Abstract
Objectives:
To investigate the preferences of general dental practitioners (GDPs) and endodontists in using endodontic intra-canal medications (ICMs).
Methods:
This observational and descriptive study was conducted in 2014 in the western province of Saudi Arabia. Following ethical clearance and 2 pilot studies, a web-based questionnaire was electronically sent to 375 randomly and systematically selected GDPs and all endodontists in the western province (n=49). An accompanying e-mail explained the study’s aims and confirmed that the data yielded would remain confidential. The responses were collected, and the data was analyzed using the Chi-square test at p=0.05.
Results:
Significantly, the highest proportion of respondents (53.7%) reported disinfection of the root canals as the main function of ICMs. Calcium hydroxide (CH) was the preferred material of the majority of those who used the same ICM in all cases (85.7%). While the vast majority of all endodontists (87.5%) used CH after pulp extirpation, 48.5% of GDPs used formocresol (p<0.001). Almost 30% of those who used ICMs after pulp extirpation did not do so after cleaning and shaping of vital cases. Most endodontists used CH (62.5%) and antibiotics (37.5%) in necrotic pulp cases without apical lesions, which were significantly greater than those of GDPs who did the same (43.8% and 17.2%).
Conclusions:
Participants were aware that the main function of ICMs is disinfection of the root canal system. However, it is clear that GDPs should reduce their reliance on phenol- and formaldehyde-based medications. There was a distinct trend toward the use of ICMs, especially CH, in necrotic pulp cases.
A successful root canal treatment (RCT) must involve the complete elimination of microorganisms, which can be mainly achieved by efficient cleaning and shaping (C&S) of the root canal system. However, the role of intra-canal medications (ICMs) cannot be ignored. Traditionally, it is believed that ICMs have an adjunct impact on the complete disinfection of root canals. Due to the complexity of the root canal morphology, hand and rotary files cannot clean areas such as the isthmuses, lateral canals, and dentinal tubules. In such cases, effective irrigation, as well as the use of ICMs, is essential. In addition, ICMs may indirectly contribute to the healing of the affected periapical tissues.1,2 The ICMs may be used for a number of purposes; for instance, to reduce or prevent inter-appointment pain and to provide a supplementary coronal seal in temporary restorations.3 Currently, a variety of ICMs is available including calcium hydroxide (CH), antibiotics, and phenol-based and anti-inflammatory agents. However, each of these iterations may have certain disadvantages; for example, formaldehyde- and phenol-based formulations are no longer recommended due to their toxicity and potential carcinogenic effects.4-6 Because of its antibacterial effects, CH has been commonly used, especially in cases of apical periodontitis;7 however, it may not be efficient against certain bacterial or fungal strains.8
To date, there have been few reports on the preferences of dental practitioners regarding their use of ICMs and their method of delivery into the root canal system.9,10 In one study in Saudi Arabia, it was reported that formocresol was the most commonly used medication (46% of respondents).10 The remaining participants used different formulations including camphorated monochlorophenol (CMCP) (23%), CH (19%), and iodoform (11%). Only 1% reported using ICMs between appointments.10 However, the authors did not investigate other aspects of ICMs’ usage in depth, such as preference for specific types of ICMs in various clinical scenarios.10
It is generally accepted that questionnaire studies facilitate the gathering of valuable information on the preferences, experiences, and practices of the participants.11-13 However, they should be conducted systematically to enable a good response rate and must be free from bias so that the results can be representative.11-13 In the current study, the aim was to explore the practice and preferences of general dental practitioners (GDPs) and endodontists regarding the use of ICMs during RCTs. The general purpose of the survey was to answer the following questions:
What are the primary ICMs used by GDPs and endodontists for specific endodontic conditions?
What is the most commonly used method for inserting ICMs into the root canal system?
Based on these questions, the following null hypotheses (H0) were tested:
H0 (1): There would be no significant differences among the different proportions of dental practitioners using various ICMs for a specific endodontic condition.
H0 (2): There would be no significant differences between endodontists and GDPs using ICMs for each specific endodontic condition.
H0 (3): There would be no significant differences among different proportions of dental practitioners using different ICMs regarding the method used for their insertion.
Methods
This observational and descriptive survey study was carried out between August and December 2014 in the western province of Saudi Arabia. Ethical approval was obtained from the Research Ethics Committee at College of Dentistry, Taibah University. The ethical committee approved this study without the need to obtain consent from participants because their identities and e-mail addresses remained anonymous. A pilot study was conducted on 50 GDPs to make sure that the questions could be easily answered without the risk of subjective interpretation. The final web-based questionnaire was constructed using the Google Drive tool. It comprised 15 main closed questions, covering demographics, general endodontic practice, the primary ICM used in all endodontic conditions, the primary ICM used in specific endodontic conditions, methods used for inserting paste-based ICMs, and the main function of ICMs.
The inclusion criterion was any dental clinician who was practicing dentistry in Saudi Arabia. The sample size was calculated based on the expected response rate (40-60%) and the target population size (number of dentists working in the specified region). A total of 375 GDPs were randomly and systematically selected by another individual with no connection to the research. For this purpose, a simple randomization method was applied. The questionnaire was electronically sent to all participants, with an accompanying e-mail that explained the study’s aims and confirmed that participants’ identities would remain anonymous. Responses were retrieved from the Google Drive Excel sheet. Any participant who had not been performing RCTs was excluded from the study. The data were analyzed using SPSS, Version 19 (SPSS Inc., Chicago, IL, USA) and the Chi-square test at p ≤ 0.05 was applied.
