ABSTRACT
Objective: This study aimed to determine the degree and determinants of inequality in up-to-date fully immunization (UTDFI) coverage among children of Zhejiang province, east China.
Method: We used data from the Zhejiang provincial vaccination coverage survey of 2014 and the health outcome was the UTDFI status among children aged 24–35 months. The household income per month was used as an index of socio-economic status for the inequality analysis. The concentration index (CI) was used to quantify the degree of inequality and the decomposition approach was applied to quantify the contributions from demographic factors to inequality in UTDFI coverage.
Results: The UTDFI coverage was 80.63% and the CI for UTDFI coverage was 0.12028 (95% CI: 0.10852–0.13175), indicating that immunization practice significantly favored children with relatively higher socio-economic status. The results of decomposition analysis suggested that 68.2% of the socio-economic inequality in UTDFI coverage should be explained by the mother's education level. Furthermore, factors such as birth order, ethnic group, maternal employment status, residence, immigration status, GDP per-capital and percentage of public health spending of the total health spending also could explain the disparity in UTDFI coverage.
Conclusion: There exists inequality in UTDFI coverage among the socio-economic disadvantage children. Health interventions of narrowing the socio-economic inequality in UTDFI coverage will benefit from being supplemented with strategies aimed at poverty and illiteracy reduction.
KEYWORDS: Coverage, Concentration index, Decomposition, Inequality, Up-to-date full immunization
Introduction
The expanded program on immunization (EPI) was launched since 1974, with the primary aim of reducing childhood mortality worldwide.1,2 China started EPI in 1978 with 4 vaccines and this program continues with 11 vaccines by now.3 The eradication, elimination, and significant reduction in the incidence of some childhood vaccine preventable diseases (VPDs), is one of the outstanding examples of Chinese EPI's success. All vaccines of Chinese EPI are provided free of charge and Chinese EPI aims to improve and sustain routine immunization coverage of all antigens to 90%, which is required to reach the herd immunity and interrupt the transmission for VPDs.3
The distribution of health inequality is becoming prominent since the average health indicator has been considered as an inadequate indicator of the health performance.4 Socio-economic inequalities in the childhood health indicators are major concerns in developing countries, where the gaps in these health related outcomes between the socio-economic advantage population and the disadvantage population are always large.5 Furthermore, we need not only to quantify the magnitude of the inequality, but also to identity the most vulnerable sub-population. As such, it is necessary to identity the risk factors for the relevant inequalities. Previous studies had evaluated the socio-economic inequalities in health performance through plotting the concentration curve and calculating the concentration index (CI). Furthermore, these studies had decomposed the general inequality to explore the pathways of the socio-economic inequality in childhood health.6-9
In the 2011 vaccination coverage survey of Zhejiang province, the coverage of primary vaccination was over 90% for each individual antigen among children at one year of age.10 However, we did not have the estimates on the coverage of up-to-date fully immunization (UTDFI) among children with one year of age at the provincial level. Besides, we had found there was a larger disparity in UTDFI coverage of children with different socio-economic status. For example, Yiwu city, located in the middle of Zhejiang province, had a low UTDFI coverage of 69.3% in 2011.11 We consider the inequality in vaccination coverage within the province should have a substantially negative influence on the childhood health. Therefore, assessing the inequality among socio-economic disadvantaged children is critical in developing the appropriate interventions. On the other hand, as we known, few studies have been published on attempting to decompose the inequality in UTDFI coverage to understand the related risk factors under the Chinese context.
Given this background, our study aimed to evaluate the socio-economic inequality in UTDFI coverage among the children aged 24–35 months in Zhejiang province through taking advantage of the 2014 cross-sectional vaccination survey data. Further, we attempted to decompose the inequality by quantifying the contribution attributable to both the household/individual variables and the specific variables of different cities.
