Abstract
Objective
Because little is known about promising interventions to prevent and control chronic disease in Korean Americans, we conducted a systematic literature review to investigate: (1) theoretical frameworks and strategies employed by interventions targeting Korean Americans; (2) cultural factors considered by these interventions; and (3) the extent of their success in engaging Korean participants and improving their health.
Design
Following the PRISMA guidelines, PubMed, PsycInfo, and Web of Science were searched to identify primary research articles evaluating interventions to prevent or control chronic disease, tailored to Korean Americans, and published from 1980 through 2011. Of 238 articles identified, 21 articles describing16 unique intervention tests met inclusion criteria. These interventions targeted cancer (10), hypertension (2), diabetes (1), mental health (1), tobacco cessation (1), and general health (1).
Results
All included studies were published since 2000, reflecting the relatively recent establishment of intervention research with Korean Americans. All 16 programs delivered linguistically appropriate messages and education. The 11 programs that realized significant intervention effects also provided or coordinated social support from culturally relevant and well-trained lay health workers, nurses, or family members during an intervention and/or follow-up period.
Conclusions
Culturally matched and linguistically appropriate messages and education may not be enough to prevent or control chronic disease among immigrant Korean Americans. Culturally sensitive and committed social support should be provided to catalyze behavioral changes and sustain the effect of the interventions.
Keywords: Asian Americans, cultural competency, health promotion, immigrants, patient navigation, social support
Introduction
Korean Americans are a rapidly growing ethnic group in the United States (USA). The number of Americans with Korean ancestry has increased from fewer than 70,000 in 1970 to more than 1.1 million in 2000, representing 0.3% of the total US population (APIAHF 2006). Today, Korean Americans are the fifth-largest Asian American ethnic group in the USA. Of that population, about 65% are first-generation (Korea-born) immigrants (APIAHF 2011). Most studies of Koreans in the USA interchangeably use the terms, Korean Americans and Korean American immigrants. The present review uses Korean Americans to include both groups.
Overall, immigrants are one of the most vulnerable populations in the context of public health (Aday 2002). Previous research has shown that immigrants arrive in the USA with generally better health than US citizens (Frisbie et al. 2001). However, immigrants have a propensity to gain weight and develop chronic diseases as they adopt a more westernized diet and sedentary lifestyle (Abate and Chandalia 2003). Associations have been found between the adoption of a more sedentary lifestyle and westernized dietary habits and the increasing prevalence of overweight and obesity-related illnesses such as cardiovascular and coronary artery disease, colon cancer, and Type 2 diabetes among Korean Americans (Cho and Juon 2006; Hofstetter et al. 2008). About 34% of Korean Americans lack health insurance, almost 2.5 times higher than the rate among non-Latino whites (14%), so visit doctors significantly less than their counterparts in Korea (APIAHF 2006). A considerable number of Korean Americans suffer not only from chronic diseases, but also from a loss of self-confidence, social deprivation, and depression stemming from cultural and English language barriers (Sohn 2004). An estimated 90% of first-generation Korean immigrant adults speak Korean only, and 70% have trouble understanding medical terminology, even when the materials have been translated into Korean (Kim et al. 2009).
To reduce health disparity gaps for this vulnerable population, a growing number of interventions targeting Korean Americans have been implemented. Many of the interventions are culturally tailored to incorporate elements from Korean culture to increase their attractiveness and appropriateness. In work with African-Americans, Resnicow et al. (1999) conceptualized two primary dimensions of cultural appropriateness of interventions – surface structure and deep structure. Surface structure refers to the tailoring of external intervention components – such as materials, communication channels, settings, staff, and recruitment strategies – to reflect the characteristics of a target population. In educational materials, for example, surface structure may relate to the display of people, places, language, music, foods, brand names, locations, and clothing that are familiar to and preferred by the target audience. The second dimension, deep structure, acknowledges that cultural, social, historical, environmental, and psychological forces may influence health behavior differently across a diverse racial/ethnic population. This dimension reflects a deep understanding of culturally normative practices and beliefs embedded in the target population, rather than just its outward appearance.
Surface structure increases the receptivity or acceptance of messages, whereas deep structure conveys salience (Resnicow et al. 1999). Researchers have argued that surface structure establishes the feasibility of a program, whereas deep structure determines its effectiveness. While the two structures can be differentiated by the depth of their characteristics, they also somewhat overlap. For example, surface characteristics such as communication styles and music preferences may reflect inner cultural values, which are classified as deep structure. Nevertheless, the theoretical distinction is useful in examining the specific elements that make an intervention effective.
To date, little is known about effectiveness of interventions targeting Korean Americans, and even less is known about culturally appropriate intervention delivery factors that may be effective in this population. To consolidate this research, this systematic review examined interventions to control chronic disease in Korean Americans to identify: (1) theory guiding these interventions; (2) if formative research was used to guide intervention development; (3) how Korean culture was reflected, for example, through deep and surface structures; and (4) how successfully the interventions engaged Korean participants and improved health. This elucidation of the theory, formative research, cultural reflections, and outcomes of successful interventions can inform public health policy-making, intervention design, and clinical recommendations to the benefit of Korean Americans.
Method
Search strategies
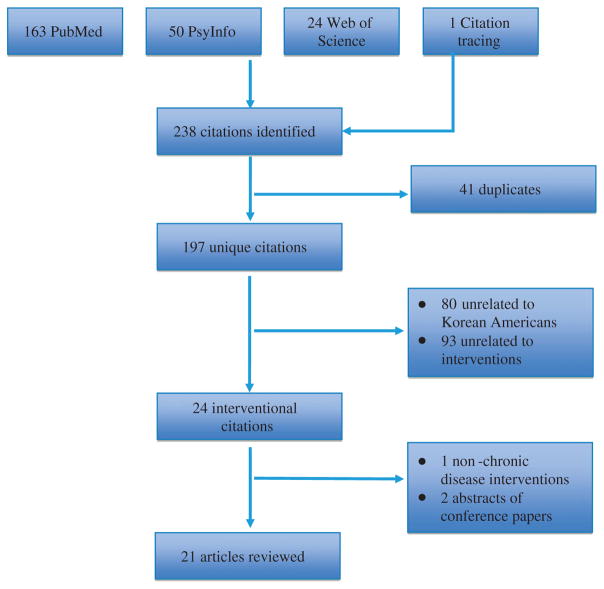
Articles were identified by searching the PubMed, Web of Science, and PsycInfo databases for articles dated from January 1980 through November 2011. Keywords used in various combinations included Korean immigrant, Korean American, intervention, health education program, and evaluation. Inclusion criteria were: (1) a primary research article that reports on the testing of intervention strategies tailored to Korean American adults (both immigrants and non-immigrants) for the treatment or prevention of chronic disease; (2) study conducted in the USA; (3) publication in English; and (4) study reported in a peer-reviewed journal. An initial search of the databases, followed by citation tracing, yielded 238 potentially eligible articles. The abstracts of these articles were reviewed, and 197 unique remained after removing 41 duplicates. A further 173 were eliminated because 80 were not related to Korean American populations and 93 did not report on an intervention. Finally, one article was excluded because it did not relate to treatment or control of chronic disease, and two were excluded because they were the abstracts of the conference proceedings, rather than full research articles. This paper presents a review of the 21 eligible articles. Figure 1 shows the flowchart of the process of inclusion of eligible studies for the present review, based on the PRISMA Guidelines (Moher et al. 2009).
