Abstract
Background:
Research using video recordings can advance understanding of healthcare communication and improve care, but making and using video recordings carries risks.
Aim:
To explore views of hospice patients, carers and clinical staff about whether videoing patient–doctor consultations is acceptable for research and training purposes.
Design:
We used semi-structured group and individual interviews to gather hospice patients, carers and clinical staff views. We used Braun and Clark’s thematic analysis.
Setting/participants:
Interviews were conducted at one English hospice to inform the development of a larger video-based study. We invited patients with capacity to consent and whom the care team judged were neither acutely unwell nor severely distressed (11), carers of current or past patients (5), palliative medicine doctors (7), senior nurses (4) and communication skills educators (5).
Results:
Participants viewed video-based research on communication as valuable because of its potential to improve communication, care and staff training. Video-based research raised concerns including its potential to affect the nature and content of the consultation and threats to confidentiality; however, these were not seen as sufficient grounds for rejecting video-based research. Video-based research was seen as acceptable and useful providing that measures are taken to reduce possible risks across the recruitment, recording and dissemination phases of the research process.
Conclusion:
Video-based research is an acceptable and worthwhile way of investigating communication in palliative medicine. Situated judgements should be made about when it is appropriate to involve individual patients and carers in video-based research on the basis of their level of vulnerability and ability to freely consent.
Keywords: Communication, method acceptability, palliative medicine, stakeholder consultation, video recording
What is already known about the topic?
Research and training using video recordings of actual practice can advance understandings of healthcare communication and improve care, but making and using video recordings raises concerns about threats to confidentiality and the risk of negatively affecting patient care.
There is a concern that when patients are particularly vulnerable – including in palliative and end-of-life (EoL) care – dangers might be greater.
A previous study in a hospice context found that patients support videoing of their consultation with a doctor in order to support that doctor in their own personal development.
What this paper adds?
Hospice patients, carers and clinical staff view video-based research on communication in palliative care as valuable because of its potential to improve communication, care and staff training.
Hospice patients, carers and clinical staff express some concerns about video-based research including its potential to affect people’s communication and threats to confidentiality; however, they do not see these as sufficient grounds for rejecting video-based research.
They see video-based research as acceptable and useful providing that measures are taken to minimise its possible risks across the recruitment, recording and dissemination phases of the research process.
Implications for practice, theory or policy.
Video recording can be used in research to improve understanding and practice of palliative care.
Involvement of people – particularly patients and carers – in video-based research is possible on condition that clear safeguards and operating procedures are adopted, including case-by-case judgements about whether individual patients and carers can be involved in research.
Background
Communication is a core part of good palliative and end-of-life (EoL) care.1–6 Previous studies explored healthcare professionals’ (HCPs), patients’ and carers’ views on communication retrospectively through interviews.7–17 Although these studies provided valuable insights on what can count as good EoL communication, they did not examine how such communication can be realised. Video-based research allows one to directly observe and examine how HCPs and patients communicate;18–22 findings from this kind of research can be used to improve healthcare communication.23,24 However, it raises several concerns about threats to confidentiality and the risk of negatively affecting HCP–patient communication, for instance by putting undue pressure on professionals or by inhibiting patients from voicing their concerns.25–35 These risks can be greater in settings where patients’ vulnerability is heightened, as in palliative and EoL care.36–38 Therefore, we need to ask whether it is acceptable to video-record interactions in palliative and EoL care settings.
There is one previous study that sheds some light on whether recording is acceptable. In that study, Hargreaves and Peppiatt39 surveyed 31 day hospice patients who had already had one of their conversations with a doctor video recorded. The majority (27/31) viewed the purpose of the recording (doctors wishing to improve their communication skills) as positive and regarded video recording as a good way of doing so; 30/31 said they would agree to another recording in future. Two of 31 of the patients reported that the camera had affected the consultations; 7/31 that they were unable to forget about the camera; but none felt that video recording had made the consultation less confidential, and none reported that it had made them feel nervous or less willing to talk. That study made some inroads into exploring views about the acceptability of video recording, but the purpose of the video recording was limited to improving doctors’ consultation skills – acceptability of video recording for research was not investigated. Additionally, only patients took part, leaving out other stakeholders. The questionnaire design meant relatively shallow exploration of perceived benefits and risks of video recording, whether anticipated benefits outweigh perceived costs and what safeguards might increase recording’s acceptability and safety. Our study addressed these questions in depth by examining stakeholders’ views on the acceptability of video recording patient and carer conversations with palliative medicine doctors for research and teaching purposes.
