Abstract
Electronic cigarette (e-cigarette) use has gained recent widespread popularity and acceptance in the general population. What effect e-cigarettes may have on pediatric health remains unknown. Although many jurisdictions have laws that prevent the sale of e-cigarettes to minors and the use of e-cigarettes in public places, infants, children, and adolescents are increasingly exposed to them. In this pediatric-focused review, we discuss the history of these devices, user demographics, known health effects, and current legislative efforts to protect minors from exposure.
Electronic cigarettes (e-cigarettes) are designed to deliver vaporized nicotine for absorption through the respiratory tract through noncombustible means. The current incarnation of the e-cigarette was developed in China in 2003 and introduced in China in 2004, Europe in 2006, and the United States in 2007. Conventional cigarette manufacturer Philip Morris conducted research with e-cigarettes as early as the 1990s.1,2 The basic components of an e-cigarette include a cartridge containing a nicotine solution, a heating element that vaporizes the solution, and a power source for the heating element, which is frequently a rechargeable lithium battery (Figure). Activation of the e-cigarette through inspiration by the user or manual activation with a button triggers the delivery of a vaporized nicotine solution that can be inhaled (termed vaping).
Figure. Schematic of an Electronic Cigarette (E-cigarette).
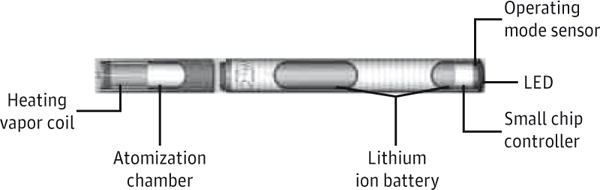
This schematic depicts a disposable e-cigarette. Electronic cigarettes with refillable or replaceable cartridges typically have the cartridge on the end of the e-cigarette with the heating vapor coil. LED indicates light-emitting diode. Adapted from Wollscheid and Kremzner.3
Some e-cigarettes are single-use devices, whereas others have replaceable or refillable cartridges. In addition, larger commercially available devices known as tanks can operate with higher voltages and can release carcinogens, such as formaldehyde, in levels similar to those of conventional tobacco smoke.4 In addition to commercially available devices, some e-cigarette users build or modify their own devices, known as personal vaporizers or mechanical mods. The lack of uniformity among devices can lead to differences in vapor particle size and deposition in the respiratory tract, even when the same nicotine solution is used.5 This lack of uniformity in turn can provide a different user experience in terms of vapor production, systemic absorption of nicotine and nicotine solution components, and “throat hit,”6 that is, the sensation a user experiences in the oropharynx and lungs during inhalation of vapor.
The nicotine solutions for e-cigarettes are commercially available in several different concentrations of nicotine, ranging from 0% to 3.6%. However, studies have shown discrepancies in the actual content of nicotine vs the reported content, with variation ranging from 1% to 31% for different batches of the same brand of e-cigarettes.7,8 In addition, variable systemic absorption of nicotine can occur, even with similar concentrations of nicotine solutions, with naive users absorbing less nicotine compared with experienced users owing to different patterns of inhalation.9 The e-cigarette solutions may also contain flavorings, such as traditional tobacco blends, menthol, and nontraditional flavorings (eg, bubble gum, cocktail, and candy flavors). Whether these additives have the potential to produce toxic byproducts during vaping has not been determined. In addition, electronic nicotine delivery systems have been used for vaping nonnicotine substances,10 including the active ingredients in marijuana. Because of the lack of regulations governing manufacturing and sales of these devices and the variability among electronic nicotine delivery systems, their components, and their solutions,11 the health risks associated with e-cigarette use and bystander exposure are not understood completely.
User Demographics
Among adolescents and adults, the rates of awareness and first use of e-cigarettes have doubled from 2008 through 2012.12 From 2011 through 2012 among middle school students in the United States, e-cigarette use (ever) increased from 1.4% to 2.7%, and current use (defined as any use within the past 30 days) increased from 0.6% to 1.1%. For high school students, ever use increased from 4.7% to 10.0%, and current use increased from 1.5% to 2.8%(P < .05 for all).13 As of 2011, awareness among US adults was 57.9%, with 6.2% of adults reporting ever having used them.14 The prevalence of trying e-cigarettes is higher among smokers of conventional cigarettes compared with former smokers and those who never smoked.12,14 The International Tobacco Four-Country Survey (the United States, the United Kingdom, Canada, and Australia)1 found that awareness of e-cigarettes was associated with being a heavy smoker (>1 pack a day), white, male, and young (18–24 years); with having a moderate educational level; and with having a moderate to high income. On the other hand, trying an e-cigarette was associated with being a nondaily smoker, female, and young; with having a high income level; and with perceiving reduced harm compared with conventional cigarettes. In the same survey, current use was associated with being a smoker and having a high educational level.
