Abstract
IN BRIEF Although the Look AHEAD (Action for Health in Diabetes) trial, which spanned more than 8 years, did not find significant differences in cardiovascular morbidity and mortality between study groups, it did demonstrate significant differences in weight loss and maintenance. Using lessons learned from the Look AHEAD protocol, clinicians can help people with type 2 diabetes lose weight, improve glucose management, increase physical activity, alter eating patterns, and support long-term positive health outcomes. It remains important, however, to avoid assigning a higher priority to weight loss goals than to improvements in glucose management, long-term health outcomes, and quality of life.
The Look AHEAD (Action for Health in Diabetes) trial has yielded years’ worth of data on the impact of an intensive lifestyle intervention (ILI) on health outcomes, including cardiovascular disease (CVD) morbidity and mortality, weight changes, and glycemic control relative to a control group receiving diabetes support and education (DSE). The study, a randomized clinical trial of >5,000 overweight or obese people with type 2 diabetes, sought to determine the impact of the ILI focusing on weight loss on CVD outcomes; the ultimate finding was that the intervention did not reduce the rate of cardiovascular events between the two study groups (1). However, there were significant differences between the two study groups in other areas of interest, and the wealth of available data and long duration of the trial left ample room to mine and translate information for implementation in clinical practice.
The Look AHEAD trial was significant because it was the largest and longest randomized trial evaluating the impact of an ILI on weight (2). The study’s long duration also allowed for fully assessing the intervention’s impact on the maintenance of weight loss; although the greatest weight losses were achieved by 1 year, many subjects sustained a portion of their weight loss throughout the 8-year study period. Deeper analysis of study subgroups continues to generate information that can inform diabetes treatment methods.
The Look AHEAD Trial: A Brief Summary
Study subjects were randomized to the ILI group or a group receiving enhanced usual care that included DSE (3). The primary goals of the ILI were to achieve significant weight loss (defined as ≥7% of baseline weight) and increase physical activity to ≥175 min/week of moderate activity (3). Weight loss was achieved primarily through reduction of caloric intake, and participants were prescribed calorie thresholds based on their baseline weight: 1,200–1,500 kcal/day for participants weighing <250 lb and 1,500–1,800 kcal/day for participants weighing ≥250 lb. These intake levels were achieved via structured, portion-controlled meal plans, calorie-counting references (booklets provided), and meal replacements. From months 1 to 6, participants were encouraged to replace two meals and one snack daily with liquid shakes or meal bars, and from month 7 onward, one meal per day was to be replaced with a shake or meal bar. Although carbohydrate intake was unspecified, the goal intake for fat was <30% of total calories with <10% from saturated fat, with a minimum of 15% of calories coming from protein (4). During year 1, the ILI included one individual session plus three group meetings monthly for 6 months, followed by one individual session plus two group meetings monthly for months 7–12. In years 2–4, study subjects had one visit plus a second contact via email, mail, or telephone each month (3).
Lessons Learned
Translating Positive Results Into Clinical Outcomes
Since the discontinuation of the trial and the publication of its results focusing on CVD outcomes, the question has arisen regarding how to interpret the study data to provide the best clinical outcomes for people with type 2 diabetes. The results of the Look AHEAD study indicate that, even without significant differences in CVD outcomes, supporting people who are overweight or obese and have type 2 diabetes in altering their intake, physical activity, and engagement with health care providers and community groups yields positive outcomes, including improvements in lipids and blood pressure (1), sleep apnea (5), renal disease (6), fitness (7), and depression (8). Although analyses of the data are ongoing, there already have been several positive lessons learned from the trial that can be implemented in clinical practice. These include effective ways to help clients achieve higher levels of physical activity, improve diabetes management, use structured programs to improve nutrition therapy, and enhance engagement with their health care team over a multi-year timeframe.
