Abstract
Objective.
The purpose of this study is to explore current practice regarding insulin administration by nurses in a Greek public hospital.
Design and methods.
A mixed-methods qualitative data collection design was used with ad hoc nonparticipant observation and post hoc interviews with the staff involved. Insulin management and administration was observed and compared to international guidelines. A sample of 20 nurses from two medical wards was assessed on 100 occasions of insulin administration, and 8 nurses were subsequently interviewed.
Results.
Inter-rater agreement was found to be satisfactory (average κ 0.840). In 61% of all instances, nurses washed their hands before administering insulin, and, in 70%, they donned gloves before injections. In 64.5% of all instances, the nurses did not clean the insulin bottle before inserting the needle, and in 42.7% of instances, they did not check for air bubbles in the syringe. In 89.1% of instances, nurses did not check the injection site for appropriateness or other possible complications. However, in 90.9%, they cleaned the skin at the injection site with an alcohol swab. In 70.9% of all instances, the needle was placed vertically to the skin but without a skinfold. In 89.1% of instances, post-injection care was rated as poor.
Conclusion.
Overall, compliance with international guidelines regarding insulin administration techniques, as observed in these sample wards, is not satisfactory. Nurses in this Greek hospital tend to administer subcutaneous injections in ways not reflected in current research findings, practice guidelines, or evidence-based care recommendations. Evidently, Greek nurses in this sample require updating on current evidence-based practice, clinical guidelines, and protocols of care regarding routine insulin administration.
Diabetes is a chronic condition requiring dietary restraint and often pharmacological management, including insulin therapy with precise injection technique. In routine clinical practice, insulin administration is an essential nursing skill. Insulin is the main pharmacological treatment for type 1 diabetes. Proper insulin administration is of great clinical importance for the regulation of blood glucose levels. Therefore, state-of-the-art clinical craftsmanship is crucial when administering and teaching patients to self-administer insulin (1,2).
However, insulin is now recognized as being among the top 10 most high-risk medications worldwide (3). There has been increasing concern about in-hospital administration of subcutaneous insulin, which is frequently performed in an unsafe manner (4). Although appropriate subcutaneous injection technique requires skills and knowledge that are taught in standard nursing education programs worldwide, criticisms prevail regarding practitioners’ unsafe injection practices. These include lack of current knowledge, slapdash technique, and lack of aspiration with regard to imparting improved long-term clinical outcomes for patients (5).
Studies of diabetes self-care have found that patients with diabetes tend to self-administer their insulin in limited and narrow sites within the abdominal area, which can result in lipodystrophy (6–8). In a study by Davis et al. (9), patients were randomized to receive insulin administered either via pen devices or with conventional vials and syringes. The pens were found to be easier to use, increased patient satisfaction, and were cost-effective. Because of financial restraints in most Greek hospitals, the norm is to use insulin vials and syringes rather than pens. However, patients are taught how to use pen devices in hospital outpatient diabetes clinics either before they are discharged from an inpatient hospitalization or as outpatient day cases.
Safe and optimal administration of insulin requires that certain steps are conducted and precautions are in place in all clinical and nonclinical settings in which insulin is administered. For all insulin preparations except rapid- and short-acting insulin and insulin glargine, the vial or pen should be rolled gently in the palms of the hands (not shaken) to re-suspend the insulin because violent shaking may cause frothing or create air bubbles. Both of these effects are unfavorable to the patient because frothing may weaken the insulin molecules, and air bubbles in the syringe will “occupy” volume intended for the medication per se (10). After the insulin is drawn into the syringe, the fluid should be inspected for air bubbles, and, if necessary, one or two quick flicks of the forefinger against the upright syringe should allow the bubbles to escape. Air bubbles themselves are not dangerous, but they can cause the injected dose to be decreased (11). Patients should be aware that air bubbles can reduce the rate of insulin flow and cause under-delivery even if the needle remains under the skin for as long as 10 seconds after depressing the plunger (12).
Optimal Insulin Administration
Insulin injections are delivered into the subcutaneous tissue. Most individuals should be able to grasp a fold of skin lightly between their index finger and thumb and inject at a 90° angle. Thin individuals or children can use short needles or may need to pinch the skin and inject at a 45° angle to avoid an intramuscular injection, especially in the thigh area. Routine aspiration (i.e., drawing back on the injected syringe to check for blood) is not necessary (13).
