Abstract
Background
Popular social media could extend the reach of smoking cessation efforts. In this systematic review, our objectives were: 1) to determine whether social media interventions for smoking cessation are feasible, acceptable, and potentially effective; 2) to identify approaches for recruiting subjects; and 3) to examine the specific intervention design components and strategies employed to promote user engagement and retention.
Methods
We searched Scopus, Medline, EMBASE, Cochrane Central, PsychINFO, CINAHL, and Web of Science through July 2016 and reference lists of relevant articles. Included studies described social media interventions for smoking cessation and must have reported outcomes related to feasibility, acceptability, usability, or smoking-related outcomes.
Results
We identified 7 studies (all were published since 2014) that enrolled 9755 participants (median=136 [range 40 to 9042]). Studies mainly used Facebook (n=4) or Twitter (n=2), and emerged as feasible and acceptable. Five studies reported smoking-related outcomes such as greater abstinence, reduction in relapse, and an increase in quit attempts. Most studies (n=6) recruited participants using online or Facebook advertisements. Tailored content, targeted reminders, and moderated discussions were used to promote participant engagement. Three studies found that active participation through posting comments or liking content may be associated with improved outcomes. Retention ranged from 35% to 84% (median=70%) across the included studies.
Conclusions
Our review highlights the feasibility, acceptability and preliminary effectiveness of social media interventions for smoking cessation. Future research should continue to explore approaches for promoting user engagement and retention, and whether sustained engagement translates to clinically meaningful smoking cessation outcomes.
Keywords: tobacco, cessation, smoking, social networking, social media, technology
1. Introduction
Smoking is the leading preventable cause of death in the United States, accounting for about 480,000 deaths annually and over $300 billion in direct medical care and lost productivity costs.1 Since the 1980’s the overall prevalence of cigarette smoking has declined, yet it is estimated that 40 million adults in the United States continue to smoke cigarettes.2 Several population groups also show disproportionately higher rates of tobacco use. For example, over the past 30 years there has been little change in smoking rates among young adults despite widespread public health efforts.3 Additionally, persons living below the poverty line and people with mental illness or physical disabilities are more likely to smoke cigarettes compared to the general population.1 It is critical to identify innovative approaches to advance population wide tobacco cessation efforts and to specifically target segments of the population at elevated risk for tobacco use.
Unprecedented growth in the use and availability of social media may afford new avenues for supporting tobacco cessation efforts. Social media encompasses interactive web and mobile platforms through which individuals and communities can share, co-create, or exchange information, ideas, photos, or videos within a virtual network. Nearly two thirds of adults in the United States use social media4, and for most of these individuals social media has become an important fixture of their daily lives, capturing their attention at repeated time points throughout the day.5 The barriers to using social media are low given that most social media platforms are freely available and can be accessed at any time of day from any device with connection to the Internet including mobile phones, tablets, or computers. Social media use remains highest among young people and individuals with higher education, though use has steadily increased among older age groups, low-income individuals, and among people from rural areas.4 Men and women use social media at comparable rates, and there are few differences in social media use between racial and ethnic groups (e.g., 56% of African Americans, 65% of Hispanics, and 65% of non-Hispanic whites use social media).4
Social media platforms such as Facebook or Twitter have been increasingly used for health promotion and supporting public health efforts, as highlighted in a recent systematic review of 73 studies.6 For example, this prior review found that social media appeared promising for reaching adolescents and young adults, and for targeting problem alcohol or substance use behaviors, mental health, and individuals at-risk of sexually transmitted diseases.6 One study demonstrated the feasibility and acceptability of engaging homeless youth in an HIV-prevention program using YouTube and online communities on Facebook and MySpace.7 Another study showed that Facebook could successfully support recruitment of young adult veterans with high rates of mental illness, problem drinking and substance use.8 Given the popularity of social media and mounting evidence supporting the use of these platforms for public health efforts and for reaching at-risk groups, there may be opportunities to reach people who have disproportionately elevated risk of smoking cigarettes and who have been difficult to engage through traditional tobacco cessation efforts.
Social media interventions could build on the success of existing web-based smoking cessation efforts. For instance, several studies support the effectiveness of web-based programs for smoking cessation9,10, with some programs achieving quit rates that exceed 24%.11 Despite this success, there have been limitations in effectiveness due to substantial drop-off in participation9, and the continued reliance on the static delivery of text-based information through self-directed learning, didactic sessions led by professionals, and few opportunities for interaction with other individuals who are also trying to quit smoking.12 Interactive elements such as discussion boards or forums have been included as part of several web-based programs and appear promising for engaging users10, though these components have not been central to these interventions. In contrast, social media is highly interactive by its very nature, and may represent an avenue through which to support smoking cessation efforts by allowing users to connect with and support each other, and share their experiences or challenges in quitting smoking by posting text, photos, images, or videos.13
Research shows that health behaviors can disseminate rapidly on social media, including the onset of smoking behaviors through exposure to images or depictions of tobacco use14,15, as well as interest in quitting by connecting with and learning from others who share similar health goals.16,17 Longitudinal data suggest that individuals who were able to successfully quit smoking had more network ties and had more direct interactions with others over social media compared to those who did not quit.18 Social interaction may be key for supporting smoking cessation on social media, yet public health campaigns on social media have largely focused on dissemination rather than engaging and interacting with users.19 The success of tobacco cessation efforts on social media will likely depend on whether the interactive features of these platforms may be effectively leveraged to engage users and members of their online networks towards encouraging and supporting the decision to quit smoking.
As social media platforms continue to evolve rapidly and use of these platforms becomes more prevalent across diverse population groups, it is critical to determine whether social media is feasible, acceptable, and potentially effective for delivering smoking cessation interventions. Identifying the features of social media interventions that appear effective and the strategies that have been successful for overcoming challenges with reaching target populations will inform the design of future smoking cessation interventions. The purpose of this systematic review is to summarize the evidence on the use of social media for smoking cessation. We address the following objectives: 1) to determine whether social media interventions for smoking cessation are feasible, acceptable, and potentially effective; 2) to identify effective strategies for recruiting subjects; and 3) to examine the specific intervention design components and strategies employed to promote user engagement and retention.
2. Methods
2.1 Search Strategy
We registered our search strategy protocol to the PROSPERO International prospective register of systematic reviews (Registration number: CRD42016044080). We searched the following databases through July 31st, 2016: Scopus, Medline, EMBASE, Cochrane Central, PsychINFO, CINAHL, and Web of Science. We used search terms for social media. These terms were combined with tobacco, smoking, smoking cessation, tobacco reduction, tobacco consumption, and cigarette. Each term was entered as a key word and corresponding medical subject heading (MeSH) term. MeSH terms refer to the United States Library of Medicine’s controlled vocabulary thesaurus and are primarily used for indexing articles in Medline. Combining MeSH terms with general free text search terms is important in order to identify as many relevant records as possible.20 No language limits were applied. The complete search strategy used in Medline is listed in Table 1. We also searched reference lists of included studies, prior systematic reviews, and Google Scholar to identify additional relevant studies.
Table 1.
