Abstract
Introduction:
Increasing numbers of patients with hip fractures also have advanced comorbidities. A majority are treated surgically. However, a significantly increasing percentage of medically unfit patients with unacceptably high risk of perioperative death are treated nonoperatively. Important questions about patients’ prefracture quality of life (QOL) and future perspectives should be asked before considering different treatment options to assess what kind of treatment is advisable in frail elderly high-risk patients with a hip fracture.
Objective:
The aim of this review was to provide an overview of differences in mortality, health-related QOL [(HR)QOL], functional outcome, and costs between nonoperative management (NOM) and operative management (OM) of hip fractures in patients above 65 years.
Methods:
A systematic literature search was performed in EMBASE, OvidSP, PubMed, Cochrane Central, and Web of Science for observational studies and trials. Observational studies and randomized controlled trials comparing NOM with OM in hip fracture patients were selected. The methodological quality of the selected studies was assessed according to the Methodological Index for Nonrandomized Studies (MINORS) or Furlan checklist.
Results:
Seven observational studies were included with a total of 1189 patients, of whom 242 (20.3%) were treated conservatively. The methodological quality of the studies was moderate (mean: 14.7, standard deviation [SD]: 1.5). The 30-day and 1-year mortalities were higher in the nonoperative group (odds ratio [OR]: 3.95, 95% confidence interval [CI]: 1.43-10.96; OR: 3.84, 95% CI: 1.57-9.41). None of the included studies compared QOL, functional outcome, or health-care costs between the 2 groups.
Conclusion:
This systematic review and meta-analysis demonstrated that only a few studies with small number of patients comparing NOM with OM were published. A significantly higher 30-day and 1-year mortality was revealed in nonoperatively treated hip fracture patients. No data were found examining (HR)QOL and costs. Further work is needed to enable shared decision-making and to initiate NOM in frail elderly patients with advanced comorbidity and limited life expectancy.
Keywords: hip fracture, (non)operative treatment, elderly, mortality, quality of life
Introduction
Early surgical repair has been shown to give the best outcomes in frail elderly patients with a hip fracture. With a 30-day mortality rate of 10% to 13% and a 1-year mortality rate ranging from 22% to 33%, there may be some patients who are at the end of life and would be better served with nonoperative management (NOM).1,2
Randomized controlled trials (RCTs) on the effectiveness of surgical treatment are scarce, due to ethical issues. In 2008, Handoll and Parker published a Cochrane systematic review comparing conservative with operative treatment for hip fractures.3 They reported insufficient evidence with potentially serious bias to prove that operative management (OM) is better than bed rest and traction. In addition to mortality, other outcomes with major impact for elderly patients with a hip fracture are functional outcome, (health-related) quality of life [(HR)QOL], and health status.4,5 The importance of these factors on determination of OM or NOM is unknown.
The aim of this systematic review was to provide an overview and update of the literature comparing NOM with OM for hip fractures in people older than 65 years. To obtain an overview of outcome measures, we searched for mortality, (HR)QOL, functional outcome, and health-care costs. We also attempted to examine the relationship of comorbidities to decision for OM or NOM within these studies.
Materials and Methods
Search Strategy
A systematic literature search was conducted for hip fractures and treatment in EMBASE, OvidSP, PubMed, Cochrane Central, and Web of Science from 1966 up to May 2015. In addition, references of all retrieved articles were screened for eligible studies that were not found in the initial search.
The literature search included keywords related to “proximal femoral fracture,” “elderly,” “surgery,” “conservative treatment,” “mortality,” “ comorbidity,” “quality of life,” “function,” and “costs.” The search strategy is outlined in Supplemental Appendix 1.
Study Selection
Studies comparing NOM with OM in hip fracture patients were selected. The following inclusion and exclusion criteria were used to determine the eligibility of a study: (1) Elderly patients (age ≥65 years) who sustained a hip fracture; (2) Hip fractures were defined as femoral neck, pertrochanteric, intertrochanteric, or subtrochanteric fractures, and greater trochanteric fractures, isolated lesser trochanteric fractures, acetabular fractures, and pelvic fractures were excluded; (3) The main outcome measure was 30-day and/or 1-year mortality; (4) The study was published in a peer-reviewed English-language journal; and (5) A full text of the article was available. Studies that only included mechanically stable (femoral neck Garden 1) fractures were excluded. Also, case reports, comments, editorials, guidelines, meta-analyses, and reviews were excluded.