Results
Totally, 2772 children aged 24–35 months were included in this study (Table 1). 50.32% of the surveyed children were male and 70.42% were first born. The majority of children were Han ethnic group. 65.87% of mothers were under 30 y of age. More than 90% of mothers had at least secondary level education. 86.76% of mothers had a fixed job. 50.87% of households were located in rural areas and 40.08% were migrant. The UTDFI coverage was 80.63% at the provincial level. In the univariate analysis, the UTDFI coverage was significantly associated with the birth order of child, the ethnic group of child, the maternal education level, the maternal employment status, the household residence, the household immigration status, and the household socio-economic status. The UTDFI coverage seemed not differ by either the sex of child or the maternal age.
Table 1.
Summary distribution of the demographic and socio-economic characteristics of children and the proportion of up-to-date fully immunized children by determinants.
| FI children |
||||
|---|---|---|---|---|
| Variables | No. of children (%) | n (%) | χ2 | p |
| Sex of child | 0.306 | 0.58 | ||
| Male | 1395(50.32) | 1119(80.21) | ||
| Female | 1377(49.68) | 1116(81.05) | ||
| Birth order of child | 25.301 | <0.01 | ||
| 1 | 1952(70.42) | 1622(83.07) | ||
| 2 | 651(23.48) | 490(75.22) | ||
| ≥ 3 | 169(6.10) | 124(73.37) | ||
| Ethnic group of child | 132.162 | <0.01 | ||
| Han | 2525(91.09) | 2104(83.34) | ||
| Others | 247(8.91) | 131(53.04) | ||
| Age of mother (years) | 0.615 | 0.433 | ||
| <30 | 1826(65.87) | 1480(81.04) | ||
| ≥ 30 | 946(34.13) | 755(79.81) | ||
| Maternal education level | 127.25 | <0.01 | ||
| No/primary | 183(6.60) | 101(55.08) | ||
| Second level | 1690(60.97) | 1328(78.60) | ||
| College level | 899(32.43) | 806(89.66) | ||
| Maternal employment status | 37.345 | <0.01 | ||
| Home fulltime | 367(13.24) | 339(92.38) | ||
| Employed | 2405(86.76) | 1896(78.84) | ||
| Residence | 19.682 | <0.01 | ||
| Urban | 1362(49.13) | 1052(77.24) | ||
| Rural | 1410(50.87) | 1183(83.92) | ||
| Immigration status | 284.96 | <0.01 | ||
| Resident | 1661(59.92) | 1484(89.35) | ||
| Migrant | 1111(40.08) | 751(67.60) | ||
| Socio-economic status | 15.645 | <0.01 | ||
| Q1 (poorest) | 924(33.3) | 713(77.12) | ||
| Q2 | 924(33.3) | 742(80.30) | ||
| Q3 (least poor) | 924(33.3) | 780(84.42) | ||
Fig. 1 showed the large disparities in the coverage of vaccine doses such as HBV1 and MCV1, with the poorer children having the lower coverage for these 2 vaccine doses. The coverage for other vaccine doses separately was consistently lower in the poorest group than those in the least poor group. Similarly, the UTDFI coverage of the poorest group (77.12%) was also lower than that of the least poor group (84.42%), with a difference of 7.3%.
Figure 1.
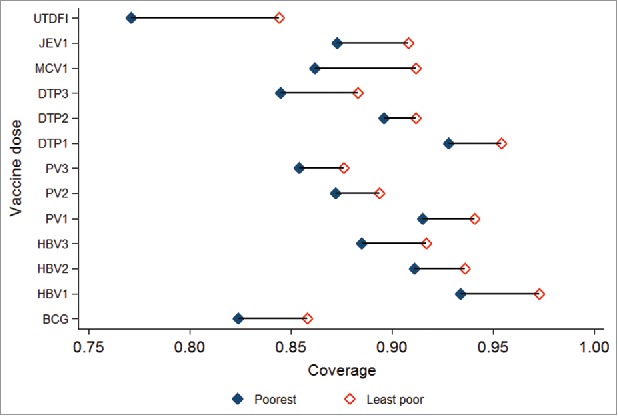
The vaccination coverage for individual vaccine dose by the socio-economic status.