Search strategy used in Medline
| Search | Search Terms |
|---|---|
| #1 | "Social Media" OR "Social Media"[Mesh] |
| #2 | tobacco OR smoking OR "smoking cessation" OR "tobacco reduction" OR "tobacco consumption" OR "cigarette" OR "Tobacco Use Disorder"[Mesh] OR "Smoking Cessation"[Mesh] OR "Tobacco Use Cessation"[Mesh] OR "Tobacco Use"[Mesh] OR "Tobacco"[Mesh] OR "Tobacco Products"[Mesh] |
| #3 (final search) | #1 AND #2 |
Mesh indicates Medical Subject Heading
2.2 Study Selection Criteria
We only included studies that recruited participants and that evaluated an intervention for smoking cessation delivered through social media. Participants could be from any population group. We defined social media as interactive web and mobile platforms through which individuals and communities share, discover, co-create, or exchange information, ideas, photos, or videos within a virtual network.21 We included all types of study designs, but eligible studies had to report outcomes. All types of outcomes were deemed eligible. This could include outcomes related to feasibility, acceptability, safety, usability, efficacy, implementation, or effectiveness. Therefore, we excluded research protocols, review articles, non-intervention studies, and discussion articles.
2.3 Data Extraction and Analysis
One researcher (JN) independently screened titles of retrieved studies for eligibility. In this initial step, articles were excluded that were not relevant, such as articles that were not about cigarette smoking or tobacco use, that did not describe intervention studies, or did not involve the use of social media. The same researcher then screened abstracts of potentially eligible articles and discussed inclusion/exclusion of relevant articles with a second researcher (LM). Both researchers (JN & LM) then reviewed the final list of relevant studies for inclusion. The same two researchers then extracted the following data from the included studies: country of origin, social media platform, study design, sample size, sample gender, intervention description and characteristics, main outcomes, recruitment strategies, procedures for encouraging engagement with the intervention, and participant attrition. The researchers then organized these data into tables, and re-reviewed inclusion criteria before deciding on the final list of included studies. Both researchers (JN & LM) met on a weekly basis to discuss studies for inclusion and to reach consensus. In cases where there was uncertainty, a third researcher (SJK) was consulted. Three additional researchers (SJK, KA, & MB) also reviewed the final list of included studies. In many cases, results from a single study are published as multiple manuscripts, such as reporting of secondary outcomes. Therefore, we were careful to avoid over counting studies, though secondary analyses from studies that met our inclusion criteria were also reviewed to supplement data extraction. All authors reviewed the final tables. Given that many studies were preliminary and involved pilot evaluations, used varying study designs, and reported heterogeneous outcomes, a meta-analysis of quantitative findings was not possible.
2.4 Quality Assessment
We assessed the methodological quality of the included studies using a 12-item quality assessment scale adapted from prior systematic reviews.22,23 The scale covers four key domains related to the quality of the study methods: 1) study sample; 2) follow- up and attrition; 3) data collection; and 4) data analyses. Each domain has between 2 and 4 criteria, leading to a total of 12 quality assessment criteria. The quality criteria and domains are presented in Table 2. When the criteria were met the studies received positive scores (“Yes”), and when the criteria were not met the studies received negative scores (“No”). Two researchers (JN and LM) independently completed the quality assessments for the included studies. Both researchers then reviewed the ratings to ensure consistency and to reach consensus. All authors reviewed the final quality ratings.
Table 2.
Description of the adapted criteria used to assess the methodological quality of the included studiesa
| Criteria | Description | |
|---|---|---|
| Study Sample | ||
| 1. | Recruitment | Sufficient details provided about the recruitment methods to allow replication |
| 2. | Participation rate | Participation rate of at least 80% among individuals who met eligibility criteria. This helps to demonstrate that the sample is representative of the target population. |
| 3. | Baseline characteristics | Description of baseline study sample provided. Must include the following key characteristics: age, gender, and smoking status |
| Follow-up and Attrition | ||
| 4. | Follow-up | Number of participants listed for each follow-up measurement (e.g., CONSORT diagram included) |
| 5. | Duration | Follow-up is a minimum of 2 months |
| 6. | Attrition | Response at final follow-up measurement was at least 75% |
| 7. | Non-response | Non-response is not selective at follow-up measurement(s) and attrition is the same across all study arms |
| Data Collection | ||
| 8. | Outcomes | Smoking related outcomes collected (either objective or subjective) |
| 9. | Objective measures | Objective clinical outcomes collected |
| Data Analyses | ||
| 10. | Statistical analyses | Appropriate statistical model was used |
| 11. | Statistical model | The number of cases was at least 10 times the number of independent variables |
| 12. | Interpretation | Presentation of confidence intervals, standard error, or effect size to assist with interpretation of clinically meaningful differences in outcomes |
Criteria were adapted from methodological quality assessment tool used by te Velde et al. (2012)22
3. Results
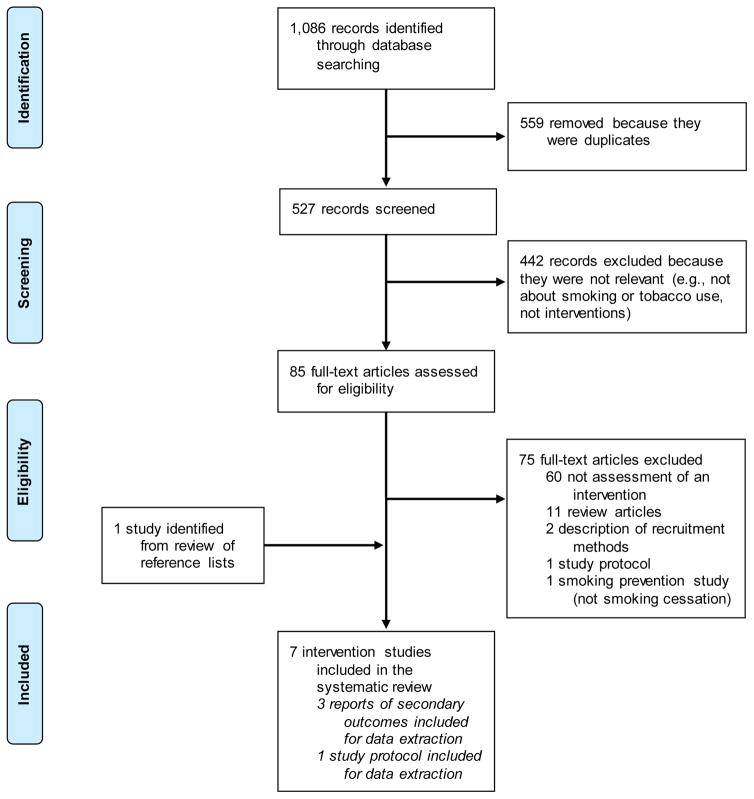
Our search of the different databases yielded 527 articles after removal of duplicates, of which 85 were relevant and required full-text review (Figure 1). We found one study evaluating an anti-smoking Facebook campaign for college students24, though we excluded this study because our primary focus in this review was smoking cessation rather than prevention. In total, 7 studies met our inclusion criteria, all of which were published since 2014. Among the included studies, two were from Canada25,26, one was from Hong Kong27, and four were from the United States.28–31 The studies enrolled a combined total of 9755 participants (range 40 to 9042; median = 136). Study samples ranged from 26% to 77% male. Four studies were randomized controlled trials24,27,28,30, one study employed a quasi-experimental design25, and the remaining three studies were pilot or initial feasibility studies.26,29,31 We also identified three articles reporting secondary outcomes32–34 and one study protocol35 corresponding to the included studies. We referred to these additional articles during our data extraction and analysis to ensure that complete methodological details and outcomes could be reported for each study. Characteristics of the included studies are summarized in Table 3.
