Abstract
Some recent studies have suggested that the use of dipeptidyl peptidase-4 inhibitors (DPP4i) is associated with cancer development. However, some other studies suggest no such association. The aim of the present study was to evaluate the effect of DPP4i on the risk of developing cancers. The electronic databases PubMed, Medline, EMBASE, Web of Science and Cochrane Library and the clinical trial registry were searched for published and unpublished randomized clinical trials on humans. Eligible studies were RCTs conducted in patients with type 2 diabetes mellitus, comparing DPP4i with a placebo or other active drugs. A total of 72 trials with 35,768 and 33,319 patients enrolled for DPP4i and the comparison drugs, respectively. Overall, no significant associations were detected between the use of DPP4i and cancer development, in comparison with the use of other active drugs or placebo. The results were consistent across pre-defined subgroups stratified by type of DPP4i, type of cancer, drug for comparison, trial duration, or baseline characteristics. The results of this meta-analysis suggest that patients with type 2 diabetes treated with DPP4i do not have a higher risk of developing cancers than patients treated with a placebo or other drugs.
Introduction
Diabetes is one of the serious public health problems of the 21st century. The International Diabetes Federation estimated that the number of people with diabetes was 415 million, and it will reach 642 million by 20401. In high-income countries, approximately 87% to 91% of all people with diabetes have type 2 diabetes2–5. Glucagon-like peptide-1 (GLP-1) and glucose-dependent insulinotropic polypeptide, also called gastric inhibitory polypeptide (GIP), are the two main physiological incretins synthesized in the intestinal tract and play an important role in the regulation of blood glucose6. GLP-1 inhibits the release of glucagon, reduces postprandial hepatic glucose generation and delays gastric emptying, which results in decreased postprandial glucose absorption7. Because these incretins are rapidly degraded by the enzyme dipeptidyl peptidase 4, their half-lives are short (GLP-1 1–2 minutes, GIP 7 minutes)8. Oral dipeptidyl peptidase-4 inhibitors (DPP4i), which reduce the release of GLP-1 and extend its half-life, have become relatively new incretin-based agents for treating type 2 diabetes9. Presently, there are over 10 DPP4i approved for clinical use, with several of them extensively studied, including data regarding malignancy outcomes, namely, sitagliptin, vildagliptin, saxagliptin, linagliptin and alogliptin, and they are currently recommended by international and national guidelines worldwide.
However, the long-term effect of DPP4i for the treatment of type 2 diabetes has been debated. Because the major complication in patients with type 2 diabetes is cardiovascular disease, the focus of many studies was to evaluate the cardiovascular safety of DPP4i or whether DPP4i could lower cardiovascular risk10–12. In addition, the association between DPP4i and cancer has been studied by many researchers. An analysis based on the US Food and Drug Administration (FDA) adverse event reporting system (AERS) database reported increased rates of pancreatic cancer with the use of sitagliptin compared with other anti-diabetes drugs. The reported event rate for pancreatic cancer was 2.7 times higher with sitiagliptin than other therapies (p = 0.008)13. Type 2 diabetes is an independent risk factor of colon cancer14, but whether DPP4i therapy affects the development of colon cancer has not been well investigated. Two large multicenter randomized controlled trials (RCTs), Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus-Thrombolysis in Myocardial Infarction 53 (SAVOR-TIMI 53) and Trial Evaluating Cardiovascular Outcomes with Sitagliptin (TECOS), were conducted to assess the cardiovascular safety of saxagliptin and sitagliptin, respectively11,12. The results of the two trials indicated that there was no significant increase in the risk of pancreatic cancer. Interestingly, a protective effect of saxagliptin against colon cancer was found in the SAVOR-TIMI 53 trial (hazard ratio = 0.51, 95% CI = 0.27–0.92, p = 0.026)15.
There have been many RCTs to assess the efficacy and safety of DPP4i in diabetic patients. A meta-analysis conducted by Monami et al.16 had evaluated the effect of DPP4i on the developing pancreatic cancer in 2014. However, currently no published meta-analysis on the association between DPP4i and the risk of other types of cancers in patients with type 2 diabetes was reported. Given that previous published meta-analyses may not extract data from those completed and private RCTs, besides, some new clinical trials were published recently. Therefore, the purpose of this meta-analysis of RCTs was to systematically and comprehensively evaluate the effect of DPP4i use on the risk of developing cancers.
Results
Study Search
A total of 536 studies were identified through a search of the electronic databases and the www.clinicaltrials.gov website. After excluding duplicate publications, 445 studies remained. After the titles and abstracts were reviewed, 73 studies were excluded because they were systematic reviews or not human studies, leaving 372 studies for full text evaluation. Among them, 300 studies were excluded because of the following reasons: 8 studies were not randomized trials, 265 studies did not report cancer outcomes, in 5 studies the drugs for comparison were also DPP4i, 11 studies had a duration shorter than 24 weeks, and 11 studies reported on the website were published in the electronic databases, given the quality score of the studies, we excluded those studies both in the literature and in the registry from the trial registry. As a result, 72 RCTs, including 13 from electronic database and 59 from the trial registry were selected in the final meta-analysis. The details of the study search flow were shown in Fig. 1.
Figure 1.

Flowchart of study selection process. DPP-4: dipeptidyl peptidase-4.
Study Characteristics
Table 1 summarizes the study characteristics of the 72 trials totaling 69,087 patients, with 35,768 received various DPP4i (sitagliptin, saxagliptin, alogliptin and linagliptin) and 33,319 received other active anti-diabetic drugs or placebo11,17–29. The DPP4i tested were sitagliptin in 38 trials, saxagliptin in 13, alogliptin in 10, and linagliptin in 11. The adverse events of cancers were classified into 10 types based on the location of the cancer: 80 studies included reproductive system cancers, 89 included digestive system cancers, 30 included integumentary system cancers, 32 included urinary system cancers, 13 included hematologic system cancers, 23 included respiratory system cancers, 5 included motor system cancers, 17 included endocrine system cancers, 2 included nervous system cancers and 2 included cardiovascular system cancers. The mean age of the included patients ranged from 49.7 to 74.9 years. The sample sizes of individual trials were between 21 and 16492 patients and the duration of trial ranged from 24 weeks to 5 years. Among all of the patients included, the mean HbA1c was 8.0 ± 1.5%, mean BMI was 29.9 ± 2.3 kg/m2 and mean duration of diabetes was 6.9 ± 3.7 years.
Table 1.
Characteristics of included randomized controlled trials.
