Abstract
Many studies have examined associations between religious involvement and health, linking various dimensions of religion with a range of physical health outcomes and often hypothesizing influences on health behaviors. However, far fewer studies have examined explanatory mechanisms of the religion-health connection, and most have overwhelmingly relied on cross-sectional analyses. Given the relatively high levels of religious involvement among African Americans and the important role that religious coping styles may play in health, the present study tested a longitudinal model of religious coping as a potential mediator of a multidimensional religious involvement construct (beliefs; behaviors) on multiple health behaviors (e.g., diet, physical activity, alcohol use, cancer screening). A national probability sample of African Americans was enrolled in the RHIAA (Religion and Health In African Americans) study and three waves of telephone interviews were conducted over a 5-year period (N=565). Measurement models were fit followed by longitudinal structural models. Positive religious coping decreased modestly over time in the sample, but these reductions were attenuated for participants with stronger religious beliefs and behaviors. Decreases in negative religious coping were negligible and were not associated with either religious beliefs or religious behaviors. Religious coping was not associated with change in any of the health behaviors over time, precluding the possibility of a longitudinal mediational effect. Thus, mediation observed in previous cross-sectional analyses was not confirmed in this more rigorous longitudinal model over a 5-year period. However, findings do point to the role that religious beliefs have in protecting against declines in positive religious coping over time, which may have implications for pastoral counseling and other faith-based interventions.
Keywords: Longitudinal, religion, African American, religious coping, mediation, health behaviors
Introduction
The study of religious involvement and health has produced a body of literature of sufficient scope as to be reviewed in two editions of an exhaustive volume, the Handbook of Religion and Health (Koenig, King, & Carson, 2012; Koenig, McCullough, & Larson, 2001) and a more specific one reviewing population-based research in the US, Religion Families and Health (Ellison & Hummer, 2010). Much of this research has reported salutary associations between religious involvement and health-related outcomes. For the present purpose, we define religious involvement as partaking in “an organized system of [religious] beliefs, practices, rituals, and symbols” (Thoresen, 1998). Given that most contemporary research on religion and health recognizes religious involvement as a multidimensional construct (Hill & Hood, 1999) we utilize a model of religious involvement that includes both religious beliefs (e.g., personal relationship with God or other higher power) and behaviors (e.g., service attendance) (Lukwago, Kreuter, Bucholtz, Holt, & Clark, 2001; Roth et al., 2012).
The church and religious involvement have historically played an important role in African American life (Lincoln & Mamiya, 1990). The church is more than a worship center, but has taken a lead role in providing resources and support for African Americans since the time of slavery. African Americans are therefore historically high in religious involvement (Taylor, Chatters, & Levin, 2003). This group also experiences a disproportionate burden of many chronic diseases and adverse health outcomes (Williams, 2012). There is also quite a bit of evidence that religious involvement is linked to health-related outcomes, particularly in African Americans (Ellison & Hummer, 2010). Therefore, it is important to develop a deeper knowledge of the religion-health connection in African Americans in light of the potential implications for better understanding health disparities and informing public health interventions, including those delivered in faith-based settings.
Given these strong and persuasive links between religious involvement and health, researchers have begun to empirically examine reasons for, or mechanisms of, these observed associations, often through mediation analyses. Several explanatory mechanisms of the “religion-health connection” have been proposed, including that religiously involved people may have better mental health, which in turn impacts their physical health outcomes (Ellison & Levin, 1998; Levin & Vanderpool, 1989; Oman & Thoresen, 2002) or that religion may facilitate positive self-perceptions (Chatters, 2000; Ellison & Levin, 1998; Levin & Vanderpool, 1989), provide a protective source of social support (Chatters, 2000; Ellison & Levin, 1998; George, Larson, Koenig, & McCullough, 2000; Levin & Vanderpool, 1989; Musick, Traphagan, Koenig, & Larson, 2000; Oman & Thoresen, 2002), promote beliefs about living healthier lifestyles or avoiding risky health behaviors (Chatters, 2000; Ellison & Levin, 1998; George et al., 2000; Levin & Vanderpool, 1989; Musick et al., 2000; Oman & Thoresen, 2002), or provide a sense of meaning in life (George et al., 2000; Musick et al., 2000). Cross-sectional evidence suggests that viewing illness as punishment from a higher power can also play a negative role in the religion-health association (Holt, Clark, & Roth, 2014).
Religious coping
One important potential mediator is religion, which may promote better adaptation to stress (Ellison & Levin, 1998; Musick et al., 2000), specifically through religious coping (Holt, Clark, Debnam, & Roth, 2014). Religious coping refers to bringing religious resources to bear in one’s efforts to deal with stressful situations (Pargament, Smith, Koenig, & Perez, 1998). Religious coping has been associated with individuals’ adjustment to major life stressors such as cancer or trauma as well as their management of less severe stressors (Pargament, Koenig, & Perez, 2000), and has been shown to predict health and well-being above and beyond secular types of coping (e.g., Park, Edmondson, & Blank, 2009; Pargament, Falb, Ano, & Wachholtz, 2013). Importantly, different types of religious coping have been identified and hypothesized to be linked to different outcomes (Pargament, Feuille, & Burdzy, 2011). Most contemporary research distinguishes positive and negative religious coping. Positive religious coping reflects a confident and trusting connection with God (Hebert, Zdaniuk, Schulz, & Scheier, 2009) and includes strategies such as seeking religious support and making benevolent religious reappraisals. Negative religious coping reflects a less secure relationship with God (Hebert et al., 2009) and includes strategies such as expressing religious discontent and making punitive religious reappraisals.
Using positive religious coping to deal with specific stressors is sometimes (Pargament et al., 1998), but not always (Gerber, Boals, & Schuettler, 2011; Sherman, Plante, Simonton, Latif, & Anaissie, 2009; Sherman, Simonton, Latif, Spohn, & Tricot, 2005), related to higher levels of well-being. More consistent findings have been reported for negative religious coping, which tends to be used much less frequently but is generally found to be strongly related to poorer mental and physical health (Exline & Rose, 2013).
Even though there has been much previous research demonstrating associations between religious coping and health, including theorized mediation of religious coping on religiousness-health links, only a handful of studies have examined whether religious coping accounts for the link between religiousness and health outcomes (Roesch & Ano, 2003). One previous study that tested the mediational effect of religious coping in the religion-health link was a cross-sectional analysis of our present sample of African Americans. We found that the relationship between religious beliefs and vegetable consumption was mediated by religious coping, such that positive coping was related to greater vegetable consumption while negative coping was related to less consumption (Holt, Clark, Debnam, et al., 2014); and the relationship between religious behaviors and vegetable consumption was also mediated by greater positive religious coping.