Results
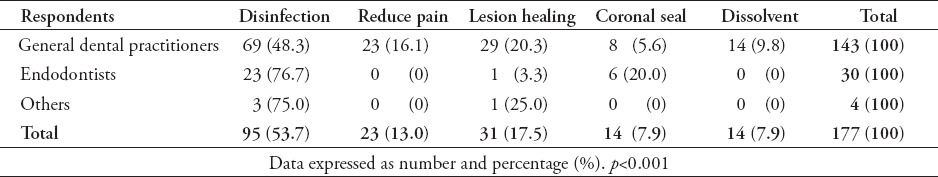
Out of all respondents, there were 175 (80.3%) GDPs, 29 (13.3%) endodontists, 4 (1.8%) endodontic postgraduate students or residents, and 10 (4.6%) others (including periodontists, orthodontists, and oral surgeons and residents in these disciplines). The overall response rate was 51.4% (218/424). The final responses of non-endodontists (GDPs, postgraduate students, and others) was 50.4% (189/375) and endodontists 59.1% (29/49). In total, 11 GDPs (6.3%) and 4 others (40%) had never performed RCTs, while 36.4% of endodontists performed 15 or more RCTs in a week, and 30% of GDPs performed 3-5 cases in the same period (p=0.001) (Table 1). The number of weekly RCTs was positively associated with the participants’ experience (p<0.001). There was no significant relationship between the number of cases performed per week and the use of different ICMs for different pulpal diseases (p=0.100). In addition, there was no correlation between participants’ experience and the use of different ICMs (p=0.607). The highest proportion of participants (53.7%) reported that the main function of ICMs is to disinfect the root canal system (p<0.001), with a significantly higher proportion of endodontists (76.7%) than GDPs (48.3%) (p<0.001) (Table 2).
Table 1.
Number of root canal treatment (RCT) per week and its correlation with participants’ experience.
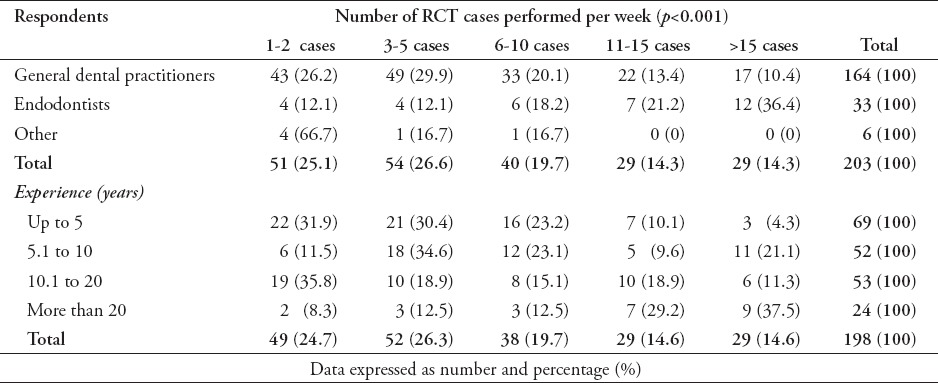
Table 2.
Respondents details regarding the main function of intra-canal medications (ICMs).
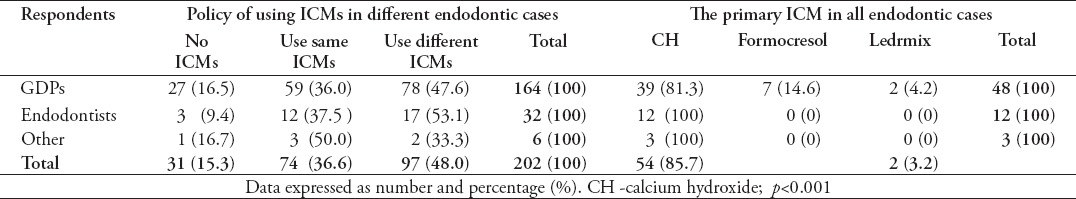
The proportion that used different ICMs for differently treated RCTs (48%) was not significantly different to that using the same ICMs (36.6%) (p=0.079), with no significant variation between GDPs and endodontists (p=0.518) (Table 3). The greatest proportion of those who used different ICMs in different cases (45%) did so because ICMs have varying effects (p<0.001). The majority (85.7%) used non-setting CH as an ICM in all cases (p<0.001); no notable difference was shown between endodontists (100%) and GDPs (81.3%) in this regard (p=0.266) (Table 3). Most (63.2%) used a specific ICM in all cases because of its superior antibacterial effects (p<0.001), with no significant differences between GDPs and endodontists (p=0.409).
Table 3.
Policy of using intra-canal medications (ICMs) in different cases and the same ICM in all cases.
The proportion of GDPs who used ICMs following pulp extirpation (88.2%) was greater than that of endodontists (57.1%) (p=0.029). There were also significant differences between the groups as to the types of ICM used (p=0.002). While the vast majority of endodontist ICM users in this scenario (87.5%) chose CH, most GDPs (48.5%) used formocresol, while 27.3% opted for CH (Table 4).
Table 4.
