Abstract
Meckel diverticulum is the most prevalent congenital abnormality of the gastrointestinal tract in children. The aim of this study was to review and analyze clinical data on the diagnosis and management of Meckel diverticulum in pediatric patients. The records of 102 pediatric patients (<14 years old) who underwent surgery for Meckel diverticulum at our institute between 2001 and 2015 were reviewed. Clinical, imaging, laboratory, surgical, and pathological data were recorded. The series comprised 65 males and 37 females with a median age of 5.6 years. Lower gastrointestinal bleeding was the most frequently identified clinical manifestation of Meckel diverticulum, and this manifestation was observed in 41 patients. Intussusception secondary to Meckel diverticulum was identified in 32 patients. Twelve patients presented clinical features of peritonitis; of these patients, 8 had perforated Meckel diverticulum and 4 had Meckel diverticulitis. In 10 patients, Meckel diverticulum was incidentally diagnosed during other surgeries, including appendectomy and neonatal enterostomy. Seven patients were diagnosed with intestinal obstruction. Technetium-99m pertechnetate imaging offered high diagnostic yield. Open surgery was performed on 59 patients, while a laparoscopic approach was employed in 35 patients. The remaining 8 patients did not undergo resection of the Meckel diverticulum. Histology revealed ectopic gastric mucosa in 42 patients (44.7%), ectopic pancreatic tissue in 35 patients (37.2%), mucosa of the small intestine in 15 patients (16.0%), and both gastric and pancreatic ectopic tissue in 2 patients (2.1%). All patients recovered uneventfully except 2 patients in whom an intestinal adhesion obstruction was identified after discharge. Meckel diverticulum had various clinical manifestations in children. Technetium-99m pertechnetate imaging may be useful for diagnosing Meckel diverticulum. Surgical excision of the Meckel diverticulum may be safe and effective in symptomatic patients, and relatively better outcomes can be achieved using this approach.
Keywords: children, gastrointestinal bleeding, intussusception, Meckel diverticulum
1. Introduction
Meckel diverticulum is the most common congenital malformation of the gastrointestinal tract and occurs secondary to persistence of the congenital vitello-intestinal duct.[1] Embryologically, Meckel diverticulum is caused by failure of closure of the vitelline duct at the fifth week of fetal growth. This condition can cause many complications, such as hemorrhage, intussusception, intestinal obstruction and perforation, especially in children.[2] Because Meckel diverticulum is rarely observed in children, the condition of remains frequently misdiagnosed during the preoperative period. It is important for pediatric surgeons to be well aware of its possible presentations. When the condition is correctly diagnosed and properly treated at an early stage, Meckel diverticulum is curable in children. However, at present, only a few studies evaluating pediatric Meckel diverticulum have been published, and these publications have mainly consisted of small case series and case reports. To better understand the clinical characteristics and management of pediatric Meckel diverticulum, we reviewed a series of 102 patients with Meckel diverticulum who were treated at our institute over the 15-year period between 2001 and 2015.
2. Patients and methods
From January 2001 to December 2015, a total of 102 patients (<14 years old) with Meckel diverticulum were treated at the Second Affiliated Hospital and Yuying Children's Hospital of Wenzhou Medical University (Wenzhou, China). Data for all clinical, radiological, laboratory, and pathological findings were collected from the department's database.
3. Results
From 2001 to 2015, 65 male and 37 female pediatric patients were diagnosed with Meckel diverticulum based on surgical findings. The clinical characteristics of these Meckel diverticulum patients are shown in Table 1. The ages of the patients ranged from 1 month to 14 years, with a median age of 5.6 years. Of the cases, 52.0% were ≤4 years of age, 35.3% were between 5 and 9 years of age, and 12.7% were between 10 and 14 years of age.
Table 1.
Clinical features of 102 patients with Meckel diverticulum.