Methods
Design
We interviewed key stakeholders at one hospice. We used qualitative, semi-structured group and individual interviews40 to explore their views on the use of video-based research in the palliative care setting and to inform the design of a study where we recorded consultations at the same hospice for purposes of research and teaching about healthcare communication.41
NRES Committee Yorkshire & The Humber (UK) ethically approved the interview study on 29 April 2013 (reference: 13/YH/0127).
Setting
We interviewed stakeholders in 2013 at the same hospice where we planned to conduct the video-based study. The hospice provided outpatient, day therapy and inpatient services, as well as a substantial educational programme for health and social care staff in the surrounding region. Our decision to limit the enquiry to one hospice was dictated by the nature of the study as a stakeholder consultation preliminary to a subsequent broader study in the same setting.
Recruitment and study sample
We interviewed hospice patients, carers with experience of accompanying patients to healthcare consultations, hospice doctors, senior hospice nurses and communication skills training educators. This was a sample of convenience, formed by stakeholders who were available at the hospice. Our sampling strategy was also purposeful; we involved representatives of all the groups that would later be affected by the video study (we would be recording consultations involving patients, carers and doctors; nurses would help with patient recruitment; educators would use the video recordings thereby generated in communication training).42 We sought to involve people with diverse characteristics (diagnoses for patients, types of relationship to patients for carers).
Members of the care team made a first face-to-face approach to patients who had capacity to consent and whom the team judged were neither acutely unwell nor severely distressed. Carers of current or past patients were also approached by the care team; several were members of the hospice’s carer and patient user group. The care team gave prospective participants an information sheet; R.P. approached them at least 24 h later to invite them to be interviewed. R.P. invited all educators at the hospice, and all doctors who had qualified as or were training to be palliative medicine specialists (i.e. those at UK consultant and speciality registrar levels). Totally, 11 patients, 5 carers, 4 senior nurses, 7 doctors and 5 educators took part (Table 1). The overall number of participants was dictated by time and financial constraints as well as participants’ availability. We excluded one patient interview from the analysis because the patient had severe dysarthria and their talk was not sufficiently intelligible for transcription. R.P. obtained written informed consent from the participants.
Table 1.
Participants and data.
| Stakeholder group | Number of participants and gender | Data collected | Duration (h) | Additional information |
|---|---|---|---|---|
| Patients | 10 (7 F, 3 M) | 10 individual interviews | 2.57 | Diagnoses: Motor neurone disease (3), breast cancer + MS (1), cancer of the tongue (1), myotonic dystrophy (1), heart failure + ischaemic heart disease (1), multi system atrophy (1), gastric and ovarian cancers (1), COPD + bronchiectasis + heart failure + osteoporosis (1) |
| Carers | 5 (4 F, 1 M) | 1 group interview (2 participants) 3 individual interviews |
2.55 | Relationship to patient: wife (2), daughter (2), father (1) |
| Doctors | 7 (6 F, 1 M) | 2 group interviews (one of 5 participants, one of 2 participants) | 1.54 | Role: consultant (5), specialist registrar (2) |
| Senior nurses | 4 (4 F) | 2 group interviews (2 participants each) | 1.41 | – |
| Communication skills educators | 5 (5 F) | 1 group interview (4 participants) 1 individual interview |
2.24 | – |
M: male; F: female; MS: multiple sclerosis; COPD: chronic obstructive pulmonary disease.
Data collection
We used small group interviews to promote discussion among participants, and so more comprehensively elicit their views.43 We did two group interviews for doctors, two for nurses, one for educators and one for carers. Individual interviews were more suitable for the patients’ health circumstances and were also conducted for participants unavailable on group interview dates (Table 1).
R.P. designed topic guides in consultation with a project advisory group (see Acknowledgements) and experienced clinicians and communication skills trainers at the hospice, some of whom also took part in the interviews. These multiple involvements were motivated by the collaborative nature of the stakeholder consultation, which was aimed at paving the way for a subsequent video-based study at the hospice. R.P. conducted the interviews. Table 2 contains information on how R.P. introduced herself and the research to the participants, and the topic guides. The breadth of views elicited through these guides was partly limited by the nature of the study, which also served as a stakeholder consultation to support the design of our subsequent video-based study. For instance, while we invited doctors to imagine being asked to take part in a video-based study, we did not do this with participating nurses because we were not planning to record patient–nurse interactions.
Table 2.