| Study | NCT code | Comparison drug(s) | No. of patients | Trial duration (weeks) | Males/Females | Mean Age (years) | HbA1c (%) | BMI (kg/m2) | DM duration (years) | Cancer type | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| DPP-4i | Control | ||||||||||
| Sitagliptin | |||||||||||
| NCT01590771 | NCT01590771 | Placebo | 249 | 249 | 24 | 249/249 | 57 | 8.55 | NA | NA | Cervix carcinoma |
| NCT01189890 | NCT01189890 | Glimepiride | 241 | 239 | 30 | 202/278 | 70.7 | 7.78 | 29.7 | 8.69 | Colon cancer, Malignant melanoma, Prostate cancer |
| NCT01076088 | NCT01076088 | Placebo | 120 | 127 | 24 | 161/86 | 52.7 | 8.86 | 25.7 | 1.1 | Renal cancer |
| NCT00420511 | NCT00420511 | Placebo | 10 | 11 | 48 | 14/7 | 60.9 | 6.1 | 32.7 | 3 | Renal cancer |
| NCT01076075 | NCT01076075 | Placebo/Pioglitazone | 210 | 212 | 24 | 193/229 | 54.9 | 8.4 | 28.5 | 7.75 | Prostate cancer |
| Arjona 2013 | NCT00509262 | Glipizide | 210 | 212 | 54 | 170/252 | 64.2 | 7.8 | 26.76 | 10.4 | Breast cancer, Leukemia, Lung cancer, Pancreatic cancer |
| Green 2015 | NCT00790205 | Placebo | 7332 | 7339 | 5 years | 10374/4297 | 65.5 | 7.2 | 30.2 | 11.6 | Gastric cancer, Colon cancer, Salivary gland neoplasm, Cervix carcinoma, Bladder cancer, Bone cancer, Breast cancer, Pancreatic cancer, Prostate cancer, Rectal cancer, Renal cancer, Bronchial carcinoma, Lung cancer, Thyroid cancer, Ovarian cancer, Endometrial cancer, Gallbladder cancer, Hepatic cancer, Bile duct cancer, Laryngeal cancer, Anal cancer, Leukemia, Lymphoma, Lip carcinoma |
| NCT00885352 | NCT00885352 | Placebo | 157 | 156 | 26 | 195/118 | 56 | 8.8 | 29.9 | 9.8 | Basal cell carcinoma |
| NCT00509236 | NCT00509236 | Glipizide | 64 | 65 | 54 | 77/52 | 59.5 | 7.8 | 26.8 | 17.5 | Prostate cancer |
| NCT00095056 | NCT00095056 | Placebo | 65 | 26 | 54 | 47/44 | 67.9 | 7.7 | 26.6 | 13.5 | Colon cancer, Pancreatic cancer, Prostate cancer, Skin cancer |
| NCT00395343 | NCT00395343 | Placebo | 322 | 319 | 24 | 326/315 | 57.8 | 8.7 | 31 | 12.5 | Breast cancer, Rectal cancer |
| NCT00722371 | NCT00722371 | Pioglitazone | 231 | 230 | 54 | 249/212 | 52.03 | 8.8 | 31.3 | 4.1 | Bladder cancer, Breast cancer, Malignant melanoma, Skin cancer |
| NCT00337610 | NCT00337610 | Placebo | 96 | 94 | 30 | 88/102 | 54.8 | 9.2 | 30.2 | NA | Pancreatic cancer, Colon cancer, Lymphoma |
| NCT01177384 | NCT01177384 | Placebo | 191 | 189 | 24 | 194/186 | 57.1 | 8.08 | NA | NA | Breast cancer, Thymoma |
| NCT00305604 | NCT00305604 | Placebo | 102 | 104 | 24 | 97/109 | 71.9 | 7.8 | 30.95 | 7.1 | Basal cell carcinoma, Colon cancer, Malignant melanoma, Skin cancer |
| NCT00701090 | NCT00701090 | Glimepiride | 516 | 519 | 30 | 563/472 | 56.3 | 7.5 | 30 | 6.8 | Basal cell carcinoma, Lung cancer, Pancreatic cancer |
| NCT00449930 | NCT00449930 | Metformin | 528 | 522 | 24 | 484/566 | 56 | 7.3 | 30.8 | 2.4 | Lung cancer, Malignant melanoma |
| NCT00637273 | NCT00637273 | Pioglitazone | 166 | 165 | 26 | 165/166 | 52.6 | 8.5 | 32 | 5.5 | Thyroid cancer |
| NCT01137812 | NCT01137812 | Canagliflozin | 378 | 377 | 52 | 422/333 | 56.5 | 8.1 | 31.6 | 9.6 | Cervix carcinoma, Lung cancer, Oesophageal cancer, Uterine cancer |
| NCT01098539 | NCT01098539 | Albiglutide | 246 | 249 | 52 | 266/229 | 63.3 | NA | NA | NA | Brain cancer, Breast cancer, Malignant melanoma, Prostate cancer, Renal cancer |
| Aschner 2012 | NCT00751114 | Insulin glargine | 253 | 227 | 24 | 246/234 | 53.6 | 8.5 | 31.09 | 4.5 | Prostate cancer |
| NCT00106704 | NCT00106704 | Placebo/Pioglitazone | 222 | 219 | 54 | 234/207 | 56 | 8.34 | 31 | 8.8 | Lung cancer, Skin cancer |
| NCT00881530 | NCT00881530 | Metformin | 56 | 56 | 78 | 57/55 | 57.55 | 8.09 | 29.3 | NA | Breast cancer, Cervix carcinoma |
| NCT00482729 | NCT00482729 | Metformin | 625 | 621 | 44 | 709/537 | 49.7 | 9.87 | 33.3 | 3.3 | Colon cancer, Endometrial cancer, Laryngeal cancer, Lung cancer, Malignant melanoma, Renal cancer, Ovarian cancer, Prostate cancer |
| NCT00086502 | NCT00086502 | Placebo | 175 | 178 | 24 | 196/157 | 56.2 | 8 | 31.5 | 6.1 | Lung cancer |
| NCT00532935 | NCT00532935 | Pioglitazone | 261 | 256 | 32 | 277/240 | 52.3 | 8.9 | 29.8 | 3.3 | Basal cell carcinoma, Colon cancer, Renal cancer |
| NCT01046110 | NCT01046110 | Insulin degludec | 222 | 225 | 26 | 262/185 | 55.7 | 8.9 | NA | NA | Bladder cancer |
| NCT02008682 | NCT02008682 | Liraglutide | 184 | 183 | 26 | 219/148 | 51.5 | 8.12 | 27.24 | 5.27 | Thyroid cancer,Thymoma |
| Ahren 2014 | NCT00838903 | Placebo/Metformin | 302 | 101 | 104 | 189/214 | 54.8 | 8.1 | 32.6 | 6 | Thyroid cancer, Breast cancer, Lung cancer, Malignant melanoma, Prostate cancer, Rectal cancer, Renal cancer |
| NCT00094770 | NCT00094770 | Glipizide | 588 | 584 | 104 | 694/478 | 56.7 | 7.7 | 31.2 | 6.35 | Basal cell carcinoma, Bladder cancer, Breast cancer, Colon cancer, Lymphoma, Gastric cancer, Hepatic cancer, Malignant melanoma, Bone cancer, Oesophageal cancer, Prostate cancer, Rectal cancer, Renal cancer, Skin cancer, Uterine cancer |
| Pratley 2012 | NCT00700817 | Liraglutide | 219 | 221 | 52 | 236/204 | 55 | 8.4 | 32.9 | 6.4 | Pancreatic cancer, Renal cancer, Bile duct cancer, Breast cancer, Colon cancer |
| NCT00289848 | NCT00289848 | Placebo | 352 | 178 | 28 | 306/224 | 50.9 | 8.74 | 25 | 2 | Ovarian cancer |
| NCT00813995 | NCT00813995 | Placebo | 197 | 198 | 24 | 200/195 | 54.6 | 8.5 | 25.3 | 6.85 | Colon cancer, Lip carcinoma |
| NCT00094757 | NCT00094757 | Placebo/Pioglitazone | 205 | 110 | 54 | 179/136 | 54.85 | 8 | 32 | 4.6 | Breast cancer, Bone cancer, Pancreatic cancer, Thyroid cancer, Uterine cancer |
| NCT01519674 | NCT01519674 | Metformin | 195 | 194 | 24 | 205/184 | 55.84 | 8.4 | 29.4 | NA | Pancreatic cancer, Thyroid cancer |
| NCT00086515 | NCT00086515 | Placebo/Glipizide | 464 | 237 | 104 | 400/301 | 54.5 | 8 | NA | 6.2 | Lymphoma, Basal cell carcinoma, Bladder cancer, Breast cancer, Renal cancer, Thyroid cancer, Hepatic cancer, Lung cancer, Ovarian cancer, Pancreatic cancer, Thyroid cancer, Skin cancer |
| NCT01907854 | NCT01907854 | Liraglutide | 204 | 202 | 27 | 242/164 | 56.4 | 8.3 | NA | NA | Bladder cancer |
| Weinstock 2015 | NCT00734474 | Dulaglutide | 315 | 304 | 104 | 297/322 | 53.7 | 8.1 | 31.21 | 7.1 | Breast cancer, Colon cancer, Gastric cancer, Laryngeal cancer, Prostate cancer,Thyroid cancer, Uterine cancer |
| Saxagliptin | |||||||||||
| NCT00327015 | NCT00327015 | Metformin | 335 | 328 | 24 | 332/331 | 51.96 | 9.5 | 30.2 | 1.7 | Pancreatic cancer |
| NCT00121641 | NCT00121641 | Placebo | 106 | 95 | 24 | 101/100 | 53.91 | 7.95 | 31.65 | 2.41 | Colon cancer, Cervix carcinoma, Malignant melanoma, Renal cancer |
