Abstract
Objective
We examined the degree to which a resilient personality prototype predicted adjustment among war Veterans with and without a traumatic brain injury (TBI) while covarying the level of combat exposure.
Method
A total of 127 war Veterans (107 men, 20 women; average age = 37 years) participated. Personality prototypes were derived from the Multidimensional Personality Questionnaire (Patrick, Curtain, & Tellegen, 2002). Measures were administered at baseline, and a subset was administered at 4- and 8-month follow-ups.
Results
Veterans with resilient personalities reported less sleep disturbance, more health-promoting behaviors, psychological flexibility, and emotional distress tolerance than Veterans with undercontrolled or overcontrolled prototypes. Path models revealed that resilience significantly predicted posttraumatic stress disorder (PTSD), depression, quality of life, and social support over time. TBI had unique and consistent effects only on PTSD.
Conclusion
Personality characteristics influence distress and quality of life among war Veterans with and without TBI. Implications for assessment, interventions, and research are discussed.
Keywords: Resilience, PTSD, depression, combat exposure, traumatic brain injury
Although traumatic brain injury (TBI) has been labeled the “signature wound” of the Iraq and Afghanistan conflicts, research has yet to clarify the persistent psychosocial difficulties uniquely attributable to TBI. From 2009 to 2011 almost 10% of Iraq and Afghanistan Veterans using Veterans Health Administration services were classified as having sustained a TBI (Cifu et al., 2014), the majority of which were classified as mild (76.7% out of 212,742 cases; Armed Forces Health Surveillance Center, 2011). A significant minority of Iraq/Afghanistan Veterans also experience posttraumatic stress disorder (PTSD; 12% to 23%) and depression (15%; Fulton et al., 2015; Hoge et al., 2004; Seal, Bertenthal, Miner, Sen,&Marmar, 2007). Moreover, many of the emotional problems and postconcussive symptoms that are often attributed to TBI are also characteristic of PTSD and depression, including anxiety, fearfulness, worry, irritability, social withdrawal, sadness, interpersonal sensitivity, sleep disturbance, somatic complaints, fatigue, and difficulties concentrating (Bailie et al., 2016; Lange et al., 2014; Morissette et al., 2011).
Although several studies find that deployment-related TBI is significantly associated with postconcussive symptoms, distress, and decreased health-related quality of life (Brickell, Lange, & French, 2014; Dretsch, Silverberg, & Iverson, 2015; Vanderploeg et al., 2012), critical and meta-analytic reviews of the literature (Broshek, De Marco, & Freeman, 2015; Panayioutou, Jackson, & Crowe, 2010) and longitudinal studies of predeployment characteristics (Lee, Garber, & Zamorski, 2015) indicate that a variety of psychological and contextual factors (e.g., litigation) account for much of the variance associated with chronic emotional and psychosocial problems reported post-TBI. Consequently, research is needed to isolate the psychological characteristics associated with complicated adjustment among Veterans with deployment-related TBI, preferably with variables that can inform assessment practices and psychological interventions. This kind of research may be best conducted with a wide range of Veterans (e.g., Veterans who have TBI, PTSD, both, or neither) who vary in the degree to which they are exposed to combat (Bahrani et al., 2014).
The aim of the present study was to examine the degree to which resilient personality characteristics (Block, 1993; Block & Block, 1980) might be associated with Iraq/Afghanistan Veterans’ adjustment and distress. The majority of returning Veterans display few, if any, psychological problems after warzone deployment, consistent with our contemporary understanding of resilience (Bonanno et al., 2012). Unfortunately, the lack of a comprehensive, clinically relevant theoretical model confounds attempts to identify the mechanisms through which resilience facilitates adjustment under specific situations, thwarting the development of interventions that promote resilience (Davydov, Stewart, & Chandieu, 2010; Fletcher & Sarkar, 2013).
Recent cross-sectional studies find that self-reported resilience is associated with adjustment in expected directions among persons with TBI (Losoi, et al., 2015; Merritt, Lange, & French, 2015; Sullivan, Edmed, Allan, Smith, & Karlsson, 2015; see McCauley, et al., 2013, for a more complicated pattern). However, the measures in these studies are limited because they were developed with “no real theoretical model for their concept of resilience, leaving clinicians and researchers with a relatively face-valid, self-report measure and little guidance for working with respondents” (Elliott & Erosa, 2016, p. 208).
We rely on a theoretical model of resilience that has clear implications for clinical practice. Most contemporary descriptions emphasize the presence of stressful conditions or events to reveal individual characteristics that signify “resilience” (e.g., the ability to “bounce back” or demonstrate “better than expected” adjustment or development in the face of adversity; Fletcher & Sarkar, 2013). The Block theory of ego control and resiliency (Block, 1993; Block & Block, 1980) stipulates that resilience develops from healthy attachments during infancy and childhood and is characterized by various resources and capacities that facilitate effective adaptation to change and conflict.
Resilient children and adults are more socially competent than those who are not, and they are more likely to exhibit better physical and emotional health outcomes (Caspi & Silva, 1995; Chapman & Goldberg, 2011; Dennissen, Asendorpf, & van Aken, 2008). Resilient individuals exhibit proactive behavior, pursue personally meaningful goals, and report greater flexibility, resourcefulness, and active engagement with the environment under routine and stressful circumstances (Block & Kremen, 1996; Ong, Bergeman, & Boker, 2009). Studies informed by this model also find that resilient individuals have a propensity for positive emotions, and that positive emotions appear to be pivotal in “undoing” the negative effects of pain and traumatic disability (Ong, Zautra, & Reid, 2010; Walsh et al., 2016).
In contrast, children who experience unhealthy attachments are more likely to develop personality patterns indicative of an undercontrolled or overcontrolled prototype. The former are more prone to externalizing problem behaviors (e.g., lacking self-control, disagreeable, impulsive) and the latter to internalizing behaviors (e.g., tense, sensitive, emotionally brittle; Robins, John, Caspi, Moffitt, & Stouthamer-Loeber, 1996). For example, children with an undercontrolled personality prototype have a greater risk of injury than other children (Berry & Schwebel, 2009). Mistrust of others (including family members) and conflicts in social relationships are observed among undercontrolled prototypes (Asendorpf, Borkenau, Ostendorf, & Van Aken, 2001; Steca, Alessandri, & Caprara, 2010). Overcontrolled individuals are more likely to use ineffectual coping strategies and report more difficulties coming to terms with acquired disability (Berry, Elliott, & Rivera, 2007), have lower self-rated health (Kinnunen et al., 2015), and report more socially isolated and fewer recreational activities in older age (Steca et al., 2010). In sum, the overcontrolled and undercontrolled subtypes are at higher risk for a wide variety of negative outcomes in comparison to the resilient subtype.
This model dictates several testable hypotheses concerning self-reported adjustment and quality of life among Iraq/Afghanistan Veterans with and without TBI. We expect that Veterans with a resilient personality prototype will report fewer symptoms of PTSD and depression and a greater quality of life than Veterans with undercontrolled or overcontrolled personality profiles, regardless of TBI status. Veterans self-reporting a resilient personality prototype are also expected to report fewer health problems and more psychological resources, including greater distress tolerance, psychological flexibility, health promoting behaviors, adaptive coping behaviors, and social support than the other prototypes.
We also tested the association of deployment-related TBI with each dependent variable to better understand the association between TBI and these outcomes. In a previous study, we established the existence of the three personality prototypes in a sample of 127 Veterans recruited for a larger longitudinal study of war zone experiences and postdeployment adjustment (entitled Project SERVE; Elliott et al., 2015). That paper did not systematically examine differences between the personality prototypes and the TBI status on the wide array of adjustment variables administered during the course of the project. The present study relies on the same sample to examine different patterns of self-reported adjustment and quality of life on measures that were administered at baseline and others that were administered 4 months and 8 months later.
Method
Participants and Procedure
The local institutional review board approved all procedures. Participants were recruited through in-service presentations, mailings to Veterans enrolled in a regional Veterans’ health care system, and advertisements at recruitment sites and Veterans’ service organizations. Eligible participants were required to be enrolled in the local VA health care system; however, they were not required to be receiving treatment. Initial eligibility was determined in a phone interview and later confirmed during an in-person interview.
Prospective participants were eligible if they were (a) an Iraq/Afghanistan war Veteran, (b) able to provide informed consent, and (c) able to complete measures in the baseline assessment. Exclusion criteria included (a) a diagnosis of bipolar or psychotic disorder, (b) recently initiated psychiatric medications or psychotherapy (to ensure a period of stabilization so that symptoms assessed at baseline could not be attributed to starting or stopping these therapies), (c) suicidality or homicidality warranting crisis intervention, or (d) plans to move out of the area within 4 months of enrollment.
Participants were screened by telephone with a scripted interview. Eligible participants were scheduled for an in-person assessment. Informed written consent was obtained before the baseline interview and inclusion/exclusion criteria were also confirmed (e.g., diagnostic assessment of exclusionary diagnoses) with diagnostic interviews completed by trained master’s-level and doctoral-level assessors. Diagnostic consensus was reached on all interviews under the supervision of a clinical psychologist. The self-report measures were administered during the baseline interview and at two follow-up mailed assessments 4 and 8 months later. Several measures were administered only at baseline.
