Abstract
Background
Source material used to fill calvarial defects includes autologous bones and synthetic alternatives. While autologous bone is preferable to synthetic material, autologous reconstruction is not always feasible due to defect size, unacceptable donor-site morbidity, and other issues. Today, advanced three-dimensional (3D) printing techniques allow for fabrication of titanium implants customized to the exact need of individual patients with calvarial defects. In this report, we present three cases of calvarial reconstructions using 3D-printed porous titanium implants.
Methods
From 2013 through 2014, three calvarial defects were repaired using custommade 3D porous titanium implants. The defects were due either to traumatic subdural hematoma or to meningioma and were located in parieto-occipital, fronto-temporo-parietal, and parieto-temporal areas. The implants were prepared using individual 3D computed tomography (CT) data, Mimics software, and an electron beam melting machine. For each patient, several designs of the implant were evaluated against 3D-printed skull models. All three cases had a custom-made 3D porous titanium implant laid on the defect and rigid fixation was done with 8 mm screws.
Results
The custom-made 3D implants fit each patient's skull defect precisely without any dead space. The operative site healed without any specific complications. Postoperative CTs revealed the implants to be in correct position.
Conclusion
An autologous graft is not a feasible option in the reconstruction of large calvarial defects. Ideally, synthetic materials for calvarial reconstruction should be easily applicable, durable, and strong. In these aspects, a 3D titanium implant can be an optimal source material in calvarial reconstruction.
Keywords: Skull, Titanium, Three-dimensional printing
INTRODUCTION
A cranial bone defect can occur from trauma, infection, and tumor surgery and result in aesthetic and functional deficiencies [1,2,3]. Depressed scalp or asymmetry of calvaria can affect social relationship. In functional terms, patients can suffer from varied neurologic symptoms like dizziness, irritability, anxiety, and intolerance [2,3].
Calvarial reconstruction should provide biomechanical stability, cerebral protection, and restoration of the cranial contour. Historically, source material for cranioplasty included autografts, xenografts, and allografts [1]. While autologous bone is most widely used today, significantly large defects require synthetic materials such as inert metals, ceramics, plastics, and absorbable polymers. Developments in medical imaging and computer software allow computer-assisted-design implants to be fabricated to the shape of individual defects for precise fit [4,5,6]. In this report, we present the experiences with reconstruction of three large calvarial defects using custom fabricated titanium implants.