To our knowledge, there are no existing longitudinal studies that have examined whether religious coping mediates the effects of religious involvement on physical- or mental health-related outcomes. Cross-sectional mediation models can be informative, but also have serious limitations concerning temporal and cause-and-effect interpretations. Furthermore, cross-sectional analyses have been shown to yield biased estimates of underlying longitudinal mediation mechanisms (Maxwell & Cole, 2007). The current prospective design has the advantage of being able to assess and control for known confounders relevant in religion-health research (Powell, Shahabi, & Thoresen, 2003) and for baseline values, thus allowing us to examine change over time.
The present study
The present study aimed to examine religious coping as a mediator of religious involvement and a variety of health behaviors using longitudinal data from a national sample of African Americans. Critics of studies in religious involvement and health argue that cross-sectional studies, particularly those that do not control for relevant covariates or confounders, lack the ability to rule out the possibility of reverse causality, whereby healthier people are either attracted to religious participation and/or are physically able to attend worship services (Maselko, Hayward, Hanlon, Buka, & Meador, 2012; Roth, Usher, Clark, & Holt, 2016). All of this leads to the importance of investigations that model the relationships between religious involvement, psychosocial mediators such as religious coping, and health-related outcomes over time.
Given our previous cross-sectional research examining religious coping as a mediator of the religion-health connection, and informed by theory and research in religious coping (Pargament et al., 2011), we proposed a series of hypotheses based on the study conceptual model shown in Figure 1. First, it was hypothesized that both religious beliefs (e.g., having a strong personal relationship with God) and religious behaviors (e.g., attendance and participation in church activities) would be predictive of stability, or potentially of modest increases in positive religious coping and decreases in negative religious coping over time (the “al” and “ah” paths in Figure 1). Second, based on previous research linking religious coping and health outcomes (Pargament et al., 2011), we expected that positive religious coping would be associated with increases in adaptive health behaviors and decreases in maladaptive health behaviors over time, and that the opposite would be true for negative religious coping- that it would predict growth in poor health behaviors over time and attenuation in positive health behaviors (the b32 paths in Figure 1). Detecting an effect of the mediator on change over time in the outcome would be a prerequisite for detection of mediation in the overall model (discussed below).
Figure 1.
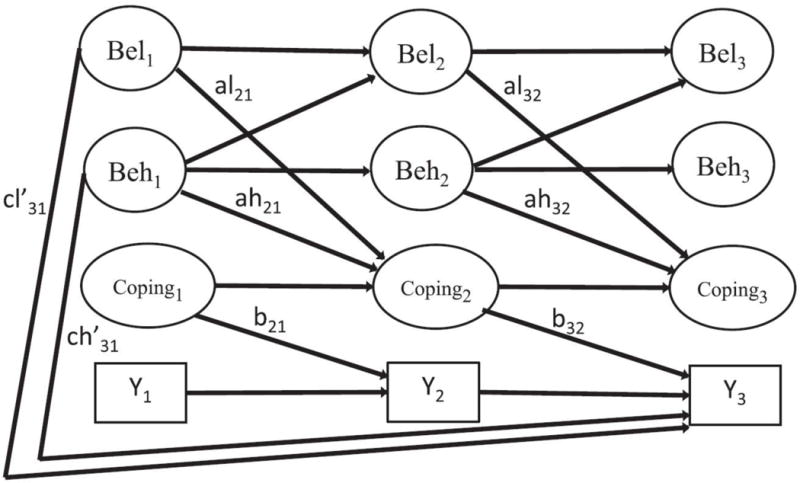
Longitudinal model of religious coping as a possible mediator of the religious involvement – health behavior connection.
Third, consistent with our previous cross-sectional research (Holt, Clark, Debnam, et al., 2014) we hypothesized that religious beliefs would have stronger linkages in the longitudinal religion-health behavior model than would religious behaviors. Fourth, based on our previous work examining the differential effects of positive and negative religious coping (Park, Holt, Le, Christice, & Williams, In Press), we expected that negative religious coping would have stronger associations with the health behaviors than would positive religious coping. Fifth, we anticipated that both positive and negative religious coping would serve as mediators of the association between religious involvement and change in a number of the health behaviors over time in our longitudinal data.
Based on a previous longitudinal analysis of the current study data (Roth et al., 2016), we further hypothesized that religious behaviors would predict changes in religious beliefs over time. Because extensive previous research suggests overall effects of religious beliefs/behaviors on health-related outcomes, we did not put forth additional hypotheses about the unmediated or direct effects (“cl’ ” and “ch’ ” in Figure 1).
Method
RHIAA Study
Participants were African American adults from the “Religion and Health in African Americans” (RHIAA) study, which was designed specifically to examine religion-health associations and mediators in a national sample of African American adults. The RHIAA study was not originally designed to be a longitudinal study, and 2,370 participants completed an initial telephone interview (wave 1). Later, when additional support for the study became available, attempts were made to re-contact participants for longitudinal assessments, and follow-up telephone interviews were conducted at waves 2 and 3 at 2.5 and 5.0 years after the initial interview, respectively (Holt et al., 2015). The study sample was enrolled and data collection conducted by an external subcontractor (OpinionAmerica). Sampling and recruitment methods are described in more detail elsewhere (Holt et al., 2015; Roth et al., 2012). Eligible participants spoke English, self-identified as African American, and were 21 years of age or older at the initial interview. Participants provided verbal assent after the interviewers read them an informed consent script, and they received a $25 gift card by mail after completing each interview.
Measures
Religious involvement
Religious involvement was assessed using an instrument previously validated for use with African Americans (Lukwago et al., 2001; Roth et al., 2012). This 9-item instrument assesses two dimensions of involvement: religious beliefs (e.g., “I feel the presence of God in my life.”; “I have a close personal relationship with God.”; Cronbach’s α = .93 in present sample) and religious behaviors (e.g., church service attendance, involvement in other church activities; talking openly about faith with others; Cronbach’s α = .73 in present sample). Seven items use a 5-point Likert-type format, and two service attendance items use a 3-point response format. Subscale scores can range from 4–20 for religious beliefs and 5–21 for religious behaviors, with higher scores indicating greater religious involvement.
Religious coping
The Brief RCOPE was used to assess religious coping (Fetzer Institute: National Institute on Aging Working Group, 1999; Pargament et al., 2011). Positive and negative coping were each assessed using 3 items (e.g., “I work together with God as partners to get through hard times.”, “I wonder whether God has abandoned me.”, respectively). Participants rated each item from 1 (“not at all”) to 4 (“a great deal”) to the extent each statement described how they “try to understand and deal with major problems in your life”. Previous studies have supported the two-factor structure of the Brief RCOPE, with high internal consistency and evidence of discriminant and criterion-related validity (Pargament et al., 2000). Given its brevity (Nunnally & Bernstein, 1994), reliability of the Brief RCOPE was modest in the present sample, (α=.80 for positive religious coping; α=.54 for negative religious coping). Items comprising each scale are summed, yielding a range of 3 to 12 with higher scores indicating great use of religious coping.