Figure 1.
Study selection with flow based on the PRISMA 2009 guidelines.
Analysis framework
The interventions besides being reviewed for intervention component (including theoretical grounding), evaluation approach, and outcomes were also examined in terms of their cultural tailoring. Specifically, we looked for five reflections of surface structures: (1) materials (materials and messages designed for education sessions or counseling); (2) communication channels (how materials or messages are delivered); (3) settings (venues for delivering materials and messages and recruiting participants); (4) staff (culturally relevant recruiters and educators); and (5) recruitment strategies (methods for recruiting participants). We also looked for two reflections of deep structure: (1) provision of social support by lay community workers, educators, counselors, or family members during the intervention period or follow-up period; and (2) incorporation of cultural contextualization in educational materials and sessions (e.g., reflection/immersion of deep cultural beliefs, norms, and values in the message process of the interventions). Finally, interventions were examined for use of formative research in their design, which is especially useful in designing culturally tailored interventions. Qualitative research and discussions with indigenous community members can provide insights into cultural characteristics and reveal community priorities relating to attitudes, beliefs, and behaviors. The combined use of formative research and the cultural sensitivity structures may explain how and why certain intervention components and approaches are more effective than others for a specific population.
To understand which intervention components for Korean Americans were most effective, we examined associations between the level of ‘success’ of the intervention and the use of formative research, surface structure, and deep structure. For this review, the effectiveness of interventions was determined by assessing whether the findings of each study were consistent with the study’s proposed primary hypotheses or the research questions related to behavioral changes and were statistically significant. Even though it is not plausible to draw statistical relationships between each intervention components and its effectiveness due to the limitation of literature review, the descriptive trend will be informative for researchers to identify useful components in their future interventions.
Results
Overview of study characteristics
All 21 articles were published since 2000, reflecting the relatively recent establishment of intervention research with Korean Americans. Several interventions were the subject of multiple articles, and they were reviewed together. For example, Han et al. (2010) and Kim et al. (2008, 2011) reported on the same Self-Help Intervention Program for High Blood Pressure (SHIP-HBP). Another study by Kim et al. (2006) reported on SHIP-HBP, but it was a quasi-experimental pilot study of SHIP-DM involving different participants, so was considered separately. Two articles relating to diabetes management were considered as one intervention because they reported on different outcomes for the same participants in the same intervention study (Kim et al. 2009; Song et al. 2010). Similarly, two articles reporting on different aspects of the same chronic mental illness intervention were regarded as one (Shin and Lukens 2002; Shin 2004). Although two articles (Kim and Menon 2009; Kim et al. 2010) tested the same intervention program (‘Go Early’), the articles were considered as separate intervention tests because they reported on studies that had different participants, study periods, and designs. However, two intervention articles for promoting a breast and cervical cancer screening program (‘Health is Strength’) were regarded as one study despite the recruitment of different participants during different study periods because the former article was considered as an interim assessment study for the latter article (Moskowitz et al. 2007; Wismer et al. 2001). Thus, data are presented for 16 unique intervention tests.
Shown in Table 1 for each intervention are its focus, study population, study location, theoretical framework, program design (and duration), outcome variables, and measurement tools used in evaluation (Table 1). With regard to intervention focus, 10 interventions focused on cancer screening, 2 on hypertension, 1 on diabetes, 1 on chronic mental illness, 1 on smoking cessation, and 1 on general health. With regard to testing, five interventions were tested by randomized controlled trial (RCT), nine using a quasi-experimental, nonequivalent group, pre-/posttest design, one was tested by a cross-sectional, two-group pre-/interim-/posttest design, and one was tested using a one-group, pre-post design. Nine interventions were conducted on the East Coast of the USA (Maryland-DC, New York, and Pennsylvania), five were conducted on the West Coast (California and Washington), and two were conducted in the Midwest (Illinois). As for study participants, six articles clearly mentioned that their participants were first-generation Korean immigrants (Fang et al. 2007; Maxwell et al. 2010; Kim et al. 2006, 2009; Sin et al. 2005; Song et al. 2010), whereas the other articles just mentioned that they recruited Korean Americans.
Table 1.
Overview of study characteristics.
| No. | Author, year | State | Study population (n) | Area | Theory/ approach | Design | Duration | Outcome measures | Measurement tools |
|---|---|---|---|---|---|---|---|---|---|
| Cancer screening | |||||||||
| 1 | Fang et al. (2007) | MD | KA women (102) | Cervical cancer screening | HBM and SCT | Quasi-experimental, pre-posttest, intervention/control | 2-hr session and patient navigation, 6-mo follow-up | Psychosocial variables (perceived risk, benefits, barriers, self-efficacy) | Telephone interview |
| 2 | Han et al. (2009) | MD | KA women (93) | Breast cancer screening | TTM and HBM, CBPR | Quasi-experimental, pre-posttest | 2-hr session, 6-mo Lay Health Workers follow-up counseling, 6-mo follow-up | Breast cancer knowledge, perceived susceptibility, benefits and barriers, modesty and utilization of oriental medicine, receipt of a mammogram, Clinical Breast Examination and Breast Self-Examination | Interview |
| 3 | Juon et al. (2006) | MD | KA women (200) | Breast cancer screening | TTM | Quasi, pre-posttest, intervention/control | 90-min session, 6-mo follow-up | Intention, perceived pros and cons, decision balance, knowledge | Follow-up phone interview |
| 4 | Kim and Menon (2009) | IL | KA women (300) | Breast cancer screening | TTM and HBM | Quasi-experiment, pre-posttest, three groups (precontemplate, contemplate, relapse) | 45-min session, 6-wk follow-up | Knowledge, beliefs, stages of readiness for mammography use | Questionnaire |
| 5 | Kim et al. (2010) | IL | KA women (180) | Breast cancer screening | TTM and HBM | Quasi-experiment, pre-posttest, intervention/ control | 45-min session, 16 and 24-wk follow-up | Knowledge, beliefs, stages of readiness for mammography use | Questionnaire |
| 6 | Kim and Sarna (2004) | CA | KA women (141) | Breast cancer screening | PRECEDE/ PROCEED model, CBPR | Quasi-experiment, pre-posttest, three groups (peer group education and low-cost mammography/low-cost mammography alone/control) | 1-hr session, 2-mo follow-up | Mammography use, attitudes, knowledge | Questionnaire |
| 7 | Maxwell et al. (2008) | CA | KA women (656) | Breast cancer screening | HBM and TRA/TPB | Quasi-experimental, pre-post, intervention/ control | Mailed print intervention, 3-mo follow-up | Reach, acceptability of intervention, repeated screening | Clinical records |
| 8 | Maxwell et al. (2010) | CA | KA women at risk (176) | Breast cancer screening | HBM | RCT, pre-posttest, intervention/control | Peer navigation, 6-mo follow-up | Completion of follow-up exam | Telephone survey (pre), questionnaire (post) |
| 9 |
Wismer et al.
