Abstract
Understanding the factors that influence veterans’ functional outcome after deployment is critical to provide appropriately targeted care. Mild traumatic brain injury (mTBI) and posttraumatic stress disorder (PTSD) have been related to disability, but other psychiatric and behavioral conditions are not as well examined. We investigated the impact of deployment-related psychiatric and behavioral conditions on disability among 255 OEF/OIF/OND service members and veterans. Structured clinical interviews assessed TBI and the psychiatric conditions of depression, PTSD, anxiety, and substance use. Self-report questionnaires assessed disability and the behavioral conditions of sleep disturbance and pain. Over 90% of participants had a psychiatric and/or behavioral condition, with approximately half presenting with ≥ 3 conditions. Exploratory factor analysis revealed 4 clinically relevant psychiatric and behavioral factors which accounted for 76.9% of the variance: (a) depression, PTSD, and military mTBI (deployment trauma factor); (b) pain and sleep (somatic factor); (c) anxiety disorders, other than PTSD (anxiety factor); and (d) substance abuse or dependence (substance use factor). Individuals with the conditions comprising the deployment trauma factor were more likely to be substantially disabled than individuals with depression and PTSD, but no military mTBI, OR = 3.52; 95% CI [1.09, 11.37]. Depression, PTSD, and a history of military mTBI may comprise an especially harmful combination associated with high risk for substantial disability.
Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) US service members and veterans face a host of challenges re-entering civilian life after military service. Disability in occupational functioning, social functioning, and quality of life has been related to psychiatric symptoms in returning veterans (Erbes, Kaler, Schult, Polusny, & Arbisi, 2011; Pietrzak, Goldstein, Malley, Johnson, & Southwick, 2009; Pittman, Goldsmith, Lemmer, Kilmer, & Baker, 2012; Schnurr, Lunney, Bovin, & Marx, 2009). This cohort of veterans could potentially have many years of productive contribution to society ahead, or in some cases, significant, costly disability.
The etiology of the reintegration problems and degree of disability faced by veterans is likely due to a number of interacting factors. Mild traumatic brain injury (mTBI; Hoge et al., 2008; Terrio et al., 2009) and posttraumatic stress disorder (PTSD; Hoge et al., 2004; Seal et al., 2009; Thomas et al., 2010) are among the most frequent and challenging consequences of the recent conflicts in Iraq and Afghanistan. TBI occurs in roughly 10%–23% of soldiers returning from OEF/OIF/OND, and the majority of these injuries are mild in nature (Cifu et al., 2013; Hoge et al., 2008; Terrio et al., 2009). Similarly, PTSD is estimated to occur in 12%–30% of service members and veterans returning from OEF/OIF/OND deployments (Higgins et al., 2014; Hoge et al., 2004; Seal et al., 2009; Thomas et al., 2010). Previous studies have found that mTBI occurs much more frequently in combination with PTSD than in isolation (Lew et al., 2009), and that PTSD is more common and severe among veterans who sustain a TBI compared to other injuries (Hoge et al., 2008; Schneiderman, Braver, & Kang, 2008). These findings suggest that the co-occurrence of mTBI and PTSD may be more detrimental to functional outcome than either diagnosis alone.
Critically, OEF/OIF/OND veterans represent a clinically complex group with multiple comorbidities above and beyond mTBI and PTSD. High co-prevalence of other psychiatric (e.g., depression, substance misuse, and anxiety disorders) and behavioral disorders (e.g., chronic pain and sleep disorders) has been documented (Hoge et al., 2008; Schneiderman et al., 2008). The high number of overlapping symptoms shared by mTBI and PTSD (Bryant, 2011; Stein&McAllister, 2009), and other psychiatric and behavioral diagnoses, can complicate the diagnosis and treatment of each of these issues.
Although our knowledge of these disorders has advanced, the field is constrained by regarding them as independent clinical entities. Each condition on its own may have a negative effect, but cumulatively the impact may well result in increased disability after deployment. We propose that the identification, diagnosis, and treatment of veterans who suffer from deployment-related injuries and behavioral consequences must be informed by recognizing the frequency of different disorders, the high prevalence of comorbidity, and their combined impact upon disability. Further, examining the pattern of co-occurrence of these disorders and how they impact functional outcome is an essential step in assisting veterans’ reintegration into civilian life after return from military service (Beder, Coe, & Sommer, 2011; Sayer et al., 2010).
The current study investigated the prevalence of a history of military mTBI and psychiatric and behavioral conditions, and how these different disorders impacted disability in a sample of returning OEF/OIF/OND veterans. A secondary objective was to conduct an empirical, exploratory factor analysis to determine how these diagnoses grouped together and the extent to which these groups of diagnoses were related to disability.
Method
Participants and Procedure
The sample of 255 was drawn from 284 OEF/OIF/OND veterans consecutively studied at the VA Boston TBI Center of Excellence, the Translational Research Center for TBI and Stress Disorders (TRACTS). Participants were recruited from the Boston Metropolitan area via a fulltime recruitment specialist who attended Yellow Ribbon Events, Task Force Meetings, and other events involving U.S. Air Force, Marine, Army, National Guard, and Reserve units. Participants were not specifically recruited from medical or mental health clinics; however, a minority of participants also contacted our recruitment specialist in response to flyers posted in our VA (Veterans Affairs) medical center. The Institutional Review Board of Human Studies Research at the VA Boston Healthcare System approved all procedures. All participants provided informed consent and completed an extensive evaluation lasting 8–10 hours. Participants were reimbursed $210 for their time and travel costs. Exclusion criteria included prior serious medical or neurological illness (unrelated to TBI), active suicidal and/or homicidal ideation requiring intervention, and a current diagnosis of bipolar disorder or psychotic disorder (except psychosis NOS due to trauma-related hallucinations) according to the Diagnostic and Statistical Manual of Mental Disorders (4th ed., DSM-IV; American Psychiatric Association [APA], 1994). The initial group of 284 was reduced by 18 participants who had not deployed, 10 who reported a premilitary history of moderate or severe TBI, and 1 with an incomplete psychological assessment, yielding the sample of N = 255.