Figure 1.
Flow diagram of studies included in the review
Table 3.
Summary of intervention studies using social media for smoking cessation
| Study | Origin | Social Media Platform | Study Design | Study Follow Up | Sample Description | Intervention Description | Key Findings |
|---|---|---|---|---|---|---|---|
| Bakersville et al (2016)25 | Canada | Interactive website, social media including Facebook and YouTube, and smartphone application | Quasi- experimental controlled trial | 3 months | 238 young adults (range 19–29 years); 43% male | Break-it-Off campaign encourages young adults to end their bad relationship with tobacco. Users can access interactive website, learn about methods for quitting, upload videos, connect to social media, and download free smartphone app to overcome triggers. Compared to Smokers’ Helpline telephone counseling smoking cessation service. | Break-it-Off users had higher 7-day and 30-day quit rates compared to Smoker’s Helpline users. At 3-months, Break-It-Off participants (32.4%) were more likely than SHL participants (14%) to have quit smoking for 30 days (p<0.001) and Break-it-Off participants (91%) were more likely than SHL participants (79%) to have made a quit attempt (p=0.04). |
| Cheung et al (2015)27 | Hong Kong | WhatsApp & Facebook | Pilot cluster RCT | 6 months | 136 recent quitters who completed an 8-week treatment program (mean age = 40.5 years [SD=9.9]); 77% male | Self-help booklet on smoking cessation and healthy diet and 2-month group discussion moderated by a smoking cessation counselor on WhatsApp compared to Facebook. 3 reminders sent each week by program moderator who was a social worker or nurse with smoking cessation counseling experience to reinforce abstinence and program content. Compared to self-help booklet only control group. | Lower relapse in the WhatsApp group compared to control group at 2-months (17% vs. 42.6%; p<0.05) and 6-months (52.5% vs. 61.1%; p<0.05). No differences in relapse in the Facebook group compared to control at 2-months (30% vs. 42.6%) and 6-months (52.2% vs. 61.1%). There was a trend for more posts in the WhatsApp group from the moderator (p=0.07) and participants (p=0.07) compared to the Facebook group, which could explain increased effectiveness. Biochemically verified abstinence did not differ between groups. |
| Cobb et al (2016)28
Study protocol:
Cobb et al (2014)35 |
United States | RCT | 30 days | 9,042 smokers (mean age = 43.9 years [SD=14.1]); 30% male | UbiQUITous Facebook app based on US Public Health Service ‘5As’ model (Ask, Advise, Assess, Assist and Arrange). Users interact with Dr. Youkwitz, a character who supports quitting and setting a quit date. App is also available for non-smoker supporters. Trial compared 3 app components: duration of use, content sharing, and use by non-smoker supporters. | Diffusion of the application through Facebook was primary outcome. Combined strategies for sharing and increasing duration of use contributed to highest level of diffusion. Involving non- smoker supporters did not affect diffusion. No smoking-related outcomes reported. | |
| Haines- Saah et al (2015)26 | Canada | Mixed methods feasibility study | 12 weeks | 60 young adult smokers or recent quitters (range 19–24 years); 57% male | “Picture Me Smokefree” is a Facebook photography group. Participants are encouraged to post pictures with captions related to quitting smoking. M oderator posts photo-challenges, topics, or contests. | Photo group appeared feasible and provided opportunity for young adults to access peer support for quitting smoking. Participants indicated preference for mixed gender groups. Challenges with attracting and retaining participants. M ore interactive features are necessary in future interventions. | |
| Pechmann et al (2015)29 | United States | Pre-post feasibility study | 60 days | 40 smokers (mean age = 36.5 years [SD=9.5]; range 20–57 years); 40% male | Tweet2Quit includes closed groups on Twitter with 20 people and daily automated messages to encourage group discussion about evidence- based smoking cessation topics, or to provide individualized feedback to participants about their interaction in the group. Automated Twitter intervention combined with evidence-based practices. Participants were sent nicotine patches, were referred to the National Institutes of Health online quit-smoking guide, and were instructed | M ore frequent tweeting was not related to abstinence. Tweeting about smoking related topics such as setting a quit date or using nicotine patches (p=0.024), overcoming barriers to quitting smoking (p=0.008), and expressing confidence about quitting (p=0.032) were related to abstinence. | |
| Pechmann et al (2016)30
Secondary outcomes: Lakon et al (2016)32 |
United States | RCT | 60 days | 160 smokers (mean age = 35.7 years [SD=9.9]; range 18–59 years); 26% male | Tweet2Quit consists of automated tweets to encourage discussion about quitting smoking sent daily and individualized automated feedback text messages sent to participants’ phones daily for 100 days. Combined with usual care consisting of nicotine patches, referral to smokefree.gov cessation website, and instructions to set a quit date within 7 days. Compared to usual care only control condition. | Intent-to-treat analyses showed that sustained abstinence was greater among Tweet2Quit participants compared to control participants at 7 days (41.25% vs. 37.50%), 30 days (57.50% vs. 38.75%), and 60 days (55.00% vs. 41.25%; p=0.021). Among study completers at 60 days follow-up, Tweet2Quit showed greater sustained abstinence (40.0%, 26/65) compared to the control group (20.0%, 14/70; p=0.017). Greater tweet volume was associated with sustained abstinence (p<0.001). | |
| Ramo et al (2015)31 Secondary outcomes: Ramo et al (2014)33 and Thrul et al (2015)34 |
United States | Pre-post feasibility study | 12 months | 79 young adult smokers (mean age = 20.8 years [SD=2.1]; range 18–25 years); 69% male | Secret Facebook groups tailored to participants’ stage of change: Precontemplation (“Not Ready to Quit”), Contemplation (“Thinking About Quitting”), or Preparation (“Getting Ready to Quit”). Targeted Facebook posts daily for 90 days consistent with US Public Health Service guidelines. Weekly interactive sessions moderated by the lead researcher to address any questions related to smoking or quitting. Additional optional group cognitive behavioral therapy counseling through Facebook chat. | Participants prepared to quit increased from 10 (13%) to 36 (46%) at 12-months. 28 (35%) participants reduced cigarette consumption by 50% or greater; 52 (66%) made a 24-hour quit attempt during the study. Assuming that missing participants are still smoking, then biochemically verified abstinence was 5% at 3-months, 8% at 6- months, and 8% at 12-months, compared to self- reported 7-day point prevalence of 9% at 3- months, 18% at 6-months, and 13% at 12-months. Posting more comments in the Facebook group was associated with biochemically verified abstinence at 3-months (p=0.036). |
3.1 Types of interventions
As described in Table 3, the studies ranged in duration from as little as 30 days up to 12-months, with the median follow-up of 84 days (range = 30 to 365 days). All seven studies focused on smoking cessation, of which four used Facebook.26–28,31 One study compared the use of closed discussion groups on Facebook with closed discussion groups on WhatsApp for preventing relapse among recent quitters.27 In another study participants in a closed Facebook group were encouraged to post photos related to their experiences quitting smoking26, while in another study the researchers posted content in the Facebook group that was tailored to participants’ stage of readiness to quit smoking.31 One study involved a Facebook game where users could interact with a cartoon character that provided support and encouragement to set a quit date.28,35 There were also two studies using Twitter, where daily “Tweets” were posted to a closed group to encourage discussion among participants about the benefits of quitting smoking and to provide targeted support and feedback.29,30 The Twitter messages in these two studies were combined with use of nicotine patches.29,30 Another study used an interactive website, social media including Facebook and YouTube, and a smartphone application as part of a campaign framed around the theme of a “break up” to encourage young adults to end their “bad relationship” with tobacco products.25