(2001) Moskowitz et al. (2007) |
CA | KA women (818 in 1994; 724 in 1997; 1084 in 2002) | Breast and cervical cancer screening | PRECEDE/ PROCEED model and community sensitivity research principles | Quasi-experimental, pre-, interim-, and post-intervention, cross-sectional | A 45 min. workshop, health counselor, 4-yr follow-up | Screening frequencies and differences over time, community intervention program exposure | Telephone survey |
| 10 | Ma et al. (2009) | PA | KA (167) | Colorectal cancer screening | HBM and SCT, CBPR | Quasi-experiment, pre-posttest, intervention/ control | 2-hr, 6-wk sessions, post-intervention and 12-mo follow-up | Knowledge, HBM variables, screening behavior | Questionnaire and verified in the physician’s office |
| Chronic disease | |||||||||
| 11 | Kim et al. (2006) | MD-DC | Hyper-tensive KA seniors (31) | Hyper-tension | Learned resource-fullness model and CBPR | Quasi-experiment, pre-posttest | 2-hr, 6-wk sessions, 6-mo follow-up | Knowledge, adherence to HBP therapy, BP, quality of life | Interview and transmitted monitoring of BP |
| 12 | Kim et al. (2008) | MD-DC | Hyper-tensive KA (380) | Hyper-tension | Learned resource-fullness model and CBPR | RCT, Pre-posttest, intervention (mail education)/control (in-class) | 2-hr, 6-wk sessions, 3-mo follow-up | BP, belief, knowledge, self-efficacy, medical adherence | Interview and transmitted monitoring of BP |
| Han et al. (2010) | MD-DC | Hyper-tensive KA (360) | Hyper-tension | Learned resource-fullness Model and CBPR | RCT, Pre-posttest, intervention (bi-weekly)/control (monthly) | After 6-wk sessions, 12-mo. telephone counseling, 15-mofollow-up | Success rates in telephone outreach, adherence to medication, smoking, alcohol consumption, exercise | Interview and transmitted monitoring of BP | |
| Kim et al. (2011) | Hyper-tensive KA (359) | BP, belief, knowledge, self-efficacy, medical adherence, depression | Questionnaire and transmitted monitoring of BP | ||||||
| 13 | Song et al. (2010) | MD-DC | KA (79) | Diabetes | CBPR | RCT pilot, pre-posttest, intervention/ control | Two 2-hr nutrition sessions out of 6-wk sessions, 18-and 30-wk follow-up | Nutrition knowledge, satisfaction | Questionnaire |
| Kim et al. (2009) | 2-hr 6-wk sessions, home glucose monitoring, 24-wk telephone counseling, 18-and 30-wk follow-up | A1C level, psychosocial variables (knowledge, self-efficacy, self-care activities, depression, diabetes-related quality of life) | Questionnaire and transmitted monitoring | ||||||
| Chronic mental illness | |||||||||
| 14 | Shin and Lukens (2002) | NY | KA with Schizophrenia (48) | Schizophrenia | Not mentioned | RCT, pre-posttest, intervention/control | 90-min, 10-wk sessions, weekly individual supportive sessions | Psychiatric symptoms, attitudes and coping skills | Questionnaire |
| Shin (2004) | SCT, family systems theory, Stress theory | Stigma, devaluation, family empowerment, coping skills | |||||||
| Tobacco cessation | |||||||||
| 15 | Fang et al. (2006) | PA | KA and Chinese smokers (66) | Smoking cessation | Cognitive-social health information processing model | RCT, pre-posttest, intervention/control | A 90–120 min. session, 1-wk, 1-mo, 3-mo follow-up | Health beliefs, self-efficacy, smoking cessation rates, distress | Telephone survey |
| General health | |||||||||
| 16 | Sin et al. (2005) | WA | KA seniors (13) | Physical activity | Quality health outcome model | Non-experimental, pre-posttest | Three times weekly, 50-min session for 12 wks, post-intervention follow-up | Health outcomes (Arm curl test, 8-foot-UP-and-Go test, BP), satisfaction | Program log and test |
Guiding theory
All 16 interventions were guided by theoretical foundations and/or known research approaches, and eight interventions mentioned more than one guiding theory and/or model (Table 1). Eight studies were guided by individual-level theory, including the Health Belief Model (HBM) and the Transtheoretical Model (TTM) alone or in combination (Fang et al. 2007; Han et al. 2009; Kim and Menon 2009; Kim et al. 2010; Juon et al. 2006; Ma et al. 2009; Maxwell et al. 2008, 2010). Of these, several also were guided by other models, for example, HBM plus the Theory of Planned Behavior (TPB) guided one study to promote cancer screening (Maxwell et al. 2008), and HBM and the Social Cognitive Theory (SCT) guided two studies to promote cancer screening (Fang et al. 2007; Ma et al. 2009). The Learned Resourcefulness Model guided two interventions in the area of chronic disease management (Han et al. 2010; Kim et al. 2006, 2008, 2011). Stress Theory in combination with SCT and Family Systems Theory directed the intervention related to chronic mental illness (Shin 2004; Shin and Lukens 2002). The Cognitive-Social Health Information Processing Model guided a study related to tobacco cessation (Fang et al. 2006). Community-based Participatory Research (CBPR) guided two studies (Kim et al. 2009; Song et al. 2010; Kim and Sarna 2004), community-sensitive research principles directed one study (Moskowitz et al. 2007; Wismer et al. 2001), and the Quality Health Outcome Model guided one study (Sin et al. 2005).
Basing the intervention on a theory of behavior change did not necessarily mean that the intervention yielded findings that supported the hypothesized changes in knowledge, attitudes, and behaviors. Of the 16 interventions based on theoretical frameworks, 11 were successful and five were not.
In summary, theoretical frameworks or research approaches guided all interventions reviewed in this study. Individual-level or/and interpersonal-level theories guided 12 interventions, and community-level approaches guided four interventions. Interpersonal-level theory (SCT) was always used in combination with individual-level theory in the reviewed interventions, and often it was only the concept of self-efficacy that was operationalized from SCT. These trends revealed that interventional activities targeting Korean Americans have concentrated more on trying to change people (individual-level or/and interpersonal-level) than on changing the environment (community or policy-level). Researchers suggest that multi-level theory is the most powerful approach to increase the effectiveness of interventions aiming to help people change behavior (Glanz, Rimer, and Viswanath 2008).
