Abstract
Mural thrombus in non-atherosclerotic or aneurysmatic thoracic aorta is a relatively uncommon entity. Currently there is no consensus on the appropriate therapeutic algorithm of its management. We aim to present the current knowledge on the treatment of thoracic aorta mural thrombi (TAMT) in minimally atherosclerotic vessels and we hope that the juxtaposed discussions will shed light on the uncharted waters regarding this rare syndrome. The MEDLINE/PubMed database was searched for publications with the medical subject “aortic mural thrombus” and keywords “thoracic”, “embolism”, “normal vessel”, “minimally atherosclerotic vessel” or “treatment”. We restricted our search to English language, till January 2017. The electronic literature search yielded 23 reports that were deemed appropriate for further analysis. Anticoagulation is the standard of care for the treatment of the thrombus whereas surgical and interventional treatment seems to be related with increased mortality and lower recurrence rates. TAMT treatment is controversial. Anticoagulants are the mainstay of treatment but surgery seems to gain ground in several settings as an only therapy or a combined treatment modality. More data are needed on the role of novel oral anticoagulants and endografts.
Keywords: Thoracic aorta; mural thrombus; minimally atherosclerotic; normal-appearing; endovascular, anticoagulants
Introduction
Thoracic aorta mural thrombus (TAMT) in the absence of atherosclerotic or aneurysmatic disease is characterized as “cryptogenic” and represents a relatively uncommon entity. Although the cause of aortic thrombus is idiopathic in many clinical situations, pro-thrombotic conditions such as primary polycythemia vera (1), antiphospholipid antibody syndrome (2), hypercoagulable states (2-5), malignant diseases (infiltration of aortic wall, paraneoplastic syndrome due to malignancy in visceral organs) (6,7), primary endothelial disorders or even iatrogenic causes (intra-aortic balloon pumping) (4,6,7) have also been reported. In addition, heparin-Induced thrombocytopenia (HIT) (7), hyperhomocysteinemia (6,8) and familial dysfibrinogenemia (6) have been suggested as well.
The first case of TAMT was published in 1967 (9). Since then, few case reports or cases series of patients with “cryptogenic” thrombus are available in the literature (10-13). Advanced imaging modalities, such transthoracic echocardiography (TTE), trans-esophageal echocardiography (TEE), and the computed tomography (CT)/magnetic resonance imaging (MRI) have increased the diagnostic accuracy of this entity and can partially explain the increased number of cases diagnosed the recent years (10,14,15).
Currently there is no consensus on the appropriate therapeutic algorithm of managing this entity. Factors such as the presenting symptoms, the age and performance status of the patient but also thrombus-related characteristics such as the location and the morphology seem to be crucial for the design of any therapeutic plan.
We aim to present the current knowledge on the treatment of TAMT in minimally atherosclerotic vessels and we hope that the juxtaposed discussions will shed light on the uncharted waters; it is to be hoped that some global insights will emerge.
Methods
The MEDLINE/PubMed database was searched for publications with the medical subject “aortic mural thrombus” and keywords “thoracic”, “embolism”, “normal vessel”, “minimally atherosclerotic vessel” or “treatment”. The search was conducted both on basis of the MeSH tree and as a text search. We restricted our search to English language, till January 2017. We sought to review all updates on the subject after the introduction of endovascular surgery in the treatment armamentarium.
Definitions
In our review, we searched all the cases of “cryptogenic” aortic mural thrombus. As “cryptogenic” was defined the thrombus attached to the aortic wall in the absence of any atherosclerotic or aneurysmatic aortic disease and a cardiac source of embolus. The thrombus could be either sessile (eccentric or concentric thrombus with no free floating component) or pedunculated (with a free-floating intraluminal segment of variable length). We restricted our search only in type II thrombus (localized in descending thoracic aorta (DTA), distal to left subclavian artery up to celiac artery), a classification that has been recently proposed by Verma et al. (16). Moreover, symptomatic was defined the patient who has experienced embolization either to the viscera circulation or most commonly the upper/lower extremities.
Results
The electronic literature search yielded 23 reports that were presented in Table S1.
The role of the characteristics of the thrombus
The etiology of TAMT is not clear. Factors such as young age, smoking, family history of atherosclerotic disease, malignancy, hypercoagulable state, primary endothelial disorders or even iatrogenic causes may be crucial for the appropriate treatment modality (5,13,21,30,37-39). Moreover, the morphological (sessile vs. pedunculated) and dynamic (mobile/floating vs. fixed) properties of the thrombus, the size of the thrombus, the length of the aortic involvement and the site of thrombus could play a role on the embolic phenomena and they deserve special attention to defend this clinical situation. The most common site of thrombus consistently reported in almost all cases is the zone between the distal aortic arch and DTA (74%) without evident cause followed by the abdominal (14%) and the ascending aorta (12%) (16). Embryologic defects at the aortic isthmus and shear, bending attributed to aortic trauma during blunt chest injuries have also been reported (5,30,40).