Health behaviors
An adaptation of National Cancer Institute’s 5-A-Day Survey was used to assess fruit and vegetable consumption (Block et al., 1986; Kreuter et al., 2005). Seven items assess fruit consumption and 5 items assess vegetable consumption (e.g., “In a typical week, about how many times do you have…a piece of fresh fruit, like an apple, orange, banana, or pear?”). Fifteen different fruits and 18 vegetables are assessed specifically within these items. The response scale ranges from 0 to 8 or more servings per week. Servings per day are computed by summing all items and dividing by 7.
Alcohol and tobacco use were assessed using modules from the Behavioral Risk Factor Surveillance System (BRFSS). Adequate test-retest reliability has been shown in a previous sample of African Americans (Stein, Lederman, & Shea, 1993). The alcohol consumption module included an initial question on any alcohol use in the preceding 30 days. For those who answered “yes,” additional items assessed binge and heavy drinking (“Considering all types of alcoholic beverages, how many times during the past 30 days did you have 4/5 or more drinks on an occasion?”; “During the past 30 days, what is the largest number of drinks you had on any occasion?”). The tobacco use module asked whether the individual smoked cigarettes every day, some days, or not at all. The short form of the International Physical Activity Questionnaire (IPAQ) (Craig et al., 2003) was used to assess physical activity in the last week. This instrument asks about the number of days in the past week and amount of time participants spent engaging in vigorous and moderate activity and walking. Minutes per week are computed.
Cancer screening behaviors
Participants were asked about age-and sex-appropriate cancer screening behaviors using items based on the BRFSS. Screenings included mammography for women, prostate specific antigen and digital rectal examination for men, and fecal occult blood testing, flexible sigmoidoscopy, and colonoscopy for all age-eligible participants. Participants reported whether they ever had the screening, in that recall of screening tests can be difficult for participants and often results in over-reporting and telescoping (McPhee et al., 2002; Rauscher, Johnson, Cho, & Walk, 2008). Finally, the aim was to capture cumulatively over time any changes in the number of people reporting screening tests. Due to ceiling effects, mammography was analyzed as past two years vs. more than two years ago (including never).
Demographics
Participant sex, date of birth, marital status, years of education, employment status, and self-rated health status were recorded in the survey demographics module. This list was based on recommendations about potential confounding variables in religion-and-health research (Powell et al., 2003).
Statistical analyses
All analyses reported here were conducted using structural equation modeling (SEM) procedures as conducted by Mplus version 7.0 (Muthén & Muthén, 2013). Maximum likelihood estimation was used. A modification of the traditional two-step approach (Anderson & Gerbing, 1988) was used such that confirmatory factor analysis models were run first that specified latent factors for religious beliefs, religious behaviors, and the mediator (positive religious coping or negative religious coping) from the observed items for these constructs across all the three assessment waves. After satisfactory fit was obtained for the longitudinal measurement model, structural models were then estimated that included both mediated and unmediated causal effects among the latent constructs. Positive religious coping and negative religious coping were examined in separate models, and each outcome variable was also examined individually. The basic autoregressive structural model used to test the mediation relationships is illustrated in Figure 1.
For the measurement models (not illustrated in Figure 1), factor loadings were constrained to be invariant across the waves for the latent factors that were extracted for each construct. That is, the factor loading for each item on its respective factor was constrained to be equal across waves 1, 2, and 3. This ensured that the identification of the latent factor was identical across time. Item measurement residuals were also estimated at each measurement wave and allowed to correlate across time for each item. The correlated measurement residuals accounted for any item-specific method variance that could not be accounted for by the underlying latent factors.
Structural models were estimated after achieving adequate measurement model fit. These structural models tested the significance of the longitudinal mediation effects, the unmediated or direct effects of religious involvement at wave 1 on health behaviors at wave 3, and the longitudinal predictive effects hypothesized for religious behaviors on subsequent religious beliefs. Autoregressive paths were included such that each latent variable (religious beliefs, religious behaviors, and the mediator) and the outcome variable (denoted as Y in Figure 1) at waves 2 and 3 was predicted by the same latent variable at the previous measurement wave. Consequently, any other variable that predicts a latent variable at wave t is actually predicting a change in that latent variable from wave t-1 to wave t. This applies to both the mediated and the unmediated (or direct) effects.
The mediation paths in Figure 1 extend on the classic a, b, and c’ paths from the mediation literature (MacKinnon, 2008; Maxwell & Cole, 2007; Roth & MacKinnon, 2012). Religious beliefs, religious behaviors, and the mediator are all drawn with ovals in Figure 1 to indicate that these are latent variables extracted from individual items in the measurement model (that is not shown in Figure 1 for clarity). In our notation of the predictive paths in the mediation models, we use subscripts to denote measurement waves, and “l” and “h” to denote paths from religious beliefs and religious behaviors, respectively. Path a121, for example, predicts the mediator at wave 2 from religious beliefs at time 1 (after accounting for the other predictive paths or covariates). Similarly, ch’31 depicts the unmediated or direct effect of religious behaviors at wave 1 on the health outcome at wave 3. Unanalyzed correlations were also estimated among all four variables at each measurement wave (i.e., pairwise residual correlations between Bel3, Beh3, Med3 and Y3 at wave 3, and also at wave 2 and wave 1).
Because this was purely an observational study, with no interventions, and a fairly consistent inter-wave interval of approximately 2.5 years, additional parsimony was achieved by 1) restricting the analysis to 565 African American participants who provided data at all 3 waves, and 2) constraining to be equal the wave 1 → wave 2 paths with the wave 2 → wave 3 paths for the same variables as long as those effects were also adjusted for the same covariates at each wave. Thus, the autoregressive paths for religious beliefs, religious behaviors, and the mediator were all constrained to be equal (e.g., Bel1 → Beh2 was constrained to be equal to Bel2 → Bel3). In addition, al21 and ah21 were constrained to be equal to al32 and ah32, respectively.
All effects in Figure 1 were adjusted for age, sex, years of education, and self-rated health assessed at wave 1. Standardized regression coefficients (STDYX in Mplus) adjusted for covariates and for other predictors illustrated in the model are reported in the tables and tested for statistical significance. The mediation effects (al21*b32 for religious beliefs, ah21*b32 for religious behaviors) were tested for statistical significance using Sobel’s delta method (Sobel, 1982). Models with sex-specific outcomes (e.g., mammography utilization) were not controlled for sex. Model fit for all models was evaluated with chi-square goodness-of-fit tests and the root mean square error of approximation (RMSEA). An RMSEA less than 0.06 was considered to be indicative of excellent model fit (Hu & Bentler, 1999).