3.2 Study outcomes
As highlighted in Table 3, five studies reported smoking-related outcomes. Participants in a WhatsApp group reported lower relapse rates compared to a control group at 2-months and 6-months, but no differences in relapse in a Facebook group compared to a control group at 2-months and 6-months.27 There was a trend for more posts in the WhatsApp group from the moderator and participants compared to the Facebook group, which could explain the increased effectiveness.27 This study also reported biochemically verified abstinence at 2-months and 6-months collected in-person by research staff using exhaled carbon monoxide and saliva cotinine tests, though there were no differences between groups.27 One study using a closed Facebook group tailored to participants’ stage of readiness to quit contributed to reduced cigarette consumption and an increase in quit attempts.31 This study also collected biochemical measures of smoking abstinence using mailed saliva cotinine test kits. With the assumption that missing participants continue smoking, biochemically verified abstinence was 5% at 3-months, 8% at 6-months, and 8% at 12-months, compared to self-reported 7-day point prevalence of 9% at 3-months, 18% at 6-months, and 13% at 12-months.31 In this study, more commenting in the Facebook group was associated with biochemically verified abstinence at 3-month follow-up.31 In a pilot study using Twitter, more frequent tweeting about smoking related topics such as setting a quit date, using nicotine patches, overcoming barriers to quitting, and expressing confidence about quitting was significantly associated with abstinence.29 A subsequent randomized controlled trial of this Twitter intervention demonstrated greater abstinence compared to a usual care control condition, and showed that greater tweet volume significantly predicted sustained abstinence.30 A quasi-experimental study of a smoking cessation campaign for young adults involving an interactive website connected to social media and a free smartphone application showed greater abstinence compared to standard smokers helpline telephone counseling.25 Of the two remaining studies, one demonstrated the feasibility of a closed Facebook photography group for young adult smokers26, and the other reported the diffusion of a game for smoking cessation through the Facebook network.28,35
3.3 Participant recruitment strategies
The included studies primarily recruited participants using Facebook, Google, or other online advertisements (see Table 4).25,28–31,35 Of these studies, one reported that the cost to recruit each participant using Facebook advertisements was $8.80.31,33 Another study recruited participants using a combination of online and traditional face-to-face approaches, including Facebook advertisements, Twitter posts, as well as flyers, posters, print ads, and craigslist postings.26 One study recruited participants from a clinical setting who successfully completed a treatment program.27
Table 4.
Participant recruitment, engagement and retention in intervention studies using social media for smoking cessation
| Study | Social media platform | Recruitment | Methods for promoting participant engagement | Participant engagement outcome | Methods for promoting participant retention | Participant retention outcome |
|---|---|---|---|---|---|---|
| Bakersville et al (2016)25 | Interactive website, social media campaign, and smartphone app | The Break-It-Off campaign was promoted through ads on Facebook, Google, Yahoo, and M icrosoft, and through television, radio, and print ads. Participants in the research study were recruited through the BIO website and ads on online classified services. The Smokers Helpline comparison group participants were recruited by phone. From January to M arch 2012 there were 44,172 total visits and 37,325 unique visitors to the BIO website. 342 registered for the study. | Participants received a $10 iTunes gift card for enrolling in the research study and a $15 iTunes gift card for completing the follow-up survey. | BIO campaign includes mobile app and integrated social media. Of the 37,325 visitors, 3937 downloaded the mobile app and 339 posted content on the social media components (Facebook and YouTube). | Participants received a $15 iTunes gift card for completing the follow-up survey. | 102 (34%) of BIO participants and 136 (52%) of Smokers Helpline control group participants completed 3-month follow-up assessments. |
| Cheung et al (2015)27 | WhatsApp and Facebook | Recent quitters with mobile phones and Internet access were recruited through a smoking cessation clinical setting. 247 participants were screened, and 136 were enrolled in the study. | 3 reminders sent each week by moderators to reinforce program content. | There were more posts in the WhatsApp groups (M =55.0; SD=50.7) compared to the Facebook groups (M =21.0; SD=34.4). Posts about sharing smoking or quitting experiences were most common in the WhatsApp (39%) and Facebook (66%) groups. The WhatsApp group may have been more effective at preventing relapse due to greater interaction among participants. | Participants were compensated approximately US $12.80 (HK $100) if they confirmed abstinence based on exhaled carbon monoxide and saliva sample. Participants were unaware of the incentive prior to follow-up. | At 2-months 37 (88%) WhatsApp, 38 (95%) Facebook, and 43 (80%) control group participants completed follow-up assessments. At 6-months 34 (81%) WhatsApp, 28 (70%) Facebook, and 38 (70%) control group participants completed follow-up assessments. |
| Cobb et al (2016)28
Study protocol: Cobb et al (2014)35 |
Facebook advertising. 10% of eligible individuals were subsampled to complete a brief survey. | Users of the Facebook app receive alerts to check-in, prompts to confirm their quit date, or daily reminders to set a quit date. Game mechanics employed to promote engagement. Users can invite friends to the app. | Participants were more likely to view more content if they received prompts (p<0.001). | Participants were compensated $20 for each completed survey. | Subsample of 857 users surveyed; 407 (48%) completed follow-up surveys. | |
| Haines-Saah et al (2015)26 | Facebook advertising, Twitter page to promote the study, development of a brand identity to market study to youth, and combination of community recruitment efforts including flyers, posters, magnets, print ads in campus newspapers, referrals from participants, craigslist postings, and email lists. 134 inquiries about the study, required 10-months to enroll of 60 participants. 21/134 (16%) inquiries were referrals from friends participating in the study. | Participants received $10 each week for actively posting, commenting, or liking content. Weekly reminders to post content in the group were sent to participants via Facebook and email. | There were over 1,800 actions including photos, comments, likes, and shares. Participants posted a total of 283 photos. | Cumulative payment for engagement was provided to participants at the end of 12-week study period. | 12 (20%) of participants dropped out of the study; 39 (65%) of participants completed follow-up survey. | |
| Pechmann et al (2015)29 | Participants were recruited using Google ads with a direct link to the Tweet2Quit website and study information and application form. Recruitment was completed with a $2000/month budget and required 4 months per group. 813 people completed the online form, 106 completed the screening survey, 45 were eligible, and 40 were enrolled. | Daily automated messages were used to encourage tweeting and discussion related to quitting smoking among participants. The messages encouraged participants to share their experiences (23%), list benefits (19%) or barriers (9%) to quitting, strategies for overcoming barriers to quitting (13%), provide emotional support to others for quitting (9%), set a quit date or use nicotine patches (6%), or express confidence about quitting (5%). Text messages and phone call reminders were used to improve response rates. | Participants posted a total of 2867 Tweets (average of 72 Tweets), and 31 (78%) of participants tweeted at least once. 653 (23%) Tweets were responses to auto messages, while 2214 (77%) Tweets were spontaneous. Daily Facebook use was correlated with greater engagement in the Tweet2Quit intervention. | Participants received a 56-day supply of nicotine patches for enrolling in the study. | Retention was 31 (78%) at 7 days, 31 (78%) at 30 days, and 28 (70%) at 60 days post quit date. | |