So the appropriate management ranges from anticoagulation to surgery (open/endovascular) keeping in mind the aforementioned factors and the patient’s general health status.
Anticoagulation as standard of care
Anticoagulation has been proposed as the primary modality of treatment by several authors with complete resolution of aortic thrombus, thus favoring a non-surgical approach (3,6,13,14,28). However, more than 25% of the patients experienced secondary aortic surgery to treat recurrence of peripheral arterial embolization or persistence or recurrence of aortic mural thrombus. Recurrent embolization significantly increases the risk of major amputation and the life-threatening visceral ischemia (16,21). The proposed anticoagulant treatment is still unclear. Some authors published their experience using unfractionated heparin followed by lifelong anticoagulants (coumadin derivates) in case of hypercoagulable states or malignant diseases. On the other hand, aspirin was maintained only in cases without hypercoagulable/malignant states and normal findings on follow-up CT aortography (16). The duration of oral anticoagulation is not clear either. This discrepancy in the literature varies from short duration until the symptoms resolve to lifelong (18,41-43). In a review of 23 cases, anticoagulants achieved complete thrombus resolution occurred in 74% of the cases (11,13,20,22,26,35).
The role in thrombolysis in the treatment of TAMT
Minimally invasive options such as catheter aspiration/systemic or catheter-directed thrombolysis and thrombectomy using an aortic balloon catheter have been described with varying success rates (10,44). Although, the main complication of this approach was the high risk of distal embolization during the procedure itself and the no reliability of complete removal or exclusion of thrombus (10,44). Reber et al. (10), discussed the underestimated potential of embolic events after thrombolysis due to the liberation of thrombi into the bloodstream and thus causing massive embolization. Similarly, a recent study (17) reported a case of massive distal embolization and death after streptokinase treatment in a patient with TAMT.
Surgery as the last resort of treatment in TAMT
Surgical treatment is reserved for patients who fail to respond in anticoagulants. This method has the advantage that the aortic wall could be evaluated during the procedure, which may be of diagnostic utility in this relatively unknown entity. Surgical options include thrombectomy with or without resection of the minimally atherosclerotic plaque, with repair of the aorta using either Dacron or polytetrafluoroethylene (PTFE) graft (17). Another study (19) suggested that the surgery should be considered for non-responders after 2 weeks of anticoagulation with heparin on therapeutic doses. Additional to the failed anticoagulant treatment, mobile thrombi, large thrombi and recurrent embolisms have been proposed as indications for surgical approach (45). However, the surgical options are not complication-free with a reported mortality of 2.6% (19) and perioperative complications ranging from 28.9% to 71% (45,46). This was the main reason why some investigators do not consider operative management of aortic thrombus as first-line management (25,31).
Endovascular treatment as a new tool in the therapeutic armamentarium
Endovascular stenting has been recently suggested as a therapeutic option for TAMT (23,24,27,29,30,32-34,36,47). Several publications reported their results with decrease of the size of residual thrombus and recurrent embolization in comparison to anticoagulation alone (27,29,34,36). Another benefit of the endovascular approach is the fact that it facilitates peripheral embolectomy through the same surgical access. In addition, fewer perioperative complications in comparison to open surgical thrombectomy have been reported (40). The selection of the appropriate stent for exclusion of TAMT has also been described in the literature with the bare metal stents (BMS) and stent grafts (SG) to be the most common. BMS are characterized from low radial force and a closed-cell design to be effective for TAMT lesions. Closed-cell stents have a theoretical advantage of preserving flow to the arteries supplying the anterior spinal cord and lowering the risk of spinal cord ischemia (16).
The presence of symptoms and its role to therapeutic plan
Owing to rarity of the TAMT, no definitive consensus on treatment for symptomatic and asymptomatic patients exists. In symptomatic emboli anticoagulation is indicated, not necessarily accompanied by surgery (16). When appropriate, endovascular approach seems to be feasible and safe. In cases of non-favorable thrombus location and size, open approach should be considered after taking into consideration the increased related early mortality and morbidity rates. In asymptomatic or patients with small thrombi, surgical or endovascular treatment should be avoided. Anticoagulation therapy, without surgical procedures has shown good outcomes (20,44).