Primary summary data for the total sample, including demographics, military information, and psychiatric and behavioral conditions are presented in Table 1. This study employed a convenience sample; however, there were no significant differences in age, gender, or branch of service between our sample and the OEF/OIF/OND veterans utilizing VA Health Care (U.S. Department of Veterans Affairs, 2012). Additionally, there was no significant difference in race between our sample and active duty enlisted members and selected reserve members (U.S. Department of Defense, 2012). Thus, the present sample is representative of the OEF/OIF/OND cohort in general demographic characteristics. By contrast, the psychological, neurological, and employment status of the sample may be more specific to our particular cohort of veterans.
Table 1.
Demographic, Current Psychiatric, and Behavioral Status for Total Sample and by TBI Status
| Variable | Total (N = 255a) | mTBI (n = 99) | No mTBI (n = 156) | χ2 or t | |||
|---|---|---|---|---|---|---|---|
|
|
|
|
|||||
| n or M | % or SD | n or M | % or SD | n or M | % or SD | ||
| Age | 32.24 | 8.48 | 31.17 | 7.41 | 32.91 | 9.05 | 1.67 |
| Males | 227 | 89.0 | 92 | 92.9 | 135 | 86.5 | 2.53 |
| Education (years) | 13.87 | 1.90 | 13.67 | 1.82 | 13.99 | 1.94 | 1.28 |
| Race | |||||||
| White | 178 | 69.8 | 71 | 71.7 | 107 | 68.6 | 3.91 |
| Black | 25 | 9.8 | 10 | 10.1 | 15 | 9.6 | |
| Hispanic | 41 | 16.1 | 16 | 16.2 | 25 | 16.0 | |
| Other | 7 | 2.7 | 2 | 2.0 | 5 | 3.2 | |
| Unknown/missing | 4 | 1.6 | 0 | 0.0 | 4 | 2.6 | |
| Service Branch | |||||||
| Army | 67 | 26.4 | 34 | 34.7 | 33 | 21.2 | 8.95 |
| Navy | 7 | 2.8 | 3 | 3.1 | 4 | 2.6 | |
| Marines | 35 | 13.8 | 16 | 16.3 | 19 | 12.2 | |
| Air Force | 13 | 5.1 | 4 | 4.1 | 9 | 5.8 | |
| National Guard | 101 | 39.8 | 33 | 33.7 | 68 | 43.6 | |
| Reserves | 31 | 12.2 | 8 | 8.2 | 23 | 14.7 | |
| Deployments | |||||||
| Number | 1.40 | 0.70 | 1.47 | 0.84 | 1.35 | 0.60 | −1.26 |
| Months | 14.32 | 8.54 | 15.44 | 9.73 | 13.61 | 7.63 | −1.59 |
| Months since last | 34.56 | 28.40 | 37.02 | 28.90 | 33.49 | 28.09 | −0.97 |
| Combat exposure | 15.85 | 11.84 | 21.77 | 11.9 | 12.25 | 10.27 | −6.60*** |
| n of military mTBIs | 0.65 | 1.32 | 0 | 0 | 1.69 | 1.66 | |
| PTSD | 146 | 57.3 | 76 | 76.7 | 70 | 44.9 | 25.18*** |
| Depressive disorders | 74 | 29.0 | 41 | 41.4 | 33 | 21.2 | 12.07*** |
| Major | 70 | 27.5 | 38 | 38.4 | 32 | 20.5 | 9.71** |
| Other | 4 | 1.6 | 3 | 3.0 | 1 | 0.6 | 2.24 |
| Anxiety disorders | 50 | 19.6 | 15 | 15.2 | 35 | 22.4 | 2.04 |
| Panicr | 17 | 6.7 | 8 | 8.1 | 9 | 5.8 | 0.52 |
| Social phobia | 16 | 6.3 | 3 | 3.0 | 13 | 8.3 | 2.90 |
| GAD | 16 | 6.3 | 3 | 3.0 | 13 | 8.3 | 2.90 |
| Other | 15 | 5.9 | 6 | 6.1 | 9 | 5.8 | 0.01 |
| Substance use disordersb | 39 | 15.3 | 19 | 19.2 | 20 | 12.8 | 1.90 |
| Alcohol | 37 | 14.5 | 18 | 18.2 | 19 | 12.2 | 1.76 |
| Other | 7 | 2.8 | 2 | 2.0 | 5 | 3.2 | 0.32 |
| Current pain | 161 | 67.91 | 71 | 79.8 | 90 | 60.8 | 9.18** |
| 30-day average pain | 29.31 | 25.28 | 35.95 | 26.68 | 25.40 | 23.65 | −3.13** |
| Sleep disturbance | 182 | 74.3 | 78 | 83.9 | 104 | 68.4 | 7.21** |
| Sleep quality | 9.36 | 4.75 | 10.82 | 4.90 | 8.47 | 4.43 | −3.87*** |
| n Psych/behav conditions | 2.56 | 1.49 | 3.03 | 1.35 | 2.26 | 1.50 | −4.17*** |
| 3+ comorbidities | 130 | 51.0 | 67 | 67.7 | 63 | 40.4 | 18.05*** |
Note. The percentages displayed in this table are column percentages. TBI = traumatic brain injury; mTBI = mild traumatic brain injury; GAD = generalized anxiety disorder; Psych/behav = psychiatric or behavioral.
n ranged from 237 to 255 due to missing data.