If an injection seems especially painful, or if blood or clear fluid is seen after withdrawing the needle, the patient should apply pressure for 5–8 seconds without rubbing. Correct and pain-minimizing injections may be achieved by:
Injecting insulin at room temp-erature
Making sure no air bubbles remain in the syringe before injection
Waiting until topical alcohol (if used) has evaporated completely before injection
Keeping muscles in the injection area relaxed, not tense, when injecting
Penetrating the skin quickly
Not changing the direction of the needle during insertion or withdrawal
Not reusing needles
Adequately cleaning hands and the injection site before injecting (14–17)
Insulin may be injected into the subcutaneous tissue of the upper arm; anterior and lateral aspects of the thigh; buttocks; or abdomen (with the exception of a circle with a 2-inch radius around the navel). Intramuscular injection is not recommended for routine injections. Rotating the injection site is important to prevent lipohypertrophy or lipoatrophy. Rotating within one area is recommended (e.g., rotating injections systematically around the abdomen) rather than rotating from one area to another with each injection (e.g., from abdomen to thigh to arm). This practice may decrease variability in absorption from day to day (18,19).
Objective
The purpose of this study was to explore whether insulin administration via syringes, conducted by nursing staff in routine clinical practice at two internal medicine wards in a Greek public hospital, follows current standards and international guidelines.
Design and Methods
This qualitative observational study used a mixed-methods data collection design with ad hoc nonparticipant observation and post hoc interviews with the staff involved. The nonparticipant observation design was employed to record and compare insulin management and administration by nursing staff in a main hospital in Northern Greece. The interviews that followed with the nursing staff involved were conducted to collect demographic data and information about nurses’ knowledge of insulin administration (i.e., clinical experience, injection technique, and knowledge of diabetes therapeutic regimens). There was also an open-ended question about subcutaneous injections.
A basic step in nonparticipant observation is that the researcher should not participate or interact with the object of observation. This ensures an objective record of the observed phenomena from the objective perspective of an observer only and not from interaction with subjects (in this case, the nursing staff involved in the study) (20). Therefore, data collection was performed by student nurses who were already assigned to the selected wards. The student nurses worked in pairs and observed staff nurses administering insulin as part of their routine learning. During these observations, and without the knowledge of the staff nurses, the students kept a mental record of the insulin administration process used by each nurse. Immediately afterward, the student pairs retreated to a quiet room to discuss the process they had observed to reach intra-rater agreement on whether the predefined criteria for correct insulin administration were met. These data were encoded via a systematic process presented in the results section below.
The rationale for using student nurses as data collectors was that, as recipients of daily nurse training, they had direct access to observe these processes on a daily basis. Also, early in-hospital experience for trainee nurses is purely observational, so their role as observers would not have been seen as obtrusive or unusual. To increase their research skills, the student nurses had been given relevant education by and participated in discussions about clinical guidelines for insulin administration with the lead investigator shortly before the study began.
Although international standards and guidelines differ, the nonparticipant part of the study included a checklist of predefined domains drawn from the international literature of key protocols and clinical guidelines regarding insulin administration from drug preparation to post-injection care (21). It should be noted that the hospital wards under investigation did not have an official policy or guidelines for this procedure. The students observing nurse-administered insulin took mental notes on:
Clean, washed hands
Use of gloves
Flacon (insulin vial) antisepsis
Air bubbles in the syringe
Location check
Use of antiseptic solution
Angle of needle
Post-injection care
Measurement Tools
A structured observation sheet was created (observational protocol) that included the predefined variables to be studied. After each observation, data were systematically recorded, discussed thoroughly, and later analyzed. Thus, the dataset consisted of two parts: observations of insulin administration by nurses, as recorded by student nurse observers, and answers to interview questions, including how to inject optimally, the injection technique itself, and the antisepsis process. It should be noted that the official nursing policy in the study hospital was to use antiseptic locally before insulin injection.
Sample
The sample consisted of 20 nurses in two internal medicine wards in a hospital in Northern Greece. The majority (n = 12) were observed administering insulin six times each during the study period. Six nurses administered insulin five times each, and two nurses were observed giving insulin four times each. After completion of all 110 observations (mean five times each; range four to six times) over a 5-week period, the study was revealed to the 20 staff nurses, of whom a random subsample of 8 were then interviewed, as described above.