Policy of using ICMs after pulp extirpation and after C&S of vital cases.
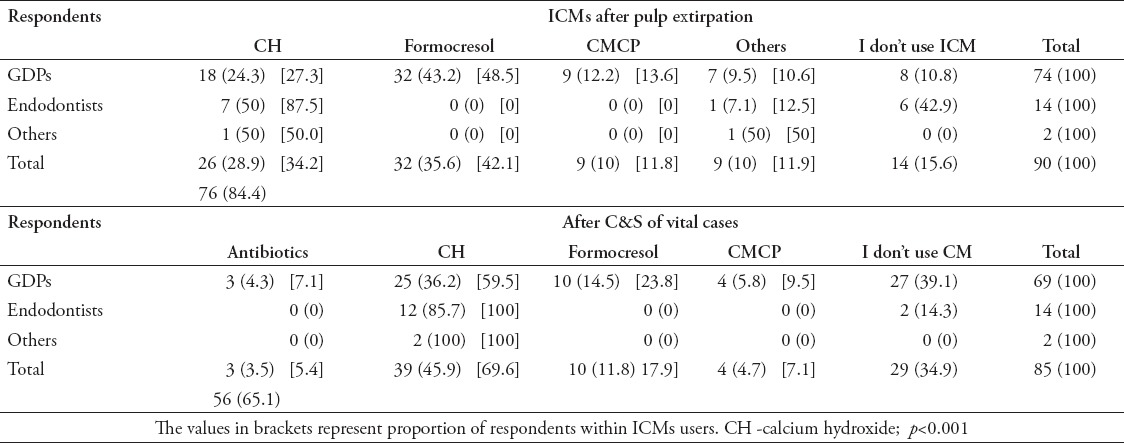
The proportion of those who used ICMs after C&S of vital cases (65.1%) was significantly greater than that of those who did not do so (34.9%) (p=0.003); there were no significant differences between GDPs and endodontists in this regard (p=0.075) (Table 4). In addition, within those who used ICMs, the highest proportion of GDPs (59.5%) and all endodontists (100%) used CH. Almost 30% of those who used ICMs after pulp extirpation did not do so after C&S of vital cases, which was a significant reduction in the GDPs group (p=0.001) (this was not the case with the endodontists; [p=0.604]).
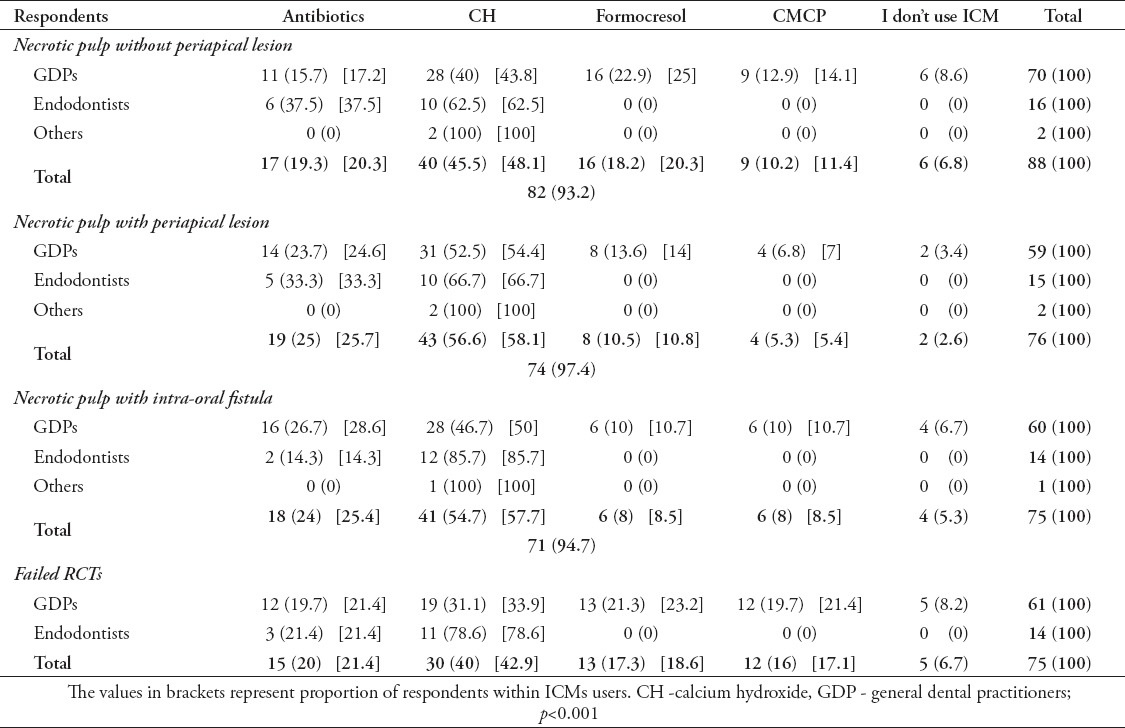
The overwhelming majority (93.2%) used ICMs during the management of necrotic pulp without apical lesions (p<0.001), with CH being the most commonly used ICM (45.5%) (p<0.001) (Table 5). The highest proportions of endodontists used CH (62.5%) and antibiotics (37.5%), which were significantly greater than those of GDPs (43.8% for CH, and 17.2% for antibiotics) (p=0.021). All endodontists (100%) and 96.6% of GDPs used ICMs in cases of necrotic pulp with periapical lesions, with CH being, significantly, the most commonly used ICM (56.6%) (p<0.001) (Table 5). Only 4 respondents (GDPs) did not use ICMs in cases associated with intra-oral sinus tracts. Calcium hydroxide was used by most respondents (54.7%) (p<0.001), with significantly more endodontists favoring it (85.7%) compared with GDPs (46.7%) (p<0.035).