| Pechmann et al (2016)30
Secondary outcomes: Lakon et al (2016)32 |
Participants were recruited using Google ads with $10,000/month budget. The ads contained statements such as “Discover New Ways to Quit. Free patches and support through Twitter”. The ads linked to a study website with details about the study. 614 people completed the online form and were screened for eligibility, 444 did not meet inclusion criteria, 10 were excluded because enrolment closed, and 160 were enrolled and randomized. | Automated messages containing discussion topics were sent daily for 100 days. Participants also received individualized automated text messages sent to their phones to promote engagement in the intervention. | 60 (75%) Tweet2Quit participants tweeted. In total there were 4,705 tweets with 58.8 tweets (SD=68.1) per participant. Participants tweeted for an average of 47.4 days (SD=38.9). Greater tweet volume predicted sustained abstinence. Responses to the daily automated messages accounted for 24% of all tweets. | Participants received a 56-day supply of nicotine patches for enrolling in the study. | 65 (81%) Tweet2Quit participants and 70 (88%) control participants completed 60-day follow up. Tweet2Quit participants who tweeted were more likely to complete follow-up (88%; 53/60) compared to non-tweeters (60%; 12/20) (p=0.005). | |
| Ramo et al (2015)31
Secondary outcomes: Ramo et al (2014)33 and Thrul et al (2015)34 |
Facebook ads tailored by age, location and language, contained a link to an online screening survey or study Facebook page. 36 different types of ads including standard, newsfeed, promoted posts, and sponsored stories were delivered over 7 weeks. The ads generated 3,198,373 impressions, 5895 unique clicks. Images of smoking and newsfeed ads viewable on mobile phones were most effective. 586 (10%) people were study eligible and 230 (39%) consented at an average cost of $8.80 per participant. | Participants could be randomized to receive an additional $50 gift card for engaging in the intervention. | 48 (61%) participants commented on at least one Facebook post; 40 (51%) liked at least one post; 28 (35%) participants reported reading most or all of the posts. The 21 (27%) most active participants accounted for 83% of all comments. Participants were more likely to comment on posts if they quit smoking (p=0.036) or received incentives (p=0.015). | Participants received $130 in gift cards for completing all assessments. | Of 230 consented participants, 79 (34.3%) completed baseline assessments. Of these, 65 (82%) completed 6 month assessments and 57 (72%) completed 12 month assessments. |
3.4 Strategies to promote engagement
As illustrated in Table 4, many studies used different strategies to promote participant engagement with the intervention content.26–31 These included use of three weekly reminder messages sent by a program moderator who was a social worker or nurse with smoking cessation counseling experience27, automated alerts and daily prompts sent through Facebook to use the program and to set a quit date28,35, daily automated Tweets to encourage tweeting and discussion related to quitting smoking29, and use of telephone calls or text message reminders.29,30 One study used weekly Facebook and email reminders and paid participants up to $10 each week to actively post, comment, or like content in a closed Facebook group.26 In another study, some participants were randomly assigned to receive a $50 gift card to promote engagement in a Facebook intervention.31 Participants across different studies were more likely to view Facebook content if they received prompts or reminders sent directly through the Facebook platform28, or comment on Facebook posts if they successfully quit smoking or received incentives.31
3.5 Participant retention
Participant retention is listed in Table 4, where rates of participant follow-up ranged from 35% to 84% (median = 70%). Four studies reported using financial incentives to compensate participants for completing follow-up assessments.25,27,28,31 Few studies reported reasons for not completing follow up assessments, though one study found that no baseline characteristics were predictive of participant retention, but that participants who responded to automated Tweets as part of the intervention were more likely to complete follow-up assessments.30
3.6 Methodological quality
As reflected in Table 5, the included studies had moderate to high methodological quality. Across studies, the recruitment strategies were well defined, the sample characteristics were clearly presented, and the flow of participants through the study including retention at follow-up data collection points were described in detail. The quality scores were lowest for the item related to achieving participant follow-up greater than or equal to 75%. Additionally, only two included studies verified smoking cessation using a biochemically verified measure.27,31 This reflects that in studies of social media-based interventions for smoking cessation, most data collection occurred through self-reported online surveys.
Table 5.
Quality assessment of social media for smoking cessation studies
| Quality Criteria |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Author (year) |
Recruitment | Participation Rate |
Detailed description of baseline sample |
Numbers at follow-up reported (e.g., CONSORT diagram included) |
Follow-up duration (min 2- months) |
Response rate at last follow-up ≥75% |
Not selective non- response |
Measure of self- reported smoking outcomes |
Use objective/ biochemical smoking outcomes |
Statistical model is appropriate |
Number of cases 10 times number of independent variables |
Presentation of confidence intervals, standard error or effect size |
Quality Score (%) |
| Bakersville et al (2016)25 | Y | N | Y | Y | Y | N | N | Y | N | Y | Y | Y | 67% |
| Cheung et al (2015)27 | Y | N | Y | Y | Y | N | Y | Y | Y | Y | Y | Y | 83% |
| Cobb et al (2016)28
[Study protocol: Cobb et al (2014)35] |
Y | Y | Y | Y | N | N | Y | N | N | Y | Y | Y | 67% |
| Haines-Saah et al (2015)26 | Y | Y | Y | Y | Y | N | Y | N | N | N | N | N | 50% |
| Pechmann et al (2015)29 | Y | Y | Y | Y | Y | N | Y | Y | N | Y | Y | Y | 83% |
| Pechmann et al (2016)30
[Secondary outcomes: |
Y | Y | Y | Y | Y | Y | Y | Y | N | Y | Y | Y | 92% |
| Lakon et al (2016)32] | |||||||||||||
| Ramo et al (2015)31
[Secondary outcomes: Ramo et al (2014)33 and T hrul et al (2015)34] |
Y | N | Y | Y | Y | Y | Y | Y | Y | Y | Y | Y | 92% |
4. Discussion
We identified 7 studies that evaluated the feasibility, acceptability, or effectiveness of smoking cessation programs delivered on social media platforms including Facebook and Twitter. Social media appears to offer a feasible and acceptable platform for supporting smoking cessation efforts as demonstrated by the ability to recruit and retain smokers online, to deliver targeted smoking cessation interventions, and to collect clinically meaningful smoking-related outcome measures. We also observed that many of the social media interventions showed preliminary effectiveness in terms of increasing motivation or interest in quitting, prompting quitting attempts, and preventing relapse or sustaining abstinence. Despite findings of acceptability and potential effectiveness of social media interventions, future rigorous trials are necessary to establish effectiveness, evaluate the costs and sustainability of these programs, and determine whether these programs can reach low-income individuals, young people, or other vulnerable groups who smoke cigarettes at disproportionately higher rates compared to the general population.
