Abstract
Our goal was to describe our experience of the folded radial forearm flap (RFF) flap in through-and-through buccal defect reconstructions.
Patients who had received a folded RFF flap for full-thickness cheek defect reconstruction were included. The flap success rate and functional results were evaluated.
Six patients were enrolled. All flaps survived totally without any complication; the mean flap size was 75.5 (range 32–135) cm2. The mean mouth-open width was 4.2 (range 3.5–4.7) cm at 6 months after operation. All patients were satisfied with the appearance and were capable of maintaining a regular oral diet, and no patients complained of an inability to eat in a public setting, microstomia, or drooling.
Radial forearm flap was a reliable method for through-and-through buccal reconstruction with high success rate and good functional result.
Keywords: folded radial forearm flap, full-thickness buccal defects, microsurgery, mouth-open width
1. Introduction
Buccal squamous cell carcinoma (SCC) is a common malignant tumor among oral cancers; it poses significant threat to patients’ life and severely affects their quality of life.[1] Complete and extensive resection is the traditional treatment strategy.[2] Liu et al[3] presented their 10 patients with full-thickness buccal defects who underwent reconstruction using folded anterolateral thigh (ALT) flaps; 3 ALT flaps received primary trimming and the success rate was 90%. Valentini et al[4] described a case report in which a radial forearm-free (RFF) flap was successfully transfered for 1-stage reconstruction of a through-and-through buccal defect with the lip commissure involved. Recently, Yang et al[5] reported the feasibility of the folded extended vertical lower trapezius island myocutaneous flap for reconstruction of large full-thickness defects of oral cavity. In the current study, we aimed to describe our experience of the folded RFF flap in repairing through-and-through buccal defects.
2. Materials and methods
The Zhengzhou University Institutional Research Committee approved our study, and all participants signed an informed consent agreement.
From January 2002 to December 2013 in the Department of Stomatology, the First Affiliated Hospital, Zhengzhou University, in all, 144 patients with buccal defect required reconstruction. After screening in purpose, 6 patients who had received a folded RFF flap for full-thickness cheek defect reconstruction were included (Fig. 1). Their medical records were reviewed.
Figure 1.
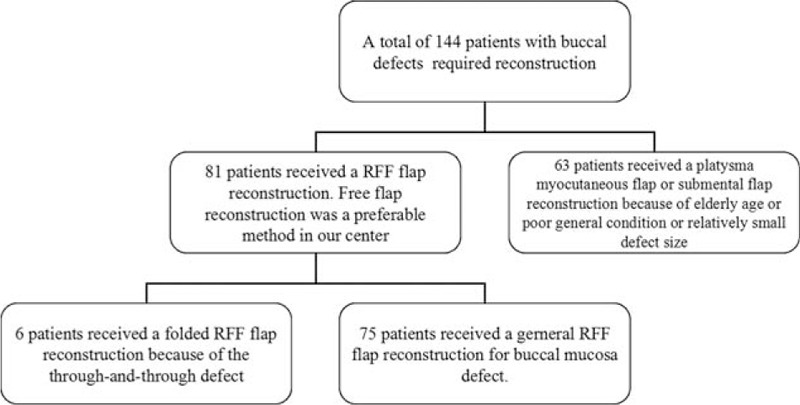
A screening flowchart of selected patients.
The RFF flap was harvested according to previous studies.[4,6] The flap size was determined based on the defect dimension (Fig. 2 and Fig. 3). After vascular anastomosis, the flap was transplanted into the oral cavity and folded to provide the facial side of the cheek and intraoral mucosal lining (Fig. 4 and Fig. 5). The junction area was then de-epithelialized and sutured to the superior edge. The donor site was closed using a full-thickness skin graft.
Figure 2.
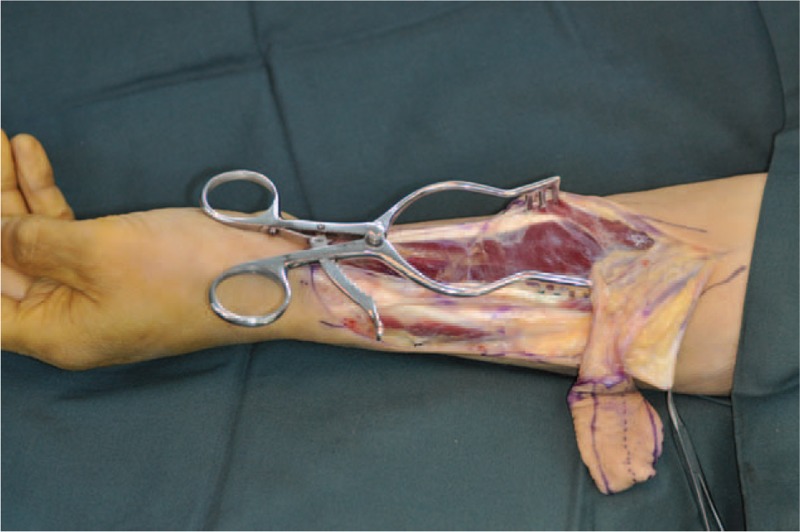
The harvest of a radial forearm flap.