METHODS
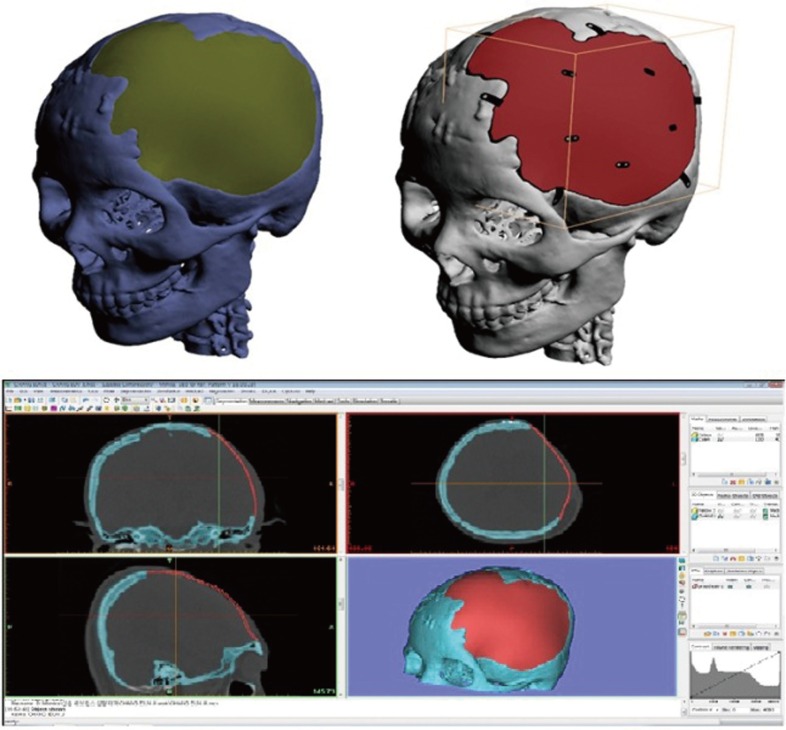
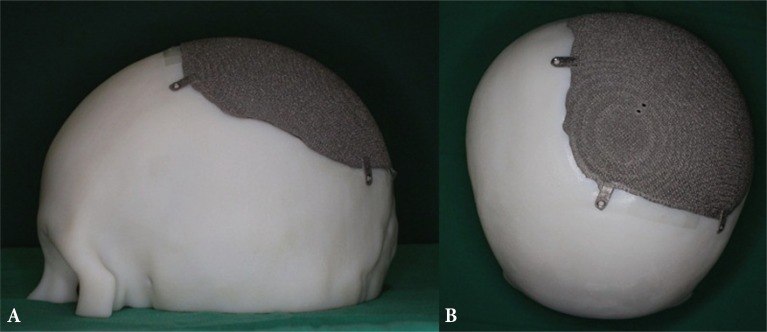
From 2013 through 2014, three calvarial defects were repaired using custom-made 3D porous titanium implants by a single reconstructive surgeon at a tertiary academic hospital. The titanium implants were manufactured by Medyssey Company (Dongducheon, Korea) using three-dimensional (3D) computed tomography (CT) data, Mimics software, and an electron beam melting machine (Figs. 1, 2). For each patient and calvarial defect, the engineer and surgeon tried several different implant designs against 3D-printed skull models. Design factors (thickness, fixation type, porosity, etc.) were considered before this step. The final implant design incorporated 2 mm thickness for bone-like rigidity. After manufacturing the 3D implant, we simulated the operation with it to the patient's rapid prototyping (RP) model. The defects were secondary to traumatic subdural hematoma or meningioma and were located in parieto-occipital, fronto-temporo-parietal, and parieto-temporal areas. Intraoperatively, an incision was made on the scalp and the dissection was made under the periosteum. For each patient, the 3D-printed titanium implant was laid into the defect and rigidly fixed with 8 mm screws.
Fig. 1. Three-dimensional (3D) implant design process. Custom-made 3D titanium implants were manufactured by Medyssey Co., Ltd. using 3D computed tomography (CT) data, Mimics software.
Fig. 2. (A, B) Custom-made 3-dimensional (3D) titanium implant by 3D printer. Custom-made 3D titanium implants were manufactured by electron beam melting machine. We tried to simulate the operation on the patient's rapid prototyping model.
RESULTS
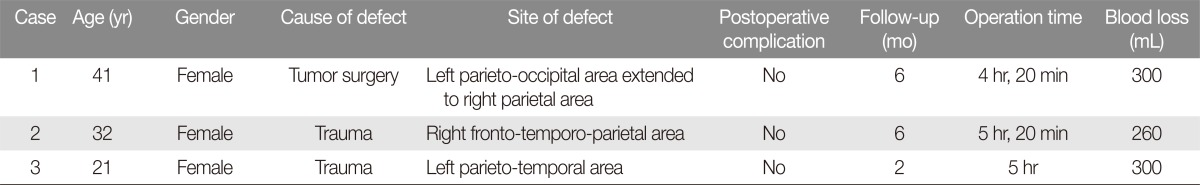
During the operation, we were able to confirm that the custommade 3D implants fit each skull defect precisely without any perceptible dead spaces. The operation times were 4 hours 20 minutes, 5 hours 20 minutes and 5 hours. The blood loss was 300 mL, 260 mL, and 300 mL, respectively (Table 1). Scalp depressions were eliminated with return of a more normal contour, and all of the patients expressed satisfaction. Postoperative CT confirmed accurate positioning of the implant. There were no complications during the follow up period.
Table 1. Summary of patients.