Table 5.
Usage of intra-canal medications (ICMs) in different scenarios of non-vital cases.
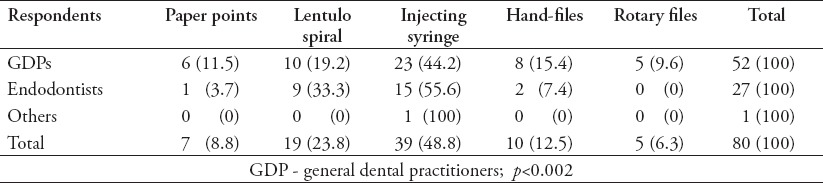
Most respondents (48.8%) were in the habit of using injecting syringes to insert paste-based ICMs, significantly outweighing the lentulo spiral users (23.8%) (p=0.009), with no significant differences between GDPs and endodontists (p=0.386) (Table 6).
Table 6.
Methods for inserting past-based intra-canal medications (ICMs).
Discussion
While survey studies are considered an important research tool, this is with the proviso that they receive adequate attention of planning and preparation.11 In a pilot study, initial data were collected from a group of GDPs to confirm that the questions could be easily answered, which would prevent any bias in the interpretation.11 Other studies saw a response rate of 70-80% being preferred, to eliminate the risk of favorability.14-16 However, as seen elsewhere, a minimum non-response bias could be obtained with a 43% response rate.17 Consequently, the 50.4% and response rates for GDPs and endodontists 59.1%, we obtained in the current study can be seen as acceptable. In fact, this is a good level of response, considering that web-based questionnaires usually have poor response rates.18-20 In addition, good sampling and non-biased responses are other key factors that can validate the results of survey studies.11,12 Small randomized samples with good response rates have been considered more valuable than large non-randomized samples, even when there is a high response rate.14 The GDPs in the current study were randomly and systematically selected from the local dental register. No significant differences were observed between the proportion of respondents who used the same ICM for all cases (35.8%) and that of late respondents who did so (41.4%). This study recruited only dentists working in the western province of Saudi Arabia, which could be considered as one limitation. Nonetheless, our unpublished data showed no remarkable differences in RCTs’ aspects between dental practitioners in the western province and those in other areas of Saudi Arabia.
The majority of GDPs (76.2%) did not perform a high number of RCTs (10 or less per week). The GDPs are usually involved in a range of general dentistry procedures, dividing their working time accordingly. They may also refer complicated cases to endodontists. Another possible reason for their low rate of conducting RCTs is the cost of providing good endodontic care, set off against the low fees charged to patients. This is an especially valid explanation, as 6.3% of GDPs never perform RCTs. A previous study attributed the negative attitude of the majority of its respondents toward the performance of RCTs (66%) to the low charges.21 Based on this, it is paramount to undertake further research to investigate GDPs’ preferences as regards to performing RCTs and to explore the influencing factors. In contrast, the majority of endodontists (57.6%) performed 11 or more RCTs per week. These professionals’ major focus remains on specialized endodontic procedures. Unsurprisingly, the number of RCTs they performed per week was directly correlated with their level of experience. Over time, professionals are expected to improve their skills and to work faster and more efficiently, allowing them to handle more cases. However, participants’ experience did not have an impact on their preferences for using different ICMs in different cases. Additional statistical analysis was performed to investigate in depth the impact of experience on certain aspects of using ICMs; it was found that clinicians’ experience had no impact on their practice in this regard. For instance, there were no significant correlations between years of experience and the use of different ICMs after C&S in vital cases (p=0.231) and during necrotic cases (p=0.097).
It is generally believed that ICMs are used to relieve inflammation of pulpal or periapical tissues, to neutralize tissue debris, and to obstruct microleakage from temporary restorations and dry weeping canals.3 The ICMs should only be used for root canal disinfection as a secondary measure to mechanical C&S.1,3 To some extent, the current study reflected this school of thought, as the highest proportion of respondents (53.7%) used ICMs for the disinfection of root canals. The proportion of endodontists who did so (77%) was significantly greater than that of GDPs (48%), which reflects their superior understanding and awareness of ICMs’ main function. This is reinforced by the fact that the second highest proportion of endodontists (20%) believed that ICMs provide a coronal seal, which was significantly greater than the level of GDPs who believed the same (6%). In addition, the second highest proportion of GDPs (20%) believed that ICMs contribute to the healing of periapical lesions. It is widely accepted among endodontists that such an aim is accomplished by the elimination of infection, which can be mainly achieved using biomechanical instrumentation rather than by relying on the chemical effects of ICMs.1,3
The GDPs and endodontists did not differ significantly in terms of their use of the same or different ICMs; however, a greater number of GDPs (16.5%) than endodontists (9.4%) never used any ICMs. Endodontists tend to believe that the use of ICMs during appointments has beneficial effects.22,23 The key reasons for using chemical canal preparation using various ICMs are to eradicate bacteria and to achieve analgesic and anti-inflammatory effects.2,24 Most respondents who used the same ICM in all cases (85.7%) preferred non-setting CH as a primary ICM, with all endodontists (100%) falling into this group. Most participants (63.2%) did so because of its superlative antibacterial effects. This reflects the participants’ perception and awareness of its excellent properties.