Figure 3.

Extent of full-thickness excision of the cheek.
Figure 4.

Postoperative image of the outer paddle of a radial forearm flap at 6 months after the operation.
Figure 5.

Postoperative image of the inner paddle of a radial forearm flap at 6 months after the operation.
3. Results
Six patients (4 male and 2 female) were enrolled finally. These patients received no preoperative radiotherapy or other treatment. The mean age was 63.7 (range 55–76) years. All tumors were classified as T4 stage according american joint committee on cancer 2007 system (Table 1). All patients received an operation of primary tumor excision and selective neck dissection (SND). The oral commissure was not involved in all patients.
Table 1.
Detailed information of the included patients.
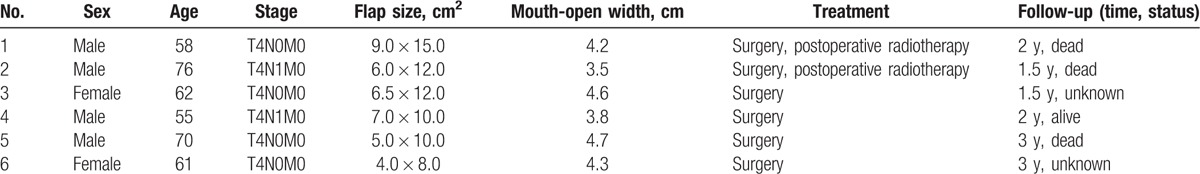
The mean flap size was 75.5 (range 32–135) cm2. All flaps survived totally without any complication. After discharging from the hospital, 2 patients had received postoperative radiotherapy. The mean mouth-opening width was 4.2 (range: 3.5–4.7) cm at 6 months after operation. All patients were satisfied with the appearance during our follow-up, and were capable of maintaining a regular oral diet, and no patients complained of an inability to eat in a public setting, microstomia, or drooling. Three patients were dead of the disease, 1 patient was alive without disease, and the rest was lost to follow-up.
4. Discussion
As both the facial skin and the oral mucosa require appropriate reconstruction, through-and-through buccal resections are a great challenge for the plastic surgeon. In a previous article, the authors described 4 patients who suffered full-thickness cheek defects were successfully reconstructed with the pectoralis major flap combined with the cervicothoracic flap,[7] but this procedure would increase operation difficulty. Moreover, the harvest of this flap might induce shoulder dysfunction.[8] Some other options may be suitable. Huang et al[9] had presented the reliability of the chimeric lateral femoral circumflex perforator flaps in repair of through-and-through cheek defects, and it was likely to result in good aesthetic appearance. But, in some cases, an anterolateral thigh folded flap was too bulky for through-and-through buccal defects; primary thinning might be required, but this procedure sometimes would increase potential flap necrosis possibility.[3] Recently, Yang et al[5] showed their experience of the folded extended vertical lower trapezius island myocutaneous flap in reconstruction of through-and-through oral cavity defects, and the outcome was fascinating. But 1 problem with this procedure was the difficulty in positioning the patient for simultaneous flap dissection and tumor resection, and the other problem was that the flap was very bulky and suitable for more complex reconstructions rather than full-thickness defects restricted in the buccal area.
The RFF flap was first introduced by Yang et al[10] and is known for a reliable anatomy, long pedicle length, suitable thinness, and has been a workhorse for head and neck reconstruction.[2,6,11] Hsu et al[12] reported the RFF flap was thinner than peroneal flap and anterolateral thigh flap, Savant et al[13] for the first time presented the possibility of folded RFF flap in the reconstruction of full-thickness defects of the cheek, flap edema was noted in 4 (30.8%) patients during early postoperative period in the study, and the success rate was 92.3% finally. Other authors also reported the complication rate of the folded RFF flap was low for through-and-through buccal defects.[4,14–16] The findings were consistent with ours. It suggested the folded RFF flap was a reliable method for full-thickness buccal reconstruction. In cases reported by Tuncel and Aytac,[16] this flap was harvested as a free folded osseocutaneous radial forearm flap that would increase the risk of postoperative forearm fracture. In what was described by Kang et al,[15] 2 RFF flaps were elevated first then anastomosed with each other, and then this flap was folded to reconstruct the defect. Therefore, such flap is more difficult to be harvested compared with ours; secondly, it might be suggested for relatively larger defects.
Good postoperative function is the main concern. The mouth-open width must be taken into consideration. A previous study had revealed the RFF flap could preserve the original mouth-open width well.[2] Similarly, we noted the mean postoperative mouth-open width was 4.2 (range 3.5–4.7) cm, which was enough for everyday life; it suggested the RFF flap could also achieve good functional outcomes in full-thickness buccal reconstruction. But Li et al[17] described their patient had some difficulty in the mouth movement even at 3 years postoperatively after the RFF flap reconstruction. Possible explanations might be that first, the cause for the buccal defect was different, high-voltage electrical injury commonly resulted in serious soft-tissue destruction and vascular intimae lesions, and lead to an insufficient blood supply; and, second, this patient seemed to suffer from scar diathesis.