Data Collection
Two reviewers (CLPvdR and MACDJ) independently selected potentially relevant studies based on title, abstract, and full text of the studies retrieved in the literature search. Discrepancies in selection between the 2 reviewers were resolved by consensus. In case of persistent disagreement, a third reviewer (TG) was consulted. The search procedure was documented according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses flow diagram (PRISMA).6 Eligibility criteria were reported in accordance with Participants, Intervention, Comparison, Outcome, and Study design. The following study characteristics were extracted from the included studies: first author, year of publication, country, design, year of inclusion, sample size, type of fracture, type of NOM and OM, mean age, gender, and length of follow-up. In case of absence of one of these characteristics, the corresponding author was contacted. Outcome measures such as mortality, (HR)QOL, function, and costs were reported. Other outcomes of the included studies were described as present or not: pain, causes of death, complications, residential status, length of stay, comorbidity and American Society of Anesthesiologists (ASA) classification.
Quality Assessment
The quality of the included studies was independently assessed by 2 reviewers (CLPvdR and MACDJ). Disagreements were resolved by consensus. For RCTs, we used the 12 risk-of-bias criteria of Furlan et al.7 Each item was scored as “‘yes,” “no,” or “unsure.” For observational or nonrandomized surgical studies, we used the 12-item Methodological Index for Nonrandomized Studies (MINORS).8 MINORS is a valid instrument and designed to assess the methodological quality of nonrandomized surgical studies, whether comparative or noncomparative. Each item was scored a “0” (not reported), “1” (not adequately reported), or “2” (adequately reported). The maximum score was 24 for comparative studies. MINORS was not converted to a degree of bias by the authors.
Data and Statistical Analysis
We included all eligible articles and performed a meta-analysis of mortality in hip fracture patients. The 30-day and 1-year mortality rates were extracted from the studies and included in the meta-analysis. Effect measures of interest were crude and pooled odds ratio (OR) and corresponding 95% confidence interval (CI). The P-value was based on a 2-sided test and was considered statistically significant at P < .05. Heterogeneity between the studies was determined using I 2.9 Interpretation of I 2 of 30% to 60% may represent moderate heterogeneity, and substantial heterogeneity was defined as I 2 ≥60.10 The random-effects model was used to calculate the pooled OR (95% CI), due to heterogeneity between cohorts. Analyses were performed with Review manager (Revman) version 5.3.11
Results
Search Results
A total of 1481 studies were found (815 from EMBASE, 437 from OvidSP, 3 from PubMed, 11 from Cochrane Central, and 215 from Web of Science). After removal of duplicate articles (n = 487), 994 unique titles and abstracts were screened for eligibility. Finally, 7 articles fulfilled the inclusion criteria. The most common reasons for exclusion were the absence of a comparison between NOM and OM and a population aged under 65 years. The flow diagram of the study is shown in Figure 1.
Figure 1.
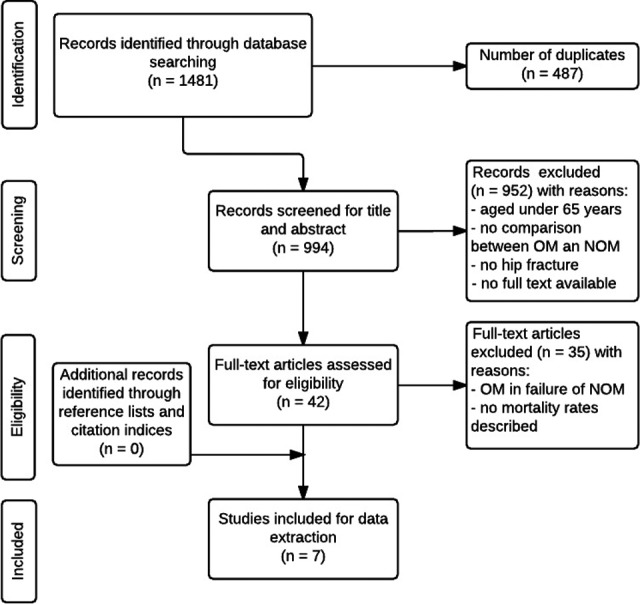
Flow diagram; selection of articles: operative versus nonoperative management in elderly patients with a hip fracture.