RHIAA sample
The RHIAA study included 2,370 individuals at wave 1. Initial Wave 1 response rates were 19% calculated as #accepted / [#accepted + # non-interviewed] (Holt, Clark, Debnam, et al., 2014). Upper bound response rates, or those that included only those individuals who screened as eligible but then refused, were 94% (Holt, Clark, Debnam, et al., 2014). Retention rates from Waves 1 to 3 were 24% (Holt et al., 2015). Previous analyses of retention in the RHIAA study found that the retained participants were slightly but significantly older, more educated, more likely to be female, and less likely to report “poor” self-rated health status than those who were not retained (Holt et al., 2015). The analytic sample for the present paper is comprised of individuals who provided data at each of the three waves of data collection (N=565). Table 1 shows participant characteristics. Table 2 shows the distributions for all study outcome variables.
Table 1.
Baseline characteristics for all participants who were interviewed for all 3 waves
| Variable | All participants (n=565) |
|---|---|
|
| |
| Age, mean ± SD | 58.55 ± 12.08 |
|
| |
| Sex, n (%) | |
| Female | 376 (66.55) |
| Male | 189 (33.45) |
|
| |
| Education, n (%) | |
| ≥College | 333 (59.15) |
| ≤High school | 230 (40.85) |
|
| |
| Marital status, n (%) | |
| Never been married | 56 (9.95) |
| Currently single | 97 (17.23) |
| Separated or divorced | 106 (18.83) |
| Widowed | 95 (16.87) |
| Currently married or living with partner | 209 (37.12) |
|
| |
| Employment, n (%) | |
| Part-time employed | 66 (11.74) |
| Not currently employed | 53 (9.43) |
| Retired | 181 (32.21) |
| Receiving disability | 66 (11.74) |
| Full-time employed | 196 (34.88) |
|
| |
| Health status, n (%) | |
| Poor | 24 (4.25) |
| Fair | 124 (21.95) |
| Good | 199 (35.22) |
| Very good | 144 (25.49) |
| Excellent | 74 (13.10) |
|
| |
| Income, n (%) | |
| ≤$30,000 | 235 (48.16) |
| >$30,000 | 253 (51.84) |
Table 2.
Descriptives of study outcomes at the three study waves
| Variable | N | Wave 1 | Wave 2 | Wave 3 |
|---|---|---|---|---|
| Religious beliefs (/20 max) | 560 | 17.64 (2.98) | 17.72 (2.86) | 17.66 (2.86) |
| Religious behaviors (/21 max) | 553 | 16.21 (3.39) | 16.52 (3.39) | 16.39 (3.39) |
| Positive religious coping (/12 max) | 548 | 10.21 (2.09) | 9.93 (2.16) | 9.76 (2.19) |
| Negative religious coping (/12 max) | 546 | 4.15 (1.65) | 4.13 (1.57) | 4.00 (1.53) |
| Fruit servings per day (/8 max) | 564 | 2.62 (1.34) | 2.38 (1.21) | 2.38 (1.21) |
| Vegetable servings per day (/5.71 max) | 564 | 2.21 (0.94) | 2.12 (0.94) | 1.98 (0.88) |
| Drinking alcohol Y/N in the past 30 days (%) | 563 | 0.40 (0.49) | 0.40 (0.49) | 0.39 (0.49) |
| 4/5 or more alcohol drinks (%) | 509 | 0.51 (2.28) | 0.37 (1.96) | 0.52 (2.73) |
| Largest number of drinksˆ | 520 | 1.01 (1.94) | 0.92 (1.79) | 0.93 (2.07) |
| Currently smoking (%) | 562 | 0.17 (0.38) | 0.16 (0.37) | 0.15 (0.36) |
| Vigorous activities minutes / week | 536 | 170.07 (268.43) | 162.29 (234.51) | 138.59 (226.48) |
| Moderate activities minutes / week | 523 | 148.41 (249.87) | 131.59 (206.18) | 133.15 (219.34) |
| Walking minutes / week | 527 | 232.24 (294.37) | 217.78 (280.85) | 176.72 (249.50) |
| Ever had a mammogram (%) | 348 | 0.95 (0.21) | 0.95 (0.22) | 0.97 (0.17) |
| Last mammogram: past 2 years vs. > 2 years or never (%) | 348 | 0.90 (0.30) | 0.88 (0.33) | 0.89 (0.31) |
| Ever had a PSA test (%) | 157 | 0.78 (0.42) | 0.87 (0.34) | 0.89 (0.32) |
| Ever had a colonoscopy (%) | 382 | 0.74 (0.44) | 0.82 (0.38) | 0.87 (0.34) |
NOTE: Sample sizes, means, standard deviations, and percentages are reported.
Means reflect the majority of participants who reported 0 drinks in the past 30 days for whom a value of 0 was entered.
Results
Measurement model
The measurement model included the previously published 2-factor religious involvement model at wave 1 (Roth, Mwase, et al., 2012) that was expanded by adding waves 2 and 3 and by adding all 3 waves of religious coping items.. For the model that included religious beliefs, religious behaviors, and positive religious coping, excellent fit to the observed data was found (χ2 = 1319.06, df = 666, RMSEA = .042). Excellent fit was also found for the model that included religious beliefs, religious behaviors, and negative religious coping (χ2 = 1286.19, df = 666, RMSEA = .041). All observed items had reasonable and highly significant standardized factor loadings greater than 0.40 on their appropriate latent factors.
Structural mediation models
Positive religious coping mediation effects
Examination of the subscale means in religious coping at the three waves shown in Table 2 shows a slight decrease in positive religious coping over time. The mediation model findings for the latent variable structural models for positive religious coping are shown in Table 3. Overall model fit was good, with RMSEA values at.04 for most models. The al paths, representing the effect of religious beliefs to change in positive religious coping at the following wave, were consistently significant, suggesting that religious beliefs were associated with less decline in positive religious coping over time (ps < .001), while those with low religious beliefs showed greater declines. The ah paths were also significant, suggesting that high religious behaviors were also predictive of less decline in positive religious coping over time (most ps < .01), with those less religiously involved showing greater declines.
Table 3.