Smoking related outcomes were largely collected through self-report25,29,30 , though two studies also confirmed abstinence biochemically.27,31 Outcome measurement is an important consideration for web-based tobacco cessation research given the need to balance scalability with clinical effectiveness. For example, a Facebook program for smoking cessation may hold promise for reducing tobacco use at a population level, yet it will be necessary to confirm that such an approach is effective through rigorous measurement of objective outcomes prior to widespread dissemination. Future success of social media interventions for smoking cessation will likely be dependent on whether effectiveness studies can first demonstrate biochemically confirmed abstinence. An ongoing study of a Facebook intervention for smoking cessation among young adults will verify abstinence by having participants send photos of themselves using mailed saliva cotinine test kits.36 It will also be necessary to determine whether social media interventions can achieve long-term smoking abstinence. Six studies included in this review collected outcomes after at least 2-months follow-up25–27,29–31, of which only one reported 12-month outcomes.31 It has been suggested that access to social media interventions could be extended over longer periods of time, with occasional posts to check in with participants and to support continued abstinence following the active phase of the program.31
We observed that low participant retention was potentially a concern because only two studies achieved at least 75% retention at follow-up.30,31 Efforts to promote engagement appeared effective and these included use of automated reminders or prompts sent through social media27,28, telephone calls or text message reminders29,30, or financial incentives.26,31 Existing web-based tobacco cessation efforts have similarly faced challenges due to low participant engagement and poor retention.9 However, many of these existing programs have relied extensively on didactic or text-based communication approaches to delivering smoking cessation content modeled after national guidelines.13 Social media platforms can allow users to share their experiences, interact with others, and provide or receive support using a combination of self-generated photos, text, audio, or video content.13 Future studies are necessary to determine how best to leverage social media platforms to achieve better participant engagement compared to previous online programs.34 It is important to note that social media interventions should be considered an approach for augmenting existing in-person smoking cessation programs and for reaching individuals who may be reluctant or unable to access traditional smoking cessation treatment. Additional careful consideration of the risks, harms, and potential limitations associated with social media interventions for smoking cessation is warranted. Lastly, several studies included in this review had small sample sizes or lacked adequate comparison conditions, highlighting that social media for smoking cessation is an emerging research area and that future large scale rigorous controlled studies are necessary for establishing the effectiveness of interventions delivered through these popular platforms.
Despite limitations with the included studies, a key finding from our review is that popular social media such as Facebook and Twitter are viable platforms for supporting smoking cessation. Use of social media for behavioral health interventions is a nascent field of research, and there are many innovative ways that online networks could potentially be leveraged to support tobacco cessation efforts. For example, we found that Facebook could be used to reach and engage smokers interested in quitting as demonstrated by the dissemination of smoking cessation content through an online network.28 From the randomized controlled trial of a Twitter intervention included in this review30, we identified a report on secondary findings from this study illustrating characteristics of the network ties between participants enrolled in the intervention.32 This secondary analysis demonstrated that abstainers and nonabstainers interacted with each other, suggesting that participants who are successful at quitting smoking as well as those who are not successful both engage in the social media program and content.32 Therefore, it may be possible to support participants who face challenges quitting smoking through their extended network connections with participants who successfully quit. There are also ways to use social media to facilitate peer recruitment as demonstrated in a recent study where smokers referred friends to participate in a cessation program.37 As prior research has documented the spread of smoking-related behaviors between members within a social network38, future research could examine ways of leveraging these network ties using social media platforms to substantially extend the reach of smoking cessation efforts.
For smoking cessation interventions using social media to achieve long-term sustainability, it will be necessary to identify the underlying behavioral mechanisms that contribute to the success of these interventions and improvement in smoking-related outcomes over time. Given that social media platforms will continue to change rapidly in the years ahead, it is important to further our understanding of how interpersonal connections within online networks contribute to the adoption, modification, and spread of health behaviors39, and how best to mobilize these online relationships to support smoking cessation. If not, we risk developing and evaluating interventions that are suitable only for the social media platforms of today, such as Facebook or Twitter, without considering how these platforms will evolve over time or how emerging social media platforms may be used to target tobacco use among younger generations (e.g., Snapchat). Understanding mechanisms of behavior change could help inform strategies that could be used across different social media platforms.
The success of social media interventions may be driven by several different behavioral mechanisms. For example, social media could provide a platform for social modeling, where participants develop personal skills and obtain new knowledge by learning about the successes and challenges of quitting smoking from other participants.40 There may be opportunities to leverage features of social media platforms to increase self-efficacy for quitting by helping participants manage tempting situations41, or to facilitate verbal or social persuasion by sending personalized encouragement or prompts to help individuals feel confident so that they can quit smoking.40 Social media may also yield new ways to foster social support for health behavior change through motivation, encouragement, and learning from peers who share similar experiences or health goals.42 Research suggests that engaging existing friends in online networks may be an important strategy for achieving better behavioral health outcomes.43 Therefore, careful and frequent assessment of the mechanisms responsible for influencing health behaviors is necessary to better understand how specific components of social media interventions may contribute to successfully quitting smoking and preventing relapse.41
Social media interventions also afford unique opportunities to overcome barriers such as cost, geographic distance, and stigma that could impede attempts to quit smoking. Most popular social media platforms are free to use, can be accessed from nearly any location through mobile devices, and allow users to choose a certain degree of privacy and anonymity. We found that several studies used closed Facebook groups, where group membership is concealed from individuals’ other friends on Facebook. For many other social media platforms, users can create accounts using pseudonyms to conceal their identity. These are important considerations for smokers who may feel embarrassed or ashamed about being a smoker or who may also have other stigmatizing health conditions. Given the widespread use of social media, even among population groups at disproportionately elevated risk for tobacco use4,21,44,45, there may be opportunities to leverage these popular online platforms to support smoking cessation among those at greatest risk. However, in this review, we did not identify any studies of social media for smoking cessation among vulnerable population groups such as people with mental illness or other disabilities, though we believe that this is an important area for future investigation.
4.1 Limitations
There are limitations with our review that warrant consideration. First, the included studies employed varying designs, analytic techniques, and outcome measures (smoking-related outcome measures were heterogeneous across most of the studies in which they were reported); therefore, we were unable to conduct a meta-analysis to assess estimates of effect for the different interventions. Second, our search strategy did not include the names of the numerous popular social media platforms; therefore, it is possible that studies using popular social media platforms without specifically describing it as social media may have been missed in our search strategy. Third, we did not search the grey literature, which refers to unpublished work or studies that are not formally published in books or journals20, and it is possible that there are social media smoking cessation programs that have not undergone formal evaluation and publication in peer-reviewed journals. All of the studies included in our review were published since 2014, highlighting that there likely will be increasing interest in using social media for smoking cessation in the coming years. Our review provides an initial overview of this rapidly advancing field, and offers important insight for guiding future research.