Abuse or dependence.
p < .05.
p < .01.
p < .001.
Measures
Demographics, military service branch, and number and duration of deployments were determined using self-report questionnaires. Combat exposure was assessed with the Deployment Risk and Resilience Inventory (King, King, Vogt, Knight, & Samper, 2006) Combat Experiences Scale (CES). It has been shown to have adequate reliability and validity in veterans of recent wars (Guyker et al., 2013). In our sample, CES scores ranged from 0 to 64 and Cronbach’s α was .92.
The Boston Assessment of TBI-Lifetime (BAT-L; Fortier et al., 2014), a validated, semistructured clinical interview with strong interrater reliability (κ > .80), was administered by doctoral-level psychologists to document a history of TBI. A history of military mTBI was defined as a period of self-reported loss of consciousness ≤ 30 minutes, posttraumatic amnesia ≤ 24 hours, or altered mental status ≤ 24 hours following a credible injury mechanism (U.S. Department of Veterans Affairs and U.S. Department of Defense, 2009) acquired during military service.
The Clinician Administered PTSD Scale (CAPS; Blake et al., 1990) using the DSM-IV standard scoring rule of 3 (Weathers, Ruscio, & Keane, 1999) was administered by doctoral-level psychologists to determine the presence and history of PTSD. Weathers, Keane, and Davidson (2001) reported moderate interrater reliability (κ = .58). In our sample, CAPS total scores ranged from 0 to 125 and Cronbach’s α was .94. Psychologists also administered the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First, Spitzer, Gibbon, &Williams, 1996; Lobbestael, Leurgans, & Arntz, 2011; Williams et al., 1992) nonpatient edition to assess for mood disorders, anxiety disorders, and substance use disorders, and to screen for psychotic disorders. Interrater reliability for the SCID is well documented (http://www.scid4.org/psychometric/). Both BAT-L diagnoses and psychiatric assessments were reviewed at weekly diagnostic consensus meetings consisting of at least three doctoral-level psychologists and a psychiatrist.
The Pittsburgh Sleep Quality Index (PSQI; Carpenter & Andrykowski, 1998), which has previously been validated in TBI populations (Fichtenberg, Putnam, Mann, Zafonte, & Millard, 2001; Fichtenberg, Zafonte, Putnam, Mann, & Millard, 2002) was used to determine the presence of sleep disturbance. The recommended global score cutoff of >5 was used to define sleep disturbance. In our sample, PSQI global scores ranged from 0 to 20 and Cronbach’s α was .79. Pain was assessed using the Short Form McGill Pain Questionnaire (SFMPQ; Grafton, Foster, & Wright, 2005; Melzack, 1987), which has been used previously in mild to moderate TBI (Bay & de-Leon, 2011; Walker, McDonald, Ketchum, Nichols, & Cifu, 2013). Current pain was diagnosed when the current overall level of pain was rated as mild or greater.
The World Health Organization (WHO) Disability Assessment Schedule II (WHODAS; WHO, 2010) was used to determine the presence of functional disability. The WHODAS has six subdomains: Understanding and Communicating, Getting Around, Self-Care, Getting Along with People, Life Activities, and Participation in Society. The WHODAS has been shown to have high internal consistency, stable factor structure, and high test-retest reliability (Strauss, Sherman, & Spreen, 2006), and with TBI (Soberg, Finset, Roise, & Bautz-Holter, 2012). The DSM-5 (APA, 2013) recommends the WHODAS for assessment of disability in clinical settings. WHODAS subdomain and overall scores range from 0 to 100, with higher scores indicating worse functioning. Each item contributes to its respective subdomain score equally, and each subdomain score is divided by the total possible points. Every subdomain score contributes equally to the overall score. For participants who were not currently working or in school (n = 44), the Life Activities subdomain raw score was divided by 16 potential points (four total questions), rather than 32 potential points (eight total questions), in accordance with the guidelines offered by the WHO (2004). In our sample, WHODAS overall total scores ranged from 0 to 69.5 and Cronbach’s α was .96.
We employed the Validity-10 Scale (Vanderploeg et al., 2014), which is embedded in the Neurobehavioral Symptom Inventory (NSI; Cicerone & Karlmar, 1995), to examine possible symptom exaggeration on self-report measures. Total scores > 22 on the Validity-10 scale indicate possible invalid responding.
Data Analysis
Descriptive statistics for demographics, military service, and clinical characteristics for the final sample were calculated. One-way ANOVAs and χ2 tests were performed to examine possible differences between participants with and without a history of military mTBI. Due to time constraints during testing, 12 participants did not complete the NSI, 12 did not complete the CES, 10 did not complete the PSQI, 18 did not complete the SFMPQ, and 15 did not complete the WHODAS. Two participants did not indicate their level of education. These individuals were therefore excluded from relevant analyses.
A multiple linear regression analysis was performed to analyze the contribution of a history of military mTBI, current psychiatric diagnoses, and current behavioral issues to disability. Separate multiple regression analyses were also conducted for each of the six WHODAS domains, using the same independent variables described above. For each regression, a square-root transformation of the functional status score was applied to meet the regression assumptions of linearity and normality of residuals. We computed a correlation matrix to examine the simple associations between each of the independent variables (Supplemental Table A).
An exploratory factor analysis was performed to determine which psychiatric and behavioral conditions, all coded as presence or absence of the condition, shared common variance. SPSS (version 20) and SAS (version 9.3) software were used for all analyses. We used the bootstrap method to adjust the p value for multiple comparisons (proc multtest in SAS; UCLA Statistical Counseling Group, 2014).
