The many challenges of multimorbidity
The dramatic rise in long-term conditions (LTCs) represents a major challenge for individuals, families, and healthcare systems worldwide [1]. Due to the scale of this rise, the management of patients with LTCs largely falls within the domain of primary rather than secondary care, at least in countries with well-developed primary care systems. For example, in the UK, which has a comprehensive primary care system based around general practice (trained family physicians working in multidisciplinary teams) and funded by the National Health Service (NHS), primary care contacts account for around 90% of the total activity of the NHS, and patients with LTCs account for 80% of general practice consultations [2]. Effective primary care and community-based management of people with LTCs is thus a top priority [2–6].
Multimorbidity (usually defined as the co-existence of two or more LTCs in an individual, though definitions vary) [7] is the norm rather than the exception for people with LTCs in the UK [8, 9] and elsewhere [10–12], and is related to both increasing age [13] and socio-economic deprivation [9]. Multimorbidity cuts across the vertical paradigms in which most health research is envisaged and funded [14]. Patients with multimorbidity are usually excluded from such research and thus the nature and complex needs of such patients are not well understood and the evidence-base on which to treat them is lacking [14–17].
Our knowledge and understanding of variations in the effect of multimorbidity on issues such as illness burden [18], quality of life and well-being [19], treatment burden [20], and unmet needs [9], remain poor. Furthermore, studies on the quality of primary care [21, 22] and other community-based resources [23] and their impact on patients with multimorbidity are also rare.
Where should we begin?
Despite the high prevalence of multimorbidity and the key role of primary care in its management, the evidence-base for interventions in this group in primary care is extremely limited [24]. More research on interventions in primary care for people with multimorbidity is urgently needed, but what should these interventions be based on? How do we know what is likely to help?
An important precursor to developing effective interventions is knowledge of the effects of multimorbidity over time and the factors which influence these effects. Prospective cohort studies are the most robust method of studying and describing the natural history and development of morbidity and also for the development and implementation of prognostic models [25, 26]. However, a recent systematic review of prospective cohort studies of multimorbidity in primary care identified only a handful of studies [27]. Although the studies identified provide some useful information, they also demonstrate the significant gaps that exist in knowledge.
To plan future healthcare services and treatment guidelines for those with multimorbidity we must better understand the personal experience, treatment, and health service use, and the psychological, physical, and social factors that influence multimorbidity. Fortunately, several new large cohort studies are underway in Canada and Europe, which will yield important information in the years to come [28–30].
The MALT study
We have also been working to establish such a cohort in Scotland, a devolved nation within the UK that is responsible for its own health budget and for how NHS services are configured. The Scottish Multiple And Long-Term conditions (MALT) cohort study aims to support essential research on issues such as:
The natural history and impact of multimorbidity (including predictors of poor outcomes)
The relationships between multimorbidity and the accessibility, use, and costs of primary care, other health and social care services and community-based resources
The influence of multimorbidity on patient engagement, activation, and self management
The process and outcome of clinical encounters over time and factors promoting or hindering the development of preventive (anticipatory) patterns of care
The quality and safety of care in such patients
The components and combinations of primary care and other supports that work best in multimorbidity.
Additionally, future linked studies could include complex interventions and genetic and environmental predictors of morbidity and poor outcomes in multimorbidity. The framework for the MALT study is shown in Figure 1.
Figure 1.
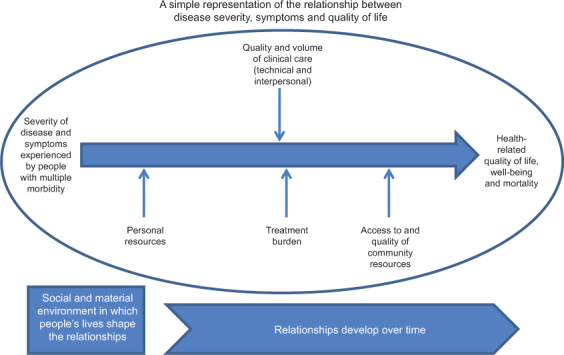
Framework for the Scottish Multiple And Long-Term conditions (MALT) prospective, cohort study.