None of the patients complained of microstomia or drooling in current study; the possible reason was that the lip was not involved. If some important structures were needed to be repaired, some modifications could be applied. If the oral commissure was resected, a RFF flap combined with a vermillion advancement flap might be suggested. Yokoo et al[18] used this procedure in 2 patients, and there was no functional impairment such as lip incompetence with food or saliva in both cases. If the mandible was needed to be repaired, the RFF flap could be harvested as an osseocutaneous flap. Tuncel and Aytac[16] described this method was performed in 2 patients; the results revealed that both cases had good oral competence and could completely retain solid or liquid food without drooling.
In summary, the radial forearm flap was a reliable method for through-and-through buccal reconstruction with a high success rate and good functional results.
Footnotes
Abbreviations: ALT flap = anterolateral thigh flap, RFF flap = radial forearm flap, SCC = squamous cell carcinoma.
The authors have no conflicts of interest to disclose.
References
- [1].Fang QG, Shi S, Li ZN, et al. Squamous cell carcinoma of the buccal mucosa: analysis of clinical presentation, outcome and prognostic factors. Mol Clin Oncol 2013;1:531–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Fang QG, Safdar J, Shi S, et al. Comparison studies of different flaps for reconstruction of buccal defects. J Craniofac Surg 2013;24:e450–1. [DOI] [PubMed] [Google Scholar]
- [3].Liu ZM, Wu D, Liu XK, et al. Reconstruction of through-and-through cheek defects with folded free anterolateral thigh flaps. J Oral Maxillofac Surg 2013;71:960–4. [DOI] [PubMed] [Google Scholar]
- [4].Valentini V, Saltarel A, Cassoni A, et al. One-stage reconstruction of a defect of the oral commissure and of the cheek with a radial forearm free flap. J Craniofac Surg 2008;19:1508–11. [DOI] [PubMed] [Google Scholar]
- [5].Yang ZH, Zhang DM, Chen WL, et al. Reconstruction of through-and-through oral cavity defects with folded extended vertical lower trapezius island myocutaneous flap. Br J Oral Maxillofac Surg 2013;51:731–5. [DOI] [PubMed] [Google Scholar]
- [6].Fang QG, Li ZN, Zhang X, et al. Clinical reliability of radial forearm free flap in repair of buccal defects. World J Surg Oncol 2013;11:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Liu FY, Xu ZF, Li P, et al. The versatile application of cervicofacial and cervicothoracic rotation flaps in head and neck surgery. World J Surg Oncol 2011;9:135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Fang QG, Shi S, Zhang X, et al. Assessment of the quality of life of patients with oral cancer after pectoralis major myocutaneous flap reconstruction with a focus on speech. J Oral Maxillofac Surg 2013;71:2004.e1-2004.e5. [DOI] [PubMed] [Google Scholar]
- [9].Huang WC, Chen HC, Jain V, et al. Reconstruction of through-and-through cheek defects involving the oral commissure, using chimeric flaps from the thigh lateral femoral circumflex system. Plast Reconstr Surg 2002;109:433–41. [DOI] [PubMed] [Google Scholar]
- [10].Yang G, Chen B, Gao W, et al. Forearm free skin flap transplantation. Natl Med J China 1981;61:139–41. [Google Scholar]
- [11].Jeremic JV, Nikolic ZS. Versatility of radial forearm free flap for intraoral reconstruction. Srp Arh Celok Lek 2015;143:256–60. [DOI] [PubMed] [Google Scholar]
- [12].Hsu KC, Tsai WH, Ting PS, et al. Comparison between anterolateral thigh, radial forearm, and peroneal artery flap donor site thickness in Asian patients: a sonographic study. Microsurgery 2017;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [13].Savant DN, Patel SG, Deshmukh SP, et al. Folded free radial forearm flap for reconstruction of full-thickness defects of the cheek. Head Neck 1995;17:293–6. [DOI] [PubMed] [Google Scholar]
- [14].Rajacic N, Starovic B. Reconstruction of full-thickness cheek defects with a bipaddled radial forearm flap. Br J Oral Maxillofac Surg 1993;31:108–12. [DOI] [PubMed] [Google Scholar]
- [15].Kang SH, Nam W, Cha IH, et al. Double continuous radial forearm flap for the reconstruction of full-thickness buccal cheek defect. J Plast Reconstr Aesthet Surg 2009;62:e95–6. [DOI] [PubMed] [Google Scholar]
- [16].Tuncel U, Aytac S. Reconstruction of full-thickness cheek defects with using free osseocutaneous radial forearm flap. J Craniofac Surg 2012;23:e357–9. [DOI] [PubMed] [Google Scholar]
- [17].Li YY, Sun JE, Li G, et al. Reconstructing a full-thickness cheek defect of electrical burn with a folding radial forearm flap. J Oral Maxillofac Surg 2013;71:1811e1–e18113. [DOI] [PubMed] [Google Scholar]
- [18].Yokoo S, Tahara S, Tsuji Y, et al. Functional and aesthetic reconstruction of full-thickness cheek, oral commissure and vermilion. J Craniomaxillofac Surg 2001;29:344–50. [DOI] [PubMed] [Google Scholar]