Results
Participants with a history of military mTBI were significantly more likely to report increased combat exposure and had more psychiatric and behavioral conditions than veterans without a history of military mTBI (see Table 1). History of military mTBI increased the odds of a PTSD diagnosis by 300% and depressive disorders, pain, and sleep disturbance by at least 140%.
The average WHODAS score was 17.11 (SD=16.60), which suggests that overall the TRACTS cohort had worse functioning than approximately 80% of the general international population (WHO, 2010). Linear regression models, presented in Table 2, revealed that symptom exaggeration, depressive disorder, PTSD, pain, and sleep disturbance were all significantly related to disability. A history of military mTBI was not significantly related to disability. Regression analyses for the WHODAS subscales were similar to those found with the WHODAS total score (Table 3).
Table 2.
Multiple Linear Regression of WHODAS Total Score and Demographic, Psychiatric, and Behavioral Conditions
| Variable | B | SE | β | t |
|---|---|---|---|---|
| Age | 0.015 | 0.011 | .062 | 1.34 |
| Sex | 0.113 | 0.311 | .016 | 0.36 |
| Education (years) | −0.033 | 0.052 | −.029 | −0.63 |
| Combat exposure | 0.001 | 0.009 | .005 | 0.10 |
| Symptom exaggeration | 1.150 | 0.538 | .099 | 2.13* |
| mTBI | 0.330 | 0.212 | .075 | 1.55 |
| Depressive disorder | 1.646 | 0.234 | .349 | 7.05*** |
| PTSD | 1.009 | 0.235 | .236 | 4.30*** |
| Anxiety disorder | 0.448 | 0.240 | .084 | 1.86 |
| Substance use disorder | 0.180 | 0.260 | .031 | 0.69 |
| Pain | 1.086 | 0.216 | .238 | 5.04*** |
| Sleep disturbance | 0.814 | 0.232 | .167 | 3.51** |
Note. n = 232. R2 = .59. Adjusted R2 = .57. WHODAS = World Health Organization Disability Assessment Schedule II; mTBI = mild traumatic brain injury; PTSD = posttraumatic stress disorder.
p < .05.
p < .01.
p < .001.
Table 3.
Standardized β for WHODAS Domains Associated with Demographic, Psychiatric, and Behavioral Conditions
| Variable | UC | GA | SC | GAWP | LA | PS |
|---|---|---|---|---|---|---|
| Age | .052 | .091 | .030 | .051 | .044 | .050 |
| Sex | −.015 | −.031 | .033 | .043 | .040 | .003 |
| Education (years) | −.004 | −.052 | .058 | −.008 | .010 | −.033 |
| Combat exposure | .025 | .005 | .032 | .050 | −.059 | .016 |
| Symptom exaggeration | .115* | .174** | .059 | .029 | .084 | .049 |
| mTBI | .058 | .110 | .151* | .040 | .029 | .040 |
| Depressive disorder | .223*** | .265*** | .358*** | .340*** | .280*** | .365*** |
| PTSD | .240*** | −.066 | .105 | .317*** | .159* | .279*** |
| Anxiety disorder | .146** | .020 | −.003 | .073 | .069 | .042 |
| Substance use disorder | .087 | −.017 | −.014 | −.034 | .029 | .049 |
| Pain | .218*** | .261*** | .134* | .088 | .247*** | .233*** |
| Sleep disturbance | .147** | .156** | .085 | .141** | .144* | .109* |
Note. n = 233. Adjusted R2: Understanding and Communicating (UC) = .45, Getting Around (GA) = .34, Self-Care (SC) = .29, Getting Along with People (GAWP) = .46, Life Activities (LA) = .33, Participation in Society (PS) = .54. WHODAS = World Health Organization Disability Assessment Schedule II; mTBI = mild traumatic brain injury; PTSD = posttraumatic stress disorder.
p < .05.
p < .01.
p < .001.
To investigate how these diagnoses were related, an exploratory factor analysis (eigenvalue > 0.88) with the individual psychiatric and behavioral conditions was conducted. Loadings from the rotated solution are presented in Table 4. The four factor solution selected accounted for 76.9% of the total variance. They were labeled (a) deployment trauma (depressive disorder, PTSD, and military mTBI), (b) somatic (pain and sleep disturbance), (c) anxiety (any non-PTSD anxiety disorder), and (d) substance use (alcohol or other substance abuse/dependence).
Table 4.
Principal Factors Analysis of mTBI, Psychiatric Conditions, and Behavioral Conditions
| Variable | Deployment trauma | Somatic | Anxiety | Substance use |
|---|---|---|---|---|
| mTBI | .644 | .039 | −.413 | −.015 |
| Depressive disorder | .767 | .041 | .121 | .021 |
| PTSD | .797 | .064 | .124 | .173 |
| Pain | .039 | .910 | −.043 | .021 |
| Sleep disturbance | .076 | .904 | −.013 | −.073 |
| Anxiety disorder | .121 | −.045 | .925 | .017 |
| Substance use | .095 | −.041 | .018 | .986 |
| % variance explained | 23.8 | 23.6 | 15.1 | 14.4 |
| Eigenvalue | 1.89 | 1.58 | 1.05 | 0.88 |
Note. N = 236. mTBI = mild traumatic brain injury; PTSD = posttraumatic stress disorder.