Adolescent characteristics associated with ever using e-cigarettes have also been reported to be different from those of adults. The proportion of adults who have never smoked but who have tried e-cigarettes was reportedly lower than the same proportion of adolescents.15 A recent survey of more than 15 000 US adolescents in grades 6 through 12 found that e-cigarette use was significantly lower in girls and in African American and Hispanic youth and higher for those who smoked conventional cigarettes or who had friends who smoked.16 Among older adolescent children of alcoholic fathers, Lessard and colleagues17 reported that e-cigarette use was associated with current use of cigarettes, alcohol, and marijuana. In another study,18 adolescent users of e-cigarettes were found to be just as likely as tobacco users to report the use of alcohol, cigars, smokeless tobacco, and marijuana but were more likely to report the use of blunt wraps and hookahs. Common locations for adolescent use of e-cigarettes based on focus group data from male high school students in the US Southwest include everywhere (38%), school bathrooms (26%), home (21%), school staircases (11%), and school cafeterias (4%).19
Although 76.3% of adolescent e-cigarette users also smoke conventional cigarettes,13,20 recent analyses of data from the National Youth Tobacco survey21 (adolescents in grades 6–12) revealed that the use of e-cigarettes increased from 79 000 to more than 263 000 (0.9% of the nonsmoking youth population who use e-cigarettes) from 2011 through 2013 among US youths who have never smoked cigarettes. This 3-fold increase in e-cigarette use among adolescents who have never smoked suggests increased acceptance of e-cigarettes in this population. Whether widespread e-cigarette acceptance in the adolescent population will increase addiction to nicotine is unknown.
Health Risks of Primary Exposure to E-cigarettes
Few studies have examined the short- and long-term health effects of e-cigarettes on primary users. One study22 reported higher levels of exhaled nitric oxide in e-cigarette users, suggesting that e-cigarettes can cause airway inflammation. Other studies in adults23,24 have found minimal acute cardiovascular and pulmonary effects in adult e-cigarettes users. Although nicotine exposure by itself does not cause tumors, it has been shown to promote tumor growth and metastasis.25 Therefore, whether the long-term use of e-cigarettes can increase the risk for malignant disease in people with a predisposition for tumor development is unknown. Addiction to nicotine is also a potential concern for e-cigarette users because of the high nicotine content in many e-cigarette solutions. A study in adolescents who smoke conventional cigarettes found that certain subgroups of smokers were more likely to become addicted to nicotine.26 Nicotine dependence occurs in several stages, beginning with experimentation and leading to long-term use, abuse, and dependence in susceptible individuals.27 Symptoms in experimental or nondaily smokers that predicted an increased likelihood of becoming daily smokers at 48 months included the need to smoke in the morning, choosing to spend money on smoking instead of lunch, smoking when ill, and smoking when it was forbidden. Whether these same subgroups of adolescents will be at risk for nicotine addiction when trying or using e-cigarettes remains unclear.
Although some manufacturers of e-cigarette liquids describe their products as being made from US Pharmacopeial Convention– or food-grade ingredients, the inhalational properties of the chemical compounds have not been assessed. The carrier agents and flavorings may also have health effects independent of those of nicotine. Known and suspected carcinogens, such as formaldehyde, acetaldehyde, and acrolein, are generated when carrier agents, such as propylene glycol or vegetable glycerin, are heated to high temperatures.28 Although the primary components of vaporization for e-cigarettes are nicotine and its carrier agent, e-cigarette solutions may contain flavoring agents and other chemicals, some of which are known carcinogens. Chromatographic and spectroscopic analysis of 12 brands of e-cigarettes detected the presence of several groups of known toxins and/or carcinogens, including carbonyls, volatile organic compounds, nitrosamines, and heavy metals, albeit in levels lower than those found in conventional cigarette smoke.28
Health Risks of Secondary, Tertiary, and Unintentional Exposure to E-cigarettes
There are limited data about the health effects on a bystander exposed to secondary e-cigarette vapor. In contrast to conventional cigarettes, secondary exposure to e-cigarette vapor does not involve exposure to combustion byproducts, and e-cigarettes reportedly generate minimal sidestream emissions.29 Although the exposure to the exhalant vapors of e-cigarettes may be less harmful than exposure to those of conventional cigarettes, recent studies suggest that e-cigarette vapor may not be entirely harmless. Schober and colleagues22 reported an increase in the concentration of particle numbers, 1,2-propanediol, glycerin, and nicotine in indoor air during sessions of e-cigarette use. Previously, Schripp and colleagues30 also found increased levels of 1,2-propanediol, diacetin, and nicotine by gas chromatography from 1 exhaled e-cigarette puff delivered by a user. Indoor nicotine levels and particle concentrations generated by e-cigarette users have been shown to be higher than background levels but lower than levels generated by conventional cigarette smoking.29,31 Nevertheless, Flouris and colleagues24 reported similar levels of serum cotinine in adults passively exposed to e-cigarettes compared with adults exposed to secondary tobacco smoke. Ballbè and colleagues32 also reported similar salivary and urine cotinine levels in nonsmokers who were exposed to e-cigarette emissions or conventional cigarettes. Another study documented higher particulate levels with e-cigarettes containing nicotine-free solutions compared with those containing nicotine,31 suggesting that the use of e-cigarettes with flavored non–nicotine-containing solutions may still pose a risk to bystanders. The potential for tertiary (or thirdhand) exposure from e-cigarettes has been demonstrated recently by Goniewicz and Lee,33 who reported measurable nicotine levels in samples from hard surfaces exposed to e-cigarette emissions. In summary, the currently available data suggest that indirect exposure to e-cigarette vapor may result in exposure of nonusers to toxic compounds through secondary and tertiary exposure.
