Abstract
Purpose
To examine disparities and changes over time in the population-level distribution of smokers along a cigarette quitting continuum among African American smokers compared with non-Hispanic Whites.
Methods
Secondary data analyses of the 1999, 2002, 2005, and 2008 California Tobacco Surveys (CTS). The CTS are large, random-digit-dialed, population-based surveys designed to assess changes in tobacco use in California. The number of survey respondents ranged from n = 6,744 to n = 12,876 across CTS years. Current smoking behavior (daily or nondaily smoking), number of cigarettes smoked per day, intention to quit in the next 6 months, length of most recent quit attempt among current smokers, and total length of time quit among former smokers were assessed and used to recreate the quitting continuum model.
Results
While current smoking rates were significantly higher among African Americans compared with non-Hispanic Whites across all years, cigarette consumption rates were lower among African Americans in all years. There were significant increases in the proportion of former smokers who had been quit for at least 12 months from 1999 (African Americans, 26.8% ± 5.5%; non-Hispanic Whites, 36.8% ± 1.6%) to 2008 (African Americans, 43.6% ± 4.1%; non-Hispanic Whites, 57.4% ± 2.9%). The proportion of African American former smokers in each CTS year was significantly lower than that of non-Hispanic Whites.
Conclusions
Despite positive progression along the quitting continuum for both African American and non-Hispanic White smokers, the overall distribution was less favorable for African Americans. The lower smoking consumption levels among African Americans, combined with the lower rates of successful smoking cessation, suggest that cigarette addiction and the quitting process may be different for African American smokers.
Keywords: African American, behavioral theories, health disparities, race/ethnicity, smoking and tobacco use, stages of change/transtheoretical model
African American smokers bear a disproportionate burden of tobacco-related diseases (American Cancer Society, 2014; U.S. Department of Health and Human Services, 1998, 2000a). Some population-based studies have shown that African Americans are only half as likely to successfully quit smoking as non-Hispanic Whites, despite reports citing lower cigarette consumption (Trinidad, Pérez-Stable, White, Emery, & Messer, 2011; U.S. Department of Health and Human Services, 1998). Few reports have studied this relationship over time and none have examined trends in the distribution of African American smokers along a continuum of quitting behaviors. Smoking cessation is a process rather than a specific event (U.S. Department of Health and Human Services, 2000b) and understanding the distribution of African American smokers along a quitting continuum can provide detailed information that informs the development of appropriate population-based interventions that seek to increase cessation among African American smokers.
Many studies have used varying lengths of cigarette smoking abstinence to classify quitting. Some have used abstinence lengths of 7 days (Webb Hooper, Rodriguez de Ybarra, & Baker, 2013), 30 days (Chow et al., 2010), 90 days (Brandon, Collins, Juliano, & Lazev, 2000; Hymowitz et al., 1997), 6 months (Pierce & Gilpin, 2003; Yeomans et al., 2011), and 12 months (Zhu, Melcer, Sun, Rosbrook, & Pierce, 2000). Preceding actual quitting behaviors, researchers have examined cigarette consumption levels (Okuyemi, Ahluwalia, Richter, Mayo, & Resnicow, 2001) as well as intentions and cognitions related to future quitting plans (Fagan et al., 2007; Trinidad, Pérez-Stable, Messer, White, & Pierce, 2010). These prequitting measures and the actual lengths of smoking abstinence have been combined to define a quitting continuum. From a sample of California smokers, Pierce, Farkas, and Gilpin (1998) identified eight distinct levels on a quitting continuum (QC), using addiction, quitting history, and intention-to-quit variables. This QC is based on the stages of change/transtheoretical model (DiClemente et al., 1991; Prochaska & DiClemente, 1983) and provides a measure of a smoker’s status in the quitting process, with each level in the continuum representing a meaningful advance toward successful cessation, defined as 12-month continuous abstinence. The levels of the QC are behaviorally operationalized in the Methods section.
Changes in the population distribution of smokers along the QC over time have never been examined in great detail across a period of years. However, the California Tobacco Surveys (CTS), which have been conducted in the state since the 1990s, allow for this rare examination. Particularly after the 1998 Master Settlement Agreement between the State Attorneys General and the tobacco industry, smoking rates have decreased for all racial/ethnic groups in general (Sloan & Trogdon, 2004; Sung, Hu, Ong, Keeler, & Sheu, 2005). California is one of a few states in the nation that has had a continuously funded comprehensive tobacco control program since the Master Settlement Agreement, and smoking rates in the state have been several years ahead of other states or the nation as a whole. As such, examining progress on advancing population groups of smokers along the QC in this state can yield valuable information on the status of racial/ethnic disparities in smoking cessation and may be relevant to other states in the nation.
Because of the high burden of smoking-related diseases and elevated adult smoking rates among African Americans (Flack, Ferdinand, & Nasser, 2003; Haiman et al., 2006; Harris, Zang, Anderson, & Wynder, 1993), of particular interest is studying how the distribution of African American smokers along the QC relative to non-Hispanic Whites has changed over time. We analyzed the CTS from 1999 to 2008 (the latest available year of data) among adults 18 years and older and categorized smokers using the QC, which will help us understand whether lower cigarette consumption levels and lower rates of smoking cessation among African Americans relative to non-Hispanic Whites have persisted over time. Findings from this report may help focus smoking cessation efforts for sociodemographic groups experiencing less quitting success.
Methods
Data Source
The CTS are large, population-based, random-digit-dialed surveys designed to monitor changes in tobacco use and attitudes in California. They have been conducted every 3 years from 1990 to 2008, as part of the evaluation of the California Tobacco Control Program (Bal, Kizer, Felten, Mozar, & Niemeyer, 1990). The detailed procedural and technical methods for each CTS, including the use of replicate weights for sample representativeness, are described elsewhere (Social Sciences Data Collection, University of California San Diego, 1990–2008). Briefly, the CTS used a random-digit-dialing procedure with a sample of randomly selected phone numbers stratified to cover region, minority populations, and age. Person-level weights were calculated to be used in analyses to provide the appropriate representation of the California population. Population numbers were based on the U.S. Census Bureau’s Current Population Survey (Bureau of Labor Statistics & U.S. Census Bureau, 2002) to generate denominators. A 5-minute screener interview with a household adult collected demographic information, including age, gender and race/ethnicity, as well as smoking status information for each resident. Some household residents were then selected for an approximate 25-minute extended interview, with the probability of selection being much higher if the person was reported to have smoked within the past 5 years. The present analysis uses data from the extended interview of adults.