Use of formative research
Twelve interventions specifically reported using formative research methods (e.g., using focus groups and in-depth interviews) to guide intervention design (Table 2), while four did not. Formative research was reported as an operational strategy, to help researchers and practitioners avoid various pitfalls in developing a program and its delivery and evaluation strategies.
Table 2.
Association between culturally sensitive components of interventions and outcomes.
| No. | Author, year | Formative research | Surface structure |
Deep structure |
Significant results | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Material | Channel | Setting | Staff | Sensitive recruitment | Social support | Cultural value | ||||
| Cancer screening | ||||||||||
| 1 | Fang et al. (2007) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| 2 | Han et al. (2009) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 3 | Juon et al. (2006) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 4 | Kim and Menon (2009) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| 5 | Kim et al. (2010) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| 6 | Kim and Sarna (2004) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 7 | Maxwell et al. (2008) | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | ||
| 8 | Maxwell et al. (2010) | ✓ | ✓ | ✓ | ✓ | ✓ | N/A | ✓ | ✓ | ✓ |
| 9 | Moskowitz et al. (2007) [Wismer et al. (2001)] | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| 10 | Ma et al. (2009) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Chronic disease | ||||||||||
| 11 | Kim et al. (2006) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 12 |
Kim et al.
(2008) Han et al. (2010) Kim et al. (2011) |
✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| 13 |
Song et al.
(2010) Kim et al. (2011) |
✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ |
| Chronic mental illness | ||||||||||
| 14 |
Shin and
Lukens (2002) Shin (2004) |
✓ | N/A | N/A | ✓ | N/A | ✓ | ✓ | ✓ | |
| Tobacco cessation | ||||||||||
| 15 | Fang et al. (2006) | ✓ | ✓ | N/M | ✓ | ✓ | ✓ | |||
| General health | ||||||||||
| 16 | Sin et al. (2005) | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
Note: N/A: not available and N/M: not mentioned.
Among the 10 cancer-focused interventions, 9 interventions included formative research, and 6 interventions were successful. For example, Han et al. (2009) conducted weekly community-academic partner team meetings at the Korean Resource Center to explore and understand social and cultural contexts in developing their successful breast cancer screening intervention. Juon et al. (2006) conducted eight focus groups with breast cancer survivors and family members with cancer experience to identify reasons for not having annual screenings (which included beliefs of low risk of getting breast cancer, confidence in their health, lack of knowledge of cancer screening guidelines, misconceptions of family history, no time, and no insurance), and these were addressed in a photo-novel, to promote breast cancer screening. Focus group members also were involved in designing and pretesting of the photo-novel, and in the evaluation of this intervention, which was found to be successful. Kim and Menon (2009) and Kim et al. (2010) modified the graphics, including font size, slide color, and pictures of the educational contents corresponding to the focus group discussions prior to implementation of their breast cancer screening intervention, which was not successful in changing participant behaviors. Kim and Sarna (2004) were informed by a women’s advisory committee throughout all phases of their successful breast cancer screening study. Maxwell et al. (2008) conducted one-on-one, semi-structured, in-depth interviews with Korean American women who had received one or more mammograms through the National Breast and Cervical Cancer Early Detection Program (NBCCEDP) at a community clinic to gain an initial understanding of the barriers and motivations of regular screening. In addition, researchers conducted focus groups with Korean American clinic staff and Korean American women to develop print intervention materials for promoting breast cancer screening. Wismer et al. (2001) and Moskowitz et al. (2007) worked closely with the Korean Community Advisory Board, which engaged in developing their breast and cervical cancer screening intervention (not successful). Ma et al. (2009) conducted several focus groups prior to implementation of their colorectal cancer screening intervention (successful).
All phases of successful interventions to reduce hypertension reported by Kim et al. (2006, 2008, 2011) and Han et al. (2010) were informed by focus groups and in-depth interviews with key informants. This research helped to identify Korean Americans needs, priorities, and barriers in health behaviors, as well as to engage community members in program development and evaluation. Interventions focused on chronic mental illness (successful), tobacco cessation (not successful), and general health (successful) were not informed by formative research.
In summary, 12 of the 16 studies designed their interventions based on formative research. Of these, eight were successful and four were not. At the same time, three interventions that were not based on formative research were successful. Based on this evidence, it does not appear that gathering formative data necessarily guarantees intervention success.
Cultural tailoring
All the studies described their interventions and highlighted ways in which they were culturally tailored for Korean Americans. As shown in Table 2, all 16 interventions included components of culturally tailored interventions supported by all five tenets of surface structure. For example, they all offered bilingual material and staff and used culturally appropriate communication channels and settings to deliver the intervention. A total of 13 interventions used culturally sensitive recruiting methods, while the other three interventions included participants who were recruited from a pool of clinical records or at clinics. Looking at deep structure, all 16 reflected deep cultural values.
However, only 11 of the reviewed interventions also reflected the second tenets of deep structure – social support – during the intervention and/or follow-up period (Fang et al. 2007; Han et al. 2009, 2010; Juon et al. 2006; Ma et al. 2009; Maxwell et al. 2010; Kim et al. 2006, 2008, 2009, 2011; Shin 2004; Shin and Lukens 2002; Sin et al. 2005; Song et al. 2010; Kim and Sarna 2004). Purveyors of social support included bilingual and/or bicultural lay health workers, nurses, nutritionists or family members. In general, these individuals assisted participants to access healthcare systems, understand health education, manage emotional conflicts, and adhere to targeted health behaviors. In studies promoting cancer screening, five interventions reported that well-trained lay health workers or navigators also arranged appointments and transportation and helped with paperwork and language translation (Fang et al. 2007; Han et al. 2009; Juon et al. 2006; Maxwell et al. 2010; Ma et al. 2009). Another included a peer group education function in the program to increase social support (Kim and Sarna 2004). In the area of chronic disease management, bilingual nurses continued to provide social support via telephone counseling following in-class education sessions or interventions with mailed print education materials (Han et al. 2010; Kim et al. 2006, 2009, 2008, 2011; Song et al. 2010). In the intervention program for Korean American schizophrenia patients, Shin and Lukens (2002) offered parallel education sessions to family members for supporting patients. Sin et al. (2005) did not directly mention the use of social support in their article; however frequent education sessions (three times per week) with small groups (13 participants) appeared to include provision of social support.
