Abstract
Background
The relationship between changes in proteinuria and myocardial infarction (MI) remains unclear in people with diabetes or pre-diabetes. We aimed to evaluate the predictive value and independent role of changes in proteinuria over a 2-year period in the incidence of MI in people with diabetes or pre-diabetes.
Methods
Based on the baseline and 2-year dipstick screening results from the Kailuan prospective cohort study, participants were divided into four categories: no proteinuria, remittent proteinuria, incident proteinuria, and persistent proteinuria. Four multivariable Cox proportional hazard models were built to adjust for the effects of different confounding covariates.
Results
Among the 17,625 participants in this study, there were a total of 238 incidents of MI during a median follow-up of 6.69 years. After adjusting for demography factors and laboratory indices, the association between persistent proteinuria and MI incidence was maintained (hazard ratio [HR] 2.50, 95% confidence interval [CI] 1.48–4.22). Every decrease of proteinuria from 2006 to 2008 was observed to be responsible for a 21% decline of MI incidence (HR 0.79, 95% CI 0.68–0.90). The interaction between changes in proteinuria and diabetes was confirmed with no effect on MI (P = 0.3371).
Conclusions
Persistent proteinuria is an independent risk factor for MI incidence in the pre-diabetic and diabetic population. These findings may help clinicians to interpret proteinuria changes in the outpatient setting and provide possible preventive approaches for people with pre-diabetes or diabetes.
Electronic supplementary material
The online version of this article (doi:10.1186/s12933-017-0586-7) contains supplementary material, which is available to authorized users.
Keywords: Myocardial infarction, Proteinuria, Diabetes, Pre-diabetes
Background
Patients with chronic kidney disease (CKD) are three times more likely to have myocardial infarction (MI) and to suffer from increased morbidity and higher mortality [1–4]. Proteinuria, a common and important indicator of CKD, has been widely accepted as an independent predictor of cardiovascular disease (CVD) across different populations [5–7]. A pooled analysis from 7 prospective cohorts showed that proteinuria (≥1+ on dipstick) was associated with a 1.75-fold increased risk of cardiovascular disease mortality in the general population [8]. Brenda et al. also reported that the risk of MI was significantly increased in patients with higher levels of proteinuria in a large population of 597,870 participants [9].
However, a limitation of previous studies is that renal impairment as measured by proteinuria was assessed only once, and the interval between this single measurement and adverse events showed a large variation up to several decades. Proteinuria is not immutable. Rather, this condition can be affected by many factors, such as adiposity [10, 11] and blood pressure [12]. Additionally, previous studies did not give consideration to how proteinuria changes (none, remittent, incident and persistent) over time and its potential impact on the future risk for the incidence of MI.
Several studies have shown that people with diabetes and pre-diabetes are at high risk of developing MI accompanied by proteinuria [13, 14]. Thus, it is important to estimate the association between proteinuria changes and the incidence of MI in these populations. This study therefore used a large Chinese population from the Kailuan prospective study to evaluate the predictive value and independent role of proteinuria changes over a 2-year period in the incidence of MI in people with diabetes or pre-diabetes.
Methods
Study design and population
The Kailuan study is a prospective, population-based cohort study involving 101, 510 people (81,110 males and 20,400 females, 18–98 years old) in the Kailuan community in Tangshan, China. The design, methods, rationale and examination details of the study have been described in detail previously [15]. All participants provided their written informed consent and finished questionnaire interviews, anthropometric measurements, clinical examinations, and laboratory assessments in 2-year cycles until the present day. The study followed the guidelines of the Helsinki Declaration and was approved by the Ethics Committees of both the Kailuan General Hospital and Beijing Tiantan Hospital.
In the present study, 1316 participants and 75 participants were excluded due to MI at baseline (2006) or the second follow-up (2008). 70, 675 participants did not meet the inclusion criteria (that is, with a normal glucose metabolism) at baseline. Next, 7878 participants and 3914 participants were excluded due to missing the second follow-up data or incomplete data. The remaining 17,625 individuals were available for our analyses. The flow chart of the study cohort is presented in Fig. 1.
Fig. 1.
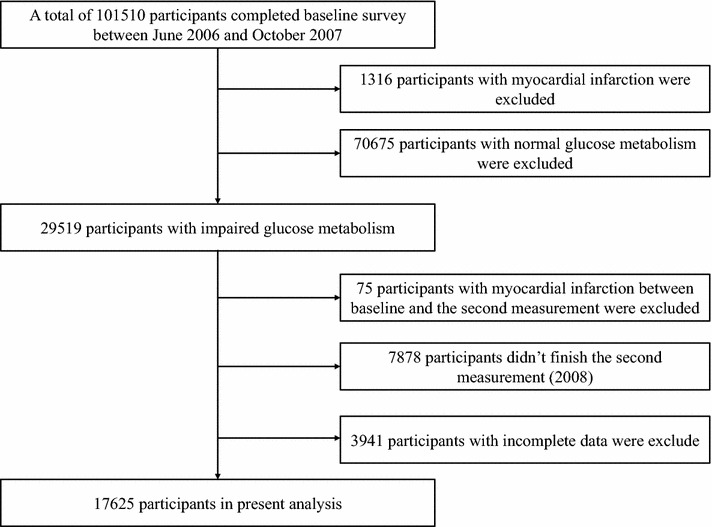
Flowchart of the study cohort
Changes in proteinuria
Proteinuria was captured by urine dipstick, reported as none, trace, 1+, 2+, and 3+. Present proteinuria was defined as 1+, 2+ and 3+. “No proteinuria” was defined as without proteinuria both in 2006 and 2008. “Remittent proteinuria” was defined as proteinuria that was present during the baseline collection period but was not present at the 2-year mark. “Incident proteinuria” was defined as proteinuria that was not present at baseline but did occur for the first time at the 2-year mark. “Persistent proteinuria” was defined as proteinuria present during the baseline collection period and present at the 2-year mark.