The CI value was 0.12028 (95% CI: 0.10852–0.13175), which indicated that immunization practice significantly favored children with relatively higher socio-economic status (Fig. 2). Furthermore, Table 2 presented the CIs of each determinant and the contributions to the inequality in UTDFI coverage. Based on the decomposition results, the significant determinants that increased the concentration of the UTDFI coverage among the least poor group included the birth order one, the Han ethnic group, the higher maternal education level, the home fulltime mothers, living in rural areas and the resident children. Both the GDP per-capital and the percentage of the public health spending of the total health spending had positive associations with the UTDFI coverage.
Figure 2.
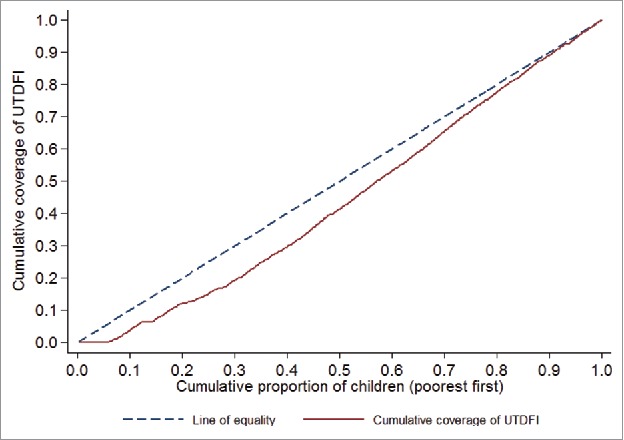
The concentration curve of inequality in the coverage of up-to-date fully immunization.
Table 2.
The concentration index and contributions of determinants to inequality in the coverage of up-to-date fully immunization.
| Variables | Level | Concentration index (95%CIa) | b | c | Contribution | % of contribution |
|---|---|---|---|---|---|---|
| Up-to-date fully immunization | - | 0.12028(0.10852:0.13175) | - | |||
| Birth order of child | ≥ 3 | Ref | ||||
| 2 | -0.05242(-0.06055:-0.043806) | 0.11526 | 0.2348 | -0.00176 | -0.69 | |
| 1 | 0.16813(0.15209:0.18122) | 0.20509 | 0.7042 | 0.03012 | 11.75 | |
| Ethnic group of child | Others | Ref | ||||
| Han | 0.22306(0.21026:0.23149) | 0.11283 | 0.9109 | 0.02843 | 11.09 | |
| Maternal education level | No/primary | Ref | ||||
| Second level | 0.32109(0.30258:0.34513) | 0.50153 | 0.6097 | 0.07564 | 29.52 | |
| College level | 0.58637(0.55977:0.60238) | 0.61027 | 0.3243 | 0.09912 | 38.68 | |
| Maternal employment status | Home fulltime | Ref | ||||
| Employed | -0.08262(-0.07271:-0.088608) | 0.08464 | 0.8676 | -0.00075 | -0.29 | |
| Residence | Urban | Ref | ||||
| Rural | 0.20651(0.19615:0.21902) | 0.18514 | 0.5087 | 0.02412 | 9.41 | |
| Immigration status | Resident | Ref | ||||
| Migrant | -0.26233(-0.24583:-0.27265) | 0.20227 | 0.4008 | -0.02638 | -10.29 | |
| GDP per-capital (CNY) | 0.00123(0.00110:0.00184) | 0.00001 | 68804.68 | 0.00105 | 0.41 | |
| % of public health spending of the total health spending | 0.12255(0.11530–0.12974) | 0.01512 | 7.41 | 0.01703 | 6.65 |
Note: a: 95% of confidence interval; b: the marginal effect of : the mean of .