Summary of topic guides used for the individual and group interviews.
| Introduction |
|---|
| R.P. conducted the interviews. At that time, she held a PhD in Social Sciences and was employed as a Senior Research Fellow at the University of Nottingham. At the start of the interviews, R.P. told the participants about her background in physiotherapy, her experience in conducting video research in healthcare settings and her interest in conducting video research in the future at the same hospice. The purpose of the research, as explained to participants, was to assess their views about the possibility of conducting a subsequent video-based study at the same hospice where the interviews were taking place. In that subsequent study we recorded conversations between hospice doctors, patients and carers (when present). R.P. further told them the purpose of the interviews was to gather views about whether or not collecting video data at the hospice would be acceptable, and why or why not; she also described measures, gleaned from the literature, that could be adopted to make video recording safer and asked the interviewees’ views on those and any other safeguards they deemed important. |
| Interview guide |
| • Patients and companions were asked to imagine that they had been asked to consider allowing a video recording to be made of their next conversation with their hospice doctor, for research on how doctors communicate. • Senior doctors, who were also potential participants in the subsequent study, were similarly asked to imagine they had been asked to consider allowing video recordings to be made of their next conversations with some of their patients. • Senior nurses and educators were asked about the overall acceptability of the proposal to video-record doctor patient consultations at the hospice (because the subsequent study did not aim to record nurses and educators). |
| Subsequent topics |
| • As worded for patients and companions. The same topics, but with amended wording, were covered with other interviewees. |
| If they said video recording would be unacceptable for them, they were asked: • To elaborate on their reasons. • About whether they thought it would ever be acceptable, even though they would not participate personally. |
| If they said recording would be acceptable, they were asked about: • What they (and their companions) would want to know about the study. • How long they would need in order to decide whether to participate. • The acceptability of prospective verbal assent with written consent sought after recording. • Whether or not the camera operator should be present within the room. • Their views on having a remote control available in the room allowing recording to be stopped at any time. • How long after recording consent should be discussed. • Whether participants should be given an opportunity to see the recording or receive a copy. • Whether or not it would be acceptable for people beyond the small research team to view recordings – specifically: other experts viewing them with the aim of strengthening the analysis; other researchers attending presentations of findings; and closed groups of health and social care staff or trainees attending communication skills training. The fact that some participants in the recordings would have died by the time clips were used in such training was explicitly addressed unless the interviewer judged raising this would be distressing for the interviewee. • Measures that could be adopted to make video recording safer. |
| Towards the end of interviews, participants were invited to add other thoughts and comments. Throughout, the interviewer attempted to facilitate the raising of relevant matters not specifically covered by the guide. |
R.P. had a prior association with two interviewees, both doctors; R.P. had consulted them about conducting research at the hospice and had also observed their work as a formal visitor to the hospice. Four of the consultants she interviewed also took part in the subsequent video-based study. The interviews took place in quiet rooms at the hospice and were audio recorded. R.P. took brief field notes during the interviews and expanded these afterwards.
Data analysis
M.P. transcribed the interviews verbatim and analysed the data using thematic analysis as described by Braun and Clarke; we broadly adopted thematic analysis as a ‘realist’ method, treating what people said as reflecting their views and perspectives.44 Nevertheless, we also endeavoured to take into account the way in which the interviewer’s questions shaped interviewee responses.45,46 We did not use specialist software; instead, we designed customised forms and tables with word-processing software. M.P. and R.P. met regularly to discuss and refine emerging analyses; differences of interpretation were discussed and resolved. We derived themes from the data inductively. We shared emerging findings with two carers, two doctors and two educators, all of whom were also study participants, seeking and building in their comments. We deemed that these stakeholders’ insider knowledge would help our understanding of the meanings conveyed in the interviews, which contained several references to processes and dynamics specific to the hospice setting. We did not consult patients in this way because they all had such rapidly deteriorating conditions.
Results
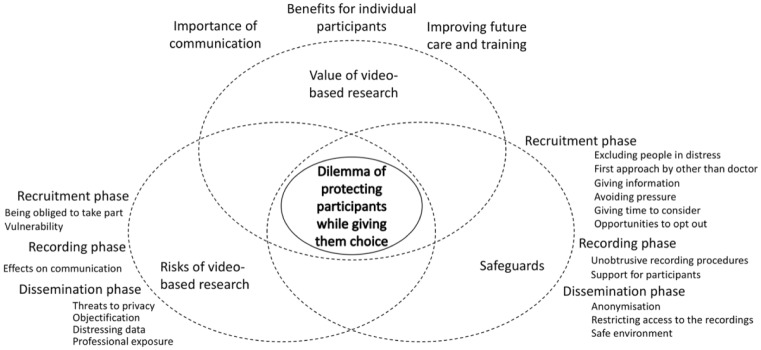
We grouped our analyses into three themes: participants’ views about the value of video-based research, their concerns about its risks and their views on ways of mitigating those risks (Figure 1). The overarching theme is the central dilemma of protecting participants (particularly patients) from the risks associated with video-based research while giving them the opportunity to make their own decisions about involvement in research.