Outcome ascertainment
Participants were followed via face-to-face interviews at every 2-year routine medical examination until the 31st of December 2015 or until the event of interest or death. The primary outcome was the first occurrence of MI, including fatal and non-fatal MI. The diagnosis of MI events was confirmed from biennial personal interviews, discharge summarized from the 11 hospitals, and medical records from medical insurance, using the International Classification of Disease, 10th Revision code I21 for MI [16]. Diagnose of MI were based on combinations of chest pain symptoms, ECG changes and cardiac enzyme levels. The criteria were consistently applied across all the 11 hospitals.
Assessment of other potential covariates
The candidate baseline variables presented in Table 1 were chosen for their common availability and use in previous studies. The demographic data and information about lifestyle characteristics, medication use, clinical history, and family history were obtained using questionnaires that were administered by trained doctors from the hospitals. Blood samples were collected in the morning after an overnight fast and analyzed at the central laboratory of the Kailuan General Hospital. Fasting plasma glucose (FPG) was measured using the hexokinase/glucose-6-phosphate dehydrogenase method. Total cholesterol (TC), triglycerides (TG), low-density lipoprotein (LDL), and high-density lipoprotein (HDL) levels were all measured enzymatically. Estimated glomerular filtration rate (eGFR) at baseline in 2006 and follow-up in 2008 were calculated using the Chronic Kidney Disease Epidemiology Collaboration equation [17].
Table 1.
Characteristics of the study population at baseline
| Variable | Total | No proteinuria | Remittent proteinuria | Incident proteinuria | Persistent proteinuria | P |
|---|---|---|---|---|---|---|
| No. of participants | 17,625 | 15,149 | 473 | 1584 | 419 | |
| Age in years, mean (SD) | 52.71 (10.92) | 52.44 (10.86) | 53.40 (10.93) | 54.22 (11.26) | 55.87 (10.76) | <0.0001 |
| Gender female, n (%) | 2993 (16.98) | 2604 (17.19) | 89 (18.82) | 230 (14.52) | 70 (16.71) | 0.0380 |
| High school or above, n (%) | 3474 (19.71) | 3113 (20.55) | 82 (17.34) | 211 (13.32) | 68 (16.23) | <0.0001 |
| Income ≧ 800 RMB/month, n (%) | 2691 (15.27) | 2384 (15.74) | 75 (15.86) | 176 (11.11) | 56 (13.37) | <0.0001 |
| Current smoker, n (%) | 6743 (38.26) | 5855 (38.65) | 186 (39.32) | 574 (36.24) | 128 (30.55) | 0.0023 |
| Current alcohol, n (%) | 7522 (42.68) | 6604 (43.59) | 199 (42.07) | 581 (36.68) | 138 (32.94) | <0.0001 |
| Active physical activity, n (%) | 3280 (18.61) | 2861 (18.89) | 112 (23.68) | 240 (15.15) | 67 (15.99) | <0.0001 |
| BMI, kg/m2, mean (SD) | 25.89 (3.46) | 25.81 (3.42) | 26.53 (3.63) | 26.19 (3.46) | 27.04 (4.01) | <0.0001 |
| Hypertension, n (%) | 9052 (51.36) | 7415 (48.95) | 320 (67.65) | 986 (62.25) | 331 (79.00) | <0.0001 |
| Diabetes mellitus, n (%) | 5442 (30.88) | 4301 (28.39) | 202 (42.71) | 677 (42.74) | 262 (62.53) | <0.0001 |
| Dyslipidemia, n (%) | 7759 (44.02) | 6482 (42.79) | 233 (49.26) | 782 (49.37) | 262 (62.53) | <0.0001 |
| Anti-hypertension agents, n (%) | 2595 (14.72) | 2120 (13.99) | 114 (24.10) | 262 (16.54) | 99 (23.63) | <0.0001 |
| Anti-diabetic agents, n (%) | 1495 (8.48) | 1190 (7.86) | 50 (10.57) | 180 (11.36) | 75 (17.90) | <0.0001 |
| Anti-lipidemic agents, n (%) | 211 (1.20) | 164 (1.08) | 7 (1.48) | 29 (1.83) | 11 (2.63) | <0.0001 |
| Systolic blood pressure, mmHg, mean (SD) | 134.70 (21.13) | 133.50 (20.61) | 143.39 (24.86) | 139.85 (21.95) | 148.47 (21.63) | <0.0001 |
| Diastolic blood pressure, mmHg, mean (SD) | 85.25 (11.83) | 84.72 (11.53) | 89.90 (14.33) | 87.41 (12.63) | 91.28 (12.77) | <0.0001 |
| Heart rate, beats/min, mean (SD) | 76.00 (10.52) | 75.82 (10.33) | 79.86 (12.81) | 75.67 (10.43) | 79.58 (12.92) | <0.0001 |
| High-sensitive C-reactive protein, mg/dl, median (IQR) | 0.90 (0.37-2.30) | 0.89 (0.34-2.10) | 1.50 (0.49-3.36) | 1.30 (0.45-4.20) | 1.80 (0.68-6.18) | <0.0001 |
| Fasting plasma glucose, mmol/l, mean (SD) | 7.03 (2.25) | 6.90 (2.10) | 7.66 (2.64) | 7.67 (2.83) | 8.69 (3.21) | <0.0001 |
| Total cholesterol, mmol/l, mean (SD) | 5.19 (1.11) | 5.18 (1.08) | 5.35 (1.21) | 5.16 (1.22) | 5.37 (1.74) | 0.0052 |
| Triglycerides, mmol/l, mean (SD) | 1.94 (1.68) | 1.90 (1.65) | 2.24 (1.95) | 2.13 (1.68) | 2.73 (2.14) | <0.0001 |
| Low-density lipoprotein, mmol/l, mean (SD) | 2.53 (0.93) | 2.54 (0.88) | 2.58 (1.01) | 2.46 (1.18) | 2.44 (1.41) | <0.0001 |
| High-density lipoprotein, mmol/l, mean (SD) | 1.52 (0.40) | 1.51 (0.39) | 1.55 (0.45) | 1.58 (0.45) | 1.58 (0.49) | <0.0001 |
| Creatinine, μmol/l, mean (SD) | 89.99 (32.26) | 89.24 (31.20) | 88.01 (27.62) | 95.36 (40.30) | 98.84 (36.95) | <0.0001 |
| eGFR, ml/(min 1.73 m2), mean (SD) | 83.76 (26.31) | 84.24 (23.57) | 85.32 (30.82) | 80.68 (43.79) | 76.33 (24.81) | <0.0001 |