Eight of the 145 participants who enrolled in the study were excluded because of schizophrenia or bipolar disorder. Missing items on the personality measure excluded an additional nine individuals. Another individual was excluded because validity criteria on the personality instrument were not met. The final number of participants included in the current analyses was 127 (average age = 37.64 years, standard deviation [SD] = 10.54; average years of education = 14.17, SD = 2.542). The majority of the sample was male (n = 107) and identified as White/Caucasian (n = 80; African American, n = 23; other, n = 24); 33 participants (30%) identified their ethnicity as Hispanic. Approximately 64% of the sample had a service-connected pension for a disability.
Independent Variables
Personality prototypes
Personality prototypes were determined from the Multidimensional Personality Questionnaire Brief Form (MPQ; Patrick et al., 2002) administered at baseline. The MPQ contains 155 items (with a true/false response format) and comprises 11 primary trait scales that constitute three higher order dimensions: Positive Emotionality (PEM), Negative Emotionality (NEM), and Constraint (CON). Higher PEM scores reflect a positive, active engagement with the environment and a capacity for positive emotions (e.g., enthusiasm, zest). Higher NEM scores reflect a predisposition for anger, resentment, anxiety, and negatively valenced emotional relationships. Higher CON scores reflect a tendency for caution, harm avoidance, and convention; lower scores are associated with impulsivity and sensation-seeking behaviors.
A two-step cluster analysis with Ward’s method followed by a K-means analysis was conducted to create clusters from PEM, NEM, and CON scores (see Elliott et al., 2015, for details). Following conventional guidelines, K-means clustering methods assigned each participant into one of the three resulting clusters, and the Cohen’s Kappa coefficient (.67) indicated substantial agreement (Landis & Koch, 1977). The three resulting personality prototypes served as an independent variable. Consistent with the Block conceptualization, the resilient prototype (n = 51) was characterized by the highest PEM and CON scores and the lowest NEM scores of the three clusters. The overcontrolled prototype (n = 27) had the highest NEM scores, and the undercontrolled group (n = 49) had the lowest CON scores and the lowest PEM scores.
Assessment of TBI
The Brief Traumatic Brain Injury Screen (BTBIS; Schwab et al., 2007) was administered at baseline. A total of 57 Veterans (44.8% of the sample) screened positive for TBI based on endorsement of a head injury during deployment (e.g., from a blast, vehicular accident, fall, bullet, fragment) that resulted in altered consciousness (e.g., being disoriented, “dazed,” or confused, seeing “stars”), loss of consciousness, or posttraumatic amnesia.
Covariate: Combat Exposure
Because the Veterans differed in the degree of combat experience, the 18-item Full Combat Exposure Scale (FCES; Hoge et al., 2004), administered at baseline, was entered as a covariate in all analyses to account for any variance attributable to combat experiences during warzone deployment (e.g., being attacked or ambushed, handling human remains, incoming mortars). Higher scores indicate greater exposure. Internal consistency was .92.
Dependent Variables
Sleep quality
The Pittsburgh Sleep Quality Index (PSQI; Buysse, Reynolds, Monk, Berman & Kupfer, 1989) was used to assess sleep quality at baseline. Eighteen items assess sleep quality and disturbances over the previous month. Responses are scored as seven sub-scores: subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication, and daytime dysfunction due to fatigue. These sub-scores are summed to obtain the participant’s total score. Higher scores indicate greater sleep disturbance. The internal consistency of the PSQI scores for this sample was .84.
Self-reported resilience
The Connor-Davidson Resilience Scale (CDRISC; Connor & Davidson, 2003) was administered at baseline to assess self-reported resilience. The authors developed the instrument to assess “personal qualities that enables one to thrive” in stressful circumstances (Connor & Davidson, 2003, p. 76). It contains 25 items rated on a 5-point Likert-type scale ranging from 0 (not true at all) to 4 (true nearly all of the time). Higher total scores reflect greater resilience. The CD-RISC demonstrates acceptable psychometric properties in studies of Veterans (Green et al., 2014; Tsai, Harpaz-Rotem, Pietrzak, & Southwick, 2012). The psychometric properties of the CDRISC are considered the best in comparisons with other self-report resilience measures (Windle, Bennett, & Noyes, 2011). Internal consistency for this sample was .96.
Health behaviors
The Health-Promoting Lifestyle Profile II (HPLP; Walker, Sechrist, & Pender, 1995) assessed health behaviors at baseline. The scale has 52 items that are rated on a 4-point Likert-type scale ranging from 1 (never) to 4 (regularly). The instrument has a total score and several subscales including health responsibility, physical activity, nutrition, spiritual growth, interpersonal relations, and stress management. Higher scores on each scale indicate healthier styles. We used the total score and the separate subscale scores as dependent variables. The internal consistency for each subscales and the total score were all above .80 (health responsibility = .82; physical activity = .89; nutrition = .84; spiritual growth = .91; interpersonal relations = .91; stress management = .82; and total score = .96).
Distress tolerance
The Distress Tolerance Inventory (DT; Kruse, 2008; Telch & Smith, 2016) was used to assess the extent to which participants tolerate physical (six items; e.g., “I’ll take fairly extreme measures to stop physical discomfort or pain”) and emotional (10 items; e.g., “I usually follow through with tasks that are emotionally upsetting”) distress. Participants rated the extent to which they agreed with each item using 6-point Likert scales with response options ranging from 1 (strongly agree) to 6 (strongly disagree). Summary scores were created by calculating the average for items across the physical and emotional subscales. Higher scores on each indicate greater tolerance. The physical DT and the emotional DT scales had internal consistency coefficients of .76 and .87, respectively.
Psychological inflexibility
The Acceptance and Action Questionnaire-II (AAQ-II; Bond et al., 2011) was administered at baseline to assess psychological inflexibility and experiential avoidance of unwanted emotions, cognitions, and physiological sensations (Hayes et al., 2004). The AAQ-II features seven items rated on a 7-point Likert-type scale ranging from 1 (never true) to 7 (always true). The AAQ-II exhibits a single-factor structure, good internal consistency, good test–retest reliability, and good convergent associations with the original AAQ (Bond et al., 2011). In a prior study with this sample, psychological inflexibility was shown to be distinct from the related constructs of negative emotionality and the avoidance symptoms of PTSD (Meyer, Morissette, Kimbrel, Kruse, & Gulliver, 2013). Higher scores indicate greater inflexibility. Internal consistency was .94.
Coping
The Brief COPE (B-COPE, Carver, 1997) assessed coping styles at each measurement occasion. The Brief COPE consists of 28 items that are rated on a 4-point Likert-type scale, ranging from 0 (I haven’t been doing this at all) to 3 (I’ve been doing this a lot). We relied on a previous factor analysis of the B-COPE (Grosso et al., 2014) to create two factor scores for analysis: action-oriented and avoidant coping. Higher scores reflect a greater proclivity for that coping style. Internal coefficients ranged from .83 to .84 (action-oriented coping) and .67 to .76 (avoidant coping) across the three time points.
Social support
The DRRI-Postdeployment Social Support scale (PDSS) from the Deployment Risk and Resilience Inventory (King, King, Vogt, Knight, & Samper, 2006) was used to assess perceived availability of social support at each measurement occasion. This 15-item self-report scale uses a 5-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). Validated for use with Iraq/Afghanistan Veterans (Vogt, Proctor, King, King, & Vasterling, 2008), the PDSS assesses perceived emotional and instrumental forms of social support from family, friends, employers, and the community after deployment. Higher scores indicate greater social support. Internal consistency values ranged from .88 to .90 across the three time points.
PTSD symptoms
The PTSD Checklist–Military Version (PCL-M; Weathers, Litz, Herman, Huska, & Keane, 1993) was administered at each measurement occasion. The 17-item PCL-M assesses military-related PTSD symptoms experienced during the past month according to the Diagnostic and Statistical Manual of Mental Disorders Fourth Edition (American Psychiatric Association, 1994) criteria. The PCL-M has excellent internal consistency and validity (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). Higher scores indicate greater PTSD symptomology; a cutoff score of 50 is often used to indicate probable PTSD (Forbes, Creamer, & Biddle, 2001;Weathers et al., 1993). Internal consistency estimates ranged from .96 to .97 across the three measurement occasions.
Depression
The Beck Depression Inventory-II (BDI-II; Beck, Steer, & Brown, 1996) was administered at each measurement occasion. The BDI-II contains 21 items rated on a 4-point Likert-type scale. Higher scores indicate greater severity of depressive symptoms. Internal consistency coefficients ranged from .95 to .96 across the three measurement occasions.
Health-related quality of life
The Veterans Rand 12-item survey (VR-12; Kazis et al., 2006) was used to assess health-related quality of life (HRQL) at each measurement occasion. The two composite scores are computed from responses to the VR-12 and these were used as dependent variables: the mental composite summary and the physical composite summary. Scores range from 0 to 100 for each and higher scores denote greater HRQL. The internal consistency coefficients for the composite scores ranged from .88 to .90 across the three time points.
Quality of life
The Quality of Life Scale (QLS; Burckhardt, Woods, Schultz, & Ziebarth, 1989) assessed global quality of life at each measurement occasion. The QLS has 16 items that are rated on a 7-point satisfaction scale. Higher scores indicate greater well-being and satisfaction. Across the three measurement occasions, internal consistency coefficients ranged from .94 to .95.