Case 1
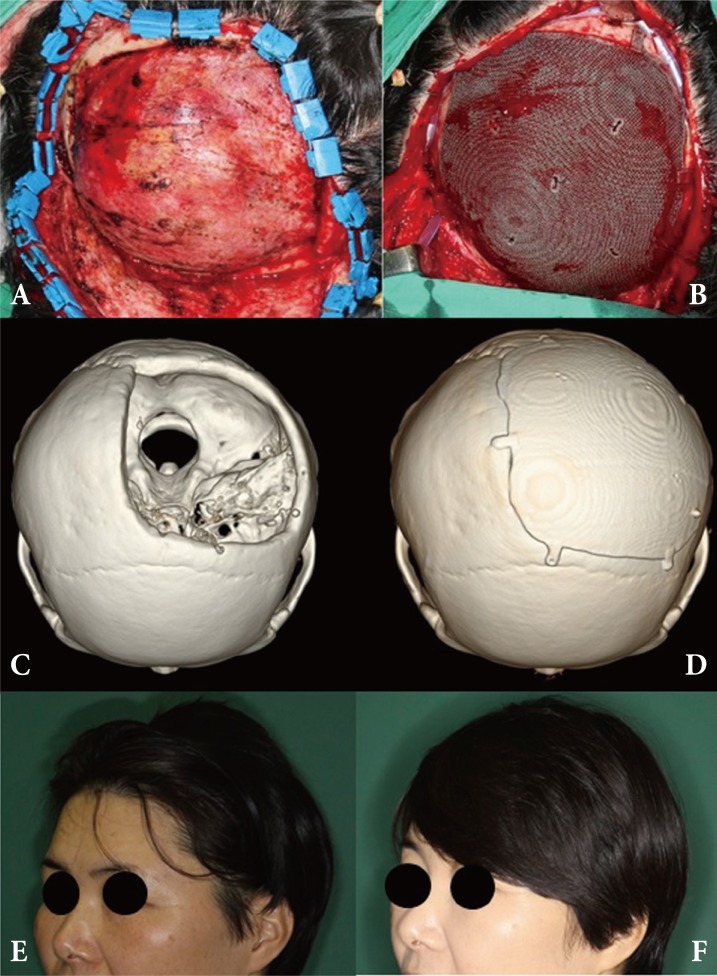
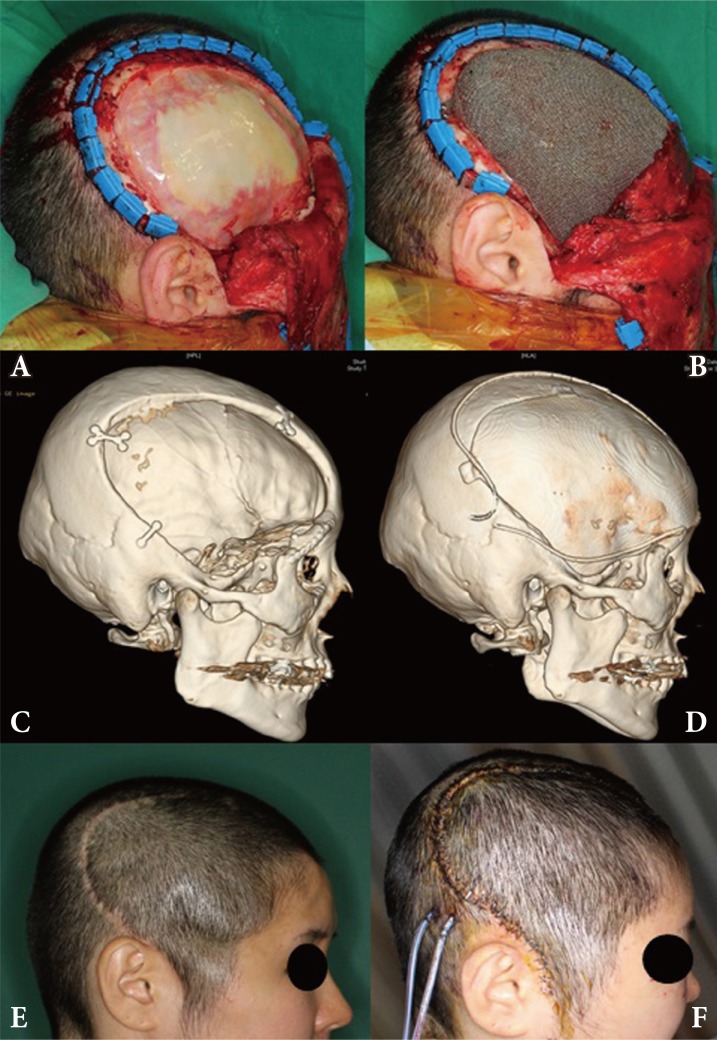
The first patient was a 41-year-old female with a calvarial defect secondary to meningnioma resection one year ago. The 12×14 cm2 defect was located in the left parieto-occipital area and crossed the midline into the right parietal area. Intraoperatively, a coronal incision was made and the dura was exposed. The 3D-printed titanium implant was laid on the skull defect and rigid fixation was done with 8 mm screws. The postoperative follow-up was six months without any complications (Fig. 3).
