Abstract
A palliative approach involves adapting and integrating principles and values from palliative care into the care of persons who have life-limiting conditions throughout their illness trajectories. The aim of this research was to determine what approaches to nursing care delivery support the integration of a palliative approach in hospital, residential, and home care settings. The findings substantiate the importance of embedding the values and tenets of a palliative approach into nursing care delivery, the roles that nurses have in working with interdisciplinary teams to integrate a palliative approach, and the need for practice supports to facilitate that embedding and integration.
Keywords: end-of-life care, health services research, hospice and palliative care nursing, knowledge synthesis, nursing services, palliative approach, person-centered care, practice patterns, nurses
PEOPLE who have chronic life-limiting conditions have complex and multifaceted needs that arise at different points during their illness trajectory. Many receive care over time from health care professionals within various health care sectors, including hospital, residential, and home care. Good care for people who have life-limiting conditions requires that principles of palliative care are adapted and integrated into contexts of care that do not provide specialized palliative care services, regardless of the health care sector in which the care is provided. This is often referred to as a “palliative approach” to care.1–3 Broadly conceptualized, a palliative approach involves adapting and integrating principles from palliative care (eg, patient- and family-centered care focused on quality of life of the person and not just on the disease) into the care received by persons who have life-limiting conditions as they encounter various health care sectors throughout their illness trajectory.4,5 This blending of chronic disease management and palliative care requires an “upstream” orientation to care delivery that addresses the needs of patients and their families related to the advancing nature of their illness and necessitates the integration of care delivery systems and partnerships among service providers to address these needs across all sectors of care.6
Statements of Significance
What is known or assumed to be true about this topic:
Although specialized palliative care is necessary for addressing the needs of some populations, the majority who have life-limiting conditions do not receive specialized palliative care and yet have nursing care needs related to the advancing nature of their condition.
A palliative approach involves adapting and integrating principles and values from palliative care into the care received by persons who have life-limiting conditions.
What this article adds:
This article illustrates the value of an integrated approach to health services nursing research that combines literature synthesis of general knowledge with concurrent analyses of contextualized knowledge.
To meet the needs of persons who have life-limiting conditions, it is imperative that the values and tenets of a palliative approach are embedded in nursing care delivery across sectors of care.
This research reveals important understandings about the nature and integral role of nursing in providing a palliative approach.
Practice supports are necessary but can be implemented only in concert with fundamental values that are in keeping with a palliative approach.
People living with life-limiting conditions spend considerable time with nurses across sectors of the health care system. Consequently, nursing has a significant role in determining the quality of care for this population.7 However, conventional nursing care for these people has been oriented to a curative focus rather than to the implications of the life-limiting nature of the condition.4 It follows that many nurses do not recognize the full range of patients' and families' needs that arise throughout their illness trajectories.8 There is an urgent need to enhance our approach to nursing care delivery such that it becomes more responsive to the needs of patients who have chronic life-limiting conditions.
The current health care context provides considerable opportunity for this enhancement of nursing care delivery and the integration of practice supports to improve the quality of nursing care for populations who have complex needs associated with chronic life-limiting conditions. To do so, nursing managers, educators, clinicians, health care administrators, and policy makers must make evidence-informed decisions about nursing care delivery that will ensure positive outcomes for patients, promote quality practice environments for nurses, and utilize resources effectively. This requires both the synthesis of general knowledge about care delivery and the contextualization of that knowledge to particular practice settings.9 General knowledge from the literature must be tested and adapted to local contexts to ensure its relevance and applicability. Given the growing population of persons with chronic life-limiting conditions and the demands for improvement in nursing care delivery systems, there is a need to synthesize and integrate available knowledge about nursing care delivery and practice supports consistent with a palliative approach to care.
PURPOSE
As part of an overarching initiative, Initiative for a Palliative Approach in Nursing: Evidence and Leadership (iPANEL, www.ipanel.ca), we conducted a collaborative research project with the aim to identify approaches to nursing care delivery and practice support strategies that facilitate the integration of a palliative approach in acute medical, residential care, and home health settings. The objectives were to contribute both general knowledge based on a synthesis of existing evidence from the literature about a palliative approach to nursing care delivery, and contextualized knowledge about the application of a palliative approach in particular health care settings and systems. Herein, we describe our research approach to integrated knowledge synthesis that links general knowledge with contextualized knowledge and present the overarching results of the project.
METHODS
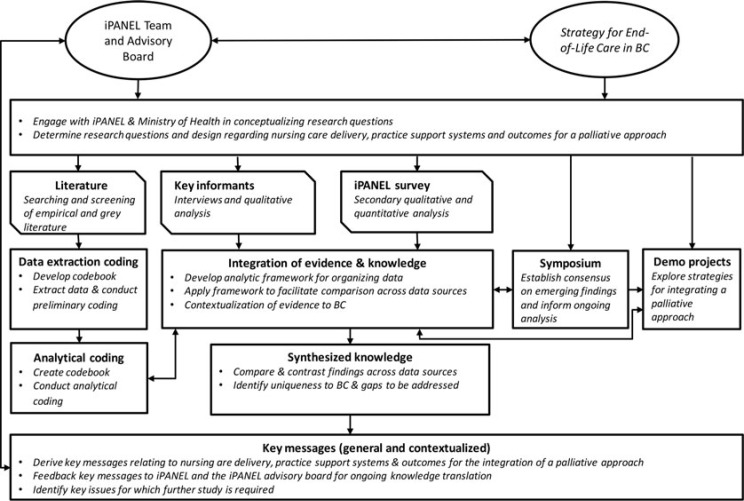
This project combined knowledge synthesis10 and integrated knowledge translation methods11,12 in an iterative design consisting of 4 intersecting research strategies, including 1 designed to identify general knowledge from the literature and 3 designed to contextualize that knowledge (see Table 1). The first strategy, which focused on general knowledge, involved a systematic synthesis of literature about nursing care delivery and practice support strategies and tools relevant to a palliative approach. The 3 remaining research strategies focused on contextualization of knowledge. This included secondary analyses of a province-wide nursing survey about a palliative approach8 and primary analyses of interviews with key informants (research strategy 2). Contextualization was further informed by 2 integrated knowledge translation activities: engagement of stakeholders through a province-wide symposium (research strategy 3) and 2 demonstration projects (research strategy 4). The overall integrated analytical approach involved several iterations of relating synthesized knowledge from the literature to experiences and perspectives of nurses in particular practice settings. An overview of the analytic processes integrating these 4 research strategies and the linkages with the overarching iPANEL team and the Strategy for End-of-Life Care in our province13 is provided in Figure 1. In presenting our findings, the term general knowledge refers to that which has been derived from the literature synthesis. Contextualized knowledge refers to findings derived from the particular practice settings (hospital, residential, and home care) and the context of the regional health care system.