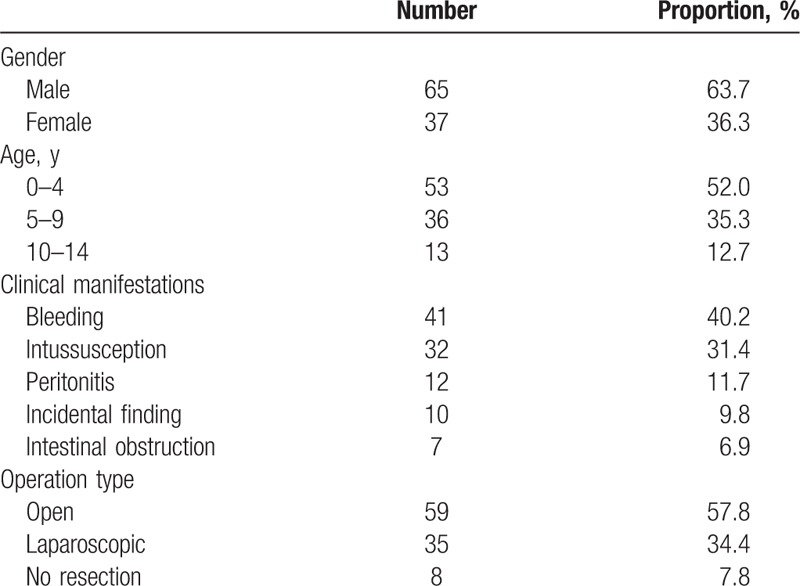
The clinical manifestations of Meckel diverticulum were various in nature. The most common presentation of Meckel diverticulum was lower gastrointestinal bleeding, which was observed in 41 patients (40.2%). Second, Meckel diverticulum also served as a pathological lead point for intussusception in 32 patients. Twelve patients presented clinical features of peritonitis; of these patients, 8 had perforated Meckel diverticulum and 4 had Meckel diverticulitis. Ten patients with Meckel diverticulum were incidentally diagnosed during other surgeries including 8 appendectomies and 2 neonatal enterostomies. Seven patients were diagnosed with intestinal obstruction.
Ultrasonography (US) was performed on all patients, but none displayed evidence of Meckel diverticulum. Forty-eight patients also underwent a computed tomography (CT) scan, but only 3 patients had suspected Meckel diverticulum revealed using this imaging approach. All 41 patients with lower gastrointestinal bleeding were examined by technetium-99m pertechnetate imaging. Among these patients, 34 (82.9%) had positive results. Routine blood tests were also performed on all patients, with elevated white blood cell counts identified in 59 (57.8%) patients.
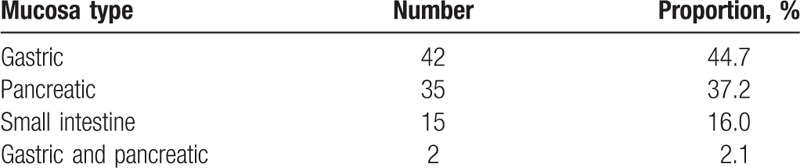
Resection of the Meckel diverticulum and intestinal anastomosis were offered to 94 patients. Fifty-nine patients were subjected to open surgery using an abdominal approach, while a laparoscopic approach was used for surgical resection in 35 patients. Ten patients had incidentally diagnosed Meckel diverticulum. Resection of the Meckel diverticulum was performed on 2 patients. The size of the Meckel diverticulum ranged from 1.5 cm × 0.5 cm to 2 cm × 3 cm. All of the Meckel diverticulum were located in the distal ileum and within 100 cm of the ileocecal valve. Of the 94 patients who underwent resection of the Meckel diverticulum, histology revealed ectopic gastric mucosa in 42 patients (44.7%), ectopic pancreatic tissue in 35 patients (37.2%), mucosa of the small intestine in 15 patients (16.0%), and both gastric and pancreatic ectopic tissue in 2 patients (2.1%) (Table 2).