The factor of age and the treatment choices
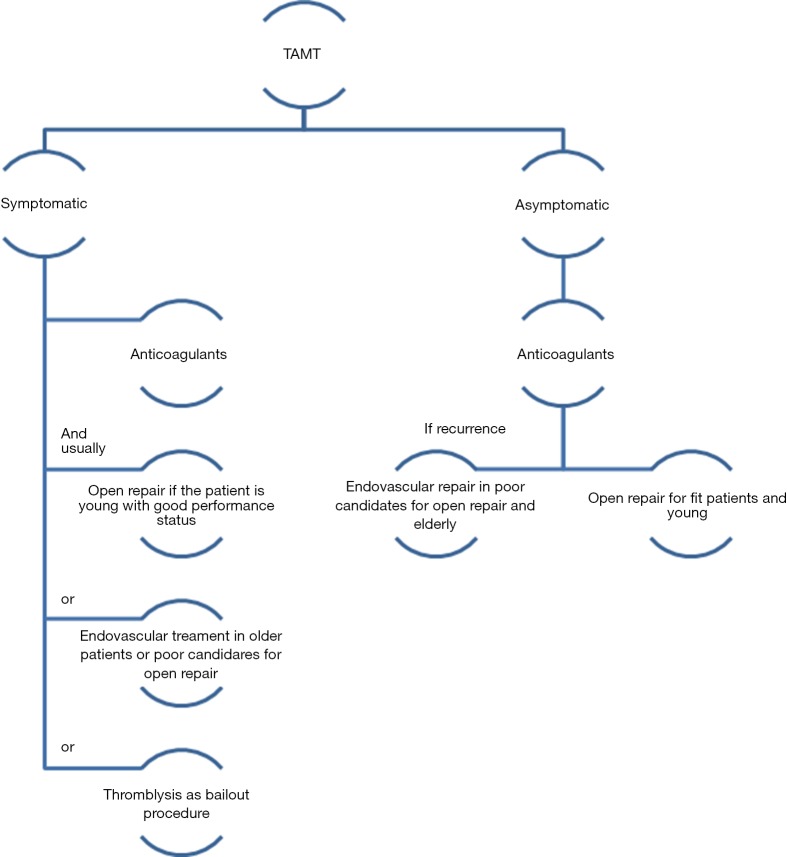
TAMT is likely an underestimated problem and should be suspected in those patients with peripheral arterial emboli and no identifiable cause (10,48,49). This is particularly true in younger patients with an established hypercoagulable state and a history of smoking. In these patients TAMT can be considered as a variant of atherosclerosis and characterized by pure and local clot formation (12). The diagnostic work-up of these patients should include a combination of imaging studies such as TEE, CT angiography (CTA) to thoroughly evaluate the heart and entire thoracic aorta. On the other hand, in elderly patients TAMT is suspected due to the presence of extensive atherosclerosis that can generate thrombus formation, which can liberate distal emboli. Figure 1 illustrates the proposed algorithm for the treatment of TAMT.
Figure 1.
Proposed algorithm for the treatment of TAMT. TAMT, thoracic aorta mural thrombus.
Discussion
TAMT in normal or minimally atherosclerotic aorta is a rare entity with potential dismal outcomes due to the generation of multiple or massive distal emboli (1-6). Nevertheless, even with the expanding availability of advanced diagnostic modalities (CT, TEE, MRI etc.), that have increased the sensitivity in detecting TAMT the last few years, the condition is today still very sporadically observed.
Because of its low incidence and thus, the lack of well-designed studies, there are not clear and valid guidelines on the treatment of TAMT. To date, anticoagulation should be considered as the standard of care in TAMT (19,28). There are reports of thrombus resolution with anticoagulation therapy (28,50,51) but its value is not validated with long-term results. The main drawback of the anticoagulants is the relative high recurrences varying from 26.4% to 50% (19,28,52,53) and a tendency for distal (limb) emboli (53). On the other hand, the role of antiplatelets as a therapeutic or recurrence-prevention modality is not well-established (19,28). Of interest would be the evaluation of novel oral anticoagulants in this setting, but no data are available to date.
Surgical intervention (open/endovascular), as primary or adjuvant treatment, is mainly indicated in cases where conservative treatment has failed or is contraindicated. Reports of open surgical treatment of symptomatic mobile thrombus with thrombectomy only (10,52,54) or graft replacement (19), is performed through a thoracotomy (10,19,52,54) or trans-abdominally (10), with simple aortic clamping or left atrial to femoral artery bypass (55). These interventions are associated with high mortality rate (2.6–5.7%) but lower than conservative treatment alone (6.2%) (45,53). So, there is discussion about whether it is necessary to treat a symptomatic mobile thrombus by such an invasive surgical approach in generally poor-conditioned patients.