Discussion
This study presents - to our knowledge - first time evidence on the composition of the socio-economic inequality in child health care in Zhejiang province in terms of not being fully immunized at the age of 12 months. Childhood immunization is considered as one of the most cost-effective public health interventions as it contributes substantial reduction of VPDs globally. For example, smallpox have been eradicated with the use of relevant vaccine. However, many developing countries including China, still face the challenge of the low vaccination coverage in the sub-population or the specific geopolitical zones, which can induce the endemic of VPDs.12,13 Using the cross-sectional survey data on immunization, this article showed a fifth of children were not fully immunized at the time point of their 12 months of age. Larger disparities in the coverage of vaccine doses were observed for HBV1 and MCV1, and the CI analysis results demonstrated that more children were fully immunized from the socio-economic advantage households. As we known, the childhood routine immunization is free of charge in Zhejiang province, which should narrow the inequality related to the socio-economic status theoretically. However, our results indicated that the socio-economic status still remained as an important determinant of the UTDFI coverage. There are several reasons for the suboptimal coverage in the socio-economic disadvantage population. First, poor people may favor to spend time on the income earning opportunities rather than on accessing the healthcare services whose benefits are difficult to tangible.11 Second, the attitude and the practice of seeking public health service may be another explanation of the inequality in UTDFI coverage.14 Third, we assume that the indirect cost is the potential obstacle of getting the vaccination, for example, the travel fee or the working time lost associated with the reception of the vaccination.3
After the decomposition analysis of the determinants of inequality in UTDFI coverage, maternal education level stood out with a contribution of 68.2%. It made the maternal education as the greatest contributor to the disparity in UTDFI coverage between the different socio-economic groups. Mother's education have been frequently considered as a determinant of child health indicators in many countries.15-21 These studies indicated that the educated mothers could be able to enhance the childhood survival through their level of education, which is not surprising in the context of Zhejiang province. In fact, we had found a strong link between mother's education and the UTDFI coverage. Therefore, addressing the inequality in UTDFI coverage will require a strong focus on increasing the educational level of mothers especially by paying attention to the disparity in the education attainment between the different socio-economic groups. Except for using the traditional education system, there is an extra necessity to establish a system that will inform the mothers on the importance of vaccination. Specifically, irrespective of the literacy status, creating the awareness on immunization among mothers or other family decision makers needs to be a core strategy for improving vaccination coverage.16
The birth order was identified as a determinant that contributed to the inequality in UTDFI coverage. Child was less likely to be fully vaccinated at the age of 12 months if the birth order was second or higher. Our finding was similar to the previous reports from Philippines22 and U.S.23 A possible explanation for this association is the allocation of the family resources, which specifically means that the parental initiative and the dedication of time in addition to the financial expense. For example, parents may be busy in looking after other younger children and be unable to find time to take the elder one to get vaccination service.
Children of other ethnic groups were more likely to be not fully immunized at the age of 12 months, which was in resonance with another study from Karachi.24 People of other ethnic groups are usually considered as the marginalized populations, and have the lower parental education and the lower socio-economic status, leading to the poor awareness on the primary health care such as immunization. Thus, a special focus is needed to increase the awareness on vaccination among the other minority ethnic groups.25
Urban location was found as a negative impact factor contributed to the inequality in UTDFI coverage. It is a new finding relative to the other published articles in this field. This finding can be summarized as the acceptability and the accessibility due to the difference in the provision methods of the public health services in the rural and the urban areas.26 Due to a better patient-doctor trust in rural areas, it is convenient for physicians to perform the health promotion and to recommend the receipt of vaccinations personally. On the other hand, due to the increasing urbanization in Zhejiang province, most physicians in the urban areas do not have enough time to explain the importance of immunization to parents. Therefore, the direct connection between the parent and the provider is lacking. These urban-rural difference in public health service system suggests that the diverse methods of health education should be implemented to close the gaps of the acceptability and the accessibility of the vaccination service.
The association between the migrant children and the suboptimal vaccination coverage have been well established in Zhejiang province.27 We assume that the migrants would face the challenges of adapting to the new sociocultural environment. However, the residents are better able to avail themselves of the immunization services, as they are familiar with the living areas.
In this study, we found increasing the proportion of the public health spending of the total health spending had translated into the improved the UTDFI coverage. This result was consistent with a previous study on the association between the public health funding and the health outcomes. Findings from Taiwan demonstrated that the disparities in appendicitis cases have narrowed due to the introduction of the national health insurance program.28 We assumed that the health service utilization, the quality of service, and the social inclusions will be improved through increasing the public health care investment.