Adjusted mediation model using positive religious coping as mediator
| Outcome | al | ah | b32 | Indirect effect | cl | ch | RMSEA | |
|---|---|---|---|---|---|---|---|---|
| al*b32 | ah*b32 | |||||||
| Fruit servings per day1 | 0.230*** | 0.142** | −0.077 | −0.018 | −0.011 | −0.153* | 0.239** | 0.043 |
| Vegetable servings per day1 | 0.230*** | 0.147** | −0.074 | −0.017 | −0.011 | −0.107 | 0.124 | 0.044 |
| Drinking alcohol Y/N in the past 30 days1 | 0.232*** | 0.136** | −0.036 | −0.008 | −0.005 | 0.127* | −0.122 | 0.045 |
| 4/5 or more alcohol drinks1 | 0.232*** | 0.133** | −0.008 | −0.002 | −0.001 | −0.131 | 0.090 | 0.043 |
| Largest number of drinks1 | 0.228*** | 0.141** | −0.004 | −0.001 | −0.001 | 0.062 | −0.039 | 0.043 |
| Currently smoking1 | 0.237*** | 0.131* | 0.018 | 0.004 | 0.002 | −0.002 | 0.000 | 0.044 |
| Vigorous activities minutes / week1 | 0.232*** | 0.139** | −0.037 | −0.009 | −0.005 | 0.042 | 0.023 | 0.042 |
| Moderate activities minutes / week1 | 0.232*** | 0.140** | 0.013 | 0.003 | 0.002 | −0.065 | 0.038 | 0.042 |
| Walking minutes / week1 | 0.228*** | 0.143** | −0.021 | −0.005 | −0.003 | −0.004 | −0.026 | 0.042 |
| Last mammogram (within last 2 years vs. > 2 years or never)2 | 0.125 | 0.124 | −0.035 | −0.004 | −0.004 | 0.082 | −0.019 | 0.045 |
| Ever had a PSA test2 | 0.259*** | 0.204* | −0.115 | −0.030 | −0.023 | −0.063 | 0.346* | 0.053 |
| Ever had a colonoscopy1 | 0.233*** | 0.137** | 0.033 | 0.008 | 0.004 | 0.026 | −0.098 | 0.042 |
Note.
Age, gender, education and self-rated health were adjusted.
Age, education and self-rated health were adjusted.
= p < .05;
= p < .01;
= p < .001
The b32 paths, representing the effect of positive religious coping at wave 2 on the change in the outcome from wave 2 to wave 3, were non-significant. Consequently, none of the al*b32 and ah*b32 paths, representing the indirect/mediation effect of religious beliefs and religious behaviors, respectively, through a change in positive religious coping from wave 1 to wave 2, on the change in the outcome from wave 2 to wave 3, were statistically significant. This indicates that there is no evidence that positive religious coping mediates the relationship between religious beliefs/behaviors and the health behaviors examined.
Negative religious coping mediation effects
Examination of the means in religious coping at the three waves shown in Table 2 shows a negligible decrease in negative religious coping over time. The mediation model findings for the latent variable structural models for negative religious coping are shown in Table 4. Overall model fit was good, with RMSEA values around .04 for most models. The al and ah paths, representing the effect of religious beliefs and religious behaviors, respectively, to change in negative religious coping at the following wave, were non-significant, suggesting that neither religious beliefs nor religious behaviors were not associated with a subsequent change in negative religious coping over time.
Table 4.
Adjusted mediation model using negative religious coping as mediator
| Outcome | al | ah | b32 | Indirect effect | cl | ch | RMSEA | |
|---|---|---|---|---|---|---|---|---|
| al*b32 | ah*b32 | |||||||
| Fruit servings per day1 | 0.016 | −0.105 | 0.035 | 0.001 | −0.004 | −0.177** | 0.212** | 0.040 |
| Vegetable servings per day1 | 0.019 | −0.106 | −0.047 | −0.001 | 0.005 | −0.120 | 0.079 | 0.041 |
| Drinking alcohol Y/N in the past 30 days1 | 0.007 | −0.096 | −0.065 | 0.000 | 0.006 | 0.096 | −0.132* | 0.041 |
| 4/5 or more alcohol drinks1 | 0.015 | −0.095 | 0.010 | 0.000 | −0.001 | −0.131* | 0.087 | 0.041 |
| Largest number of drinks1 | 0.013 | −0.097 | 0.051 | 0.001 | −0.005 | 0.058 | −0.033 | 0.040 |
| Currently smoking1 | 0.024 | −0.109 | 0.002 | 0.000 | 0.000 | 0.015 | −0.008 | 0.041 |
| Vigorous activities minutes / week1 | 0.009 | −0.094 | 0.003 | 0.000 | 0.000 | 0.022 | 0.012 | 0.039 |
| Moderate activities minutes / week1 | 0.012 | −0.097 | −0.023 | 0.000 | 0.002 | −0.065 | 0.059 | 0.040 |
| Walking minutes / week1 | 0.014 | −0.100 | −0.047 | −0.001 | 0.005 | 0.001 | −0.053 | 0.040 |
| Last mammogram (within last 2 years vs. > 2 years or never)2 | 0.073 | −0.129 | −0.004 | 0.000 | 0.001 | 0.081 | −0.023 | 0.044 |
| Ever had a PSA test2 | 0.029 | −0.103 | −0.136 | −0.004 | 0.014 | −0.133 | 0.316** | 0.050 |
| Ever had a colonoscopy1 | 0.016 | −0.103 | −0.097 | −0.002 | 0.010 | 0.029 | −0.094 | 0.040 |
Note.
Age, gender, education and self-rated health were adjusted.
Age, education and self-rated health were adjusted.
= p < .05;
= p < .01;
= p < .001
The b32 paths, representing the effect of negative religious coping at wave 2 on the change in the outcome from wave 2 to wave 3, were non-significant. The al*b32 paths, representing the indirect/mediation effect of religious beliefs through a change in negative religious coping from wave 1 to wave 2, on the change in the outcome from wave 2 to wave 3, were non-significant. This indicates that there is no evidence that negative religious coping mediated the relationship between religious beliefs and the health-related outcomes examined. The same was true for the ah*b32 paths, representing the indirect/mediation effect of religious behaviors through a change in negative religious coping from wave 1 to wave 2, on the change in the outcome from wave 2 to wave 3.
Unmediated effects
The cl’ paths, representing the unmediated/direct effect of religious beliefs at wave 1 on the change in outcomes from wave 2 to wave 3, were largely non-significant. However, religious beliefs at wave 1 were associated with decreases in reported fruit servings per day (p < .05), increases in drinking any alcohol in the past 30 days (p < .05), decreases over time in number of instances of consuming 4 or 5 or more drinks (p < .05). The ch’ paths, representing the unmediated/direct effect of religious behaviors at wave 1 on the change in outcomes from wave 2 to wave 3, were also largely non-significant. However, religious behaviors at wave 1 were associated with increases in fruit servings per day (p < .01), decreased likelihood of alcohol usage in the past 30 days (p < .05), and increases in men’s reporting of ever having had a prostate specific antigen test (p < .05). The findings on fruit servings per day are noteworthy in both the positive and negative religious coping models in that the unmediated effect was positive for religious behaviors but negative for religious beliefs. Because the latent factors for religious beliefs and religious behaviors at wave 1 are substantially correlated (r = 0.69, p < .001 in positive religious coping model and r = 0.14, p < .001 in negative religious coping models) these opposing direct effects on fruit consumption represent suppression effects, with the small negative effect for religious beliefs only emerging as statistically significant when controlling for the stronger positive effect of religious behaviors. The longitudinal predictive paths from religious behaviors at one wave to religious beliefs at the subsequent data collection wave were highly consistent and statistically significant (ps < .001) across all combinations of mediator and outcome models. For the positive coping–fruit servings per day model, for example, the standardized, constrained estimate was 0.156 (standard error = 0.044, p < .001).