Study Characteristics
The included observational studies were published between 2001 and 2013. In 5 studies, the data were retrospectively gathered.12–16 The mean follow-up was 11.3 months (range: 1-24 months). Sample sizes ranged from n = 2316 to n = 666.13 A total of 1189 patients were included, 242 (20.3%) of whom were treated conservatively. The mean age ranged from 76.914 to 101.816 years. Five studies included intracapsular and extracapsular fractures and made no distinction between mechanically stable and unstable femoral neck fractures.12,14–17 Two studies published only about displaced femoral neck fractures.13,18 Table 1 demonstrates the characteristics of all included studies and Table 2 presents an overview of the outcome measures.
Table 1.
Overview of Included Studies Comparing Operative Versus Nonoperative Management.
| Study, Year of Publication | Setting | Design | Prospective | Year | Study Population (Number; Years) | Type of Fracture | NOM | OM | Mean Age | % Female | FU, months |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Beloosesky et al12 | Israel | Cohort | No | 1993-1999 | N = 78; >65 years | Intracapsular (47.4%), extracapsular (46.2%), subtrochanteric (6.4%) | N = 64; 82.1%; EM (even in bedridden patients) | N = 14; 17.9%; IF, HA | ♀ 81.2; ♂ 82.0; range: 65-98 | 65.4 | 12 |
| Dedovic et al17 | Bosnia and Herzegovina | Non-RCT | Yes | 2011-2012 | N = 66; >65 years High cardiac risk | Femoral neck (27.3%), intertrochanteric (53.0%), subtrochanteric (19.7%) | N = 32; 48.5%; unknown | N = 34; 51.5%; unknown | 78.5 (5.46; 65-92) | NOM: 75; OM: 67.6 | 6 |
| Gregory et al18 | United Kingdom | Non-RCT | Yes | 2005-2006 | N = 102; >70 years | Displaced femoral neck | N = 22; 21.6%; EM | N = 80; 78.4%; uncemented Austin Moore HA | 84 | 66.7 | 12 |
| Ishimaru et al13 | Japan | Cohort | No | 2001-2009 | N = 666; >70 years | Displaced femoral neck (42.6%), ≥type 2 trochanteric (57.4%) | N = 20; 3.0%; traction | N = 646; 97%; IF, HA | NOM: 83.7; OM: 85.4 | NOM: 95; OM: 81.6 | 12 |
| Jain et al14 | Canada | Case control | No | 1989-1995 | N = 170; >65 years | Femoral neck (50%), intertrochanteric (50%) | N = 62; 36.5%; BR: n = 41; EM: n = 21 | N = 108; 63.5%; IF, HA, THA | BR: 76.9 (17.0); EM: 78.8 (10.8); OM: 79.1 (13.2) | NOM: 64.5; OM: 63.9 | 1 |
| Ooi et al15 | Singapore | Cohort | No | 1998-1999 | N = 84; >90 years | Femoral neck (56.0%), intertrochanteric (44.0%) | N = 38; 45.2%; Hamilton-Russell traction | N = 46; 54.8%; HA, DHS, PFN, B-HA | – | 86.9 | 24 |
| Shabat et al16 | Israel | Cohort | No | 1990-2001 | N = 23; >100 years | Femoral neck (17.3%), pertrochanteric (82.7%) | N = 4; 17.4%; BR with skin traction | N = 19; 82.6%; DHS, Thompson HA | 101.8 | 73.9 | 12 |
Abbreviations: B-HA, bipolar hemiarthroplasty; BR, bed rest; DHS, dynamic hip screw; EM, early mobilization; FU, follow-up; HA, hemiarthroplasty; IF, internal fixation; NOM, nonoperative management; OM, operative management; PFN, proximal femoral nail; RCT, randomized controlled trial; THA, total hip arthroplasty.
Table 2.