In developing the MALT study (see Figure 2), we have been assisted by a 2-year international Visiting Professor Award (J.G.) and funding for two part-time post-doctoral researchers by the Scottish School of Primary Care. Work to date has included a systematic review [27], ongoing secondary analysis of a nationally representative cross-sectional primary care database of 1.8 million people with up to 40 LTCs, and identification of existing longitudinal data amendable to secondary analysis. A series of stakeholder meetings have also been held with affiliated MALT researchers in Scotland, qualitative interviews with senior policy makers and NHS strategists, and a 1-day international workshop with experts in multimorbidity research from Canada, Australia, Ireland, England, and Scotland.
Figure 2.
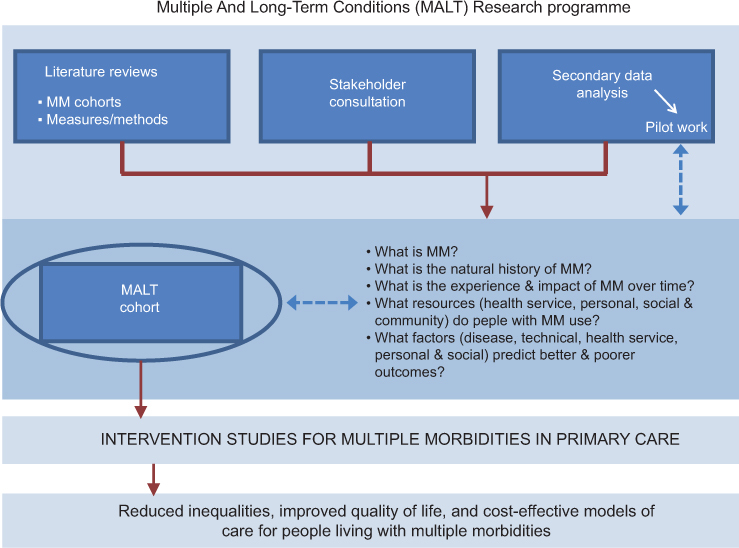
Research programme of the Scottish Multiple And Long-Term conditions (MALT) prospective, cohort study. MM, multimorbidity.
Key areas of discussion in these meetings included defining the primary aims of the prospective cohort study, how best to define and measure multimorbidity, and whether to include a wide range of conditions in order to be as inclusive as possible or to focus on a limited number of LTCs of key public health concern. Consideration was also given as to how best to capture the required data, including what can be measured from routinely collected data, data linkage issues, and what new data need to be collected by direct methods, including survey methods and longitudinal qualitative interviews. The importance of international collaboration was also emphasized so that studies carried out in one country might have relevance in other countries, with the possibility of linked cohorts to aid our global understanding of the common issues in multimorbidity and its management.
Central to all future work on multimorbidity must be a focus on the patient as a functioning person, integrated within a family and a community. Nowhere in medicine is person-centred care more appropriate than in individuals with multimorbidity, with their complex physical and psychosocial needs [9, 10, 13, 31], and yet there has been surprisingly little research on this in this group in terms of patients’ expectations, the doctor–patient relationship, the process and outcomes of clinical encounters, and the importance of human aspects of care such as practitioner empathy [32].
The need for prospective cohort studies
In conclusion, multimorbidity now represents the norm not the exception in individuals with LTCs, and is arguably the biggest challenge facing healthcare systems globally. Strong primary care systems are required to deliver the holistic, person-centred care that the complexity of multimorbidity demands. However, the evidence-based for effective interventions in multimorbidity in primary care is weak, and prospective cohort studies are required to gain a better understanding of the natural history and trajectory of multimorbidity in different populations, and how healthcare and other services can best be configured to meet the needs of people with multimorbidity. Given the vertical paradigm that currently still dominates healthcare, medical education, and research, there is much work that needs to be done.
Acknowledgments
We would like to thank the Scottish School of Primary Care for funding the 2-year Visiting Professor Award held by Professor Jane Gunn with the University of Glasgow, Scotland. This funding also supports Emma France and Gary Mclean, whose valuable input we would also like to acknowledge.
Professor Stewart Mercer, Professor Jane Gunn, and Professor Sally Wyke are the Principal Investigators of the MALT Study. Co-investigators are (in alphabetical order): Dr Diane Dixon, University of Strathclyde, Glasgow; Dr Josie Evans, University of Stirling, Scotland; Dr Elisabeth Fenwick, University of Glasgow; Professor Bruce Guthrie, University of Dundee, Scotland; Professor Phil Hannaford, University of Aberdeen; Scotland, Professor Kate Hunt, MRC Social and Public Health Sciences Unit, Glasgow; Professor Frances Mair, University of Glasgow; Professor Alex McConnachie, University of Glasgow; Professor Margaret Maxwell, University of Stirling; Professor Graham Watt, University of Glasgow.