Measures
Sociodemographic characteristics of interest in the CTS included race/ethnicity (African American and non-Hispanic White), age group (18–34, 35–49, 50–64, and 65 years and older), gender, and education level (less than high school, high school graduate, some college, college graduate).
Smoking Behavior
Respondents who had ever smoked 100 cigarettes in their lifetime were considered ever smokers. Ever smokers who currently smoked either every day or some days were considered current smokers. Ever smokers who reported no longer smoking at the time of the survey were considered former smokers. Current smokers were also asked to report the number of cigarettes they usually smoked on the days they smoked in order to estimate their cigarette consumption.
Quitting Behaviors and Intentions
Current smokers who reported quitting smoking intentionally for at least 1 day in the past year were considered to have made a quit attempt (but they relapsed to being current smokers). Among these current smokers, quit length was the reported length of the respondent’s most recent quit attempt in the past year. Current smokers who reported intending to quit within the next 6 months were considered to have an intention to quit smoking. Among former smokers, the total length of time that they had been quit was calculated by subtracting the date a respondent had reported having been quit from the survey date.
The Quitting Continuum
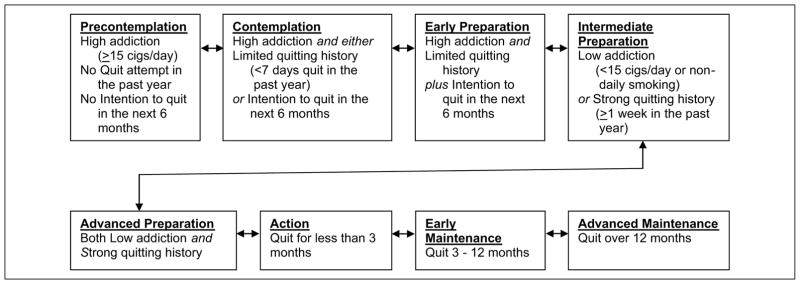
In their prior study, Pierce et al. (1998) used eight levels to define the various stages in the QC. We used this same model in this investigation (see Figure 1). The lowest level on the QC is Precontemplation and includes current smokers with high addiction (cigarette consumption of at least 15 cigarettes per day), with no quit attempts in the past year and with no short-term intention to try to quit smoking. Smokers in the Contemplation level are those who smoke at least 15 cigarettes per day but have some limited quitting history (e.g., less than 7 days in the past year) or an intent to quit in the next 6 months. Those in the Early Preparation level have the same smoking and quitting criteria as Contemplators and also indicate an intention to quit in the next 6 months. Those in the Intermediate Preparation level are smokers with relatively lower addiction (smoking consumption of <15 cigarettes/day) or were intermittent smokers (i.e., identified as nondaily smokers) or quit for at least a week in the past year. Smokers in the Advanced Preparation level are those who smoked fewer than 15 cigarettes per day or were intermittent smokers and those who quit for at least a week in the past year. Those in the Action level are ever smokers who did not currently smoke at the time of interview (i.e., former smokers) and reported having quit for less than 3 months when interviewed. Those in the Early Maintenance level are former smokers who have ceased smoking between 3 and 12 months at the time of interview. Those in the Advanced Maintenance level are former smokers who have been quit for at least 12 months, the currently accepted standard definition of successful quitting (Pierce & Gilpin, 2003).
Figure 1.
Levels of the quitting continuum.
Statistical Analysis
Each survey was weighted so that population estimates could be computed. Base weights were computed from the probability of household selection and the probability of being selected for an extended interview (Social Sciences Data Collection, University of California San Diego, 1990–2008). These weights were then further adjusted for nonresponse to the latest available California census totals. We used SAS software version 9.3 (SAS Institute, 2012) procedures specifically developed to account for complex survey designs (e.g., Procs SURVEYFREQ, SURVEYMEANS, SURVEYREG) to compute estimates, including jackknife methods (Efron, 1982) to calculate variances for use in the computation of the 95% confidence intervals. Nonoverlapping confidence limits for weighted estimates were used as a conservative method of delineating statistically significant differences between rates for unadjusted proportions.
Because of marked differences over time in the unadjusted rates for the Advanced Preparation, Action, and Advanced Maintenance levels for African Americans and non-Hispanic Whites, we examined whether the adjusted rates for these levels of the QC changed significantly over time. Specifically, we tested whether there was a significant difference between 1999 and 2008 proportions for these levels in the QC by stratifying by gender and age group. Using unweighted data, proportions for each gender by age group stratum were estimated via a least square means approach for the QC level of interest (e.g., Advanced Preparation). We tested the null hypothesis that the proportions for independent samples (i.e., from 1999 and 2008), were not statistically significantly different from each other. Z tests of proportions for independent samples were conducted and 95% confidence intervals were constructed for each of the strata.
Results
Demographics and General Smoking Overview
Table 1 presents the number of adults that completed the extended interview and the percentages of African Americans and non-Hispanic Whites for each CTS year. With the exception of 2008, in all CTS years there were more African American women than men respondents. In 1999 and 2002 there were larger proportions of African American and non-Hispanic White respondents in the younger age groups compared to the older age groups. This continued for non-Hispanic Whites in 2005 and 2008, whereas the distribution for African Americans was more evenly distributed. Across all CTS years, the proportion of those who reported graduating from college was lower among African Americans compared with non-Hispanic Whites. Response rates ranged from 68% in 1999 to 53% in 2008.
Table 1.