Statistical Analyses
Two different analytic strategies were utilized based on the number of times the dependent measures were administered. For measures collected only at baseline, analyses of covariance (ANCOVA) were used with TBI status (TBI: positive or negative) and personality prototypes (overcontrolled, undercontrolled, or resilient) as the between-subject factors and combat exposure as a covariate. For all ANCOVAs, η2 values were computed as effect sizes, with cutoffs of .01, .06, and .14 denoting small, medium, and large effect sizes (Cohen, 1988). Significant main effects were followed up with post-hoc pairwise t tests with a Bonferroni correction. Simple main effect tests were conducted as follow up for significant interaction effects. These analyses were conducted with SPSS 22.0.
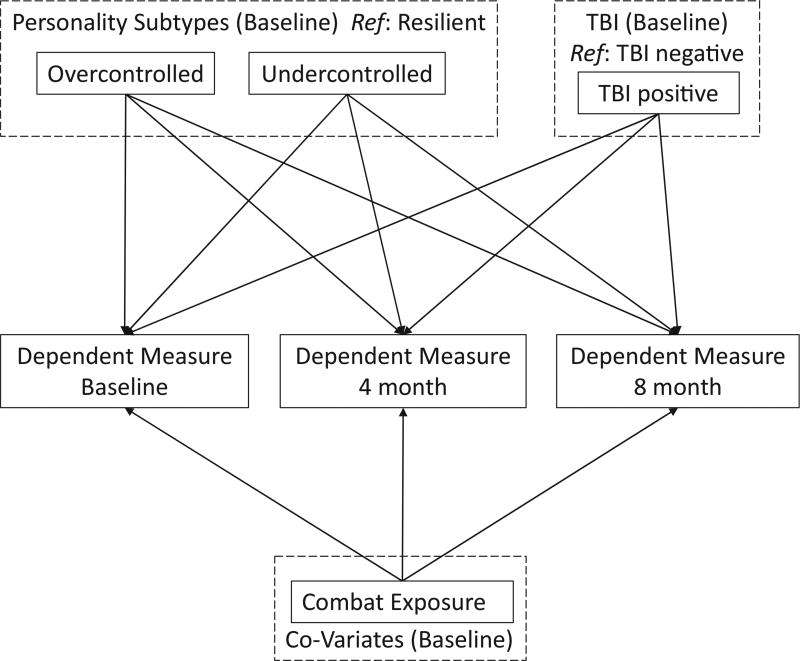
Path analyses under the Structural Equation Modeling (SEM) framework were conducted to model the effects of the independent variables on the dependent measures that were administered at each measurement occasion. Figure 1 depicts the model testing the relation of personality and TBI with each dependent measure at each time point. Personality prototype was recoded into two dummy variables: overcontrolled vs. resilient and undercontrolled vs. resilient. Hence, the dependent variables assessed at three time points (baseline, 4 months, and 8 months) were predicted by TBI and the two personality variables, and combat exposure served as a co-variate in each model.
Figure 1.
General path model for testing personality prototypes and TBI effects on adjustment measures at three time points.
For each path model, we began with a saturated model and excluded one non-significant path from the model to estimate model fit. Model fit was evaluated by the following criteria: chi-square test was nonsignificant at alpha = .05; the comparative fit index (CFI) and Tucker-Lewis index (TLI) were both above .95 (Hu & Bentler, 1999; Yu, 2002); the root mean square error of approximation (RMSEA) was below .08 (Browne & Cudeck, 1992); and the standardized root mean square residual (SRMR) was below .08 (Hu & Bentler, 1999). All the path analyses were conducted with Mplus 7.11 (Muthén & Muthén, 1998–2013). Missing data were accommodated with the maximum likelihood estimation method, to use all available information from the 127 participants. In addition, 1,000 bootstrapping samples were conducted to estimate the 95% confidence intervals (CIs) for all path coefficients (Effron, 1988; Effron & Tibshirani, 1993). The overall R2 values were estimated for each path model. As recommended by Cohen (1995), effect sizes were interpreted using the cutoffs of .02, .15, and .35 as small, medium, and large, respectively.
Results
Of the participants, 90% completed the assessments at each measurement occasion. The preliminary chi-square test of independence found one’s personality type is related to the TBI screen results, χ2 (2) = 12.10, p < .01. Follow-up residual estimates found that individuals in the overcontrolled group were more likely to be positive for TBI (n = 17, 63%, adjusted residual = 2.2), and individuals in the resilient group were more likely to be screened negative for TBI (n = 37; 71%, adjusted residual = 3.4). Individuals in the undercontrolled group did not have different probabilities for either positive and negative TBI screens. More men screened positive for TBI than women, χ2 (1) = 12.84, p < .001. No significant associations were found between gender and personality prototype.
Table 1 contains the mean scores for the dependent variables that were assessed only at baseline by personality prototype and TBI status. Table 2 depicts the F values and effect sizes for the separate ANCOVAs conducted on these variables. Personality prototypes were significantly associated with all but one of these variables (the distress tolerance physical subscale). Combat exposure significantly covaried with two dependent variables (the psychological inflexibility total score and sleep disturbance total score). Importantly, TBI status had no significant main effect on any of the dependent variables at baseline. Although we had no theoretical or clinical interest in the TBI X Personality interactions, none of these were statistically significant (all Fs < 2).
Table 1.
Means and Standard Deviations for Baseline-Only Dependent Variables by Personality Prototype and Traumatic Brain Injury Status
| Personality prototype | Traumatic brain injury | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||
| Overcontrolled | Undercontrolled | Resilient | Negative | Positive | ||||||
|
|
|
|
|
|
||||||
| Measure | M | SD | M | SD | M | SD | M | SD | M | SD |
| Combat exposure | 31.08 | 16.48 | 23.26 | 14.98 | 18.34 | 11.56 | 16.94 | 10.59 | 31.44 | 14.90 |
| PSQI | 13.48 | 4.18 | 12.02 | 5.26 | 7.42 | 4.20 | 9.29 | 4.97 | 12.18 | 4.94 |
| CD-RISC | 61.78 | 21.48 | 61.87 | 18.64 | 80.96 | 14.03 | 70.84 | 19.69 | 67.57 | 20.13 |
| HPLP | 109.27 | 23.82 | 108.80 | 23.83 | 139.49 | 24.91 | 124.71 | 29.14 | 115.38 | 26.25 |
| HPLP-h | 18.19 | 3.50 | 18.35 | 4.65 | 21.90 | 5.72 | 19.86 | 5.16 | 19.29 | 5.16 |
| HPLP-p | 14.96 | 4.70 | 16.52 | 5.56 | 20.12 | 6.00 | 17.68 | 5.82 | 17.24 | 6.04 |
| HPLP-n | 17.84 | 4.48 | 18.65 | 5.01 | 22.34 | 5.73 | 20.83 | 5.40 | 18.40 | 5.18 |
| HPLP-s | 21.72 | 6.78 | 20.36 | 5.03 | 28.48 | 4.66 | 24.89 | 6.56 | 22.35 | 6.06 |
| HPLP-i | 21.04 | 6.92 | 19.62 | 4.94 | 26.63 | 5.29 | 23.41 | 6.64 | 21.71 | 5.79 |
| HPLP-st | 16.46 | 4.52 | 15.85 | 4.13 | 20.42 | 4.38 | 18.11 | 4.88 | 17.43 | 4.61 |
| DT-p | 3.95 | 1.06 | 4.03 | 1.02 | 4.54 | 0.80 | 4.42 | 0.92 | 3.98 | 0.98 |
| DT-e | 2.73 | 0.72 | 3.33 | 0.93 | 4.14 | 0.80 | 3.67 | 0.98 | 3.37 | 0.98 |
| AAQ-II | 30.26 | 11.74 | 27.17 | 9.92 | 15.71 | 7.84 | 19.94 | 10.82 | 27.29 | 10.96 |
Note. M = mean; SD = standard deviation; PSQI = Pittsburgh Sleep Quality index total score; CD-RISC = Connor-Davidson Resilience Scale total score; HPLP = Health-Promoting Lifestyle Profile total score; HPLP-h = HPLP health responsibility; HPLP-p = HPLP physical activity; HPLP-n = HPLP nutrition; HPLP-s = HPLP spiritual growth; HPLP-I = HPLP interpersonal relationships; HPLP-st = HPLP stress management; DT-p = Distress Tolerance Scale physical; DT-e = Distress Tolerance emotional; AAQ-II = Action and Acceptance Questionnaire total score.
Table 2.