Outcome Measures of the Included Studies.a
| Study | Mortality | Comorbidity | (HR)QOL | Function and Mobility | Costs | Pain | Causes of Death | ASA | Complications | Residential Status | Length of Stay |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Beloosesky et al12 | +c | + | − | + | − | − | − | + | + | + | + |
| Dedovic et al17 | +a,b | + | − | − | − | − | − | − | − | − | − |
| Gregoryet al18 | +a,c | + | − | + | − | − | + | + | + | + | + |
| Ishimaru et al13 | +c | + | − | − | − | − | + | + | + | − | − |
| Jain et al14 | +a | + | − | − | − | − | − | + | + | − | + |
| Ooi et al15 | +a,b,c,d | + | − | + | − | − | + | + | + | − | + |
| Shabat et al16 | +a,c | + | − | + | − | − | − | + | + | + | + |
Abbreviation: ASA, American Society of Anesthesiologists; (HR)QOL, health-related quality of life.
Outcome measures: +: present or −: lacking.
aThirty days.
bSix months.
cOne year.
dTwo years.
Quality Assessment
The mean MINORS score for the included observational studies was 14.7 (standard deviation [SD]: 1.5; Table 3). One study used prospectively collected data and these were adequately reported.18 None of the studies reported about blinding evaluation for unbiased assessment. All studies had an adequate control group, because OM is recognized as the optimal intervention in case of hip fractures. Jain et al14 reported adequate baseline equivalence of the 2 groups, NOM and OM. They also presented an adequate measure of effect with an OR (95% CI).
Table 3.
Quality Assessment of the Included Studies.
| MINORS | Beloosesky et al12 | Dedovic et al17 | Gregory et al18 | Ishimaru et al13 | Jain et al14 | Ooi et al15 | Shabat et al16 | |
|---|---|---|---|---|---|---|---|---|
| 1 | A clearly stated aim | 2 | 1 | 0 | 2 | 2 | 2 | 2 |
| 2 | Inclusion of consecutive patients | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 3 | Prospective collection of data | 1 | 1 | 2 | 0 | 0 | 0 | 0 |
| 4 | End points appropriate to the aim of the study | 2 | 2 | 1 | 2 | 2 | 2 | 2 |
| 5 | Unbiased assessment of the study end point | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 6 | Follow-up period appropriate to the aim of the study | 1 | 1 | 2 | 2 | 1 | 2 | 2 |
| 7 | Loss to follow-up less than 5% | 1 | 0 | 2 | 1 | 2 | 2 | 2 |
| 8 | Prospective calculation of the study size | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 9 | An adequate control group | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 10 | Contemporary groups | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 11 | Baseline equivalence of groups | 1 | 1 | 1 | 1 | 2 | 0 | 0 |
| 12 | Adequate statistical analyses | 1 | 0 | 1 | 1 | 2 | 1 | 0 |
| Total | 15 | 12 | 15 | 15 | 17 | 15 | 14 |
Abbreviation: MINORS, Methodological Index for Nonrandomized Studies.
Meta-Analysis: Mortality
Thirty-day mortality was reported in 5 studies14–18 and 1-year mortality was reported in 4 studies13,15,16,18 for both treatment groups. Beloosesky et al12 reported a 1-year mortality of 32% without a significant difference between OM and NOM. This author was contacted by e-mail but did not respond to the request of sending the mortality rates for both groups.
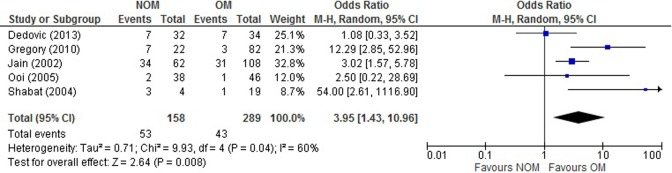
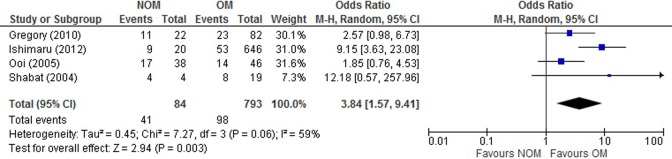
The forest plots of the meta-analyses of 30-day and 1-year mortality comparing NOM and OM are shown in Figures 2 and 3. The plots show moderate degree of heterogeneity of effects in the observational studies. The unadjusted pooled OR of 30-day mortality revealed a 3.95-fold higher mortality for NOM than for OM (95% CI: 1.43-10.96). For 1-year mortality, an unadjusted pooled OR revealed a 3.84-fold higher mortality for NOM than for OM (95% CI: 1.57-9.41).
Figure 2.
Thirty-day mortality.