| NCT00316082 | NCT00316082 | Placebo | 71 | 74 | 24 | 72/73 | 54.9 | NA | NA | NA | Uterine cancer, Pancreatic cancer, Hepatic cancer |
| NCT00121667 | NCT00121667 | Placebo/Metformin | 191 | 179 | 24 | 199/171 | 54.72 | 8.1 | 31.4 | 6.5 | Breast cancer, Uterine cancer |
| NCT00295633 | NCT00295633 | Placebo | 186 | 184 | 24 | 174/196 | 52.34 | 8.3 | 30.05 | 5.15 | Colon cancer |
| NCT00575588 | NCT00575588 | Glipizide | 428 | 430 | 104 | 444/414 | 57.55 | 7.7 | 31.4 | 5.4 | Bladder cancer, Colon cancer, Salivary gland neoplasm, Leukemia, Thyroid cancer, Bladder cancer, Bronchial carcinoma, Lung cancer, Malignant melanoma, Renal cancer, Breast cancer |
| NCT00757588 | NCT00757588 | Placebo/Insulin | 304 | 151 | 24 | 188/267 | 57.2 | 8.7 | 32.3 | 11.9 | Breast cancer, Pituitary tumor, Uterine cancer, Pancreatic cancer, Prostate cancer |
| NCT01128153 | NCT01128153 | Placebo | 129 | 128 | 24 | 154/103 | 57 | 8.28 | 29.2 | NA | Laryngeal cancer |
| Schernthaner 2015 | NCT01006603 | Glimepiride | 360 | 360 | 52 | 445/275 | 72.6 | 7.6 | 29.6 | 7.6 | Breast cancer, Basal cell carcinoma, Bladder cancer, Colon cancer, Hepatic cancer, Lung cancer, Pancreatic cancer, Prostate cancer, Salivary gland neoplasm |
| NCT00313313 | NCT00313313 | Placebo/Glyburide | 253 | 267 | 24 | 233/287 | 54.96 | 8.45 | 29 | 6.8 | Thyroid cancer |
| NCT01006590 | NCT01006590 | Metformin | 147 | 139 | 24 | 164/122 | 58.7 | 7.8 | 31.7 | 6.5 | Prostate cancer, Tongue cancer |
| Leiter 2016 | NCT01107886 | Placebo | 8280 | 8212 | 2.9 years | 11037/5455 | 65 | 8 | 31.1 | 10.3 | Thyroid cancer, Bladder cancer, Breast cancer, Bronchial carcinoma, Cervix carcinoma, Colon cancer,Gastric cancer, Hepatic cancer, Lung cancer, Lymphoma, Ovarian cancer, Prostate cancer, Pancreatic cancer, Oesophageal cancer, Endometrial cancer, Leukemia, Lymphoma, Laryngeal cancer, Skin cancer, Vascular neoplasm, Bile duct cancer, Gallbladder cancer, Hodgkin’s disease, Malignant melanoma, Testis cancer, Bone cancer, Lip carcinoma, Haemangioma, Brain cancer, Rectal cancer, Renal cancer, Uterine cancer |
| NCT00374907 | NCT00374907 | Placebo/Metformin | 20 | 16 | 116 | 14/22 | 55.5 | NA | 33.01 | NA | Colon cancer |
| Alogliptin | |||||||||||
| White 2013 | NCT00968708 | Placebo | 2701 | 2679 | 41 months | 3651/1738 | 61 | 7.2 | 28.7 | 7.2 | Colon cancer, Prostate cancer, Breast cancer, Bladder cancer, Gastric cancer, Renal cancer, Lung cancer |
| NCT00286468 | NCT00286468 | Placebo | 198 | 99 | 26 | 150/147 | 56.7 | 8.11 | 30 | 7.6 | Basal cell carcinoma, Bladder cancer |
| NCT00286442 | NCT00286442 | Placebo | 213 | 104 | 26 | 151/166 | 55.33 | 7.93 | 32 | 6 | Endometrial cancer, Prostate cancer |
| NCT00856284 | NCT00856284 | Glipizide | 878 | 869 | 104 | 881/866 | 55.4 | 7.61 | 31.2 | 5.45 | Breast cancer, Basal cell carcinoma, Colon cancer, Bladder cancer, Endometrial cancer,Lymphoma, Ovarian cancer, Renal cancer, Lung cancer |
| NCT00286429 | NCT00286429 | Placebo | 129 | 130 | 26 | 106/153 | 55.4 | 9.3 | 32.4 | 12.8 | Cervix carcinoma |
| NCT01263496 | NCT01263496 | Voglibose | 97 | 83 | 40 | 131/49 | NA | NA | NA | NA | Pancreatic cancer, Breast cancer |
| NCT00395512 | NCT00395512 | Pioglitazone | 164 | 163 | 26 | 166/161 | 52.1 | 8.78 | 31.47 | 3.14 | Colon cancer |
| NCT00707993 | NCT00707993 | Glipizide | 222 | 219 | 52 | 198/243 | 69.9 | NA | 29.79 | 6.1 | Breast cancer, Cervix carcinoma |
| NCT00432276 | NCT00432276 | Metformin | 404 | 399 | 52 | 414/389 | 55.1 | 8.15 | 31.55 | 7.16 | Colon cancer |
| Mita 2016 | NA | OAD | 172 | 169 | 2 years | 199/142 | 64.6 | 7.25 | 24.75 | 8.6 | Thyroid cancer, Prostate cancer, Cholangioma |
| Linagliptin | |||||||||||
| NCT01084005 | NCT01084005 | Placebo | 162 | 79 | 24 | 165/76 | 74.9 | 7.78 | 29.67 | NA | Lung cancer, Malignant melanoma, Prostate cancer |
| NCT01087502 | NCT01087502 | Placebo/Glimepiride | 113 | 122 | 52 | 149/86 | 66.6 | 8.05 | 32.09 | NA | Bladder cancer, Lung cancer, Basal cell carcinoma, Colon cancer, Prostate cancer |
| NCT01734785 | NCT01734785 | Placebo | 606 | 110 | 24 | NA | NA | NA | NA | NA | Colon cancer, Basal cell carcinoma, Bladder cancer |
| Bajaj 2014 | NCT00996658 | Placebo | 183 | 89 | 24 | 132/140 | 53.79 | 8.42 | 28.27 | NA | Colon cancer |
| NCT00954447 | NCT00954447 | Placebo | 631 | 630 | 52 | 658/603 | 60 | 8.3 | 31 | 8.3 | Bile duct cancer, Colon cancer, Gastric cancer, Hepatic cancer, Lung cancer, Ovarian cancer, Renal cancer, Uterine cancer |
| NCT00798161 | NCT00798161 | Placebo | 142 | 72 | 24 | 116/98 | 56.03 | 8.69 | 28.84 | NA | Breast cancer |
| Gallwitz 2012 | NCT00622284 | Glimepiride | 776 | 775 | 2 years | 933/618 | 59.8 | 7.7 | 30.25 | 5 | Breast cancer, Bronchial carcinoma, Colon cancer, Endometrial cancer, Laryngeal cancer, Hepatic cancer, Bone cancer, Ovarian cancer, Pancreatic cancer, Prostate cancer, Rectal cancer, Renal cancer, Lung cancer, Thyroid cancer, Vulval cancer |
| NCT01215097 | NCT01215097 | Placebo | 205 | 100 | 24 | 152/153 | 55.5 | 7.99 | 25.6 | NA | Gastric cancer |
| NCT00621140 | NCT00621140 | Placebo | 336 | 167 | 24 | 243/260 | 55.7 | 8 | 29.05 | NA | Breast cancer, Lymphoma |
| NCT00654381 | NCT00654381 | Placebo | 159 | 80 | 52 | 395/166 | 60 | NA | NA | NA | Gastric cancer, Prostate cancer |
| Barnett 2012 | NCT00740051 | Placebo/Glimepiride | 151 | 76 | 52 | 88/139 | 56.5 | 8.1 | 29.5 | NA | Colon cancer |
NA, not available; NCT: national clinical trial; DPP4i: dipeptidyl peptidase-4 inhibitors; OAD: oral antidiabetes drug (excluding other DPP-4 inhibitors, GLP-1 analogs, and insulin).
The quality assessment of the 72 RCTs is summarized in Table S1. Among these studies, 49 (68.06%) were conducted with appropriate randomization, allocation concealment, blinding and reporting, which met the Cochrane criteria risk of bias for low risk of bias. The remaining 23 studies (31.94%) studies had unclear risk of bias. All of the trials were funded by industrial companies except one, which was funded by Juntendo University Graduate School of Medicine18.
Effect of DPP4i on the risk of overall cancers
The pooled RRs and 95% CIs were calculated to assess the effect of DPP-4i on the overall risk of developing cancers using a fixed-effect model. No significant associations were detected between DPP4i and cancer, compared with active drugs or placebo (MH-RR = 1.01, 95% CI = 0.91–1.12, p = 0.885). No heterogeneity was observed among these studies (I 2 = 0.0%, p = 0.928) (Table 2, Fig. 2).
Table 2.
Meta-analysis results.