Inclusion criteria in the study dictated that that nursing staff participants regularly administered insulin as part of their routine clinical role (at least twice per week). Also, participating nurses had to be certified nurses, rather than nurse assistants, and employed in the public sector.
Ethical Considerations
The investigators presented the study objective, protocol, and observation form to the study hospital for the necessary ethical approval. They also presented information about measures taken to ensure anonymity and confidentiality; individuals and wards were symbolized on the data collection forms by sequential letters and numbers to ensure that data could not be traced back to specific individuals within the sample.
Statistical Analysis
Completed observation forms were processed systematically, and the κ statistic was used to measure agreement between observers to maximize consistency, which is an important factor in reliability, as emphasized by standards laid down in the 1960s by Becker and Blanche (22) and Glaser (23). Also, the relative likelihood agreement between observers (Pr[a]) and the possibility of arbitrary agreement (Pr[e]) were incorporated as shown in Eq. 1.
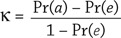 |
SPSS statistical software version 19 (SPSS, Inc., Chicago, Ill.) was used. Although there is no generally accepted minimum value indicating agreement between two individuals, a value of ∼0.8 or higher generally is considered likely to indicate adequate agreement.
Results
Table 1 shows the κ statistics measuring agreement between the members (E, G, and F) of the observer pairs collecting data. As seen in the table, there was acceptable observational agreement on all parameters observed, with the highest (1.00) for “injection angle” (measuring whether the correct angle was employed throughout the injection process) and the lowest (0.794) for “air bubbles” (measuring whether the nurse took measures to prevent, inspect for, and manage air bubbles in the syringe). It should also be noted that the level of agreement was similar for all three pairs of observers.
TABLE 1.
κ Statistic for Each Pair of Data Collectors’ Observations
| Observation | E–G | G–F | E–F |
|---|---|---|---|
| Clean, washed hands | 0.814 | 0.821 | 0.814 |
| Use of gloves | 0.822 | 0.811 | 0.822 |
| Flacon antisepsis | 0.904 | 0.818 | 0.832 |
| Air bubbles | 0.794 | 0.801 | 0.801 |
| Location check | 0.820 | 0.817 | 0.810 |
| Use of antiseptic solution | 0.832 | 0.838 | 0.842 |
| Angle of needle | 1.00 | 0.852 | 0.858 |
| Post-injection care | 0.912 | 0.867 | 0.872 |
| Mean | 0.862 | 0.828 | 0.831 |
Clean, Washed Hands
Observations indicated that, in 61% of all instances, nursing staff washed their hands, of which 49% used antiseptic soap and water and 12% used alcohol or Sterillium (a commercial hand disinfectant) to clean their hands before starting aspiration of insulin. However, it was also observed that, before administering insulin, staff did not re-wash their hands or use gloves in 39% of instances. Furthermore, consecutive interviewing showed that reasons for violation of hand hygiene standards included the following: lack of sinks and taps in each room, limited access to detergent and clean towels, shortage of time, and heavy workload. On a personal note, some nurses complained that frequent washing dries out and cracks the skin on their hands. Furthermore, as revealed by the open-ended question, some staff argued that, “Once hands are cleaned, they stay clean.”
Use of Gloves
In most instances (70%), nurses who injected insulin used clean gloves; however, in 30% of instances, no gloves were used. Of the 77 instances in which gloves were used, the gloves were not changed between patients, even for noninjection tasks. This practice could potentially lead to cross-infection of hospitalized patients or increased dispersal of microorganisms because of poor handling. Interview data suggest that reasons for this poor glove practice are limited resources and a lack of appreciation for cross-infection risks.
Flacon Antisepsis
In the great majority of instances (104 [94.5%]), nurses did not clean the top of the flacon before inserting the needle, whereas in 6 instances (5.5%), this cleaning was performed adequately with the use of an alcohol swab.
Air Bubbles
In 64 instances (57.3%), nurses preparing insulin for injection checked for air bubbles in the syringe and consequently flicked it to remove them. In the remaining 47 observations (42.7%), it was noted that there was no discernable effort to inspect for or remedy air bubbles.