Discussion
The present study tested a model of religious coping as a possible mediator of the impact of religious involvement on a variety of health behaviors in a national sample of African Americans. With African Americans having a historically greater level of religious participation than other groups (Taylor, Chatters, & Levin, 2003), and due to the high burden of health disparities that affect this group (Williams, 2012), it is important to identify psychosocial factors that can bolster health outcomes and the mechanisms of those effects. Though there are a number of previous cross-sectional mediational studies of the religion-health connection, including religious coping, there are limitations on conclusions that can be drawn about mediational relationships using cross-sectional data. The present models examined change over time and are therefore considerably more rigorous. In the present case, we are able to assess whether religious beliefs are associated with changes in religious coping over time, and whether those changes are associated with changes in health-related behaviors.
Religious beliefs and behaviors are associated with change in positive religious coping
Consistent with hypothesis one, findings indicate that a person’s religious beliefs (e.g., having a close personal relationship with God or a higher power) and behaviors (e.g., service attendance), appeared to attenuate the modest decreases in positive religious coping observed over the 5-year study period. Stated another way, people low on religious beliefs and behaviors at wave 1 declined more in their use of positive religious coping over time than persons with higher religious beliefs and behaviors. In the absence of theoretical guidance on how religious coping might change over time among African Americans, more research is needed to further examine and interpret the decrease in positive religious coping over time. It is possible that something in the historical context influenced religious coping strategies in the sample such as changes in the economic or political context. Yet we must also consider the meaning of an almost half-point decline on a 12-point scale. Notably, neither religious beliefs nor participation/behaviors were associated with a change in negative religious coping over time. Negative religious coping remained uniformly rare in this sample over the study period relative to positive coping, which is consistent with previous cross sectional literature (Pargament et al., 2011).
Religious coping and change in health behaviors over time
The second hypothesis involved the relationship between the mediator and the outcome. Our longitudinal findings indicate that neither positive nor negative religious coping had any effects for predicting changes on health outcomes. The absence of these mediator-outcome relationships precluded the ability to detect mediation effects. In our previous cross-sectional analysis, we did find concurrent associations between religious coping and some of the health behaviors within this study sample (Holt, Clark, Debnam, et al., 2014). We reported that positive religious coping was positively associated with vegetable servings, while negative religious coping was negatively associated with vegetable servings and positively with heavy drinking behaviors. These relationships were not confirmed with the more rigorous prospective analyses. It could be that the cross-sectional associations observed previously are due to other third variables, or that the relationships remain stable across this time period, limiting opportunities to detect causal relationships that may evolve more slowly over longer time periods.
Role of religious beliefs vs. behaviors
The findings provide modest support for the third hypothesis, that religious beliefs have a greater presence in the models overall than do religious behaviors. However, the ability to draw such conclusions is somewhat limited by the overall absence of mediation in the models we tested. Both religious beliefs and behaviors showed direct effects with regard to the health behaviors. Similar effects were previously reported in this sample using cross-sectional data (Holt, Clark, Debnam, et al., 2014). However the present study examined the role of religious involvement in change over time in these behaviors, making for a more dynamic analysis. For example, religious behaviors were positively associated with increases in men’s reports of having a prostate specific antigen test over time. This could be due to the religious social support that African American men receive from religious participation, which may facilitate interaction with the health care system.
Role of positive vs. negative religious coping
Based on previous research, our fourth hypothesis was that negative religious coping would be a stronger predictor in the structural models than positive religious coping. This hypothesis was not supported in the current analysis due to the absence of significant coping-health outcome relationships. To our knowledge, aside from our earlier cross-sectional analyses of the present sample, very little research has examined religious coping in the context of health behaviors. We had speculated that a higher reliance on generally salutary positive religious coping might thus resolve people’s problems more effectively, leaving more resources for engaging in healthy lifestyle behaviors while reliance on negative religious coping might lead individuals to turn to unhealthy behaviors such as a poor diet or lack of exercise as alternative coping efforts (Park & Iacocca, 2014).
Religious coping as a religion-health mediator
The present study failed to support the fifth hypothesis involving a mediational role of either positive or negative religious coping largely due to the lack of an association between coping and changes in the health behaviors over time. In our previous cross-sectional analysis (Holt, Clark, Debnam, et al., 2014), both positive and negative religious coping mediated the relationship between religious beliefs and vegetable consumption, and, in addition, positive religious coping mediated the relationship between religious behaviors and vegetable consumption. Further, negative religious coping mediated the relationship between religious beliefs and both heavy drinking behaviors. The current lack of mediational findings do not necessarily negate the previous cross-sectional evidence for mediation because it is possible that the previous analyses highlighted a causal process that occurred earlier in the life histories of the study sample or that the relationships remain constant over time. The conflicting findings do suggest that future research could be helpful in continuing to clarify these complex relationships.
Strengths and limitations
The current study has a number of strengths. The RHIAA dataset provided a very rare opportunity to observe and examine complex longitudinal relationships between religious involvement and a variety of health protective and risk behaviors in an important group from a public health and health disparities perspective. Rather than conducting an opportunistic secondary data analysis that may result in sub-optimal operationalization of constructs, the RHIAA study was designed specifically to examine multidimensional religious involvement and relationships with health while being able to control for recognized confounders (Powell et al., 2003). There are also limitations of this work that should be acknowledged. Because the RHIAA study was not originally designed for participant re-contact, retention rates are limited and may introduce some bias (as previously described). While the sample was probability-based, it should not be considered representative. The RHIAA sample was comprised of more women than men. Educational level in the sample is comparable to national data (U. S. Census Bureau, 2015). We did not have sufficient power to examine denominational differences, a potential avenue for future research. The sample was 54.4% Baptist, which is somewhat greater than the national average for African Americans (40%; Pew Forum US, 2009), and all other denominations in the RHIAA sample comprised no more than 5.5%. Finally, many of the study variables had limited opportunity to exhibit change during the 5-year study period as opposed to having a longer follow-up. This may have limited the ability of the present longitudinal models to detect mediation.