Five interventions (Fang et al. 2006; Kim et al. 2009, 2010; Maxwell et al. 2008; Moskowitz et al. 2007; Wismer et al. 2001) did not address the deep-structure tenet of social support in their intervention (Table 2). These same five studies did not yield statistically significant results consistent with the study’s primary hypotheses or proposed research questions related to behavioral changes. Kim and Menon (2009) and Kim et al. (2010) conducted the intervention, titled ‘Go Early,’ to promote breast cancer screening use. Although they hired community navigators, these navigators focused on helping participants sign consent forms, rather than following-up to help participants access screening. As shown in Table 3, their studies did not show significant improvement on mammography use, even though there was a significant improvement in health beliefs (perceived risk, pros, cons, fear, self-efficacy, modesty, and fatalism) (Kim and Menon 2009) and a significant increase in knowledge and modifying beliefs (Kim et al. 2010). Maxwell et al. (2008) conducted interventions with mailed print education materials to promote breast cancer screening for Korean American women, but showed no significant increase in repeated screening. When the investigators modified the program to include a bilingual patient navigator, they observed a significant increase in completion of follow-up tests (Maxwell et al. 2010). The two studies reporting on ‘Health is Strength,’ which aimed to promote breast and cervical cancer screening among Korean American women, employed lay health counselors (Moskowitz et al. 2007; Wismer et al. 2001). However, the health counselors had difficulty fulfilling their activities because women were uncomfortable in discussing breast and cancer screenings with people they did not know, and the study ended with no significant improvements in screening utilization. Fang et al. (2006) reported insignificant improvement in smoking quit rates at 3-month follow-up without any social support.
Table 3.
Characteristics of outcomes.
| No. | Author, year | Theoretical framework | Exposure | Knowledge | Psychosocial outcomes
|
Behavioral outcomes
|
|||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Health belief | Self-efficacy | Stage of readiness | Depression/ distress | Satisfaction | Self-reported | Objective | |||||
| Cancer screening | |||||||||||
| 1 | Fang et al. (2007) | HBM and SCT | ↑ | ↑ | ↑ | ||||||
| 2 | Han et al. (2009) | TTM and HBM, CBPR | – | – | ↑ | ||||||
| 3 | Juon et al. (2006) | TTM | ↑ | ↑ | ↑ | ↑ | |||||
| 4 | Kim and Menon (2009) | TTM and HBM | ↑ | ↑ | ↑ | – | |||||
| 5 | Kim et al. (2010) | TTM and HBM | ↑ | ↑ | ↑ | – | |||||
| 6 | Kim and Sarna (2004) | PRECEDE–PROCEED model and CBPR | ↑ | ↑ | ↑ | ||||||
| 7 | Maxwell et al. (2008) | HBM and TRA/TPB | – | – | |||||||
| 8 | Maxwell et al. (2010) | HBM | ↑ | ||||||||
| 9 | Wismer et al. (2001) | PRECEDE/ PROCEED model and community-sensitive research principles | – | – | |||||||
| Moskowitz et al. (2007) | ↑ | – | |||||||||
| 10 | Ma et al. (2009) | HBM and SCT, CBPR | ↑ | ↑ | ↑ | ↑ | |||||
| Chronic disease | |||||||||||
| 11 | Kim et al. (2006) | Learned resource-fullness model and CBPR | ↑ | ||||||||
| 12 | Kim et al. (2008) | ↑ | |||||||||
| Han et al. (2010) | ↑ | ↑ | |||||||||
| Kim et al. (2011) | ↑ | ||||||||||
| 13 | Song et al. (2010) | CBPR | ↑ | ↑ | |||||||
| Kim et al. (2009) | ↑ | ↑ | ↑ | ↑ | |||||||
| Chronic mental illness | |||||||||||
| 14 | Shin and Lukens (2002) | SCT, Family systems theory, stress theory | ↑ | ↑ | |||||||
| Shin (2004) | ↑empowerment | ↑ | ↑ | ||||||||
| Tobacco cessation | |||||||||||
| 15 | Fang et al. (2006) | Cognitive-social health information processing model | – | ↑ | – | ↑(at
1-month) – (at 3-month) |
|||||
| General health | |||||||||||
| 16 | Sin et al. (2005) | Quality health outcome model | ↑ | ↑ | |||||||
Notes: ↑(significant improvement), – (insignificant results/ no change) at p < 0.05 or p < 0.01.
‘Stage of readiness’ can be replaced with ‘decisional balance’.
Outcomes
Outcome variables varied across studies. As shown in Table 3, outcome variables in the reviewed articles fell into two categories: psychosocial variables and behavioral variables. Psychosocial variables included health beliefs, self-efficacy, stage of readiness (or decisional balance), and satisfaction with interventions. Behavioral variables, as relevant to the intervention, included the use of cancer screening, physiological outcomes (e.g., A1C, blood pressure), symptom severity, smoking quit rates, and general health outcomes (e.g., arm-curl test).
Theoretical frameworks guided the selection of outcome measures. For example, the interventions that used the HBM measured knowledge and health beliefs, while the interventions that used the TTM measured stage of change and decisional balance. The variables related to health beliefs were frequently measured (n=8) in the interventions for preventing cancer (screening =7, smoking cessation =1). In the area of management of chronic disease, three interventions analyzed the findings using the outcome variables related to depression or perception of stigma (Kim et al. 2009, 2011; Shin and Lukens 2002).
A total of 14 of the 16 interventions measured behavioral outcomes. Of these, six employed objective measurements, and eight employed self-reported measures. Among those researchers collecting objective measures, some used home blood pressure or glucose monitoring with tele-transmission for acquiring the physiological outcomes such as A1C and blood pressure (Han et al. 2010; Kim et al. 2006, 2009, 2008). Maxwell et al. (2008) conducted their RCT in a community clinic and were able to use charted clinical data to analyze the use of breast cancer screening. Ma et al. (2009) verified the use of colorectal cancer screening in the physician’s office. Sin et al. (2005) tested health outcomes (e.g., arm-curl test) in a practical way.
In sum, theoretical frameworks determined the characteristics of outcome variables. The majority of interventions used both psychosocial variables and behavioral variables to evaluate both the process of behavior changes and the changes themselves, but one study used only psychosocial variables. All psychosocial outcomes were measured using the self-report method as is conventional. In contrast, behavior change outcomes were measured by either the self-report or objective methods.
Discussion
This article is the first to provide a systematic review of intervention programs to prevent and control chronic disease among Korean Americans. The purpose of this review was to examine principles and components of interventions culturally tailored for Korean American in the context of improvement of health and prevention of disease. Specifically, the review looked at which theories guided the interventions, how the components of interventions reflected surface and deep structures to attract participants and promote their health, and how these approaches associated with behavioral outcomes.
The characteristics of the study designs reviewed in this study greatly varied. Some were RCTs, or quasi-experimental studies and others were brief, small-scaled pilot studies. Theoretical frameworks or research approaches guided all 16 interventions. However, basing an intervention on a theory of behavior change or research approach resulted in a successful outcome for only about 69% of the time. Half of the interventions used more than one guiding theory and/or approach. Individual-level and/or interpersonal-level theories led the interventions three times more than community-level principles or approaches. These trends illustrated that the focus of interventions targeting Korean Americans has been predominantly on promoting individuals to change their health behaviors rather than making changes to environments relevant to health and that these interventions are mono-level. For example, only 6 interventions targeting Korean Americans employed CBPR principles in combination of individual- or interpersonal-level theories. CBPR refers to a process for creating knowledge and tailoring interventions through partnerships between community and academic entities (Minkler and Wallerstein 2010). It is increasingly gaining popularity and potential to help underserved populations tackle health disparities in mainstream and other ethnic communities of the USA. Even though a limited number of interventions targeting Korean Americans used CBPR, a growing number of researchers have employed it to benefit Korean Americans in terms of prevention and control of chronic disease (Han et al. 2007; Ma et al. 2012).