The feasibility and efficiency of endografts as treatment modality on TAMT have been recently highlighted in the literature (23,24,27,29,30,32-34,36,47). This treatment modality mandates a vascular team with a high level expertise in endovascular surgery and the availability of necessary logistic programs for the appropriate planning, sizing and accurate deployment of the stent. There are a few considerations when deciding to treat TAMT with endografts. First of all, meticulous and careful handling of wires should take place to avoid chopping the thrombus and cause distal embolization. In this frame, angiography can be used to map the affected aortic segment and design the appropriate proximal and distal landing zones of the endograft. Finally, it is crucial to evaluate the mesenteric and lower extremity vessels after the procedure (55). Unfortunately, endovascular treatment does facilitate the histological analysis of the thrombus to offer insights about its origin, including malignancy. Moreover, there were no reports found about the cost-effectiveness of this therapeutic option and a comparative study would be compulsory.
Conclusions
Treatment of TAMT is still a matter of controversy. Each available treatment modality is correlated with crucial advantages but major drawbacks. Of course, they are not mutually exclusive. Instead, it is likely that a triple therapeutic approach may be needed to best treat TAMT. Anticoagulation is the mainstay of treatment related with effective thrombus resolution but also high recurrence rates. Open surgical approach is a definite treatment linked with increase early mortality and morbidity rates. Endovascular treatment could be an alternative to open approach with the drawback of high expenses and strict follow-up.
Table S1. Summary of the findings of studies included in the present review.
| Author | Year | Type of study | No. of patients | Age (years) | Gender | Presence of symptoms | Comorbidities | Localization of thrombus | Diagnosis tools | Relevant concomitant disease | Anticoagulation treatment acute/chronic | Surgical therapy | Endovascular therapy | Follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Crutchfield et al. (17) | 1998 | CR | 1 | 33 | M | Yes | NR | Descending aorta | TEE | NR | − | + | − | NR |
| Hahn et al. (18) | 1999 | CS | 1/6 with TAMT | 67 | F | Yes | Arthritis, HTN | From the posterior aortic arch to the descending aorta | CT, TEE | NR | + | − | − | 2 |
| Onwuanyi et al. (13) | 2001 | CR | 1 | 48 | F | Yes | HTN, DM,PAD | Aortic arch-descending aorta | TEE | + | − | − | 1 | |
| Choukroun et al. (19) | 2002 | RS | 2/9 with TAMT | mean age 49.2 (28–68) years | 6 M/3 F | Yes | HTN, heavy smokers (n=6/9) | Descending aorta (n=5) | TEE/CT/MRI | NR | + | + | − | 24 |
| Bowdish et al. (3) | 2002 | RS | 1/5 with TAMT | NR | NR | Yes | Asthma, DM, gout | Descending aorta | CT | Familial dysfibrinogenemia | + | + | − | 2 |
| Takagi et al. (20) | 2003 | CR | 1 | 49 | M | Yes | NR | Thoracoabdominal aorta | CT | NR | + | + | − | 3 |
| Hazirolan et al. (21) | 2004 | CR | 1 | 52 | F | Yes | HTN, DM, DVT | Descending aorta | CT/MRI | Protein S deficiency | + | + | − | NR |
| Mark et al. (22) | 2005 | CR | 1 | 57 | M | Yes | Smoker | Descending aorta | Thoracic aortogram, CT | Lung AdenoCa | + | − | − | 9 |
| Slabbekoorn et al. (6) | 2006 | CR | 1 | 38 | F | Yes | Smoker | Descending aorta | CT/MRI/TEE | Hyperhomocysteinemia | + | − | − | 2 |
| Piffaretti et al. (23) | 2008 | CR | 1 | 56 | M | Yes | Thymic hyperplasia, myasthenia gravis | Descending aorta | CT | Thrombophilia | − | − | + | 6 |
| Luebke et al. (24) | 2008 | CR | 1 | 47 | F | Yes | NR | Descending aorta | CT | NR | − | − | + | NR |