5. Conclusion
Globally there are over 2 billion social media users46, and in the United States about two thirds of adults use social media4, highlighting opportunities for social media smoking cessation efforts to achieve wide reach. However, efforts are necessary to overcome substantial methodological and practical challenges related to participant engagement and retention, measuring and sustaining clinically meaningful outcomes, and identifying underlying behavioral mechanisms that could inform the scalability of smoking cessation efforts across diverse social media platforms. Consideration of the costs and cost-effectiveness of social media interventions is equally important to ensure that efficient payment models can be implemented to support the delivery and sustainability of social media interventions targeting tobacco use. It will also be critical for behavioral health and tobacco researchers to collaborate across disciplines including computer science, engineering, data science, marketing, and communication, and to consider the perspectives and preferences of patients and families who actively use social media. This is an important time for tobacco cessation research, because social media platforms allow access to a highly dynamic, scalable, and popular online network with the potential to reach individuals who have previously not been possible to engage in behavior health interventions.
Highlights.
Social media interventions for smoking cessation emerged as feasible and acceptable.
Several social media interventions contributed to improved smoking-related outcomes.
Engagement in social media programs may predict improved smoking-related outcomes.
Social media holds potential to support population wide smoking cessation efforts.
Acknowledgments
Role of Funding Sources This study was supported by the National Institute on Drug Abuse (P30 DA029926). Additional support was received from the Health Promotion Research Center at Dartmouth supported by funding from the United States Centers for Disease Control and Prevention (Cooperative Agreement Number U48 DP005018). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Contributors JAN designed the study and wrote the search strategy and protocol. SJK reviewed the search strategy and study protocol. JAN completed the literature search. JAN and LJM screened records for relevant articles for inclusion and compiled the final list of included studies. SJK and KAA reviewed the list of included studies to confirm eligibility. JAN and LJM extracted the data and assessed the methodological quality of the included studies. JAN wrote the first draft of the manuscript. SJK, KAA, MFB, and JD assisted with the interpretation of the findings and contributed to multiple revisions of the manuscript. LJM, SJB, and LAA contributed to subsequent revisions to the manuscript. All authors reviewed the final list of included studies, and contributed to and approved the final manuscript.
Conflict of Interest The authors report no conflicting interests.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.US Department of Health and Human Services. 2014 Surgeon General's Report: The Health Consequences of Smoking—50 Years of Progress. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2014. [Google Scholar]
- 2.Jamal A, Homa DM, O’Connor E, et al. Current cigarette smoking among adults—United States, 2005–2014. MMWR Morb Mortal Wkly Rep. 2015;64(44):1233–1240. doi: 10.15585/mmwr.mm6444a2. [DOI] [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration. Results from the 2013 National Survey on Drug Use and Health: Summary of National Findings. Rockville, MD: U.S. Department of Health and Human Services Substance Abuse and Mental Health Services Administration Center for Behavioral Health Statistics and Quality; 2014. [Google Scholar]
- 4.Perrin A. [Accessed October 15, 2016];Social media usage: 2005–2015. 2015 http://www.pewinternet.org/files/2015/10/PI_2015-10-08_Social-Networking-Usage-2005-2015_FINAL.pdf.
- 5.Duggan M, Ellison NB, Lampe C, Lenhart A, Madden M. [Accessed October 15, 2016];Social media update 2014. 2015 http://www.pewinternet.org/files/2015/01/PI_SocialMediaUpdate20144.pdf.
- 6.Capurro D, Cole K, Echavarría MI, Joe J, Neogi T, Turner AM. The use of social networking sites for public health practice and research: a systematic review. Journal of medical Internet research. 2014;16(3):e79. doi: 10.2196/jmir.2679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rice E, Tulbert E, Cederbaum J, Adhikari AB, Milburn NG. Mobilizing homeless youth for HIV prevention: a social network analysis of the acceptability of a face-to-face and online social networking intervention. Health education research. 2012;27(2):226–236. doi: 10.1093/her/cyr113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pedersen ER, Helmuth ED, Marshall GN, Schell TL, PunKay M, Kurz J. Using facebook to recruit young adult veterans: online mental health research. JMIR research protocols. 2015;4(2):e63. doi: 10.2196/resprot.3996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shahab L, McEwen A. Online support for smoking cessation: a systematic review of the literature. Addiction. 2009;104(11):1792–1804. doi: 10.1111/j.1360-0443.2009.02710.x. [DOI] [PubMed] [Google Scholar]
- 10.Civljak M, Stead LF, Hartmann-Boyce J, Sheikh A, Car J. Internet-based interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2013;(7) doi: 10.1002/14651858.CD007078.pub4. Article Number: CD007078. [DOI] [PubMed] [Google Scholar]
- 11.Swartz L, Noell J, Schroeder S, Ary D. A randomised control study of a fully automated internet based smoking cessation programme. Tobacco control. 2006;15(1):7–12. doi: 10.1136/tc.2003.006189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Park E, Drake E. Systematic review: Internet-based program for youth smoking prevention and cessation. Journal of Nursing Scholarship. 2015;47(1):43–50. doi: 10.1111/jnu.12104. [DOI] [PubMed] [Google Scholar]
- 13.Jacobs MA, Cha S, Villanti AC, Graham AL. Using Tumblr to Reach and Engage Young Adult Smokers: A Proof of Concept in Context. American journal of health behavior. 2016;40(1):48–54. doi: 10.5993/AJHB.40.1.6. [DOI] [PubMed] [Google Scholar]
- 14.Depue JB, Southwell BG, Betzner AE, Walsh BM. Encoded exposure to tobacco use in social media predicts subsequent smoking behavior. American Journal of Health Promotion. 2015;29(4):259–261. doi: 10.4278/ajhp.130214-ARB-69. [DOI] [PubMed] [Google Scholar]
- 15.Huang GC, Unger JB, Soto D, et al. Peer influences: the impact of online and offline friendship networks on adolescent smoking and alcohol use. Journal of Adolescent Health. 2014;54(5):508–514. doi: 10.1016/j.jadohealth.2013.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang M, Yang CC. The effectiveness of smoking cessation intervention on facebook: a preliminary study of posts and users. International Conference on Smart Health; 2013; pp. 7–17. [Google Scholar]
- 17.Struik LL, Baskerville NB. The role of Facebook in Crush the Crave, a mobile-and social media-based smoking cessation intervention: qualitative framework analysis of posts. Journal of medical Internet research. 2014;16(7):e170. doi: 10.2196/jmir.3189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Murnane EL, Counts S. Unraveling abstinence and relapse: smoking cessation reflected in social media. Paper presented at: Proceedings of the 32nd annual ACM conference on Human factors in computing systems; 2014; Toronto, Canada. [Google Scholar]