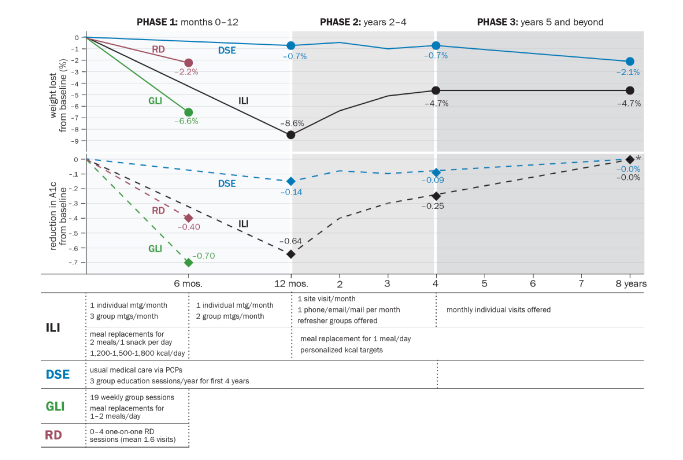
At the end of year 1, Look AHEAD’s ILI participants had lost an average of 8.6% of initial body weight compared to a 0.7% weight loss in the DSE group, a statistically significant difference (4). In previous trials, maintenance of weight loss after initial rapid weight loss has been difficult (9). In Look AHEAD, weight regain was seen in the ILI group after the first year, although a slowing rate of regain was seen in progressive years, and maintenance of an average loss of ∼4% of initial body weight was seen through year 8 (2,10). The ILI group had significantly better A1C levels than the DSE group for most years of the study (1). Figure 1 shows weight and A1C trends across study groups. The authors also hypothesized that the “initial weight losses delayed progression of [study subjects’] diabetes” (11). The study protocol was also successful in increasing the physical fitness and amount of physical activity performed by ILI group subjects. Although energy expenditure increased the most in the first year and declined in subsequent years, the ILI group had significantly more exercise and energy expended in physical activity (2). The goals of increased physical activity were to assist with weight maintenance efforts and also with reduction of blood glucose, insulin, blood pressure, and lipid levels, as well as the risks of cardiovascular morbidity and mortality, independent of weight loss. The findings on physical activity are relevant to clinical practice because the protocol focused on unsupervised, at-home exercise (3), which is easily translatable to nonstudy populations.
FIGURE 1.
Weight loss and A1C reduction over time in the Look AHEAD and IDOLc studies. Six-month weight loss values and A1C values for the ILI and DSE groups were not published as individual data points. Eight-year A1C values are estimated from a published chart (1) because data were not presented in tables elsewhere. mos, months; mtg, meeting; PCP, primary care provider.
The Look AHEAD trial also presented a comprehensive intervention based on frequent, in-depth sessions both in groups and one on one. Several elements of this ILI can inform future clinical practice. The groups fostered cohesion and a sense of community among study participants, who progressed through the curriculum with the same cohort (3). The group environment was paired with individual support, which allowed for patient-provider engagement, reduced loss to follow-up, and facilitated greater individualization to tailor the protocol to participants’ specific needs and differences (3).
Finally, the study’s “toolbox” technique lends itself to implementation in clinical settings. The study focused on using advanced behavioral strategies such as motivational interviewing (MI), development of problem-solving skills among participants, and increased contact with study staff to help subjects achieve weight loss goals (3). These are skills clinicians working with clients with type 2 diabetes can foster in their own counseling practices. The curriculum for the ILI group in the second 6-month study period included material on improving body image and self-esteem, which are important factors in improving patients’ quality of life independent of weight change. Subjects with decreased adherence in the first months of the intervention lost less weight, and weight loss achieved at month 2 was predictive of weight loss and maintenance at year 8 (12). The toolbox technique is also helpful in that study subjects who were struggling with adherence to protocols or did not lose weight per the study’s goals were offered additional resources and support.
Potential Difficulties in Real-World Implementation
There are some potential concerns in interpreting the results of Look AHEAD for clinical practice. A weakness of weight loss intervention trials is that initial weight loss is often achieved, but further loss or even maintenance is not sustained (9). The Look AHEAD protocol sought to avoid this pattern, seen often with very-low-calorie diets, by focusing instead on “moderate weight loss goals,” with the concurrent goal of weight loss maintenance (3). However, its results still showed the pattern of larger losses followed by a period of regain. Furthermore, although the average weight loss maintenance of the ILI group was significantly greater, not all study subjects lost weight or maintained losses. The greatest losses and improvements in CVD risk factors also occurred within the first year (11).
A potentially important factor in considering the weight trends from the Look AHEAD data is the way weight cycling (the repeating processes of losing weight and regaining it) can negatively affect metabolic outcomes, body image, and other biological and mental health outcomes (13). However, the study team’s analysis of the Look AHEAD data found “no negative associations of losing and regaining weight” compared to never having lost weight because the hypothesized mechanisms of increased risk of insulin resistance, type 2 diabetes, or dyslipidemia were not supported. The authors’ conclusions encouraged larger up-front losses to offset eventual weight regain and maintain “long-term improvements in triglyceride, HDL-C [cholesterol], and A1C levels” (11). This goal proved difficult for portions of the ILI cohort and could be problematic in general clinical populations. An analysis of weight patterns among the 1,428 subjects in the ILI group found that 32% (n = 455) achieved and maintained large or moderate weight losses, but 35% (n = 499) had large or moderate losses followed by full weight regain at 4 years, 11% (n = 158) had minimal weight changes, and 22% (n = 316) had large losses followed by some regain at 4 years, although still maintaining a significant change from baseline (11).