Table 1. Research Strategies and Goals.
| General Knowledge | Contextualized Knowledge | ||
|---|---|---|---|
| Synthesis of existing studies and grey literature | Qualitative analyses of survey and key informant interviews | Knowledge translation activity: Provincial symposium | Knowledge translation activity: Demonstration projects |
| Contribution to the development of recommendations about (a) approaches to nursing care delivery, (b) practice supports that facilitate the integration of a palliative approach within various health care contexts, (c) and outcomes for a palliative approach. | Identify approaches and challenges pertaining to the integration of a palliative approach and to use this knowledge to adapt knowledge from the literature to particular contexts of nursing care delivery. | Establish consensus on emerging findings and inform ongoing analysis. | Explore how a palliative approach to nursing care delivery could meet the needs of patients, residents, clients, and their families. |
Figure 1.
Overview of knowledge integration process.
General knowledge
The project involved a synthesis of empirical knowledge (based on research findings in primary studies and reviews) and nonempirical discourses (no explicit reference to research findings) in published literature on nursing care delivery and practice supports relevant to the integration of a palliative approach. Established knowledge synthesis methods were used to identify relevant sources, systematically extract information, and conduct a synthesis by using methods of thematic and content analysis.10 A comprehensive search of library databases (Ageline, Biomedical Reference Collection, CINAHL, Cochrane Systematic Reviews, Embase, Healthsource, MEDLINE, ProQuest Dissertations, PsycINFO, and Web of Science) was implemented as part of an overarching knowledge synthesis on a palliative approach conducted by iPANEL.5 This search strategy, which is described elsewhere, identified documents relevant to a palliative approach based on the intersection of (a) concepts associated with palliative care (including hospice care, comfort care, end-of-life care, etc) and (b) concepts reflective of chronic life-limiting conditions (including a selection of the most common chronic life-limiting conditions). Through this process, 629 documents were identified as “relevant” (ie, about a palliative approach) or “related” (ie, addresses health care information of relevance to a palliative approach). For the synthesis described herein, these articles were subsequently screened on the basis of specific inclusion criteria corresponding to the objectives of this project. Documents focusing predominantly on specialized palliative care (provided by specialized palliative care professionals) or on the management of one particular symptom (rather than overall care of a person who has a life-limiting condition) were excluded. Following standard recommendations, all documents were double-screened for relevance. Documents for which relevance was inconclusive were reviewed by other research team members to establish relevance by consensus. Consistent with the exploratory nature of this review and to avoid selection bias due to constraints in publishing details on methods, empirical documents were not reviewed for quality. The final selection included 177 relevant empirical documents and 269 nonempirical documents.
A data extraction codebook was developed and applied using the EPPI-Reviewer system14 to extract descriptive information from the 177 empirical documents. Thematic analysis and content analysis methods were utilized to iteratively construct and verify common overarching thematic patterns pertaining to the research aim.10 A subsequent review of nonempirical literature (269 documents) was conducted to further explore ambiguities and gaps in knowledge revealed in the synthesis of empirical literature in relation to nursing care delivery and roles. Data were extracted and analyzed for 40 documents that explicitly focused on nursing care delivery and roles.
Contextualized knowledge
Contextualization of knowledge was achieved via the following 3 strategies: (1) qualitative analyses of interviews and focus groups with survey respondents and key informants, (2) a provincial symposium on a palliative approach and nursing care delivery in the provincial health system, and (3) 2 demonstration projects that explored how a palliative approach could be integrated within particular care teams. Research ethics approvals were obtained from related ethics review boards and all participants provided written informed consent.
Qualitative analysis of data from survey respondents and key informants
The first strategy involved qualitative analyses of interviews and focus groups with survey respondents and interviews with key informants. The goal was to identify approaches and challenges pertaining to the integration of a palliative approach and to use this knowledge to contextualize emerging general recommendations within particular settings and the provincial health care system. We relied on interpretive description15 as the qualitative approach for concurrent data analysis and ongoing data collection, each informing the other in an iterative process as the preliminary thematic patterns were inductively generated from the data.
The secondary qualitative analyses were conducted on interviews and focus groups with 25 nurses and 5 health care workers who participated in a nurse survey (N = 1468 in 114 nursing care settings across the province of British Columbia, Canada, which is described elsewhere).8 This reanalysis focused on the perspectives of point-of-care nursing staff regarding approaches to nursing care delivery and practice supports that facilitate the integration of a palliative approach in particular nursing care settings.
Additional open-ended interviews were conducted with key informants to ascertain nursing leadership perspectives regarding the project's research aim. Purposive, snowball sampling was used to gather perspectives within several health care contexts. The 12 key informants were experts involved in nursing administration, education, or nursing care delivery who provided leadership at various levels in the health care system. They were from diverse care settings, spanning 5 health regions in British Columbia, including 4 directors, 3 advanced practice nurses, 1 chief nursing officer, 1 licensed practice nurse, 1 registered nurse, 1 nurse practitioner, and 1 educator of health care workers. Interview questions related to nursing care delivery and practice supports for a palliative approach were used to prompt in-depth responses from these key informants.
A provincial symposium
A provincial symposium (the third strategy) was held to engage local leaders in nursing care delivery (nursing care providers, managers and educators, health care administrators, and decision and policy makers) in building consensus on emerging findings. Perspectives were solicited from the 81 attendees on the following 3 key topics: nursing care delivery, practice supports, and outcomes pertaining to a palliative approach. Each topic was introduced with a short presentation on emerging study results, followed by moderated round table discussions. Attendees were asked to formulate key recommendations for each topic.
Demonstration projects
Finally, the fourth strategy involved 2 demonstration projects through which we engaged nurses in different care settings to explore how aspects of a palliative approach could be integrated into local care delivery systems. In the first demonstration project, nursing staff and interdisciplinary team members in a residential care facility collaboratively reviewed the care received by a resident and family while considering how care might have been different had a palliative approach been used. The review informed a change in care processes based on daily care team meetings (“huddles”) to discuss residents for whom there were concerns and to explore how to best integrate a palliative approach. The second demonstration project, which was in a home health setting, began by reflecting on the practices of the long-term care nurse case managers who serve a client population with conditions or disabilities affecting their ability to manage at home. Many of these clients have life-limiting conditions, while not receiving palliative care services that, in this health care system, are reserved for those who are expected to die within 6 months. Using regular meeting times with the case managers and their leaders, the project focused on particular care processes in the home health setting that could be improved to better address the palliative needs of all clients with life-limiting conditions, regardless of their expected prognosis.
Five focus groups were held at the demonstration project sites to explore the integration of a palliative approach using broad questions related to the process of understanding a palliative approach, the practice changes at each site, and the influence of the practice contexts. Thematic analysis was applied to the transcripts of the focus group recordings and the facilitators' field notes to identify recurring, converging, and opposing thematic patterns, key concepts, and illustrative examples from the data.
RESULTS
To answer the question of what approaches to nursing care delivery support the integration of a palliative approach, we broadly organized the results into 3 thematic patterns: embedding the values and tenets of a palliative approach, nursing roles within a palliative approach, and practice support for a palliative approach. To enhance clarity around the origins of the data, we discuss each of those thematic patterns in terms of general knowledge and contextualized knowledge. The documents included in the literature synthesis involved predominantly published manuscripts and included reports of primary research (qualitative, quantitative, and mixed methods) as well as 20 knowledge synthesis studies (see Table 2). Most of the research was conducted in the United Kingdom or the United States. The studies addressed a wide variety of chronic conditions and sectors of care, as shown in Table 3. The majority of the nonempirical documents focused on the nursing roles pertaining to qualifications and responsibilities of nurses (33), other overlapping topics included those pertaining to models/framework (15), policy (3), and outcomes relating to patient/family, nursing and organizational levels (5).