Fig. 3. Case 1. (A) Preoperative skull defect was noted. (B) Titanium implant was laid on the defect. (C) Preoperative three-dimensional (3D) facial computed tomography (CT). (D) Postoperative 3D facial CT scan. (E) Preoperative depression of scalp was noted. (F) Patient was satisfied with postoperative scalp contour.
Case 2
The second patient was a 32-year-old female with a calvarial defect in the right fronto-temporo-parietal area. Due to a subdural hematoma after a traffic accident, she had a craniectomy one year ago. The defect size was 14×11 cm2. Intraoperatively, a coronal incision was made and the previously inserted implant was removed. Reconstruction was done using the same method as above with 3D titanium implant. The postoperative follow-up was six months without any complications (Fig. 4).
Fig. 4. Case 2. (A) Preoperative skull defect was noted. (B) Titanium implant was laid on the defect. (C) Preoperative three-dimensional (3D) facial computed tomography (CT). (D) Postoperative 3D facial CT scan. (E) Preoperative depression of scalp was noted. (F) Patient was satisfied with postoperative scalp contour.
Case 3
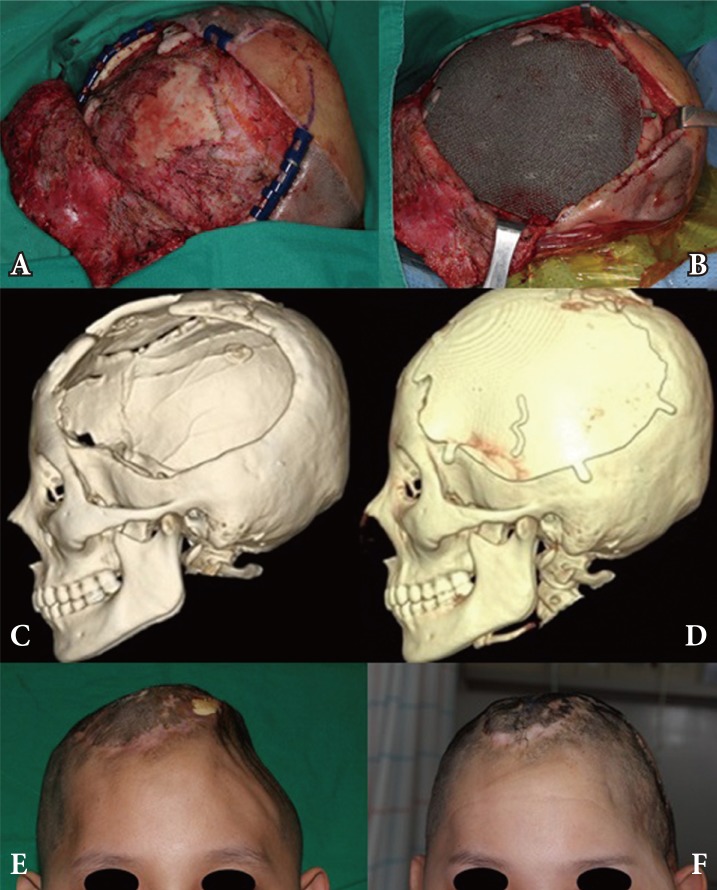
The third patient was a 21-year-old female with a calvarial defect in the left parieto-temporal area. She also had a craniectomy two years ago due to an epidural hematoma after a traffic accident. Before then, she previously had a cranioplasty with MedPor at another hospital and the implant had been removed due to infection. The defect size was 15×15 cm2 and reconstruction was done with a 3D titanium implant. The postoperative follow-up was two months without complications (Fig. 5).
Fig. 5. Case 3. (A) Preoperative skull defect was noted. (B) Titanium implant was laid on the defect. (C) Preoperative three-dimensional (3D) facial computed tomography (CT). (D) Postoperative 3D facial CT scan. (E) Preoperative depression of scalp was noted. (F) Patient was satisfied with postoperative scalp contour.
DISCUSSION
In this study, we report three cases successful calvarial reconstruction using custom-made 3D titanium implants. Although the number of cases was small with short follow-up period, custom-made implants are highly reasonable options for skull reconstruction. The method has many advantages including shorter operating time, decreased techincal demand, and the lack of need for a donor graft.
