Abstract
Background
Surgical disease burden falls disproportionately on individuals in low- and middle-income countries. These populations are also the least likely to have access to surgical care. Understanding the barriers to access in these populations is therefore necessary to meet the global surgical need.
Methods
Using geospatial methods, this study explores the district-level variation of two access barriers in Ghana: poverty and spatial access to care. National survey data were used to estimate the average total household expenditure (THE) in each district. Estimates of the spatial access to essential surgical care were generated from a cost-distance model based on a recent surgical capacity assessment. Correlations were analyzed using regression and displayed cartographically.
Results
Both THE and spatial access to surgical care were found to have statistically significant regional variation in Ghana (p < 0.001). An inverse relationship was identified between THE and spatial access to essential surgical care (β −5.15 USD, p < 0.001). Poverty and poor spatial access to surgical care were found to co-localize in the northwest of the country.
Conclusions
Multiple barriers to accessing surgical care can coexist within populations. A careful understanding of all access barriers is necessary to identify and target strategies to address unmet surgical need within a given population.
Introduction
Surgical conditions represent one of the leading contributors to the global burden of disease, accounting for up to a third of all disability-adjusted life years incurred annually [1]. The burden incurred from unmet surgical needs falls disproportionately on low- and middle-income countries (LMICs), whose populations are least able to access timely, affordable, and quality care [2, 3]. Before global surgical needs can be met, a thorough understanding of the barriers to accessing surgical care is required.
Access to care may be obstructed by a variety of factors including the availability, acceptability, or the affordability of a service [4]. The affordability of surgery is of particular concern in LMICs due to the cost of health care relative to average annual total household expenditures in many of these settings (THE). Impoverishment through healthcare seeking, known as catastrophic healthcare expenditure (CHE), is often defined by ten percent or more of annual THE being spent to access health care. Using this definition, one recent study suggested that over half of the world’s population, including a significant proportion of Ghana’s population, would be pushed into poverty should they require surgical care [1]. In addition to this high CHE, the acceptability and the availability of essential surgery have also been identified as access barriers for subsets of the Ghanaian population, suggesting that all of the major dimensions of access have relevance in Ghana [5, 6].
Although it is useful to consider the dimensions of service accessibility independently, it is perhaps more important to examine how they combine within a given population to develop targeted strategies to redress access inequalities. As the potential non-medical cost burden (i.e., travel costs, lodging, food, lost wages) associated with surgical care increases with travel time, poor availability of surgical care has the potential to increase the risk of CHE and rates of unmet surgical needs [7, 8]. Research from high-income countries has previously demonstrated that care is less accessible in more impoverished areas, suggesting these non-medical costs may be higher among the poor [9]. If this relationship was true for LMICs, recent estimates of CHE may underestimate the burden of non-medical costs for impoverished areas [2].
To clarify the relationship between poverty and access to essential surgical care in Ghana, we used geospatial methods to correlate a national poverty survey with a recent surgical capacity assessment. By identifying areas at elevated risk of CHE, it may be possible to target protective interventions at a more local level.
Methods
Study design
This study is an observational geospatial analysis of the relationship between annual THE and the spatial accessibility of essential surgical care in Ghana.
Study data
Data on annual THE in Ghana were obtained from the Ghana Living Standards Survey (GLSS), which is a nationally representative survey on consumption expenditure that was conducted between 2012 and 2013 on 18,000 households [10]. District administrative boundaries and population data were obtained from the Ghana Statistical Service and the WorldPop project, respectively [11, 12]. Data on national transportation networks were obtained from the Center for Remote Sensing and Geographic Information Services (CERSGIS) and OpenStreetMap, which are both providers of high-quality road network data in Ghana [13, 14]. The locations of hospitals capable of providing essential surgical services were obtained from a recent capacity assessment [5, 15, 16]. All geospatial analyses were conducted with ArcMap 10.1 (Esri, Redlands, CA). Statistical analyses were conducted using Stata v14.0 (StataCorp, College Station, TX).