| Cañadas et al. (25) | 2008 | CS | 2/3 with TAMT | 47 & 52 | F/M | Yes | HTN, hypercholesterolemia, smoker | Aortic isthmus | TEE | NR | + | + | − | NR |
| Roche-Nagle et al. (26) | 2010 | CR | 1 | 42 | M | Yes | HTN, DM, DVT | Descending aorta | TEE, CT | V Leiden mutation | + | − | − | NR |
| Martens et al. (27) | 2010 | CS | 3 | 51/57/52 | F/M/M | Yes | smoking/ex-alcoholic, HTN | Descending aorta | TEE, CT/CT/CT | Antithrombin III/chronic myeloproliferative syndrome/NR | + | + | + | 1/NR/NR |
| Tsilimparis et al. (28) | 2011 | CS | 8 | mean age 55 (45–68) years | 7/8 (F) | Yes | NR | Descending aorta | CT, MRA, TEE | Hypercoagulable disorders & malignant diseases | + | + | − | 24 |
| Giovanni et al. (29) | 2011 | CS | 1/2 with TAMT | 45 | F | Yes | Negative medical history | Descending aorta | TEE/CTA/MRI | Uterine fibroma (F) | − | − | + | 36 |
| Morris et al. (30) | 2011 | CS | 1/2 with TAMT | 44 | F | Yes | HTN, menorrhagia, estrogen therapy | Aortic arch & descending aorta | CT | NR | − | − | + | NR |
| Krishnamoorthy et al. (31) | 2011 | CR | 1 | 63 | F | Yes | HTN, rheumatoid arthritis | Descending aorta | CT/TEE | Thrombocytosis, rheumatoid arthritis | − | + | − | NR |
| Trindade et al. (32) | 2012 | CR | 1 | 50 | F | Yes | IBD | Descending aorta | TEE, CT | Inflammatory bowel disease | − | − | + | 1 |
| Boufi et al. (33) | 2014 | RS | 10/13 with TAMT | mean age 53 (37–76) years | M (69.2%) | Yes | DM, HTN, smoking | Descending aorta (n=6) | CTA, TEE | Malignancy, steroid therapy, coagulation disorders | + | + | + | 32 |
| Lohrmann et al. (34) | 2014 | CR | 1 | 58 | F | Yes | None | Descending | CTA, TEE | NR | + | − | + | 6 |
| Maloberti et al. (35) | 2016 | CR | 1 | 40 | M | No | HTN, dyslipidaemia | Ductus arteriosus | CT, TEE | NR | + | − | − | 1 |
| Fukuhara et al. (36) | 2015 | CR | 1 | 62 | M | Yes | NR | Descending aorta | CT | Polycythemia vera | − | − | + | NR |
DM, diabetes mellitus; HTN, hypertension; CR, case report; RS, retrospective study; NR, not reported; CT, computerized tomography; CTA, computerized tomography angiography; TEE, transesophageal echo; IBD, inflammatory bowel disease; MRI, magnetic resonance imaging; DVT, deep vein thrombosis; PAD, peripheral artery disease; M, male; F, female; AdenoCa, adenocarcinoma; TAMT, thoracic aorta mural thrombus.
Acknowledgements
None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Bosma J, Rijbroek A, Rauwerda JA. A rare case of thromboembolism in a 21-year old female with elevated factor VIII. Eur J Vasc Endovasc Surg 2007;34:592-4. 10.1016/j.ejvs.2007.05.019 [DOI] [PubMed] [Google Scholar]
- 2.Thalheimer A, Fein M, Geissinger E, et al. Intimal angiosarcoma of the aorta: report of a case and review of the literature. J Vasc Surg 2004;40:548-53. 10.1016/j.jvs.2004.06.035 [DOI] [PubMed] [Google Scholar]
- 3.Bowdish ME, Weaver FA, Liebman HA, et al. Anticoagulation is an effective treatment for aortic mural thrombi. J Vasc Surg 2002;36:713-9. 10.1016/S0741-5214(02)00123-4 [DOI] [PubMed] [Google Scholar]
- 4.Aggeli C, Barberis VI, Vlachopoulos C, et al. Acute thoracic aortic thrombosis after intra-aortic balloon pumping. Eur J Echocardiogr 2006;7:175-6. 10.1016/j.euje.2005.04.001 [DOI] [PubMed] [Google Scholar]
- 5.Rafiq MU, Jajja MM, Qadri SS, et al. An unusual presentation of pedunculated thrombus in the distal arch of the aorta after splenectomy for B-cell lymphoma. J Vasc Surg 2008;48:1603-4. 10.1016/j.jvs.2007.05.062 [DOI] [PubMed] [Google Scholar]
- 6.Slabbekoorn M, Henneman OD, Geelhoed-Duijvestijn PH, et al. Mural aortic thrombus and peripheral embolisation in a patient with hyperhomocysteinaemia. Neth J Med 2006;64:20-2. [PubMed] [Google Scholar]