Demographic Characteristics and Smoking Behaviors, 1999–2008.
| Characteristic | 1999 | 2002 | 2005 | 2008 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||||||||
| African American (n = 758) | Non-Hispanic White (n = 9,410) | African American (n = 1,713) | Non-Hispanic White (n = 11,163) | African American (n = 1,543) | Non-Hispanic White (n = 7542) | African American (n = 1,588) | Non-Hispanic White (n = 5,156) | |||||||||
|
|
|
|
|
|
|
|
|
|||||||||
| % | [95% CI] | % | [95% CI] | % | [95% CI] | % | [95% CI] | % | [95% CI] | % | [95% CI] | % | [95% CI] | % | [95% CI] | |
| Gender | ||||||||||||||||
| Male | 43.8 | [39.5, 48.2) | 48.7 | [47.7, 49.8] | 48.2 | [45.1, 51.4] | 49.9 | [48.4, 51.5] | 45.1 | [40.1, 50.1] | 49.9 | [47.3, 52.4] | 49.4 | [43.9, 54.9] | 50.1 | [47.8, 52.4] |
| Female | 56.2 | [51.8, 60.5) | 51.3 | [50.2, 52.3] | 51.8 | [48.6, 54.9] | 50.1 | [48.5, 51.6] | 54.9 | [49.9, 59.9] | 50.1 | [47.6, 52.7] | 50.6 | [45.1, 56.1] | 49.9 | [47.6, 52.2] |
| Age group (years) | ||||||||||||||||
| 18–34 | 36.9 | [33.1, 40.8] | 27.8 | [26.9, 28.7] | 33.4 | [31.5, 35.3] | 26.7 | [25.7, 27.7] | 32.2 | [28.3, 36.0] | 22.3 | [20.6, 23.9] | 30.4 | [26.7, 34.1] | 21.7 | [20.2, 23.3] |
| 35–49 | 31.2 | [26.9, 35.5] | 31.8 | [30.6, 33.0] | 33.8 | [31.0, 36.6] | 31.6 | [30.1, 33.0] | 33.3 | [28.1, 38.5] | 30.1 | [28.0, 32.2] | 30.3 | [26.8, 33.7] | 30.2 | [28.2, 32.1] |
| 50–64 | 18.4 | [14.8, 22.1] | 21.2 | [20.2, 22.1] | 21.1 | [19.4, 22.8] | 22.1 | [20.9, 23.3] | 20.7 | [17.3, 24.1] | 24.8 | [23.0, 26.6] | 20.5 | [18.5, 22.4] | 26.2 | [24.4, 28.0] |
| 65+ | 13.4 | [10.1, 16.8] | 19.2 | [18.1, 20.2] | 11.7 | [10.1, 13.3] | 19.6 | [18.5, 20.7] | 13.8 | [10.6, 17.1] | 22.8 | [20.9, 24.6] | 18.9 | [17.3, 20.5] | 21.9 | [19.9, 24.0] |
| Education | ||||||||||||||||
| Less than high school | 12.4 | [11.8, 13.1] | 8.2 | [7.9, 8.4] | 7.6 | [6.4, 8.8] | 7.0 | [6.7, 7.4] | 19.5 | [15.3, 23.8] | 6.7 | [6.3, 7.0] | 9.1 | [6.6, 11.5] | 3.2 | [2.6, 3.8] |
| High school graduate | 27.2 | [25.3, 29.0] | 24.5 | [24.0, 25.0] | 27.7 | [25.6, 29.9] | 21.4 | [20.4, 22.4] | 24.2 | [19.3, 29.0] | 22.6 | [21.8, 23.4] | 27.4 | [24.2, 30.6] | 21.9 | [20.6, 23.3] |
| Some college | 36.8 | [33.2, 40.4] | 33.1 | [31.9, 34.2] | 39.7 | [37.1, 42.2] | 31.9 | [30.5, 33.2] | 30.4 | [26.5, 34.2] | 30.9 | [28.2, 33.5] | 34.3 | [30.3, 38.2] | 29.1 | [26.8, 31.4] |
| College graduate | 23.6 | [20.3, 26.9] | 34.3 | [33.3, 35.3] | 25.0 | [23.1, 26.8] | 39.7 | [38.5, 40.9] | 26.0 | [22.7, 29.2] | 39.9 | [37.3, 42.4] | 29.3 | [26.3, 32.3] | 45.8 | [43.6, 48.0] |
| Cigarette consumption | ||||||||||||||||
| Never smokers | 59.8 | [57.6, 62.1] | 49.7 | [49.1, 50.4] | 59.3 | [58.2, 60.5] | 53.5 | [52.8, 54.1] | 57.4 | [55.3, 59.4] | 54.0 | [52.2, 55.9] | 63.5 | [61.4, 65.6] | 56.2 | [54.6, 57.7] |
| Ever smokers | 40.2 | [37.9, 42.4] | 50.3 | [49.6, 50.9] | 40.7 | [39.5, 41.8] | 46.5 | [45.9, 47.2] | 42.6 | [40.6, 44.7] | 46.0 | [44.1, 47.8] | 36.5 | [34.4, 38.6] | 43.8 | [42.3, 45.4] |
| Current smokers | 50.4 | [47.0, 53.7] | 38.6 | [37.9, 39.3] | 47.2 | [45.4, 49.0] | 36.8 | [36.1, 37.5] | 49.8 | [45.8, 53.7] | 32.2 | [30.5, 34.0] | 42.0 | [37.6, 46.4] | 30.1 | [28.8, 31.4] |
| Former smokers | 49.6 | [46.3, 53.0] | 61.4 | [60.7, 62.1] | 52.8 | [51.0, 54.6] | 63.2 | [62.5, 63.9] | 50.2 | [46.3, 54.2] | 67.8 | [66.0, 69.5] | 58.0 | [53.6, 62.4] | 69.9 | [68.6, 71.2] |
| Quitting continuum level | ||||||||||||||||
| Precontemplation | 1.1 | [0.1, 2.0] | 8.2 | [7.5, 8.8] | 3.9 | [2.3, 5.4] | 7.5 | [6.9, 8.1] | 3.3 | [1.4, 5.1] | 6.5 | [5.7, 7.3] | 2.1 | [0.8, 3.4] | 5.8 | [5.0, 6.7] |
| Contemplation | 5.7 | [3.5, 8.0] | 7.3 | [6.6, 8.0] | 4.7 | [3.0, 6.4] | 7.0 | [6.4, 7.6] | 2.8 | [0.8, 4.9] | 5.3 | [4.6, 6.1] | 3.1 | [1.4, 4.8] | 4.8 | [4.2, 5.4] |
| Early preparation | 3.8 | [2.3, 5.4] | 4.1 | [3.7, 4.6] | 3.7 | [2.3, 5.2] | 3.3 | [2.8, 3.7] | 1.7 | [0.0, 3.4] | 2.9 | [2.1, 3.7] | 3.2 | [1.4, 5.1] | 2.3 | [1.7, 2.8] |
| Intermediate preparation | 5.3 | [2.2, 8.5] | 1.9 | [1.4, 2.4] | 2.1 | [1.2, 3.1] | 1.8 | [1.3, 2.2] | 3.5 | [0.9, 6.2] | 1.3 | [0.8, 1.8] | 2.5 | [0.9, 4.1] | 1.3 | [0.8, 1.7] |
| Advanced preparation | 36.1 | [32.4, 39.8] | 17.7 | [16.8, 18.5] | 33.8 | [31.6, 36.0] | 17.4 | [16.6, 18.2] | 39.3 | [34.3, 44.2] | 16.7 | [15.0, 18.3] | 33.1 | [28.4, 37.7] | 17.1 | [15.9, 18.3] |
| Action | 17.2 | [12.6, 21.8] | 19.8 | [18.4, 21.3] | 7.9 | [5.3, 10.5] | 7.9 | [7.0, 8.8] | 5.4 | [2.9, 7.8] | 8.8 | [7.0, 10.5] | 9.7 | [6.3, 13.2] | 7.1 | [5.1, 9.1] |
| Early maintenance | 3.9 | [1.9, 5.9] | 4.2 | [3.6, 4.9] | 2.9 | [1.5, 4.3] | 3.2 | [2.7, 3.7] | 1.8 | [0.9, 2.8] | 3.8 | [2.7, 4.8] | 2.7 | [0.8, 4.6] | 4.3 | [2.9, 5.8] |