| Myocardial infarction, n (%) | 238 (1.35) | 179 (1.18) | 5 (1.06) | 33 (2.08) | 21 (5.01) | <0.0001 |
BMI body mass index, SD standard deviation, IQR interquartile range, eGFR estimated glomerular filtration rate
As was previously reported [18], hypertension was defined as systolic blood pressure (SBP) ≥140 mmHg or diastolic blood pressure (DBP) ≥90 mmHg, any use of anti-hypertension agents, or self-reported history of hypertension. Diabetes was defined as fasting glucose level ≥7.0 mmol/l, any use of anti-diabetic agents, or any self-reported history of diabetes. Pre-diabetes was defined as fasting glucose level between 5.6 and 6.9 mmol/l recognized by The American Diabetes Association (ADA) [19]. Dyslipidemia was defined as serum TG ≥ 1.69 mmol/l, LDL ≥ 3.62 mmol/l, HDL ≤ 1.04 mmol/l, any use of anti-lipidemic agents, or any self-reported history of dyslipidemia.
Statistical analyses
The SAS version 9.4 (SAS Institute, Cary, NC, USA) was used for the statistical analyses. The differences in continuous and categorical variables across the four groups for proteinuria changes were assessed using ANOVA or Kruskal–Wallis and χ2 tests, as deemed appropriate. Four multivariable Cox proportional hazard models were built to adjust for the effects of confounding covariates: (1) Model 1: unadjusted; (2) Model 2: adjusted for age and gender; (3) Model 3: adjusted for age, gender, level of education, income, smoking, alcohol abuse, amount of physical activity and body mass index (BMI); (4) Model 4: adjusted for variables in model 3 plus hypertension, diabetes mellitus, dyslipidemia, anti-hypertension agents, anti-diabetic agents, anti-lipidemic agents, SBP, heart rate, high-sensitive C-reactive protein (CRP), TC, TG, LDL, HDL, FPG and eGFR. “Per degree decrease” was defined as one proteinuria degree decline from the first measurement (2006) to the second measurement (2008). To address the different effects of diabetes status (diabetes and pre-diabetes) on the relationship, separate analyses were performed to dichotomize the cohort into 2 subgroups: those with diabetes and those with pre-diabetes.
Sensitivity analyses were also performed to verify the robustness of the study findings. First, proteinuria was re-defined as positive if the dipstick results showed trace or more (trace+) proteinuria. The participants were re-grouped into no proteinuria (reference group), remittent proteinuria, incident proteinuria, and persistent proteinuria. To eliminate the possibility that impaired renal function may have an effect on the relationship between proteinuria and MI, all of the analyses were repeated by excluding the population with eGFR less than 30 ml/min/1.73 m2 [20].
Results
Baseline data
A total of 17,625 eligible participants (73.02% men) were analyzed in the study. The mean age was 52.71 ± 10.92 years. The number of participants with ‘no proteinuria’, ‘remittent proteinuria’, ‘incident proteinuria’ and ‘persistent proteinuria’ were 15,149 (85.95%), 473 (2.68%), 1, 584 (8.99%), and 419 (2.38%), respectively. Participant characteristics by changes in proteinuria groups are shown in Table 1. Compared with participants with no proteinuria, participants in the other groups had a higher proportion of men, lower educational levels, lower incomes, less drinking, a higher BMI and a higher prevalence of hypertension, diabetes mellitus, and dyslipidemia (all P < 0.05). Moreover, differences in laboratory indices such as SBP, DBP, heart rate, CRP, TC, TG, LDL, HDL, FBP, creatinine and eGFR among the four groups were all statistically significant (all P < 0.05).
There were a total of 238 (1.35%) incidents of MI during a median follow-up of 6.69 years. Among the four groups, the highest incidence rate occurred in participants with persistent proteinuria (5.01%), and the lowest incidence rate occurred in participants with remittent proteinuria (1.06%). The difference was statistically significant (P < 0.0001).
Changes in proteinuria and risk of MI
The relationship between changes in proteinuria and risk of MI is shown in Fig. 2. In the unadjusted model, the incidence of MI was significantly higher in participants with persistent proteinuria (hazard ratio [HR] 4.31, 95% confidence interval [CI] 2.69–6.90) and incident proteinuria (HR 1.74, 95% CI 1.18–2.57) compared with those with no proteinuria. After adjusting for demography factors and laboratory indices, only the association between persistent proteinuria and the incidence of MI was maintained (HR 2.50, 95% CI 1.48–4.22) in model 4. We also found that every decrease of proteinuria from 2006 to 2008 was responsible for a 21% decline of MI incidence (HR 0.79, 95% CI 0.68–0.90). The interaction between proteinuria changes and diabetes was confirmed with no effect on the incidence of MI (P = 0.3371), suggesting that people in the diabetic or pre-diabetic state with proteinuria changes have the same risk of MI.