Effects of Combat Exposure, Traumatic Brain Injury (TBI), and Personality Prototypes on Adjustment at Baseline: ANCOVA Results and Eta Squares (η2)
| TBI X | ||||||||
|---|---|---|---|---|---|---|---|---|
| Combat exposure | TBI | Personality prototype | Personality prototype | |||||
|
|
|
|
|
|||||
| F | η2 | F | η2 | F | η2 | F | η2 | |
| PSQI | 4.42* | 0.03 | < 0.01 | 0.00 | 8.77*** | 0.13 | 1.29 | 0.02 |
| CD-RISC | 0.96 | 0.01 | 1.83 | 0.01 | 11.36*** | 0.17 | 0.31 | 0.00 |
| HPLP | 0.08 | 0.00 | 0.091 | 0.00 | 16.54*** | 0.24 | 0.38 | 0.01 |
| HPLP-h | 0.93 | 0.01 | 0.38 | 0.00 | 8.34*** | 0.14 | 1.66 | 0.03 |
| HPLP-p | 0.67 | 0.01 | 0.71 | 0.01 | 10.97*** | 0.18 | 0.74 | 0.01 |
| HPLP-n | 0.04 | 0.00 | 0.38 | 0.00 | 3.84* | 0.07 | 0.29 | 0.01 |
| HPLP-s | 0.40 | 0.00 | 0.07 | 0.00 | 19.18*** | 0.28 | 0.24 | 0.00 |
| HPLP-i | < 0.01 | 0.00 | 0.16 | 0.00 | 13.90*** | 0.21 | 0.71 | 0.01 |
| HPLP-st | 0.07 | 0.00 | 1.14 | 0.01 | 9.58*** | 0.16 | 1.35 | 0.02 |
| DT-p | 0.32 | 0.00 | 0.95 | 0.01 | 2.86 | 0.05 | 0.72 | 0.01 |
| DT-e | 0.01 | 0.00 | 0.10 | 0.00 | 23.95*** | 0.30 | 0.01 | 0.00 |
| AAQ-II | 8.60** | 0.05 | 0.16 | 0.00 | 15.68*** | 0.18 | 0.16 | 0.00 |
Note. PSQI = Pittsburgh Sleep Quality Index total score; CD-RISC = Connor-Davidson Resilience Scale total score; HPLP = Health-Promoting Lifestyle Profile total score; HPLP-h = HPLP health responsibility; HPLP-p = HPLP physical activity; HPLP-n = HPLP nutrition; HPLP-s = HPLP spiritual growth; HPLP-I = HPLP interpersonal relationships; HPLP-st = HPLP stress management; DT-p = Distress Tolerance Scale physical; DT-e = Distress Tolerance Scale emotional; AAQ-II = Action and Acceptance Questionnaire total score.
p < .05.
p < .01.
p < .001.
The significant association between personality and sleep disturbance (the PSQI), F(2, 98) = 8.77, p < .001, η2 = .13, was attributable to the lower scores observed among the resilient group: Post hoc tests indicated that this group reported fewer sleep problems when corrected for combat exposure than either the overcontrolled or the undercontrolled groups. These latter two personality groups reported a comparable number of sleep problems. A similar pattern was observed in the association between personality and self-reported resilience (CD-RISC), F(2, 103) = 11.36, p < .001, η2 = .17, and psychological inflexibility (AAQ-II), F(2, 103) = 15.68, p < .001, η2 = .18. Pairwise t-test results revealed that the resilient group reported more resilience and less psychological inflexibility when controlling for combat exposure than either the overcontrolled or undercontrolled groups, which did not differ on either of these dependent variables.
A significant main effect occurred for personality on overall health-promoting lifestyle, F(2, 99) = 16.54, p<.001, η2 = .24. Pairwise t-test results indicated that, after controlling for combat exposure, Veterans with a resilient personality reported more health promotive behaviors than Veterans in the overcontrolled or undercontrolled groups. A significant main effect occurred for personality on each of the health-promoting lifestyle (HPLP-II) subscale scores: health responsibility, F(2, 99) = 8.34, p < .001, η2 = .14, physical activity, F(2, 97) = 10.97, p < .001, η2 = .18, nutrition, F(2, 96) = 3.84, p <.05, η2 = .07, spiritual growth, F(2, 93) = 19.18, p < .001, η2 = .28, interpersonal relationships, F(2, 97) = 13.90, p < .001, η2 = .21, and stress management, F(2, 96) = 9.58, p < .001, η2 = .16. Pairwise t-test results indicated that, after controlling for combat exposure, Veterans with a resilient personality reported more responsibility for their health, were more physically active, focused more on spiritual growth, experienced greater intimacy and closeness in their relationships, and endorsed more stress management strategies than Veterans in the overcontrolled or undercontrolled groups. These two latter groups did not significantly differ on any of these subscales. Additional post hoc test results showed that Veterans in the resilient personality group reported eating a healthier diet than those with the overcontrolled prototype. However, no difference was found in the nutrition scores between the overcontrolled and undercontrolled groups, or between the resilient and undercontrolled groups.
The effects of personality on distress tolerance were mixed. The main effect on the DT physical subscale was not statistically significant, F(2, 104) = 2.86, p = .062, η2 = .05. However, a main effect was found on the DT emotional subscale, F(2, 104) = 23.95, p < .001, η2 = .30. The resilient group reported the highest emotional distress tolerance among the three personality prototypes, followed by undercontrolled and overcontrolled groups, which did not differ from one another.
Inspection of the effect sizes indicate that personality had large effects on tolerance for emotional distress, psychological inflexibility, personal responsibility for health, stress management, spiritual growth, interpersonal relationships, and physical activity. A medium to large effect size was observed in the relationship between personality and sleep quality.
Path Analyses
The means and standard deviations for the repeated measures are in Tables 3 and 4. Table 5 presents the results of the path analyses for the adjustment measures administered at three time points. Predictor variables and dependent variables were allowed to correlate in these models to reflect naturally occurring relationships. For all eight path models, the paths from combat exposure to each of the dependent measures at 4 months were nonsignificant. Therefore, these paths were excluded in all the path models (and the paths from combat exposure to baseline and 8 months were retained). The corrected models fit the data adequately for all eight dependent variables, χ2 (1) = .06~1.59, p > .05; CFI = .99~1.00; TLI = .97~1.00; RMSEA = .00~.07; SRMR = .00~.02. Thus, the path coefficients were considered interpretable from the corrected models. Additionally, all R2 values for the path models were above .02 (indicative of a small effect size) with a range from .02 to .45 (a large effect size), indicating that 2% to 45% of the variance in dependent variables were explained by the predictors in the final models.
Table 3.
Means and Standard Deviations for Adjustment and Quality of Life Measures Over Time by Personality Prototypes
| Overcontrolled | Undercontrolled | Resilient | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||||||||
| Baseline | 4 months | 8 months | Baseline | 4 months | 8 months | Baseline | 4 months | 8 months | ||||||||||
|
|
|
|
|
|
|
|
|
|
||||||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Cope action | 11.78 | 3.71 | 10.08 | 3.92 | 8.98 | 2.88 | 9.28 | 3.64 | 7.91 | 3.42 | 8.05 | 3.79 | 12.50 | 3.65 | 10.20 | 3.97 | 10.60 | 4.33 |
| Cope avoid | 3.98 | 2.47 | 4.24 | 2.73 | 3.52 | 2.07 | 3.79 | 1.98 | 3.20 | 1.97 | 3.51 | 2.31 | 1.93 | 1.48 | 1.77 | 1.96 | 2.27 | 2.25 |
| Social Support | 51.79 | 9.95 | 47.10 | 9.78 | 47.50 | 9.62 | 49.07 | 9.79 | 47.63 | 8.56 | 45.39 | 9.78 | 60.24 | 7.86 | 57.06 | 8.38 | 56.65 | 9.17 |
| PTSD | 57.56 | 16.95 | 56.00 | 14.85 | 60.24 | 15.13 | 54.31 | 17.33 | 50.51 | 15.22 | 51.50 | 17.76 | 32.64 | 15.70 | 33.50 | 17.14 | 33.98 | 16.57 |
| BDI | 26.30 | 14.93 | 29.63 | 14.16 | 32.13 | 12.66 | 24.85 | 10.86 | 25.38 | 11.63 | 24.20 | 12.99 | 7.12 | 6.40 | 11.22 | 12.31 | 11.08 | 9.84 |
| VR12 MCS | 33.62 | 11.15 | 38.95 | 14.72 | 30.50 | 9.36 | 36.13 | 13.67 | 40.68 | 14.23 | 35.02 | 13.40 | 51.08 | 9.98 | 41.32 | 13.67 | 47.92 | 11.16 |
| VR12 PCS | 34.32 | 8.62 | 41.64 | 11.99 | 33.20 | 9.66 | 42.94 | 10.51 | 42.84 | 12.09 | 42.04 | 11.15 | 46.44 | 10.16 | 39.97 | 12.32 | 46.18 | 10.98 |
| QLS | 63.93 | 22.26 | 59.88 | 18.41 | 55.09 | 15.17 | 67.56 | 15.45 | 63.07 | 15.89 | 63.69 | 16.77 | 85.60 | 14.18 | 82.66 | 16.10 | 81.19 | 18.74 |
Note. M = mean; SD = standard deviation; Cope action: Action coping factor score; Cope avoid: Avoidance coping factor score; PTSD = PCL total score; BDI = Beck Depression Inventory II total score; VR12 MCS = VR12 mental composite score; VR12 PCS = VR 12 physical composite score; QLS = Quality of Life total score.
Table 4.