Location Check
Before administering insulin in most instances (89.1%), nurses did not check the injection site for appropriateness or for possible factors such as adequate cleanliness, intact skin, and absence of inflammation, swelling, redness, lipohypertrophy, lipoatrophy, or lipodystrophy. This was confirmed by student observations during which they noted that the nurse was too quick in choosing a site, forgot to ask the patient where the last injection was administered (which is not routinely recorded in the nursing notes), did not feel the area carefully (e.g., for hardness), or failed to instruct the observing students about the correct procedure for checking injection sites. This procedure was performed correctly on only 12 (10.9%) occasions.
Use of Antiseptic Solution
In 100 instances (90.9%), the skin was cleaned with an alcohol swab or Sterillium, whereas in 10 instances (9.1%), the injection site was not cleaned at all.
Angle of Needle
On 78 occasions (70.9%), the needle was placed vertically to the skin but without a skinfold. In the remaining 32 instances (29.1%), the needle was placed at a 45° angle, again without a skinfold.
Post-Injection Care
In 98 instances (89.1%), post-injection care was rated as poor because there was not adequate time before needle withdrawal or inspection of the site; instead, the insulin syringe was withdrawn immediately after injection administration. These measures were observed to be carried out in 12 instances (10.9%). Although most insulin package inserts recommend waiting for 5–6 seconds before withdrawing the needle, in Greece, there is no hospital protocol on this issue.
Discussion
The results of this observational study indicate that, overall, compliance with international guidelines regarding insulin administration technique, as observed in the two sample hospital wards, is not satisfactory. Nurses commented that, because of serious staff shortages and hence the large workload that exists in Greek hospitals, they often are unable to deal effectively with both insulin administration and the education of patients with diabetes.
Although the majority in this sample administered insulin with either clean, washed hands or gloves, this can be regarded as lip service to patients in that the majority did not change their gloves between patients or maintain clean hands throughout the procedure. Moran and Arnott (24) suggest that both clean, washed hands and the use of gloves should be practiced routinely within a hospital environment. Although these gloves are not sterile, it is recommended that they be used to help prevent the transfer of resident bacteria from the fingers to the vial or injection site, thus minimizing infection. As clearly observed, when multiple insulin withdrawals were made from a single vial and without the flacon top being disinfected between each withdrawal, microorganisms could potentially colonize in the contents of the vial.
The practice of disinfecting the flacon top before aspiration was not followed routinely by the majority of nurses in this sample. As explained in the confirmatory interviews, in most cases, this was not perceived to be “so important” clinically. Yet, according to the American Diabetes Association (25), wiping the rubber cover of the insulin vial with a 70% alcohol swab is a standardized measure for infection prevention.
As noted in the international literature, bubbles in the insulin syringe are considered dangerous because they can result in a lower dose of insulin and also are associated with localized pain (26). Rolling the vial rather than shaking it may reduce the risk of inconsistent concentrations of insulin and consequently minimize the likelihood of bubble formation in the syringe. Although the majority of this sample checked for air bubbles in the syringe, there was limited effort in taking measures to avoid air bubble formation, which would have saved time by making it unnecessary to flick the syringe to remove bubbles.
This study also yielded evidence that injection sites were selected haphazardly. Furthermore, after the student observations where concluded, discussions with staff nurses indicated little appreciation of site selection, which also was not recorded formally after each subcutaneous injection. Yet, site selection is paramount and should take into consideration the variable absorption among sites. The abdomen has the fastest rate of absorption, followed by the arms, thighs, and buttocks. Exercise increases the rate of absorption at injection sites, probably by increasing blood flow to the skin and perhaps also by local actions. Areas of lipohypertrophy usually have slower absorption. The rate of absorption also differs between subcutaneous and intramuscular sites, with the latter being faster. Although intramuscular sites are not recommended for routine use, they can be used under circumstances such as diabetic ketoacidosis or dehydration, although this practice may be questionable when using analog insulin formulations (27).
As early as 1978, an article published in The Lancet (28) reported that routinely cleaning the skin with alcohol before a subcutaneous injection substantially reduces skin bacterial counts but does not necessarily prevent infection at injection sites. These early observations were reconfirmed by the World Health Organization (29), whose recommendations regarding skin preparation before injection read, “Wash skin that is visibly soiled or dirty. Swabbing of the clean skin before giving an injection is unnecessary.”
Despite these recommendations, wiping the skin site with alcohol before injection is a longstanding medical ritual still assumed to be correct in Greece. This study showed that on >90% of occasions, the skin was treated with an alcohol swab, although this practice is not substantiated with sufficient evidence. It may be that Greek nurses apply this practice to subcutaneous injection sites because they are influenced by techniques recommended for intramuscular or intravenous injections.