The current research revealed that the intervention design in 75% of the reviewed studies was informed by formative research. In these studies, a success rate of 67% was observed indicating a similar success rate when using models. In spite of this, many researchers reported that formative research in collaboration with Korean American communities based on CBPR principles was practically useful in identifying: the needs of the interventions; existing health-related knowledge, attitudes, barriers, and motivations; and internal cultural values, norms, and beliefs that should be considered in designing, delivering, and evaluating a program (Han et al. 2007; Ma et al. 2012). Similarly, previous research targeting other ethnic groups in the USA emphasized the importance of formative research to ensure the success of the interventions (Campbell et al. 2007; Mier, Ory, and Medina 2010; Resnicow et al., 1999). Therefore, the important role of formative research along with culturally sensitive strategies in designing and implementing intervention programs for Korean American cannot be overlooked.
Based on the cultural sensitivity framework proposed by Resnicow et al. (1999), the effective components of the culturally tailored interventions were identified in this review. The cultural component most associated with successful interventions was the providing of social support (deep structure) via bilingual or ethnically matched lay health workers, nurses, nutritionists, peer group, or family members during the intervention and/or the follow-up period. Integrating social support into intervention resulted in a successful outcome about 91% of the time. Even though all interventions in the current review did not indicate a direct association between the effectiveness of the interventions and social support, this review revealed that social support generally contributes to improvement in health behaviors. This finding is consistent with previous research on other target population. For example, Mier, Ory, and Medina (2010) found that emotional and social support, as well as family involvement, correlate significantly with healthy eating in various age groups and are strong predictors of exercise in Hispanic women.
Furthermore, this review found that the quality of social support via patient navigators is critical to ensuring intervention effectiveness. Moskowitz et al. (2007) argued that the impact of programs varied depending on the presence of well-trained and highly motivated community health workers. Although they recruited a large number of patient navigators to distribute the breast and cervical cancer screening educations, Korean Americans’ exposure to the program was low. Researchers pointed out that community health workers may need more training to help Korean American women resolve barriers to breast and cervical cancer screening. In Wells et al.’s review (2008), most patient navigators in the USA are receiving a certain level of training, but the quality and training of that training are unclear. In line with increasing interest in the quality of patient navigators, Braun et al. (2012) analyzed patient navigators’ tasks affiliated with five Community Network Programs targeting ethnic minorities (e.g., immigrant Asian Americans, Native Hawaiians) and underserved low-income populations in the USA. Patient navigators in these five programs generally performed similar tasks across the cancer care continuum (education and outreach, screening, diagnosis and staging, treatment, survivorship, and end-of-life). However, researchers found that patient navigators in each program adjusted their tasks to fit target populations’ cultural contexts. This article suggests that the depth of social support via culturally competent patient navigators is vital to help diverse and hard-to-reach ethnic minority groups in practical ways.
Surface structures supported by materials, communication channels, settings, staff, and recruitment strategies, are important elements in behavioral interventions when blended with cultural values. Many of the interventions in this review incorporated surface structure elements combined with cultural values, one of the deep-structure elements. Specifically, all interventions used five elements: four elements of surface structure (material, setting, communication channel, and staff) and one element of deep structure (cultural value). Integrating surface structure and cultural value into intervention resulted in a successful outcome from about 68% to 73% of the time. Despite the medium level of success rate, practical importance of inclusion of surface structure and cultural values cannot be ignored. To increase program acceptance and convey a clear understanding of its contents, all reviewed studies integrated cultural values into the outward appearance of the program and materials. The findings are consistent with the previous conceptualization of cultural sensitivity, and these trends might reflect the importance of engraving cultural values into culturally appropriate visualization of the program. Researchers have argued that integrating cultural values and norms into the translation of materials, using culturally relevant settings and communication channels, and recruiting culturally competent staff are required to retain consistent meaning and context (Kreuter et al. 2002). Therefore, the breadth and depth of cultural components supported by surface and deep structures should be considered throughout all phases of interventions targeting Korean Americans.
Implications for policy
The current review implies that culturally sensitive and committed social support should be provided to catalyze the behavioral changes and sustain the effect of the interventions targeting Korean Americans. This implication is consistent with the current US policy-level efforts to tackle health disparities among underserved ethnic minorities. There is a growing body of federal and state laws, regulations, and standards that seek to integrate cultural knowledge into public health practices in the USA. The US Office of Minority Health (2001) highlights the importance of cultural and linguistic competence to eliminate disparities in the health status of people of diverse racial, ethnic, and cultural backgrounds. It suggested 14 national standards for healthcare-related agencies named Culturally and Linguistically Appropriate Services (CLAS). Specifically, culturally competent care and language access services are mandates for recipients of federal funds or federal, state, and nationally accredited healthcare-related agencies. Although the CLAS directs that federally funded health facilities must provide interpretation for all patients who request it, practical implementation is uneven (Derose, Escarce, and Lurie 2007). Many people do not know of the law, and there are few financial reimbursements to implement and enforce CLAS in the USA (e.g., only 10 states require Medicaid to cover access to an interpreter).
To fill this practical gap, Derose, Escarce, and Lurie (2007) suggested the use of Medicaid funds for community-based health promoters that can reach underserved immigrants in the USA. European countries have implemented innovative policies to reduce health inequalities among ethnic minority groups. ‘Cultural mediators’ in Belgium interpret in about two-thirds of their interventions and are involved in helping patients navigate the health care system, while the National Health Services (NHS) in Scotland has developed the Minority Ethnic Health Inclusion Project (MEHIP) and has provided ethnic minority groups with links to patient navigators (Lorant and Bhopal 2011). Therefore, it is essential for policy-makers to consider the inclusion of various forms of social support via culturally and linguistically competent patient navigators in the national standards to reduce health disparities among hard-to-reach ethnic minority groups.
Limitations
Despite important contribution of this review, some methodological limitations remain due to the nature of literature review. First, the association between specific components of the interventions and their effectiveness could not be clearly delineated, since outcome variables in each study were not comparable and all confounding variables could not be captured. Second, operationalization of culturally sensitive strategies was not always clearly delineated, as these strategies were embedded in the process of designing and implementing the interventions. We relied on the method sections or process evaluations to discern the culturally sensitive strategies that were employed. Third, the studies reviewed did not consistently define the demographics of their study populations in detail (e.g., first-generation Korean Americans). Thus, it is not clear as to which culturally tailored intervention elements may be applicable to new immigrants versus other subgroups of Korean Americans.