There were several limitations for this study. First, some sensitive variables such as the monthly household income might be inaccurate under the condition of a face-to-face interview. We assumed that this bias would probably underestimate the CI value due to the socio-economic advantage people might underreport the monthly household income. Second, this study was a secondary use of the 2014 cross-sectional vaccination survey data. Hence, the variables included in our analysis might not be as comprehensive as necessary and this limitation might not be able to be addressed. Theoretically, we would miss other potential important determinants of the inequality in UTDFI coverage due to this issue. Third, data limitation might be very likely as some children could not be vaccinated due to the underlying medical conditions such as HIV infection or immunocompromise. This issue had not been accounted for in the survey and subsequent analysis, but we assumed that it would not affect the results substantially as child with such underlying conditions was very rare. Forth, the impact on our findings from the selection bias could not be ignored as the last step of the sampling procedure was not random.
Conclusions
The main policy implication of this study is that the decision-makers need to be aware of the existence of the inequality in UTDFI coverage in Zhejiang province. Health interventions of narrowing the socio-economic inequality in UTDFI coverage will benefit from being supplemented with strategies aimed at poverty and illiteracy reduction. These strategies will not only improve the vaccination coverage but also put Zhejiang province on the road to the sustainable development of EPI.
Methods
Data
This study took advantage of Zhejiang provincial vaccination coverage survey toward children aged 24–35 months (born from September 1, 2011 to August 31, 2012). It was a household-based cluster survey implemented in 2014. The sample size was obtained based on the formula as follow: . To reach the estimate of coverage at city level with a 2-tailed α error of 5% and a permissible error (d) of 0.08, assuming the expected UTDFI coverage (p) at 70% and a design effect (deff) of 2, the minimum sample size required for each city was 252 eligible children, divided in 6 clusters (towns) of 42, corresponding to 2772 children in total. The sampling procedures included 4 steps. First, 6 clusters for each city were selected from a list of all towns (with the population size) under the jurisdiction, on the basis of the probability proportional to population size. Second, one community was randomly selected from each cluster through the simple ballot from the list of all communities under the jurisdiction. Third, the index household was selected randomly from the list of all households in the selected community, by using the table of random numbers. Fourth, we selected the subsequent 41 households, by turning to the right while exiting the index household and visiting the adjacent one. Immunization data were transcribed from the immunization cards and were validated through ZJIIS (the provincial electronic immunization registry).29 Demographic and socio-economic information was collected through a pre-tested, standard questionnaire developed by Zhejiang provincial center for disease control and prevention (CDC).
Definitions
In this study, the UTDFI is defined as a child received 12 vaccine doses scheduled before 8 months of age according to the Chinese EPI. These vaccine doses include one dose of bacillus calmette-guerin vaccine (BCG) scheduled at birth, 3 doses of hepatitis B vaccine (HBV) scheduled at birth, 1 month and 6 months of age, 3 doses of diphtheria-tetanus-pertussis combined vaccine (DTP) scheduled at 3–4–5 months of age, 3 doses of polio vaccine (PV) scheduled at 2–3–4 months of age, one dose of measles containing vaccine (MCV) scheduled at 8 month of age, one dose of Japanese encephalitis vaccine (JEV) scheduled at 8 months of age. The UTDFI was defined as a binary outcome variable, namely whether each eligible child received all 12 recommended vaccination doses at the time point of the 12 months of age or not (child fully immunized = 1, child not fully immunized = 0). For the core analysis, the UTDFI was considered as a dependent variable to standardize the interpretation. The socio-economic distribution was group into tertiles on the basis of the household income per month, with the first tertile representing the poorest group and the last tertile representing the least poor group.
Two sets of independent variables were considered for the decomposition analysis. The individual/household variables included sex and birth order and ethnic group of child, education level and age of mother, maternal employment status, household socio-economic status, household resident status and household immigration status. The city specific variables included the gross domestic product (GDP) per-capital and the percentage of public health spending of the total health spending.
Analytical method
We used STATA MP version 14.0 (StataCorp. 2015, Stata statistical software, college station, TX, USA) for data analysis. The distribution of the demographic variables, the socio-economic characteristic, the UTDFI coverage, and the coverage of vaccine doses were described.