Figure 3.
One-year mortality.
Bed rest in conservatively treated patients revealed a 3.8-fold higher 30-day mortality (95% CI: 1.1-14.0) than early mobilization.14 Dedovic et al reported 6-month mortality and we calculated an unadjusted pooled OR of death associated with NOM to OM, which was 1.09 (95% CI: 0.33-3.52). The calculated unadjusted pooled OR for 2-year mortality given by Ooi et al was 1.95 (95% CI: 0.82-4.67). We also calculated the unadjusted pooled OR for 1-year mortality in 3 studies (ie, Gregory et al, Ooi et al, Shabat et al) in which patients survived beyond 30 days, which was 1.57 (95% CI: 0.77-3.20).
Quality of Life
None of the articles reported (HR)QOL after NOM or OM.
Function and Mobility
Two studies used the Katz Index of Activities of Daily Living to assess functional status as a measurement of the patient’s ability to perform basic activities of daily living (BADL) independently without comparing NOM to OM.12,16 Beloosesky et al discovered no significant difference in survival between prefracture independent patients versus partially and completely dependent patients. Shabat et al did not distinguish between OM and NOM in their population of patient ages 100 and older. Sixteen patients had not been able to perform any of the BADL prefracture, whereas 7 patients had only been partially able to perform their BADL. After the hip fracture, 3 of these patients had a slight reduction in the BADL and 4 were unable to do BADL. Among 19 of 23 operated patients, 11 had ambulated with a walker prior to the fracture and 8 patients had been nonambulatory. Of the 11 patients, only 4 patients regained their walking ability with a walker and 7 became nonambulatory. In the conservatively treated group (n = 4), 2 patients had been able to walk prior to the fracture and all of them could not anymore walk after the fracture. One study distinguished between independent and dependent ambulators and found that operative treatment significantly increased the ability for independent ambulation in patients who were independent prior to fracture (P < .01).15 Gregory et al18 only analyzed mobility in 11 survivors of NOM at 1-year follow-up without using an adequate measuring instrument.
Costs
None of these studies reported on the direct or indirect medical costs.
Comorbidity
The most prevalent comorbidities were dementia, cardiac diseases, and diabetes mellitus (Table 4). ASA classification was given in 6 articles. None of these studies involved patients with ASA grade V. The main causes of surgical delay and unstable medical conditions described by Beloosesky et al were cardiac problems (38.5%), infections (37.2%), and diabetic or electrolyte abnormalities (12.8%).
Table 4.
Comorbidity Reported in Included Studies.
| Study | Beloosesky et al,12 n (%) | Dedovic et al,17,a n (%) | Gregory et al,18,b n (%) | Ishimaru et al,13 n (%) | Jain et al,14 n (%) | Ooi et al,15,c n (%) | Shabat et al,16 n (%) | |
|---|---|---|---|---|---|---|---|---|
| Dementia | NOM | 38 (48.8)d | 3 (13.6) | 10 (50.0) | 22 (35.5) | 46 (54.8)d | 15 (65.2)d | |
| OM | 247 (38.2) | 28 (25.9) | ||||||
| Ischemic heart disease/chronic heart failure | NOM | 67 (85.9)d | 31 (96.9) | 11 (50.0) | 12 (60.0) | 19 (30.6) | 8 (34.8)d | |
| OM | 31 (91.2) | 158 (24.5) | 44 (40.7) | |||||
| CVA/TIA | NOM | 12 (37.5) | 6 (27.3) | 6 (30.0) | 8 (12.9) | |||
| OM | 16 (47.1) | 91 (14.1) | 24 (22.2) | |||||
| Diabetes mellitus | NOM | 20 (25.6)d | 20 (62.5) | 6 (27.3) | 3 (15.0) | 5 (8.1) | 10 (43.5)d | |
| OM | 22 (64.7) | 86 (13.3) | 14 (13.0) | |||||
| COPD/asthma | NOM | 16 (20.5)d | 3 (13.6) | 3 (15.0) | 15 (24.2) | |||
| OM | 44 (6.8) | 32 (29.6) | ||||||
| Renal insufficiency | NOM | 11 (14.1)d | 6 (18.8) | 5 (25.0) | 7 (11.3) | |||
| OM | 1 (2.9) | 31 (4.8) | 9 (8.3) | |||||
| Malignancy | NOM | 5 (6.4)d | 4 (18.2) | 4 (20.0) | 14 (22.6) | |||
| OM | 60 (9.3) | 9 (8.3) | ||||||
| ASA score I/II | NOM | 33 (51.6) | 1 (4.5) | 2 (10.0) | 3 (4.8) | 62 (73.8)d | ||
| OM | 13 (92.9) | 30 (37.5) | 385 (59.6) | 4 (3.7) | ||||
| ASA score III/IV | NOM | 31 (48.4) | 21 (95.5) | 18 (90.0) | 59 (95.2) | 22 (26.2)d | ||
| OM | 1 (7.1) | 50 (62.5) | 261 (40.4) | 104 (96.3) |
Abbreviations: ASA, American Society of Anesthesiologists; COPD, Chronic obstructive pulmonary disease; CVA, cerebrovacuscular accident; N, number of patients; NOM, nonoperative management; OM, operative management; TIA, Transient Ischaemic Attack.