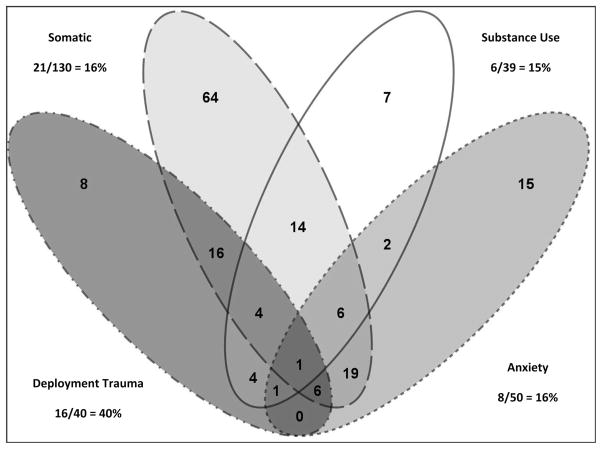
We established each study participants’ clinical profile based on the conditions comprising each factor. Figure 1 displays the total number of participants who were diagnosed with the conditions that comprise these factors, which are not mutually exclusive. As shown, 40 (16.9%) participants were diagnosed with the three co-occurring conditions comprising the deployment trauma factor (i.e., depressive disorder, PTSD, and military mTBI), 130 (55.1%) reported conditions comprising the somatic factor, 39 (16.5%) were diagnosed with the conditions comprising the substance use factor, and 50 (21.2%) were diagnosed with the conditions comprising the anxiety factor.
Figure 1.
Extracted factors and the percentage of participants who reported substantial disability. The factors were based on number of participants with the diagnosis comprising each factor. Substantial disability (numerator) was calculated as the number of participants who reported substantial disability (WHODAS ≥ 45) over the number of participants with the diagnosis comprising each factor (denominator).
Exploratory analyses were conducted to determine whether the empirically derived clinical factors were differentially associated with disability. To ensure the deployment trauma factor’s association to disability was not simply a matter of burden of illness, or driven by the individual or pairwise components of the deployment trauma factor, we conducted a series of post hoc t tests. Participants in the deployment trauma group were compared to nondeployment trauma participants with three or more comorbidities and to participants with pairwise components of the deployment trauma factor (Table 5 and Supplemental Table B). When compared to nondeployment trauma participants with three or more comorbidities, participants in the deployment trauma group reported significantly worse general functioning (i.e., WHODAS total score). Additionally, when compared to participants with PTSD and a military mTBI, but no depressive disorder, participants in the deployment trauma group reported worse general functioning overall and in all subdomains except Getting Around. Finally, when compared to participants with depressive disorder and PTSD, but no military mTBI, participants in the deployment trauma group reported numerically worse general functioning which was not, however, statistically lower (p = .113). Participants in the deployment trauma group reported significantly greater disability in Self-Care and Getting Along with People, with worse scores on every WHODAS subscale. Of note, participants in the deployment trauma group did report significantly more combat exposure than participants with current PTSD and depression only; however, adjustment for combat exposure provided nearly identical results as reported in Table 5.
Table 5.
Reported Disability in Participants With and Without the Components of the Deployment Trauma Factor
| Variable | Deployment trauma (n = 40) | Other trauma + 3 comorbidities (n = 106) | Depression + PTSD (n = 28) | PTSD + mTBI (n = 36) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
||||||||
| M | SD | M | SD | t | M | SD | t | M | SD | t | |
| WHODAS | |||||||||||
| Total | 38.41 | 20.11 | 20.05 | 13.30 | −5.11*** | 31.12 | 14.08 | −1.61 | 19.08 | 11.52 | −4.97*** |
| UC | 39.81 | 23.03 | 27.06 | 17.88 | −3.42*** | 38.89 | 19.23 | −0.17 | 26.59 | 15.66 | −2.82** |
| GA | 28.06 | 24.27 | 16.43 | 19.50 | −2.89** | 26.85 | 21.89 | −0.20 | 18.68 | 22.06 | −1.69 |
| SC | 18.75 | 17.17 | 4.88 | 9.17 | −4.63*** | 7.64 | 10.73 | −3.15** | 5.88 | 10.87 | −3.77*** |
| GAWP | 47.22 | 25.73 | 22.67 | 17.58 | −5.32*** | 35.37 | 18.55 | −2.03* | 20.59 | 15.06 | −5.32*** |
| LA | 40.10 | 27.70 | 24.08 | 20.68 | −3.18** | 34.61 | 22.83 | −0.84 | 20.96 | 17.02 | −3.51*** |
| PS | 48.09 | 26.22 | 21.99 | 17.42 | −5.56*** | 37.04 | 20.15 | −1.82 | 18.75 | 13.50 | −5.93*** |
Note. The groups being compared to the deployment trauma (DT) group are not mutually exclusive. Some ns in this table differ from Supplemental Table B due to missing data. Statistics were computed only between the DT group and each of the other groups. The p values are adjusted for multiple comparisons using a bootstrap method. WHODAS = World Health Organization Disability Assessment Schedule II; UC = Understanding and Communicating; GA = Getting Around; SC = Self-Care; GAWP = Getting Along with People; LA = Life Activities; PS = Participation in Society.
p < .05.
p < .01.
p < .001.
Finally, we examined participants with a WHODAS overall score ≥ 45 (n = 22), indicating substantial disability (Von Korff et al., 2005). Forty percent of participants with the deployment trauma factor reported substantial disability compared to 15%–16% of participants with each of the other three factors. Further, approximately 75% of those who reported substantial disability had the conditions comprising the deployment trauma factor. Thus, individuals with the three deployment trauma conditions represented a disproportionate subgroup of the sample with substantial disability. To determine whether the individual and paired constituents of the deployment trauma factor were related to substantial disability, we examined these subgroups. Participants with the deployment trauma factor were 3.52 times more likely to report substantial disability than participants with depressive disorder and PTSD, but no military, mTBI 95% CI [1.09, 11.37]; χ2(1, N = 63)= 4.59; p = .032).