Contributors to the international workshop on cohorts studies in multimorbidity held in Glasgow, Scotland in April 2011 included, in addition to those named above: Dr Pete Bower, University of Manchester, England; Professor Martin Fortin, Sherbrooke University, Canada (invited keynote speaker); Maureen Johnson, University of Glasgow; Professor Anne-Louis Kinmonth, University of Cambridge, England; Kerry Kuluski, visiting researcher from Canada, based at the University of Oxford, England; Andrew Murphy, University of Galway, Ireland; Rosaleen O’Brien, University of Glasgow; Professor Chris Salisbury, University of Bristol, England; Professor Susan Smith, Trinity College, Dublin, Ireland.
Conflicts of interest
None declared.
Funding
Scottish School of Primary Care.
References
- 1.Mathers CD, Lancar D. Updated projections of global mortality and burden of disease, 2002–2030: data sources, methods, and results. Evidence and Information for Policy Working Paper. Geneva: World Health Organization; 2005. Available from: http://www.who.int/healthinfo/statistics/bod_projections2030_paper.pdf [last accessed Nov 1, 2011] [Google Scholar]
- 2.Department of Health. Supporting people with long term conditions: an NHS and Social Care Model to support local innovation and integration. London: Department of Health; 2005. [Google Scholar]
- 3.Audit Scotland. Managing long-term conditions. Edinburgh: Audit Scotland; 2007. Available from: at http://www.audit-scotland.gov.uk/docs/health/2007/nr_070816_managing_long_term.pdf [last accessed Nov 1, 2011]. [Google Scholar]
- 4.Building a health service fit for the future: a national framework for service change in the NHS in Scotland (‘The Kerr Report’) Scottish Executive Health Department, Edinburgh: Scottish Executive; 2005. ISBN: 075594545X. [Google Scholar]
- 5.Scottish Government. Better Health, Better Care. A discussion document. Scottish Government Health Department; 2007. [Google Scholar]
- 6.Scottish Executive Health Department. Delivering for Health. Edinburgh: Scottish Executive; 2005. [Google Scholar]
- 7.Valderas JM, Starfield B, Sibbald B, Salisbury C, Roland M. Defining comorbidity: implications for health and health services. Ann Fam Med. 2009;7:357–63. doi: 10.1370/afm.983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Measuring long-term conditions in Scotland. Edinburgh: Information Services Division, NHS National Services, Scotland; 2008. Available from: http://www.isdscotland.scot.nhs.uk [last accessed Nov 1, 2011] [Google Scholar]
- 9.Mercer SW, Watt GMC. The inverse care law: clinical primary care encounters in deprived and affluent areas of Scotland. Ann Fam Med. 2007;5:503–7. doi: 10.1370/afm.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wong SYS, Mercer SW, Woo J, Leung S. The influence of multi-morbidity, self-perceived socio-economic standing on the prevalence of depression in an elderly Hong Kong population. BMC Public Health. 2008;8:119. doi: 10.1186/1471-2458-8-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fortin M, Bravo G, Hudon C, Vanasse A, Lapointe L. Prevalence of multimorbidity among adults seen in family practice. Ann Fam Med. 2005;3:223–8. doi: 10.1370/afm.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol. 1998;51:367–75. doi: 10.1016/s0895-4356(97)00306-5. [DOI] [PubMed] [Google Scholar]
- 13.Lyness J, Niculescu A, Tu Xin, Reynolds CF, Caine ED. The relationship of medical comorbidity and depression in older, primary care patients. Psychosomatics. 2006;47:435–9. doi: 10.1176/appi.psy.47.5.435. [DOI] [PubMed] [Google Scholar]
- 14.Mercer SW, Smith SM, Wyke S, O’Dowd T, Watt GCM. Multimorbidity in primary care: developing the research agenda. Fam Pract. 2009;26:79–80. doi: 10.1093/fampra/cmp020. [DOI] [PubMed] [Google Scholar]
- 15.Smith SM, O’Dowd T. Chronic diseases: what happens when they come in multiples? Br J Gen Pract. 2007;57:268–70. [PMC free article] [PubMed] [Google Scholar]