Table 2.
Histopathological findings in Meckel diverticulum.
All patients recovered uneventfully except 2 patients in whom an intestinal adhesion obstruction was identified approximately 2 and 7 months after discharge, both of whom were cured after conservative treatment. Eight patients who did not undergo resection of the Meckel diverticulum also had no symptoms identified during long-time follow-up.
4. Discussion
Meckel diverticulum was first described in a paper published in 1809 by Johann Friedrich Meckel, who described this congenital abnormality as a remnant of the omphalomesenteric duct.[3] The incidence of Meckel diverticulum in the general population has been estimated at approximately 2%, but reports from autopsy and retrospective studies range from 0.14% to 4.5%.[4–6] Meckel diverticulum is more common in males than females, with the previously reported male to female ratio ranging from 2:1 to 4:1.[7–9] In children, large proportion of Meckel diverticulum cases occur in those younger than 2 years of age (almost 50%).[1] In our series, approximately half of the patients were younger than 4 years old, the youngest of whom was only 1 month old. The male to female ratio was nearly 2:1, which was similar to the results of other studies.
The clinical manifestations of Meckel diverticulum have been found to be various in nature, with little specificity. This congenital abnormality has been reported to not only result in common complications, including ulceration, bleeding, intussusception, intestinal obstruction and perforation, but can also may be associated with the development of some rare complications such as vesicodiverticular fistula and tumors. Bemelman et al[10] found that intestinal obstruction was the most common presentation in patients below the age of 10 years, and bleeding was commonly observed in patients below the age of 20 years. Park et al[11] found that clinical presentation differed between older and younger patients, and the most common presentation in a child was obstruction, while bleeding in an adult. Blevrakis et al[12] reported peritonitis to be the most common symptomatic presentation of Meckel diverticulum in children. Rattan et al[13] showed intestinal obstruction to be the most common complication of this abnormality in their study. However, in our series, the most common presentation of Meckel diverticulum was lower gastrointestinal bleeding, followed by intussusception which was rare in adult patients. Peritonitis and intestinal obstruction were observed in 12 and 7 patients, respectively. Patients who presented clinical features of peritonitis and intestinal obstruction were more likely to be preoperatively misdiagnosed. Some studies have shown that symptomatic Meckel diverticulum, defined as cases in which the surgeon believed that the diverticulum was the main contributing factor to preoperative diagnosis, was only observed in 4% to 6% of patients.[8,14] However, in our series, 10 patients with Meckel diverticulum were incidentally diagnosed during operations including 8 appendectomy and 2 neonatal enterostomy. We also found that Meckel diverticulum was not associated with the preoperative diagnosis in these patients.
Preoperative diagnosis of Meckel diverticulum may be difficult. The diagnosis of this condition cannot be made with plain radiographs or US. CT scans have been found to be often nonspecific but occasionally helpful.[15,16] The most useful method for Meckel diverticulum detection has been identified as technetium-99m pertechnetate imaging, which relies upon the determination of technetium-99m uptake by the ectopic gastric mucosa. Data suggest that this method has a sensitivity of 80% to 90%, a specificity of 95% and an accuracy of 90% in children.[17] In our series, 41 patients with lower gastrointestinal bleeding were examined by technetium-99m pertechnetate imaging, and 34 patients (82.9%) had positive results. However, there is no routine technetium-99m pertechnetate imaging protocol for emergent patients who do not present with lower gastrointestinal bleeding. It is necessary to improve auxiliary examinations before the operation. This can not only preoperatively identify the etiology but also avoid intraoperative omission.