Poverty mapping
Mean district THE was calculated by aggregating household-level THE estimates to the district corresponding to the household’s primary sampling unit. Household weights were applied as an adjustment for the two-stage sampling design. The design of the GLSS does not permit the estimation of welfare measures at the district level; therefore, areal interpolation was performed using the Kriging method to obtain estimates of nominal THE in the nine districts that were not sampled [17].
Access estimates
Using previously described methods, cost-distance analyses were performed to model the average travel time to surgical care for each district [16]. Briefly, a grid (i.e., cost surface) was superimposed over the country; each cell was assigned an impedance value, which corresponded to the time required to traverse that cell. The cost surface was constructed using the national road network and each road’s corresponding speed limit. Background cells were assigned a value corresponding to a speed of travel of 5 km h−1 (i.e., the average speed of walking). The technique identified the least time-consuming path from any point on the grid to the nearest facility capable of providing essential surgical care [5, 18].
District-level mean travel times to essential surgical care were then calculated by averaging the values of the cells within each district. Averages were weighted by population distribution using a 100 m2 grid-based population layer [12].
Correlations between a district’s predicted THE and its average travel time to essential surgical care were analyzed using linear regression. Additionally, THE and travel time were divided into quantiles and displayed using a bivariate choropleth map to illustrate where these correlations were observed. Spatial autocorrelation of access and poverty were explored using the Global Moran’s Index [19].
Results
The GLSS sampled 18,000 households and interviewed 16,772 persons (response rate = 93 %). Following areal interpolation, the median THE was 2257 USD annually [Interquartile range (IQR) 1830–2753 USD]. Districts with lower annual THE, representing more impoverished areas, were concentrated in the northwest of the country. In contrast, districts with higher mean THE were concentrated in the southwest. Overall, THE was found to be strongly spatially dependent in Ghana (Moran Index 0.55, p < 0.001) implying that districts with similarly high or low THE tend to cluster together.
Following population-weighted aggregation of the cost-distance analysis to the district level, median travel time to a facility capable of providing essential surgical services was 61.7 min (IQR 35.6–96.8 min). The accessibility of essential surgical care exhibited a similar spatial pattern, with the northwest having worse access to surgical care than the south of the country. Nationally, essential surgical care access was found to be strongly spatially dependent (Moran Index 0.66, p < 0.001) suggesting that availability of essential surgical care is not evenly distributed over space but instead tends to cluster in a few areas.
An inverse relationship between mean travel time to essential surgical care and annual THE was identified and is illustrated in Fig. 1a. This association was confirmed by linear regression (β −5.15 USD, p < 0.001). A positive association was also found between THE and population density, suggesting poverty is concentrated in the more rural districts (Fig. 1b). A bivariate choropleth map illustrating the geographic distribution of poverty and access to surgical care is provided in Fig. 2. This map illustrates a concentration of impoverished districts with poor access to surgical care in the northwest of the country, representing districts that may be at particular risk of high rates of CHE.
Fig. 1.
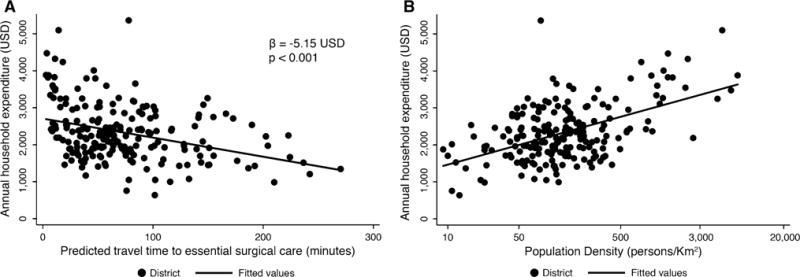
a Scatter plot with fitted line demonstrating an inverse relationship between total household expenditure and travel time to emergency surgical care. b Scatter plot with fitted line demonstrating a positive relationship between total household expenditure and population density. Note population density is expressed on a log scale
Fig. 2.