Table 2. Description of Studies Included in the Literature Synthesis (n = 177).
| Document Type | # | Study Method | # | Country | # |
|---|---|---|---|---|---|
| Published manuscript | 147 | Quantitative | 53 | Australia | 20 |
| Thesis/Dissertation | 3 | Qualitative | 71 | Canada | 13 |
| Presentation/newsletter/abstract | 21 | Mixed methods | 32 | United Kingdom | 64 |
| Other | 6 | Knowledge synthesis | 20 | United States | 54 |
| Othera | 26 |
aChina (2), Germany (2), Global (15), Italy (2), Netherlands (2), Sweden (2), and New Zealand (1).
Table 3. Classification of Studies by Health Conditions and Health Care Sectors.
| # Articles by Health Care Sectora | |||||
|---|---|---|---|---|---|
| Health Conditions | # Articles | Hospital | Residential | Home and Community | Otherb |
| Multiple chronic diseases | 45 | 19 | 13 | 18 | 7 |
| Cancer | 27 | 13 | 5 | 15 | 4 |
| Dementia | 13 | 4 | 9 | 2 | 1 |
| Chronic obstructive pulmonary disease | 10 | 7 | 0 | 5 | 1 |
| Neurological diseases | 10 | 5 | 5 | 6 | 5 |
| Acquired immunodeficiency syndrome | 1 | 0 | 0 | 0 | 1 |
| Renal disease | 10 | 7 | 0 | 2 | 2 |
| Frail elderly | 3 | 0 | 1 | 2 | 0 |
| Congestive heart failure | 7 | 4 | 0 | 3 | 1 |
| Other | 3 | 1 | 2 | 0 | 0 |
| Not specified | 48 | 14 | 22 | 12 | 11 |
| Total | 177 | ||||
aCoding is not mutually exclusive as some studies addressed multiple health care sectors.
bHospice care, education, unspecified.
Embedding the values and tenets of a palliative approach
General knowledge
Although the term “a palliative approach” is often not explicitly used in the literature, there is broad recognition that the tenets of a palliative approach, which are adapted from palliative care principles and values, are applicable to and must be integrated into nursing care delivery across all sectors of care for people who have life-limiting conditions. A palliative approach is described as a patient-centered approach to care guided by the understanding that the person is on a progressive life-limiting illness trajectory.16–20 Communication related to the patients' and families' evolving understandings, personal preferences, and goals of care is understood as essential,21–24 as is aptly illustrated in the following quote by Schofield et al:
... the traditional sharp transition point from a curative to palliative goal of care is blurred. Hence, a palliative approach, also referred to as simultaneous care, acknowledges the likelihood of gradual transition, emphasizing quality of life considerations during the active treatment phase. It recognizes that treatment goals will evolve from seeking a cure, to control of disease and complications, maintaining physical functioning and quality of life, and ultimately to symptom control.25(p398)
A palliative approach is rarely discussed in terms of distinct nursing care delivery models or systems; rather, it is understood as being embedded within all levels, including the system, the care delivery of each setting, and the health care team. As such, it represents a set of underlying values and premises associated with care. Forbes-Thompson and Gessert, in a study of care homes, documented an example of one such setting in which a palliative approach “permeated” the organization's mission, values, care planning, and care delivery such that “it was clear that ‘caring for dying people' was integrated into daily care processes.”26(p553)
The synthesis also revealed that embedding a palliative approach into existing care delivery systems requires an emphasis on effective communication within and across interdisciplinary teams, including nonprofessional health care workers. The necessity of care delivery by teams composed of diverse members arises because of the inherent complexity and multidimensional nature of the needs of this patient population.27 According to Ross et al, this teamwork requirement pertains to both system redesign and clinical approaches, such that “comprehensive and compassionate”28(p5) care becomes possible through deployment of a cadre of personnel with specific expertise providing consultation to those delivering direct services.
These themes of system embeddedness and interdisciplinary teamwork are understood as integral to the delivery of a palliative approach to people who have life-limiting chronic conditions, including, for example, dementia, chronic obstructive pulmonary disease, and heart failure.16,17,29,30 Although our literature synthesis confirmed that there is no established nursing care delivery model for a palliative approach, it revealed examples of systems or models that aim to integrate a palliative approach into particular sectors of care. One of the most extensively studied systems of this form of care is the Gold Standards Framework (GSF), a quality improvement program developed to optimize end-of-life care in generalist primary care and nursing home settings, which has been incorporated into the End of Life Care Strategy in the United Kingdom.31–41 Although multidisciplinary in focus, there is evidence that the GSF is highly relevant to the practice of nurses. However, although it has been widely adopted in UK primary care and nursing home care contexts where care is provided over an extended period of time, it has not been as readily applicable to the acute care context, where the focus remains more on episodic and task-oriented care.
Contextualized knowledge
Analyses of the contextual information derived from qualitative interviews and focus groups in this study confirmed that a palliative approach was better understood as a philosophy that was integrated throughout all aspects of care rather than demonstrated in isolated practices and systems of care delivery. One key informant captured this idea by saying: “It needs to be a shift of thinking, and I think that is the key. It's going to be very challenging to actually embed it and change the thinking of practice.” Informants emphasized that the integration of a palliative approach must be grounded in understandings and expertise that often differ across contexts of care. What is appropriate, feasible, and effective practice for a palliative approach in acute medical units will be different for residential and home health settings.
The accounts of nurses and key informants revealed that the integration of a palliative approach is influenced by various definitions of the term “palliative” as they have been understood within particular practice contexts. This challenge of different meanings was seen as particularly pertinent in acute care where the term “palliative” often refers to specialist palliative care for the dying. As one key informant commented:
In the acute care setting, as soon as somebody is identified as palliative, the referrals go out to the experts... to provide direction, which misses the opportunity for the nurses to define and to work with the family to define the care that the family and the individual would like to have happen at the end-of-life.
The focus groups and key informant interviews also revealed a sense of readiness for the integration of a palliative approach, especially in the context of residential and home care settings where the progressive nature of chronic conditions was acknowledged. Observing that as one nurse expressed it “in residential care, everyone has a life-limiting illness,” many of the nurses have begun to integrate a palliative approach from admission onward. Similarly, in home care, the nurses described the implications of acknowledging the life-limiting nature of chronic conditions. As one nurse explained:
It's all about anticipatory care and understanding what that journey could potentially look like.... I think that a lot of nurses maybe wouldn't recognize that they're providing a palliative approach but they would say that they're providing person-centered care.
In several instances, nurses pointed to recent specific local initiatives, such as advance care planning or disease specific programs aimed at quality of life with chronic conditions, as the kinds of approaches they felt exemplified the palliative approach ideal. Although the palliative approach to some extent represented a new way of thinking about care, it also felt familiar in that it reflected fundamental nursing values. As one explained, “It's an exciting time because there's things shifting. And it's not like pushing a boulder, it's more like pushing a snowball.”