- 16.Fortin M, Soubhi H, Hudon C, Bayliss EA, van den Akker M. Multimorbidity’s many challenges. Br Med J. 2007;334:1016–7. doi: 10.1136/bmj.39201.463819.2C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Starfield B. Threads and yarns: weaving the tapestry of comorbidity. Ann Fam Med. 2006;4:1. doi: 10.1370/afm.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Corbin JM, Strauss A. Unending work and care: managing chronic illness at home. San Francisco: Jossey-Bass; 1988. [Google Scholar]
- 19.Fortin M, Bravo G, Hudon C, Lapointe L, Almirall J, Dubois MF, et al. Relationship between multimorbidity and health-related quality of life of patients in primary care. Qual Life Res. 2006;15:83–91. doi: 10.1007/s11136-005-8661-z. [DOI] [PubMed] [Google Scholar]
- 20.May C, Montori VM, Mair FS. We need minimally disruptive medicine. Br Med J. 2009;339:485–7. doi: 10.1136/bmj.b2803. [DOI] [PubMed] [Google Scholar]
- 21.Heath I, Rubinstein A, Stange KC, van Driel ML. Quality in primary health care: a multidimensional approach to complexity. Br Med J. 2009;338:b1242. doi: 10.1136/bmj.b1242. doi:10.1136/bmj.b1242. [DOI] [PubMed] [Google Scholar]
- 22.Higashi T, Wenger NS, Adams JL, Fung C, Roland M, et al. Relationship between number of medical conditions and quality of care. N Engl J Med. 2007;356:2496–504. doi: 10.1056/NEJMsa066253. [DOI] [PubMed] [Google Scholar]
- 23.“Gaun Yersel!”: The self-management strategy for long term conditions in Scotland. Glasgow: Long-term Conditions Alliance Scotland; 2009. Available from: http://www.ltcas.org.uk/index.php?id=47 [last accessed Nov 1, 2011] [Google Scholar]
- 24.Smith SM, Soubhi H, Fortin M, Hudon C, O’Dowd T. Interventions to improve outcomes in patients with multimorbidity in primary care and community settings. Cochrane Database of Systematic Reviews: Protocols 2007. Issue 2. Chichester, UK: John Wiley & Sons, Ltd; 2007. [Google Scholar]
- 25.Gordis L. Epidemiology. 2nd Ed. Philadelphia: W.B. Saunders & Co.; 2000. [Google Scholar]
- 26.Moons K, Royston P, Vergouwe Y, Grobbe D, Altman D. Prognosis and prognostic research: what, why and how? Br Med J. 2009;338:375. [Google Scholar]
- 27.France E, France EF, Wyke S, Gunn JM, Mair F, McLean G, et al. A systematic review of prospective cohort studies of multimorbidity in primary care. Br J Gen Pract. doi: 10.3399/bjgp12X636146. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van den Akker M, Spigt M, De Raeve L, van Steenkiste B, Metsemakers JF, van Voorst EJ, et al. The SMILE study: a study of medical information and lifestyles in Eindhoven, the rationale and contents of a large prospective dynamic cohort study. BMC Public Health. 2008;8:19. doi: 10.1186/1471-2458-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Haggerty J, Fortin M, Beaulieu M-D, Denis J-L, Roberge D, Hudon C, et al. Program of Research on the Evolution of a Cohort Investigating Health System Effects (PRECISE) Available from: http://www.programmeprecise.ca/en/home [last accessed Nov 1, 2011] [Google Scholar]
- 30.Schafer I, Hansen H, Schon G, et al. The German MultiCare-study: Patterns of multimorbidity in primary health care – protocol of a prospective cohort study. BMC Health Serv Res. 2009;9:145. doi: 10.1186/1472-6963-9-145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gunn J, Ayton D, Densley K, Pallant J, Chondros P, Herrman H, et al. The association between chronic illness, multimorbidity and depressive symptoms in an Australian primary care cohort. Soc Psychiatr Epidemiol. 2010 doi: 10.1007/s00127-010-0330-z. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 32.Neumann M, Bensing J, Mercer S, Ernstmann N, Ommen O, Pfaff H. Analyzing the ‘‘nature’’ and ‘‘specific effectiveness’’ of clinical empathy: A theoretical overview and contribution towards a theory-based research agenda. Patient Educ Counsel. 2009;74:339–46. doi: 10.1016/j.pec.2008.11.013. [DOI] [PubMed] [Google Scholar]