Means and Standard Deviations for Adjustment and Quality of Life Measures Over Time by Traumatic Brain Injury Status
| Negative | Positive | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||||||
| Baseline | 4 months | 8 months | Baseline | 4 months | 8 months | |||||||
|
|
|
|
|
|
|
|||||||
| M | SD | M | SD | M | SD | M | SD | M | SD | M | SD | |
| Cope action | 11.04 | 4.06 | 9.17 | 4.14 | 9.56 | 4.26 | 11.00 | 3.71 | 9.44 | 3.67 | 8.96 | 3.57 |
| Cope avoid | 2.94 | 2.38 | 2.48 | 2.67 | 2.69 | 2.39 | 3.37 | 1.75 | 3.17 | 1.67 | 3.39 | 2.13 |
| Social Support | 57.16 | 9.87 | 54.55 | 9.01 | 53.69 | 10.07 | 52.33 | 10.10 | 48.71 | 10.00 | 47.11 | 9.92 |
| PTSD | 39.38 | 19.15 | 38.00 | 18.06 | 37.41 | 18.40 | 55.93 | 16.22 | 53.06 | 15.32 | 55.04 | 15.94 |
| BDI | 14.46 | 13.27 | 16.19 | 14.66 | 15.05 | 12.15 | 22.49 | 12.87 | 25.85 | 12.81 | 26.46 | 13.98 |
| VR12 MCS | 44.49 | 14.38 | 42.29 | 13.14 | 44.11 | 13.24 | 36.71 | 12.11 | 38.47 | 15.14 | 33.80 | 11.97 |
| VR12 PCS | 44.61 | 10.07 | 43.45 | 11.61 | 43.69 | 11.36 | 39.57 | 11.46 | 39.54 | 12.60 | 39.38 | 11.80 |
| QLS | 75.78 | 20.42 | 73.28 | 21.88 | 73.98 | 20.25 | 70.80 | 16.84 | 66.81 | 15.25 | 63.24 | 18.65 |
Note. M=mean; SD=standard deviation; Cope action: Action coping factor score; Cope avoid: Avoidance coping factor score; PTSD = PCL total score; BDI = Beck Depression Inventory II total score; VR12 MCS = VR12 mental composite score; VR12 PCS = VR 12 physical composite score; QLS = Quality of Life total score.
Table 5.
Unstandardized Path Coefficients of Personality Prototypes and TBI on Adjustment and Quality of Life Over Time
| Overcontrolled vs. Resilient | Undercontrolled vs. Resilient | TBI positive vs. TBI negative | ||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||
| Coefficients | 95% CIa | Coefficients | 95% CIa | Coefficients | 95% CIa | R2 | ||
| Cope action | ||||||||
| Baseline | −1.10 | [−2.86, 0.67] | −3.37*** | [−4.89, −1.85] | 0.09 | [−1.38, 1.56] | .15 | |
| 4 months | −0.66 | [−2.71, 1.39] | −2.31** | [−3.90, −0.72] | 0.83 | [−0.51, 2.18] | .07 | |
| 8 months | −1.55 | [−3.41, 0.30] | −2.60** | [−4.35, −0.84] | −0.66 | [−2.24, 0.91] | .09 | |
| Cope avoid | ||||||||
| Baseline | 2.02*** | [0.81, 3.22] | 1.89*** | [1.15, 2.63] | −0.31 | [−1.12, 0.50] | .21 | |
| 4 months | 2.65*** | [1.22, 4.08] | 1.56** | [0.69, 2.42] | 0.04 | [−0.83, 0.91] | .20 | |
| 8 months | 0.92 | [−0.45, 2.28] | 1.25* | [0.22, 2.27] | 0.29 | [−0.85, 1.42] | .09 | |
| Social support | ||||||||
| Baseline | −8.42*** | [−13.25, −3.58] | −11.34*** | [−15.75, −6.94] | −1.93 | [−6.00, 2.14] | .27 | |
| 4 months | −8.41*** | [−13.63, −3.18] | −8.23*** | [−12.19, −4.27] | −0.29 | [−4.38, 3.80] | .24 | |
| 8 months | −6.80** | [−11.62, −1.98] | −10.40*** | [−14.37, −6.44] | −3.88* | [−7.63, −0.13] | .27 | |
| PTSD | ||||||||
| Baseline | 17.74*** | [9.10, 26.39] | 17.25*** | [10.87, 23.63] | 7.51* | [0.88, 14.14] | .42 | |
| 4 months | 17.81*** | [9.33, 26.29] | 14.81*** | [8.17, 21.44] | 10.59*** | [4.38, 16.80] | .34 | |
| 8 months | 18.99*** | [10.18, 27.79] | 14.27*** | [7.71, 20.84] | 7.69* | [1.14, 14.25] | .38 | |
| BDI | ||||||||
| Baseline | 17.25*** | [10.56, 23.94] | 16.91*** | [13.29, 20.52] | 1.24 | [−2.77, 5.25] | .45 | |
| 4 months | 16.36*** | [9.13, 23.60] | 12.98*** | [8.10, 17.86] | 4.90* | [0.06, 9.74] | .31 | |
| 8 months | 14.83*** | [8.23, 21.42] | 11.42*** | [7.01, 15.83] | 3.38 | [−1.07, 7.82] | .37 | |
| VR12 MCS | ||||||||
| Baseline | −15.06*** | [−21.06, −9.06] | −14.75*** | [−19.71, −9.79] | −0.16 | [−5.18, 4.86] | .39 | |
| 4 months | −0.69 | [−9.06, 7.68] | 0.66 | [−5.95, 7.26] | −3.51 | [−9.80, 2.78] | .02 | |
| 8 months | −12.55*** | [−18.29, −6.81] | −11.80*** | [−16.77, −6.83] | −3.44 | [−8.70, 1.82] | .34 | |
| VR12 PCS | ||||||||
| Baseline | −9.95*** | [−14.92, −4.98] | −2.85 | [−7.08, 1.37] | −2.12 | [−6.77, 2.52] | .19 | |
| 4 months | 3.91 | [−2.58, 10.40] | 4.65 | [−0.82, 10.11] | −5.16* | [−10.23, −0.09] | .06 | |
| 8 months | −10.30*** | [−16.41, −4.18] | −3.68 | [−8.12, 0.76] | 1.18 | [−3.71, 6.06] | .25 | |
| QLS | ||||||||
| Baseline | −22.20*** | [−32.07, −12.33] | −18.38*** | [−24.55, −12.20] | 0.87 | [−5.70, 7.43] | .25 | |
| 4 months | −22.53*** | [−31.59, −13.48] | −19.48*** | [−26.13, −12.84] | −0.19 | [−6.35, 5.97] | .28 | |
| 8 months | −21.60*** | [−29.94, −13.25] | −17.26*** | [−24.30, −10.22] | −1.73 | [−9.41, 5.95] | .26 | |
Note. Resilient personality prototype is the reference group. Cope action: Action coping factor score; Cope avoid: Avoidance coping factor score; PTSD = PCL total score; BDI = Beck Depression Inventory II total score; VR12 MCS = VR12 mental composite score; VR12 PCS = VR 12 physical composite score; QLS = Quality of Life total score.
95% confidence intervals (CIs) were calculated from 1000 bootstrapping samples.
p < .05.
p < .01.
p < .001.
For all the path coefficients in the final models, the statistically significant results based on the p values were consistent with the 95% CI constructed from 1,000 bootstrapping samples (e.g., if a p value was smaller than .05, the corresponding 95% CI would not contain zero, and vice versa). Therefore, the following results were interpreted based on their corresponding p values. After accounting for combat exposure, personality prototype had significant and consistent effects across time on social support, PTSD, depression, and overall quality of life (all ps < .001). A resilient personality prototype predicted significantly fewer symptoms of PTSD and depression, more social support, and a greater quality of life than an undercontrolled or overcontrolled prototype. The contributions of TBI to these models were mixed: A positive TBI screen predicted higher PTSD scores at each assessment, higher depression scores at 4 months, and lower social support at 8 months (all ps < .05). TBI was not significantly associated with overall quality of life at any time point.
Compared to the resilient prototype, an undercontrolled personality prototype predicted less action oriented and more avoidant strategies across the three time points (all ps < .05). The overcontrolled group also applied more avoidant coping strategies than the resilient group at baseline and 4 months (all ps < .001), but these two groups did not differ in avoidant coping at 8 months. The overcontrolled group did not differ from the resilient group in action coping. TBI did not significantly predict either coping strategy at any time.
A mixed pattern was observed in the models in predicting health-related quality of life. The overcontrolled personality prototype predicted lower mental and physical composite scores than the resilient group at baseline and at 8 months, but these groups did not differ on this dimension at 4 months. The undercontrolled prototype was significantly associated with lower mental composite scores compared to the resilient groups at baseline and at 8 months. A positive TBI screen significantly predicted lower physical composite scores only at 4 months.
Discussion
Studies of personality characteristics and TBI often examine the degree to which these characteristics are associated with postconcussive symptoms (e.g., Gardner, Sullivan, & Lange, 2010), or they use omnibus personality instruments to assess adjustment that may be differentially associated with varying levels of TBI severity (e.g., Kennedy, Cooper, Reid, Tate, & Lange, 2015). In much of this work, personality characteristics are construed as covariates or as dependent variables, without regard to any theoretical model of personality functioning and corresponding hypotheses concerning individual differences in adjustment. The current study relied on a theoretical model of personality to examine predicted effects of personality prototypes and TBI on adjustment, taking into account the intricacy of myriad factors affecting long-term recovery of warzone Veterans.