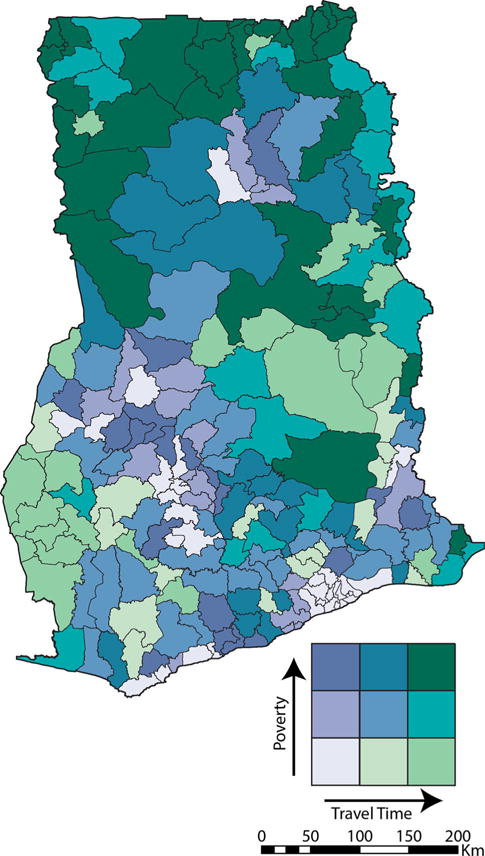
Bivariate choropleth map demonstrating the colocalization of poverty and poor accessibility of surgical care in Ghana
Discussion
This study is an observational geospatial analysis of the regional variability of poverty and essential surgical accessibility in Ghana. Both annual THE and travel time to essential surgical care were found to be spatially dependent in this analysis. More notably, there was a significant inverse correlation between poverty and essential surgical accessibility in Ghana, suggesting impoverished areas have worse access to essential surgical care. The relationship between poverty and population density suggests the rural areas of Ghana are particularly at risk due to their lower mean THEs and their poorer access to centrally located healthcare resources. Poverty and low accessibility to essential surgical care were found to be highly co-localized in the predominantly rural northwestern region of the country, which represents a potential target for interventions designed to improve access to essential surgery.
Although no definition of CHE is universally accepted, one definition describes CHE as occurring when ten percent of the overall household expenditure is used to access health care [20]. Regardless of the specific definition used, the risk of CHE is thought to concentrate among the poor, particularly in healthcare systems predominately financed by out-of-pocket payments [21, 22]. Exacerbating the direct costs of accessing health care are the non-medical costs associated with food, travel, and lodging [22]. These costs are expected to increase with travel distance, making them particularly burdensome for patients accessing centralized services such as essential surgery [7]. By subsidizing travel costs or improving access to essential surgery in areas where poverty and poor access co-localize, it may be possible to offset some of the financial burden of healthcare seeking and therefore have a positive impact on the rates of both CHE and unmet surgical needs.
The observation that the availability of medical care tends to vary inversely with the need for it in the population is not new. This observation, referred to as the inverse care law, was first formalized in 1971 and has subsequently been observed in several high-income settings [9, 23–25]. More recently, the inverse care law has even been described for primary care in sub-Saharan Africa [26]. To date, there has been little discussion of the inverse care law related to essential surgery in LMICs, which will be a vital consideration to achieving the United Nations Sustainable Development Goals [27]. In recent models of CHE, nonmedical costs are represented as a proportion of the medical costs, but these data suggest this could potentially underestimate the magnitude of impoverishment experienced by the poor who require surgical care [22]. Therefore, future models need to include sub-national estimates of non-medical costs to fully appreciate the impacts that these costs have on poverty and health-seeking behavior.