Studies have shown that applying alcohol does not sterilize the skin but rather only cleans the top layer and that skin is just as clean when washed with soap and water. In most cases, the areas of the body used for injections are covered by clothing most of the time, so they generally are kept clean. Moreover, insulin needles are not good carriers of bacteria because they are small and slick, and some insulin preparations have bacteriostatic additives that inhibit the growth of bacteria in the vial (30).
Thus, despite the well-acknowledged fact that using alcohol swabs on already clean or covered skin before injecting insulin is unnecessary, this remains a well-embedded routine practice in Greek hospitals. If nurses continue to use alcohol swabs, however, they should be aware that the alcohol must be fully dry on the skin before the injection. Furthermore, the focus should not be on skin preparation, but rather avoiding infections, which are more likely to be caused by contaminated syringes, needles, or solutions.
The recommended needle angle for subcutaneous injections is 90°, bearing in mind that this is dependent on the amount of subcutaneous tissue and the size of the needle; a 45° angle may be used for very thin patients or young children. For either angle, injecting into a skinfold created using the index finger and thumb only is recommended in both cases (31,32). In the sample studied here, however, most injections were given at a 90° angle, with the remainder at a 45°, but skinfolds were not used with either angle. Insulin should be administered subcutaneously to ensure slow absorption. To achieve this, Greek nurses typically are taught to administer injections with the needle at a 45° angle. However, because there is no reliable method to determine whether one has sufficient subcutaneous fat, and given that needles in Greek hospitals are usually ≥8 mm in length, it should be recommended as a rule of thumb that an adequate skinfold be created and that injections be administered at 90°.
The use of gloves is routine for all injection administrations in Greece. As this study has shown, in the majority of observed insulin administrations, staff nurses used standard latex gloves. Although gloves must be worn for all invasive procedures, when used incorrectly, they protect neither the patient nor the nurse (33). Thus, it should be noted that the observation of glove use was concerned with the correct use of gloves throughout the injection procedure, rather than simply whether gloves were used at all. In this light, it can be argued that this practice was not to patients’ advantage in that gloves were not changed between patients.
As shown in this study, nurses practiced poor post-injection procedures, giving time constraints as a reason. However, it is highly recommended that a syringe stay in situ for at least 10 seconds before needle withdrawal and that inspection of the site should follow its removal to check for bleeding, torn skin, bruising, soreness, welts, redness, pain, and early signs of lipodystrophy or other local or generalized complications (34).
The observing students reported that staff nurses commented not only on serious staff shortages, but also on a lack of time to teach the students appropriate technique. This raises concerns about whether other nursing interventions are carried out correctly, although this is beyond the scope of this article. The results of this study suggest that there is an unawareness on the part of staff nurses about updated information and guidelines regarding insulin administration. Thus, it could be argued that providing continuing education for the nursing staff with regard to insulin procedures would not only improve the insulin administration technique of current staff, but also benefit new and future staff generations.
This study raises concerns about the insulin administration practices of some nursing staff in Northern Greece. Also, the apparent lack of local protocols and concrete teaching may negatively influence the skill status of student nurses. Optimal insulin injection technique is vital for glycemic control, and staff nurses are responsible for educating both student nurses and patients about the safe and correct technique for this task. Still, international evidence shows that patients’ self-injection techniques are often flawed (35). For example, a study in Pakistan showed poor technique and lack of knowledge regarding efficacious insulin administration among nurses from three different hospitals (36). Similarly, in India, poor practices regarding insulin administration led to the recently published First Insulin Technique (FIT) national guidelines (37).
Conclusion
The goal of any effective insulin therapy is to achieve optimal blood glucose levels. To achieve this important goal, nurses need to know and routinely practice optimal injection technique, from safe medication preparation to appropriate post-injection care.
As this study shows, nurses in this Greek hospital tend to administer subcutaneous injections in ways not reflected in current research findings, practice guidelines, or evidence-based care recommendations. Instead, they seem to be comfortable with techniques reminiscent of those used for intramuscular or other injections, which are heavily focusing on practices such as skin swabbing and less focused on post-injection care. Although individualized patient assessment is practiced (i.e., choosing to use a 45° or 90° needle angle depending on a patient’s body structure), this is not accompanied by the recommended creation of a skinfold in which to inject.