Another lesson to mine from the Look AHEAD data is the impact of the intervention on glycemic control. There were significant differences seen in A1C between the ILI and DSE groups up until year 8, but the data also show a marked decrease in A1C in year 1, followed by increases thereafter (1). Although the Look AHEAD trial focused on weight loss as a key metric of success, in a study of people with type 2 diabetes, it remains appropriate to keep blood glucose outcomes as a central focus; improving diabetes management (or glucose management) and lowering A1C can improve health outcomes and reduce risks for complications. Even with the relative maintenance of weight losses in the study, A1C levels worsened through the follow-up period (1,11). A tension continues to be that significant initial weight loss yields changes in glucose management but is difficult to achieve in real-world settings and difficult to continue over time. Thus, it is important to avoid prioritizing weight loss as a primary goal of treatment and instead to shift attention to improving blood glucose levels and reducing diabetes-related complications.
Although Look AHEAD data indicated an overall improvement in health-related quality of life and depression (8), it is also worth considering the way prescribed diets themselves can potentially negatively affect eating behaviors. Dieting is a risk factor for the development of binge eating (BE) behaviors (14). The Look AHEAD research team explored the impact of BE behaviors on the ability to achieve or maintain weight loss, finding that BE reduced weight loss (15). It would be worth exploring how and why BE behaviors changed for those who engaged in BE only at the start of the study or for those who began BE during the trial. It is also important to avoid punitive framing in conversations about weight, physical activity, and eating habits.
Enhancing patients’ confidence and competence in eating and decision-making around food choices can equip them with diabetes management skills to use when meal replacements are not appealing or feasible. The reliance on meal replacements for nutrient intake may be a barrier to incorporating the study protocol into the lives of a wider clinical population. Current medical nutrition therapy recommendations for the management of type 2 diabetes emphasize choosing a variety of nutrient-dense foods, maintaining the pleasure of eating by providing positive messages about food choices, and focusing on eating patterns composed of foods in appropriate portions sizes (16). Study subjects with the highest adherence to using meal replacement products for 2 meals/day had the highest rate of weight loss or maintenance throughout the 8-year follow-up period (2). This information may be helpful regarding the efficacy of meal replacements, but patients in a clinical setting may be resistant to such a high use of these products and may be more interested in conventional foods and meals as their primary source of nutrition. Can clinicians incorporate more than meal replacements and structured meal plans to help patients make decisions about meals? There is also the concern that the cost of meal replacement products may prevent adoption of the Look AHEAD protocol on a clinical basis.
Ongoing Studies and Clinical Translation
Studies exploring the implementation of the Look AHEAD trial results in wider populations are underway. The goal of the Improving Diabetes Outcomes through Lifestyle change (IDOLc) study is to test the implementation of a protocol similar to that of Look AHEAD but using the 19 group education sessions without the one-to-one visits to reduce required resources. The protocol compares a group lifestyle intervention (GLI) with the current standard of care of referral to a registered dietitian (RD) nutritionist and has found similar initial results to the Look AHEAD trial: at 6 months, the GLI group had lost 6.6% of body weight compared to 2.2% in the RD group and had a decrease in A1C of 0.7% compared to 0.4% in the RD group (not statistically significant) (17) (Figure 1). The IDOLc trial also uses meal replacements and prepackaged entrees for 1–2 meals/day. Although initial 6-month results were similar to those of the Look AHEAD trial, longer-term data are not yet available. These data will be important for evaluating the full impact of the intervention given the difficulty of sustained weight loss or weight maintenance with many weight loss interventions.
Another study, the Reach Ahead for Lifestyle and Health-Diabetes (REAL HEALTH-Diabetes) trial, is in its recruitment phase, with the aims of translating the Look AHEAD ILI for use at community health centers and comparing in-person group programming, telephone conference call groups, referral to medical nutrition therapy, and standard care (18). This trial has an estimated completion date of 2019.
Conclusion
Given the finding of no difference between the ILI and DSE groups in terms of CVD outcomes, the results of the Look AHEAD trial speak more to the impact of the ILI on achieving and maintaining weight loss. It is important to keep the frame of improving our clients’ lives and health outcomes centered in this discussion; improving diabetes (or glucose) management, reducing cardiovascular morbidity and mortality, increasing physical activity, and improving nutrition status and intake are central pillars to helping our clients with type 2 diabetes.
A meta-analysis of weight loss interventions for overweight and obese adults with type 2 diabetes found that a majority of these interventions did not result in significant weight loss or improved metabolic outcomes, leading the authors to conclude that “weight loss for many overweight or obese individuals with type 2 diabetes might not be a realistic primary treatment strategy for improved glycemic control” (9). The Look AHEAD trial was one of two exceptions to this finding. However, given the trend toward weight regain, are future weight loss attempts warranted in the years after participating in the study protocol? A majority of Look AHEAD subjects (86–89%) had attempted intentional weight loss before enrolling (19). Key questions in interpreting the data for use in real-world settings address the extent to which focusing on weight loss for improving diabetes and long-term health outcomes should be prioritized and how to integrate helpful elements of the study on a wider clinical scale, offering support to clients to achieve improved diabetes (or glucose) management and better long-term health outcomes.