Fig. 2.
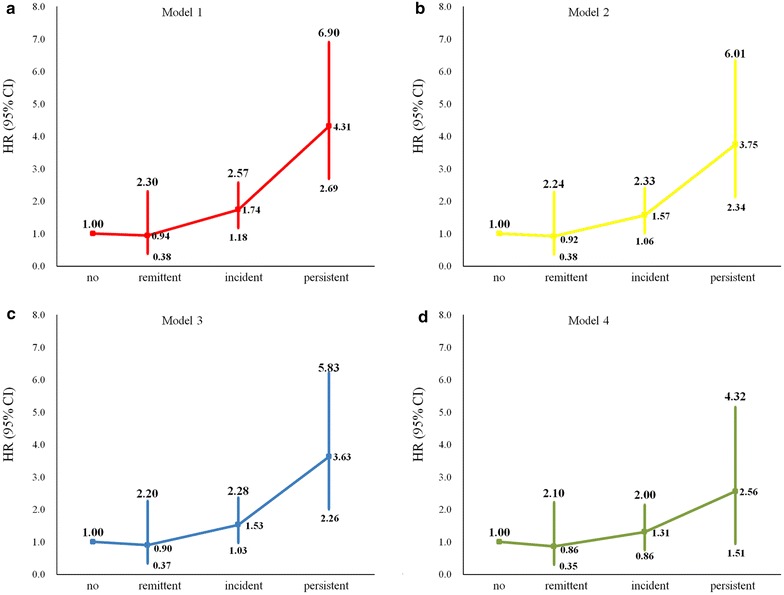
Hazard ratios for the association between changes in proteinuria and myocardial infarction. a–d Model 1: unadjusted; Model 2: adjusted for age and gender; Model 3: adjusted for age, gender, level of education, income, smoking, alcohol abuse, amount of physical activity and body mass index; Model 4: adjusted for variables in model 3 plus hypertension, diabetes mellitus, dyslipidemia, anti-hypertension agents, anti-diabetic agents, anti-lipidemic agents, systolic blood pressure, heart rate, high-sensitive C-reactive protein, total cholesterol, triglycerides, low-density lipoprotein, high-density lipoprotein, fasting plasma glucose, and estimated glomerular filtration rate. Proteinuria was defined as 1+, 2+ and 3+
Figure 3 shows the Kaplan–Meier cumulative risk for the incidence of MI defined by changes in proteinuria. Participants in the persistent proteinuria group experienced a higher risk than participants of the other groups during the 6.69-year follow-up period for MI events (log-rank test, P < 0.0001).
Fig. 3.
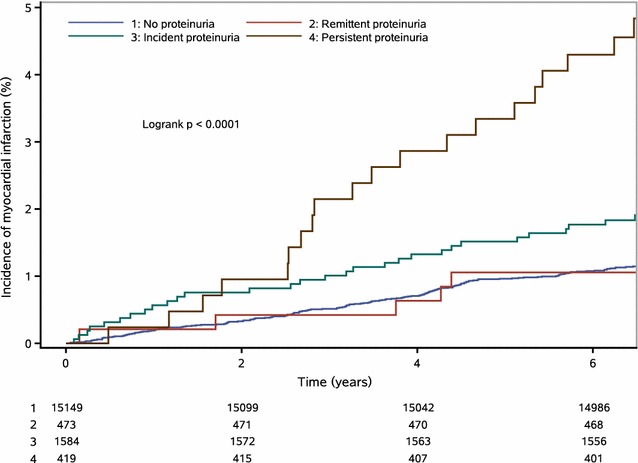
Survival curves of changes in proteinuria and myocardial infarction
Additional file 1: Table S1 shows the comparison of demographic and other characteristics at baseline of participants (n = 17,625) and non-participants (n = 11,819) who were excluded due to missing the second follow-up data or incomplete data. In general, it was observed that non-participants were older, less likely to be females, had lower educational levels, lower incomes, less likely to be smokers, less likely to drink, had higher BMI, higher prevalence of hypertension, and diabetes mellitus but a lower prevalence of dyslipidemia (all P < 0.05).
Sensitivity analysis
The results appeared to be more robust after defining proteinuria as trace, 1+, 2+ and 3+. After adjusting for demography factors and laboratory indices, the association between persistent proteinuria and MI incidence were maintained (HR 1.94, 95% CI 1.25–3.01) in model 4 (Table 2). When all of the analyses were repeated by excluding the population with eGFR less than 30 ml/min/1.73 m2, similar results were obtained. Only the association between persistent proteinuria and MI incidence was statistically significant (HR 2.49, 95% CI 1.47–4.20) in model 4 (Table 3). The interaction between changes in proteinuria and diabetes was still not found suggesting no effect on MI incidence in the subgroups.
Table 2.