| Advanced maintenance | 26.8 | [21.3, 32.3] | 36.8 | [35.2, 38.4] | 41.0 | [38.0, 44.0] | 51.9 | [50.8, 53.1] | 42.2 | [38.2, 46.3] | 54.8 | [51.9, 57.7] | 43.6 | [39.5, 47.7] | 57.4 | [54.5, 60.2] |
The percentage of ever smokers among African Americans was lower than for non-Hispanic Whites across all survey years. In 1999, the African American ever smoking prevalence was 40.2% (95% CI = 37.9–42.4) compared with 50.3% (95% CI = 49.6–50.9) for non-Hispanic Whites. Similarly, the 2008 ever smoking prevalence was lower among African Americans (36.5%; 95% CI = 34.4–38.6) than non-Hispanic Whites (43.8%; 95% CI = 42.3–45.4). Despite the lower ever smoking prevalence for African Americans in all years, the percentage of African American current smokers across all survey years was higher than for non-Hispanic Whites. In 1999, the African American current smoking prevalence was 50.4% (95% CI = 47.0–53.7) compared with 38.6% (95% CI = 37.9–39.3) for non-Hispanic Whites. Current smoking prevalence in 2008 among African Americans was lower than prior years (42.0%; 95% CI = 37.6–46.4), but remained higher than for non-Hispanic Whites (30.1%; 95% CI = 28.8–31.4) throughout the period.
Quitting Continuum
Table 1 also presents information on the distribution of African American and non-Hispanic White smokers along the QC from 1999 to 2008. These are illustrated in Figure 2 for African Americans and non-Hispanic Whites, respectively. The proportions of smokers in the Precontemplation level were generally smaller among African Americans compared with non-Hispanic Whites, reflecting lower rates of heavy cigarette consumption (about 1% to 3% vs. about 6% to 8% per year, respectively). The proportions of African American smokers in the Contemplation, Early Preparation, and Intermediate Preparation levels were low, similar and stable for both racial/ethnic groups over time.
Figure 2.
Distribution of African American and non-Hispanic White smokers along the quitting continuum, 1999 to 2008 California Tobacco Surveys.
In 1999, the proportion of African American smokers in the Advanced Preparation level was significantly higher than those in the Advanced Maintenance level (36.1% ± 3.7% vs. 26.8% ± 5.5%). However, in 2002, this reversed as the proportion of those in the Advanced Maintenance level increased (33.8% ± 2.2% vs. 41.0% ± 3.0%). The percentage of African American smokers in the Advanced Preparation level fluctuated in 2005 (39.3% ± 5.1%) and 2008 (33.1% ± 4.7%), but the rates across years were not statistically significantly different from each other or from earlier years. After the increase in the proportion of smokers in the Advanced Maintenance level in 2002 just mentioned, the rate remained relatively level in 2005 (42.2% ± 4.1%) and 2008 (43.6% ± 4.1%).
Similar to African American smokers, the proportion of non-Hispanic White smokers in the Advanced Preparation level remained fairly stable across CTS years (1999, 17.7% ± 0.9%; 2002, 17.4% ± 0.8%; 2005, 16.7% ± 1.6%; 2008, 17.1% ± 1.2%). Unlike for African Americans, however, these rates for non-Hispanic Whites were consistently much lower than those for the Advanced Maintenance level (1999, 36.8% ± 1.6%; 2002, 51.9% ± 1.2%; 2005, 54.8% ± 2.9%; 2008, 57.4% ± 2.8%).
There were significantly marked decreases in the proportions of those in the Action level from 1999 to 2002 for both African Americans (1999, 17.2% ± 4.6%; 2002, 7.9% ± 2.6%) and non-Hispanic Whites (1999, 19.8% ± 1.4%; 2002, 7.9% ± 0.9%). The proportions of smokers in the Action level then remained stable on through 2008 for both African Americans (2005, 5.4% ± 2.4%; 2008, 9.7% ± 3.5%) and non-Hispanic Whites (2005, 8.8% ± 1.7%; 2008, 7.1% ± 2.0%). For both racial/ethnic groups, the decreases in the Action level after 1999 corresponded with increases in Advanced Maintenance level.
As shown in Table 2, stratified analyses comparing least square means proportions for each gender-by-age-group stratum revealed statistically significant differences (p < .05) between 1999 and 2008 proportions for the Advanced Preparation, Action, and Advanced Maintenance levels in the QC for both African Americans and non-Hispanic Whites, in general. The most notable exceptions (i.e., where the comparisons of least square means were not statistically significantly different between 1999 and 2008) were among African American females in the 18- to 34-, 35- to 49-, and 50- to 64-year-old age groups and males in the 18- to 34- and 35- to 49-year-old age groups in the Advanced Maintenance level of the QC.