- 7.Antecol DH, Walley VM, Chan KL. Massive acute thrombosis of the descending thoracic aorta in heparin-associated thrombocytopenia and thrombosis. J Am Soc Echocardiogr 1994;7:550-2. 10.1016/S0894-7317(14)80016-3 [DOI] [PubMed] [Google Scholar]
- 8.Bakoyiannis C, Karaolanis G, Moris D, et al. Homocysteine as a risk factor of restenosis after carotid endarterectomy. Int Angiol 2015;34:166-71. [PubMed] [Google Scholar]
- 9.Oliver DO. Embolism from mural thrombus in the thoracic aorta. Br Med J 1967;3:655-6. 10.1136/bmj.3.5566.655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reber PU, Patel AG, Stauffer E, et al. Mural aortic thrombi: An important cause of peripheral embolization. J Vasc Surg 1999;30:1084-9. 10.1016/S0741-5214(99)70047-9 [DOI] [PubMed] [Google Scholar]
- 11.Hassan I, Zehr KJ, Freeman WK. A case of asymptomatic thoracic aorta mural thrombi. Ann Thorac Surg 2001;72:1735-7. 10.1016/S0003-4975(01)02612-1 [DOI] [PubMed] [Google Scholar]
- 12.Laperche T, Laurian C, Roudaut R, et al. Mobile thromboses of the aortic arch without aortic debris. A transesophageal echocardiographic finding associated with unexplained arterial embolism. The Filiale Echocardiographie de la Societe Francaise de Cardiologie. Circulation 1997;96:288-94. 10.1161/01.CIR.96.1.288 [DOI] [PubMed] [Google Scholar]
- 13.Onwuanyi A, Sachdeva R, Hamirani K, et al. Multiple aortic thrombi associated with protein C and S deficiency. Mayo Clin Proc 2001;76:319-22. 10.4065/76.3.319 [DOI] [PubMed] [Google Scholar]
- 14.Shapiro MD, Neilan TG, Jassal DS, et al. Multidetector computed tomography for the detection of left atrial appendage thrombus: a comparative study with transesophageal echocardiography. J Comput Assist Tomogr 2007;31:905-9. 10.1097/rct.0b013e31803c55e3 [DOI] [PubMed] [Google Scholar]
- 15.Romero J, Husain SA, Kelesidis I, et al. Detection of left atrial appendage thrombus by cardiac computed tomography in patients with atrial fibrillation: a meta-analysis. Circ Cardiovasc Imaging 2013;6:185-94. 10.1161/CIRCIMAGING.112.000153 [DOI] [PubMed] [Google Scholar]
- 16.Verma H, Meda N, Vora S, et al. Contemporary management of symptomatic primary aortic mural thrombus. J Vasc Surg 2014;60:1524-34. 10.1016/j.jvs.2014.08.057 [DOI] [PubMed] [Google Scholar]
- 17.Crutchfield EH, Katras T, Stanton PE., Jr The descending thoracic aorta as a source of arterial embolic disease: a case report. Am Surg 1998;64:1079-81. [PubMed] [Google Scholar]
- 18.Hahn TL, Dalsing MC, Sawchuk AP, et al. Primary aortic mural thrombus: presentation and treatment. Ann Vasc Surg 1999;13:52-9. 10.1007/s100169900220 [DOI] [PubMed] [Google Scholar]
- 19.Choukroun EM, Labrousse LM, Madonna FP, et al. Mobile thrombus of the thoracic aorta: diagnosis and treatment in 9 cases. Ann Vasc Surg 2002;16:714-22. 10.1007/s10016-001-0314-2 [DOI] [PubMed] [Google Scholar]
- 20.Takagi H, Mori Y, Umeda Y, et al. Surgical treatment of thoracoabdominal aortic mural and floating thrombi extending to infrarenal aorta. J Vasc Surg 2003;37:1324-7. 10.1016/S0741-5214(02)75466-9 [DOI] [PubMed] [Google Scholar]
- 21.Hazirolan T, Perler BA, Bluemke DA. Floating thoracic aortic thrombus in "protein S" deficient patient. J Vasc Surg 2004;40:381. 10.1016/j.jvs.2003.11.029 [DOI] [PubMed] [Google Scholar]
- 22.Mark HK, Ho NS, Tse CC, et al. Recurrent lower limb embolism from thoracic aortic mural thrombus: a rare presentation of occult malignancy. Hong Kong Med J 2005;11:503-6. [PubMed] [Google Scholar]
- 23.Piffaretti G, Tozzi M, Mariscalco G, et al. Mobile thrombus of the thoracic aorta: management and treatment review. Vasc Endovascular Surg 2008;42:405-11. 10.1177/1538574408324737 [DOI] [PubMed] [Google Scholar]