Autologous bone is widely used in calvarial reconstruction. It has excellent osteoconductive properties and has been the gold standard [7]. However, it requires meticulous harvesting technique. Donor site morbidity is an issue, and bone grafts cannot be used to fill large defects. In some studies, bone resorption has been reported at rates from 3% to 12% [8,9,10], which often necessitate secondary interventions to compensate for the loss [11,12].
Plastic surgeons have searched for an ideal material to use in skull reconstruction. Such material should be easy to manufacture, be durable, strong, lightweight, non-ferromagnetic, and noncarcinogenic. Materials such as polymethylmethacrylate (PMMA), hydroxyapatite (HA) and polyethylene have proven to be biocompatible but have individual shortcoming. Compared to titanium, PMMA and HA are associated with an increased risk of infection. Polyethylene is not as strong [11,13].
The bio-compatibility of titanium is well established [14,15]. It is robust enough to resist secondary trauma while providing maximal stability of the cranial vault. Furthermore, titanium implants generally cause less inflammation and conducts well with surrounding mineralized bone [16]. In a previous experience with porous titanium implants (not custom made), we found tissue ingrowth into the implant. However, these off-the-shelf implants were too hard to be altered during an operation, and it was necessary to be able to prefabricate custom implant using computer-assisted-design and manufacturing. Like other metallic implants, it may produce imaging artifacts on CT and magnetic resonance imaging [7].
A major concern in calvarial reconstruction has been the complex geometry which can affect preoperative planning and aesthetic outcomes [17]. With advancement in computer-assisted manufacturing processes, titanium implants could be fabricated using electron beams to print titanium structure in 3D [18]. In our experience, the implants fit the defect precisely without any dead space. A disadvantage of alloplastic materials is its high susceptibility to infection [19]. However, titanium is resistant to bacterial colonization and causes less inflammation. Though our experience represents only three cases, none of the titanium implants became infected during the follow up period. We feel that proper perioperative antibiotic prophylaxis and adequate soft tissue coverage was helpful in minimizing these complications.
In South Korea, the cost of manufacturing custom-made implants is not currently covered by the national health insurance, and the cost born by patients for each implant was expensive. In Europe, the costs of implants range from €2500 to €5050 (mean, €3733) [20]. Despite this, patients were satisfied with the choice to receive custom titanium implants and did not complain regarding the cost of implant.
The limitations of this study are small sample size and lack of long-term follow-up data. Although there are no early complications and patients remain satisfied, long-term follow up is needed for signs of infection and impaired wound healings as reported in previously published cases [20]. The ideal material for skull reconstruction remains controversial [20]. Biomechanical stability, cerebral protection, and cosmetic outcome are significant factors to consider when selecting a source material. In these aspects, custom-made 3D titanium implants can be a great option for skull reconstruction.
References
- 1.Durand JL, Renier D, Marchac D. The history of cranioplasty. Ann Chir Plast Esthet. 1997;42:75–83. [PubMed] [Google Scholar]
- 2.Dujovny M, Aviles A, Agner C, Fernandez P, Charbel FT. Cranioplasty: cosmetic or therapeutic? Surg Neurol. 1997;47:238–241. doi: 10.1016/s0090-3019(96)00013-4. [DOI] [PubMed] [Google Scholar]
- 3.Dujovny M, Agner C, Aviles A. Syndrome of the trephined: theory and facts. Crit Rev Neurosurg. 1999;9:271–278. doi: 10.1007/s003290050143. [DOI] [PubMed] [Google Scholar]