Hazard ratios for the association between changes in proteinuria and myocardial infarction, redefining proteinuria as trace, 1+, 2+ and 3+
| No proteinuria | Remittent proteinuria | Incident proteinuria | Persistent proteinuria | |
|---|---|---|---|---|
| All participants | ||||
| Model 1 | Reference | 1.04 (0.61–1.78) | 1.58 (1.09–2.31) | 3.17 (2.13–4.73) |
| Model 2 | Reference | 1.00 (0.59–1.72) | 1.47 (1.01–2.15) | 2.76 (1.85–4.12) |
| Model 3 | Reference | 1.00 (0.59–1.72) | 1.45 (0.99–2.12) | 2.69 (1.80–4.02) |
| Model 4 | Reference | 0.81 (0.46–1.45) | 1.27 (0.84–1.90) | 1.94 (1.25–3.01) |
| Diabetes$ | ||||
| Model 4 | Reference | 1.08 (0.48–2.41) | 1.99 (1.18–3.35) | 1.97 (1.08–3.60) |
| Prediabetes | ||||
| Model 4 | Reference | 0.62 (0.27–1.45) | 0.66 (0.32–1.33) | 2.13 (1.12–4.06) |
Model 1: unadjusted
Model 2: adjusted for age and gender
Model 3: adjusted for age, gender, level of education, income, smoking, alcohol abuse, amount of physical activity, and body mass index
Model 4: adjusted for variables in model 3 plus hypertension, diabetes mellitus, dyslipidemia, anti-hypertension agents, anti-diabetic agents, anti-lipidemic agents, systolic blood pressure, heart rate, high-sensitive C-reactive protein, total cholesterol, triglycerides, low-density lipoprotein, high-density lipoprotein, fasting blood glucose and estimated glomerular filtration rate
$ P for interaction is 0.0750
Table 3.
Hazard ratios for the association between changes in proteinuria and myocardial infarction, after excluding the population with estimated glomerular filtration rate less than 30 ml/min/1.73 m2
| No proteinuria | Remittent proteinuria | Incident proteinuria | Persistent proteinuria | |
|---|---|---|---|---|
| All participants | ||||
| Model 1 | Reference | 0.94 (0.39–2.29) | 1.74 (1.18–2.58) | 4.35 (2.72–6.97) |
| Model 2 | Reference | 0.92 (0.38–2.23) | 1.57 (1.06–2.34) | 3.79 (2.37–6.06) |
| Model 3 | Reference | 0.90 (0.37–2.20) | 1.54 (1.04–2.29) | 3.66 (2.28–5.87) |
| Model 4 | Reference | 0.84 (0.34–2.07) | 1.30 (0.85–1.98) | 2.49 (1.47–4.20) |
| Diabetes$ | ||||
| Model 4 | Reference | 0.70 (0.17–2.87) | 1.60 (0.93–2.75) | 2.25 (1.10–4.59) |
| Prediabetes | ||||
| Model 4 | Reference | 0.92 (0.28–3.01) | 0.88 (0.45–1.74) | 3.28 (1.51–7.14) |
Proteinuria was defined as 1+, 2+ and 3+
Model 1: unadjusted
Model 2: adjusted for age and gender
Model 3: adjusted for age, gender, level of education, income, smoking, alcohol abuse, amount of physical activity and body mass index
Model 4: adjusted for variables in model 3 plus hypertension, diabetes mellitus, dyslipidemia, anti-hypertension agents, anti-diabetic agents, anti-lipidemic agents, systolic blood pressure, heart rate, high-sensitive C-reactive protein, total cholesterol, triglycerides, low-density lipoprotein, high-density lipoprotein, fasting blood glucose and estimated glomerular filtration rate
$ P for interaction is 0.3363
Discussion
In this large longitudinal cohort, the value of changes in proteinuria alteration, as measured by repeated urine dipstick 2 years apart, for future MI risk prediction among people with diabetes and pre-diabetes was investigated. The results show that persistent proteinuria is independently associated with about a twofold high risk of MI in people with diabetes and pre-diabetes after adjusting for major confounding factors, including smoking, hypertension, diabetes mellitus, dyslipidemia, and other laboratory indices. Every decrease of proteinuria was responsible for a 21% decline of MI incidence. However, the association was not observed in people with no proteinuria, remittent proteinuria and incident proteinuria, suggesting that only a long-term progression of proteinuria would have an effect on MI incidence.
Urinary albumin excretion can be measured by several ways, including 24-h urine albumin excretion, albumin creatinine ratio (ACR) and dipstick test [21]. Although studies showed that albuminuria is more powerful in predicting mortality and cardiovascular disease, the dipstick test has an advantage in the cost-effectiveness and the convenience of the examination [22], especially for developing countries. Due to the practical circumstances and restrained facilities, the former two ways are not routinely applied in mass health screenings, for example, in our study. In addition, dipstick test is easy to implement and positive findings were tightly correlated with elevated levels of ACR [23]. A study found that dipstick urine protein of 1+ and above has a high negative predictive value and specificity (97.6 and 95.4%, respectively) to ACR of 30 mg/g and above [24]. Thus, it is reasonable to use proteinuria identified through dipstick test as a surrogate marker for renal function.
Proteinuria is an independent risk factor for MI [9, 25, 26]. In fact, increased MI risk has been demonstrated at all levels of proteinuria, including moderate albuminuria [27] and GFR values, according to several observational studies. A prospective cohort study in Bangladesh on more than 10,000 participants reported that proteinuria as detected by the dipstick method was a predictor of all-cause mortality in general and CVD-related mortality in particular [28]. Sacarese et al. reported that a 10% reduction in urinary albumin excretion was associated with 13% reduction of MI incidence in diabetic and/or hypertensive patients [29]. In addition, a large community-based study suggested that proteinuria of increasing severity was associated with a faster rate of renal decline, regardless of baseline eGFR [30]. In the present study, we classified our participants into four groups to investigate the relationship between changes in proteinuria and MI incidence. According to the full adjusted model, only a long-term change in proteinuria has a certain association with MI incidence. Based on a large number of individuals with diabetes or pre-diabetes identified in routine health examinations, our study approved the prior findings and provided more evidence regarding changes in proteinuria over time.
In addition, we did not determine an interaction between diabetes or pre-diabetes and proteinuria changes for risk of MI, indicating that there was no difference for the risk of MI in patients with diabetes and pre-diabetes when they presented persistent proteinuria. This finding should serve as a reminder that people with pre-diabetes are also a high-risk group for MI incidence if they have persistent proteinuria.