| Variables | No. of studies | Pooled Relative Risk | Model of meta-analysis | Heterogeneity test | ||
|---|---|---|---|---|---|---|
| RR (95% CI) | P Z | I 2 (%) | P H | |||
| Overall | 72 | 1.01 (0.91–1.12) | 0.89 | Fixed | 0.0 | 0.93 |
| Type of DPP-4 inhibitors | ||||||
| Sitagliptin | 38 | 1.03 (0.88–1.21) | 0.68 | Fixed | 0.0 | 0.79 |
| Saxagliptin | 13 | 0.96 (0.81–1.13) | 0.63 | Fixed | 0.0 | 0.81 |
| Alogliptin | 10 | 1.53 (0.93–2.53) | 0.10 | Fixed | 0.0 | 0.68 |
| Linagliptin | 11 | 0.84 (0.55–1.28) | 0.41 | Fixed | 0.0 | 0.70 |
| Type of cancers | ||||||
| Reproductive system | 80 | 0.87 (0.73–1.05) | 0.15 | Fixed | 0.0 | 1.00 |
| Cervix carcinoma | 8 | 1.38 (0.54–3.50) | 0.50 | Fixed | 0.0 | 0.75 |
| Prostate cancer | 22 | 0.89 (0.69–1.14) | 0.37 | Fixed | 0.0 | 0.97 |
| Breast cancer | 25 | 0.72 (0.50–1.06) | 0.09 | Fixed | 0.0 | 0.98 |
| Ovarian cancer | 8 | 1.06 (0.48–2.35) | 0.89 | Fixed | 0.0 | 0.87 |
| Endometrial cancer | 6 | 0.53 (0.22–1.28) | 0.16 | Fixed | 0.0 | 0.70 |
| Uterine cancer | 9 | 1.77 (0.77–4.04) | 0.18 | Fixed | 0.0 | 0.85 |
| Vulval cancer | 1 | 0.33 (0.01–8.16) | 0.50 | Fixed | — | — |
| Testis cancer | 1 | 0.33 (0.01–8.11) | 0.50 | Fixed | — | — |
| Digestive system | 89 | 0.93 (0.77–1.13) | 0.46 | Fixed | 0.0 | 1.00 |
| Colon cancer | 27 | 0.96 (0.71–1.31) | 0.81 | Fixed | 0.0 | 0.98 |
| Pancreatic cancer | 16 | 0.83 (0.51–1.35) | 0.46 | Fixed | 0.0 | 0.93 |
| Gastric cancer | 8 | 1.35 (0.76–2.40) | 0.30 | Fixed | 0.0 | 0.92 |
| Salivary gland neoplasm | 3 | 1.40 (0.28–7.10) | 0.68 | Fixed | 0.0 | 0.55 |
| Rectal cancer | 6 | 0.41 (0.18–0.95) | 0.04 | Fixed | 0.0 | 0.53 |
| Gallbladder cancer | 2 | 1.00 (0.14–7.06) | 1.00 | Fixed | 0.0 | 0.34 |
| Hepatic cancer | 8 | 1.02 (0.54–1.91) | 0.96 | Fixed | 0.0 | 0.85 |
| Bile duct cancer | 4 | 0.77 (0.28–2.12) | 0.61 | Fixed | 0.0 | 0.60 |
| Laryngeal cancer | 6 | 0.71 (0.28–1.81) | 0.47 | Fixed | 0.0 | 0.58 |
| Anal cancer | 1 | 0.20 (0.01–4.17) | 0.30 | Fixed | — | — |
| Lip carcinoma | 3 | 4.33 (0.74–25.54) | 0.11 | Fixed | 0.0 | 0.90 |
| Oesophageal cancer | 3 | 0.75 (0.17–3.33) | 0.70 | Fixed | 0.0 | 0.58 |
| Tongue cancer | 1 | 0.32 (0.01–7.68) | 0.48 | Fixed | — | — |
| Cholangioma | 1 | 2.95 (0.12–71.86) | 0.51 | Fixed | — | — |
| Integumentary system | 30 | 1.12 (0.75–1.67) | 0.58 | Fixed | 0.0 | 1.00 |
| Malignant melanoma | 12 | 0.87 (0.48–1.59) | 0.66 | Fixed | 0.0 | 0.90 |
| Basal cell carcinoma | 11 | 0.95 (0.42–2.12) | 0.90 | Fixed | 0.0 | 0.60 |
| Skin cancer | 7 | 1.79 (0.86–3.71) | 0.12 | Fixed | 0.0 | 1.00 |
| Urinary system | 32 | 1.22 (0.92–1.61) | 0.16 | Fixed | 0.0 | 0.98 |
| Renal cancer | 17 | 1.38 (0.89–2.13) | 0.15 | Fixed | 0.0 | 0.96 |
| Bladder cancer | 15 | 1.12 (0.77–1.61) | 0.56 | Fixed | 0.0 | 0.80 |
| Hematologic system | 13 | 1.05 (0.65–1.68) | 0.85 | Fixed | 0.0 | 0.92 |
| Leukemia | 4 | 0.93 (0.45–1.93) | 0.85 | Fixed | 0.0 | 0.74 |
| Lymphoma | 8 | 1.29 (0.67–2.49) | 0.45 | Fixed | 0.0 | 0.88 |
| Hodgkin’s disease | 1 | 0.20 (0.01–4.13) | 0.30 | Fixed | — | — |
| Respiratory system | 23 | 1.08 (0.82–1.41) | 0.61 | Fixed | 0.0 | 0.91 |
| Lung cancer | 19 | 1.00 (0.76–1.33) | 0.98 | Fixed | 0.0 | 0.95 |
| Bronchial carcinoma | 4 | 2.55 (0.86–7.59) | 0.09 | Fixed | 0.0 | 0.55 |
| Motor system | 5 | 1.68 (0.57–5.01) | 0.35 | Fixed | 0.0 | 0.64 |
| Bone cancer | 5 | 1.68 (0.57–5.01) | 0.35 | Fixed | 0.0 | 0.64 |
| Endocrine system | 17 | 0.78 (0.43–1.41) | 0.41 | Fixed | 0.0 | 0.91 |
| Thyroid cancer | 14 | 0.73 (0.38–1.40) | 0.35 | Fixed | 0.0 | 0.91 |
| Thymoma | 2 | 2.98 (0.31–28.48) | 0.34 | Fixed | 0.0 | 0.91 |
| Pituitary tumor | 1 | 0.17 (0.01–4.05) | 0.27 | Fixed | — | — |
| Nervous system | 2 | 3.01 (0.31–28.84) | 0.34 | Fixed | 0.0 | 0.99 |
| Brain cancer | 2 | 3.01 (0.31–28.84) | 0.34 | Fixed | 0.0 | 0.99 |
| Cardiovascular system | 2 | 0.99 (0.14–7.04) | 0.99 | Fixed | 0.0 | 0.34 |
| Vascular neoplasm | 1 | 2.98 (0.12–73.03) | 0.50 | Fixed | — | — |
| Haemangioma | 1 | 0.33 (0.01–8.11) | 0.50 | Fixed | — | — |
| Type of comparators | ||||||
| Placebo | 30 | 0.98 (0.87–1.11) | 0.79 | Fixed | 0.0 | 0.89 |
| Sulfonylureas | 14 | 1.40 (0.99–1.96) | 0.05 | Fixed | 13.6 | 0.31 |
| Thiazolidinediones | 7 | 0.60 (0.27–1.33) | 0.21 | Fixed | 11.6 | 0.34 |
| Metformin | 10 | 1.14 (0.57–2.28) | 0.72 | Fixed | 0.0 | 1.00 |
| SGLT inhibitors | 1 | 0.33 (0.04–3.18) | 0.34 | Fixed | — | — |
| GLP-1 RAs | 5 | 0.85 (0.39–1.83) | 0.68 | Fixed | 6.3 | 0.37 |
| Other antidiabetic agents | 5 | 0.88 (0.32–2.42) | 0.80 | Fixed | 0.0 | 0.77 |
| Trial duration | ||||||
| Less than 52 weeks | 44 | 1.32 (0.93–1.89) | 0.12 | Fixed | 0.0 | 0.98 |
| 52 weeks or more | 28 | 0.98 (0.88–1.10) | 0.73 | Fixed | 0.0 | 0.49 |
| Mean age | ||||||
| Less than 60 years | 54 | 1.10 (0.85–1.40) | 0.49 | Fixed | 0.0 | 0.97 |
| 60 years or more | 16 | 0.99 (0.88–1.12) | 0.89 | Fixed | 17.8 | 0.25 |
| Mean HbA1c | ||||||
| Less than 8% | 21 | 1.06 (0.91–1.24) | 0.43 | Fixed | 0.0 | 0.49 |
| 8% or more | 44 | 0.94 (0.81–1.10) | 0.45 | Fixed | 0.0 | 0.95 |
| Mean BMI | ||||||
| Less than 30 kg/m2 | 25 | 1.28 (0.88–1.86) | 0.20 | Fixed | 0.0 | 0.80 |
| 30 kg/m2 or more | 37 | 0.97 (0.86–1.10) | 0.58 | Fixed | 0.0 | 0.87 |
| Mean diabetes duration | ||||||
| Less than 8 years | 37 | 1.23 (0.96–1.58) | 0.10 | Fixed | 0.0 | 0.80 |
| 8 years or more | 14 | 0.97 (0.86–1.10) | 0.61 | Fixed | 0.0 | 0.66 |
SGLT: sodium-glucose co-transporter; GLP-1 RAs: glucagon-like peptidase-1 receptor agonists.
Figure 2.
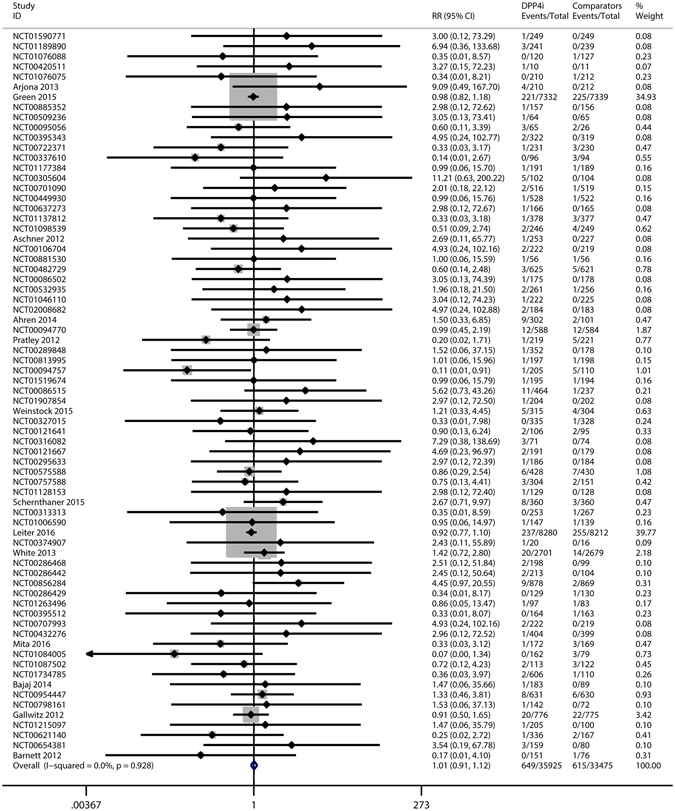
Risk of cancers in patients with type 2 diabetes who were treated with DPP-4 inhibitors versus other drugs. DPP4i: dipeptidyl peptidase-4 inhibitors.