Recent animal studies have shown CH to be an ICM that improves the success rate, regardless of the number of visits.25 However, partial antibacterial effects have also been reported in humans.8 The main action of CH is antibacterial, due to its high pH (11-12) and ionic dissociation. The CH eradicates bacteria by damaging bacterial DNA and plasma membrane, and causing protein denaturation.26 In addition, it denatures bacterial products,27 regulates periapical inflammatory exudate,3,28 and induces hard tissue formation.29,30 Nevertheless, CH has certain limitations and its role must not be overestimated.31,32 For example, it is not completely effective against certain bacterial species (for example, Enterococcus faecalis) and fungal pathogens (for example, Candida albicans).8 In contrast to organic medicaments, CH-based medicaments are not volatile and are available in either powder or paste form. Therefore, physical contact with CH is essential to benefit from its therapeutic actions.1 The highest proportion of respondents who used different ICMs in different cases (45%) did so because they believe that ICMs have different effects. This may reflect their understanding of the various pathological conditions of different endodontic cases that necessitate the use of different ICMs. The main purpose of C&S and ICMs is to eradicate all microorganisms from the root canals. The ICMs vary in terms of their chemical nature and mode of action. For example, formocresol is bactericidal; CH is bactericidal, denatures bacterial products, and is stable over a long period; and sodium hypochlorite is a disinfectant.1
The greatest proportion of endodontists (42.9%) did not rely on the use of ICMs after pulp extirpation, while the majority of GDPs (89.2%) did so. This reflects, to some extent, the different perceptions, and courses of action of endodontists and GDPs pertaining to this endodontic procedure. It can be speculated that GDPs, due to their lack of experience and skills, may unintentionally leave pulp tissue remnants that may cause postoperative pain. This could mean that they tend to target ICMs to control such pain. These findings are consistent with those of a previous study in which more than 50% used formocresol as an ICM.33 In addition, the residual pulp remnants may lead to inter-appointment infection, which could be another reason why GDPs use ICMs. This corresponds to the fact that most GDPs do not use rubber dams.34 The possibility of inter-appointment pain or infection may explain why 48% and 27% of GDPs were using formocresol and CH after pulp extirpation. The former has been used for a range of endodontic applications such as pain reduction, root canals disinfection, and fixation of pulp tissue remnants.35 In spite of these benefits, its popularity has fallen recently due to serious concerns including its role in the suppression of inflammatory response at initial stages,35 risks of mutagenicity,36 induction of immune reactions,37,38 cytotoxicity,39-41 and teratogenicity.42,43 Formocresol may elute though pulpal or periapical tissues to yield systemic effects.1 Therefore, GDPs need to be aware of these unwanted aspects, as such an understanding could ultimately result in a reduction of the possible side effects in patients. However, whether such a strategy can or cannot improve the treatment outcome is an interesting aspect, which necessitates future investigation. Endodontists, due to their superior skills, usually remove pulp tissues completely when performing pulp extirpation. This means that there is no need for an ICM until the next visit, especially considering that the majority of endodontists deploy rubber dam isolation during their procedures.34 However, there is still the possibility of inter-appointment infections of the root canal system, for example in cases of loss of coronal seal or where there are minor residual pulp remnants. The CH can provide a supplementary coronal seal against leakage caused by temporary restoration. In addition, the unique biological properties of CH make it an effective material for ICM applications.24,31,32,44
A significantly greater proportion of respondents (65.1%) used ICMs after C&S of the root canal system in vital cases. Almost 30% of those who used ICMs after pulp extirpation did not do so after C&S in vital cases; this was a significant reduction within the GDPs group, but not within the endodontists group. Such trends can be explained by taking into account the participants’ understanding of the main role of mechanical instrumentation in eliminating intra-canal infection, rather than relying on the chemical effects of ICMs; this is especially true of the endodontists’ group. This again supports our speculation that the reason for using ICMs after pulp extirpation and not after C&S is to avoid post-operative pain resulting from pulp tissue remnants. With complete C&S, the root canal is almost free of these remnants. However, caution should be exercised to ensure that the canals remain free of infection after C&S until the next visit. This explains why CH remains the ICM of choice for both GDPs and endodontists.
Periapical conditions, including periapical granuloma and abscess, are sequelae of pulp tissue necrosis and an immunological self-defense phenomenon against pathogenic microorganisms.45 The clinical management of periapical lesions is based on the same principles; namely, the removal of pathologic pulp tissues and bacteria by efficient C&S, followed by sealing of the root canal system.1 In the current study, the respondents did not report any significant differences in the use of ICMs based on the pathological conditions (with/without lesions and with/without intra-oral sinus tract). Regardless of the respondent category, there was an extremely clear trend of using ICM in necrotic pulp cases, with and without periapical lesions (100 and 93.2%). Chong et al3 stressed the application of ICMs for asepsis control and disinfection of infected root canals. Teeth with necrotic pulpal tissue remnants or periapical lesions are more prone to bacterial infections; in this scenario, the role of chemicals becomes vital. Unsurprisingly, CH remained the dominant ICM among both GDPs (52.5%) and endodontists (66.7%), followed by antibiotics (23.7 and 33.3%). There was no significant difference in the trends of using ICMs in necrotic pulp cases with intraoral sinus tract; the only exception was that usage of CH by endodontists was significantly greater (85.7%).