- 24.Luebke T, Aleksic M, Brunkwall J. Endovascular therapy of a symptomatic mobile thrombus of the thoracic aorta. Eur J Vasc Endovasc Surg 2008;36:550-2. 10.1016/j.ejvs.2008.07.004 [DOI] [PubMed] [Google Scholar]
- 25.Cañadas V, Vilacosta I, Luaces M, et al. Thrombosis of an apparently normal thoracic aorta and arterial embolism. Rev Esp Cardiol 2008;61:196-200. 10.1157/13116207 [DOI] [PubMed] [Google Scholar]
- 26.Roche-Nagle G, Wooster D, Oreopoulos G. Symptomatic thoracic aorta mural thrombus. Vascular 2010;18:41-4. 10.2310/6670.2009.00028 [DOI] [PubMed] [Google Scholar]
- 27.Martens T, Van Herzeele I, Jacobs B, et al. Treatment of symptomatic mobile aortic thrombus. Acta Chir Belg 2010;110:361-4. 10.1080/00015458.2010.11680635 [DOI] [PubMed] [Google Scholar]
- 28.Tsilimparis N, Hanack U, Pisimisis G, et al. Thrombus in the non-aneurysmal, non-atherosclerotic descending thoracic aorta--an unusual source of arterial embolism. Eur J Vasc Endovasc Surg 2011;41:450-7. 10.1016/j.ejvs.2010.11.004 [DOI] [PubMed] [Google Scholar]
- 29.Giovanni N, Daniela M, Giovanni M, et al. Endovascular treatment of thoracic aortic floating thrombus in patients presenting with acute lower limb ischemia. Int J Vasc Med 2011;2011:604362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Morris ME, Galinanes EL, Nichols WK, et al. Thoracic mural thrombi: a case series and literature review. Ann Vasc Surg 2011;25:1140.e17-21. 10.1016/j.avsg.2011.05.030 [DOI] [PubMed] [Google Scholar]
- 31.Krishnamoorthy V, Bhatt K, Nicolau R, et al. Transesophageal echocardiography-guided aortic thrombectomy in a patient with a mobile thoracic aortic thrombus. Semin Cardiothorac Vasc Anesth 2011;15:176-8. 10.1177/1089253211415123 [DOI] [PubMed] [Google Scholar]
- 32.Trindade VD, Bettio J, Albuquerque LC. Endovascular treatment of a mobile thrombus of the thoracic aorta in association with ulcerative colitis. Tex Heart Inst J 2012;39:592-3. [PMC free article] [PubMed] [Google Scholar]
- 33.Boufi M, Mameli A, Compes P, et al. Elective stent-graft treatment for the management of thoracic aorta mural thrombus. Eur J Vasc Endovasc Surg 2014;47:335-41. 10.1016/j.ejvs.2013.11.014 [DOI] [PubMed] [Google Scholar]
- 34.Lohrmann GM, Peters F. Thoracic endovascular aortic repair in a patient with mobile aortic thrombosis. Case Rep Vasc Med 2014;2014:302346. 10.1155/2014/302346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Maloberti A, Oliva F, De Chiara B, et al. Asymptomatic aortic mural thrombus in a minimally atherosclerotic vessel. Interact Cardiovasc Thorac Surg 2016;22:371-3. 10.1093/icvts/ivv349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fukuhara S, Tyagi S, Clarke-Pearson E, et al. Endovascular stent graft repair of thoracic aortic mural thrombus in a patient with polycythemia vera: a word of caution. Vascular 2015;23:89-92. 10.1177/1708538114525154 [DOI] [PubMed] [Google Scholar]
- 37.Losanoff JE, Richman BW, Amiridze N, et al. Floating thrombus of the thoracic aorta: a rare consequence of blunt trauma. J Trauma 2004;57:892-4. 10.1097/01.TA.0000046264.14796.14 [DOI] [PubMed] [Google Scholar]
- 38.Cogert G, Siegel RJ. Giant floating aortic thrombus: a rare finding on transesophageal echocardiography. Am J Cardiol 2007;99:739-40. 10.1016/j.amjcard.2006.09.126 [DOI] [PubMed] [Google Scholar]
- 39.Ryu YG, Chung CH, Choo SJ, et al. A case of antiphospholipid syndrome presenting with a floating thrombus in the ascending aorta. J Thorac Cardiovasc Surg 2009;137:500-2. 10.1016/j.jtcvs.2008.01.028 [DOI] [PubMed] [Google Scholar]