Despite the readiness and familiarity that was apparent in the residential and home care sectors, the informants confirmed that some current policies and practice structures were not well aligned with nursing care delivery for a palliative approach. For example, within residential care, the close monitoring of weight and concern about weight loss seem at cross-purposes with the understanding of an illness trajectory, which inevitably involves decline. Similarly, within community care, the criterion for entry into a provincial palliative benefits program (ie, “a life expectancy of up to six months”)13,42(p1) contributed to misunderstandings of the term “palliative” and limited recognition of the palliative needs of persons who have life-limiting conditions other than cancer. In the acute care setting, there was an even stronger recognition that current systems of care delivery remain incongruent with, and therefore constrain, the integration of a palliative approach. For example, the emphasis on addressing the primary reason for admission and focusing on discharge planning limits the opportunity to engage in proactive care planning in a more holistic way. As one key informant aptly expressed it: “The approach is to address and [treat] the acute condition, [rather than] all these underlying issues—like dementia, heart failure, pneumonia, stroke...—And everything else is secondary.”
Thus, interpreting the general knowledge from the evidentiary literature in the context of the experiential understandings derived from practice builds a portrait of the complexity associated with embedding the values and tenets of a palliative approach into a nursing care delivery system. From both sources, we can see that it must be taken up across high functioning and communicative interdisciplinary care teams and firmly established in core values and care delivery systems to be realized in a meaningful way.
Nursing role within a palliative approach
General knowledge
In emphasizing the need for an interdisciplinary team to deliver a palliative approach, our review of the literature revealed a rather surprising gap with respect to the nature of the nursing role. The available studies have predominantly focused on the work of interdisciplinary health care teams, with relatively limited explication of the roles of the individual disciplines. Where individual disciplines are discussed, it is generally recognized that nurses and other allied health care professionals such as spiritual care and social work play a more dominant role than physicians when the needs become primarily emotional, social, and spiritual.19 Reports of established initiatives such as the Comprehensive, Adaptable, Life-Affirming, Longitudinal (CALL) Palliative Care Project illustrate this characteristic sense of interchangeability and fluidity in the roles of team members:
Interdisciplinary team members included the champion and coordinator, physicians, nurses, social workers, chaplains, pharmacists, and others who had contact with patients or families. The interdisciplinary team met routinely to discuss the patient and family needs and learn from each other's observations... Teams pragmatically assigned responsibility for the various interventions based on licensure, availability, and relationship to the patient and family.43(p1218)
Our synthesis revealed several studies that focused on advanced practice nursing roles in the delivery of a palliative approach,21,44 with broad consideration of appropriate roles for generalist and specialist nurses. For example, in developing a framework for a model of integrated malignant and nonmalignant palliative care for the western Scottish isles, Senior and Hubbard45 examined the region's existing nursing roles for both generalist and specialist nurses and made recommendations to enhance coordination of the care they delivered. Such studies illustrate the importance of defining the responsibilities at the nursing generalist and specialist level within each context of care, as a palliative approach requires both the capacity to integrate a palliative approach within generalist practice and also the expertise and consultative support of specialist nurses.17,45
Because the role of nurses within a palliative approach was not extensively described in the empirical literature, we also reviewed nonempirical literature to address this gap. Such papers were typically written for a defined nursing specialty audience, such as the patient population contexts of gerontology, nephrology, neurology, or heart failure, or by setting, such as the community or nursing homes. These sources revealed a shared understanding that the nursing role in a palliative approach includes provision of patient education concerning their condition and care choices, communication regarding decision making such as advance care planning and goals of care, monitoring of the patient's health status, management of symptoms, and provision of direct care for the imminently dying patient.46,47 The nonempirical literature also articulated various barriers to nurses enacting these roles. Among the barriers identified were communication challenges for nurses, such as concern that patients would be upset or that hope would be removed by discussing topics such as advance care planning,48 and concern that the authority of nurses to be involved in the decision making regarding end-of-life care might be contested.46,47,49 As Cohen and Nirenberg explained:
Another barrier preventing nurses from assisting patients with ADs [advance directives] is the lack of perceived authority that nurses have in decisions about EOL [end-of-life] care for their patients. Traditionally, the physician has discussed ADs with patients. Nurses view their role in decisions regarding palliative care to be limited and indirect.46(p549)
Contextualized knowledge
Although the study participants fully understood the value of an interdisciplinary team to deliver a palliative approach, they emphasized the need for empowerment among the nursing members of such teams as a high priority. In particular, they saw the role of the registered nurse as integral to the implementation of a palliative approach by establishing the plan of care and providing leadership across the spectrum of nursing services. They were particularly emphatic about the need for empowered nursing engagement in anticipatory care and advocating for informed decision making. As one RN key informant explained it, nursing leadership in initiating these conversations was essential to effecting a palliative approach:
I think we have to start the conversation. I think that's where our accountability is. And not be afraid to say, “You know what? People die. People die when they're in healthcare.” Our responsibility is to make sure that we support people throughout every step of their life from wherever their life takes them.
Another aspect of the nursing role highlighted by the key informants was the capacity to support all members of the nursing care team to work at their full scope of practice. They considered this a fundamental feature of a palliative approach in practice and in several instances provided examples of how this was being enacted within the care process redesign initiatives underway in their settings. As one explained,
Some of the tools or things that we're doing now as part of the care delivery model redesign are absolutely imperative to move this way in terms of providing [a palliative approach]. The intent is to get to a place where each healthcare professional works to the maximum of their scope.
They felt that, for all members of the nursing spectrum to practice at full scope, an affirmation of the various nursing roles at the level of leadership and other health team members was essential:
So part of it is getting everybody to understand each other's role; part of it is getting everybody to work to their optimum scope; part of it is helping people to see the need to communicate with each other and to look outside their departmental box or their individual role and service provision.
The informants further acknowledged that a palliative approach necessitated shifts in the roles of both the patient and the family:
If we're shifting the scope and responsibilities of care providers themselves, we have to shift the scope and understanding of the patient and give them some responsibility too.... Informed people are more able to have care aligned with values and beliefs, provide information, share decision, shared a care plan—a “living care plan.”
This focus on empowerment extended beyond the various professional nursing role categories and included the nonprofessional health care workers who also play a key role in nursing care, especially within home and residential care contexts. Nurses viewed themselves as having an important role to play in recognizing, empowering, and facilitating the work of these nonprofessional health care workers whose contributions to patient care were viewed as centrally important. Reflecting on the experience of implementing a palliative approach in our home health demonstration project, one nurse explained:
I think we can come in and do our approach or set up a wonderful care plan in my perspective, but unless it's carried through all the way down, it's not going to really make any difference to the client and the family. And there's a trust that's important, that needs to be there. And that building of trust is usually on the confidence of the workers in the situation to know what to do, to be supported and to feel that they can handle it. So a lot of it has to happen at a layer a lot lower than us just because mainly we just do the planning, but they do the implementation.