Failure of endodontically treated teeth is usually caused by opportunistic or more resistant microorganisms such as Enterococcus faecalis (E. faecalis) and Candida albicans (C. albicans).46 Considering the existence of resistant strains in failed endodontic cases, most endodontists relied on CH (79%) and antibiotics (21%). Although CH is a highly alkaline (pH 11-12) medicament and exhibits good antibacterial properties, it is not highly efficient against C. albicans and E. faecalis.8 To enhance its efficacy, antibacterial agents can be added to CH. For example, a combination of CH and 2% chlorhexidine has been reported to disinfect Enterococcus faecalis-infected root canals. However, further clinical trials are required to establish the therapeutic effects.47 The GDP respondents used various ICMs, including antibiotics, CH, and formocresol, with no significant differences.
A range of methods are used for inserting paste-based ICMs such as paper points, lentulo spirals, injecting syringes, hand files, and rotary files.48 We observed no significant difference between endodontists and GDPs, with most using injecting syringes (48.8%), followed by lentulo spirals (23.8%). The former is considered a convenient and cost-effective delivery method for both patients and operators. Unlike lentulo spirals, disposable injecting syringes are effective in terms of better cross-infection control and eliminate the need for sterilization. Lentulo spirals, due to their rotation motion, are prone to fracture with in the root canal system,49 especially where there is reduced corrosion resistance due to repeated sterilization cycles.50 Such an adverse outcome may further complicate endodontic treatment.51
In conclusion, the participants demonstrated good understanding and awareness of the main function of ICMs in disinfecting the root canal system. However, they need to update their knowledge of the reasons for using ICMs in certain cases, which can be achieved through continuous postgraduate education. In addition, participants should be aware of the side effects of and serious concerns relating to formocresol as an ICM; such awareness could reduce unwanted complications in patients in the long term. There was a clear trend for using ICMs in necrotic pulp cases. Calcium hydroxide remains the dominant ICM among endodontists and is also commonly used by GDPs.
Footnotes
References
- 1.Kawashima N, Wadachi R, Suda H, Yeng T, Parashos P. Root canal medicaments. Int Dent J. 2009;59:5–11. [PubMed] [Google Scholar]
- 2.Law A, Messer H. An evidence-based analysis of the antibacterial effectiveness of intracanal medicaments. J Endod. 2004;30:689–694. doi: 10.1097/01.don.0000129959.20011.ee. [DOI] [PubMed] [Google Scholar]
- 3.Chong B, Ford TP. The role of intracanal medication in root canal treatment. Int Endod J. 1992;25:97–106. doi: 10.1111/j.1365-2591.1992.tb00743.x. [DOI] [PubMed] [Google Scholar]
- 4.Sjögren U, Hägglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16:498–504. doi: 10.1016/S0099-2399(07)80180-4. Chinese. [DOI] [PubMed] [Google Scholar]
- 5.Zhao J, Li SH, Zhu ZH. Clinical studies of calcium hydroxide disinfecting infectious root canal of deciduous tooth. Shanghai Kou Qiang Yi Xue. 2003;12:109–111. [PubMed] [Google Scholar]
- 6.Huang T, Ding S, Kao C. Biocompatibility of various formula root filling materials for primary teeth. J Biomed Mater Res B Appl Biomater. 2007;80:486–490. doi: 10.1002/jbm.b.30621. [DOI] [PubMed] [Google Scholar]
- 7.Furusawa M, Hayakawa H, Ida A. Effectiveness of calvital, a calcium hydroxide formulation, on persistent apical periodontitis caused by over-enlargement of apical foramen. Bull Tokyo Dent Coll. 2011;52:209–213. doi: 10.2209/tdcpublication.52.209. [DOI] [PubMed] [Google Scholar]
- 8.Kim D, Kim E. Antimicrobial effect of calcium hydroxide as an intracanal medicament in root canal treatment:a literature review-Part II. in vivo studies. Restor Dent Endod. 2015;40:97–103. doi: 10.5395/rde.2015.40.2.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gaikwad A, Jain D, Rane P, Bhondwe S, Taur S, Doshi S. Attitude of general dental practitioners toward root canal treatment procedures in India. J Contemp Dent Pract. 2013;14:528–531. doi: 10.5005/jp-journals-10024-1356. [DOI] [PubMed] [Google Scholar]
- 10.Al-Fouzan KS. A survey of root canal treatment of molar teeth by general dental practitioners in private practice in Saudi Arabia. Saudi Dent J. 2010;22:113–117. doi: 10.1016/j.sdentj.2010.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lydeard S. The questionnaire as a research tool. Fam Pract. 1991;8:84–91. doi: 10.1093/fampra/8.1.84. [DOI] [PubMed] [Google Scholar]