There appears to be an education gap in the area of diabetes care in this hospital in Northern Greece; in many cases, only half of the international injection technique recommendations were either understood or practiced. Overall, it is evident that the nurses in this sample require a more thorough understanding of updated clinical guidelines and protocols of care with regard to routine insulin administration. Thus, at least some nurses in Greece, and possibly beyond, should be reeducated about insulin administration and kept up to date on recent developments in technological and pharmacological advancements in the field and their translation for routine clinical practice.
Duality of Interest
No potential conflicts of interest relevant to this article were reported.
References
- 1.Gelder C. Best practice injection technique for children and young people with diabetes. Nurs Child Young People 2014;26:32–36 [DOI] [PubMed] [Google Scholar]
- 2.Alabraba V, Floyd E, Morgan C, Kelly C, Wallymahmed M. “My diabetes, my insulin”: self-administration of insulin in hospital. J Diabetes Nurs 2014;18:296–299 [Google Scholar]
- 3.Lamont T, Cousins D, Hillson R, Bischler A, Terblanche M. Safer administration of insulin: summary of a safety report from the National Patient Safety Agency. BMJ 2010;341:c5269. [DOI] [PubMed] [Google Scholar]
- 4.Sharpe L. Improving safety of insulin administration: a pilot audit of hospital staff knowledge. J Diabetes Nurs 2012;16:8–16 [Google Scholar]
- 5.Ogston-Tuck S. Subcutaneous injection technique: an evidence-based approach. Nurs Stand 2014;29:53–58 [DOI] [PubMed] [Google Scholar]
- 6.Patton S, Eder S, Schwab J, Sisson C. Survey of insulin site rotation in youth with type 1 diabetes mellitus. J Pediatr Health Care 2010;24:365–371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dolinar R. The importance of good insulin injection practices in diabetes management. US Endocrinol 2009;5:49–52 [Google Scholar]
- 8.Vardar B, Kizilci S. Incidence of lipohypertrophy in diabetic patients and a study of influencing factors. Diabetes Res Clin Pract 2007;77:231–236 [DOI] [PubMed] [Google Scholar]
- 9.Davis E, Christensen C, Nystrom K, Foral P, Destache C. Patient satisfaction and costs associated with insulin administered by pen device or syringe during hospitalization. Am J Health Syst Pharm 2008;15;65:1347–1357 [DOI] [PubMed] [Google Scholar]
- 10.American Diabetes Association Insulin administration. Diabetes Care 2003;26(Suppl. 1): S121–S124 [DOI] [PubMed] [Google Scholar]
- 11.Shogbon A, Ngo D, Jacob B, Kimble L, Ryan G. Nurses’ perceptions and satisfaction with the use of insulin pen devices compared with insulin vial and syringes in an inpatient setting. Diabetes Technol Ther 2014;16:742–746 [DOI] [PubMed] [Google Scholar]
- 12.Saltiel-Berzin R, Cypress M, Gibney M. Translating the research in insulin injection technique: Implication for practice. Diabetes Educ 2012;38:635–643 [DOI] [PubMed] [Google Scholar]
- 13.Wood L, Wilbourne J, Kyne-Grzebalski D. Administration of insulin by injection. Practical Diabetes Int 2002;19 (Suppl. 2-1):S1–S4 [Google Scholar]
- 14.Rosindale S. Advanced preparation of insulin syringes for adult patients to administer at home: RCN guidance for nurses. 2nd ed. London, Royal College of Nursing, 2015. Available from https://www2.rcn.org.uk/__data/assets/pdf_file/0010/619804/RCNguide_insulin_syringes_WEB.pdf. Accessed 14 September 2016 [Google Scholar]
- 15.Trimble L, Meneilly G. Optimizing insulin absorption and insulin injection technique in older adults. Diabetes Care 2014;37:e127–e128 [DOI] [PubMed] [Google Scholar]
- 16.De Coninck C, Frid A, Gaspar R. Results and analysis of the 2008–2009 insulin injection technique questionnaire survey. J Diabetes 2010;2:168–179 [DOI] [PubMed] [Google Scholar]