- 40.Berneder S, van Ingen G, Eigel P. Arch thrombus formation in an apparently normal aorta as a source for recurrent peripheral embolization. Thorac Cardiovasc Surg 2006;54:548-9. 10.1055/s-2006-923976 [DOI] [PubMed] [Google Scholar]
- 41.Iyer AP, Sadasivan D, Kamal U, et al. Resolution of large intra-aortic thrombus following anticoagulation therapy. Heart Lung Circ 2009;18:49-50. 10.1016/j.hlc.2007.09.006 [DOI] [PubMed] [Google Scholar]
- 42.Blackshear JL, Jahangir A, Oldenburg WA, et al. Digital embolization from plaque-related thrombus in the thoracic aorta: identification with transesophageal echocardiography and resolution with warfarin therapy. Mayo Clin Proc 1993;68:268-72. 10.1016/S0025-6196(12)60048-2 [DOI] [PubMed] [Google Scholar]
- 43.Hino H, Terasaki T, Hashimoto Y, et al. Cerebral infarction associated with mobile thoracic ascending aortic thrombus in a patient with essential thrombocythemia. Rinsho Shinkeigaku 1999;39:705-10. [PubMed] [Google Scholar]
- 44.Krüger T, Liske B, Ziemer S, et al. Thrombolysis to treat thrombi of the aortic arch. Clin Appl Thromb Hemost 2011;17:340-5. 10.1177/1076029610364519 [DOI] [PubMed] [Google Scholar]
- 45.Yoshikawa Y, Kamikubo Y, Sonoda H, et al. Unexpectedly resolved multiple mobile thrombi in a normal thoracic aorta associated with colorectal cancer and protein C deficiency. J Cardiothorac Vasc Anesth 2014;28:714-7. 10.1053/j.jvca.2012.11.006 [DOI] [PubMed] [Google Scholar]
- 46.Turley RS, Unger J, Cox MW, et al. Atypical aortic thrombus: should nonoperative management be first line? Ann Vasc Surg 2014;28:1610-7. 10.1016/j.avsg.2014.03.028 [DOI] [PubMed] [Google Scholar]
- 47.Mahnken AH, Hoffman A, Autschbach R, et al. Bare metal stenting for endovascular exclusion of aortic arch thrombi. Cardiovasc Intervent Radiol 2013;36:1127-31. 10.1007/s00270-013-0566-6 [DOI] [PubMed] [Google Scholar]
- 48.Stöllberger C, Kopsa W, Finsterer J. Resolution of an aortic thrombus under anticoagulant therapy. Eur J Cardiothorac Surg 2001;20:880-2. 10.1016/S1010-7940(01)00902-2 [DOI] [PubMed] [Google Scholar]
- 49.Gouëffic Y, Chaillou P, Pillet JC, et al. Surgical treatment of nonaneurysmal aortic arch lesions in patients with systemic embolization. J Vasc Surg 2002;36:1186-93. 10.1067/mva.2002.128933 [DOI] [PubMed] [Google Scholar]
- 50.Sari I, Davutoglu V, Bayram N, et al. Fatal giant aortic thrombus presenting with pulmonary edema in a patient with chronic obstructive pulmonary disease. Clin Appl Thromb Hemost 2008;14:486-8. 10.1177/1076029607309180 [DOI] [PubMed] [Google Scholar]
- 51.Fayad ZY, Semaan E, Fahoum B, et al. Aortic mural thrombus in the normal or minimally atherosclerotic aorta. Ann Vasc Surg 2013;27:282-90. 10.1016/j.avsg.2012.03.011 [DOI] [PubMed] [Google Scholar]
- 52.Josephson GD, Tiefenbrun J, Harvey J. Thrombosis of the descending thoracic aorta: a case report. Surgery 1993;114:598-600. [PubMed] [Google Scholar]
- 53.Moris D, Karaolanis G, Schizas D, et al. eComment. Mural thrombus in normal appearing aorta: Unfinished saga in uncharted waters. Interact Cardiovasc Thorac Surg 2016;22:373-4. 10.1093/icvts/ivv407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hartwright D, Lagattolla NR, Taylor PR. Recurrent systemic embolus secondary to free-floating thrombus in the descending thoracic aorta. Eur J Vasc Endovasc Surg 1999;18:268-9. 10.1053/ejvs.1998.0788 [DOI] [PubMed] [Google Scholar]
- 55.Scott DJ, White JM, Arthurs ZM. Endovascular management of a mobile thoracic aortic thrombus following recurrent distal thromboembolism: a case report and literature review. Vasc Endovascular Surg 2014;48:246-50. 10.1177/1538574413513845 [DOI] [PubMed] [Google Scholar]