- 12.Fink A. How to Ask Survey Questions (Survey Kit;V. 2) 2nd Edition. KSA: Amazon; 1995. [Google Scholar]
- 13.Madarati A, Watts D, Qualtrough A. Opinions and attitudes of endodontists and general dental practitioners in the UK towards the intracanal fracture of endodontic instruments:part 1. Int Endod J. 2008;41:693–701. doi: 10.1111/j.1365-2591.2008.01425.x. [DOI] [PubMed] [Google Scholar]
- 14.Evans SJ. Good surveys guide. BMJ. 1991;302:302–303. doi: 10.1136/bmj.302.6772.302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brennan DS, Ryan P, Spencer AJ, Szuster FS. Dental service rates:age, period, and cohort effects. Community Dent Health. 2000;17:70–78. [PubMed] [Google Scholar]
- 16.Gough HG, Hall WB. A comparison of physicians who did or did not respond to a postal questionnaire. J Appl Psychol. 1977;62:777. [PubMed] [Google Scholar]
- 17.Hovland EJ, Romberg E, Moreland EF. Nonresponse bias to mail survey questionnaires within a professional population. J Dent Educ. 1980;44:270–274. [PubMed] [Google Scholar]
- 18.van Gelder MM, Bretveld RW, Roeleveld N. Web-based questionnaires:the future in epidemiology? Am J Epidemiol. 2010;172:1292–1298. doi: 10.1093/aje/kwq291. [DOI] [PubMed] [Google Scholar]
- 19.Bälter KA, Bälter O, Fondell E, Lagerros YT. Web-based and mailed questionnaires:a comparison of response rates and compliance. Epidemiology. 2005;16:577–579. doi: 10.1097/01.ede.0000164553.16591.4b. [DOI] [PubMed] [Google Scholar]
- 20.Leece P, Bhandari M, Sprague S, Swiontkowski MF, Schemitsch EH, Tornetta P, Devereaux PJ, Guyatt GH. Internet versus mailed questionnaires:a controlled comparison (2) J Med Internet Res. 2004;6:e39. doi: 10.2196/jmir.6.4.e39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Slaus G, Bottenberg P. A survey of endodontic practice amongst Flemish dentists. Int Endod J. 2002;35:759–767. doi: 10.1046/j.1365-2591.2002.00564.x. [DOI] [PubMed] [Google Scholar]
- 22.Raju TB, Seshadri A, Vamsipavani B, Abhilash K, Subhash AV, Kumari KV. Evaluation of pain in single and multi rooted teeth treated in single visit endodontic therapy. J Int Oral Health. 2014;6:27–32. [PMC free article] [PubMed] [Google Scholar]
- 23.Wong AW, Zhang S, Zhang C, Chu C. Perceptions of single-visit and multiple-visit endodontic treatment:a survey of endodontic specialists and general dentists in Hong Kong. J Investig Clin Dent. 2016;7:263–271. doi: 10.1111/jicd.12154. [DOI] [PubMed] [Google Scholar]
- 24.Byström A, Claesson R, Sundqvist G. The antibacterial effect of camphorated paramonochlorophenol, camphorated phenol and calcium hydroxide in the treatment of infected root canals. Dental Traumatology. 1985;1:170–175. doi: 10.1111/j.1600-9657.1985.tb00652.x. [DOI] [PubMed] [Google Scholar]
- 25.Silveira AMV, Lopes HP, Siqueira Jr JF, Macedo SB, Consolaro A. Periradicular repair after two-visit endodontic treatment using two different intracanal medications compared to single-visit endodontic treatment. Braz Dent J. 2007;18:299–304. doi: 10.1590/s0103-64402007000400005. [DOI] [PubMed] [Google Scholar]
- 26.Mohammadi Z, Dummer PMH. Properties and applications of calcium hydroxide in endodontics and dental traumatology. Int Endod J. 2011;44:697–730. doi: 10.1111/j.1365-2591.2011.01886.x. [DOI] [PubMed] [Google Scholar]
- 27.Safavi KE, Nichols FC. Alteration of biological properties of bacterial lipopolysaccharide by calcium hydroxide treatment. J Endod. 1994;20:127–129. doi: 10.1016/S0099-2399(06)80057-9. [DOI] [PubMed] [Google Scholar]
- 28.Tronstad L, Andreasen J, Hasselgren G, Kristerson L, Riis I. pH changes in dental tissues after root canal filling with calcium hydroxide. J Endod. 1981;7:17–21. doi: 10.1016/S0099-2399(81)80262-2. [DOI] [PubMed] [Google Scholar]
- 29.Mitchell DF, Shankwalker GB. Osteogenic potential of calcium hydroxide and other materials in soft tissue and bone wounds. J Dent Res. 1958;37:1157–1163. doi: 10.1177/00220345580370061501. [DOI] [PubMed] [Google Scholar]
- 30.Bergenholtz G, Dahlén G. Advances in the study of endodontic infections:introduction. Endodontic Topics. 2004;9:1–4. [Google Scholar]
- 31.Sathorn C, Parashos P, Messer H. Antibacterial efficacy of calcium hydroxide intracanal dressing:a systematic review and meta-analysis. Int Endod J. 2007;40:2–10. doi: 10.1111/j.1365-2591.2006.01197.x. [DOI] [PubMed] [Google Scholar]