The mechanisms linking proteinuria to MI risk is not well-understood. It is plausible of proteinuria, which may play a causal role in progressive renal disease by damaging podocytes, activating inflammation and worsening cardiometabolic risk factors [31, 32]. Furthermore, proteinuria among diabetes may represent a spectrum of metabolic disorders, e.g., higher BMI and/or higher SBP in the present study [33]. Hence, proteinuria may also contribute to the development of macroangiopathic cardiovascular disorders. Several studies have determined the association between proteinuria and structural change and dysfunction of the heart. Mochizuki et al. reported that diabetic nephropathy was a factor independently associated with left ventricular longitudinal systolic myocardial dysfunction in asymptomatic diabetes patients [34]. In another study including patients with heart failure with preserved ejection fraction, albuminuria is associated with cardiac remodeling and left and right ventricular dysfunction [35]. The persistent proteinuria indicates a continuous impairment of renal function, which is another risk factor for CVD [8].
Several of the strengths of this study include the prospective design, use of a large cohort, long follow-up period, and the availability of repeated measurements of proteinuria. The results should be interpreted in the context of some limitations. First, although potential cardiac risk factors were adjusted for, the possibility of residual confounding might have had an effect. Second, another limitation is the unbalanced distribution of gender in the Kailuan cohort study, considering that most of the participants are male coal miners. Demographic characteristics and cardiac risk factors may differ; therefore, the findings may not be generalized directly to the general Chinese population. Third, proteinuria was determined by dipstick method, meaning that albuminuria was not quantitatively measured and that this approach may not properly reflect the association. Fourth, the shortage of records using of medications, insulin and insulin resistance in this study may have an effect on proteinuria, which therefore warrants further analysis. Thus, the relationship between proteinuria changes and MI incidence in diabetic and pre-diabetic population needs to be validated in other populations.
Conclusions
Persistent proteinuria as detected by simple serial urine dipstick independently predicted future MI risk in the pre-diabetic and diabetic population. These findings may help clinicians to interpret proteinuria changes in the outpatient setting and may provide a preventive approach for people with pre-diabetes or diabetes. Therapies targeted at proteinuria reduction for MI prevention also warrant further investigation.
Authors’ contributions
AW and YS wrote the manuscript. AW researched data. Xiaoxue L, ZS, YL, JL, SC, JW, Xia L, ZZ and HZ researched data and contributed to discussion. SW reviewed and edited the manuscript. XG contributed to the discussion and reviewed/edited the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We thank all the staff and participants of the Kailuan study for their invaluable contributions.
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Consent for publication
Not applicable.
Ethics approval and consent to participate
The study followed the guidelines of the Helsinki Declaration, and was approved by the Ethics Committees of both the Kailuan General Hospital and Beijing Tiantan Hospital.
Funding
Our work was funded by Beijing Natural Science Foundation (Z160002), the Program of Natural Science Fund of China (Serial No: 81530087), and Key Projects in the National Science & Technology Program of Beijing (D141100000114003).
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Abbreviations
- CKD
chronic kidney disease
- CVD
cardiovascular disease
- MI
myocardial infarction
- HR
hazard ratio
- 95% CI
95% confidence interval
- FPG
fasting plasma glucose
- TC
total cholesterol
- TG
triglycerides
- LDL
low-density lipoprotein
- HDL
high-density lipoprotein
- SBP
systolic blood pressure
- CRP
C-reactive protein
- eGFR
estimated glomerular filtration rate
- DBP
diastolic blood pressure
- ACR
albumin creatinine ratio
Additional file
Additional file 1: Table S1. Comparison of demographic and other characteristics in 2006 of participants and nonparticipants.
Footnotes
Anxin Wang and Yang Sun contributed equally to this work
Electronic supplementary material
The online version of this article (doi:10.1186/s12933-017-0586-7) contains supplementary material, which is available to authorized users.
Contributor Information
Anxin Wang, Email: anxin0907@163.com.
Yang Sun, Email: shouyisunyang@163.com.
Xiaoxue Liu, Email: xiaoxue522@163.com.
Zhaoping Su, Email: liusu151211@163.com.
Junjuan Li, Email: lijunjuan_123@126.com.
Yanxia Luo, Email: lyx100@ccmu.edu.cn.
Shuohua Chen, Email: csh0106@qq.com.
Jianli Wang, Email: 792516098@qq.com.
Xia Li, Email: lixia_new@163.com.
Zhan Zhao, Email: zhaozhan@mail.ie.ac.cn.
Huiping Zhu, Email: zhuhuiping@ccmu.edu.cn.
Shouling Wu, Phone: +86-315-3025655, Email: drwusl@163.com.
Xiuhua Guo, Phone: +86-10-83911508, Email: statguo@ccmu.edu.cn.