For now, no data are available concerning the effects of maternal e-cigarette use on the developing fetus or neonate. In animal studies,34 exposure to nicotine during fetal development has been associated with lung abnormalities. Children exposed to maternal smoking have been reported to have a higher incidence of wheezing in early life.35,36 Other studies in rodents34,37,38 have demonstrated that nicotine exposure in utero and during neonatal life can inhibit alveolar growth and cause histologic changes similar to those caused by emphysema. Disruption of lung vascularization due to fetal and neonatal nicotine exposure has also been reported in a rodent model.39
Behavioral abnormalities have been reported in the offspring of mothers who smoked during pregnancy.34 The development of attention-deficit/hyperactivity disorder in children has been shown to be associated with maternal smoking during pregnancy, whereas rodent models have demonstrated increased hyperactivity in offspring with prenatal exposure to nicotine.40 In neonatal rats, Huang and colleagues41 reported hippocampal changes with chronic neonatal nicotine exposure, possibly accounting for cognitive changes caused by nicotine exposure. The effect of in utero and postnatal exposure to e-cigarette emissions on the health of neonates and infants remains unknown. However, infants can absorb nicotine through multiple exposure routes, including inhalation, skin absorption, oral ingestion, and breast milk.42,43 Higher urine levels of cotinine (>10-fold) have been reported in breastfed infants of mothers who smoked more than 5 cigarettes a day compared with bottle-fed infants of mothers who smoked.44 Because rapid brain and lung development takes place during early life, exposure to nicotine through e-cigarette emissions may cause adverse health concerns in this particularly vulnerable age group.
Unintentional exposure to nicotine-containing e-cigarette solutions is also an emerging health hazard. The Centers for Disease Control and Prevention reported that calls per month related to e-cigarette exposure had dramatically increased from 1 in September 2010 to 215 in February 2014.45 These calls by February 2014 accounted for 41.7% of the combined monthly calls related to cigarettes and e-cigarettes. Exposure to e-cigarettes affected primarily individuals younger than 5 years (51.1%) and older than 20 years (42.0%). Commonly reported exposures included ingestion of solutions (68.9%), inhalation (16.8%), eye exposure (8.5%), and dermal exposure (5.9%). In addition, an adverse health effect was reported in 57.8% of the calls for which severity information was recorded; commonly reported effects included emesis, nausea, and eye irritation. Many of these exposures may be preventable if childproof containers were in use, but such containers are not currently required by federal law. One suicide via intravenous injection of a nicotine solution was also reported by the Centers for Disease Control and Prevention.45 Finally, reported incidents of lithium battery explosions with recharging, leading to fires and burns, have been acknowledged by the industry.46 More studies in children are needed to determine the effect of e-cigarette exposure on childhood health, including the risk for and consequences of accidental nicotine exposures from e-cigarette solutions.47
User and Clinician Perceptions
Many adult users of conventional cigarettes believe e-cigarettes to be less harmful than conventional cigarettes, but this percentage is decreasing with time from 84.7% in 2010 to 65.0% in 2012.48 A national survey of 24 000 youth in grades 6 through 12 found that 30.6% believed that e-cigarettes were less harmful than conventional cigarettes, and 18.6% believed that they were equally or more harmful, with the remaining 50.8% reporting that they had not heard of or did not know enough about e-cigarettes.49 Focus groups of male high school students suggested that common reasons for adolescent use of e-cigarettes included concealment (40%), social approval (26%), harm reduction compared with conventional cigarettes (19%), and lack of odor compared with conventional cigarettes (15%).19
Unfortunately, available data suggest that clinicians may not be informed adequately regarding the use of e-cigarettes and their potential effects on health. A 2013 survey of clinicians who treated adolescents in Minnesota50 stated that 92% of respondents were aware of e-cigarettes, but most (83.1%) described knowing nothing to a little about e-cigarettes, and only 24% had heard of e-cigarettes through professional sources. Although little research has been published on the short- and long-term safety of e-cigarettes, most clinicians in that study agreed that e-cigarettes were safer than conventional cigarettes (65.5%). Those who believed that e-cigarettes were safer were less likely to believe that discussing their use with patients or their parents was important. In terms of potential prenatal counseling, a 2012 survey of members of the American College of Obstetricians and Gynecologists51 reported that only 5% of respondents described themselves as fully informed about e-cigarettes. Of those surveyed, 29.0% reported that e-cigarettes were safer than conventional cigarettes, and 13.5% believed that they had no health effects at all. From the observation that people usually smoke before progressing to the use of illicit drugs, recent animal studies52,53 have demonstrated that nicotine can augment the potential for cocaine addiction by increasing activation of nicotinic acetylcholine receptors in the amygdala. Whether the use of nicotine-containing e-cigarettes by adolescents who have never smoked will increase the prevalence of illicit drug use in this population is unknown.