Discussion
This study demonstrated that there are several prevalent conditions that must be considered, in addition to mTBI and PTSD, in returning OEF/OIF/OND service members and veterans. Strikingly, over 90% of the sample was diagnosed with a current psychiatric or behavioral condition, and 50% had three or more psychiatric and behavioral comorbidities. Without other variables in the model, a history of military mTBI was associated with increased presence of mental health issues. PTSD was 300% more likely and depressive disorders, pain, and sleep disturbance were at least 140% more likely in this group. The association between mTBI and mental health issues is similar to previous findings (Taylor et al., 2012).
In addition to a high prevalence of psychiatric diagnoses, this sample also reported significant disability. Remarkably, the TRACTS cohort reported worse functioning on the WHODAS disability scale than approximately 80% of the worldwide sample (WHO, 2010) and endorsed difficulties in all functional domains. The impairments in completing tasks in major life domains can also be conceptualized as reintegration issues. We are not the first group to demonstrate that veterans struggle with difficulties in postdeployment functioning, particularly in social and occupational roles (Beder et al., 2011; Sayer et al., 2010). Identification of the psychiatric and behavioral factors that predict disability can guide strategic treatment to improve functional outcome.
Although participants diagnosed with the conditions that comprise the deployment trauma factor significantly differed from participants with the combination of PTSD and depression without mTBI on only two of the WHODAS subscales, they obtained nominally higher disability scores on all subscales and the total score. The specific combination of depressive disorder, PTSD, and mTBI may cause a unique vulnerability for compromised functional outcome/disability. Participants who were diagnosed with the conditions comprising the deployment trauma factor reported more disability than participants who were diagnosed with any three other co-occurring conditions. Interestingly, PTSD and depression, but not military mTBI, were associated with overall disability and specific areas of functioning. This is not completely unexpected, as a history of mTBI has previously been shown to be unrelated to general functioning (Lippa et al., 2014). As the current data support, however, mTBI may be a critical moderating factor in predicting functional status after deployment when other clinical conditions are present (e.g., PTSD, depression, among other psychiatric and behavioral comorbidities). Our findings suggest that the most concerning combination of diagnoses may actually be depression, PTSD, and mTBI. It is possible that the specific combination of these three diagnoses may be biologically significant and increase the risk for other clinical issues (e.g., sleep disturbance, substance abuse) and substantial disability. Perhaps not surprisingly, invalid NSI responding was associated with increased disability. Reduced effort has previously been associated with functional outcomes among veterans with mTBI (Lippa et al., 2014).
The primary limitation of this study was the relatively small subsample (n = 40, 16%) of individuals with the three conditions comprising the deployment trauma factor. Nevertheless, if this proportion represents a true estimate of the incidence at which these three conditions co-occur, there are hundreds of thousands of service members and veterans at risk for substantial disability. Given the potentially critical implications, cross validation and replication in larger epidemiological studies are warranted. Additionally, we did not have the statistical power to investigate the relationship between predeployment TBI and psychiatric diagnoses and functional outcome. Predeployment physical and psychiatric diagnoses likely play important roles in functional outcome, however, and should be investigated in future studies. Finally, as these data were cross sectional, we were unable to infer causality between our variables of interest. Future studies should explore physiological, genetic, neuropsychological, and environmental correlates of the deployment trauma factor and whether any of these correlates serve as risk or resiliency factors.
In summary, this study demonstrated high rates of co-occurring psychiatric and behavioral diagnoses in returning service members and veterans. Indeed, roughly a quarter of participants fit into multiple clinical factors. The interacting effects of these multiple psychiatric and behavioral conditions in the cohort likely leads to additive, if not multiplicative, functional impairments in daily living, as demonstrated by increased disability. The combination of current depressive disorder, PTSD, and a history of military mTBI may represent a biologically significant clinical phenotype (deployment trauma factor) that increases the risk for other clinical issues (e.g., sleep disturbance, substance abuse) and substantial disability.
OEF/OIF/OND veterans represent a complicated, polymorbid population that does not fit into typical standard of care models, which target one diagnosis at a time. Given the tendency for enduring symptoms in one domain to thwart rehabilitative progress in other domains (Vanderploeg, Belanger, & Curtiss, 2009), OEF/OIF/OND veterans will not likely benefit from treatment of either cognitive or emotional symptoms in isolation. Rather, they require highly integrative interventions that will be appropriate for the range of treatment challenges they present.