Figure 1.
Themes.
The value of video-based research
On being presented with the hypothetical scenario of their next medical consultation being recorded, 9 of the 10 patients said they would consent to this and to the recording being used in training. One of these nine said he would only agree to audio recording because of how the illness had changed his appearance. The one patient who said she would not consent said this was because of both her changed appearance and the fact that she found herself getting emotional and tearful during consultations and would not want this to be recorded: ‘I am so close to the edge all the while and I wouldn’t want anybody seeing that’ (Interviewee 3). She nevertheless supported the idea of doing the research and thought that others would have different reactions to the idea of being recorded.
Participants in all stakeholder groups commented that communication was a crucial aspect of good care, thought there was scope and need for improving knowledge and training and viewed video-based research as a good vehicle for doing so. Participants in different groups approached this theme from different angles. The educators reported the need for more resources for training. Several patients mentioned contributing to others as a reason for participating in video-based research. One patient said, ‘I want to know that by doing this [research, it] is gonna help someone at the end of the day’ (Interviewee 9). Another patient compared the authorisation to use her voice and image to organ donation: ‘This is the same when you ask if somebody died whether you donate your organs. You’re dead. So why not? If you’re going [it’s] going to help somebody else’ (Interviewee 6). Carers suggested that participating in research could in itself be beneficial to those who take part; for instance, a carer expressed that involvement in research can be one of the ways to make sense of a person’s dying: ‘something good has got to come out of something so bad’ (Interviewee 13).
What concerns does video-based research raise?
Interviewees expressed concerns about possible risks associated with the recruitment, recording and dissemination phases of video-based research.
Recruitment phase
Several participants referred to power imbalances between patients and staff, leading to a risk that patients and carers could feel obliged to take part. According to a carer, ‘they [patients] will probably say yes to a doctor. My mother-in-law would have said yes to any doctor’ (Interviewee 13). Some participants mentioned circumstances where patients’ and carers’ vulnerability would be heightened and informed consent could be at risk: ‘They will come in to that appointment, particularly if it’s a crisis, I could not retain anything’ (Interviewee 21 – carer); ‘You wouldn’t do that [seek written consent] immediately after the consultation […] because there may be a lot of distress’ (Interviewee 20 – senior nurse). These considerations led to discussions about whether and when participants should be approached and given a choice to take part. There was consensus that some individuals would be so vulnerable that they should not even be approached, for example, people who were obviously very distressed:
If such a person had reached the door of [the hospice] it would perhaps not be appropriate to ask and that would just be another raft of questions and dilemmas to offer them [when] they were already dealing with a lot of stuff. (Interviewee 14 – carer)
At the same time, several participants emphasised that there should be equity of opportunities for patients to be involved and furthermore that they should be regarded as capable of making their own decisions. One senior nurse commented, ‘I don’t think you should discriminate amongst age or disfigurement […] you shouldn’t rule out people’ (Interviewee 20). At the other end of the spectrum, one educator said that sometimes it is not in a patient’s best interest to be invited to take part and that professionals should make those decisions on their behalf: ‘I think they say they want that but […] they don’t always know what will be helpful [for them]’ (Interviewee 18). Notably, none of the patients expressed concerns about feeling pressured in the recruitment stage; however, three mentioned that they would need time to consider whether to take part in the research.
Summarising the above, there was some divergence in the perspectives voiced within different stakeholder sub-groups; some carers and HCPs voiced concerns relating to patients’ recruitment whereas patients did not express such concerns. This discrepancy connects to the overarching theme of this study (centre of Figure 1): the dilemma of protecting participants (particularly patients) from the risks associated with video-based research while giving them the opportunity to make their own decisions about involvement in research. While it is important to let patients make up their own mind about participation, HCPs and researchers have a duty to protect patients in circumstances where the initial approach to take part in research could be in itself a source of unjustifiable distress, or when there are reasons to believe that patients’ conditions could hamper their ability to provide informed consent.