Economics and Marketing of E-cigarettes
In the late 2000s, multiple small businesses launched the sales and marketing of e-cigarettes,54 with most of these small businesses focusing on a single e-cigarette and/or product. However, with the growing popularity of e-cigarettes, all of the major international corporations that sell conventional cigarettes have purchased e-cigarette brands or introduced their own brands, including Green Smoke and MarkTen (Phillip Morris/Altria), Vuse (Reynolds American/Lorillard), Vype (British American Tobacco), Puritane (Imperial Tobacco), and Blu (Lorillard sale pending to Imperial Tobacco). With the entry of these corporations into the marketplace, 10 companies are estimated to hold more than 70% of the US market share.54 Bloomberg Industries55 estimates that global sales were $3.5 billion in 2013 and expected to rise to $7.5 billion in 2015. A Bloomberg Industries projection54 suggests that sales of e-cigarettes could exceed those of conventional cigarettes by as early as 2023. In addition, e-cigarettes are becoming more readily available as the percentage of tobacco-selling retailers also selling e-cigarettes increased from 24.7% to 59.9% from 2012 to 2013 in a study conducted in Virginia and North Carolina.56 In contrast to conventional cigarettes, which are taxed at the federal and state levels (and within some local jurisdictions) throughout the United States, government taxation on e-cigarettes is limited to state taxes only in Minnesota and North Carolina.57
Despite the potential health risks to children posed by e-cigarette use and nicotine addiction, advertisements for e-cigarettes can be seen readily by minors in the United States. Exposure to e-cigarette advertisements on television (primarily cable) has been estimated to have increased by 256% from 2011 through 2013 for youth aged 12 to 17 years.58 As much as 8.0% of the online audience for e-cigarette advertisements is estimated to be younger than 18 years, and some advertisement occurs on websites, where as many as 35% of the audience may be younger than 18 years.59 No federal restrictions on e-cigarette advertising currently exist in the United States. More problematic, however, is that some marketing of e-cigarettes has been targeted at children according to the US Food and Drug Administration (FDA),2,60 which specifically cites the fact that candy and fruit flavors are “especially attractive to children and young adults.”60(p23146) A 2014 US Congressional investigation stated that: “The findings of this investigation reveal that e-cigarette companies may indeed be taking advantage of the regulatory vacuum that currently exists to market their products to youth.”61(p2871)
E-cigarettes as a Cessation Tool
Advertisements for e-cigarettes often indirectly reference smoking cessation to promote the purchase of e-cigarettes.59,62 A cross-sectional survey of more than 5000 smokers in the United Kingdom who had attempted to quit using conventional cigarettes found that those using e-cigarettes were more likely to report abstinence than those who used nicotine replacement therapies (adjusted odds ratio, 1.63 [95% CI, 1.17–2.27]) or no aid at all (adjusted odds ratio, 1.61 [95% CI, 1.19–2.18]).63 However, randomized clinical trials have not established an overwhelming benefit to recommend e-cigarettes as a superior method for cessation. A randomized clinical trial of 657 conventional cigarette users in New Zealand64 found no difference in abstinence rates between those randomized to e-cigarettes vs those randomized to nicotine transdermal patches. Another trial of 300 Italian users of conventional cigarettes65 found no difference in abstinence rates between those randomized to receive 1 of 2 nicotine-containing e-cigarettes vs those who received non–nicotine-containing e-cigarettes. A recent survey of more than 15 000 US adolescents in grades 6 through 1216 (of whom 3.2% of respondents reporting having used e-cigarettes) found that e-cigarette use was higher among conventional cigarette users (adjusted odds ratio, 58.44 [95% CI, 34.71–98.39]) but that e-cigarette use was not associated with a desire to quit using conventional cigarettes or with recent quit attempts. To our knowledge, no published studies have reported on the effectiveness of e-cigarettes as a means for cessation of conventional cigarette use in adolescents.
E-cigarette Legislation
A July 2014 position statement from the Forum of International Respiratory Societies2 (which includes the American College of Chest Physicians and the American Thoracic Society) called for precautionary restrictions or bans on electronic nicotine delivery devices until more information on their safety is available. Although an August 2014 policy statement from the American Heart Association23(p421) stated that “[e]ven if there are some intrinsic adverse health effects of e-cigarettes, there would be public benefit if e-cigarettes proved to be much less hazardous than combustible cigarettes and if smokers could switch entirely from conventional cigarettes to e-cigarettes,” the American Heart Association supported FDA regulation of e-cigarettes covering marketing, youth access, quality control, and so on.