Conclusion
Korean Americans, one of the most rapidly growing ethnic groups in the USA, have increased from fewer than 70,000 in 1970 to more than 1.3 million in 2000 (Jo et al. 2008). The findings of this review should be helpful for researchers as they design, deliver, and evaluate the effectiveness of interventions targeting Korean Americans and other minority populations. In turn, policy-makers in health care may gain some insight that will inform the development of more appropriate, timely, and culturally sensitive policy. Hopefully, this will enable healthcare organizations to improve their services for ethnic minorities.
Key messages.
As the Korean American population increases, more interventions have been designed and tested to help them prevent and control chronic diseases.
Formative research is useful in understanding cultural values that need to be engraved in education and messages delivered through chronic disease interventions for Korean Americans.
Culturally sensitive and committed social support should be provided to catalyze the behavioral changes and sustain the effect of the interventions targeting Korean Americans.
Social support can be successfully provided or coordinated by well-trained lay health workers, nurses, or family members during an intervention and/or follow-up period.
Acknowledgments
The authors would like to thank Dr Deon Canyon and Dr Stefan Keller for their insightful comments on an earlier version of this manuscript. The earlier version of this paper was presented at the Pacific Global Health Conference in Honolulu, USA, October 2012.
References
- Abate N, Chandalia M. The Impact of Ethnicity on Type 2 Diabetes. Journal of Diabetes and its Complications. 2003;17(1):39–58. doi: 10.1016/S1056-8727(02)00190-3. [DOI] [PubMed] [Google Scholar]
- Aday LA. At Risk in America: The Health and Health Care Needs of Vulnerable Populations in the United States. Vol. 13. San Francisco, CA: Jossey-Bass; 2002. [Google Scholar]
- APIAHF (Asian Pacific Islander American Health Forum) Koreans in the United States. Asian Pacific Islander American Health Forum Health Brief; 2006. http://www.apiahf.org/sites/default/files/APIAHF_Healthbrief08e_2006.pdf. [Google Scholar]
- APIAHF (Asian Pacific Islander American Health Forum) Demographic and socioeconomic profiles of Asian Americans, Native Hawaiians, and Pacific Islanders in the United States. 2011 http://www.apiahf.org/sites/default/files/Demographic_Socioeconomic_Profiles_AANHPI.pdf.
- Braun KL, Kagawa-Singer M, Holden AE, Burhansstipanov L, Tran JH, Seals BF, Ramirez AG. Cancer Patient Navigator Tasks across the Cancer Care Continuum. Journal of Health Care for the Poor and Underserved. 2012;23(1):398. doi: 10.1353/hpu.2012.0029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell MK, Hudson MA, Resnicow K, Blakeney N, Paxton A, Baskin M. Church-based Health Promotion Interventions: Evidence and Lessons Learned. Annual Review of Public Health. 2007;28:213–234. doi: 10.1146/annurev.publhealth.28.021406.144016. [DOI] [PubMed] [Google Scholar]
- Cho J, Juon HS. Assessing Overweight and Obesity Risk Among Korean Americans in California Using World Health Organization Body Mass Index Criteria for Asians. Preventing Chronic Disease. 2006;3(3):A79. [PMC free article] [PubMed] [Google Scholar]
- Derose KP, Escarce JJ, Lurie N. Immigrants and Health Care: Sources of Vulnerability. Health Affairs. 2007;26(5):1258–1268. doi: 10.1377/hlthaff.26.5.1258. [DOI] [PubMed] [Google Scholar]
- Fang CY, Ma GX, Miller SM, Tan Y, Su X, Shive S. A Brief Smoking Cessation Intervention for Chinese and Korean American Smokers. Preventive Medicine. 2006;43(4):321–324. doi: 10.1016/j.ypmed.2006.06.009. [DOI] [PubMed] [Google Scholar]
- Fang CY, Ma GX, Tan Y, Chi N. A Multifaceted Intervention to Increase Cervical Cancer Screening Among Underserved Korean Women. Cancer Epidemiology Biomarkers & Prevention. 2007;16(6):1298–1302. doi: 10.1158/1055-9965.epi-07-0091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frisbie WP, Cho Y, Hammer RA. Immigration and the Health of Asian and Pacific Islander Adults in the United States. American Journal of Epidemiology. 2001;153:372–380. doi: 10.1093/aje/153.4.372. [DOI] [PubMed] [Google Scholar]
- Glanz K, Rimer BK, Viswanath K, editors. Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- Han HR, Kang J, Kim KB, Ryu JP, Kim MT. Barriers to and Strategies for Recruiting Korean Americans for Community-partnered Health Promotion Research. Journal of Immigrant and Minority Health. 2007;9(2):137–146. doi: 10.1007/s10903-006-9022-x. [DOI] [PubMed] [Google Scholar]
- Han HR, Kim J, Kim KB, Jeong S, Levine D, Li C, Song H, Kim MT. Implementation and Success of Nurse Telephone Counseling in Linguistically Isolated Korean American Patients with High Blood Pressure. Patient Education and Counseling. 2010;80(1):130–134. doi: 10.1016/j.pec.2009.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han HR, Lee H, Kim MT, Kim KB. Tailored Lay Health Worker Intervention Improves Breast Cancer Screening Outcomes in Non-adherent Korean-American Women. Health Education Research. 2009;24(2):318–329. doi: 10.1093/her/cyn021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofstetter CR, Irvin V, Schmitz K, Hovell MF, Nichols J, Kim HR, Ledet R, et al. Demography of Exercise Among Californians of Korean Descent: A Cross-sectional Telephone Survey. Journal of Immigrant and Minority Health. 2008;10(1):53–65. doi: 10.1007/s10903-007-9050-1. [DOI] [PubMed] [Google Scholar]
- Jo AM, Maxwell AE, Wong WK, Bastani R. Colorectal Cancer Screening among Underserved Korean Americans in Los Angeles County. Journal of Immigrant and Minority Health. 2008;10:119–126. doi: 10.1007/s10903-007-9066-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juon HS, Choi S, Klassen A, Roter D. Impact of Breast Cancer Screening Intervention on Korean-American Women in Maryland. Cancer Detect Prevention. 2006;30(3):297–305. doi: 10.1016/j.cdp.2006.03.008. [DOI] [PubMed] [Google Scholar]
- Kim MT, Han H-R, Hedlin H, Kim J, Song HJ, Kim KB, Hill MN. Teletransmitted Monitoring of Blood Pressure and Bilingual Nurse Counseling-sustained Improvements in Blood Pressure Control During 12 Months in Hypertensive Korean Americans. The Journal of Clinical Hypertension. 2011;13(8):605–612. doi: 10.1111/j.1751-7176.2011.00479.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim MT, Han HR, Park HJ, Lee H, Kim KB. Constructing and Testing a Self-help Intervention Program for High Blood Pressure Control in Korean American Seniors – A Pilot Study. Journal of Cardiovascular Nursing. 2006;21(2):77–84. doi: 10.1097/00005082-200603000-00002. [DOI] [PubMed] [Google Scholar]