References
- 1.Soriano LC, Johansson S, Stefansson B, Rodríguez LAG. Cardiovascular events and all-cause mortality in a cohort of 57,946 patients with type 2 diabetes: associations with renal function and cardiovascular risk factors. Cardiovasc Diabetol. 2015;14:38. doi: 10.1186/s12933-015-0204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Srinivasan MP, Kamath PK, Bhat NM, Pai ND, Manjrekar PA, Mahabala C. Factors associated with no apparent coronary artery disease in patients with type 2 diabetes mellitus for more than 10 years of duration: a case control study. Cardiovasc Diabetol. 2015;14:146. doi: 10.1186/s12933-015-0307-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chang SH, Tsai CT, Yen AM, Lei MH, Chen HH, Tseng CD. Proteinuria and reduced estimated glomerular filtration rate independently predict risk for acute myocardial infarction: findings from a population-based study in Keelung, Taiwan. Zhonghua Minguo Xin Zang Xue Hui Za Zhi. 2015;31(2):106–112. doi: 10.6515/ACS20141201A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lim CC, Teo BW, Ong PG, Cheung CY, Lim SC, Chow KY, Meng CC, Lee J, Tai ES, Wong TY. Chronic kidney disease, cardiovascular disease and mortality: a prospective cohort study in a multi-ethnic Asian population. Eur J Prev Cardiol. 2015;22(8):1018–1026. doi: 10.1177/2047487314536873. [DOI] [PubMed] [Google Scholar]
- 5.Monseu M, Gand E, Saulnier PJ, Ragot S, Piguel X, Zaoui P, Rigalleau V, Marechaud R, Roussel R, Hadjadj S. Acute kidney injury predicts major adverse outcomes in diabetes: synergic impact with low glomerular filtration rate and albuminuria. Diabetes Care. 2015;38(12):2333–2340. doi: 10.2337/dc15-1222. [DOI] [PubMed] [Google Scholar]
- 6.Ritte R, Luke J, Nelson C, Brown A, O’Dea K, Jenkins A, Best JD, Mcdermott R, Daniel M, Rowley K. Clinical outcomes associated with albuminuria in central Australia: a cohort study. BMC Nephrol. 2016;17:113. doi: 10.1186/s12882-016-0328-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Åkerblom A, Clare RM, Lokhnygina Y, Wallentin L, Held C, Van de Werf F, Moliterno DJ, Patel UD, Leonardi S, Armstrong PW. Albuminuria and cardiovascular events in patients with acute coronary syndromes: results from the TRACER trial. Am Heart J. 2016;178:1–8. doi: 10.1016/j.ahj.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 8.Nagata M, Ninomiya T, Kiyohara Y, Murakami Y, Irie F, Sairenchi T, Miura K, Okamura T, Ueshima H. Group E-JR. Prediction of cardiovascular disease mortality by proteinuria and reduced kidney function: pooled analysis of 39,000 individuals from 7 cohort studies in Japan. Am J Epidemiol. 2013;178(1):1–11. doi: 10.1093/aje/kws447. [DOI] [PubMed] [Google Scholar]
- 9.Hemmelgarn BR, Manns BJ, Lloyd A, James MT, Klarenbach S, Quinn RR, Wiebe N, Tonelli M. Relation between kidney function, proteinuria, and adverse outcomes. JAMA. 2010;303(5):423–429. doi: 10.1001/jama.2010.39. [DOI] [PubMed] [Google Scholar]
- 10.Bouchi R, Ohara N, Asakawa M, Nakano Y, Takeuchi T, Murakami M, Sasahara Y, Numasawa M, Minami I, Izumiyama H. Is visceral adiposity a modifier for the impact of blood pressure on arterial stiffness and albuminuria in patients with type 2 diabetes? Cardiovasc Diabetol. 2016;15(1):1–8. doi: 10.1186/s12933-015-0324-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yong P, Hua W, Fei C, Huang FY, Xia TL, Liao YB, Hua C, Wang PJ, Zuo ZL, Wei L. The influence of body composition on renal function in patients with coronary artery disease and its prognostic significance: a retrospective cohort study. Cardiovasc Diabetol. 2016;15:106. doi: 10.1186/s12933-016-0420-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Imai E, Ito S, Haneda M, Harada A, Kobayashi F, Yamasaki T, Makino H, Chan JCN. Effects of blood pressure on renal and cardiovascular outcomes in Asian patients with type 2 diabetes and overt nephropathy: a post hoc analysis (ORIENT-blood pressure) Nephrol Dial Transplant. 2016;31(3):447–454. doi: 10.1093/ndt/gfv272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Qiu M, Shen W, Song X, Ju L, Tong W, Wang H, Zheng S, Jin Y, Wu Y, Wang W, Tian J. Effects of prediabetes mellitus alone or plus hypertension on subsequent occurrence of cardiovascular disease and diabetes mellitus: longitudinal study. Hypertension. 2015;65(3):525–530. doi: 10.1161/HYPERTENSIONAHA.114.04632. [DOI] [PubMed] [Google Scholar]
- 14.Global Burden of Metabolic Risk Factors for Chronic Diseases C Cardiovascular disease, chronic kidney disease, and diabetes mortality burden of cardiometabolic risk factors from 1980 to 2010: a comparative risk assessment. Lancet Diabetes Endocrinol. 2014;2(8):634–647. doi: 10.1016/S2213-8587(14)70102-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang A, Wu J, Zhou Y, Guo X, Luo Y, Wu S, Zhao X. Measures of adiposity and risk of stroke in China: a result from the Kailuan study. PLoS ONE. 2013;8(4):e61665. doi: 10.1371/journal.pone.0061665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Organization WH: International statistical classification of diseases and related health problems, 10th revision. http://apps.who.int/classifications/icd10/browse/2010/en#/I20-I25. Accessed 1 May 2017.