The concentration curve and the CI were applied to assess the socio-economic inequality in UTDFI coverage. The concentration curve plotted the cumulative UTDFI coverage (y-axis) against the cumulative percentage of the population. The cumulative percentage of the population was ranked by household income per months, beginning with the poorest and ending with the least poor (x-axis).30 If everyone, irrespective of the distribution of socio-economic status, had exactly the same value of the UTDFI coverage, the concentration curve would be a 45-degree line (diagonal), running from the bottom left-hand corner to the top right-hand corner. This was known as the line of equality. However, if the UTDFI coverage took higher (lower) values among the poorer, the concentration curve would lie above (below) the diagonal. The further the curve deviated the diagonal, the greater the degree of inequality.
The CI was defined as twice the area between the concentration curve and the diagonal. So, if there was no socio-economic inequality, the CI was zero. The range of CI was from -1 to +1, which occurred in the hypothetical situation where the UTDFI coverage was concentrated in the least poor group or the poorest group, respectively. Thus, the greater negative value of the CI, the more the absence of the UTDFI coverage concentrated among the poor. The formula of computation of the CI was as follow: , where h was the UTDFI coverage variable, μ was its mean, and was the fractional rank of the individual, with i = 1 for the most socio-economic disadvantage child and i = N for the least one.
A method of decomposing the health sector inequalities into the contributions of risk factors has been proposed.31 In this study, the logistic regression was adopted since the health sector (the UTDFI coverage) was a binary variable according to the formula: , where was the logistic of the predicted probability of being fully immunized, and was the logistic regression coefficient for the risk factor , and was the residual. Only the variables significantly associated with the UTDFI coverage in the univariate analysis (χ2 test) were included in the logistic regression and we used a p value of < 0.1 as a screening criterion for the variable selection. Given the relationship above, the CI could be re-written as: , where μ was the mean of the UTDFI coverage, was the mean of the , was the CI of the (defined analogously to CI). was the marginal effect between the risk factor and the probability of the UTDFI, where was the logistic density function. meant the average change in the probability of the UTDFI when the relevant risk factor changed one unit. was the generalized CI of the residual (), which was computed as follow: . was the contribution in percentage of the CI. The 5-step “bootstrap” procedure was applied to obtain the standard errors (SE) of the CI.
Ethical considerations
This study was approved by the ethical review board of Zhejiang provincial CDC. Written informed consent was obtained from a parent or a legal caregiver of each eligible child enrolled in this study.
Disclosure of potential conflicts of interest
The authors declare no conflicts of interest.
Acknowledgments
The authors would like to thank the immunization staff from 11 CDCs at city level for their investigation and data collection.
Author contributions
Yu Hu conceived and designed the experiments; Yaping Chen performed the experiments; Yu Hu and Ying Wang analyzed the data; Ying Wang contributed reagents/materials/analysis tools; Yu Hu wrote the paper.