Thus, while the literature on nursing roles focused primarily on advanced practice skill sets and team role clarification, the contextual knowledge emphasized the primary role of nursing, and the requisite conditions for empowering and supporting the full spectrum of nursing to enact a palliative approach at the everyday point of care. Rather than considering nursing as but one small component of a large multidisciplinary configuration of professionals, they considered the culture of the internal nursing work environment to be of utmost importance. As one explained:
I don't know that it's so important how many RNs, how many LPNs, how many care aides you have. It's how cohesive is your team and if your team is working well together, I think that's what's most important.
The composition of nursing staffing and skill mix must be such that it can support a person-centered and needs-based orientation within the appropriate care context.
Practice support for a palliative approach in nursing
General knowledge
For the purposes of our literature review, the concept of practice support was broadly defined and included coaching, mentorship, education, guidelines and pathways for care, and other clinical tools such as tools for patient identification, needs assessment, and decision making related to goals of care. The available evidence suggests that there is considerable interest across the various care settings in developing and implementing practice supports to facilitate the integration of a palliative approach.
We found evidence of numerous educational initiatives focusing specifically on nursing, or on interdisciplinary teams that included nurses, in residential, acute, and community care settings.50–59 These educational initiatives were either broadly about palliative care, for example, the End-of-Life Nursing Education Consortium,60 or else focused on particular conditions or sectors of care, such as dementia care51 or residential care.61 Despite the frequency with which such educational initiatives were advocated in the literature, we found little agreement on the essential content, learning outcomes, and didactic methods of an effective education for a palliative approach in nursing. In addition, it was not always clear how educational initiatives facilitating a palliative approach were differentiated from education on specialist palliative care and end-of-life care. We found little discussion in the literature as to whether such educational initiatives should be focused exclusively on nursing or on interdisciplinary teams.
Beyond education, we found considerable emphasis on the use of practice supports in the implementation of a system change such as the integration of a palliative approach. This was particularly apparent in the wide variety of tools developed to facilitate changes in care processes. The scope of these tools is articulated in Petrova et al's discussion of the implementation of the GSF in primary care:
Many facilitators worked on adapting and improving the paperwork and extending the range of tools and resources available to support implementation of the framework. They developed, for instance, out-of-hours handover forms, medication charts with advice on prescribing, audit tools, IT systems to support computer-based palliative care registers, district nurse care plans, palliative care pathways and bereavement leaflets.38(p44)
Pathways and guidelines for the care of specific patient populations using a palliative approach have been developed for use by nurses and interdisciplinary teams.62–64 Examples include a neurological care pathway,65 a Supportive Care Pathway for use in acute care,64 and guidelines for amyotrophic lateral sclerosis.66 We also noted practice support tools to guide interdisciplinary care for the imminently dying patient intended to bring “best practice in hospice care” to the acute or nursing home settings, such as have been studied in the United Kingdom, the United States, Italy, and Australia.67–76 The most commonly referenced of these pathways is the United Kingdom's Liverpool Care Pathway (LCP). The available body of research also describes the importance of education prior to implementation of the pathway and the need to adapt it to different care contexts73 or different illnesses, as is exemplified by the modification of the LCP for renal disease.72,76
Despite the enthusiasm for pathways and guidelines, the literature also confirms that there are challenges associated with implementation. Allen et al demonstrated that the Australian Government Department of Health and Aging's Guidelines for a Palliative Approach in Residential Aged Care77 were neither known nor implemented within a particular care home and thus concluded “that policy is rhetoric not reality in providing a planned trajectory of care for residents and their family members.”78(p174) In addition to the limited implementation of guidelines, there is an emerging argument that they could potentially lead to unintended consequences. For example, having conducted a systematic review using Cochrane collaborative methodology on pathways to manage end-of-life care, Chan and Webster concluded that although they were often considered “gold standard,” one could speculate possible adverse effects such as “premature diagnosis of imminent death” or “the care pathway masking the signs in improvement in patients.”79(p3) Thus Chan advocated the need for well-designed controlled studies to evaluate the use of such pathways before concluding their utility as a practice support.
Contextualized knowledge
From our focus groups and key informants, we learned that integration of practice supports for a palliative approach requires an understanding among clinicians of the tenets of a palliative approach and broad endorsement of its inherent values and beliefs throughout the health care system. Education, personal support such as debriefing, and input from interdisciplinary team members, including palliative care consultation teams, were viewed as important supports for their practice. Furthermore, beyond simply imparting theoretical knowledge, they felt that education must be integrated within a comprehensive knowledge translation strategy. As one key informant explained:
We can't leave nurses isolated in trying to do this work, right? So they have to have people that they can turn to that have the knowledge or are willing to learn along with them and support them and take that time. And that's right at the front line, to be ready with that patient, client, family, with that physician, with all of those team pieces. It has to be right down at that level and not too far out theoretically.
They also pointed out that education needs to include patients and families, and not just health care professionals. A participant in our demonstration project explained:
What education do we provide to our communities about chronic disease management and life-limiting conditions [has to include] how to be ready and prepared and how to work with the health system around a life-limiting condition and who you can have conversations with about your end-of-life planning and how to take charge of your end-of-life.
Key informants and symposium participants stressed the importance of having leaders capable of supporting the integration of a palliative approach by offering opportunities for professional development, organizing and managing day-to-day operations, and providing experience and mentorship. At the practice level, they proposed that the shift to a palliative approach could be promoted through education and mentoring of interprofessional teams who embrace a collaborative, person-centered palliative approach. They also believed that this shift would have to be reflected in shared care planning. To facilitate a shared care plan, they recommended the use of clinical tools and documents that cross all sectors and can be embedded in the daily workflow of the interprofessional teams. “Like we have to work together as a team. Whether you're in acute care working or you're residential, we have to be on the same page for the goal of care of the patient.” To assure care recipients that their goals of care are being met, they claimed it was essential to create a system that empowers direct care nurses to know patients' wishes and goals of care:
The key about having a care plan and communication that travels across sectors with these chronically ill people that may only be in hospital for 7 days, it's more about them than the team around them. [We need to] equip that team. They need the information flow. And then that has to inform the next team.
Findings from focus groups within each demonstration project not only confirmed the value of a palliative approach, but also reinforced the need to contextualize the language and strategies to each setting. Although changes at the wider system level are clearly needed, our demonstration projects confirmed that practice change could be made at the local level and illustrated the value of practice support tools that were created by and thus meaningful to the team within a particular setting. For example, the residential care setting project focused on the work of the interdisciplinary team, using daily “huddles” to identify resident and family needs and concerns and engage in goals of care conversations. The home health case managers reflected on client and family needs that were not well met by the current system, and developed strategies to work collaboratively with home care nurses in planning care, to “wrap the care around the person.”
Thus, although the general and contextual knowledge sources confirm the importance of practice supports, the evidentiary basis for such supports is not yet well developed, and it is unknown whether there may be limitations or unintended consequences. As this evidence evolves, clinicians engaged in implementing practice supports for a palliative approach in various care settings are recognizing the importance of understanding the complex health care environments within which practice supports are taken up or resisted. While there is agreement that practice supports are essential, it is also apparent that they are not in themselves sufficient to enact meaningful change such as is required to embed a palliative approach to the care of patients with chronic conditions across settings.