Although the sales of all e-cigarettes are prohibited in some countries (eg, Brazil and Mexico), sales of only nicotine-containing e-cigarettes are banned in others (eg, Australia and Canada), and sales to minors will be prohibited across the European Union by 2016, no federal regulations address marketing and sales to minors in the United States.23 In the absence of federal regulation, as of October 2014, 41 states have statutes prohibiting the sale of e-cigarettes to minors.66 Although many US municipalities have banned e-cigarette use in workplaces, only 3 states (New Jersey, North Dakota, and Utah) and the District of Columbia have banned workplace use statewide.
In April 2014, the FDA issued a proposed rule for comments on whether to regulate e-cigarettes and additional tobacco products, including cigars, pipe tobacco, certain dissolvables that are not “smokeless tobacco,” gels, and water pipe tobacco. The proposed regulations for e-cigarettes would ban sales to minors, require health warnings on packaging, require manufacturers to register with the FDA and report ingredients, and allow manufacturers to make health claims (such as being a cessation aid) only if the FDA confirms that the scientific evidence supports the claim.60 The proposed rules would not ban flavoring or advertisements. This proposal will be finalized after the FDA completes review of the public commentary.
Conclusions
Use of e-cigarettes has recently gained widespread popularity and acceptance in the general population, and the possible effect on pediatric health is unknown. Although many jurisdictions have laws that prevent sales of e-cigarettes to minors and use of e-cigarettes in public places, children and adolescents are increasingly exposed to e-cigarettes. Studies are needed to determine the effect of e-cigarette use and exposure on pediatric health in utero through adolescence. In the absence of data regarding risks to health, pediatricians and other clinicians should assess exposure to e-cigarettes as part of a history of secondary smoke exposure and be prepared to counsel on eliminating this exposure. In addition, given the potential risk for nicotine addiction, clinicians should be prepared to ask adolescents about e-cigarette use as part of a social assessment and to discuss the potential health risks associated with using e-cigarettes and vaporizers for other substances.
Footnotes
Author Audio Interview at jamapediatrics.com
Author Contributions: Dr Collaco and McGrath-Morrow had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: All authors.
Acquisition, analysis, or interpretation of data: Drummond.
Drafting of the manuscript: Collaco, McGrath-Morrow.
Critical revision of the manuscript for important intellectual content: All authors.
Administrative, technical, or material support: All authors.
Study supervision: McGrath-Morrow.
Conflict of Interest Disclosures: Drs Collaco and McGrath-Morrow have received funding from the American Academy of Pediatrics to study the health effects of e-cigarette exposure. No other disclosures were reported.
References
- 1.Adkison SE, O’Connor RJ, Bansal-Travers M, et al. Electronic nicotine delivery systems: International Tobacco Control Four-Country Survey. Am J Prev Med. 2013;44(3):207–215. doi: 10.1016/j.amepre.2012.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schraufnagel DE, Blasi F, Drummond MB, et al. Forum of International Respiratory Societies Electronic cigarettes: a position statement of the Forum of International Respiratory Societies. Am J Respir Crit Care Med. 2014;190(6):611–618. doi: 10.1164/rccm.201407-1198PP. [DOI] [PubMed] [Google Scholar]
- 3.Wollscheid KA, Kremzner ME. Electronic cigarettes: safety concerns and regulatory issues. Am J Health Syst Pharm. 2009;66(19):1740–1742. doi: 10.2146/ajhp090127. [DOI] [PubMed] [Google Scholar]
- 4.Kosmider L, Sobczak A, Fik M, et al. Carbonyl compounds in electronic cigarette vapors: effects of nicotine solvent and battery output voltage. Nicotine Tob Res. 2014;16(10):1319–1326. doi: 10.1093/ntr/ntu078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Williams M, Talbot P. Variability among electronic cigarettes in the pressure drop, airflow rate, and aerosol production. Nicotine Tob Res. 2011;13(12):1276–1283. doi: 10.1093/ntr/ntr164. [DOI] [PubMed] [Google Scholar]
- 6.Farsalinos KE, Spyrou A, Tsimopoulou K, Stefopoulos C, Romagna G, Voudris V. Nicotine absorption from electronic cigarette use: comparison between first and new-generation devices. Sci Rep. 2014;4:4133. doi: 10.1038/srep04133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Palazzolo DL. Electronic cigarettes and vaping: a new challenge in clinical medicine and public health: a literature review. Front Public Health. 2013;1:56. doi: 10.3389/fpubh.2013.00056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goniewicz ML, Hajek P, McRobbie H. Nicotine content of electronic cigarettes, its release in vapour and its consistency across batches: regulatory implications. Addiction. 2014;109(3):500–507. doi: 10.1111/add.12410. [DOI] [PubMed] [Google Scholar]