aOnly inclusion of patients with 3 or more cardiac comorbid risk factors: chronic heart failure, previous myocardial infarction or angina pectoris, insulin-dependent diabetes mellitus, previous cerebrovascular insult or transitory ischemic attack, and renal insufficiency.
bOnly report for 22 nonoperatively treated patients.
cOnly report about dementia.
dTotal reported numbers for NOM and OM.
Three studies12,13,18 reported higher overall ASA grades in nonoperatively treated patients. Jain et al14 described a significantly higher number of patients with ASA IV grade in the bed rest group compared to the early mobilization group (P = .0004). Preadmission comorbidities of both groups were similar, except for depression, which was more frequent in the early mobilization group. Ishimaru et al13 showed that heart disease was significantly more common in nonoperatively treated patients than in operatively treated patients (P < .01). Dedovic et al17 only reported about elderly patients with high cardiac risk (≥3 risk factors), based on the Lee index. Ooi et al15 reported that at least 62 of 84 patients had 1 or more diseases in terms of comorbidity. In patients with a Mini-Mental State Examination score of less than 7, the probability of death over the subsequent 24 months was significantly increased (P < .05).
Shabat et al16 showed no significant difference in the number of major background diseases between NOM and OM (2.74 ± 1.01 vs 2.75 ± 0.83; P > .05). The operatively treated group of patients with a 1-year survival had on average 2.0 ± 0.77 background diseases (survival less than 1 year: 3.75 ± 0.46; P < .0001). In 5 studies, patients who were medically unfit due to comorbidity were treated nonoperatively.12–15,18
Discussion
This review and meta-analysis aimed to provide an overview of studies comparing nonoperative with operative treatment with respect to mortality, (HR)QOL, and costs in elderly patients with a hip fracture.
In general, 30-day and 1-year mortalities were higher in the nonoperatively treated group. None of the included studies compared outcome measures of (HR)QOL, functional outcome, or health-care costs between OM and NOM.
This review included 7 nonrandomized and observational studies of moderate quality according to MINORS. The meta-analysis revealed that the unadjusted pooled 30-day and 1-year mortality ORs were almost 4 times higher for NOM compared to OM.
No RCTs have been performed since the previous Cochrane review of adults with a hip fracture. Handoll et al included 5 randomized trials, 2 of which were abstracts and 1 an unpublished study.3,19–22 Those studies were published between 1975 and 1994 and the authors did not report on (HR) QOL in these populations. Our review included studies that were published between 2001 and 2013, and we focused on frail elderly patients of 65 years and older in our systematic review. However, none of the studies that compared NOM with OM used a frailty measure. Therefore, we tried to assess the severity of the patients’ health problems at the time of admission, by describing comorbidity and ASA classification as represented in the included studies.
There are some limitations to our study. First, the reported ORs could not be adjusted for potential confounders, such as comorbidity, gender, age, mental health status, degree of frailty, or type of intervention. These unadjusted pooled ORs should be interpreted with caution. von Hippel et al showed that I 2 should be presented and interpreted with caution in small meta-analyses.23 Therefore, the heterogeneity we found may be considered as imprecise and biased. The random-effects model was used because the effect size varied from study to study and this model was more likely to fit the actual sampling distribution.24 The effect size might be higher or lower due to differences in case mix.