- Kim MT, Han HR, Song HJ, Lee JE, Kim J, Ryu JP, Kim KB. A Community-Based, Culturally Tailored Behavioral Intervention for Korean Americans With Type 2 Diabetes. Diabetes Educator. 2009;35(6):986–994. doi: 10.1177/0145721709345774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim MT, Kim EY, Han HR, Jeong S, Lee JE, Park HJ, Kim BK, Hill MN. Mail Education is as Effective as In-class Education in Hypertensive Korean Patients. Journal of Clinical Hypertension (Greenwich) 2008;10(3):176–184. doi: 10.1111/j.1751-7176.2008.07571.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JH, Menon U. Pre- and Postintervention Differences in Acculturation, Knowledge, Beliefs, and Stages of Readiness for Mammograms among Korean American Women. Oncology Nursing Forum. 2009;36(2):E80–92. doi: 10.1188/09.onf.e80-e92. [DOI] [PubMed] [Google Scholar]
- Kim JH, Menon U, Wang E, Szalacha L. Assess the Effects of Culturally Relevant Intervention on Breast Cancer Knowledge, Beliefs, and Mammography Use Among Korean American Women. Journal of Immigrant and Minority Health. 2010;12(4):586–597. doi: 10.1007/s10903-009-9246-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim YH, Sarna L. An Intervention to Increase Mammography Use by Korean American Women. Oncology Nursing Forum. 2004;31(1):105–110. doi: 10.1188/04.ONF.105-110. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Lukwago SN, Bucholtz DC, Clark EM, Sanders-Thompson V. Achieving Cultural Appropriateness in Health Promotion Programs: Targeted and Tailored Approaches. Health Education & Behavior. 2002;30(2):133–146. doi: 10.1177/1090198102251021. [DOI] [PubMed] [Google Scholar]
- Lorant V, Bhopal R. Comparing Policies to Tackle Ethnic Inequalities in Health: Belgium 1 Scotland 4. European Journal of Public Health. 2011;21(2):235–240. doi: 10.1093/eurpub/ckq061. [DOI] [PubMed] [Google Scholar]
- Ma GX, Gao W, Tan Y, Chae WG, Rhee J. A Community-Based Participatory Approach to a Hepatitis B Intervention for Korean Americans. Progress in Community Health Partnerships: Research, Education, and Action. 2012;6(1):7–16. doi: 10.1353/cpr.2012.0002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma GX, Shive S, Tan Y, Gao WZ, Rhee J, Park M, Kim J, Toubbeh JI. Community-based Colorectal Cancer Intervention in Underserved Korean Americans. Cancer Epidemiology. 2009;33(5):381–386. doi: 10.1016/j.canep.2009.10.001. [DOI] [PubMed] [Google Scholar]
- Maxwell AE, Jo AM, Chin SY, Lee KS, Bastani R. Impact of a Print Intervention to Increase Annual Mammography Screening Among Korean American Women Enrolled in the National Breast and Cervical Cancer Early Detection Program. Cancer Detection and Prevention. 2008;32(3):229–235. doi: 10.1016/j.cdp.2008.04.003. [DOI] [PubMed] [Google Scholar]
- Maxwell AE, Jo AM, Crespi CM, Sudan M, Bastani R. Peer Navigation Improves Diagnostic Follow-up after Breast Cancer Screening among Korean American Women: Results of a Randomized Trial. Cancer Causes Control. 2010;21(11):1931–1940. doi: 10.1007/s10552-010-9621-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mier N, Ory MG, Medina AA. Anantomy of Culturally Sensitive Interventions Promoting Nutrition and Exercise in Hispanics: A Critical Examination of Existing Literature. Health Promotion Practice. 2010;11(4):541–554. doi: 10.1177/1524839908328991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minkler M, Wallerstein N, editors. Community-based Participatory Research for Health: From Process to Outcomes. San Francisco, CA: Jossey-Bass; 2010. [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-analyses: The PRISMA Statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Moskowitz JA, Kazinets G, Wong JM, Tager IB. ‘Health is Strength’: A Community Health Education Program to Improve Breast and Cervical Cancer Screening Among Korean, American Women in Alameda County, California. Cancer Detection and Prevention. 2007;31(2):173–183. doi: 10.1016/j.cdp.2007.02.002. [DOI] [PubMed] [Google Scholar]
- Office of Minority Health, U.S. Department of Health and Human Services. National Standards for Culturally and Linguistically Appropriate Services in Health Care. Washington: IQ Solutions; 2001. [Google Scholar]
- Resnicow K, Baranowski T, Ahluwalia JS, Braithwaite RL. Cultural Sensitivity in Public Health: Defined and Demystified. Ethnicity and Disease. 1999;9:10–21. [PubMed] [Google Scholar]
- Shin S-K. Effects of Culturally Relevant Psychoeducation for Korean American Families of Persons with Chronic Mental Illness. Research on Social Work Practice. 2004;14(4):231–239. doi: 10.1177/1049731503262130. [DOI] [Google Scholar]
- Shin SK, Lukens EP. Effects of Psychoeducation for Korean Americans with Chronic Mental Illness. Psychiatric Services. 2002;53(9):1125–1131. doi: 10.1176/appi.ps.53.9.1125. [DOI] [PubMed] [Google Scholar]
- Sin M-K, Belza B, LoGerfo J, Cunningham S. Evaluation of a Community-based Exercise Program for Elderly Korean Immigrants. Public Health Nursing. 2005;22(5):407–413. doi: 10.1111/j.0737-1209.2005.220505.x. [DOI] [PubMed] [Google Scholar]
- Sohn L. The Health and Health Status of Older Korean Americans at the 100-year Anniversary of Korean Immigration. Journal of Cross-Cultural Gerontology. 2004;19(3):203–219. doi: 10.1023/b:jccg.0000034219.97686.69. [DOI] [PubMed] [Google Scholar]
- Song HJ, Han HR, Lee JE, Kim J, Kim KB, Nguyen T, Kim MT. Translating Current Dietary Guidelines Into a Culturally Tailored Nutrition Education Program for Korean American Immigrants with Type 2 Diabetes. Diabetes Education. 2010;36(5):752–761. doi: 10.1177/0145721710376328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells KJ, Battaglia TA, Dudley DJ, Garcia R, Greene A, Calhoun E, Raich PC. Patient Navigation: State of the Art or is it Science? Cancer. 2008;113(8):1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wismer BA, Moskowitz JM, Min K, Chen AM, Ahn Y, Cho S, Jun S, et al. Interim Assessment of a Community Intervention to Improve Breast and Cervical Cancer Screening among Korean American Women. Journal of Public Health Management and Practice. 2001;7(2):61–70. doi: 10.1097/00124784-200107020-00009. [DOI] [PubMed] [Google Scholar]