Recording phase
Within each stakeholder group, there was disquiet that recording might affect communication within the consultation, particularly by inhibiting patients and carers from disclosing concerns and expressing distress. According to one carer, ‘I think my only concern would be people sort of clamming up and not actually wanting to open up and then give all the information or share exactly how they are feeling, if they are on the camera’ (Interviewee 10). According to one of the doctors,
it does change the dynamic because […] you may forget if you get involved in the conversation but certainly initially you’ll be very aware of it. And I guess some patients themselves may be aware of it and […] that may therefore make them a bit more self-conscious or less able to open up or share sort of deepest feelings, some concerns. (Interviewee 16)
These views resonate with the responses of the patient, mentioned above, who had said she would not want to be recorded (Interviewee 3). She described conversations with her doctor as moments of heightened vulnerability which she would not want caught on camera (see above). Other patients expressed less concern about the impact of recording on within-consultation communication than did other participants. Indeed, 6 of the 10 patients said they anticipated that recording would have no effect on their communication with their doctor; another two expressed the same view while acknowledging that other patients might be affected.
Broadly, the level of concern about recording consultations varied, and no one opposed the overall idea of the research on these grounds. Rather, it was recommended that the risk of influencing in-consultation communication should be minimised through safeguards.
Dissemination phase
There were few direct comments about concerns relating to using participants’ images in the dissemination phase. One patient raised issues of anonymity and privacy: ‘I don’t want this to come back to me’ and ‘I don’t want it put on BBC’ (Interviewee 5). An educator alluded to the risk of objectification: ‘obviously you are using patients in this instance as means, not ends in themselves. So it will be of no benefit to the individual patient’ (Interviewee 18). A carer expressed some disquiet at the idea of seeing the recording after the patient’s death: ‘I’d think I’d find it bit weird down the line, but if I wasn’t to see it, and it was just medical students [that would be okay]’ (Interviewee 10). Some interviewees suggested the recordings might be distressing for some audiences if used in communication training. As previously noted, all nine patients who said they would agree to recording also said they would consent to use of the recording in training.
The vulnerability of professional participants was raised in doctors’ interviews: ‘I suppose partly I’m slightly worried with this project that actually what would come out [is that I am] not an expert on communication but that actually I’m doing it all wrong’ (Interviewee 16 – doctor). This linked to the idea of having one’s performance exposed and subjected to scrutiny: ‘It’s much more exposing to us than it is to the patient I think’ (Interviewee 17 – doctor). A carer, who had previously worked as a social care professional, said, ‘Perhaps if I was the professional person being asked to sit in on a video I might be anxious about how I would turn out’ (Interviewee 14).
What safeguards should be used?
For the recruitment phase, proposed safeguards included measures to ensure that patients and carers who were evidently in great distress would not be approached. For these individuals, informed consent and recording procedures would impose an unjustifiable additional burden. Interviewees emphasised that people approached to participate would need to be fully informed about the purpose of the study and that any kind of pressure should be avoided. Explaining the research to potential participants and giving them time to reflect was seen as important:
I think it’s about being able to explain to patients and carers in fairly succinct terms what our aims are. And for them to be able to reflect on that. Not make a quick decision because actually it’s quite big really. (Interviewee 20 – senior nurse)
Some interviewees remarked that it should be clear to people that they were being invited but not obliged to participate:
A lot of people just tell people what to do, like ‘you’re going to do this’. […] It has to be what they want to do and not what you want to do to me. So has to be clear that it is an invitation. (Interviewee 5 – patient)
Interviewees also observed that it would be important to make staff and hospice users aware that the study was taking place via briefing sessions and posters in public areas: ‘It’s about setting your stall out for everybody to understand what’s going on’ (Interviewee 20 – senior nurse). The opportunity to opt out of the research after the recording was also seen as important. Proposed safeguards for the recording phase included measures to make the recording unobtrusive, to stop the recording during the consultation and the offer of extra support to people who had been recorded. Safeguards for the dissemination phase included use of anonymisation techniques, restriction of data access to selected audiences and screening the data in safe environments where spectators (e.g. communication skills courses trainees) could be supported.
Discussion
We interviewed hospice patients, carers and clinical staff about the acceptability of video recording palliative medicine consultations for research and teaching purposes. Compared to previous research that has supported the acceptability of video recording for the more limited purpose of improving doctors’ communication skills,39 our study explored the views of a range of stakeholders, and – by virtue of its qualitative design – allowed a broader and deeper exploration of reasons underlying judgements around acceptability of video recording for communication research and training.