Second, due to missing information about types of intracapsular fractures, we could not distinguish between mechanically stable and unstable fractures.12,14–17 We excluded all studies selectively reported Garden 1 femoral neck fractures, as these are fundamentally different from displaced fractures and may effectively be treated with NOM.25 Finally, this study is not generalizable to countries where surgery may not be an option for every patient with a hip fracture.
Future research on differences in outcome between NOM and OM should measure the pre- and postfracture status in elderly patients using instruments for frailty and (HR) QOL (eg, European Quality of Life-5 Dimensions,26 ICEpop CAPability measure for Older people,27–29 Groningen Frailty Indicator,30 with short- and long-term follow-up). Cost-effectiveness is also important, including direct and indirect medical costs with calculation of Quality-adjusted life years (QALYs). The optimal study design to overcome selection bias is an RCT. However, such a study design would lead to several ethical issues because clinicians would be faced with performing surgery on patients with a high risk to die perioperatively or with withholding surgery from patients who are very likely to benefit from an operation. Future research could help clinicians to determine which category of patients could be treated conservatively by developing risk profiles and, for example, a risk score chart.
In conclusion, this systematic review and meta-analysis demonstrated that only a few observational studies with a small number of patients comparing NOM with OM have been published. A significantly higher 30-day and 1-year mortality was revealed in nonoperatively treated hip fracture patients above 65 years compared to operatively treated patients. Comorbidity did not seem to purely drive this decision-making. No data were found examining (HR)QOL, degree of frailty, and costs. Future studies are urgently needed to provide this important information to aid patients and providers in decision-making for surgical repair, particularly in frail elderly patients.
Supplementary Material
Acknowledgments
The authors would like to thank Gerdien de Jonge for her help with the search strategy, and Lisette van Hulst for her contribution to the proofreading of the manuscript.
Authors’ Note: CLPvdR, MACDJ, CMMP, LdM, JAR, and TG contributed to conception and design of this study. Study selection and data extraction of the finally included studies were done by CLPvdR and MACDJ. CLPvdR and MACDJ independently assessed the methodological quality of each included study. CLPvdR, MACDJ, CMMP, LdM, JAR, and TG contributed to preparation of the manuscript. The final version of the article was approved by all the authors.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by a grant of the Dutch Organization for Health Research and Care Innovation (ZonMW; 842004005) section TopCare projects.
Supplemental material: Supplementary material for this article is available online.
References
- 1. Hu F, Jiang C, Shen J, Tang P, Wang Y. Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury. 2012;43(6):676–685. [DOI] [PubMed] [Google Scholar]
- 2. Maxwell MJ, Moran CG, Moppett IK. Development and validation of a preoperative scoring system to predict 30 day mortality in patients undergoing hip fracture surgery. Br J Anaesth. 2008;101(4):511–517. [DOI] [PubMed] [Google Scholar]
- 3. Handoll H, Parker MJ. Conservative versus operative treatment for hip fractures in adults. Cochrane Database Syst Rev. 2008;(3):CD000337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Johnell O, Kanis J. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporosis Int. 2004;15(11):897–902. [DOI] [PubMed] [Google Scholar]
- 5. Peeters CM, Visser E, Van de Ree CL, Gosens T, Den Oudsten BL, De Vries J. Quality of life after hip fracture in the elderly: a systematic literature review. Injury. 2016;47(7):1369–1382. [DOI] [PubMed] [Google Scholar]
- 6. Touwen DP. Voor een ander: beslissingsverantwoordelijkheden in de verpleeghuisgeneeskunde. Department of Ethics and Law of Health Care, Faculty of Medicine/Leiden University Medical Center (LUMC), Netherlands: Leiden University; 2008. [Google Scholar]
- 7. Furlan AD, Pennick V, Bombardier C, van Tulder M; Editorial Board, Cochrane Back Review Group. 2009 updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976). 2009;34(18):1929–1941. [DOI] [PubMed] [Google Scholar]
- 8. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 9. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Higgins J, Green S. Cochrane handbook for systematic reviews of interventions version 5.1. 0. The Cochrane Collaboration; 2011. http://www.cochrane-handbook, updated April 2017.