- 32.De Moor R. Calcium hydroxide-based pastes used in endodontics. Rev Belge Med Dent (1984) 2003;58:34–48. [PubMed] [Google Scholar]
- 33.Iqbal A, Akbar I, Qureshi B, Sghaireen MG, Al-Omiri MK. A Survey of Standard Protocols for Endodontic Treatment in North of KSA. ISRN Dentistry. 2014;2014 doi: 10.1155/2014/865780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Madarati AA. Why dentists don’t use rubber dam during endodontics and how to promote its usage? BMC Oral Health. 2016;16:1. doi: 10.1186/s12903-016-0175-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sipes R, Binkley CJ. The use of formocresol in dentistry:a review of the literature. Quintessence Int. 1986;17:415–417. [PubMed] [Google Scholar]
- 36.Block RM, Lewis RD, Hirsch J, Coffey J, Langeland K. Systemic distribution of [14 C]-labeled paraformaldehyde incorporated within formocresol following pulpotomies in dogs. J Endod. 1983;9:176–189. doi: 10.1016/S0099-2399(83)80090-9. [DOI] [PubMed] [Google Scholar]
- 37.Block RM, Lewis RD, Sheats JB, Burke SG. Antibody formation to dog pulp tissue altered by formocresol within the root canal. Oral Surgery, Oral Medicine, Oral Pathology. 1978;45:282–292. doi: 10.1016/0030-4220(78)90096-8. [DOI] [PubMed] [Google Scholar]
- 38.Block RM, Lewis RD, Sheats JB, Fawley J. Cell-mediated immune response to dog pulp tissue altered by formocresol within the root canal. J Endod. 1977;3:424–430. doi: 10.1016/S0099-2399(77)80113-1. [DOI] [PubMed] [Google Scholar]
- 39.Kasugai S, Hasegawa N, Ogura H. Application of the MTT colorimetric assay to measure cytotoxic effects of phenolic compounds on established rat dental pulp cells. J Dent Res. 1991;70:127–130. doi: 10.1177/00220345910700020601. [DOI] [PubMed] [Google Scholar]
- 40.Soekanto A, Kasugai S, Mataki S, Ohya K, Ogura H. Toxicity of camphorated phenol and camphorated parachlorophenol in dental pulp cell culture. J Endod. 1996;22:284–286. doi: 10.1016/S0099-2399(96)80259-7. [DOI] [PubMed] [Google Scholar]
- 41.Spangberg L, Engström B, Langeland K. Biologic effects of dental materials:3. Toxicity and antimicrobial effect of endodontic antiseptics in vitro. Oral Surgery, Oral Medicine, Oral Pathology. 1973;36:856–871. doi: 10.1016/0030-4220(73)90338-1. [DOI] [PubMed] [Google Scholar]
- 42.Friedberg BH, Gartner LP. Embryotoxicity and teratogenicity of formocresol on developing chick embryos. J Endod. 1990;16:434–437. doi: 10.1016/S0099-2399(06)81886-8. [DOI] [PubMed] [Google Scholar]
- 43.Lewis BB, Chestner SB. Formaldehyde in dentistry:a review of mutagenic and carcinogenic potential. J Am Dent Assoc. 1981;103:429–434. doi: 10.14219/jada.archive.1981.0341. [DOI] [PubMed] [Google Scholar]
- 44.Schäfer E, Bössmann K. Antimicrobial efficacy of chlorhexidine and two calcium hydroxide formulations against Enterococcus faecalis. J Endod. 2005;31:53–56. doi: 10.1097/01.don.0000134209.28874.1c. [DOI] [PubMed] [Google Scholar]
- 45.Cawson RA. Cawson’s essentials of oral pathology and oral medicine. 7th ed. Edinburgh: Churchill Livingstone; 2002. [Google Scholar]
- 46.Nair PR, Sjögren U, Krey G, Kahnberg K, Sundqvist G. Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions:a long-term light and electron microscopic follow-up study. J Endod. 1990;16:580–588. doi: 10.1016/S0099-2399(07)80201-9. [DOI] [PubMed] [Google Scholar]
- 47.Zerella JA, Fouad AF, Spångberg LS. Effectiveness of a calcium hydroxide and chlorhexidine digluconate mixture as disinfectant during retreatment of failed endodontic cases. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontology. 2005;100:756–761. doi: 10.1016/j.tripleo.2005.05.072. [DOI] [PubMed] [Google Scholar]
- 48.D’Arcangelo C, D’Amario M, Vadini M, Zazzeroni S, De Angelis F, Caputi S. An evaluation of luting agent application technique effect on fibre post retention. J Dent. 2008;36:235–240. doi: 10.1016/j.jdent.2008.01.004. [DOI] [PubMed] [Google Scholar]
- 49.Suter B, Lussi A, Sequeira P. Probability of removing fractured instruments from root canals. Int Endod J. 2005;38:112–123. doi: 10.1111/j.1365-2591.2004.00916.x. [DOI] [PubMed] [Google Scholar]
- 50.Dundeková S, Skorík V, Hadzima B, Bukovinová L. The influence of the temperature on the corrosion resistance of AISI 316L stainless steel. J Mater Sci Mater Med. 2015;26:100. [Google Scholar]
- 51.Madarati AA, Hunter MJ, Dummer PM. Management of intracanal separated instruments. J Endod. 2013;39:569–581. doi: 10.1016/j.joen.2012.12.033. [DOI] [PubMed] [Google Scholar]