Consistent with Block’s theory of ego control and resiliency, Veterans with a resilient personality reported less distress (including fewer symptoms of PTSD and depression over an 8-month period) and a higher quality of life. In addition, a resilient personality prototype was significantly associated with more personal resources that are theoretically characteristic of resilience, including psychological flexibility, tolerance for emotional distress, social support, adaptive health behaviors, and self-reported resilience. In contrast, Veterans with an overcontrolled or undercontrolled personality prototype reported more sleep disturbance and distress, a lower quality of life, and fewer personal resources than those with a resilient prototype. Finally, these significant associations were independent of TBI status and combat exposure.
These findings highlight the role of personality in long-term outcomes and adjustment in returning Veterans. Furthermore, these data suggest that personality characteristics are associated with Veteran adjustment in ways that are more central than those suggested in prior studies that focused on symptom exaggeration and distress among those with and without TBI. Veterans with overcontrolled or undercontrolled profiles report fewer personal and interpersonal resources known to facilitate adjustment, including psychological flexibility, social support, health-promoting behaviors, restful sleep, ability to tolerate emotional distress, and a sense of resilience (as reflected in the Connor-Davidson instrument).
Based on our understanding of the Block model of ego resiliency, these individuals are expected to be susceptible to prolonged experiences of negative affect, have difficulty developing and pursuing meaningful goals and activities, and be worrisome and pessimistic. Consequently, Veterans with these profiles would be more likely than those with resilient profiles to be vigilant for possible health-related problems, have negative expectations about their health, and overinterpret and misattribute symptoms to a negative diagnostic condition (e.g., TBI).
Effects on adjustment consistently attributable to TBI were found for PTSD only. This is of concern given that 12% to 23% of returning service members experience TBI (Fulton et al., 2015; Hoge et al., 2008; Wilk, Herrell, Wynn, Riviere, & Hoge, 2012) as well as the high rates of comorbidity between these conditions (e.g., Carlson et al., 2009). TBI had significant but inconsistent associations with depression (at 4 months), health-related quality of life (to the physical composite score at 4 months), and social support (at 8 months). These data are consistent with other studies demonstrating that after accounting for PTSD symptoms, mild TBI is not associated with several important postdeployment outcomes, including quality of life (Polusny et al., 2011).
A meta-analysis by Panayiotou et al. (2010) found that mild TBI had negligible effects on emotional distress, a known factor contributing to quality of life, and was associated only with acute distress in the context of PTSD (Miskey, Shura, Yoash-Gantz & Rowland, 2015). Although the significant associations between TBI and PTSD in the present study may have some unique predictive value, it is also possible that these relationships were due, in part, to the overlap of postconcussive symptoms with specific items on the PCL instrument (Sumpter & McMillian, 2006; Morissette et al., 2011).
From the present study, it appears that a history of mild TBI has less influence on current adjustment than more enduring factors such as personality. Alternatively, TBI may have already exerted its influence on personality closer in time to the injury (or reciprocally, personality increasing risk for TBI), after which personality primarily contributed to the sustained effects on adjustment. The inconsistent, yet significant association of TBI with depression, social support and physical health-related quality of life speaks to the importance of understanding the effect of the complex relationships among these factors both concurrently and over time.
Our results raise important clinical considerations. Although our findings indicate the value of identifying individuals who have resilient personality characteristics and those who do not, the personality prototypes described in this study are created from cluster analyses of specific samples from behavioral ratings or, more commonly, with measures of “normal” personality traits. Identifying a person as exhibiting a resilient, overcontrolled or undercontrolled personality cannot be achieved for a single individual in a clinically efficient and useful fashion at this time. To date, none of the instruments used in prior studies of the personality prototypes have developed and provided an algorithm to make this determination in an individual report (although the developers and the publishers likely have the requisite normative data to do so).
Nevertheless, according to the prevailing theoretical and explanatory models of resilience in the contemporary literature, long-standing, clinically significant levels of depression or PTSD provide de facto evidence that a person is probably not “resilient,” at least when confronted with the traumatic stressors to which military personnel are commonly exposed. There is little evidence to suggest that interventions designed to promote resilience have any measureable, appreciable effects (Denning et al., 2014; Steenkamp, Nash, & Litz, 2013). The results of the present study illustrate that individuals who lack resilient personality traits may also lack important psychological resources or may be less able to make use of such resources that are associated with optimal adjustment. And it is critical to emphasize that many of the personal resources–including psychological flexibility, social support, restful sleep, ineffectual coping, distress tolerance, stress management strategies, and health-promoting behaviors–can be addressed in existing evidenced-based psychological interventions.
Study strengths include the longitudinal assessment, high retention rates over time, and use of psychometrically sound instruments. However, findings should be interpreted in the context of several limitations. First, the sample size was relatively small and included primarily Caucasian male Veterans who served in support of the wars in Iraq and Afghanistan and were enrolled in the local VA healthcare system. Thus, findings may not generalize to women Veterans, other races, or those who are not enrolled in VA healthcare. The size of the sample falls below some recommendations for using path analyses in studies of this nature (Weston, Chan, Gore, & Catalano, 2008). Conversely, our analyses are theory driven, and our sample size conforms with Kline’s (2005) recommendations for 10 to 20 participants per indicator in each model. The bootstrap analyses provide additional support for our findings.
Data on predeployment personality were not available. We are unable to speak to how personality prototypes may have changed during deployment and in relation to combat exposure and TBI. Similarly, data on predeployment TBI were not available, and our screening measure was unable to account for postdeployment TBI, total number of TBIs, TBI severity, or the role of postconcussive symptoms. Veterans with multiple or more severe TBIs may respond with more distress and have fewer psychological resources compared to those who only experienced a single TBI. Our measurement of TBI was based on retrospective reporting, which could affect findings.
Collectively, our findings indicate the presence of a resilient personality prototype among war Veterans that appears to constitute a “protective trait” (Ong et al., 2009) that facilitates personal and social adjustment. In contrast, Veterans with overcontrolled or undercontrolled profiles appeared to lack important resources that promote adjustment and were more likely to experience chronic problems with depression, PTSD, and a compromised quality of life. Evidenced-based interventions are available to Veterans to address these needs; such services may be critical for long-term recovery, psychological adjustment, physical health, and quality of life.
The present study also demonstrates the value of a trait model of resilience and the potential use of nonpathological personality measures in conceptualizing and predicting adjustment of warzone Veterans with and without TBI. Although TBI was significantly associated with PTSD symptoms over time in this study, it may be limited as an explanatory variable in the larger context of other factors affecting adjustment, particularly when it is measured using a simple positive or negative screening. Additional prospective research is needed to continue to disentangle factors that should be weighted more heavily in prioritizing treatment targets and in efforts to improve long-term adjustment and quality of life among war Veterans.
Acknowledgments
This research was supported by Merit Award #I01RX000304-01 to Dr. Morissette and #I01RX000304-04 to Dr. Meyer and Morissette from the Rehabilitation Research and Development (R&D) Service. Dr. Kimbrel was supported by a Career Development Award (#1IK2 CX000525) from the Clinical Science R&D Service of the VA Office of R&D. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
This study is one in a series conducted from a larger project investigating adjustment of Veterans who served in support of the wars in Iraq and Afghanistan. A complete list of publications from the project is available upon request from Dr. Morissette at Sandra. Morissette@va.gov
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Armed Forces Health Surveillance Center. DoD numbers for traumatic brain injury [data file] 2011 Retrieved from http://www.dvbic.org/TBI-Numbers.aspx.