- 17.Levey AS, Stevens LA, Schmid CH, Zhang YL, Rd CA, Feldman HI, Kusek JW, Eggers P, Van LF, Greene T. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–612. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li Z, Wang A, Cai J, Gao X, Zhou Y, Luo Y, Wu S, Zhao X. Impact of proteinuria and glomerular filtration rate on risk of ischaemic and intracerebral hemorrhagic stroke: a result from the Kailuan study. Eur J Neurol. 2015;22(2):355–360. doi: 10.1111/ene.12580. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care. 2012;35(suppl 1):64–71. doi: 10.2337/dc12-s064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Levey A, Coresh J, Balk E, Kausz A, Levin A, Steffes M, Hogg R, Perrone R, Lau J, Eknoya G. Clinical guidelines national kidney foundation practice guidelines for chronic kidney disease: evaluation, classificaiton, and stratification. Ann Intern Med. 2003;139(7):605. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- 21.Levin A, Stevens PE. Summary of KDIGO 2012 CKD guideline: behind the scenes, need for guidance, and a framework for moving forward. Kidney Int. 2014;85(1):49–61. doi: 10.1038/ki.2013.444. [DOI] [PubMed] [Google Scholar]
- 22.Sato H, Konta T, Ichikawa K, Suzuki N, Kabasawa A, Suzuki K, Hirayama A, Shibata Y, Watanabe T, Kato T, Ueno Y, Kayama T, Kubota I. Comparison of the predictive ability of albuminuria and dipstick proteinuria for mortality in the Japanese population: the Yamagata (Takahata) study. Clin Exp Nephrol. 2016;20(4):611–617. doi: 10.1007/s10157-015-1193-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thomas MC. The assessment and management of albuminuria in primary care. Diabetes Res Clin Pract. 2008;80(1):83–88. doi: 10.1016/j.diabres.2007.10.024. [DOI] [PubMed] [Google Scholar]
- 24.White SL, Yu R, Craig JC, Polkinghorne KR, Atkins RC, Chadban SJ. Diagnostic accuracy of urine dipsticks for detection of albuminuria in the general community. Am J Kidney Dis. 2011;58(1):19–28. doi: 10.1053/j.ajkd.2010.12.026. [DOI] [PubMed] [Google Scholar]
- 25.Jeon HJ, Kim CT, An JN, Lee H, Kim H, Park SK, Joo KW, Lim CS, Jung IM, Ahn C, Kim YS, Kim YH, Lee JP. Time-varying maximal proteinuria correlates with adverse cardiovascular events and graft failure in kidney transplant recipients. Nephrology (Carlton). 2015;20(12):945–951. doi: 10.1111/nep.12529. [DOI] [PubMed] [Google Scholar]
- 26.Konno S, Munakata M. Moderately increased albuminuria is an independent risk factor of cardiovascular events in the general Japanese population under 75 years of age: the Watari study. PLoS ONE. 2015;10(4):e0123893. doi: 10.1371/journal.pone.0123893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmieder RE, Mann JF, Schumacher H, Gao P, Mancia G, Weber MA, McQueen M, Koon T, Yusuf S, Investigators O. Changes in albuminuria predict mortality and morbidity in patients with vascular disease. J Am Soc Nephrol. 2011;22(7):1353–1364. doi: 10.1681/ASN.2010091001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pesola GR, Argos M, Chen Y, Parvez F, Ahmed A, Hasan R, Rakibuz-Zaman M, Islam T, Eunus M, Sarwar G, Chinchilli VM, Neugut AI, Ahsan H. Dipstick proteinuria as a predictor of all-cause and cardiovascular disease mortality in Bangladesh: a prospective cohort study. Prev Med. 2015;78:72–77. doi: 10.1016/j.ypmed.2015.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Savarese G, Dei Cas A, Rosano G, D’Amore C, Musella F, Mosca S, Reiner MF, Marchioli R, Trimarco B, Perrone-Filardi P. Reduction of albumin urinary excretion is associated with reduced cardiovascular events in hypertensive and/or diabetic patients. A meta-regression analysis of 32 randomized trials. Int J Cardiol. 2014;172(2):403–410. doi: 10.1016/j.ijcard.2014.01.065. [DOI] [PubMed] [Google Scholar]
- 30.Turin TC, James M, Ravani P, Tonelli M, Manns BJ, Quinn R, Jun M, Klarenbach S, Hemmelgarn BR. Proteinuria and rate of change in kidney function in a community-based population. J Am Soc Nephrol. 2013;24(10):1661–1667. doi: 10.1681/ASN.2012111118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Koop K, Eikmans M, Wehland M, Baelde H, Ijpelaar D, Kreutz R, Kawachi H, Kerjaschki D, De HE, Bruijn JA. Selective loss of podoplanin protein expression accompanies proteinuria and precedes alterations in podocyte morphology in a spontaneous proteinuric rat model. Am J Pathol. 2008;173(2):315–326. doi: 10.2353/ajpath.2008.080063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang L, Brozovic S, Xu J, Long Y, Kralik PM, Waigel S, Zacharias W, Zheng S, Epstein PN. Inflammatory gene expression in OVE26 diabetic kidney during the development of nephropathy. Nephron Exp Nephrol. 2011;119(1):8–20. doi: 10.1159/000324407. [DOI] [PubMed] [Google Scholar]
- 33.Afghahi H, Miftaraj M, Svensson AM, Hadimeri H, Gudbjornsdottir S, Eliasson B, Svensson MK, Swedish National Diabetes R Ongoing treatment with renin-angiotensin-aldosterone-blocking agents does not predict normoalbuminuric renal impairment in a general type 2 diabetes population. J Diabetes Complicat. 2013;27(3):229–234. doi: 10.1016/j.jdiacomp.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 34.Mochizuki Y, Tanaka H, Matsumoto K, Sano H, Toki H, Shimoura H, Ooka J, Sawa T, Motoji Y, Ryo K. Clinical features of subclinical left ventricular systolic dysfunction in patients with diabetes mellitus. Cardiovasc Diabetol. 2015;14:37. doi: 10.1186/s12933-015-0201-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Katz DH, Burns JA, Aguilar FG, Beussink L, Shah SJ. Albuminuria is independently associated with cardiac remodeling, abnormal right and left ventricular function, and worse outcomes in heart failure with preserved ejection fraction. JACC Heart Fail. 2014;2(6):586–596. doi: 10.1016/j.jchf.2014.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.