Subgroup analysis
Subgroup analysis was performed to determine whether the type of DPP4i, cancer subtype, drug for comparison, trial duration, or the baseline characteristics (age, HbA1c, BMI, or diabetes duration) had an effect on the RR of cancers with DPP4i (Table 2, Fig. 3).
Figure 3.

Overall and subgroup meta-analysis of DPP-4 inhibitors on risk of cancers.
Effect of individual DPP4i on the risk of cancers
The risk of cancers (MH-RR) with individual DPP4i was 1.03 (95% CI = 0.88–1.21, p = 0.679) for sitagliptin (N = 38 trials), 0.96 (95% CI = 0.81–1.13, p = 0.627) for saxagliptin (N = 13 trials), 1.53 (95% CI = 0.93–2.53, p = 0.095) for alogliptin (N = 10 trials) and 0.84 (95% CI = 0.55–1.28, p = 0.410) for linagliptin (N = 11 trials). There was no statistically significant association between the risk of cancers and any of the individual DPP4i, with insignificant heterogeneity detected across these studies.
Effect of DPP4i on the risk of individual cancers
We next preformed a subgroup analysis according to the different types of cancers.
A total of eighty studies examined the association between DPP4i and the risk of reproductive system cancers. The MH-RR of the reproductive system cancer risk with DPP4i was 0.87 (95% CI = 0.73–1.05, p = 0.152). Among all of the reproductive system cancers, prostate cancer and breast cancer were reported more frequently, 0.89 (95% CI = 0.69–1.14, p = 0.365) and 0.72 (95% CI = 0.50–1.06, p = 0.094), respectively. Eighty-nine studies assessed the association between DPP4i and the risk of digestive system cancers. The MH-RR of the digestive system cancer risk with DPP4i was 0.93 (95% CI = 0.77–1.13, p = 0.464). The result showed no significant association between DPP4i and colon cancer or pancreatic cancer risk (MH-RR = 0.96, 95% CI = 0.71–1.31; MH-RR = 0.83, 95% CI = 0.51–1.35, respectively). Analysis of twelve studies indicated that DPP4i were not associated with a significantly increased risk of developing malignant melanoma (MH-RR = 0.87, 95% CI = 0.48–1.59, p = 0.655). In addition, there were seventeen, fifteen, nineteen and fourteen studies on renal, bladder, lung and thyroid cancers, respectively. The results of MH-RR all showed that DPP4i were not associated with these cancers.
Effect of type of comparison drug, trial duration and baseline characteristics on the risk of cancers
We performed analyses based on different types of comparison drugs, including placebo, sulfonylureas, thiazolidinediones, metformin, SGLT inhibitors, GLP-1 RAs and other antidiabetic agents. Among the studies, 30 used a placebo, 14 used sulfonylureas and 10 used metformin. There were no differences in the risk of cancers between DPP4i and any of these three comparison drugs (MH-RR = 0.98, 95% CI = 0.87–1.11, p = 0.789; MH-RR = 1.40, 95% CI = 0.99–1.96, p = 0.053; MH-RR = 1.14, 95% CI = 0.57–2.28, p = 0.718, respectively). Then we conducted a subgroup analysis stratified according to the duration of treatment. For a duration of less than 52 weeks, with 44 studies, no statistically significant difference was observed between patients in the DPP4i and comparison drug groups (MH-RR = 1.32, 95% CI = 0.93–1.89, p = 0.124). No significantly increased risk of digestive system cancers was observed for a duration of 52 weeks or more (MH-RR = 0.98, 95% CI = 0.88–1.10, p = 0.731). Moreover, subgroup analyses based on baseline characteristics were performed. Similarly, we found no significant differences in adverse events of cancers among studies with different mean age, mean HbA1c, mean BMI or mean diabetes duration.
Sensitivity analysis and publication bias
Sensitivity analysis was performed to evaluate the stability of results among studies. The results of sensitivity analysis using alternative statistical method (random-effect model, MH-RR = 0.99, 95% CI = 0.89–1.11), effect measure (MH-OR = 1.01, 95% CI = 0.90–1.13), and excluding studies with more than three items with unclear risk of bias (MH-RR = 1.02, 95% CI = 0.88–1.18) did not show any significant changes in pooled effects.
Finally, publication bias was assessed by funnel plots, and the asymmetry of the funnel plots were evaluated by Begg’s and Egger’s tests. Based on the Begg’s test (p = 0.120), Egger’s test (p = 0.083), and that the funnel plot was asymmetrical on visual inspection, there was a possibility of publication bias. Because of this, we conducted a sensitivity analysis using the trim and fill method, based on the assumption that the funnel plot asymmetry was caused by publication bias, and used the iterative method to estimate missing studies those were negative unpublished. After removing the most extreme small studies from the positive side of the funnel plot and adding hypothetical studies, we re-calculated the pooled RR and 95% CI until the funnel plot was symmetric; if the changes were not statistically significant, publication bias had little effect on the results and the results were stable. The results of trim and fill method showed that there was no statistical significance between the risk of cancers and DPP4i (MH-RR = 0.95, 95% CI = 0.86–1.06) (Fig. 4).
Figure 4.
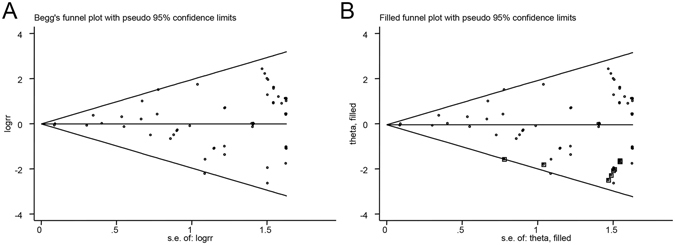
Funnel plot for the analysis of the effect of DPP-4 inhibitors on the risk of cancers. (A) Begg’s funnel plot of publication bias for the analysis of the pooled RRs. (B) The adjusted funnel plot using Trim and Fill method for publication bias.
Discussion
DPP4i is a class of new drugs that treat type 2 diabetes effectively. The advantages of using DPP4i for diabetes therapy are their insignificance on body weight gain and the low risk of hypoglycemia. However, some potential adverse events have been detected in the clinic30–33. Currently, many studies focus on the effect of DPP4i on cardiovascular disease, bone fracture and heart failure34–37. However, cancer adverse events of DPP4i during the treatment of type 2 diabetes should not be neglected. The aim of the present study was to assess the association of DPP4i use and cancer risk in the patients with type 2 diabetes.
The current meta-analysis, which analyzed the results of 72 RCTs, indicated that there was no significantly increased risk of cancer associated with DPP4i (MH-RR = 1.01, 95% CI = 0.91–1.12, p = 0.885). Same results were found using pre-defined subgroup analyses that grouped the studies by type of DPP4i, cancer subtype, comparison drug, trial duration, and baseline characteristics (age, HbA1c, BMI, and diabetes duration). Our result was also in agreement with a previous meta-analysis conducted by Monami et al.38, which reported that no significant difference in cancer incidence was observed between DPP4i and the comparison drug groups (MH-OR = 1.020, 95% CI = 0.74–1.40, p = 0.90).
Many types of cancer were observed during the RCTs. We divided these cancers into several groups based on the location of the cancer. The number of some types of cancer was small, for instance, vulval cancer, testis cancer, anal cancer, tongue cancer and so on, causing the RR of cancer to be small and the confidence intervals of risk estimates to be large. With the currently available information, very few studies had specifically explored the association between cancers and DPP4i, except for pancreatic cancer, thyroid cancer and colon cancer. Although RCTs were considered as the most rigorous studies to clarify the cause-effect relationships between drug exposure and outcome via double-blind and randomized controlled method, due to financial limitations, and we will rely upon more pharamcovigilance studies to assess the risk of cancers with DPP4i.