- 17.Zhou L, Fan Y, Lu X. Feasibility study of vertical subcutaneous injection of insulin with an insulin pen injector in diabetic patients with normal body mass index. J Int Med Res 2010;38:669–673 [DOI] [PubMed] [Google Scholar]
- 18.Yakushiji F, Fujita H, Terayama Y. The best insulin injection pen device for caregivers: results of injection trials using five insulin injection devices. Diabetes Technol Ther 2010;12:143–148 [DOI] [PubMed] [Google Scholar]
- 19.Partanen T, Rissanen A. Insulin injection practices. Pract Diabetes Int 2000;17:252–254 [Google Scholar]
- 20.Frid A, Hirsch L, Gaspar R. New injection recommendations for patients with diabetes. Diabetes Metab 2010;36 (Suppl. 2):S3–S18 [DOI] [PubMed] [Google Scholar]
- 21.Dougherty L, Lister S. The Royal Marsden Hospital Manual of Clinical Nursing Procedures. 8th ed. Oxford, England, Blackwell Publishing, 2011 [Google Scholar]
- 22.Becker H, Blanche G. The analysis of qualitative field data. In Human Organization Research. Adams RA, Preiss JJ, Eds. Homewood Ill., Dorsey Press, 1960, p. 267–289 [Google Scholar]
- 23.Glaser B. The constant comparative method of qualitative research. Soc Probl 1965;12:431–445 [Google Scholar]
- 24.Moran B, Arnott S. Guideline for the administration of insulin by nursing staff. Diabetes Managed Clinical Networks and National Health Service Lanarkshire, 2014. Available from http://www.nhslanarkshire.org.uk/Services/Diabetes/Diabetes%20Clinical%20Guidelines/Documents/Guideline%20for%20the%20Administration%20of%20Insulin%20by%20Nursing%20Staff%20final%20May14.pdf. Accessed 14 September 2016 [Google Scholar]
- 25.American Diabetes Association : Insulin administration (Position Statement). Diabetes Care 2002(Suppl. 1);25:S112–S115 [Google Scholar]
- 26.Shank M. Trouble with bubbles. Am J Nurs 1999;99:14–16 [PubMed] [Google Scholar]
- 27.Heinemann L. Insulin absorption from lipodystrophic areas: a (neglected) source of trouble for insulin therapy? Diabetes Sci Technol 2010;4:750–753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Koivisto V, Felig P. Is skin preparation necessary before insulin injection? Lancet 1978;311:1072–1073 [DOI] [PubMed] [Google Scholar]
- 29.World Health Organization WHO guidelines best practice for injections and related procedures toolkit, 2010. Available from http://apps.who.int/iris/bitstream/10665/44298/1/9789241599252_eng.pdf. Accessed 14 September 2016 [PubMed]
- 30.Hansen B, Kirketerp G, Ehlers G, Nordentoft E, Hansen G. Evidence-based clinical guidelines for injection of insulin for adults with diabetes mellitus. Copenhagen, Denmark, Danish Nurses Organization, 2007 [Google Scholar]
- 31.Hofman P, Derraik J, Pinto T. Defining the ideal injection techniques when using 5-mm needles in children and adults. Diabetes Care 2010;33:1940–1944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nicol M, Bavin C, Bedford-Turner S, Cronin P, Rawlings-Anderson K. Essential Nursing Skills. 2nd ed. Edinburgh, Scotland, Mosby, 2004 [Google Scholar]
- 33.Pratt R, Pellowe C, Wilson J, et al. epic2: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect 2007;65(Suppl. I):S1–S4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hicks D, Kirkland F, Pledger J, Down S. The first UK injection technique recommendations. 2nd ed. London, 2011. Available from http://fit4diabetes.com/files/2613/3102/3031/FIT_Recommendations_Document.pdf. Accessed 14 September 2016 [Google Scholar]
- 35.Strauss K, De Gols H, Hannet I, Partanen T, Frid A. A pan-European epidemiologic study of injectable therapy injection technique in patients with diabetes. Pract Diabetes Int 2002;19:71–76 [Google Scholar]
- 36.Mushtaq M. Study of insulin injection technique amongst the nursing staff. Pak J Med Sci 2006;22:310–312 [Google Scholar]
- 37.Bajwa S, Kalra S, Baruah M, Bajwa S. An acute need for awareness of insulin injection guidelines in operative and intensive care units. Anesth Essays Res 2013;7:1–3 [DOI] [PMC free article] [PubMed] [Google Scholar]