DISCUSSION
The findings from our multifaceted study demonstrate the relevance of an integrated approach to literature synthesis (general knowledge) and concurrent analyses of contextualized knowledge. Although the value of a palliative approach is supported in the literature, contextualized knowledge informs how general knowledge about a palliative approach can be integrated within different nursing care settings and cultures. The findings reveal the importance of embedding the values and tenets of a palliative approach into diverse contexts, the integral roles that nurses have in working with an interdisciplinary team to integrate a palliative approach in particular practice settings, and the need for practice supports to facilitate that embedding and integration. However, it is important to recognize that the literature synthesis, albeit substantial in scope, was of an interpretative nature and constrained by the sources included in our review. Similarly, contextualized knowledge is limited to the provincial health care environment in which the study took place. It is likely that approaches to nursing care delivery and practice support tools will need to be further contextualized in other countries and health care systems. Clearly further research in different health care sectors (including primary care) and systems is needed to enrich understandings regarding the integration of a palliative approach to best support the needs of people who have chronic life-limiting conditions and their families.
Findings from this study inform the ways in which nursing can have a significant role in enhancing care for this population through a palliative approach. Based upon these findings, a 3-faceted approach is necessary. First, there needs to be a concerted focus on knowledge translation regarding the fundamental values and tenets that constitute a palliative approach. A palliative approach is ultimately a person-centered approach to care. Therefore, knowledge translation efforts toward a palliative approach will be fulfilling an important mandate within health care internationally. Second, there needs to be a focus on empowering those in the care delivery team whose contributions have been less visible. In particular, the unregulated workforce are essential partners in care delivery to this population. These important partners must be part of the integration of a team-based approach and necessary practice supports. Third, the scaffolding of practice supports is critical to this envisioned shift. Nurses require supports that facilitate high-quality care and communication such as education, clinical pathways, assessment instruments, and documentation mechanisms. However, these supports can be implemented only in concert with fundamental values that are in keeping with a palliative approach. We need to be cautious about the implementation of these supports without due attention to shifts in philosophy and empowerment. Important lessons were learned from the implementation of the LCP about the importance of the underlying philosophy and values.80,81
Overall, given the results of our synthesis of general and contextualized knowledge, we are confident that the ideas embedded in a palliative approach to care hold tremendous promise for meaningful advances in transforming nursing care delivery so that it more fully meets the needs of the population with chronic and potentially life-limiting conditions, across settings and contexts of care.
Footnotes
Funding for this research was provided by the Michael Smith Foundation for Health Research (MSFHR), British Columbia Nursing Research Initiative (BCNRI), PJ NRP 00050 (11-2). Sawatzky holds a Canada Research Chair (Tier 2) funded by the Canadian Institutes of Health Research. The funders had no involvement in study design or other research activities or in writing or submitting this report.
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Bacon J. The Palliative Approach: Improving Care for Canadians With Life-Limiting Illnesses. Ottawa, Ontario: Canadian Hospice Palliative Care Association; Published 2013. Accessed August 15, 2013. [Google Scholar]
- 2.Kristjanson LJ, Walton J, Toye C. End-of-life challenges in residential aged care facilities: a case for a palliative approach to care. Int J Palliat Nurs. 2005;11(3):127–129. [PubMed] [Google Scholar]
- 3.Stajduhar KI, Tayler C. Taking an “upstream” approach in the care of dying cancer patients: the case for a palliative approach. Can Oncol Nurs J. 2014;24(3):144–153. [PubMed] [Google Scholar]
- 4.Stajduhar KI. Chronic illness, palliative care, and the problematic nature of dying. Can J Nurs Res. 2011;43(3):7–15. [PubMed] [Google Scholar]
- 5.Sawatzky R, Porterfield P, Lee J, et al. Conceptual foundations of a palliative approach: a knowledge synthesis. BMC Palliat Care. 2016;15(5):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Thorne S, Roberts D, Sawatzky R. Unravelling the tensions between chronic disease management and end-of-life planning. Res Theory Nurs Pract. 2016;30(2):91–103. [DOI] [PubMed] [Google Scholar]
- 7.Fakhoury W. Quality of palliative care: why nurses are more valued than doctors. Scand J Soc Med. 1998;26(2):25–26. [DOI] [PubMed] [Google Scholar]
- 8.Sawatzky R, Roberts D, Reimer-Kirkham S, Tayler C, Stajduhar K; iPANEL Team. Integration of a palliative approach in home, acute medical, and residential care settings: findings from a province-wide survey. Figshare. 2015. 10.6084/m9.figshare.1455949. [Google Scholar]
- 9.Thorne S, Sawatzky R. Particularizing the general: sustaining theoretical integrity in the context of an evidence-based practice agenda. Adv Nurs Sci. 2014;37(1):5–18. [DOI] [PubMed] [Google Scholar]
- 10.Pope C, Mays N, Popay J. Synthesizing Qualitative and Quantitative Health Evidence a Guide to Methods. Maidenhead, England: Open University Press, McGraw Hill Education; 2007. [Google Scholar]
- 11.Graham I, Tetroe J. How to translate health research knowledge into effective healthcare action. Healthc Q. 2007;10(3):20–22. [DOI] [PubMed] [Google Scholar]
- 12.Graham I, Tetroe J. The knowledge to action framework. In: Rycroft-Malone J, Bucknall T, eds. Models and Frameworks for Implementing Evidence-Based Practice: Linking Evidence to Action. Oxford, UK: Wiley-Blackwell; 2010:207–221. [Google Scholar]
- 13.British Columbia Ministry of Health. The Provincial End-of-Life Care Action Plan for British Columbia: Priorities and Actions for Health System and Service Redesign. Victoria, British Columbia, Canada: British Columbia Ministry of Health; 2013. [Google Scholar]
- 14.Thomas J, Brunton J, Graziosi S. EPPI-Reviewer 4: Software for Research Synthesis. London, UK: Social Science Research Unit, Institute of Education; 2010. [Google Scholar]
- 15.Thorne S. Interpretive Description. Walnut Creek, CA: Left Coast Press; 2008. [Google Scholar]