- 9.Farsalinos KE, Romagna G, Tsiapras D, Kyrzopoulos S, Voudris V. Evaluation of electronic cigarette use (vaping) topography and estimation of liquid consumption: implications for research protocol standards definition and for public health authorities’ regulation. Int J Environ Res Public Health. 2013;10(6):2500–2514. doi: 10.3390/ijerph10062500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malouff JM, Rooke SE, Copeland J. Experiences of marijuana-vaporizer users. Subst Abuse. 2014;35(2):127–128. doi: 10.1080/08897077.2013.823902. [DOI] [PubMed] [Google Scholar]
- 11.Shihadeh A, Eissenberg T. Electronic cigarette effectiveness and abuse liability: predicting and regulating “nicotine flux” [published online September 1, 2014] Nicotine Tob Res. doi: 10.1093/ntr/ntu175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129(19):1972–1986. doi: 10.1161/CIRCULATIONAHA.114.007667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention (CDC) Notes from the field: electronic cigarette use among middle and high school students: United States, 2011–2012. MMWR Morb Mortal Wkly Rep. 2013;62(35):729–730. [PMC free article] [PubMed] [Google Scholar]
- 14.King BA, Alam S, Promoff G, Arrazola R, Dube SR. Awareness and ever-use of electronic cigarettes among US adults, 2010–2011. Nicotine Tob Res. 2013;15(9):1623–1627. doi: 10.1093/ntr/ntt013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Carroll Chapman SL, Wu LT. E-cigarette prevalence and correlates of use among adolescents versus adults: a review and comparison. J Psychiatr Res. 2014;54:43–54. doi: 10.1016/j.jpsychires.2014.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lippert AM. Do adolescent smokers use e-cigarettes to help them quit? the sociodemographic correlates and cessation motivations of US adolescent e-cigarette use [published online June 26, 2014] Am J Health Promot. doi: 10.4278/ajhp.131120-QUAN-595. [DOI] [PubMed] [Google Scholar]
- 17.Lessard J, Henrie J, Livingston JA, Leonard KE, Colder CR, Eiden RD. Correlates of ever having used electronic cigarettes among older adolescent children of alcoholic fathers [published online August 30, 2014[ Nicotine Tob Res. doi: 10.1093/ntr/ntu148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Camenga DR, Kong G, Cavallo DA, et al. Alternate tobacco product and drug use among adolescents who use electronic cigarettes, cigarettes only, and never smokers. J Adolesc Health. 2014;55(4):588–591. doi: 10.1016/j.jadohealth.2014.06.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peters RJ, Jr, Meshack A, Lin MT, Hill M, Abughosh S. The social norms and beliefs of teenage male electronic cigarette use. J Ethn Subst Abuse. 2013;12(4):300–307. doi: 10.1080/15332640.2013.819310. [DOI] [PubMed] [Google Scholar]
- 20.Dutra LM, Glantz SA. Electronic cigarettes and conventional cigarette use among US adolescents: a cross-sectional study. JAMA Pediatr. 2014;168(7):610–617. doi: 10.1001/jamapediatrics.2013.5488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bunnell RE, Agaku IT, Arrazola R, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011–2013 [published online August 20, 2014] Nicotine Tob Res. doi: 10.1093/ntr/ntu166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schober W, Szendrei K, Matzen W, et al. Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. Int J Hyg Environ Health. 2014;217(6):628–637. doi: 10.1016/j.ijheh.2013.11.003. [DOI] [PubMed] [Google Scholar]
- 23.Bhatnagar A, Whitsel LP, Ribisl KM, et al. American Heart Association Advocacy Coordinating Committee, Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research Electronic cigarettes: a policy statement from the American Heart Association. Circulation. 2014;130(16):1418–1436. doi: 10.1161/CIR.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Flouris AD, Chorti MS, Poulianiti KP, et al. Acute impact of active and passive electronic cigarette smoking on serum cotinine and lung function. Inhal Toxicol. 2013;25(2):91–101. doi: 10.3109/08958378.2012.758197. [DOI] [PubMed] [Google Scholar]
- 25.Schaal C, Chellappan SP. Nicotine-mediated cell proliferation and tumor progression in smoking-related cancers. Mol Cancer Res. 2014;12(1):14–23. doi: 10.1158/1541-7786.MCR-13-0541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rose JS, Lee CT, Dierker LC, Selya AS, Mermelstein RJ. Adolescent nicotine dependence symptom profiles and risk for future daily smoking. Addict Behav. 2012;37(10):1093–1100. doi: 10.1016/j.addbeh.2012.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jasinska AJ, Zorick T, Brody AL, Stein EA. Dual role of nicotine in addiction and cognition: a review of neuroimaging studies in humans. Neuropharmacology. 2014;84:111–122. doi: 10.1016/j.neuropharm.2013.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133–139. doi: 10.1136/tobaccocontrol-2012-050859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Czogala J, Goniewicz ML, Fidelus B, Zielinska-Danch W, Travers MJ, Sobczak A. Secondhand exposure to vapors from electronic cigarettes. Nicotine Tob Res. 2014;16(6):655–662. doi: 10.1093/ntr/ntt203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schripp T, Markewitz D, Uhde E, Salthammer T. Does e-cigarette consumption cause passive vaping? Indoor Air. 2013;23(1):25–31. doi: 10.1111/j.1600-0668.2012.00792.x. [DOI] [PubMed] [Google Scholar]