Participants expressed concerns about the risks associated with video-based research; although these concerns did not outweigh the overall judgement that video-based research was acceptable and worthwhile, they raised a more situated dilemma of whether some participants should be invited to take part in a video-based study. Our findings raise the question: who ultimately makes the decision of whether to invite patients and carers to take part in video-based research? Most interviewees acknowledged that patients and carers should be given the opportunity to decide for themselves about involvement in research; the patients we interviewed endorsed this view.47 However, our stakeholders also emphasised that a line had to be drawn somewhere; this meant that severely distressed patients and carers should not be approached. In our subsequent video-based study at the same hospice, we adopted this as an exclusion criterion for patient and carer involvement; the care team made judgements about whether or not patients and carers could be approached on a case-by-case basis.41
Broadly, we believe that the dilemma of patient and carer recruitment to video-based research cannot be solved once and for all and that it involves local judgements taking into consideration situational factors. Elsewhere we have proposed a framework to support researchers’ situated decisions on these matters.25 This framework comprises several safeguards (e.g. the option for participants to revisit their consent in time) and diversified modes of patient, carer and HCP involvement (e.g. the option to have a consultation audio recorded, rather than video recorded).
Our findings should be taken with some caution. The people we interviewed had obviously already agreed to take part in a study (in which they were being recorded!); therefore, their favourable take on video-based research does not necessarily reflect the full range of attitudes. Some may also have been prone to express positive views in deference to the researcher – knowing that she was hoping to do video-based research at the hospice in the future. Unlike Hargreaves and Peppiatt’s study39 where patients experienced having a consultation recorded, we presented our participants with a hypothetical scenario. We also acknowledge that the number of participants in each sub-group was small and that therefore we cannot claim to have captured the full breadth of possible views on the topics explored in this study. Finally, we did not explore nurses’ reactions to the idea of being recorded; this remains an area of exploration for future research. While these limitations invite some caution when interpreting our findings, our study suggests that video-based research is positively valued by stakeholders on condition that measures are taken to manage risks associated with it. We believe our study also demonstrates the value of investigating participant acceptability of video recording; here, we have addressed video recording for research and training. Future research should examine participant acceptability of video recording for other purposes, including surveillance and quality improvement.48,49 This could generate significant insights on the ethical implications of video recording people’s activities – an increasingly pervasive presence in our daily lives.
Acknowledgments
We acknowledge the important input to the project as a whole of the VERDIS research project advisory group: Jeanne Rae, David Barnard, Sandra Winterburn, Doug Maynard, Nicola Power and Jane Seymour. We thank Idaliza Nukis for her invaluable administrative support in the course of the project. We particularly thank the following who provided valuable advice on earlier drafts of this paper and of the recommendations: Christopher Koenig, Traci Walker, Piera Margutti and the Darg group at Loughborough.
Footnotes
Data availability: The primary data for the study consist of a corpus of audio recorded interviews. The authors’ study protocol does not allow them to share the data beyond the research team in order to protect the participants’ confidentiality. However, the pseudonymised transcripts of the interviews examined in this paper can be obtained upon request by contacting the first author.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship and/or publication of this article: This research was supported in its initial stages by the University of Nottingham, including via a Research Development Fund grant from the University of Nottingham Centre for Advanced Studies; later stages of work were funded by The Health Foundation via an Insight grant RU33. The Health Foundation funded open access publication for this paper. From January 2015 onwards, R.P.’s work, including in finalising this report, was supported by National Institute for Health Research Career Development Fellowship award CDF-2014-07-046. This report presents independent research partially funded by the National Institute for Health Research (NIHR). The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health.