Although this study reports an important observation that can be used to strengthen surgical care access in Ghana and can serve as a useful model for other LMICs, several limitations need to be considered. First, the poverty data used were from a nationally representative population sample. Although the methods used to aggregate these data to the district level are well described and robust, they represent estimations with the possibility of error. Additionally, travel time estimates were also modeled. Estimating travel time is associated with unique challenges in LMICs due to the influence of variable road conditions and transportation infrastructure on overland speeds [28]. However, the methods used to model travel time in this study have previously been applied in LMICs and found to be better predict travel time than other methods [28, 29]. Finally, for the purposes of displaying CHE risk, this study assumes out-of-pocket payments and medical costs are homogeneous throughout Ghana. Although this is not strictly true, the variability in out-of-pocket payments is small and unlikely to influence the overall validity of the model [30]. Despite these limitations, these data provide strong evidence that poor access to essential surgery is concentrated among the poor in Ghana. Interventions designed to improve access to surgery should therefore be focused on these groups. Geospatial analyses are one approach that can be used to target these interventions in Ghana, and potentially other LMICs.
Acknowledgments
This study was funded in part by Grants R25TW009345 and D43TW007267 from the Fogarty International Center, US National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Compliance with ethical standards
Conflict of interest No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- 1.Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015 doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 2.Meara JG, Leather AJM, Hagander L, Alkire BC, Alonso N, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569–624. doi: 10.1016/S0140-6736(15)60160-X. [DOI] [PubMed] [Google Scholar]
- 3.Stewart B, Quansah R, Gyedu A, Ankomah J, Donkor P, et al. Strategic assessment of trauma care capacity in Ghana. World J Surg. 2015;39(10):2428–2440. doi: 10.1007/s00268-015-3132-3. [DOI] [PubMed] [Google Scholar]
- 4.Penchansky R, Thomas JW. The concept of access: definition and relationship to consumer satisfaction. Med Care. 1981;19:127–140. doi: 10.2307/3764310. [DOI] [PubMed] [Google Scholar]
- 5.Stewart B, Tansley G, Gyedu A, Ofosu A, Donkor P, et al. Mapping access to essential surgical care in Ghana using the availability of Bellwether procedures. JAMA Surg. 2016;151(8):e161239. doi: 10.1001/jamasurg.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gyedu A, Abantanga F, Boakye G, Gupta S, Otupiri E, et al. Barriers to essential surgical care experienced by women in the two northernmost regions of Ghana: a cross-sectional survey. BMC Womens Health. 2016;16:27. doi: 10.1186/s12905-016-0308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kifle YA, Nigatu TH. Cost-effectiveness analysis of clinical specialist outreach as compared to referral system in Ethiopia: an economic evaluation. Cost Eff Resour Alloc. 2010;8:13. doi: 10.1186/1478-7547-8-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Groen RS, Samai M, Stewart KA, Cassidy LD, Kamara TB, et al. Untreated surgical conditions in Sierra Leone: a cluster randomised, cross-sectional, countrywide survey. Lancet. 2012;380:1082–1087. doi: 10.1016/S0140-6736(12)61081-2. [DOI] [PubMed] [Google Scholar]
- 9.Tudor Hart J. The inverse care law. Lancet. 1971;297:405–412. doi: 10.1016/S0140-6736(71)92410-X. [DOI] [PubMed] [Google Scholar]
- 10.Ghana Statisical Service (GSS) Ghana poverty mapping report. Accra; Ghana: 2015. pp. 1–77. [Google Scholar]
- 11.Ghana Statistical Service. 2016 http://www.statsghana.gov.gh/index.html. Accessed 5 April 2016.
- 12.The WorldPop Project. WorldPop Data. n.d. http://www.worldpop.org.uk/. Accessed 11 Jan 2015.
- 13.Mensa M, Sablah E, Amamoo-Otchere E, Mensah F. Digital mapping and GIS-driven feeder road network database management system for road project: planning and implementation monitoring in the feeder road sector. Accra; Ghana: 2006. [Google Scholar]
- 14.OpenStreetMap. n.d. http://www.openstreetmap.org/#map=6/-1.494/36.310. Accessed 29 June 2015.