- 4.Ono I, Tateshita T, Satou M, Sasaki T, Matsumoto M, Kodama N. Treatment of large complex cranial bone defects by using hydroxyapatite ceramic implants. Plast Reconstr Surg. 1999;104:339–349. doi: 10.1097/00006534-199908000-00003. [DOI] [PubMed] [Google Scholar]
- 5.Eppley BL, Kilgo M, Coleman JJ., 3rd Cranial reconstruction with computer-generated hard-tissue replacement patient-matched implants: indications, surgical technique, and long-term follow-up. Plast Reconstr Surg. 2002;109:864–871. doi: 10.1097/00006534-200203000-00005. [DOI] [PubMed] [Google Scholar]
- 6.D'Urso PS, Earwaker WJ, Barker TM, Redmond MJ, Thompson RG, Effeney DJ, Tomlinson FH. Custom cranioplasty using stereolithography and acrylic. Br J Plast Surg. 2000;53:200–204. doi: 10.1054/bjps.1999.3268. [DOI] [PubMed] [Google Scholar]
- 7.Spetzger U, Vougioukas V, Schipper J. Materials and techniques for osseous skull reconstruction. Minim Invasive Ther Allied Technol. 2010;19:110–121. doi: 10.3109/13645701003644087. [DOI] [PubMed] [Google Scholar]
- 8.Aarabi B, Hesdorffer DC, Ahn ES, Aresco C, Scalea TM, Eisenberg HM. Outcome following decompressive craniectomy for malignant swelling due to severe head injury. J Neurosurg. 2006;104:469–479. doi: 10.3171/jns.2006.104.4.469. [DOI] [PubMed] [Google Scholar]
- 9.Figaji AA, Fieggen AG, Peter JC. Early decompressive craniotomy in children with severe traumatic brain injury. Childs Nerv Syst. 2003;19:666–673. doi: 10.1007/s00381-003-0804-3. [DOI] [PubMed] [Google Scholar]
- 10.Kan P, Amini A, Hansen K, White GL, Jr, Brockmeyer DL, Walker ML, Kestle JR. Outcomes after decompressive craniectomy for severe traumatic brain injury in children. J Neurosurg. 2006;105:337–342. doi: 10.3171/ped.2006.105.5.337. [DOI] [PubMed] [Google Scholar]
- 11.Moreira-Gonzalez A, Jackson IT, Miyawaki T, Barakat K, DiNick V. Clinical outcome in cranioplasty: critical review in long-term followup. J Craniofac Surg. 2003;14:144–153. doi: 10.1097/00001665-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Grant GA, Jolley M, Ellenbogen RG, Roberts TS, Gruss JR, Loeser JD. Failure of autologous bone-assisted cranioplasty following decompressive craniectomy in children and adolescents. J Neurosurg. 2004;100:163–168. doi: 10.3171/ped.2004.100.2.0163. [DOI] [PubMed] [Google Scholar]
- 13.Ducic Y. Titanium mesh and hydroxyapatite cement cranioplasty: a report of 20 cases. J Oral Maxillofac Surg. 2002;60:272–276. doi: 10.1053/joms.2002.30575. [DOI] [PubMed] [Google Scholar]
- 14.Blake GB, MacFarlane MR, Hinton JW. Titanium in reconstructive surgery of the skull and face. Br J Plast Surg. 1990;43:528–535. doi: 10.1016/0007-1226(90)90115-g. [DOI] [PubMed] [Google Scholar]
- 15.Raza SM, Thai QA, Pradilla G, Tamargo RJ. Frontozygomatic titanium cranioplasty in frontosphenotemporal ("pterional") craniotomy. Neurosurgery. 2008;62:262–264. doi: 10.1227/01.neu.0000317402.46583.c7. [DOI] [PubMed] [Google Scholar]
- 16.Neligan P, Grotting ES. Plastic surgery. 3rd ed. London: Elsevier Saunders; 2013. [Google Scholar]
- 17.Holck DE, Boyd EM, Jr, Ng J, Mauffray RO. Benefits of stereolithography in orbital reconstruction. Ophthalmology. 1999;106:1214–1218. doi: 10.1016/S0161-6420(99)90254-3. [DOI] [PubMed] [Google Scholar]
- 18.Winder J, Cooke RS, Gray J, Fannin T, Fegan T. Medical rapid prototyping and 3D CT in the manufacture of custom made cranial titanium plates. J Med Eng Technol. 1999;23:26–28. doi: 10.1080/030919099294401. [DOI] [PubMed] [Google Scholar]
- 19.Durham SR, McComb JG, Levy ML. Correction of large (>25 cm (2)) cranial defects with "reinforced" hydroxyapatite cement: technique and complications. Neurosurgery. 2003;52:842–845. doi: 10.1227/01.neu.0000054220.01290.8e. [DOI] [PubMed] [Google Scholar]
- 20.Cabraja M, Klein M, Lehmann TN. Long-term results following titanium cranioplasty of large skull defects. Neurosurg Focus. 2009;26:E10. doi: 10.3171/2009.3.FOCUS091. [DOI] [PubMed] [Google Scholar]