We found no evidence of increased risk of pancreatic cancer in patients treated with DPP4i (MH-RR = 0.83, 95% CI = 0.51–1.35), which was inconsistent with an aforementioned study published by Elashoff et al.13, who examined the reports of AEs from FAD-AERS databases from 2004–2009, and calculated the OR between the reported cases using sitagliptin and other anti-diabetes drugs; they concluded a high risk of pancreatic cancer with sitagliptin. It is known that incomplete data and reporting bias existed in the FAD-AERS database39. Furthermore, the criteria of inclusion and exclusion were not standardized; for instance, patients with back pain, urinary tract infection, chest pain, cough, and syncope were included in the control group, those diseases may had an influence on the tumorigenesis13. The reason for the increased risk of pancreatic cancer with incretin-based, in the opinion of Elashoff et al., was that the GLP-1-based therapy could induce asymptomatic low-grade pancreatitis40, and pancreatitis was relevant to the cellular transformation that leads to pancreatic cancer41, whether the GLP-1-based therapy could lead to pancreatic cancer eventually was still under debate42. In the current study, we compared the effect of DPP4i versus different types of comparison drugs and the results all showed no significant increase in pancreatic cancer, among these, sulfonylureas (MH-RR = 1.40, 95% CI = 0.99–1.96, p = 0.053), thiazolidinediones (MH-RR = 0.60, 95% CI = 0.27–1.33, p = 0.209). A new-user cohort study conducted by Gokhale et al.43 reported that the hazard of pancreatic cancer with DPP4i was similar to that with thiazolidinediones (HR = 1.0, 95% CI = 0.7–1.4) but lower than that with sulfonyureas (hazard ratio (HR) = 0.6, 95% CI = 0.4–0.9). The limitation of this study was the short treatment duration, and also it was an observational study, so the confounding bias induced by other potential variables may affect the outcomes.
Insulin resistance had been suggested as one of the causes of thyroid cancer44. Therefore, the use of antidiabetic drugs may negatively affect the development of thyroid cancer. In our study, we found that there was no statistical significance in the association between DPP4i and thyroid cancer (MH-RR = 0.73, 95% CI = 0.38–1.40, p = 0.345). This was consistent with the result concluded from the FAD-AERS database, which showed that sitagliptin was associated with a higher but not significant risk of thyroid cancer compared with control drugs (OR = 1.48, p = 0.65)13. However, a recent study evaluated such association in Taiwanese patients with newly diagnosed type 2 diabetes from 1999 to 2008 by using the reimbursement database of the National Health Insurance, and found that the overall HR for patients newly treated with sitagliptin compared with those treated with other antidiabetic drugs was 1.516 (95% CI = 1.011–2.271), indicating that sitagliptin use was associated with an increased risk of thyroid cancer45. The reason of this discrepancy may be that the database from which the Taiwanese study extracted records from lacked data for potential confounders. In addition, the validity of such a study is lower than RCTs.
In the present study, DPP4i were not associated with an increased risk of colon cancer in comparison with other drugs (MH-RR = 0.96, 95% CI = 0.71–1.31, p = 0.808). Nevertheless, Femia and colleagues studied the effect of long-term administration of sitagliptin on colon carcinogenesis in rats, at doses comparable to those used in therapeutic settings for humans with diabetes46. They found that rats had a significantly lower number of precancerous lesions in the colorectum in those treated with sitagliptin than in controls (p = 0.02), which indicated that sitagliptin had a protective effect against colon carcinogensis. The SAVOR-TIMI 53 trial showed a similar protective effect15. An in vitro study also suggested that DPP4i had anti-cancer property, and sitagliptin was found to be more potent than vildagliptin on inhibiting HT-29 colon cancer cells growth47. However, studies reporting that DPP4i had a protective effect on colon cancer were still few. Besides, Wang et al.48 found that DPP4i antidiabetic treatment did not increase the cancer risk,, and yet saxagliptin and sitagliptin could markedly increase cell migration and invasion of SW480 and HCT116 colon cancer cell lines through activation of nuclear factor E2-related factor 2 (NRF2). Therefore, further investigations also should be necessary to be performed to discuss the role of DPP4i antidiabetic drugs in diabetic patients with cancer.
A few studies also investigated the association between DPP4i and other types of cancer. A retrospective cohort study assessed the risk of prostate cancer associated with sitagliptin, also using the Taiwanese database of the National Health Insurance between 1999 and 2000, and the result of HR = 0.613 (95% CI = 0.493–0.763) showed that sitagliptin could significantly reduce the risk of prostate cancer49. Some in vivo studies explored the effect of DPP4 on tumorigenesis of the breast, ovary and prostate at the molecular level; however, it was not conclusive whether DPP4 promoted tumorigenesis50–52.
The current meta-analysis had several advantages. To the best of our knowledge, the present meta-analysis was the first to evaluate the effect of DPP4i on the risk of cancers based on RCTs. We conducted this meta-analysis using rigorous search and statistical analysis methods to ensure the accuracy and validity of the results. 11 studies were both published in the electronic databases and reported in the trial registry. We checked the data reported in publications against those in the clinical trial registry for consistency. In particular, some published studies we identified from the electronic databases did not report the data of cancer outcome, and we used the NCT codes from the publications to retrieve data on cancer from ClinicalTrials.gov. In this way, we minimized the risk of attrition and reporting bias.
However, several potential limitations in our meta-analysis also should be fully recognized. First, cancer was not the primary endpoint in any of the included trials and was reported as serious adverse events. There were no predefinition or any uniform diagnostic criteria, which could lead to misclassification. Second, the number of trials and the patients included still were insufficient to draw a definitive conclusion on the effect of DPP4i on the risk of cancers. Third, cancer is caused by many factors and cancer development is considerably complicated. In addition, more than a half of available studies the duration of treatment less than 52 weeks, so the duration of trials was still limited, which was inadequate to draw a conclusion on the occurrence of cancer with long-term DPP4i use. More RCTs with longer exposure to such drugs are required. Finally, we performed this study based on summary data; if we conducted the study with patient-level data, the assessment could be more accurate, but it was difficult for us to acquire the relevant data from electronic databases or trial registry.
In conclusion, the results of our meta-analysis showed that there is no significantly increased risk of cancer in patients with type 2 diabetes who are treated with DPP4i than those treated with a placebo or other types of drugs. Given the number of cancer adverse events and the limited duration of trials, there is still a need for large scale RCTs to be conducted to clarify the impact of DPP4i on cancers in the future, at the same time, it is also necessary to conduct pharmacovigilance programs to detect postmarketing AEs of drugs once they approve for marketing, and provide a longitudinal evidence to ensure that patients receive drugs of acceptable benefit-risk profiles.
Methods
Search strategy
The electronic databases PubMed, Medline, EMBASE, Web of Science and Cochrane Library were systematically and comprehensively searched to find published articles on randomized clinical trials in humans. The language of literature was limited to English. We combined both MeSH and free text terms to identify all of the relevant articles. Terms used for search were as follows: (1) “sitagliptin,” “vildagliptin,” “saxagliptin,” “alogliptin,” “linagliptin,” “dipeptidyl peptidase 4 inhibitors,” “DPP-4 inhibitors,” or “DPP4i”; (2) “cancer,” “carcinoma,” “tumor,” “neoplasm,” or “adenocarcinomas.” We also identified some completed but still unpublished studies through a search of the www.clinicaltrials.gov website. The literature search was conducted from the inception of each database to 25 July 2016.
Study selection
Studies were included into this meta-analysis if they met the following criteria: (a) randomized clinical trials; (b) conducted in patients with type 2 diabetes mellitus; (c) compared DPP4i with a placebo or active drugs; (d) with a duration of at least 24 weeks; (e) adverse drug events included cancer. The exclusion criteria were as follows: (a) the participants enrolled in trials had type 1 diabetes or no diabetes; (b) trials had a duration of treatment shorter than 24 weeks, because they could not yield relevant information on the incidence of cancer; (c) adverse drug events did not include tumors, the reported tumors were benign, or trials only reported cancer-specific mortality as an outcome but did not specify the type of cancer; (d) trials with incomplete original data or with two zero events. If several studies with the same population were retrieved, the one with the most complete data was used.
Data extraction and quality assessment
The title and abstract of studies were screened first, and if they met the inclusion criteria then they were reviewed in detail. The following information was extracted by two of the investigators (Ming Zhao and Xiaolong Lai) from the eligible studies: the first author’s name; year of publication; the national clinical trial (NCT) code; the type of DPP4i and the comparison drug; sample size of the treatment and control groups; the number of events per group; the duration of treatment; the numbers of males and females; mean age; mean glycosylated hemoglobin (HbA1c); mean body mass index (BMI); the duration of type 2 diabetes mellitus; and the type of cancers. Discrepancies between the two investigators were resolved by consensus or adjudication by a third investigator.
The Cochrane Collaboration’s risk of bias tool was used to assess the quality of the involved RCTs. The items for evaluating the bias of studies were classified into the following six domains: (a) random sequence generation (selection bias); (b) allocation concealment (selection bias); (c) blinding of participant, personnel and outcome assessment (performance bias and detection bias); (d) complete outcome data (attrition bias); (e) selective reporting (reporting bias); (f) drug compliance assessment (other bias). For each domain, the risk of bias was divided into low, high and unclear; an answer of “yes” indicated a low risk of bias, and an answer of “no” indicated a high risk of bias, and “unclear” indicated lack of relevant information. Given that cancer adverse event was not the primary outcome in many published RCTs, so there were not reported in the studies but on the website, we combined the published data and the data of cancer events on the www.clinicaltrials.gov website for trials reported in both places to evaluate the quality of involved RCTs.
Statistical analysis
We followed the preferred reporting items for systematic reviews and meta-analyses (PRISMA) for the reporting of this study53. The pooled relative risk (RR) and 95% confident intervals (CIs) calculated by the Mantel-Haenszel method were used to assess the relationship between DPP4i use and the risk of cancers.