In our study, surgical resection played a central role in the management of symptomatic Meckel diverticulum. The traditional procedure is open diverticulectomy or segmental bowel resection and anastomosis, depending on the length of the Meckel diverticulum and the location of the ectopic mucosa. Common ectopic mucosa locations include the gastric and pancreatic tissues. Other less common locations include the colonic, duodenal, and biliary tissues.[18,19] In our series, postoperative histology revealed the presence of ectopic gastric mucosa in 42 patients (44.7%), ectopic pancreatic tissue in 35 patients (37.2%), mucosa of the small intestine in 15 patients, and both gastric and pancreatic ectopic tissue in 2 patients. In recent years, laparoscopic surgery has also been recognized as a safe and minimally invasive surgical technique associated with short hospital stays and minimal complication rates.[20–22] Laparoscopy is not only a useful diagnostic method but also a therapeutic tool, especially in cases of bleeding Meckel diverticulum. It remains controversial whether all incidentally diagnosed Meckel diverticula should be resected. Some authors have promoted the removal of all asymptomatic Meckel diverticulum because of the high risk of subsequent complications and low risk associated with resection.[23,24] Some authors have advocated resection only in selected cases of Meckel diverticulum, such as who are suspected of having ectopic gastric mucosa or forming adhesive bands.[25,26] In our series, open diverticulectomy was performed on 2 patients who were incidentally diagnosed with Meckel diverticulum in accordance with the patients’ requests. Both of these patients recovered well without any postoperative complications. The remaining 8 patients who had not undergone resection of the Meckel diverticulum also had no symptoms identified during long-time follow-up. Of the other patients, 2 patients were diagnosed with an intestinal adhesion obstruction approximately 2 and 7 months after discharge, both of whom were cured after conservative treatment.
This study is associated with some limitations. It is a retrospective review, and some patients’ records are incomplete, including some auxiliary examinations. Multicenter studies are needed to fully assess the safe and effective management of Meckel diverticulum in future.
5. Conclusion
Meckel diverticulum presented various clinical manifestations in children. Technetium-99m pertechnetate imaging may be useful for diagnosing Meckel diverticulum. Surgical excision of the Meckel diverticulum may be safe and effective in symptomatic patients, and relatively better outcomes can be achieved by using this approach. Surgery may serve as an alternative treatment for asymptomatic Meckel diverticulum in children.
Acknowledgment
We would like to thank our colleagues from the Department of Pediatric Surgery for their assistance with data collection.
Footnotes
Abbreviations: CT = computed tomography, US = ultrasonography.
Ethical approval: All study procedures involving human participants were performed in accordance with the ethical standards of the ethics committees of the Second Affiliated Hospital and Yuying Children's Hospital of Wenzhou Medical University and the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
The authors have no conflicts of interest to disclose.
References
- [1].Sagar J, Kumar V, Shah DK. Meckel's diverticulum: a systematic review. J R Soc Med 2006;99:501–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Chan KWE, Lee KH, Wong HYV, et al. Laparoscopic excision of Meckel's diverticulum in children: what is the current evidence? World J Gastroenterol 2014;20:15158–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Edmonson JM. Johann Friedrich Meckel the younger: Meckel's diverticulum. Gastrointest Endosc 2001;54:19A–20A. [DOI] [PubMed] [Google Scholar]