- Asendorpf JB, Borkenau P, Ostendorf F, Van Aken MA. Carving personality description at its joints: Confirmation of three replicable personality prototypes for both children and adults. European Journal of Personality. 2001;15:169–198. [Google Scholar]
- Bahrani NH, Breshears RE, Hernandez TD, Schneider AL, Forster JE, Brenner LA. Traumatic brain injury and posttraumatic stress disorder. Psychiatric Clinics of North America. 2014;37:55–75. doi: 10.1016/j.psc.2013.11.002. [DOI] [PubMed] [Google Scholar]
- Bailie JM, Kennedy JE, French LM, Marshall K, Prokhorensko O, Asumssen S, Lange RT. Profile analysis of the neurobehavioral and psychiatric symptoms following combat-related mild traumatic brain injury: Identification of subtypes. Journal of Head Trauma Rehabilitation. 2016;31:2–12. doi: 10.1097/HTR.0000000000000142. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Brown GK. Beck Depression Inventory manual. 2. SanAntonio, TX: Psychological Corporation; 1996. [Google Scholar]
- Berry JW, Elliott TR, Rivera P. Resilient, undercontrolled, and overcontrolled personality prototypes among persons with spinal cord injury. Journal of Personality Assessment. 2007;89:292–302. doi: 10.1080/00223890701629813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry JW, Schwebel DC. Configural approaches to temperament assessment: Implications for predicting risk of unintentional injury in children. Journal of Personality. 2009;77:1381–1409. doi: 10.1111/j.1467-6494.2009.00586.x. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Block J. Studying personality the long way. In: Funder DC, Parke RD, Tomlinson-Keasey C, Widaman K, editors. Studying lives through time. Washington, DC: American Psychological Association; 1993. pp. 9–41. [Google Scholar]
- Block JH, Block J. The role of ego control and ego resiliency in the organization of behavior. In: Collins WA, editor. The Minnesota symposium on child psychology: Vol. 13. Development of cognition, affect, and social relations. Hillsdale, NJ: Erlbaum; 1980. pp. 39–101. [Google Scholar]
- Block J, Kremen AM. IQ and ego-resiliency: Conceptual and empirical connections and separateness. Journal of Personality and Social Psychology. 1996;70:349–361. doi: 10.1037//0022-3514.70.2.349. [DOI] [PubMed] [Google Scholar]
- Bonanno GA, Mancini AD, Horton JL, Powell TM, LeardMann CA, Boyko EJ for the Millenium Cohort Study Team. Trajectories of trauma symptoms and resilience in deployed US military service members: Prospective cohort study. British Journal of Psychiatry. 2012;200:317–323. doi: 10.1192/bjp.bp.111.096552. [DOI] [PubMed] [Google Scholar]
- Bond FW, Hayes SC, Baer RA, Carpenter KM, Guenole N, Orcutt HK, Zettle RD. Preliminary psychometric properties of the Acceptance and Action Questionnaire-II: A revised measure of psychological flexibility and experiential avoidance. Behavior Therapy. 2011;42:676–688. doi: 10.1016/j.beth.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Brickell TA, Lange RT, French LM. Health-related quality of life within the first 5 years following military-related concurrent mild traumatic brain injury and polytrauma. Military Medicine. 2014;179:827–838. doi: 10.7205/MILMED-D-13-00506. [DOI] [PubMed] [Google Scholar]
- Broshek DK, De Marco AP, Freeman JR. A review of post-concussion syndrome and psychological factors associated with concussion. Brain Injury. 2015;29:228–237. doi: 10.3109/02699052.2014.974674. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods & Research. 1992;21(2):230–258. [Google Scholar]
- Burckhardt CS, Woods SL, Schultz AA, Ziebarth DM. Quality of life of Adults with chronic illness: A psychometric study. Research in Nursing & Health. 1989;12:347–354. doi: 10.1002/nur.4770120604. [DOI] [PubMed] [Google Scholar]
- Buysse DJ, Reynolds CF, III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- Carlson K, Kehle SM, Meis L, Greer N, MacDonald R, Wilt T. Evidence report/technology assessment prepared by the Minneapolis Veterans Affairs Medical Center, Minnesota Evidence Synthesis Program. Center for Chronic Disease Outcomes Research; Minneapolis, Minnesota: 2009. The assessment and treatment of individuals with history of traumatic brain injury and post-traumatic stress disorder: A systematic review of the evidence. http://www.hsrd.research.va.gov/publications/esp/TBI-PTSD-2009.pdf. [PubMed] [Google Scholar]
- Carver CS. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Caspi A, Silva PA. Temperamental qualities at age three predict personality traits in young adulthood: Longitudinal evidence from a birth cohort. Child Development. 1995;66:486–498. doi: 10.2307/1131592. [DOI] [PubMed] [Google Scholar]
- Chapman BP, Goldberg LR. Replicability and 40-year predictive power of childhood ARC types. Journal of Personality and Social Psychology. 2011;101:593–606. doi: 10.1037/a0024289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cifu DX, Taylor BC, Carne WF, Bidelspach DE, Sayer NA, Scholten J, Hagel E. TBI, PTSD and pain diagnoses in Iraq and Afghanistan conflict veterans. Journal of Rehabilitation Research and Development. 2014;50:1169–1176. doi: 10.1682/JRRD.2013.01.0006. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Earlbaum Associates; 1988. [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1995;112:155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Connor KM, Davidson JRT. Development of a new resilience scale: The Connor-Davidson Resilience Scale (CD-RISC) Depression and Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Davydov DM, Stewart R, Ritchie K, Chaudrieu I. Resilience and mental health. Clinical Psychology Review. 2010;30:479–495. doi: 10.1016/j.cpr.2010.03.003. [DOI] [PubMed] [Google Scholar]
- Denning LA, Meisnere M, Warner KE, editors. and the Committee on the Assessment of Resiliency and Prevention Programs for Mental and Behavioral Health in Service Members and Their Families, Institute of Medicine. Preventing psychological disorders in service members and their families: An assessment of programs. Washington, DC: National Academies Press; 2014. [PubMed] [Google Scholar]
- Dennissen JA, Asendorpf JB, van Aken MAG. Childhood personality predicts long-term trajectories of shyness and aggressiveness in the context of demographic transitions in emerging adulthood. Journal of Personality. 2008;76:67–100. doi: 10.1111/j.1467-6494.2007.00480.x. [DOI] [PubMed] [Google Scholar]
- Dretsch MN, Silverberg ND, Iverson GL. Multiple past concussions are associated with ongoing post-concussive symptoms but not cognitive impairment in active-duty army soldiers. Journal of Neurotrauma. 2015;32:1301–1306. doi: 10.1089/neu.2014.3810. [DOI] [PubMed] [Google Scholar]
- Efron B. Bootstrap confidence intervals: Good or bad. Psychological Bulletin. 1988;104:293–296. [Google Scholar]
- Efron B, Tibshirani R. An introduction to the bootstrap. New York: Chapman & Hall/CRC; 1993. [Google Scholar]
- Elliott T, Erosa NA. Psychological adjustment. In: Benyamini Y, Johnstone M, Karademas V, editors. Assessment in health psychology. Boston, MA: European Association in Psychological Assessment (EAPA) Book Series, Hogrefe Publishing; 2016. pp. 201–212. [Google Scholar]
- Elliott TR, Hsiao YY, Kimbrel N, Meyer E, DeBeer B, Gulliver S, Kwok OM, Morissette S. Resilience, traumatic brain injury, depression and posttraumatic stress among Iraq/Afghanistan war veterans. Rehabilitation Psychology. 2015;60:263–276. doi: 10.1037/rep0000050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher D, Sarkar M. Psychological resilience: A review and critique of definitions, concepts, and theory. European Psychologist. 2013;18:12–23. [Google Scholar]
- Forbes D, Creamer M, Biddle D. The validity of the PTSD checklist as a measure of symptomatic change in combat-related PTSD. Behaviour Research and Therapy. 2001;39:977–986. doi: 10.1016/s0005-7967(00)00084-x. [DOI] [PubMed] [Google Scholar]
- Fulton JJ, Calhoun PS, Wagner HR, Schry AR, Hair LP, Feeling N, Beckham JC. The prevalence of posttraumatic stress disorder in Operation Enduring Freedom/Operation Iraqi Freedom (OEF/OIF) Veterans: A meta-analysis. Journal of Anxiety Disorders. 2015;31:98–107. doi: 10.1016/j.janxdis.2015.02.003. [DOI] [PubMed] [Google Scholar]
- Gardner N, Sullivan KA, Lange RT. The relationship between personality characteristics and postconcussion symptoms in a nonclinical sample. Neuropsychology. 2010;24:168–175. doi: 10.1037/a0017431. [DOI] [PubMed] [Google Scholar]
- Green KT, Hayward LC, Williams AM, Dennis PA, Bryan BC, Calhoun PS. Examining the factor structure of the Connor-Davidson Resilience Scale (CD-RISC) in a post-9/11 U.S. military veteran sample. Assessment. 2014;21:443–451. doi: 10.1177/1073191114524014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosso JA, Kimbrel NA, Dolan S, Meyer EC, Kruse MI, Gulliver SB, Morissette SB. A test of whether coping styles moderate the effect of PTSD symptoms on alcohol outcomes. Journal of Traumatic Stress. 2014;27:478–482. doi: 10.1002/jts.21943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG, Bissett RT, Pistorello J, Toarmino D, McCurry SM. Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record. 2004;54:553–578. [Google Scholar]
- Hoge CW, Castro CA, Messer SC, McGurk D, Cotting DI, Koffman RL. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. New England Journal of Medicine. 2004;351:12–22. doi: 10.1056/NEJMoa040603. [DOI] [PubMed] [Google Scholar]
- Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, Castro CA. Mild traumatic brain injury in U.S. soldiers returning from Iraq. New England Journal of Medicine. 2008;358:453–463. doi: 10.1056/NEJMoa072972. [DOI] [PubMed] [Google Scholar]
- Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal. 1999;6(1):1–55. [Google Scholar]