- 16.Armitage D, Evans J. Improving end stage dementia care: a practice development approach. Geriaction. 2005;23(2):25–29. [Google Scholar]
- 17.Boyd KJ, Worth A, Kendall M, et al. Making sure services deliver for people with advanced heart failure: a longitudinal qualitative study of patients, family carers, and health professionals. Palliat Med. 2009;23(8):767–776. [DOI] [PubMed] [Google Scholar]
- 18.Buxton KL, Stone RA, Buckingham RJ, Pursey NA, Roberts CM. Current and planned palliative care service provision for chronic obstructive pulmonary disease patients in 239 UK hospital units: comparison with the Gold Standards Framework. Palliat Med. 2010;24(5):480–485. [DOI] [PubMed] [Google Scholar]
- 19.Davison SN. End-of-life care preferences and needs: perceptions of patients with chronic kidney disease. Clin J Am Soc Nephrol. 2010;5(2):195–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gofton T, Jog M, Schulz V. A palliative approach to neurological care: a literature review. Can J Neurol Sci. 2009;36(3):296–302. [DOI] [PubMed] [Google Scholar]
- 21.Auer P. Primary care end-of-life planning for older adults with chronic illness. J Nurse Pract. 2008;4(3):185–191. [Google Scholar]
- 22.Janssen DJ, Engelberg RA, Wouters EF, Curtis JR. Advance care planning for patients with COPD: past, present and future. Patient Educ Couns. 2012;86(1):19–24. [DOI] [PubMed] [Google Scholar]
- 23.Thompson-Hill J, Hookey C, Salt E, O'Neill T. The supportive care plan: a tool to improve communication in end-of-life care. Int J Palliat Nurs. 2009;15(5):250–255. [DOI] [PubMed] [Google Scholar]
- 24.Young M, Brown M, Brooksbank M, et al. Feedback from consumers brings COPD model of care back to basics. Respirology. 2011;16(suppl 1):85. [Google Scholar]
- 25.Schofield P, Carey M, Love A, Nehill C, Wein S. “Would you like to talk about your future treatment options?” Discussing the transition from curative cancer treatment to palliative care. Palliat Med. 2006;20(4):397–406. [DOI] [PubMed] [Google Scholar]
- 26.Forbes-Thompson S, Gessert CE. End of life in nursing homes: connections between structure, process, and outcomes. J Palliat Med. 2005;8(3):545–555. [DOI] [PubMed] [Google Scholar]
- 27.Boockvar KS, Meier DE. Palliative care for frail older adults: “There are things I can't do anymore that I wish I could....” JAMA. 2006;296(18):2245–2253. [DOI] [PubMed] [Google Scholar]
- 28.Ross MM, MacLean MJ, Cain R, Sellick S, Fisher R. End of life care: the experience of seniors and informal caregivers. Can J Aging. 2002;21(1):137–146. [Google Scholar]
- 29.Crawford G, Burgess T, Crockett A, et al. What are the care needs of patients with end stage COPD and are they being met? Respirology. 2010;15(suppl 1):A59. [Google Scholar]
- 30.Lawrence V, Samsi K, Murray J, Harari D, Banerjee S. Dying well with dementia: qualitative examination of end-of-life care. Br J Psychiatry. 2011;199(5):417–422. [DOI] [PubMed] [Google Scholar]
- 31.Ashton S, McClelland B, Roe B, Mazhindu D, Gandy R. End of life care for people with dementia: an evaluation of implementation of the GSF and LCP. Palliat Med. 2010;24(2):202. [Google Scholar]
- 32.Badger F, Clifford C, Hewison A, Thomas K. An evaluation of the implementation of a programme to improve end-of-life care in nursing homes. Palliat Med. 2009;23(6):828–838. [DOI] [PubMed] [Google Scholar]
- 33.Dale J, Petrova M, Munday D, Koistinen-Harris J, Lall R, Thomas K. A national facilitation project to improve primary palliative care: impact of the Gold Standards Framework on process and self-ratings of quality. Qual Saf Health Care. 2009;18(3):174–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hall S, Goddard C, Stewart F, Higginson IJ. Implementing a quality improvement programme in palliative care in care homes: a qualitative study. BMC Geriatr. 2011;11(1):31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.King N, Martin N, Bell D, Farrell S. Now nobody falls through the net—practitioners perspectives on the GSF for community palliative care. Palliat Med. 2005;19(8):619–627. [DOI] [PubMed] [Google Scholar]
- 36.Mahmood-Yousuf K, Munday D, King N, Dale J. Interprofessional relationships and communication in primary palliative care: impact of the Gold Standards Framework. Br J Adv Pract. 2008;58(549):256–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Munday D, Mahmood K, Dale J, King N. Facilitating good process in primary palliative care: does the Gold Standards Framework enable quality performance? Fam Pract. 2007;24(5):486–494. [DOI] [PubMed] [Google Scholar]
- 38.Petrova M, Dale J, Munday D, Koistinen J, Agarwal S, Lall R. The role and impact of facilitators in primary care: findings from the implementation of the Gold Standards Framework for palliative care. Fam Pract. 2009;27(1):38–47. [DOI] [PubMed] [Google Scholar]
- 39.Shaw K, Clifford C, Thomas K, Meehan H. Improving end-of-life care: a critical review of the Gold Standards Framework in primary care. Palliat Med. 2010;24(3):317–329. [DOI] [PubMed] [Google Scholar]
- 40.Thomas K, Noble B. Improving the delivery of palliative care in general practice—an evaluation of the first phase of the GSF. Palliat Med. 2007;21(1):49–53. [DOI] [PubMed] [Google Scholar]
- 41.Walshe C, Caress A, Chew-Graham C, Todd C. Implementation and impact of the Gold Standards Framework in community palliative care: a qualitative study of three primary care trusts. Palliat Med. 2008;22(22):6. [DOI] [PubMed] [Google Scholar]
- 42.British Columbia Ministry of Health. BC Palliative Care Benefits: Prescriber Guide. Version 2.5. Victoria, British Columbia, Canada: British Columbia Ministry of Health; 2015. [Google Scholar]
- 43.London MR, McSkimming S, Drew N, Quinn C, Carney B. Evaluation of a Comprehensive, Adaptable, Life-Affirming, Longitudinal (CALL) palliative care project. J Palliat Med. 2005;8(6):1214–1225. [DOI] [PubMed] [Google Scholar]
- 44.Mahler A. The clinical nurse specialist role in developing a geropalliative model of care. Clin Nurse Spec. 2010;24(1):18–23. [DOI] [PubMed] [Google Scholar]
- 45.Senior L, Hubbard G. Integrated malignant and nonmalignant palliative care in Scotland. Br J Community Nurs. 2010;15(6):284–291. [DOI] [PubMed] [Google Scholar]
- 46.Cohen A, Nirenberg A. Current practices in advance care planning: implications for oncology nurses. Clin J Oncol Nurs. 2011;15(5):547–553. [DOI] [PubMed] [Google Scholar]
- 47.Efstathiou N, Clifford C. The critical care nurse's role in end-of-life care: issues and challenges. Nurs Crit Care. 2011;16(3):116–123. [DOI] [PubMed] [Google Scholar]
- 48.Ceccarelli CM, Castner D, Haras MS. Advance care planning for patients with chronic kidney disease—why aren't nurses more involved? Nephrol Nurs J. 2008;35(6):553–557. [PubMed] [Google Scholar]