- 31.Ruprecht AA, De Marco C, Pozzi P, et al. Comparison between particulate matter and ultrafine particle emission by electronic and normal cigarettes in real-life conditions. Tumori. 2014;100(1):e24–e27. doi: 10.1700/1430.15833. [DOI] [PubMed] [Google Scholar]
- 32.Ballbè M, Martínez-Sánchez JM, Sureda X, et al. Cigarettes vs e-cigarettes: passive exposure at home measured by means of airborne marker and biomarkers. Environ Res. 2014;135C:76–80. doi: 10.1016/j.envres.2014.09.005. [DOI] [PubMed] [Google Scholar]
- 33.Goniewicz ML, Lee L. Electronic cigarettes are a source of thirdhand exposure to nicotine [published online August 30, 2014[ Nicotine Tob Res. doi: 10.1093/ntr/ntu152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maritz GS, Harding R. Life-long programming implications of exposure to tobacco smoking and nicotine before and soon after birth: evidence for altered lung development. Int J Environ Res Public Health. 2011;8(3):875–898. doi: 10.3390/ijerph8030875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neuman Å, Hohmann C, Orsini N, et al. ENRIECO Consortium Maternal smoking in pregnancy and asthma in preschool children: a pooled analysis of eight birth cohorts. Am J Respir Crit Care Med. 2012;186(10):1037–1043. doi: 10.1164/rccm.201203-0501OC. [DOI] [PubMed] [Google Scholar]
- 36.Duijts L, Jaddoe VW, van der Valk RJ, et al. Fetal exposure to maternal and paternal smoking and the risks of wheezing in preschool children: the Generation R Study. Chest. 2012;141(4):876–885. doi: 10.1378/chest.11-0112. [DOI] [PubMed] [Google Scholar]
- 37.Maritz GS, Rayise SS. Effect of maternal nicotine exposure on neonatal rat lung development: protective effect of maternal ascorbic acid supplementation. Exp Lung Res. 2011;37(1):57–65. doi: 10.3109/01902148.2010.515650. [DOI] [PubMed] [Google Scholar]
- 38.Miller MD, Marty MA. Impact of environmental chemicals on lung development. Environ Health Perspect. 2010;118(8):1155–1164. doi: 10.1289/ehp.0901856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Petre MA, Petrik J, Ellis R, Inman MD, Holloway AC, Labiris NR. Fetal and neonatal exposure to nicotine disrupts postnatal lung development in rats: role of VEGF and its receptors. Int J Toxicol. 2011;30(2):244–252. doi: 10.1177/1091581810395332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abbott LC, Winzer-Serhan UH. Smoking during pregnancy: lessons learned from epidemiological studies and experimental studies using animal models. Crit Rev Toxicol. 2012;42(4):279–303. doi: 10.3109/10408444.2012.658506. [DOI] [PubMed] [Google Scholar]
- 41.Huang LZ, Abbott LC, Winzer-Serhan UH. Effects of chronic neonatal nicotine exposure on nicotinic acetylcholine receptor binding, cell death and morphology in hippocampus and cerebellum. Neuroscience. 2007;146(4):1854–1868. doi: 10.1016/j.neuroscience.2007.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Valcke M, Krishnan K. Evaluation of the impact of the exposure route on the human kinetic adjustment factor. Regul Toxicol Pharmacol. 2011;59(2):258–269. doi: 10.1016/j.yrtph.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 43.Xue J, Zartarian V, Moya J, et al. A meta-analysis of children’s hand-to-mouth frequency data for estimating nondietary ingestion exposure. Risk Anal. 2007;27(2):411–420. doi: 10.1111/j.1539-6924.2007.00893.x. [DOI] [PubMed] [Google Scholar]
- 44.Schulte-Hobein B, Schwartz-Bickenbach D, Abt S, Plum C, Nau H. Cigarette smoke exposure and development of infants throughout the first year of life: influence of passive smoking and nursing on cotinine levels in breast milk and infant’s urine. Acta Paediatr. 1992;81(6–7):550–557. doi: 10.1111/j.1651-2227.1992.tb12293.x. [DOI] [PubMed] [Google Scholar]
- 45.Chatham-Stephens K, Law R, Taylor E, et al. Centers for Disease Control and Prevention (CDC) Notes from the field: calls to poison centers for exposures to electronic cigarettes: United States, September 2010–February 2014. MMWR Morb Mortal Wkly Rep. 2014;63(13):292–293. [PMC free article] [PubMed] [Google Scholar]
- 46.Parker LG, Green R. Small number of e-cigarette batteries explode. NBC5 Investigates. 2013 http://www.nbcchicago.com/investigations/Exploding-E-Cigarettes-229183561.html. Accessed August 5, 2014.