References
- 1. Department of Health. End of life care strategy: promoting high quality care for all adults at the end of life. Report, Department of Health, London, 16 July 2008. [Google Scholar]
- 2. Worldwide Palliative Care Alliance. Global atlas of palliative care at the end of life. Report, Worldwide Palliative Care Alliance, London, January 2014. [Google Scholar]
- 3. Walczak A, Butow PN, Bu S, et al. A systematic review of evidence for end-of-life communication interventions: who do they target, how are they structured and do they work? Patient Educ Couns 2016; 99: 3–16. [DOI] [PubMed] [Google Scholar]
- 4. Parry R, Land V, Seymour J. How to communicate with patients about future illness progression and end of life: a systematic review. BMJ Support Palliat Care 2014; 4: 331–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. National Institute for Health and Care Excellence (NICE). Care of dying adults in the last days of life. Report, NICE, London, 16 December 2015. [PubMed] [Google Scholar]
- 6. National Palliative and End of Life Care Partnership. Ambitions for palliative and end of life care: a national framework for local action 2015–2020. Report, 2015, http://endoflifecareambitions.org.uk/wp-content/uploads/2015/09/A-Presentation-of-the-Ambitions-for-Palliative-and-End-of-Life-Care1.pdf
- 7. Almack K, Cox K, Moghaddam N, et al. After you: conversations between patients and healthcare professionals in planning for end of life care. BMC Palliat Care 2012; 11: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gaston CM, Mitchell G. Information giving and decision-making in patients with advanced cancer: a systematic review. Soc Sci Med 2005; 61(10): 2252–2264. [DOI] [PubMed] [Google Scholar]
- 9. Walczak A, Butow PN, Davidson PM, et al. Patient perspectives regarding communication about prognosis and end-of-life issues: how can it be optimised? Patient Educ Couns 2013; 90(3): 307–314. [DOI] [PubMed] [Google Scholar]
- 10. Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage 2007; 34(1): 81–93. [DOI] [PubMed] [Google Scholar]
- 11. Abdul-Razzak A, You J, Sherifali D, et al. Patient preferences for physicians’ end-of-life communication behaviors. J Palliat Care 2014; 30(3): 218. [Google Scholar]
- 12. Abdul-Razzak A, You J, Sherifali D, et al. ‘Conditional candour’ and ‘knowing me’: an interpretive description study on patient preferences for physician behaviours during end-of-life communication. BMJ Open 2014; 4: e005653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Clayton JM, Butow PN, Tattersall MH. When and how to initiate discussion about prognosis and end-of-life issues with terminally ill patients. J Pain Symptom Manage 2005; 30(2): 132–144. [DOI] [PubMed] [Google Scholar]
- 14. Seccareccia D, Wentlandt K, Kevork N, et al. Communication and quality of care on palliative care units: a qualitative study. J Palliat Med 2015; 18(9): 758–764. [DOI] [PubMed] [Google Scholar]
- 15. Stephen N, Skirton H, Woodward V, et al. End-of-life care discussions with nonmalignant respiratory disease patients: a systematic review. J Palliat Med 2013; 16(5): 555–565. [DOI] [PubMed] [Google Scholar]
- 16. Seymour J, Almack K, Kennedy S. Implementing advance care planning: a qualitative study of community nurses’ views and experiences. BMC Palliat Care 2010; 9: 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Addington-Hall J, McPherson C. After-death interviews with surrogates/bereaved family members: some issues of validity. J Pain Symptom Manage 2001; 22(3): 784–790. [DOI] [PubMed] [Google Scholar]
- 18. Fine E, Reid C, Shengelia R, et al. Directly observed patient-physician discussions in palliative and end-of-life care: a systematic review of the literature. J Palliat Med 2010; 13(5): 595–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Walshe C, Ewing G, Griffiths J. Using observation as a data collection method to help understand patient and professional roles and actions in palliative care settings. Palliat Med 2012; 26(8): 1048–1054. [DOI] [PubMed] [Google Scholar]
- 20. Drew P, Chatwin J, Collins S. Conversation analysis: a method for research into interactions between patients and health-care professionals. Health Expect 2001; 4(1): 58–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Parry R. Video-based conversation analysis. In: Bourgeault I, Dingwall R, De Vries R. (eds) The SAGE handbook of qualitative methods in health research. London: SAGE, 2010, pp. 373–396. [Google Scholar]
- 22. Heritage J, Maynard DW. Communication in medical care. Cambridge: Cambridge University Press, 2006. [Google Scholar]
- 23. Robinson JD, Heritage J. Intervening with conversation analysis: the case of medicine. Res Lang Soc Interact 2014; 47(3): 201–218. [Google Scholar]