References
- [1].Okwo-Bele JM, Cherian T. The expanded programme on immunization: a lasting legacy of smallpox eradication. Vaccine 2011; 29 Suppl 4:D74–9; PMID:22486980; https://doi.org/ 10.1016/j.vaccine.2012.01.080 [DOI] [PubMed] [Google Scholar]
- [2].John TJ, Plotkin SA, Orenstein WA. Building on the success of the Expanded Programme on Immunization: enhancing the focus on disease prevention and control. Vaccine 2011; 29:8835–7; PMID:21971446; https://doi.org/ 10.1016/j.vaccine.2011.08.100 [DOI] [PubMed] [Google Scholar]
- [3].Hu Y, Luo S, Tang X, Lou L, Chen Y, Guo J. Comparative assessment of immunization coverage of migrant children between national immunization program vaccines and non-national immunization program vaccines in east China. Hum Vaccin Immunother 2015:11(3):761–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Frenk J. The World Health Report 2000: expanding the horizon of health system performance. Health Policy Plan 2010; 25:343–5. [DOI] [PubMed] [Google Scholar]
- [5].Kruk ME, Prescott MR, de Pinho H, Galea S. Equity and the child health Millennium Development Goal: the role of pro-poor health policies. J Epidemiol Commun Health 2011; 65:327–33; PMID:20724284; https://doi.org/ 10.1136/jech.2009.096081 [DOI] [PubMed] [Google Scholar]
- [6].Lauridsen J, Pradhan J. Socio-economic inequality of immunization coverage in India. Health economics review 2011; 1:11; PMID:22828353; https://doi.org/ 10.1186/2191-1991-1-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Hong R, Chhea V. Trend and inequality in immunization dropout among young children in Cambodia. Mater Child Health J 2010; 14:446–52; PMID:19350375; https://doi.org/ 10.1007/s10995-009-0466-1 [DOI] [PubMed] [Google Scholar]
- [8].Egondi T, Oyolola M, Mutua MK, Elung'ata P. Determinants of immunization inequality among urban poor children: evidence from Nairobi's informal settlements. Int J Equity Health 2015; 14:24; PMID:25889450; https://doi.org/ 10.1186/s12939-015-0154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Wagstaff A. The bounds of the concentration index when the variable of interest is binary, with an application to immunization inequality. Health Economics 2005; 14:429–32; PMID:15495147; https://doi.org/ 10.1002/hec.953 [DOI] [PubMed] [Google Scholar]
- [10].Hu Y, Chen Y, Guo J, Tang X, Shen L. Completeness and timeliness of vaccination and determinants for low and late uptake among young children in eastern China. Hum Vaccin Immunother 2014; 10:1408–15; https://doi.org/ 10.4161/hv.28054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hu Y, Li Q, Chen E, Chen Y, Qi X. Determinants of childhood immunization uptake among socio-economically disadvantaged migrants in East China. Int J Environ Res Public Health 2013; 10:2845–56; PMID:23839061; https://doi.org/ 10.3390/ijerph10072845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hu Y, Luo S, Tang X, Lou L, Chen Y, Guo J, Zhang B. Does introducing an immunization package of services for migrant children improve the coverage, service quality and understanding? An evidence from an intervention study among 1548 migrant children in eastern China. BMC Public Health 2015; 15:664; PMID:26173803; https://doi.org/ 10.1186/s12889-015-1998-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Wagner AL, Zhang Y, Montgomery JP, Ding Y, Carlson BF, Boulton ML. Timely measles vaccination in Tianjin, China: a cross-sectional study of immunization records and mothers. BMC Public Health 2014; 14:888; PMID:25168663; https://doi.org/ 10.1186/1471-2458-14-888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Egondi T, Oyolola M, Mutua MK, Elung'ata P. Determinants of immunization inequality among urban poor children: evidence from Nairobi's informal settlements. Int J Equity Health 2015; 14:24; PMID:25889450; https://doi.org/ 10.1186/s12939-015-0154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Onsomu EO, Abuya BA, Okech IN, Moore D, Collins-McNeil J. Maternal Education and Immunization Status Among Children in Kenya. Mater Child Health J 2015; 19:1724–33; PMID:25636652; https://doi.org/ 10.1007/s10995-015-1686-1 [DOI] [PubMed] [Google Scholar]
- [16].Ding Y, Hay J. Impact of Maternal Education on Child Immunization Propensity in China. Value Health 2014; 17:A724–5; PMID:27202575; https://doi.org/ 10.1016/j.jval.2014.08.043 [DOI] [PubMed] [Google Scholar]