- 47.Durmowicz EL. The impact of electronic cigarettes on the paediatric population. Tob Control. 2014;23(suppl 2):ii41–ii46. doi: 10.1136/tobaccocontrol-2013-051468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tan AS, Bigman CA. E-cigarette awareness and perceived harmfulness: prevalence and associations with smoking-cessation outcomes. Am J Prev Med. 2014;47(2):141–149. doi: 10.1016/j.amepre.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ambrose BK, Rostron BL, Johnson SE, et al. Perceptions of the relative harm of cigarettes and e-cigarettes among US youth. Am J Prev Med. 2014;47(2 suppl 1):S53–S60. doi: 10.1016/j.amepre.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pepper JK, McRee AL, Gilkey MB. Healthcare providers’ beliefs and attitudes about electronic cigarettes and preventive counseling for adolescent patients. J Adolesc Health. 2014;54(6):678–683. doi: 10.1016/j.jadohealth.2013.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.England LJ, Anderson BL, Tong VT, et al. Screening practices and attitudes of obstetricians-gynecologists toward new and emerging tobacco products [published online May 29, 2014] Am J Obstet Gynecol. doi: 10.1016/j.ajog.2014.05.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Levine A, Huang Y, Drisaldi B, et al. Molecular mechanism for a gateway drug: epigenetic changes initiated by nicotine prime gene expression by cocaine. Sci Transl Med. 2011;3(107):107ra109. doi: 10.1126/scitranslmed.3003062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Huang YY, Kandel DB, Kandel ER, Levine A. Nicotine primes the effect of cocaine on the induction of LTP in the amygdala. Neuropharmacology. 2013;74:126–134. doi: 10.1016/j.neuropharm.2013.03.031. [DOI] [PubMed] [Google Scholar]
- 54.McArdle M. E-cigarettes: a $1.5 billion industry braces for FDA regulation. Bloomberg BusinessWeek. http://www.businessweek.com/articles/2014-02-06/e-cigarettes-fda-regulation-looms-for-1-dot-5-billion-industry. AccessedNovember 6, 2014.
- 55.Edney A. E-cigarettes target youth with festivals, lawmakers say. Bloomberg BusinessWeek. 2014 http://www.bloomberg.com/news/2014-04-14/e-cigarettes-target-youth-with-festivals-lawmakers-say.html. Accessed August 5, 2014.
- 56.Wagoner KG, Song EY, Egan KL, et al. E-cigarette availability and promotion among retail outlets near college campuses in two southeastern states. Nicotine Tob Res. 2014;16(8):1150–1155. doi: 10.1093/ntr/ntu081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dawsey J. New Jersey e-cigarettes tax plan has some fuming. Wall Street Journal. 2014 Jun 11;:A17. [Google Scholar]
- 58.Duke JC, Lee YO, Kim AE, et al. Exposure to electronic cigarette television advertisements among youth and young adults. Pediatrics. 2014;134(1):e29–e36. doi: 10.1542/peds.2014-0269. [DOI] [PubMed] [Google Scholar]
- 59.Richardson A, Ganz O, Vallone D. Tobacco on the web: surveillance and characterisation of online tobacco and e-cigarette advertising [published online February 14, 2014] Tob Control. doi: 10.1136/tobaccocontrol-2013-051246. [DOI] [PubMed] [Google Scholar]
- 60.US Food and Drug Administration. Deeming tobacco products to be subject to the Federal Food, Drug, and Cosmetic Act, as amended by the Family Smoking Prevention and Tobacco Control Act; regulations on the sale and distribution of tobacco products and required warning statements for tobacco products: proposed rule. Fed Reg. 2014;79(80):23142–23207. [PubMed] [Google Scholar]
- 61.McCarthy M. E-cigarette companies target youth, US congressional study finds. BMJ. 2014;348:g2871. doi: 10.1136/bmj.g2871. [DOI] [PubMed] [Google Scholar]
- 62.Pepper JK, Emery SL, Ribisl KM, Southwell BG, Brewer NT. Effects of advertisements on smokers’ interest in trying e-cigarettes: the roles of product comparison and visual cues. Tob Control. 2014;23(suppl 3):iii31–iii36. doi: 10.1136/tobaccocontrol-2014-051718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brown J, Beard E, Kotz D, Michie S, West R. Real-world effectiveness of e-cigarettes when used to aid smoking cessation: a cross-sectional population study. Addiction. 2014;109(9):1531–1540. doi: 10.1111/add.12623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bullen C, Howe C, Laugesen M, et al. Electronic cigarettes for smoking cessation: a randomised controlled trial. Lancet. 2013;382(9905):1629–1637. doi: 10.1016/S0140-6736(13)61842-5. [DOI] [PubMed] [Google Scholar]
- 65.Caponnetto P, Campagna D, Cibella F, et al. Efficiency and safety of an electronic cigarette (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One. 2013;8(6):e66317. doi: 10.1371/journal.pone.0066317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.National Conference of State Legislatures. Alternative nicotine products/electronic cigarettes. http://www.ncsl.org/research/health/alternative-nicotine-products-e-cigarettes.aspx. October 8, 2014.