- 24. Jenkins L, Cosgrove J, Ekberg K, et al. A brief conversation analytic communication intervention can change history-taking in the seizure clinic. Epilepsy Behav 2015; 52: 62–67. [DOI] [PubMed] [Google Scholar]
- 25. Parry R, Pino M, Faull C, et al. Acceptability and design of video-based research on healthcare communication: evidence and recommendations. Patient Educ Couns 2016; 99: 1271–1284. [DOI] [PubMed] [Google Scholar]
- 26. American Medical Association (AMA). Opinion 5.046-filming patients for the education of health professionals. Report, AMA, Chicago, IL, 2003. [Google Scholar]
- 27. Caldwell K. Non-participant observation: using video tapes to collect data in nursing research. Nurse Res 2005; 13(2): 42–54. [DOI] [PubMed] [Google Scholar]
- 28. Gelbart B, Barfield C, Watkins A. Ethical and legal considerations in video recording neonatal resuscitations. J Med Ethics 2009; 35(2): 120–124. [DOI] [PubMed] [Google Scholar]
- 29. Latvala E, Vuokila-Oikkonen P, Janhonen S. Videotaped recording as a method of participant observation in psychiatric nursing research. J Adv Nurs 2000; 31(5): 1252–1257. [DOI] [PubMed] [Google Scholar]
- 30. Arafeh S, McLaughlin M. Legal and ethical issues in the use of video in education research. NCES Working paper no. 2002-01, January 2002. Washington, DC: National Centre for Education Statistics (ED). [Google Scholar]
- 31. Broyles LM, Tate JA, Happ MB. Videorecording in clinical research: mapping the ethical terrain. Nurs Res 2008; 57(1): 59–63. [DOI] [PubMed] [Google Scholar]
- 32. Corti L, Day A, Backhouse G. Confidentiality and informed consent: issues for consideration in the preservation of and provision of access to qualitative data archives. Forum Qual Soc Res 2000; 1(3): 7. [Google Scholar]
- 33. Crow G, Wiles R. Managing anonymity and confidentiality in social research: the case of visual data in community research. ESRC National Centre for Research Methods, 2008, http://eprints.ncrm.ac.uk/459/1/0808_managing%2520anonymity%2520and%2520confidentiality.pdf [Google Scholar]
- 34. Papademas D. and The International Visual Sociology Association. IVSA code of research ethics and guidelines. Visual Stud 2009; 24(3): 250–257. [Google Scholar]
- 35. Wiles R, Prosser J, Bagnoli A, et al. Visual ethics: ethical issues in visual research. National Centre for Research Methods, 2008, http://eprints.ncrm.ac.uk/421/1/MethodsReviewPaperNCRM-011.pdf [Google Scholar]
- 36. Koffman J, Morgan M, Edmonds P, et al. Vulnerability in palliative care research: findings from a qualitative study of black Caribbean and white British patients with advanced cancer. J Med Ethics 2009; 35(7): 440–444. [DOI] [PubMed] [Google Scholar]
- 37. Casarett D. Ethical considerations in end-of-life care and research. J Palliat Med 2005; 8(Suppl. 1): S148–S160. [DOI] [PubMed] [Google Scholar]
- 38. Casarett DJ, Knebel A, Helmers K. Ethical challenges of palliative care research. J Pain Symptom Manage 2003; 25(4): S3–S5. [DOI] [PubMed] [Google Scholar]
- 39. Hargreaves PH, Peppiatt R. Is videotaping of consultations acceptable to patients attending a hospice day centre? Palliat Med 2001; 15: 49–54. [DOI] [PubMed] [Google Scholar]
- 40. Smith JA. Semi-structured interviewing and qualitative analysis. In: Smith JA, Harré R, Van Langenhore L. (eds) Rethinking methods in psychology. London: SAGE, 1995, pp. 9–26. [Google Scholar]
- 41. Pino M, Parry R, Land V, et al. Engaging terminally ill patients in end of life talk: how experienced palliative medicine doctors navigate the dilemma of promoting discussions about dying. PLoS ONE 2016; 11(5): e0156174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Patton MQ. Qualitative research & evaluation methods, 3rd ed. Thousand Oaks, CA: SAGE, 2002. [Google Scholar]
- 43. Wilkinson S. Focus group methodology: a review. Int J Soc Res Methodol 1998; 1(3): 181–203. [Google Scholar]
- 44. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 45. Rapley T. Some pragmatics of data analysis. In: Silverman D. (ed.) Qualitative research: theory, method and practice. London: SAGE, 2010, pp. 273–290. [Google Scholar]
- 46. Potter J, Hepburn A. Qualitative interviews in psychology: problems and possibilities. Qual Res Psychol 2005; 2: 281–307. [Google Scholar]
- 47. Steinhauser KE, Clipp EC, McNeilly M, et al. In search of a good death: observations of patients, families, and providers. Ann Intern Med 2000; 132: 825–832. [DOI] [PubMed] [Google Scholar]
- 48. Schwartz A. Chicago’s video surveillance cameras: a pervasive and poorly regulated threat to our privacy. Northwest J Tech Intellect Property 2013; 11(2): 4. [Google Scholar]
- 49. Weinger MB, Gonzales DC, Slagle J, et al. Video capture of clinical care to enhance patient safety. Qual Saf Health Care 2004; 13: 136–144. [DOI] [PMC free article] [PubMed] [Google Scholar]