- 15.Tansley G, Stewart B, Zakariah A, Boateng E, Achena C, et al. Population-level spatial access to prehospital care by the national ambulance service in Ghana. Prehospital Emerg care. 2016 doi: 10.3109/10903127.2016.1164775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stewart BT, Gyedu A, Tansley G, Yeboah D, Amponsah-Manu F, et al. Orthopedic care capacity assessment and strategic palnning in Ghana: mapping a way forward. Ann Glob Health. 2016;82(3):560–561. doi: 10.1016/j.aogh.2016.04.506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goodchild MF, Lam NS-N. Areal interpolation: a variant of the traditional spatial problem. Geo-processing. 1980;1:197–312. [Google Scholar]
- 18.Debas HT, Donkor P, Gawande A, Jamison DT, Kruk ME, et al., editors. Disease control priorities, vol 1: Essential surgery. 3rd. World Bank; Washington, DC: 2015. [DOI] [PubMed] [Google Scholar]
- 19.Moran P. Notes on continuous stochastic phenomena. Biometrika. 1950;37:17–23. doi: 10.2307/2332142. [DOI] [PubMed] [Google Scholar]
- 20.Xu K, Evans DB, Carrin G, Aguilar-Rivera AM, Musgrove P, et al. Protecting households from catastrophic health spending. Health Aff. 2007;26:972–983. doi: 10.1377/hlthaff.26.4.972. [DOI] [PubMed] [Google Scholar]
- 21.Meremikwu MM, Ehiri JE, Nkanga DG, Udoh EE, Ikpatt OF, et al. Socioeconomic constraints to effective management of Burkitt’s lymphoma in south-eastern Nigeria. Trop Med Int Health. 2005;10:92–98. doi: 10.1111/j.1365-3156.2004.01348.x. [DOI] [PubMed] [Google Scholar]
- 22.Shrime MG, Dare AJ, Alkire BC, O’Neill K, Meara JG. Catastrophic expenditure to pay for surgery worldwide: a modelling study. Lancet Glob Health. 2015;3(Suppl 2):S38–S44. doi: 10.1016/S2214-109X(15)70085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mercer SW, Watt GCM. The inverse care law: clinical primary care encounters in deprived and affluent areas of Scotland. Ann Fam Med. 2007;5:503–510. doi: 10.1370/afm.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pedersen A, Vedsted P. Understanding the inverse care law: a register and survey-based study of patient deprivation and burnout in general practice. Int J Equity Health. 2014;13:121. doi: 10.1186/s12939-014-0121-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Torjesen I. Analysis shows “postcode lottery” in access to GPs in England. BMJ. 2014;348:g3688. doi: 10.1136/bmj.g3688. [DOI] [PubMed] [Google Scholar]
- 26.Moosa S, Wojczewski S, Hoffmann K, Poppe A, Nkomazana O, et al. The inverse primary care law in sub-Saharan Africa. Br J Gen Pract. 2014 doi: 10.3399/bjgp14X680089.e321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.WHO (World Health Organization) Health in 2015: from MDGs, Millennium Development Goals to SDGs, Sustainable Development Goals. World Health Organization; Geneva: 2015. [Google Scholar]
- 28.Nesbitt RC, Gabrysch S, Laub A, Soremekun S, Manu A, et al. Methods to measure potential spatial access to delivery care in low- and middle-income countries: a case study in rural Ghana. Int J Health Geogr. 2014;13:25. doi: 10.1186/1476-072X-13-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gething PW, Johnson FA, Frempong-Ainguah F, Nyarko P, Baschieri A, et al. Geographical access to care at birth in Ghana: a barrier to safe motherhood. BMC Public Health. 2012;12:991. doi: 10.1186/1471-2458-12-991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Asante F, Chikwama C, Daniels A, Armar-Klemesu M. Evaluating the economic outcomes of the policy of fee exemption for maternal delivery care in ghana. Ghana Med J. 2007;41:110–117. doi: 10.4314/gmj.v41i3.55277. [DOI] [PMC free article] [PubMed] [Google Scholar]