- 19.Duke JC, Hansen H, Kim AE, Curry L, Allen J. The use of social media by state tobacco control programs to promote smoking cessation: a cross-sectional study. Journal of medical Internet research. 2014;16(7):e169. doi: 10.2196/jmir.3430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Higgins JP, Green S. Cochrane handbook for systematic reviews of interventions. Vol. 5. Wiley Online Library; 2008. [Google Scholar]
- 21.Naslund JA, Aschbrenner KA, Marsch LA, Bartels SJ. The future of mental health care: peer-to-peer support and social media. Epidemiology and Psychiatric Sciences. 2016;25(2):113–122. doi: 10.1017/S2045796015001067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Te Velde S, Van Nassau F, Uijtdewilligen L, et al. Energy balance-related behaviours associated with overweight and obesity in preschool children: a systematic review of prospective studies. obesity reviews. 2012;13(s1):56–74. doi: 10.1111/j.1467-789X.2011.00960.x. [DOI] [PubMed] [Google Scholar]
- 23.Naslund JA, Aschbrenner KA, Marsch LA, McHugo GJ, Bartels SJ. Crowdsourcing for conducting randomized trials of Internet delivered interventions in people with serious mental illness: a systematic review. Contemporary Clinical Trials. 2015;44:77–88. doi: 10.1016/j.cct.2015.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Namkoong K, Nah S, Record RA, Van Stee SK. Communication, Reasoning, and Planned Behaviors: Unveiling the Effect of Interactive Communication in an Anti-Smoking Social Media Campaign. Health communication. 2017;32(1):41–50. doi: 10.1080/10410236.2015.1099501. [DOI] [PubMed] [Google Scholar]
- 25.Baskerville NB, Azagba S, Norman C, McKeown K, Brown KS. Effect of a Digital Social Media Campaign on Young Adult Smoking Cessation. Nicotine & Tobacco Research. 2016;18(3):351–360. doi: 10.1093/ntr/ntv119. [DOI] [PubMed] [Google Scholar]
- 26.Haines-Saah RJ, Kelly MT, Oliffe JL, Bottorff JL. Picture Me Smokefree: a qualitative study using social media and digital photography to engage young adults in tobacco reduction and cessation. Journal of medical Internet research. 2015;17(1):e27. doi: 10.2196/jmir.4061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheung YTD, Chan CHH, Lai CKJ, et al. Using WhatsApp and Facebook Online Social Groups for Smoking Relapse Prevention for Recent Quitters: A Pilot Pragmatic Cluster Randomized Controlled Trial. Journal of Medical Internet Research. 2015;17(10):e238. doi: 10.2196/jmir.4829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cobb NK, Jacobs MA, Wileyto P, Vale T, Graham AL. Diffusion of an Evidence-Based Smoking Cessation Intervention Through Facebook: A Randomized Controlled Trial. American Journal of Public Health. 2016;106(6):1130–1135. doi: 10.2105/AJPH.2016.303106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pechmann C, Pan L, Delucchi K, Lakon CM, Prochaska JJ. Development of a Twitter-based intervention for smoking cessation that encourages high-quality social media interactions via automessages. Journal of medical Internet research. 2015;17(2):e50. doi: 10.2196/jmir.3772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pechmann C, Delucchi K, Lakon CM, Prochaska JJ. Randomised controlled trial evaluation of Tweet2Quit: a social network quit-smoking intervention. Tobacco control. 2016:1–7. doi: 10.1136/tobaccocontrol-2015-052768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ramo DE, Thrul J, Chavez K, Delucchi KL, Prochaska JJ. Feasibility and Quit Rates of the Tobacco Status Project: A Facebook Smoking Cessation Intervention for Young Adults. Journal of medical Internet research. 2015;17(12):e291. doi: 10.2196/jmir.5209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lakon CM, Pechmann C, Wang C, Pan L, Delucchi K, Prochaska JJ. Mapping Engagement in Twitter-Based Support Networks for Adult Smoking Cessation. American Journal of Public Health. 2016;106(8):1374–1380. doi: 10.2105/AJPH.2016.303256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramo DE, Rodriguez TM, Chavez K, Sommer MJ, Prochaska JJ. Facebook Recruitment of Young Adult Smokers for a Cessation Trial: Methods, Metrics, and Lessons Learned. Internet Interventions. 2014;1(2):58–64. doi: 10.1016/j.invent.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Thrul J, Klein AB, Ramo DE. Smoking Cessation Intervention on Facebook: Which Content Generates the Best Engagement? Journal of medical Internet research. 2015;17(11):e244. doi: 10.2196/jmir.4575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cobb NK, Jacobs MA, Saul J, Wileyto EP, Graham AL. Diffusion of an evidence-based smoking cessation intervention through Facebook: a randomised controlled trial study protocol. BMJ open. 2014;4(1):e004089. doi: 10.1136/bmjopen-2013-004089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ramo DE, Thrul J, Delucchi KL, Ling PM, Hall SM, Prochaska JJ. The Tobacco Status Project (TSP): Study protocol for a randomized controlled trial of a Facebook smoking cessation intervention for young adults. BMC Public Health. 2015;15:897. doi: 10.1186/s12889-015-2217-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sadasivam RS, Cutrona SL, Luger TM, et al. Share2Quit: Online Social Network Peer Marketing of Tobacco Cessation Systems. Nicotine & Tobacco Research. 2016:1–10. doi: 10.1093/ntr/ntw187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. New England journal of medicine. 2008;358(21):2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Centola D. The spread of behavior in an online social network experiment. Science. 2010;329(5996):1194–1197. doi: 10.1126/science.1185231. [DOI] [PubMed] [Google Scholar]
- 40.McAlister AL, Perry CL, Parcel GS. How individuals, environments, and health behaviors interact: social cognitive theory. In: Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. 4. San Francisco, CA: Jossey–Bass, John Wiley & Sons, Inc; 2008. pp. 169–188. [Google Scholar]
- 41.Dallery J, Jarvis B, Marsch L, Xie H. Mechanisms of change associated with technology-based interventions for substance use. Drug and alcohol dependence. 2015;150:14–23. doi: 10.1016/j.drugalcdep.2015.02.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moorhead SA, Hazlett DE, Harrison L, Carroll JK, Irwin A, Hoving C. A New Dimension of Health Care: Systematic Review of the Uses, Benefits, and Limitations of Social Media for Health Communication. Journal of medical Internet research. 2013;15(4):e85. doi: 10.2196/jmir.1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cavallo DN, Tate DF, Ward DS, DeVellis RF, Thayer LM, Ammerman AS. Social support for physical activity—role of Facebook with and without structured intervention. Behav Med Pract Policy Res. 2014;4:346–354. doi: 10.1007/s13142-014-0269-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Naslund JA, Aschbrenner KA, Bartels SJ. How people living with serious mental illness use smartphones, mobile apps, and social media. Psychiatric rehabilitation journal. 2016;39(4):364–367. doi: 10.1037/prj0000207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Onken LS, Carroll KM, Shoham V, Cuthbert BN, Riddle M. Reenvisioning clinical science unifying the discipline to improve the public health. Clinical Psychological Science. 2014;2(1):22–34. doi: 10.1177/2167702613497932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kemp S. [Accessed October 18, 2016];Digital, social and mobile worldwide in 2015. 2015 http://wearesocial.com/uk/special-reports/digital-social-mobile-worldwide-2015.