Table 2.
Sex- and Age Group–Adjusted Unweighted Least Square Means Comparing 1999 to 2008 Quitting Continuum Strata, by Race/Ethnicity.
| Sex | Age group (years) | African American, 1999–2008 | Non-Hispanic White, 1999–2008 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
||||||||||
| 1999 LS means | 2008 LS means | LS means difference | p value | [95% CI] | 1999 LS means | 2008 LS means | LS means difference | p value | [95% CI] | ||
| Advanced preparation | |||||||||||
| Female | 18–34 | 0.250 | 0.098 | 0.152 | .001 | [0.065, 0.239] | 0.316 | 0.154 | 0.162 | <.0001 | [0.142, 0.182] |
| 35–49 | 0.372 | 0.086 | 0.286 | <.0001 | [0.204, 0.368] | 0.197 | 0.258 | −0.061 | <.0001 | [−0.085, −0.036] | |
| 50–64 | 0.237 | 0.130 | 0.107 | .019 | [0.018, 0.196] | 0.146 | 0.237 | −0.091 | <.0001 | [−0.118, −0.064] | |
| 65+ | 0.091 | 0.053 | 0.038 | .314 | [−0.036, 0.112] | 0.105 | 0.183 | −0.078 | <.0001 | [−0.105, −0.050] | |
| Male | 18–34 | 0.417 | 0.150 | 0.266 | <.0001 | [0.150, 0.383] | 0.272 | 0.178 | 0.093 | <.0001 | [0.071, 0.116] |
| 35–49 | 0.340 | 0.184 | 0.156 | .006 | [0.045, 0.266] | 0.151 | 0.216 | −0.065 | <.0001 | [−0.089, −0.041] | |
| 50–64 | 0.235 | 0.141 | 0.094 | .068 | [−0.007, 0.194] | 0.085 | 0.163 | −0.078 | <.0001 | [−0.102, −0.053] | |
| 65+ | 0.135 | 0.071 | 0.064 | .195 | [−0.033, 0.161] | 0.060 | 0.099 | −0.039 | .002 | [−0.063, −0.015] | |
| Action | |||||||||||
| Female | 18–34 | 0.081 | 0.013 | 0.068 | <.0001 | [0.062, 0.073] | 0.084 | 0.027 | 0.058 | <.0001 | [0.057, 0.059] |
| 35–49 | 0.049 | 0.018 | 0.031 | <.0001 | [0.027, 0.034] | 0.079 | 0.048 | 0.032 | <.0001 | [0.030, 0.033] | |
| 50–64 | 0.079 | 0.033 | 0.046 | <.0001 | [0.039, 0.052] | 0.108 | 0.049 | 0.060 | <.0001 | [0.058, 0.061] | |
| 65+ | 0.273 | 0.053 | 0.220 | <.0001 | [0.206, 0.234] | 0.150 | 0.055 | 0.095 | <.0001 | [0.093, 0.097] | |
| Male | 18–34 | 0.033 | 0.035 | −0.002 | .508 | [−0.008, 0.004] | 0.081 | 0.028 | 0.053 | <.0001 | [0.052, 0.054] |
| 35–49 | 0.140 | 0.043 | 0.097 | <.0001 | [0.088, 0.107] | 0.087 | 0.052 | 0.035 | <.0001 | [0.033, 0.036] | |
| 50–64 | 0.210 | 0.049 | 0.161 | <.0001 | [0.150, 0.172] | 0.124 | 0.049 | 0.075 | <.0001 | [0.073, 0.076] | |
| 65+ | 0.243 | 0.060 | 0.183 | <.0001 | [0.165, 0.201] | 0.219 | 0.059 | 0.160 | <.0001 | [0.157, 0.163] | |
| Advanced maintenance | |||||||||||
| Female | 18–34 | 0.051 | 0.039 | 0.012 | .223 | [−0.007, 0.032] | 0.107 | 0.066 | 0.041 | .001 | [0.016, 0.065] |
| 35–49 | 0.122 | 0.123 | −0.001 | .971 | [−0.039, 0.038] | 0.176 | 0.225 | −0.049 | .012 | [−0.088, −0.011] | |
| 50–64 | 0.237 | 0.254 | −0.017 | .364 | [−0.054, 0.020] | 0.215 | 0.281 | −0.066 | .001 | [−0.104, −0.027] | |
| 65+ | 0.159 | 0.324 | −0.165 | <.0001 | [−0.209, −0.121] | 0.269 | 0.402 | −0.133 | <.0001 | [−0.181, −0.085] | |
| Male | 18–34 | 0.042 | 0.044 | −0.003 | .802 | [−0.023, 0.018] | 0.083 | 0.048 | 0.035 | .002 | [0.012, 0.057] |
| 35–49 | 0.150 | 0.121 | 0.029 | .174 | [−0.013, 0.072] | 0.171 | 0.203 | −0.032 | .121 | [−0.072, 0.008] | |
| 50–64 | 0.235 | 0.307 | −0.072 | .003 | [−0.119, −0.025] | 0.278 | 0.343 | −0.066 | .004 | [−0.111, −0.020] | |
| 65+ | 0.297 | 0.492 | −0.195 | <.0001 | [−0.259, −0.130] | 0.341 | 0.513 | −0.172 | <.0001 | [−0.232, −0.111] | |
Note. p Values and 95% confidence intervals are calculated for the 1999–2008 LS means difference. LS means = least squares means.
Discussion
While studies have examined differences in quitting rates between African Americans and non-Hispanic Whites, none have studied the population distribution of these smokers along the QC. This is the first study to track changes in the population distribution of smokers along the QC over time to examine progress in shifting a population’s smoking behaviors toward successful quitting, particularly in a state that invested considerably in tobacco control during the period of study. Overall, our findings indicate that there were similar levels of success for both African Americans and non-His-panic Whites in moving the distribution of smokers along the QC in the 2000s. From 1999 to 2002, there were impressive declines in the proportion of smokers in the Action level (i.e., former smokers quit for less than 3 months) that coincided with increases in the Advanced Maintenance level (i.e., former smokers quit for at least 12 months) for both African Americans and non-Hispanic Whites. However, the overall distribution of African American smokers along the QC was less favorable than for non-Hispanic Whites, especially as there were significantly smaller proportions in the Advanced Maintenance level in all CTS years examined. Thus, while both racial/ethnic groups showed marked increases in successful smoking cessation over time, the proportion of African American smokers in the Advanced Maintenance level in 2008 (43.6% ± 4.1%) was significantly less than for non-Hispanic Whites in the same year (57.4% ± 2.8%) and even as far as back in 2002 (51.9% ± 1.2%). This was a major disparity between African Americans and non-Hispanic Whites in the Advanced Maintenance level that widened between 2002 and 2008.