- 49.Tilden VP, Thompson S. Policy issues in end-of-life care. J Prof Nurs. 2009;25(6):363–368. [DOI] [PubMed] [Google Scholar]
- 50.Aoun S, McConigley R, Kristjanson L, et al. Palliative care for people with motor neurone disease: how effective is an educational program for service providers? Amyotroph Lateral Scler. 2011;12(suppl 1):69–77. [Google Scholar]
- 51.Arcand M, Monette J, Monette M, et al. Educating nursing home staff about the progression of dementia and the comfort care option: impact on family satisfaction with end-of-life care. J Am Med Dir Assoc. 2009;10(1):50–55. [DOI] [PubMed] [Google Scholar]
- 52.Coyne P, Paice JA, Ferrell BR, Malloy P, Virani R, Fennimore LA. Oncology end-of-life nursing education consortium training program: improving palliative care in cancer. Oncol Nurs Forum. 2007;34(4):801–807. [DOI] [PubMed] [Google Scholar]
- 53.Ersek M, Kraybill BM, Hansen NR. Evaluation of a Train-the-Trainer program to enhance hospice and palliative care in nursing homes. J Hosp Palliat Nurs. 2006;8(1):42–49. [Google Scholar]
- 54.Ferrell BR, Borneman T. Community implementation of home care palliative care education. Cancer Pract. 2002;10(1):20–27. [DOI] [PubMed] [Google Scholar]
- 55.Gnaedinger N, Robinson J, Murray K. Preliminary outcomes of the dementia difference workshop at the Lodge at Broadmead, Victoria, BC. J Palliat Care. 2010;26(2):130–132. [PubMed] [Google Scholar]
- 56.Grant M, Hanson J, Mullan P, Spolum M, Ferrell B. Disseminating end-of-life education to cancer centers: overview of program and of evaluation. J Cancer Educ. 2007;22(3):140–148. [DOI] [PubMed] [Google Scholar]
- 57.Grossman S. Educating RNs regarding palliative care in long-term care generates positive outcomes for patients with end-stage chronic illness. J Hosp Palliat Nurs. 2007;9(6):323–328. [Google Scholar]
- 58.Hahn JE, Cadogan MP. Development and evaluation of a staff training program on palliative care for persons with intellectual and developmental disabilities. J Policy Pract Intellect Disabil. 2011;8(1):42–52. [Google Scholar]
- 59.Kalisiak A, Hedlund S, Grandara E. Positive impact: integrating palliative care education and support in a community oncology practice (728). J Pain Symptom Manage. 2011;41(1):289. [Google Scholar]
- 60.Ferrell BR, Virani R, Grant M, et al. Evaluation of the End-of-Life Nursing Education Consortium undergraduate faculty training program. J Palliat Med. 2005;8(1):107–114. [DOI] [PubMed] [Google Scholar]
- 61.Ersek M, Grant MM, Kraybill BM. Enhancing end-of-life care in nursing homes: Palliative Care Educational Resource Team (PERT) program. J Palliat Med. 2005;8(3):556–566. [DOI] [PubMed] [Google Scholar]
- 62.Davidson PM, Paull G, Introna K, et al. Integrated, collaborative palliative care in heart failure: The St. George heart failure service experience 1999-2002. J Cardiovasc Nurs. 2004;19(1):68–75. [DOI] [PubMed] [Google Scholar]
- 63.Johnston B, Ostlund U, Brown H, Chochinov H. The development of a dignity care pathway (DCP) for use by community nurses with people receiving end of life care at home. Eur J Cancer. 2011;47(suppl 1):S296. [Google Scholar]
- 64.Main J, Whittle C, Treml J, Woolley J, Main A. The development of an Integrated Care Pathway for all patients with advanced life-limiting illness—The Supportive Care Pathway. J Nurs Manag. 2006;14(7):521–528. [DOI] [PubMed] [Google Scholar]
- 65.Brown JB, Sutton L. A neurological care pathway for meeting the palliative care needs of people with life-limiting neurological conditions. Int J Palliat Nurs. 2009;15(3):120–127. [DOI] [PubMed] [Google Scholar]
- 66.Bede P, Oliver D, Stodart J, et al. Palliative care in amyotrophic lateral sclerosis: a review of current international guidelines and initiatives. J Neurol Neurosurg Psychiatry. 2011;82(4):413–418. [DOI] [PubMed] [Google Scholar]
- 67.Bailey FA, Burgio KL, Woodby LL, et al. Improving processes of hospital care during the last hours of life. Arch Intern Med. 2005;165(15):1722–1727. [DOI] [PubMed] [Google Scholar]
- 68.Bookbinder M, Blank AE, Arney E, et al. Improving end-of-life care: development and pilot-test of a clinical pathway. J Pain Symptom Manage. 2005;29(6):529–543. [DOI] [PubMed] [Google Scholar]
- 69.Constantini M, Ottonelli S, Canavacci L, Pellegrini F, Beccaro M. The effectiveness of the Liverpool Care Pathway in improving end of life care for dying cancer patients in hospital. A cluster randomised trial. BMC Health Serv Res. 2011;11:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Di Leo S, Beccaro M, Finelli S, Borreani C, Constantini M. Expectations about and impact of the Liverpool Care Pathway for the dying patient in an Italian hospital. Palliat Med. 2011;25(4):293–303. [DOI] [PubMed] [Google Scholar]
- 71.Duffy A, Woodland C. Introducing the Liverpool Care Pathway into nursing homes. Nurs Older People. 2006;18(9):33–36. [DOI] [PubMed] [Google Scholar]
- 72.Hinton V, Fish M. A care pathway for the end of life in a renal setting. J Renal Care. 2006;32(3):160–163. [DOI] [PubMed] [Google Scholar]
- 73.Jackson K, Mooney C, Campbell D. The development and implementation of the pathway for improving the care of the dying in general medical wards. Intern Med J. 2009;39(39):10. [DOI] [PubMed] [Google Scholar]
- 74.Mathews K, Finch J. Provision of palliative care education in nursing homes. Nurs Times. 2006;102(5):36. [PubMed] [Google Scholar]
- 75.McNicholl MP, Dunne K, Garvey A, Sharkey R, Bradley A. Using the Liverpool Care Pathway for a dying patient. Nurs Stand. 2006;20(38):46–50. [DOI] [PubMed] [Google Scholar]
- 76.Wenham S, Hobson K, Farrington K, Gomm S. Use of the Liverpool Care Pathway in patients dying with advanced chronic kidney disease: a survey of hospital renal services in England. Palliat Med. 2010;24(suppl 4):S174. [Google Scholar]
- 77.Edith Cowan University. Guidelines for a Palliative Approach in Residential Aged Care. Canberra, Australia: Australian Government; 2006. [Google Scholar]
- 78.Allen S, O'Connor M, Chapman Y, Francis K. The implications of policy on delivering a palliative approach in residential aged care: rhetoric or reality? Contemp Nurse. 2008;29(2):174–183. [DOI] [PubMed] [Google Scholar]
- 79.Chan RJ, Webster J. End-of-life care pathways for improving outcomes in caring for the dying. Cochrane Database Syst Rev. 2013;20(1):CD008006. [DOI] [PubMed] [Google Scholar]
- 80.Neuberger J, Guthrie C, Aaronovitch D, et al. More Care, Less Pathway: A Review of the Liverpool Care Pathway. UK Department of Health; 2013:63 http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/212450/Liverpool_Care_Pathway.pdf. Published July 15, 2013. Accessed November 24, 2015. [Google Scholar]
- 81.Venkatasalu MR, Whiting D, Cairnduff K. Life after the Liverpool Care Pathway (LCP): a qualitative study of critical care practitioners delivering end-of-life care. J Adv Nurs. 2015;71(9):2108–2118. [DOI] [PubMed] [Google Scholar]