Implications and conclusions
The present findings may have implications for pastoral counseling and other faith-based interventions. To the extent that positive religious coping has been found to be associated with a wide array of health and well-being outcomes (Pargament et al., 2011), interventions to maintain this coping strategy might be considered helpful. The current findings suggest that the use of positive religious coping can change over time and those changes can include decreases, which might jeopardize well-being in African Americans. If religious beliefs can play a role in reducing such decreases in religious coping, perhaps interventions for African Americans can encourage the maintenance of a strong religious belief system, prayer, and a relationship with a higher power (such as God or another). There may also be implications for non-faith based interventions, in which therapists should understand the potential benefits of religious involvement for their religious clients, including helping to cope with life’s stressors, provision of social support, and the experience of meditation/mindfulness. Though the current findings are only an initial look into the complex longitudinal relationships between multidimensional religious involvement, religious coping strategies, and various health-related behaviors, they do point to important connections between religious beliefs and positive religious coping among African American men and women, while continuing to confirm associations between religious involvement and lifestyle behaviors related to chronic diseases that take a disproportionate toll on these communities.
Research highlights.
The longitudinal effects of religion on health for African Americans are not known.
Religious involvement may impact health through effects on religious coping.
Religious coping was found to be malleable over time.
High religious beliefs preserved positive religious coping levels over time.
Findings inform how religion and health co-evolve over time in African Americans.
Acknowledgments
The team would like to acknowledge the work of OpinionAmerica and Tina Madison who conducted participant recruitment/retention and data collection activities for the present study.
This work was supported by grants from the National Cancer Institute, (#1 R01 CA 105202; #1 R01 CA154419) and a grant from the Duke University Center for Spirituality, Theology, and Health, through the John Templeton Foundation (#11993). The study was approved by the University of Maryland Institutional Review Board (#373528-1).
Footnotes
The authors have no disclosures to report.
Literature Cited
- Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin. 1988;103(3):411–423. doi: 10.1037/0033-2909.103.3.411. [DOI] [Google Scholar]
- Block G, Hartman AM, Dresser CM, Carroll MD, Gannon J, Gardner LA. A data-based approach to diet questionnaire design and testing. American Journal of Epidemiology. 1986;124(3):453–469. doi: 10.1093/oxfordjournals.aje.a114416. [DOI] [PubMed] [Google Scholar]
- Chatters LM. Religion and health: Public health research and practice. Annual Review Public Health. 2000;21:335–367. doi: 10.1146/annurev.publhealth.21.1.335. [DOI] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, Oja P. International physical activity questionnaire: 12-country reliability and validity. Medicine and; Science in Sports and; Exercise. 2003;35(8):1381–1395. doi: 10.1249/01.mss.0000078924.61453.fb. [DOI] [PubMed] [Google Scholar]
- Ellison CG, Hummer RA. Religion families and health: Population-based research in the United States. New Brunswick, NJ: Rutgers University Press; 2010. [Google Scholar]
- Ellison CG, Levin JS. The religion-health connection: Evidence, theory, and future directions. Health Education & Behavior. 1998;25(6):700–720. doi: 10.1177/109019819802500603. [DOI] [PubMed] [Google Scholar]
- Exline JJ, Rose ED. Religious and Spiritual Struggles. In: Paloutzian RF, CL P, editors. Handbook of the psychology of religion and spirtiaulity. 2nd. New York: Guilford Press; 2013. pp. 380–397. [Google Scholar]
- Fetzer Institute: National Institute on Aging Working Group. Multidimensional measurement of religiousness/Spirituality for use in health research. Kalamazoo, MI: John E. Fetzer Institute; 1999. [Google Scholar]
- George LK, Larson DB, Koenig HG, McCullough ME. Spirituality and health: What we know, what we need to know. Journal of Social and Clinical Psychology. 2000;19(1):102–116. doi: 10.1521/jscp.2000.19.1.102. [DOI] [Google Scholar]
- Gerber MM, Boals A, Schuettler D. The unique contributions of positive and negative religious coping to posttraumatic growth and PTSD. Psychology of Religion and Spirituality. 2011;3(4):298–307. doi: 10.1037/a0023016. [DOI] [Google Scholar]
- Hebert R, Zdaniuk B, Schulz R, Scheier M. Positive and negative religious coping and well-being in women with breast cancer. Journal of Palliative Medicine. 2009;12(6):537–545. doi: 10.1089/jpm.2008.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill PC, Hood RW Jr, editors. Measures of religiosity. Birmingham, AL: Religious Education Press; 1999. [Google Scholar]
- Holt CL, Clark EM, Debnam KJ, Roth DL. Religion and Health in African Americans: The Role of Religious Coping. American Journal of Health Behavior. 2014;38(2):190–199. doi: 10.5993/AJHB.38.2.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt CL, Clark EM, Roth DL. Positive and Negative Religious Beliefs Explaining the Religion-Health Connection Among African Americans. International Journal for the Psychology of Religion. 2014;24(4):311–331. doi: 10.1080/10508619.2013.828993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt CL, Le D, Calvanelli J, Huang J, Clark E, Roth DL, Schulz E. Participant retention in a longitudinal national telephone survey of African American men and women. Ethnicity and Disease. 2015;25(1):187–192. [PMC free article] [PubMed] [Google Scholar]
- Koenig HG, King DE, Carson VB. Handbook of Religion and Health. 2nd. New York, NY: Oxford University Press; 2012. [Google Scholar]
- Koenig HG, McCullough ME, Larson DB. Handbook of Religion and Health. New York, NY: Oxford University Press, USA; 2001. [Google Scholar]
- Kreuter MW, Skinner CS, Holt CL, Clark EM, Haire-Joshu D, Fu Q, Bucholtz DC. Cultural tailoring for mammography and fruit and vegetable consumption among low-income African American women in urban public health centers. Preventive Medicine. 2005;41(1):53–62. doi: 10.1016/j.ypmed.2004.10.013. [DOI] [PubMed] [Google Scholar]
- Levin JS, Vanderpool HY. Is religion therapeutically significant for hypertension? Social Science and Medicine. 1989;29(1):69–78. doi: 10.1016/0277-9536(89)90129-9. [DOI] [PubMed] [Google Scholar]
- Lincoln CE, Mamiya LH. The black church in the African American experience. Durham, NC: Duke University Press; 1990. [Google Scholar]