The QC incorporates measures of smoking consumption and quit attempts among current smokers, and our findings revealed that the unadjusted proportion of both African American and non-Hispanic White smokers in the Advanced Preparation level (i.e., low smoking consumption and strong quitting history) remained fairly stable from 1999 to 2008. Reports have found that African Americans are more likely to be light and nondaily smokers and are more likely to make quit attempts compared with non-Hispanic Whites (Bacio, Guzman, Shapiro, & Ray, 2014; Husten, McCarty, Giovino, Chrismon, & Zhu, 1998; Trinidad et al., 2009). Thus, that the proportion of those in this level of the QC for African Americans was approximately double that of non-Hispanic Whites (about 35% compared with about 18%) is not surprising. In 1999, there was a larger proportion of African American smokers in the Advanced Preparation level than there was in the Advanced Maintenance level. Impressively, by 2002, the rate of those in the Advanced Maintenance level had become greater than those in the Advanced Preparation level. However, the relative similarity of the proportions of African American smokers in the Advanced Preparation level to those in the Advanced Maintenance level from 2002 to 2008 is a stark contrast to the distribution among non-His-panic Whites, where there were already much larger proportions of those in the Advanced Maintenance level in 1999 and continued to increase up to 2008. Thus, across survey years African American current smokers were more likely to be light and nondaily smokers and to have made quit attempts in the past year, yet the rates of successful quitting were lower than among non-Hispanic Whites. This suggests that short-term quitting rates were higher among African Americans but rates of successful quitting were lower (i.e., more relapsing). This significant disparity underscores the need to improve efforts designed to advance African American smokers along the quitting continuum and increase successful quitting. These overall findings remained generally significant across gender and age strata for both racial/ethnic groups.
Our findings suggest that large-scale interventions targeting entire population groups may not be as effective for specific sociodemographic groups and that tailored approaches to increase cessation for African Americans may be an important area for continued investigation. There are several tailored cessation programs for African American smokers that have been found to be effective (e.g., Pathways to Freedom; Hooper et al., 2013; Orleans et al., 1998; Robinson, 2006). Perhaps a wider dissemination of such programs could lead to increased population-level cessation for African American smokers. Furthermore, smoking cessation programs targeting light and intermittent smokers (Berg & Schauer, 2012; Cabriales, Cooper, Salgado-Garcia, Naylor, & Gonzalez, 2012) in general could also be beneficial, as could cessation programs geared for long-term assistance and implementation (e.g., at least 6 months duration). Finally, multilevel interventions (i.e., ones that combine population based interventions with individual level interventions) may be important to consider in order to increase successful quitting rates among African Americans.
Previous researchers have shown that ethnic minority smokers are less likely to be prescribed pharmacotherapy by their physicians and are less likely to use such aids in their cessation attempts (Houston, Scarinci, Person, & Greene, 2005; Levinson, Pérez-Stable, Espinoza, Flores, & Byers, 2004; Reed & Burns, 2008; Trinidad et al., 2011). It is possible that the lower rates of successful smoking cessation among African Americans reported here may be related to lower rates of nicotine replacement therapy use relative to non-Hispanic Whites. Future research examining methods used in quitting among African American recent quitters and former smokers is needed.
Limitations
The latest publicly available CTS data are from the 2008 cycle and thus we were not able to examine more recent data. Despite this limitation, the CTS data sets are uniquely important in that they are the only population datasets with detailed measures for the QC since the 1990s. This allowed us to track important trends and disparities in ways previously unexamined. It should be noted that in the CTS smoking status was ascertained by self-report and not validated with biochemical tests, but misclassification of smoking status by using self-report only is unlikely (Caraballo et al., 1998; Pérez-Stable, Marin, Marin, Brody, & Benowitz, 1990). The CTS also did not include measures of African American acculturation levels and thus we were not able to consider this important factor in our research (Klonoff & Landrine, 1999; Landrine & Klonoff, 1996; Webb, 2008).
We were unable to obtain weighted least square means estimates for our stratified analyses because of limitations of the CTS data. Because we used unweighted data, the results presented here can be considered to be more conservative and, thus, caution must be taken in generalizing these results too broadly. We acknowledge that random-digit-dialed telephone surveys may not accurately represent the entire population, as respondents would need to have telephone landlines to participate. Also, over the period indicated, the response rates for the CTS declined and this occurred for other state surveillance systems as well (Biener, Garrett, Gilpin, Roman, & Currivan, 2004). However, a careful analysis indicated that the samples obtained were at least as representative of the population in later years when the household response rates had declined as they were in earlier years when they were higher (Biener et al., 2004). Furthermore, estimates of adult smoking prevalence from the CTS were very similar to state-specific estimates from the Current Population Survey (Bureau of Labor Statistics & U.S. Census Bureau, 2002), which showed much less of a decline in household response rates (Biener et al., 2004).
Implications for Practice
The QC captures movement toward eventual quitting success, from being very unlikely to quit because of very high cigarette consumption and no attempts or intentions to quit all the way to being quit for at least 12 months. Our findings based on the QC indicate that both African American and non-Hispanic White smokers experienced impressive increases in successful smoking cessation over time, but unfortunately the level of success experienced by African American smokers lagged significantly behind that of non-Hispanic Whites. This sizable disparity underscores the need for improved population-level smoking cessation strategies for African American smokers.