Heterogeneity was evaluated using Cochrane Q statistic with a p < 0.1 considered statistically significant. I 2 statistic was also used to assess the magnitude of heterogeneity across studies. If I 2 <50% and P > 0.1, there was no significant heterogeneity, and a fixed-effect model was used; otherwise, a random-effect model was applied54. Pre-defined subgroup analyses were performed for trials that were stratified by the type of DPP4i (sitagliptin, saxagliptin, alogliptin, or linagliptin), location of cancer (reproductive system, digestive system, integumentary system, urinary system, hematologic system, respiratory system, motor system, endocrine system, nervous system, or cardiovascular system) (First, we combined the same adverse events of cancers and counted the number of studies based on the type of cancer, and then these cancers were classified into 10 types based on the location of cancer and counted the number again, due to a RCT may contain a variety of adverse events of cancers, so there existed duplicate in the final number of studies), drug for comparison (placebo, sulfonylureas, thiazolidinediones, metformin, sodium-glucose co-transporter (SGLT) inhibitors, GLP-1 receptor agonists (GLP-1 RAs), or other antidiabetic agents), trial duration (less than 52 weeks vs. 52 weeks or more), mean age (less than 60 years vs. 60 years or more), mean HbA1c (less than 8% vs. 8% or more), mean BMI (less than 30 kg/m2 vs. 30 kg/m2 or more), or mean diabetes duration (less than 8 years vs. 8 years or more).
In order to test the robustness of the results, sensitivity analysis was performed. We carried out the sensitivity analysis by using different statistical models (fixed-effect model vs. random-effect model), using different effect measures (relative risk vs. odds ratio (OR)) and excluding low-quality studies. Finally, publication bias was assessed by funnel plots, and the asymmetry of the funnel plots was evaluated by Begg’s and Egger’s tests; a p value ≤ 0.1 was considered statistically significant55,56. We also undertook the nonparametric “trim and fill” procedure to further assess the possible effect of publication bias in this meta-analysis. The possibility of hypothetical “missing” studies was considered to exist, and the “trim and fill” method was used to impute their RRs and recalculate a pooled RR that incorporated the hypothetical missing studies as if they actually existed57.
Meta-analysis was performed using the Stata software (version 12.0; Stata Corporation, College Station, Texas, USA).
Availability of materials and data
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Electronic supplementary material
Acknowledgements
This work was supported by Ningbo Science and Technology Innovation Team Program (2014B82002 to SB), the National Natural Science Foundation of China (81370165 to SB, 81272665 and 81471038 to QH); Fang Runhua Fund of Hong Kong, K.C. Wong Magna Fund in Ningbo University. The funding sources played no role in the design, collection, analysis, or interpretation of the data or in the decision to submit the manuscript for publication.
Author Contributions
Q.H. and S.B. designed the research, J.C. and Y.Y. conducted the research, M.Z. and X.L. obtained the data, M.Z. and F.W. analysis the data, M.Z. drafted the manuscript, Z.Z., D.M.R., F.W., and Y.X. made critical revisions to the manuscript.
Competing Interests
The authors declare that they have no competing interests.
Footnotes
A correction to this article is available online at https://doi.org/10.1038/s41598-017-16510-2.
Electronic supplementary material
Supplementary information accompanies this paper at doi:10.1038/s41598-017-07921-2
Change History: A correction to this article has been published and is linked from the HTML version of this paper. The error has been fixed in the paper.
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Qin Huang, Email: qxinyi1220@163.com.
Shizhong Bu, Email: bushizhongbu@nbu.edu.cn.
References
- 1.International Diabetes Federation website. Available: http://www.idf.org/.
- 2.Evans JM, Newton RW, Ruta DA, MacDonald TM, Morris AD. Socio-economic status, obesity and prevalence of Type 1 and Type 2 diabetes mellitus. Diabet Med. 2000;17:478–480. doi: 10.1046/j.1464-5491.2000.00309.x. [DOI] [PubMed] [Google Scholar]
- 3.Boyle JP, et al. Estimating prevalence of type 1 and type 2 diabetes in a population of African Americans with diabetes mellitus. Am J Epidemiol. 1999;149:55–63. doi: 10.1093/oxfordjournals.aje.a009728. [DOI] [PubMed] [Google Scholar]
- 4.Bruno G, et al. Incidence of type 1 and type 2 diabetes in adults aged 30–49 years: the population-based registry in the province of Turin, Italy. Diabetes Care. 2005;28:2613–2619. doi: 10.2337/diacare.28.11.2613. [DOI] [PubMed] [Google Scholar]
- 5.Holman N, Young B, Gadsby R. Current prevalence of Type 1 and Type 2 diabetes in adults and children in the UK. Diabet Med. 2015;32:1119–1120. doi: 10.1111/dme.12791. [DOI] [PubMed] [Google Scholar]
- 6.Drucker DJ, Nauck MA. The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes. Lancet. 2006;368:1696–1705. doi: 10.1016/S0140-6736(06)69705-5. [DOI] [PubMed] [Google Scholar]
- 7.Gilor C, Rudinsky AJ, Hall MJ. New Approaches to Feline Diabetes Mellitus: Glucagon-like peptide-1 analogs. J Feline Med Surg. 2016;18:733–743. doi: 10.1177/1098612X16660441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Yoon KH, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368:1681–1688. doi: 10.1016/S0140-6736(06)69703-1. [DOI] [PubMed] [Google Scholar]
- 9.Nathan DM. Finding new treatments for diabetes–how many, how fast… how good? N Engl J Med. 2007;356:437–440. doi: 10.1056/NEJMp068294. [DOI] [PubMed] [Google Scholar]
- 10.Son JW, Kim S. Dipeptidyl Peptidase 4 Inhibitors and the Risk of Cardiovascular Disease in Patients with Type 2 Diabetes: A Tale of Three Studies. Diabetes Metab J. 2015;39:373–383. doi: 10.4093/dmj.2015.39.5.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Green JB, et al. Effect of Sitagliptin on Cardiovascular Outcomes in Type 2 Diabetes. N Engl J Med. 2015;373:232–242. doi: 10.1056/NEJMoa1501352. [DOI] [PubMed] [Google Scholar]
- 12.Scirica BM, et al. Saxagliptin and cardiovascular outcomes in patients with type 2 diabetes mellitus. N Engl J Med. 2013;369:1317–1326. doi: 10.1056/NEJMoa1307684. [DOI] [PubMed] [Google Scholar]
- 13.Elashoff M, Matveyenko AV, Gier B, Elashoff R, Butler PC. Pancreatitis, pancreatic, and thyroid cancer with glucagon-like peptide-1-based therapies. Gastroenterology. 2011;141:150–156. doi: 10.1053/j.gastro.2011.02.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giovannucci E, et al. Diabetes and cancer: a consensus report. Diabetes Care. 2010;33:1674–1685. doi: 10.2337/dc10-0666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Leiter LA, et al. Frequency of cancer events with saxagliptin in the SAVOR-TIMI 53 trial. Diabetes Obes Metab. 2016;18:186–190. doi: 10.1111/dom.12582. [DOI] [PubMed] [Google Scholar]
- 16.Monami M, Dicembrini I, Mannucci E. Dipeptidyl peptidase-4 inhibitors and pancreatitis risk: a meta-analysis of randomized clinical trials. Diabetes Obes Metab. 2014;16:48–56. doi: 10.1111/dom.12176. [DOI] [PubMed] [Google Scholar]
- 17.Ahren B, et al. HARMONY 3: 104-week randomized, double-blind, placebo- and active-controlled trial assessing the efficacy and safety of albiglutide compared with placebo, sitagliptin, and glimepiride in patients with type 2 diabetes taking metformin. Diabetes Care. 2014;37:2141–2148. doi: 10.2337/dc14-0024. [DOI] [PubMed] [Google Scholar]
- 18.Mita T, et al. Alogliptin, a Dipeptidyl Peptidase 4 Inhibitor, Prevents the Progression of Carotid Atherosclerosis in Patients With Type 2 Diabetes: The Study of Preventive Effects of Alogliptin on Diabetic Atherosclerosis (SPEAD-A) Diabetes Care. 2016;39:139–148. doi: 10.2337/dc15-0781. [DOI] [PubMed] [Google Scholar]
- 19.Weinstock RS, et al. Safety and efficacy of once-weekly dulaglutide versus sitagliptin after 2 years in metformin-treated patients with type 2 diabetes (AWARD-5): a randomized, phase III study. Diabetes Obes Metab. 2015;17:849–858. doi: 10.1111/dom.12479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Schernthaner G, et al. Efficacy and tolerability of saxagliptin compared with glimepiride in elderly patients with type 2 diabetes: a randomized, controlled study (GENERATION) Diabetes Obes Metab. 2015;17:630–638. doi: 10.1111/dom.12461. [DOI] [PubMed] [Google Scholar]
- 21.Arjona Ferreira JC, et al. Efficacy and safety of sitagliptin versus glipizide in patients with type 2 diabetes and moderate-to-severe chronic renal insufficiency. Diabetes Care. 2013;36:1067–1073. doi: 10.2337/dc12-1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pratley RE, et al. Efficacy and safety of switching from the DPP-4 inhibitor sitagliptin to the human GLP-1 analog liraglutide after 52 weeks in metformin-treated patients with type 2 diabetes: a randomized, open-label trial. Diabetes Care. 2012;35:1986–1993. doi: 10.2337/dc11-2113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Leiter LA, et al. Efficacy and safety of saxagliptin in older participants in the SAVOR-TIMI 53 trial. Diabetes Care. 2015;38:1145–1153. doi: 10.2337/dc14-2868. [DOI] [PubMed] [Google Scholar]
- 24.Bajaj M, et al. Linagliptin improved glycaemic control without weight gain or hypoglycaemia in patients with type 2 diabetes inadequately controlled by a combination of metformin and pioglitazone: a 24-week randomized, double-blind study. Diabet Med. 2014;31:1505–1514. doi: 10.1111/dme.12495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.White WB, et al. Alogliptin after acute coronary syndrome in patients with type 2 diabetes. N Engl J Med. 2013;369:1327–1335. doi: 10.1056/NEJMoa1305889. [DOI] [PubMed] [Google Scholar]
- 26.Gallwitz B, et al. 2-year efficacy and safety of linagliptin compared with glimepiride in patients with type 2 diabetes inadequately controlled on metformin: a randomised, double-blind, non-inferiority trial. Lancet. 2012;380:475–483. doi: 10.1016/S0140-6736(12)60691-6. [DOI] [PubMed] [Google Scholar]
- 27.Barnett AH, et al. Linagliptin monotherapy in type 2 diabetes patients for whom metformin is inappropriate: an 18-week randomized, double-blind, placebo-controlled phase III trial with a 34-week active-controlled extension. Diabetes Obes Metab. 2012;14:1145–1154. doi: 10.1111/dom.12011. [DOI] [PubMed] [Google Scholar]
- 28.Aschner P, et al. Insulin glargine versus sitagliptin in insulin-naive patients with type 2 diabetes mellitus uncontrolled on metformin (EASIE): a multicentre, randomised open-label trial. Lancet. 2012;379:2262–2269. doi: 10.1016/S0140-6736(12)60439-5. [DOI] [PubMed] [Google Scholar]
- 29.Available from http://www.clinicaltrials.gov.