Acknowledgments
This research was supported by the Translational Research Center for TBI and Stress Disorders (TRACTS), a VA Rehabilitation Research and Development (RR&D) Traumatic Brain Injury Center of Excellence (B6796-C) and VA CSR&D Merit Review Award to Regina McGlinchey, and NIH NIA K01AG024898 to Catherine Fortier. We would like to thank Wally Musto for his championing of our work among military personnel and his tireless recruitment efforts on our behalf, as well as the entire TRACTS team for their assistance with data collection and management. We would also like to thank Drs. Patricia Dorn and Stuart Hoffman of VA RR&D for their support of our TBI CoE. Lastly, we would like to thank the anonymous reviewers of this manuscript for their thoughtful comments, which substantially strengthened the manuscript.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5. Arlington, VA: Author; 2013. [Google Scholar]
- Bay E, de-Leon MB. Chronic stress and fatigue-related quality of life after mild to moderate traumatic brain injury. Journal of Head Trauma Rehabilitation. 2011;26:355–363. doi: 10.1097/HTR.0b013e3181f20146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beder J, Coe R, Sommer D. Women and men who have served in Afghanistan/Iraq: Coming home. Social Work in Health Care. 2011;50:515–526. doi: 10.1080/00981389.2011.554279. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers F, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, Keane TM. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. Behavior Therapist. 1990;13:187–188. doi: 10.1007/BF02105408. [DOI] [Google Scholar]
- Bryant R. Post-traumatic stress disorder vs traumatic brain injury. Dialogues in Clinical Neuroscience. 2011;13:251–262. doi: 10.31887/DCNS.2011.13.2/rbryant. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter JS, Andrykowski MA. Psychometric evaluation of the Pittsburgh Sleep Quality Index. Journal of Psychosomatic Research. 1998;45:5–13. doi: 10.1016/s0022-3999(97)00298-5. [DOI] [PubMed] [Google Scholar]
- Cicerone KD, Karlmar K. Persistent postconcussion syndrome. Journal of Head Trauma Rehabilitation. 1995;10:1–17. doi: 10.1097/00001199-199506000-00002. [DOI] [Google Scholar]
- Cifu DX, Taylor BC, Carne WF, Bidelspach D, Sayer NA, Scholten J, Campbell EH. Traumatic brain injury, posttraumatic stress disorder, and pain diagnoses in OIF/OEF/OND Veterans. Journal of Rehabilitation Research and Development. 2013;50:1169–1176. doi: 10.1682/JRRD.2013.01.0006. [DOI] [PubMed] [Google Scholar]
- Erbes CR, Kaler ME, Schult T, Polusny MA, Arbisi PA. Mental health diagnosis and occupational functioning in National Guard/Reserve veterans returning from Iraq. Journal of Rehabilitation Research and Development. 2011;48:1159–1170. doi: 10.1682/jrrd.2010.11.0212. [DOI] [PubMed] [Google Scholar]
- Fichtenberg NL, Putnam SH, Mann NR, Zafonte RD, Millard AE. Insomnia screening in postacute traumatic brain injury: Utility and validity of the Pittsburgh Sleep Quality Index. American Journal of Physical Medicine and Rehabilitation. 2001;80:339–345. doi: 10.1097/00002060-200105000-00003. [DOI] [PubMed] [Google Scholar]
- Fichtenberg NL, Zafonte RD, Putnam S, Mann NR, Millard AE. Insomnia in a post-acute brain injury sample. Brain Injury. 2002;16:197–206. doi: 10.1080/02699050110103940. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for the DSM-IV Axis I Disorders. Washington, DC: American Psychiatric Press; 1996. [Google Scholar]
- Fortier CB, Amick MM, Grande L, McGlynn S, Kenna A, Morra L, … McGlinchey RE. The Boston Assessment of Traumatic Brain Injury-Lifetime (BAT-L) semistructured interview: Evidence of research utility and validity. Journal of Head Trauma Rehabilitation. 2014;29:89–98. doi: 10.1097/HTR.0b013e3182865859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grafton KV, Foster NE, Wright CC. Test-retest reliability of the Short-Form McGill Pain Questionnaire: Assessment of intraclass correlation coefficients and limits of agreement in patients with osteoarthritis. Clinical Journal of Pain. 2005;21:73–82. doi: 10.1097/00002508-200501000-00009. [DOI] [PubMed] [Google Scholar]
- Guyker WM, Donnelly K, Donnelly JP, Dunnam M, Warner GC, Kittleson J, … Meier ST. Dimensionality, reliability, and validity of the combat experiences scale. Military Medicine. 2013;178:377–384. doi: 10.7205/MILMED-D-12-00223. [DOI] [PubMed] [Google Scholar]
- Higgins DM, Kerns RD, Brandt CA, Haskell SG, Bathulapalli H, Gilliam W, Goulet JL. Persistent pain and comorbidity among Operation Enduring Freedom/Operation Iraqi Freedom/Operation New Dawn veterans. Pain Medicine. 2014;15:782–790. doi: 10.1111/pme.12388. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:13–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. New England Journal of Medicine. 2008;358:453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight JA, Samper RE. Deployment Risk and Resilience Inventory: A collection of measures for studying deployment-related experiences of military personnel and veterans. Military Psychology. 2006;18:89–120. doi: 10.1207/s15327876mp1802_1. [DOI] [Google Scholar]
- Lew HL, Otis JD, Tun C, Kerns RD, Clark ME, Cifu DX. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: Polytrauma clinical triad. Journal of Rehabilitation Research and Development. 2009;46:697–702. doi: 10.1682/jrrd.2009.01.0006. [DOI] [PubMed] [Google Scholar]
- Lippa SM, Pastorek NJ, Romesser J, Linck J, Sim AH, Wisdom NM, Miller BI. Ecological validity of performance validity testing. Archives of Clinical Neuropsychology. 2014;29:236–244. doi: 10.1093/arclin/acu002. [DOI] [PubMed] [Google Scholar]
- Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II) Clinical Psychology and Psychotherapy. 2011;18:75–79. doi: 10.1002/cpp.693. [DOI] [PubMed] [Google Scholar]
- Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein MB, Malley JC, Johnson DC, Southwick SM. Subsyndromal posttraumatic stress disorder is associated with health and psychosocial difficulties in veterans of Operations Enduring Freedom and Iraqi Freedom. Depression and Anxiety. 2009;26:739–744. doi: 10.1002/da.20574. [DOI] [PubMed] [Google Scholar]
- Pittman JO, Goldsmith AA, Lemmer JA, Kilmer MT, Baker DG. Post-traumatic stress disorder, depression, and health-related quality of life in OEF/OIF veterans. Quality of Life Research. 2012;21:99–103. doi: 10.1007/s11136-011-9918-3. [DOI] [PubMed] [Google Scholar]
- Sayer NA, Noorbaloochi S, Frazier P, Carlson K, Gravely A, Murdoch M. Reintegration problems and treatment interests among Iraq and Afghanistan combat veterans receiving VA medical care. Psychiatric Services. 2010;61:589–597. doi: 10.1176/appi.ps.61.6.589. [DOI] [PubMed] [Google Scholar]
- Schneiderman AI, Braver ER, Kang HK. Understanding sequelae of injury mechanisms andmild traumatic brain injury incurred during the conflicts in Iraq and Afghanistan: Persistent postconcussive symptoms and posttraumatic stress disorder. American Journal of Epidemiology. 2008;167:1446–1452. doi: 10.1093/aje/kwn068. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Lunney CA, Bovin MJ, Marx BP. Posttraumatic stress disorder and quality of life: Extension of findings to veterans of the wars in Iraq and Afghanistan. Clinical Psychology Review. 2009;29:727–735. doi: 10.1016/j.cpr.2009.08.006. [DOI] [PubMed] [Google Scholar]
- Seal KH, Metzler TJ, Gima KS, Bertenthal D, Maguen S, Marmar CR. Trends and risk factors for mental health diagnoses among Iraq and Afghanistan veterans using Department of Veterans Affairs health care, 2002–2008. American Journal of Public Health. 2009;99:1651–1658. doi: 10.2105/AJPH.2008.150284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soberg HL, Finset A, Roise O, Bautz-Holter E. The trajectory of physical and mental health from injury to 5 years after multiple trauma: A prospective, longitudinal cohort study. Archives of Physical Medicine and Rehabilitation. 2012;93:765–774. doi: 10.1016/j.apmr.2011.08.050. [DOI] [PubMed] [Google Scholar]
- Stein MB, McAllister TW. Exploring the convergence of posttraumatic stress disorder and mild traumatic brain injury. American Journal of Psychiatry. 2009;166:768–776. doi: 10.1176/appi.ajp.2009.08101604. [DOI] [PubMed] [Google Scholar]
- Strauss E, Sherman E, Spreen O. A compendium of Neuropsychological Tests. 3. New York, NY: Oxford University Press; 2006. [Google Scholar]
- Taylor BC, Hagel EM, Carlson KF, Cifu DX, Cutting A, Bidelspach DE, Sayer NA. Prevalence and costs of co-occurring traumatic brain injury with and without psychiatric disturbance and pain among Afghanistan and Iraq war veteran V.A. users. Medical Care. 2012;50:342–346. doi: 10.1097/MLR.0b013e318245a558. [DOI] [PubMed] [Google Scholar]
- Terrio H, Brenner LA, Ivins BJ, Cho JM, Helmick K, Schwab K, … Warden D. Traumatic brain injury screening: Preliminary findings in a US Army Brigade Combat Team. Journal of Head Trauma Rehabilitation. 2009;24:14–23. doi: 10.1097/HTR.0b013e31819581d8. [DOI] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry. 2010;67:614–623. doi: 10.1001/archgenpsychiatry.2010.54. [DOI] [PubMed] [Google Scholar]
- UCLA Statistical Counseling Group. Using proc mlttest to perform multiple comparisons. 2014 Retrieved from http://www.ats.ucla.edu/stat/sas/library/multtest.htm/
- U.S. Department of Defense. Demographics profile of the military community. Washington, DC: Author; 2012. [Google Scholar]
- U.S. Department of Veterans Affairs. Analysis of VA Health care utilization among Operation Enduring Freedom, Operation Iraqi Freedom, and Operation New Dawn veterans, from 1st qtr FY 2002 through 1st qtr FY 2012. Washington, DC: Author; 2012. [Google Scholar]
- U.S. Department of Veterans Affairs and U.S. Department of Defense. VA/DOD clinical practice guideline for the management of concussion/mild traumatic brain injury. 2009 Retrieved from http://www.healthquality.va.gov/mtbi/concussion_mtbi_full_1_0.pdf.
- Vanderploeg RD, Belanger HG, Curtiss G. Mild traumatic brain injury and posttraumatic stress disorder and their associations with health symptoms. Archives of Physical Medicine and Rehabilitation. 2009;90:1084–1093. doi: 10.1037/e717692011-007. [DOI] [PubMed] [Google Scholar]
- Vanderploeg RD, Cooper DB, Belanger HG, Donnell AJ, Kennedy JE, Hopewell CA, Scott SG. Screening for postdeployment conditions: Development and cross-validation of an embedded validity scale in the neurobehavioral symptom inventory. Journal of Head Trauma Rehabilitation. 2014;29:1–10. doi: 10.1097/HTR.0b013e318281966e. [DOI] [PubMed] [Google Scholar]
- Von Korff M, Katon W, Lin EH, Simon G, Ludman E, Oliver M, … Bush T. Potentially modifiable factors associated with disability among people with diabetes. Psychosomatic Medicine. 2005;67:233–240. doi: 10.1097/01.psy.0000155662.82621.50. [DOI] [PubMed] [Google Scholar]
- Walker WC, McDonald SD, Ketchum JM, Nichols M, Cifu DX. Identification of transient altered consciousness induced by military-related blast exposure and its relation to postconcussion symptoms. Journal of Head Trauma Rehabilitation. 2013;28:68–76. doi: 10.1097/HTR.0b013e318255dfd0. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Ruscio AM, Keane TM. Psychometric properties of nine scoring rules for the Clinician-Administered Posttraumatic Stress Disorder Scale. Psychological Assessment. 1999;11:124–133. doi: 10.1037/1040-3590.11.2.124. [DOI] [Google Scholar]
- Williams JB, Gibbon M, First MB, Spitzer RL, Davies M, Borus J, … Wittchen HU. The Structured Clinical Interview for DSMIII-R (SCID). II. Multisite test-retest reliability. Archives of General Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]
- World Health Organization. A newsletter on noncommunicable diseases and mental health. Geneva, Switzerland: Author; 2004. [Google Scholar]
- World Health Organization. Measuring health and disability: Manual for WHO Disability Assessment Schedule. Geneva, Switzerland: Author; 2010. [Google Scholar]