- [4].Sancar S, Demirci H, Sayan A, et al. Meckel's diverticulum: ten years’ experience. Ulus Cerrahi Derg 2015;31:65–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Erol V, Yoldaş T, Cin S, et al. Complicated Meckel's diverticulum and therapeutic management. Ulus Cerrahi Derg 2013;29:63–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Piñero A, Martínez-Barba E, Canteras M, et al. Surgical management and complications of Meckel's diverticulum in 90 patients. Eur J Surg 2002;168:8–12. [DOI] [PubMed] [Google Scholar]
- [7].St-Vill D, Brandt ML, Panic S, et al. Meckel's diverticulum in children: a 20-year review. J Pediatr Surg 1991;26:1289–92. [DOI] [PubMed] [Google Scholar]
- [8].Yahchouchy EK, Marano AF, Etienne JF, et al. Meckel's diverticulum. J Am Coll Surg 2001;192:658–61. [DOI] [PubMed] [Google Scholar]
- [9].Cullen JJ, Kelly KA, Moir CR, et al. Surgical management of Meckel's diverticulum: an epidemiologic, population-based study. Ann Surg 1994;220:564–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bemelman WA, Huhenholtz E, Heij HA, et al. Meckel's diverticulum in Amsterdam: experience in 136 patients. World J Surg 1995;19:734–7. [DOI] [PubMed] [Google Scholar]
- [11].Park JJ, Wolff BG, Tollefson MK, et al. Meckel diverticulum: the Mayo Clinic experience with 1476 patients (1950–2002). Ann Surg 2005;241:529–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Blevrakis E, Partalis N, Seremeti C, et al. Meckel's diverticulum in paediatric practice on Crete (Greece): a 10-year review. Afr J Paediatr Surg 2011;8:279–82. [DOI] [PubMed] [Google Scholar]
- [13].Rattan KN, Singh J, Dalal P, et al. Meckel's diverticulum in children: our 12-year experience. Afr J Paediatr Surg 2016;13:170–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Menezes M, Tareen F, Saeed A, et al. Symptomatic Meckel's diverticulum in children: a 16-year review. Pediatr Surg Int 2008;24:575–7. [DOI] [PubMed] [Google Scholar]
- [15].Daneman A, Lobo E, Alton DJ, et al. The value of sonography, CT and air enema for detection of complicated Meckel diverticulum in children with nonspecific clinical presentation. Pediatr Radiol 1998;28:928–32. [DOI] [PubMed] [Google Scholar]
- [16].Hughes JA, Hatrick A, Rankin S. Computed tomography findings in an inflamed Meckel diverticulum. Br J Radiol 1998;71:882–3. [DOI] [PubMed] [Google Scholar]
- [17].Kong MS, Chen CY, Tzen KY, et al. Technetium-99m pertechnetate scan for ectopic gastric mucosa in children with gastrointestinal bleeding. J Formos Med Assoc 1993;92:717–20. [PubMed] [Google Scholar]
- [18].Yamaguchi M, Takeuchi S, Awazu S. Meckel's diverticulum, investigation of 600 patients in the Japanese literature. Am J Surg 1978;136:247–9. [DOI] [PubMed] [Google Scholar]
- [19].Williams RS. Management of Meckel's diverticulum. Br J Surg 1981;68:477–80. [DOI] [PubMed] [Google Scholar]
- [20].Duan X, Ye G, Bian H, et al. Laparoscopic vs. laparoscopically assisted management of Meckel's diverticulum in children. Int J Clin Exp Med 2015;8:94–100. [PMC free article] [PubMed] [Google Scholar]
- [21].Papparella A, Nino F, Noviello C, et al. Laparoscopic approach to Meckel's diverticulum. World J Gastroenterol 2014;20:8173–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Hosn MA, Lakis M, Faraj W, et al. Laparoscopic approach to symptomatic Meckel diverticulum in adults. JSLS 2014;18: e2014.00349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Vane DW, West KW, Grosfeld JL. Vitteline duct anomalies. Arch Surg 1987;122:542–7. [DOI] [PubMed] [Google Scholar]
- [24].Pellerin D, Harouchi A, Delmas P. Meckel's diverticulum, revision of 250 children cases. Ann Chir Infant 1976;17:157–72. [Google Scholar]
- [25].Onen A, Cigdem MK, Ozturk H, et al. When to resect when not to resect an asymptomatic Meckel's diverticulum: an ongoing challenge. Pediatr Surg Int 2003;19:57–61. [DOI] [PubMed] [Google Scholar]
- [26].Felberbauer FX, Niederle B, Teleky B. The truth behind the ‘rule of twos’ the Meckel diverticulum revised. Eur Surg 2007;39:299–306. [Google Scholar]