- 11. Cochrane Collaboration. Review Manager (RevMan) [computer program]. Version 5.2.3 Copenhagen, Denmark: The Nordic Cochrane Centre; 2014. [Google Scholar]
- 12. Beloosesky Y, Hendel D, Hershkovitz A, Skribnic G, Grinblat J. Outcome of medically unstable elderly patients admitted to a geriatric ward after hip fracture. Aging (Milano). 2001;13(2):78–84. [DOI] [PubMed] [Google Scholar]
- 13. Ishimaru D, Ogawa H, Maeda M, Shimizu K. Outcomes of elderly patients with proximal femoral fractures according to positive criteria for surgical treatment. Orthopedics. 2012;35(3):e353–e358. [DOI] [PubMed] [Google Scholar]
- 14. Jain R, Basinski A, Kreder HJ. Nonoperative treatment of hip fractures. Int Orthop. 2003;27(1):11–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ooi L, Wong T, Toh C, Wong H. Hip fractures in nonagenarians—a study on operative and non-operative management. Injury. 2005;36(1):142–147. [DOI] [PubMed] [Google Scholar]
- 16. Shabat S, Mann G, Gepstein R, Fredman B, Folman Y, Nyska M. Operative treatment for hip fractures in patients 100 years of age and older: is it justified? J Orthop Trauma. 2004;18(7):431–435. [DOI] [PubMed] [Google Scholar]
- 17. Dedovic Z, Resic TH, Vavra-Hadziahmetovic N. Mortality among third age patients with hip fracture and high cardiac risk. Med Arch. 2013;67(1):42–44. [DOI] [PubMed] [Google Scholar]
- 18. Gregory J, Kostakopoulou K, Cool W, Ford D. One-year outcome for elderly patients with displaced intracapsular fractures of the femoral neck managed non-operatively. Injury. 2010;41(12):1273–1276. [DOI] [PubMed] [Google Scholar]
- 19. Bong S, Lau H, Leong J, Fang D, Lau M. The treatment of unstable intertrochanteric fractures of the hip: a prospective trial of 150 cases. Injury. 1981;13(2):139–146. [DOI] [PubMed] [Google Scholar]
- 20. Hansen F. Conservative vs surgical treatment of impacted, subcapital fractures of the femoral neck. Acta Orthop Scand. 1994;256(9):65–69. [Google Scholar]
- 21. Hornby R, Evans JG, Vardon V. Operative or conservative treatment for trochanteric fractures of the femur. A randomised epidemiological trial in elderly patients. J Bone Joint Surg Br. 1989;71(4):619–623. [DOI] [PubMed] [Google Scholar]
- 22. Sher JL, Stevens J, Porter BB, Checketts RG. A comparison of operative and conservative treatment for unstable trochanteric fractures [abstract]. J Bone Joint Surg. 1985;67(3):495.3972875 [Google Scholar]
- 23. von Hippel PT. The heterogeneity statistic I (2) can be biased in small meta-analyses. BMC Med Res Methodol. 2015;15(1):35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Borenstein M, Hedges LV, Higgins J, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111. [DOI] [PubMed] [Google Scholar]
- 25. Xu D, Bi F, Ma C, Wen Z, Cai X. A systematic review of undisplaced femoral neck fracture treatments for patients over 65 years of age, with a focus on union rates and avascular necrosis. J Orthop Surg Res. 2017;12(1):28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. EuroQol Group. EuroQol—a new facility for the measurement of health-related quality of life. Health Policy. 1990;16(3):199–208. [DOI] [PubMed] [Google Scholar]
- 27. Coast J, Peters TJ, Natarajan L, Sproston K, Flynn T. An assessment of the construct validity of the descriptive system for the ICECAP capability measure for older people. Qual Life Res. 2008;17(7):967–976. [DOI] [PubMed] [Google Scholar]
- 28. Flynn TN, Louviere JJ, Marley AA, Coast J, Peters TJ. Rescaling quality of life values from discrete choice experiments for use as QALYs: a cautionary tale. Popul Health Metr. 2008;6(1):6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Coast J, Flynn TN, Natarajan L, et al. Valuing the ICECAP capability index for older people. Soc Sci Med. 2008;67(5):874–882. [DOI] [PubMed] [Google Scholar]
- 30. Schuurmans H, Steverink N, Lindenberg S, Frieswijk N, Slaets JP. Old or frail: what tells us more? J Gerontol A Biol Sci Med Sci. 2004;59(9):M962–M965. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.