Future study around the question of why people have difficulty following study protocols might be beneficial for applying the Look AHEAD results in real-world settings. Qualitative research may be a potential tool to gain insight into how and why study subjects struggle with adherence and to what extent the study protocol maps realistically to their lives.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Look AHEAD Research Group; Wing RR, Bolin P, Brancati FL, et al. Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013;369:145–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Look AHEAD Research Group; Wadden TA, Bantle JP, Blackburn G, et al. Eight-year weight losses with an intensive lifestyle intervention: the Look AHEAD Study. Obesity 2014;22:5–13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Look AHEAD Research Group; Wadden TA, West DS, Delahanty LM, et al. The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity 2006;14:737–752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Look AHEAD Research Group; Pi-Sunyer X, Blackburn G, Brancati FL, et al. Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care 2007;30:1374–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kuna ST, Reboussin DM, Borradaile KE, et al. Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep 2013;36:641A–649A [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Look AHEAD Research Group; Knowler WC, Bahnson JL, Bantle JP, et al. Effect of a long-term behavioural weight-loss intervention on nephropathy in overweight or obese adults with type 2 diabetes: a secondary analysis of the Look AHEAD randomized clinical trial. Lancet Diabetes Endocrinol 2014;2:801–809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Look AHEAD Research Group; Jakicic JM, Egan CM, Fabricatore AN, et al. Four-year change in cardiorespiratory fitness and influence on glycemic control in adults with type 2 diabetes in a randomized trial: the Look AHEAD trial. Diabetes Care 2013;36:1297–1303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Look AHEAD Research Group; Rubin RR, Wadden TA, Bahnson JL, et al. Impact of intensive lifestyle intervention on depression and health-related quality of life in type 2 diabetes: the Look AHEAD Trial. Diabetes Care 2014;37:1544–1553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Franz MJ, Boucher JL, Rutten-Ramos S, VanWormer JJ. Lifestyle weight-loss intervention outcomes in overweight and obese adults with type 2 diabetes: a systematic review and meta-analysis of randomized clinical trials. J Acad Nutr Diet 2015;115:1447–1463 [DOI] [PubMed] [Google Scholar]
- 10.Look AHEAD Research Group; Wing RR, Bahnson JL, Bray GA, et al. Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes: four-year results of the Look AHEAD trial. Arch Intern Med 2010;170:1566–1575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Look AHEAD Research Group; Wing RR, Espeland MA, Clark JM, et al. Association of weight loss maintenance and weight regain on 4-year changes in CVD risk factors: the Action for Health in Diabetes (Look AHEAD) clinical trial. Diabetes Care 2016;39:1345–1355 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Unick JL, Neiberg RH, Hogan PE, et al. Weight change in the first 2 months of a lifestyle intervention predicts weight changes 8 years later. Obesity 2015;23:1353–1356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mackie GM, Samocha-Bonet D, Tam CS. Does weight cycling promote obesity and metabolic risk factors? Obes Res Clin Pract 2017;11:131–139 [DOI] [PubMed] [Google Scholar]
- 14.Goldschmidt AB, Wall M, Loth KA. Which dieters are at risk for the onset of binge-eating? A prospective study of adolescents and young adults. J Adolesc Health 2012;51:86–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gorin AA, Niemeier HM, Hogan P. Binge eating and weight loss outcomes in overweight and obese individuals with type 2 diabetes: results from the Look AHEAD trial. Arch Gen Psychiatry 2008;65:1447–1455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Evert AB, Boucher JL, Cypress M, et al. Nutrition therapy recommendations for the management of adults with diabetes. Diabetes Care 2014;37(Suppl. 1):S120–S143 [DOI] [PubMed] [Google Scholar]
- 17.Delahanty LM, Dalton KM, Porneala B, et al. Improving diabetes outcomes through lifestyle change: a randomized controlled trial. Obesity 2015;23:1792–1799 [DOI] [PubMed] [Google Scholar]
- 18.ClinicalTrials.gov. REAL HEALTH-Diabetes: reach ahead for lifestyle and health-diabetes [Internet]. Available from https://clinicaltrials.gov/ct2/show/NCT02320253. Accessed 20 February 2017
- 19.Raynor HA, Jeffery RW, Ruggiero AM, Clark JM, Delahanty LM. Weight loss strategies associated with BMI in overweight adults with type 2 diabetes at entry into the Look AHEAD Trial. Diabetes Care 2008;31:1299–1304 [DOI] [PMC free article] [PubMed] [Google Scholar]