- [17].Vikram K, Vanneman R, Desai S. Linkages between maternal education and childhood immunization in India. Soc Sci Med 2012; 75:331–9; https://doi.org/ 10.1016/j.socscimed.2012.02.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Usman HR, Rahbar MH, Kristensen S, Vermund SH, Kirby RS, Habib F, Chamot E. Randomized controlled trial to improve childhood immunization adherence in rural Pakistan: redesigned immunization card and maternal education. Trop Med Int Health 2011; 16:334–42; https://doi.org/ 10.1111/j.1365-3156.2010.02698.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Abuya BA, Onsomu EO, Kimani JK, Moore D. Influence of maternal education on child immunization and stunting in Kenya. Mater Child Health J 2011; 15:1389–99; PMID:20848172; https://doi.org/ 10.1007/s10995-010-0670-z [DOI] [PubMed] [Google Scholar]
- [20].Racine AD, Joyce TJ. Maternal education, child immunizations, and public policy: evidence from the US National Immunization Survey. Social Sci Med 2007; 65:1765–72; https://doi.org/ 10.1016/j.socscimed.2007.06.004 [DOI] [PubMed] [Google Scholar]
- [21].Streatfield K, Singarimbun M, Diamond I. Maternal education and child immunization. Demography 1990; 27:447–55; PMID:2397822; https://doi.org/ 10.2307/2061378 [DOI] [PubMed] [Google Scholar]
- [22].Bondy JN, Thind A, Koval JJ, Speechley KN. Identifying the determinants of childhood immunization in the Philippines. Vaccine 2009; 27:169–75; PMID:18789997; https://doi.org/ 10.1016/j.vaccine.2008.08.042 [DOI] [PubMed] [Google Scholar]
- [23].Anderson LM, Wood DL, Sherbourne CD. Maternal acculturation and childhood immunization levels among children in Latino families in Los Angeles. Am J Public Health 1997; 87:2018–21; PMID:9431295; https://doi.org/ 10.2105/AJPH.87.12.2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Siddiqui NT, Owais A, Agha A, Karim MS, Zaidi AK. Ethnic disparities in routine immunization coverage: a reason for persistent poliovirus circulation in Karachi, Pakistan? Asia-Pacific journal of public health / Asia-Pacific Academic Consortium for Public Health 2014; 26:67–76; ; https://doi.org/ 10.1177/1010539513475648 [DOI] [PubMed] [Google Scholar]
- [25].Orr N, Elliott MN, Burkhart Q, Haviland A, Weinick RM. Racial/Ethnic differences in Medicare experiences and immunization: the role of disease burden. Medical Care 2013; 51:823–31; PMID:23807592; https://doi.org/ 10.1097/MLR.0b013e31829c8d77 [DOI] [PubMed] [Google Scholar]
- [26].Lv M, Fang R, Wu J, Pang X, Deng Y, Lei T, Xie Z. The free vaccination policy of influenza in Beijing, China: The vaccine coverage and its associated factors. Vaccine 2016; 34:2135–40; PMID:26917011; https://doi.org/ 10.1016/j.vaccine.2016.02.032 [DOI] [PubMed] [Google Scholar]
- [27].Hu Y, Chen Y, Guo J, Tang X, Shen L. Completeness and timeliness of vaccination and determinants for low and late uptake among young children in eastern China. Human Vaccin Immunother 2014; 10:1408–15; https://doi.org/ 10.4161/hv.28054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Huang N, Yip W, Chang HJ, Chou YJ. Trends in rural and urban differentials in incidence rates for ruptured appendicitis under the National Health Insurance in Taiwan. Public Health 2006; 120:1055–63; PMID:17011602; https://doi.org/ 10.1016/j.puhe.2006.06.011 [DOI] [PubMed] [Google Scholar]
- [29].Li Q, Hu Y, Zhong Y, Chen Y, Tang X, Guo J, Shen L. Using the Immunization Information System to Determine Vaccination Coverage Rates among Children Aged 1-7 Years: A Report from Zhejiang Province, China. Int J Environ Res Public Health 2014; 11:2713–28; PMID:24603495; https://doi.org/ 10.3390/ijerph110302713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Heckley G, Gerdtham UG, Kjellsson G. A general method for decomposing the causes of socioeconomic inequality in health. J Health Econ 2016; 48:89–106; PMID:27137844; https://doi.org/ 10.1016/j.jhealeco.2016.03.006 [DOI] [PubMed] [Google Scholar]
- [31].Ataguba JE, Ojo KO, Ichoku HE. Explaining socio-economic inequalities in immunization coverage in Nigeria. Health Policy Plan 2016; 31:1212–24; PMID:27208896; https://doi.org/ 10.1093/heapol/czw053 [DOI] [PubMed] [Google Scholar]