- 30.Scirica BM, et al. Heart Failure, Saxagliptin, and Diabetes Mellitus: Observations from the SAVOR-TIMI 53 Randomized Trial. Circulation. 2015;132:e198. doi: 10.1161/CIRCULATIONAHA.115.015511. [DOI] [PubMed] [Google Scholar]
- 31.Tarapues M, Cereza G, Figueras A. Association of musculoskeletal complaints and gliptin use: review of spontaneous reports. Pharmacoepidemiol Drug Saf. 2013;22:1115–1118. doi: 10.1002/pds.3503. [DOI] [PubMed] [Google Scholar]
- 32.Berhan A, Berhan Y. Efficacy of alogliptin in type 2 diabetes treatment: a meta-analysis of randomized double-blind controlled studies. BMC Endocr Disord. 2013;13:9. doi: 10.1186/1472-6823-13-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brown NJ, Byiers S, Carr D, Maldonado M, Warner BA. Dipeptidyl peptidase-IV inhibitor use associated with increased risk of ACE inhibitor-associated angioedema. Hypertension. 2009;54:516–523. doi: 10.1161/HYPERTENSIONAHA.109.134197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scirica BM. The Safety of Dipeptidyl Peptidase 4 Inhibitors and the Risk for Heart Failure. JAMA Cardiol. 2016;1:123–125. doi: 10.1001/jamacardio.2016.0184. [DOI] [PubMed] [Google Scholar]
- 35.Kongwatcharapong J, Dilokthornsakul P, Nathisuwan S, Phrommintikul A, Chaiyakunapruk N. Effect of dipeptidyl peptidase-4 inhibitors on heart failure: A meta-analysis of randomized clinical trials. Int J Cardiol. 2016;211:88–95. doi: 10.1016/j.ijcard.2016.02.146. [DOI] [PubMed] [Google Scholar]
- 36.Kaneko M, Narukawa M. Meta-analysis of dipeptidyl peptidase-4 inhibitors use and cardiovascular risk in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2016;116:171–182. doi: 10.1016/j.diabres.2016.04.012. [DOI] [PubMed] [Google Scholar]
- 37.Fu J, Zhu J, Hao Y, Guo C, Zhou Z. Dipeptidyl peptidase-4 inhibitors and fracture risk: an updated meta-analysis of randomized clinical trials. Sci Rep. 2016;6:29104. doi: 10.1038/srep29104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Monami M, Dicembrini I, Martelli D, Mannucci E. Safety of dipeptidyl peptidase-4 inhibitors: a meta-analysis of randomized clinical trials. Curr Med Res Opin. 2011;27(Suppl 3):57–64. doi: 10.1185/03007995.2011.602964. [DOI] [PubMed] [Google Scholar]
- 39.Gale EA. Collateral damage: the conundrum of drug safety. Diabetologia. 2009;52:1975–1982. doi: 10.1007/s00125-009-1491-8. [DOI] [PubMed] [Google Scholar]
- 40.Meier JJ, Nauck MA. Risk of pancreatitis in patients treated with incretin-based therapies. Diabetologia. 2014;57:1320–1324. doi: 10.1007/s00125-014-3231-y. [DOI] [PubMed] [Google Scholar]
- 41.Bhanot UK, Moller P. Mechanisms of parenchymal injury and signaling pathways in ectatic ducts of chronic pancreatitis: implications for pancreatic carcinogenesis. Lab Invest. 2009;89:489–497. doi: 10.1038/labinvest.2009.19. [DOI] [PubMed] [Google Scholar]
- 42.Koehler JA, Baggio LL, Lamont BJ, Ali S, Drucker DJ. Glucagon-like peptide-1 receptor activation modulates pancreatitis-associated gene expression but does not modify the susceptibility to experimental pancreatitis in mice. Diabetes. 2009;58:2148–2161. doi: 10.2337/db09-0626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gokhale M, et al. Dipeptidyl-peptidase-4 inhibitors and pancreatic cancer: a cohort study. Diabetes Obes Metab. 2014;16:1247–1256. doi: 10.1111/dom.12379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shih SR, Chiu WY, Chang TC, Tseng CH. Diabetes and thyroid cancer risk: literature review. Exp Diabetes Res. 2012;2012:578285. doi: 10.1155/2012/578285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tseng CH. Sitagliptin use and thyroid cancer risk in patients with type 2 diabetes. Oncotarget. 2016;7:24871–24879. doi: 10.18632/oncotarget.8399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Femia AP, et al. Long-term treatment with Sitagliptin, a dipeptidyl peptidase-4 inhibitor, reduces colon carcinogenesis and reactive oxygen species in 1,2-dimethylhydrazine-induced rats. Int J Cancer. 2013;133:2498–2503. doi: 10.1002/ijc.28260. [DOI] [PubMed] [Google Scholar]
- 47.Amritha CA, Kumaravelu P, Chellathai DD. Evaluation of Anti Cancer Effects of DPP-4 Inhibitors in Colon Cancer- An Invitro Study. J Clin Diagn Res. 2015;9:FC14–16. doi: 10.1111/crj.12098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wang H, et al. NRF2 activation by antioxidant antidiabetic agents accelerates tumor metastasis. Sci Transl Med. 2016;8:334ra351. doi: 10.1126/scitranslmed.aad6095. [DOI] [PubMed] [Google Scholar]
- 49.Tseng CH. Sitagliptin may reduce prostate cancer risk in male patients with type 2 diabetes. Oncotarget. 2017;8:19057–19064. doi: 10.18632/oncotarget.12137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Choi HJ, et al. Dipeptidyl peptidase 4 promotes epithelial cell transformation and breast tumourigenesis via induction of PIN1 gene expression. Br J Pharmacol. 2015;172:5096–5109. doi: 10.1111/bph.13274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kajiyama H, et al. Dipeptidyl peptidase IV overexpression induces up-regulation of E-cadherin and tissue inhibitors of matrix metalloproteinases, resulting in decreased invasive potential in ovarian carcinoma cells. Cancer Res. 2003;63:2278–2283. [PubMed] [Google Scholar]
- 52.Wesley UV, McGroarty M, Homoyouni A. Dipeptidyl peptidase inhibits malignant phenotype of prostate cancer cells by blocking basic fibroblast growth factor signaling pathway. Cancer Res. 2005;65:1325–1334. doi: 10.1158/0008-5472.CAN-04-1852. [DOI] [PubMed] [Google Scholar]
- 53.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg. 2010;8:336–341. doi: 10.1016/j.ijsu.2010.02.007. [DOI] [PubMed] [Google Scholar]
- 54.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Egger M, Davey Smith G, Schneider M. & Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–1101. doi: 10.2307/2533446. [DOI] [PubMed] [Google Scholar]
- 57.Duval S, Tweedie R. Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics. 2000;56:455–463. doi: 10.1111/j.0006-341X.2000.00455.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