Conceptualizations of cigarette addiction and the quitting process, such as the QC, have been generally based on non-Hispanic White populations, who have markedly different smoking patterns than African American smokers, as reported here and by other researchers (DiClemente et al., 1991; Pierce et al., 1998; Shiffman, 2009). The lower smoking consumption levels among African Americans, combined with the lower rates of successful smoking cessation, suggest that cigarette addiction and the quitting process may be different for African American smokers specifically, or light and intermittent smokers generally, than has been traditionally conceived. Thus, the conceptualization of the smoking cessation process may need to be adapted for African American and/or light and intermittent smokers. Such efforts may lead to improved cessation programs and a reduction in the disproportionate burden of smoking-related diseases borne by African Americans.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the National Cancer Institute (grant #1R03CA150559) and the Tobacco-Related Disease Research Program of the University of California Office of the President (grant #21RT-0140).
Footnotes
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Cancer Society. Stay away from tobacco. 2014 Mar 25; Retrieved from http://www.cancer.org/docroot/PED/ped_10_1.asp?sitearea=PED.
- Bacio GA, Guzman IY, Shapiro JR, Ray LA. Differences in quit attempts between non-Hispanic Black and White daily smokers: the role of smoking motives. Addictive Behaviors. 2014;39:1769–1772. doi: 10.1016/j.addbeh.2014.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bal DG, Kizer KW, Felten PG, Mozar HN, Niemeyer D. Reducing tobacco consumption in California. Journal of the American Medical Association. 1990;264:1570–1574. [PubMed] [Google Scholar]
- Berg CJ, Schauer GL. Results of a feasibility and acceptability trial of an online smoking cessation program targeting young adult nondaily smokers. Journal of Environmental and Public Health. 2012;2012:248541. doi: 10.1155/2012/248541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biener L, Garrett CA, Gilpin EA, Roman AM, Currivan DB. Consequences of declining survey response rates for smoking prevalence estimates. American Journal of Preventive Medicine. 2004;27:254–257. doi: 10.1016/j.amepre.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Brandon TH, Collins BN, Juliano LM, Lazev AB. Preventing relapse among former smokers: a comparison of minimal interventions through telephone and mail. Journal of Consulting and Clinical Psychology. 2000;68:103–113. doi: 10.1037//0022-006x.68.1.103. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics & U.S. Census Bureau. Technical Paper 63RV. Washington, DC: U.S. Department of Commerce; 2002. Current population survey: Design and methodology. [Google Scholar]
- Cabriales JA, Cooper TV, Salgado-Garcia F, Naylor N, Gonzalez E., Jr A randomized trial of a brief smoking cessation intervention in a light and intermittent Hispanic sample. Experimental and Clinical Psychopharmacology. 2012;20:410–419. doi: 10.1037/a0029039. [DOI] [PubMed] [Google Scholar]
- Caraballo RS, Giovino GA, Pechacek TF, Mowery PD, Richter PA, Strauss WJ, … Maurer KR. Racial and ethnic differences in serum cotinine levels of cigarette smokers: Third National Health and Nutrition Examination Survey, 1988–1991. Journal of the American Medical Association. 1998;280:135–139. doi: 10.1001/jama.280.2.135. [DOI] [PubMed] [Google Scholar]
- Chow CK, Jolly S, Rao-Melacini P, Fox KA, Anand SS, Yusuf S. Association of diet, exercise, and smoking modification with risk of early cardiovascular events after acute coronary syndromes. Circulation. 2010;121:750–758. doi: 10.1161/CIRCULATIONAHA.109.891523. [DOI] [PubMed] [Google Scholar]
- DiClemente CC, Prochaska JO, Fairhurst SK, Velicer WF, Velasquez MM, Rossi JS. The process of smoking cessation: an analysis of precontemplation, contemplation, and preparation stages of change. Journal of Consulting and Clinical Psychology. 1991;59:295–304. doi: 10.1037//0022-006x.59.2.295. [DOI] [PubMed] [Google Scholar]
- Efron B. The jackknife, the bootstrap and other resampling plans. Philadephia, PA: Society for Industrial and Applied Mathematics; 1982. [Google Scholar]
- Fagan P, Augustson E, Backinger CL, O’Connell ME, Vollinger RE, Jr, Kaufman A, Gibson JT. Quit attempts and intention to quit cigarette smoking among young adults in the United States. American Journal of Public Health. 2007;97:1412–1420. doi: 10.2105/AJPH.2006.103697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flack JM, Ferdinand KC, Nasser SA. Epidemiology of hypertension and cardiovascular disease in African Americans. Journal of Clinical Hypertension. 2003;5:5–11. doi: 10.1111/j.1524-6175.2003.02152.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haiman CA, Stram DO, Wilkens LR, Pike MC, Kolonel LN, Henderson BE, Le Marchand L. Ethnic and racial differences in the smoking-related risk of lung cancer. New England Journal of Medicine. 2006;354:333–342. doi: 10.1056/NEJMoa033250. [DOI] [PubMed] [Google Scholar]
- Harris RE, Zang EA, Anderson JI, Wynder EL. Race and sex differences in lung cancer risk associated with cigarette smoking. International Journal of Epidemiology. 1993;22:592–599. doi: 10.1093/ije/22.4.592. [DOI] [PubMed] [Google Scholar]
- Hooper MW, Larry R, Okuyemi K, Resnicow K, Dietz NA, Robinson RG, Antoni MH. Culturally specific versus standard group cognitive behavioral therapy for smoking cessation among African Americans: an RCT protocol. BMC Psychology. 2013;1:1–9. doi: 10.1186/2050-7283-1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Houston TK, Scarinci IC, Person SD, Greene PG. Patient smoking cessation advice by health care providers: The role of ethnicity, socioeconomic status, and health. American Journal of Public Health. 2005;95:1056–1061. doi: 10.2105/AJPH.2004.039909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husten CG, McCarty MC, Giovino GA, Chrismon JH, Zhu B. Intermittent smokers: A descriptive analysis of persons who have never smoked daily. American Journal of Public Health. 1998;88:86–89. doi: 10.2105/ajph.88.1.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hymowitz N, Cummings KM, Hyland A, Lynn WR, Pechacek TF, Hartwell TD. Predictors of smoking cessation in a cohort of adult smokers followed for five years. Tobacco Control. 1997;6(Suppl 2):S57–S62. doi: 10.1136/tc.6.suppl_2.s57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonoff EA, Landrine H. Acculturation and cigarette smoking among African Americans: replication and implications for prevention and cessation programs. Journal of Behavioral Medicine. 1999;22:195–204. doi: 10.1023/a:1018739616989. [DOI] [PubMed] [Google Scholar]