- Kazis LE, Selim A, Rogers W, Ren XS, Lee A, Miller DR. Dissemination of methods and results from the Veterans Health Study: Final comments and implications for future monitoring strategies within and outside the veterans healthcare system. The Journal of Ambulatory Care Management. 2006;29:310–319. doi: 10.1097/00004479-200610000-00007. [DOI] [PubMed] [Google Scholar]
- Kennedy JE, Cooper DB, Reid MW, Tate DF, Lange RT. Profile analyses of the personality assessment inventory following military-related traumatic brain injury. Archives of Clinical Neuropsychology. 2015;30:236–247. doi: 10.1093/arclin/acv014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King LA, King DW, Vogt DS, Knight J, Samper RE. Deployment Risk and Resilience Inventory: A collection of measures for studying deployment-related experiences of military personnel and veterans. Military Psychology. 2006;18:89–120. [Google Scholar]
- Kinnunen M, Metsapelto R, Feldt T, Kokko K, Tolvanen A, Pulkkinen L. Personality profiles and health: Longitudinal evidence among Finnish adults. Scandinavian Journal of Psychology. 2012;53:512–522. doi: 10.1111/j.1467-9450.2012.00969.x. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2. New York: Guilford; 2005. [Google Scholar]
- Kruse MI. Individual differences in subjective responses to alcohol: Associated factors and alternative assessment strategies (Unpublished doctoral dissertation) University of Texas; 2008. [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–174. [PubMed] [Google Scholar]
- Lange RT, Brickell TA, Kennedy JE, Bailie JM, Sills C, Asumussen S, French LM. Factors influencing postconcussion and posttraumatic stress symptom reporting following military-related concurrent polytrauma and traumatic brain injury. Archives of Clinical Neuropsychology. 2014;29:329–347. doi: 10.1093/arclin/acu013. [DOI] [PubMed] [Google Scholar]
- Lee JEC, Garber B, Zamorski MA. Prospective analysis of premilitary mental health, somatic symptoms, and postdeployment postconcussive symptoms. Psychosomatic Medicine. 2015;77:1006–1017. doi: 10.1097/PSY.0000000000000250. [DOI] [PubMed] [Google Scholar]
- Losoi H, Silverberg ND, Waljas M, Turunen S, Rosti-Otajavi, Iverson GL. Resilience is associated with outcome from mild traumatic brain injury. Journal of Neurotrauma. 2015;32:942–949. doi: 10.1089/neu.2014.3799. [DOI] [PubMed] [Google Scholar]
- McCauley SR, Wilde EA, Miller ER, Frisby ML, Garza HM, McCarthy JJ. Preinjury resilience and mood as predictors of early outcome following mild traumatic brain injury. Journal of Neurotrauma. 2013;30:642–652. doi: 10.1089/neu.2012.2393. [DOI] [PubMed] [Google Scholar]
- Merritt VC, Lange RT, French LM. Resilience and symptom reporting following mild traumatic brain injury in military service members. Brain Injury. 2015;29:1325–1336. doi: 10.3109/02699052.2015.1043948. [DOI] [PubMed] [Google Scholar]
- Meyer EC, Morissette SB, Kimbrel NA, Kruse MI, Gulliver SB. Acceptance and Action Questionnaire-II scores as a predictor of posttraumatic stress disorder symptoms among war Veterans. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:521–528. [Google Scholar]
- Miskey HM, Shura RD, Yoash-Gantz RE, Rowland JA. Personality Assessment Inventory profiles of veterans: Differential effects of mild traumatic brain injury and psychopathology. Brain Imaging and Behavior. 2015;9:461–471. doi: 10.1007/s11682-015-9391-7. [DOI] [PubMed] [Google Scholar]
- Morissette SB, Woodward M, Kimbrel NA, Meyer EC, Kruse MI, Dolan S, Gulliver SB. Deployment-related TBI, persistent postconcussive symptoms, PTSD, and depression in OEF/OIF veterans. Rehabilitation Psychology. 2011;56:340–350. doi: 10.1037/a0025462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 7. Los Angeles, CA: Muthén & Muthén; 1998–2013. [Google Scholar]
- Ong AD, Bergeman CS, Boker SM. Resilience comes of age: Defining features in later adulthood. Journal of Personality. 2009;77(6):1777–1804. doi: 10.1111/j.1467-6494.2009.00600.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ong AD, Zautra AJ, Reid MC. Psychological resilience predicts decreases in pain catastrophizing through positive emotions. Psychology and Aging. 2010;25:516–523. doi: 10.1037/a0019384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panayiotou A, Jackson M, Crowe SF. A meta-analytic review of the emotional symptoms associated mild traumatic brain injury. Journal of Clinical and Experimental Neuropsychology. 2010;32:463–473. doi: 10.1080/13803390903164371. [DOI] [PubMed] [Google Scholar]
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief from of the multidimensional personality questionnaire. Psychological Assessment. 2002;14:150–163. doi: 10.1037//1040-3590.14.2.150. [DOI] [PubMed] [Google Scholar]
- Polusny MA, Kehle SM, Nelson NW, Erbes C, Arbisi PA, Thuras P. Longitudinal effects of mild traumatic brain injury and posttraumatic stress disorder comorbidity on postdeployment outcomes in National Guard soldiers deployed to Iraq. Archives of General Psychiatry. 2011;68:79–89. doi: 10.1001/archgenpsychiatry.2010.172. [DOI] [PubMed] [Google Scholar]
- Robins RW, John OP, Caspi A, Moffitt TE, Stouthamer-Loeber M. Resilient, overcontrolled, and undercontrolled boys: Three replicable personality types. Journal of Personality and Social Psychology. 1996;70:157–171. doi: 10.1037//0022-3514.70.1.157. [DOI] [PubMed] [Google Scholar]
- Schwab KA, Ivins B, Cramer G, Johnson W, Sluss-Tiller M, Kiley K, Warden D. Screening for traumatic brain injury in troops returning from deployment in Afghanistan and Iraq: Initial investigation of the usefulness of a short screening tool for traumatic brain injury. Journal of Head Trauma Rehabilitation. 2007;22:377–389. doi: 10.1097/01.HTR.0000300233.98242.87. [DOI] [PubMed] [Google Scholar]
- Seal KH, Bertenthal D, Miner CR, Sen S, Marmar C. Bringing the war back home: Mental health disorders among 103,788 US veterans returning from Iraq and Afghanistan seen at Department of Veterans Affairs facilities. Archives of Internal Medicine. 2007;167:476–482. doi: 10.1001/archinte.167.5.476. [DOI] [PubMed] [Google Scholar]
- Steca P, Alessandri G, Caprara GV. The utility of a well-known personality typology in studying successful aging: Resilients, undercontrollers, and overcontrollers in old age. Personality and Individual Differences. 2010;48:442–446. [Google Scholar]
- Steenkamp MM, Nash WP, Litz BT. Post-traumatic stress disorder: review of the Comprehensive Soldier Fitness program. American Journal of Preventive Medicine. 2013;44:507–12. doi: 10.1016/j.amepre.2013.01.013. [DOI] [PubMed] [Google Scholar]
- Sullivan KA, Edmed SL, Allan AC, Smith SS, Karlsson LJ. The role of psychological resilience and mtbi as predictors of postconcussional syndrome symptomatology. Rehabilitation Psychology. 2015;60:147–154. doi: 10.1037/rep0000037. [DOI] [PubMed] [Google Scholar]
- Sumpter RE, McMillian TM. Errors in self-report of post-traumatic stress disorder after severe traumatic brain injury. Brain Injury. 2006;20:93–99. doi: 10.1080/02699050500394090. [DOI] [PubMed] [Google Scholar]
- Telch MJ, Smith NB. Unpublished measure. Department of Psychology, the University of Texas; Austin: 2016. The Distress Tolerance Inventory. [Google Scholar]
- Tsai J, Harpaz-Rotem I, Pietrazk RH, Southwick SM. The role of coping, resilience, and social support in mediating the relation between PTSD and social functioning in veterans returning from Iraq and Afghanistan. Psychiatry. 2012;75:135–149. doi: 10.1521/psyc.2012.75.2.135. [DOI] [PubMed] [Google Scholar]
- Vanderploeg RD, Belanger HG, Horner RD, Spehar AM, Powell-Cope G, Luther SL, Scott SG. Health outcomes associated with military deployment: Mild traumatic brain injury, blast, trauma, and combat associations in the Florida National Guard. Archives of Physical Medicine and Rehabilitation. 2012;93:1887–1895. doi: 10.1016/j.apmr.2012.05.024. [DOI] [PubMed] [Google Scholar]
- Vogt DS, Proctor SP, King DW, King LA, Vasterling JJ. Validation of scales from the Deployment Risk and Resilience Inventory in a sample of Operation Iraqi Freedom veterans. Assessment. 2008;15:391–402. doi: 10.1177/1073191108316030. [DOI] [PubMed] [Google Scholar]
- Walker SN, Sechrist KR, Pender NJ. The health-promoting lifestyle profile II. Omaha: University of Nebraska Medical Center, College of Nursing; 1995. [Google Scholar]
- Walsh M, Armstrong T, Poritz J, Elliott TR, Jackson WT, Ryan T. Resilience, pain interference and upper-limb loss: Testing the mediating effects of positive emotion and activity restriction on distress. Archives of Physical Medicine and Rehabilitation. 2016;97:781–787. doi: 10.1016/j.apmr.2016.01.016. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist: Reliability, validity, and diagnostic utility. Paper presented at the Annual Meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- Weston R, Chan F, Gore PA, Jr, Catalano D. An introduction to using structural equation models in rehabilitation psychology. Rehabilitation Psychology. 2008;53:340–356. [Google Scholar]
- Wilk JE, Herrell RK, Wynn GH, Riviere LA, Hoge CW. Mild traumatic brain injury (concussion), posttraumatic stress disorder, and depression in U.S. soldiers involved in combat deployments: Association with postdeployment symptoms. Psychosomatic Medicine. 2012;74:249–257. doi: 10.1097/PSY.0b013e318244c604. [DOI] [PubMed] [Google Scholar]
- Windle G, Bennett KM, Noyes J. A methodological review of resilience measurement scales. Health and Quality of Life Outcomes. 2011;9:8. doi: 10.1186/1477-7525-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu C. Evaluating cutoff criteria of model fit indices for latent variable models with binary and continuous outcome (Unpublished doctoral dissertation) University of California; 2002. [Google Scholar]