Carroll M, Flegal K. High body mass index for age Among U.S. children and adolescents, 2003–2006. Journal of the American Medical Association. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- Osborne C, McLanahan S. Partnership instability and child wellbeing. Journal of Marriage and Family. 2007;69:1065–1083. [Google Scholar]
- Pfiefer JH, Brown CS, Juvonen J. Teaching tolerance in schools: lessons learned since Brown v. Board of Education about the development and reduction of children’s prejudice. SRCD Social Policy Reports. 2007;21(2):3–17. [Google Scholar]
- Puhl R, Brownell K. Bias, discrimination, and obesity. In: Bray G, Bouchard C, editors. Handbook of Obesity: Clinical Applications. Informa Healthcare; New York: 2008. pp. 81–90. [Google Scholar]
- Radloff LS, Locke BS. The community mental health assessment survey and the CES-D scale. In: Weissman M, Meyers J, Ross C, editors. Community Surveys of Psychiatric Disorders. Rutgers; New Brunswick, NJ: 1986. pp. 177–189. [Google Scholar]
- Rudolph KD, Conley CS. The socioemotional costs and benefits of social-evaluative concerns: do girls care too much? Journal of Personality. 2005;73:115–138. doi: 10.1111/j.1467-6494.2004.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serdula MK, Ivery D, Coates RJ, Freedman SD, Williamson DF, Byers T. Do obese children become obese adults? A review of the literature. Preventive Medicine. 1993;22:167–177. doi: 10.1006/pmed.1993.1014. [DOI] [PubMed] [Google Scholar]
- Steinberg LD. We know some things: parent–adolescent relationships in retrospect and prospect. Journal of Research on Adolescence. 2001;11:1–20. [Google Scholar]
- Teachman JD. Childhood living arrangements and the formation of coresidential unions. Journal of Marriage and Family. 2003;65:507–524. [Google Scholar]
- Vanderbilt-Adriance E, Shaw D. Protective factors and the development of resilience in the context of neighborhood disadvantage. Journal of Abnormal Child Psychology. 2008;36:887–901. doi: 10.1007/s10802-008-9220-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler H, McKenna M, Lee S, Dietz W. The Role of Schools in Preventing Childhood Obesity. National Association of State Boards of Education; Arlington, VA: 2004. [Google Scholar]
- Wu LL, Martinson B. Family structure and the risk of a premarital birth. American Sociological Review. 1993;58:210–232. [Google Scholar]