- Landrine H, Klonoff EA. African American acculturation: Deconstructing race and reviving culture. Thousand Oaks, CA: Sage; 1996. [Google Scholar]
- Levinson AH, Pérez-Stable EJ, Espinoza P, Flores ET, Byers TE. Latinos report less use of pharmaceutical aids when trying to quit smoking. American Journal of Preventive Medicine. 2004;26:105–111. doi: 10.1016/j.amepre.2003.10.012. [DOI] [PubMed] [Google Scholar]
- Okuyemi KS, Ahluwalia JS, Richter KP, Mayo MS, Resnicow K. Differences among African American light, moderate, and heavy smokers. Nicotine & Tobacco Research. 2001;3:45–50. doi: 10.1080/14622200020032097. [DOI] [PubMed] [Google Scholar]
- Orleans CT, Boyd NR, Bingler R, Sutton C, Fairclough D, Heller D, … Fleisher L. A self-help intervention for African American smokers: tailoring cancer information service counseling for a special population. Preventive Medicine. 1998;27(5 Pt 2):S61–S70. doi: 10.1006/pmed.1998.0400. [DOI] [PubMed] [Google Scholar]
- Pérez-Stable EJ, Marin BV, Marin G, Brody DJ, Benowitz NL. Apparent underreporting of cigarette consumption among Mexican American smokers. American Journal of Public Health. 1990;80:1057–1061. doi: 10.2105/ajph.80.9.1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce JP, Farkas AJ, Gilpin EA. Beyond stages of change: The quitting continuum measures progress towards successful smoking cessation. Addiction. 1998;93:277–286. doi: 10.1046/j.1360-0443.1998.93227711.x. [DOI] [PubMed] [Google Scholar]
- Pierce JP, Gilpin EA. A minimum 6-month prolonged abstinence should be required for evaluating smoking cessation trials. Nicotine & Tobacco Research. 2003;5:151–153. doi: 10.1080/0955300031000083427. [DOI] [PubMed] [Google Scholar]
- Prochaska J, DiClemente C. Self change processes, self efficacy and decisional balance across five stages of smoking cessation. Progress in Clinical and Biological Research. 1983;156:131–140. [PubMed] [Google Scholar]
- Reed MB, Burns DM. A population-based examination of racial and ethnic differences in receiving physicians’ advice to quit smoking. Nicotine & Tobacco Research. 2008;10:1487–1494. doi: 10.1080/14622200802323217. [DOI] [PubMed] [Google Scholar]
- Robinson RG. Pathways to freedom: Winning the fight against tobacco. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2006. [Google Scholar]
- SAS Institute. SAS Version 9.3 [Computer software] Cary, NC: Author; 2012. [Google Scholar]
- Shiffman S. Light and intermittent smokers: Background and perspective. Nicotine & Tobacco Research. 2009;11:122–125. doi: 10.1093/ntr/ntn020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sloan FA, Trogdon JG. The impact of the Master Settlement Agreement on cigarette consumption. Journal of Policy Analysis and Management. 2004;23:843–855. doi: 10.1002/pam.20050. [DOI] [PubMed] [Google Scholar]
- Social Sciences Data Collection, University of California San Diego. Final reports, technical documentation, questionnaires and data sets for the California Tobacco Surveys. 1990–2008 Retrieved from http://libraries.ucsd.edu/ssds/tobacco.htm.
- Sung HY, Hu TW, Ong M, Keeler TE, Sheu ML. A major state tobacco tax increase, the master settlement agreement, and cigarette consumption: the California experience. American Journal of Public Health. 2005;95:1030–1035. doi: 10.2105/ajph.2004.042697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinidad DR, Pérez-Stable EJ, Emery SL, White MM, Grana RA, Messer KS. Intermittent and light daily smoking across racial/ethnic groups in the United States. Nicotine & Tobacco Research. 2009;11:203–210. doi: 10.1093/ntr/ntn018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinidad DR, Pérez-Stable EJ, Messer K, White MM, Pierce JP. Menthol cigarettes and smoking cessation among racial/ethnic groups in the United States. Addiction. 2010;105(Suppl 1):84–94. doi: 10.1111/j.1360-0443.2010.03187.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trinidad DR, Pérez-Stable EJ, White MM, Emery SL, Messer K. A nationwide analysis of US racial/ethnic disparities in smoking behaviors, smoking cessation, and cessation-related factors. American Journal of Public Health. 2011;101:699–706. doi: 10.2105/AJPH.2010.191668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Tobacco use among U.S. racial/ethnic minority groups—African Americans, American Indians and Alaska Natives, Asian Americans and Pacific Islanders, and Hispanics: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1998. [Google Scholar]
- U.S. Department of Health and Human Services. Tobacco Control Monograph Series. Vol. 12. Bethesda, MD: Public Health Service, National Institutes of Health, National Cancer Institute; 2000a. Monograph 12: Population based smoking cessation. [Google Scholar]
- U.S. Department of Health and Human Services. Reducing tobacco use. A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2000b. [Google Scholar]
- Webb MS. Does one size fit all African American smokers? The moderating role of acculturation in culturally specific interventions. Psychology of Addictive Behaviors. 2008;22:592–596. doi: 10.1037/a0012968. [DOI] [PubMed] [Google Scholar]
- Webb Hooper M, Rodriguez de Ybarra D, Baker EA. The effect of placebo tailoring on smoking cessation: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2013;81:800–809. doi: 10.1037/a0032469. [DOI] [PubMed] [Google Scholar]
- Yeomans K, Payne KA, Marton JP, Merikle EP, Proskorovsky I, Zou KH, … Willke RJ. Smoking, smoking cessation and smoking relapse patterns: A web-based survey of current and former smokers in the US. International Journal of Clinical Practice. 2011;65:1043–1054. doi: 10.1111/j.1742-1241.2011.02758.x. [DOI] [PubMed] [Google Scholar]
- Zhu S, Melcer T, Sun J, Rosbrook B, Pierce JP. Smoking cessation with and without assistance: A population-based analysis. American Journal of Preventive Medicine. 2000;18:305–311. doi: 10.1016/S0749-3797(00)00124-0. [DOI] [PubMed] [Google Scholar]