- Lukwago SL, Kreuter MW, Bucholtz DC, Holt CL, Clark EM. Development and validation of brief scales to measure collectivism, religiosity, racial pride, and time orientation in urban African American women. Family and Community Health. 2001;24(3):63–71. doi: 10.1097/00003727-200110000-00008. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Erlbaum Associates; 2008. [Google Scholar]
- Maselko J, Hayward RD, Hanlon A, Buka S, Meador K. Religious Service Attendance and Major Depression: A Case of Reverse Causality? American Journal of Epidemiology. 2012;175(6):576–583. doi: 10.1093/aje/kwr349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maxwell SE, Cole DA. Bias in cross-sectional analyses of longitudinal mediation. Psychological Methods. 2007;12(1):23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- McPhee SJ, Nguyen TT, Shema SJ, Nguyen B, Somkin C, Vo P, Pasick R. Validation of recall of breast and cervical cancer screening by women in an ethnically diverse population. Preventive Medicine. 2002;35(5):463–473. doi: 10.1006/pmed.2002.1096. [DOI] [PubMed] [Google Scholar]
- Musick MA, Traphagan JW, Koenig HG, Larson DB. Spirituality in physical health and aging. Journal of Adult Development. 2000;7(2):73–86. doi: 10.1023/A:1009523722920. [DOI] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 7th. Los Angeles, CA: 2013. [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric theory. New York: McGraw-Hill, Inc; 1994. [Google Scholar]
- Oman D, Thoresen CE. Does religion cause health? Differing interpretations and diverse meanings. Journal of Health Psychology. 2002;7(4):365–380. doi: 10.1177/1359105302007004326. [DOI] [PubMed] [Google Scholar]
- Pargament KI, Falb K, Ano G, Wachholtz AB. The religious dimension of coping: Advances in theory, research, and practice. In: Park RPaC., editor. The Handbook of Pscyhology of Religion. 2nd. New York: Guilford Press; 2013. pp. 560–580. [Google Scholar]
- Pargament KI, Feuille M, Burdzy D. The Brief RCOPE: Current psychometric status of a short measure of religious coping. Religions. 2011;2:51–76. doi: 10.3390/rel2010051. [DOI] [Google Scholar]
- Pargament KI, Koenig HG, Perez LM. The many methods of religious coping: development and initial validation of the RCOPE. Journal of Clinical Psychology. 2000;56(4):519–543. doi: 10.1002/(sici)1097-4679(200004)56:4<519::aid-jclp6>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pargament KI, Smith BW, Koenig HG, Perez L. Patterns of positive and negative religious coping with major life stressors. Journal for the Scientific Study of Religion. 1998;37(4):710–724. doi: 10.2307/1388152. [DOI] [Google Scholar]
- Park CL, Edmondson D, Blank TO. Religious and Non-Religious Pathways to Stress-Related Growth in Cancer Survivors. Applied Psychology: Health and Well-Being. 2009;1(3):321–335. [Google Scholar]
- Park CL, Holt CL, Le D, Christice J, Williams B. Positive and negative religious coping styles as prospective predictors of well-being in African Americans. Psychology of Religion and Spirituality. doi: 10.1037/rel0000124. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park CL, Iacocca MO. A stress and coping perspective on health behaviors: theoretical and methodological considerations. Anxiety Stress Coping. 2014;27(2):123–137. doi: 10.1080/10615806.2013.860969. [DOI] [PubMed] [Google Scholar]
- Pew Forum US. A religious portrait of African-Americans. 2009 Retrieved from http://www.pewforum.org/A-Religious-Portrait-of-African-Americans.aspx.
- Powell LH, Shahabi L, Thoresen CE. Religion and spirituality: Linkages to physical health. American Psychologist. 2003;58(1):36–52. doi: 10.1037/0003-066x.58.1.36. [DOI] [PubMed] [Google Scholar]
- Rauscher GH, Johnson TP, Cho YI, Walk JA. Accuracy of self-reported cancer screening histories: A meta-analysis. Cancer Epidemiology, Biomarkers, and Prevention. 2008;17:748–757. doi: 10.1158/1055-9965.EPI-07-2629. [DOI] [PubMed] [Google Scholar]
- Roesch SC, Ano G. Testing an Attribution and Coping Model of Stress: Religion as an Orientation System. Journal of psychology and Christianity. 2003;22(Part 3):197–209. [Google Scholar]
- Roth DL, MacKinnon DP. Mediation analysis with longitudinal data. In: Newsom JT, Jones RN, Hofer SM, editors. Longitudinal data analysis: A practical guide for researchers in aging, health, and social sciences. New York: Routledge; 2012. pp. 181–216. [Google Scholar]
- Roth DL, Mwase I, Holt CL, Clark EM, Lukwago S, Kreuter MW. Religious involvement measurement model in a national sample of African Americans. Journal of Religion and Health. 2012;51(2):567–578. doi: 10.1007/s10943-011-9475-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth DL, Usher T, Clark EM, Holt CL. Religious Involvement and Health Over Time: Predictive Effects in a National Sample of African Americans. Journal for the Scientific Study of Religion. 2016;55(2):417–424. doi: 10.1111/jssr.12269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman AC, Plante TG, Simonton S, Latif U, Anaissie EJ. Prospective study of religious coping among patients undergoing autologous stem cell transplantation. Journal of Behavioral Medicine. 2009;32(1):118–128. doi: 10.1007/s10865-008-9179-y. [DOI] [PubMed] [Google Scholar]
- Sherman AC, Simonton S, Latif U, Spohn R, Tricot G. Religious struggle and religious comfort in response to illness: health outcomes among stem cell transplant patients. Journal of Behavioral Medicine. 2005;28(4):359–367. doi: 10.1007/s10865-005-9006-7. [DOI] [PubMed] [Google Scholar]
- Sobel ME. Asymptotic Confidence Intervals for Indirect Effects in Structural Equation Models. Sociological Methodology. 1982;13:290–312. doi: 10.2307/270723. [DOI] [Google Scholar]
- Stein AD, Lederman RI, Shea S. The Behavioral Risk Factor Surveillance System questionnaire: its reliability in a statewide sample. American Journal of Public Health. 1993;83(12):1768–1772. doi: 10.2105/AJPH.83.12.1768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor RJ, Chatters LM, Levin J. Religion in the lives of African Americans: Social, psychological, and health perspectives. Thousand Oaks, CA: Sage Publications; 2003. [Google Scholar]
- Thoresen CE. Spirituality, health, and science: The coming revival? In: Roth-Roemer S, Kurpius SR, editors. The emerging role of counseling psychology in health care. New York: W. W. Norton; 1998. pp. 409–431. [Google Scholar]
- U. S. Census Bureau. Educational Attainment in the United States. 2015 Retrieved from https://www.census.gov/library/publications/2016/demo/p20-578.html.
- Williams DR. Miles to go before we sleep: racial inequities in health. Journal of health and social behavior. 2012;53(3):279–295. doi: 10.1177/0022146512455804. [DOI] [PMC free article] [PubMed] [Google Scholar]


