Abstract
Introduction
This study aimed to document the growth and challenges encountered in the decade since inception of the National Ambulance Service (NAS) in Ghana, West Africa. By doing so, potentially instructive examples for other low- and middle-income countries (LMICs) planning a formal prehospital care system or attempting to identify ways to improve existing emergency services could be identified.
Methods
Data routinely collected by the Ghana NAS from 2004–2014 were described, including: patient demographics, reason for the call, response location, target destination, and ti1mes of service. Additionally, the organizational structure and challenges encountered during the development and maturation of the NAS were reported.
Results
In 2004, the NAS piloted operations with 69 newly trained emergency medical technicians (EMTs), nine ambulances, and seven stations. The NAS expanded service delivery with 199 ambulances at 128 stations operated by 1,651 EMTs and 47 administrative and maintenance staff in 2014. In 2004, nine percent of the country was covered by NAS services; in 2014, 81% of Ghana was covered. Health care transfers and roadside responses comprised the majority of services (43%–80% and 10%–57% by year, respectively). Increased mean response time, stable case holding time, and shorter vehicle engaged time reflect greater response ranges due to increased service uptake and improved efficiency of ambulance usage. Specific internal and external challenges with regard to NAS operations also were described.
Conclusion
The steady growth of the NAS is evidence of the need for Emergency Medical Services and the effects of sound planning and timely responses to changes in program indicators. The way forward includes further capacity building to increase the number of scene responses, strengthening ties with local health facilities to ensure timely emergency medical care and appropriateness of transfers, assuring a more stable funding stream, and improving public awareness of NAS services.
Keywords: developing countries, Emergency Medical Services, Ghana
Introduction
Emergency conditions are responsible for a disproportionately large burden of disease in low- and middle-income countries (LMICs).1 Inopportunely, patients in LMICs lack access to timely care for common conditions that require emergency treatment.2 As a result, the avertable burden of conditions requiring emergency care is enormous and requires a robust, multi-faceted approach to be reduced.2,3 While hospital-based emergency care improvement initiatives are important in this effort, their absolute effectiveness is limited by significant prehospital times and a large proportion of people who die before reaching the hospital in LMICs.4,5
In Ghana, West Africa, prehospital emergency care services were entirely informal and extremely limited prior to the early 2000s.6,7 Resultantly, more than one-half of seriously injured patients died prior to reaching a hospital, even in urban centers, compared to 21% in Seattle, Washington USA.8 The majority of severely ill or injured people who reached a health facility were brought there by a commercial vehicle (eg, taxi or minibus), often only after relatives paid commercial drivers for their service.5 Such practices sometimes included some form of first aid, usually carried out without any formal training. In addition to prehospital care needs, inter-hospital transfers for diagnostics or more advanced treatments are common given limited hospital-based care capacity at first- and second-level hospitals in Ghana, as they are in other LMICs.9,10 Without a formal ambulance service, inter-hospital transfers often involved a taxi, pre-payment, and long delays in care associated with families’ attempts to gather money.6,11 Further, medical care capabilities provided during transport were non-existent. For these reasons, a more formal prehospital care system urgently was required.
In an effort to improve the weak de-facto prehospital care system, courses that provided first aid training to commercial drivers were established and demonstrated some success.6 However, no organized, systematic strategy for their sustainability over the long-term was developed; thus, over time, they were dissolved.6,7 Similarly, a few health administrators and political leaders attempted to found prehospital care capabilities in several areas by providing ambulances directly to hospitals.11 Without planning for the training of staff to use them, re-stocking of supplies, ongoing monitoring, and evaluation or formal financing mechanisms, these systems ultimately failed also.11
On May 9, 2001, 127 people were trampled to death at a stadium disruption in Accra, Ghana, which was reported to the public in dramatic detail. In part due to a newfound public awareness of a deficient disaster management strategy and part the effect of long-term advocacy by health professionals, a groundswell of support for an ambulance system began. During the following Annual Sessional Address to Parliament, Ghana’s head of state, His Excellency John Agyekum Kufour, charged the Ministry of Health (Accra, Ghana) and collaborators to establish a national ambulance service.11 As a result of this directive and the immense efforts of officers in the health sector, the National Fire Service (Accra, Ghana), the Office of the State Attorney (Accra, Ghana), and others, the National Ambulance Service (NAS) was established in 2004 and became fully operational in 2006.
This study aimed to document the growth and challenges encountered in the decade since the creation of the NAS in Ghana. The examples might be instructive for other LMICs planning the foundation of a formal prehospital care system or attempting to identify ways to improve existing prehospital care services.
Methods
Setting
Ghana is a heavily indebted, lower-middle income country in West Africa with a population of 26 million and an annual per capita income of US$1,760.12 While 53% of the population live in one of several densely populated areas, 12.2 million are spread over 348,540 km2.13 Only 13% of the country’s 109,515 km of roads are paved, which are of varying quality. As proxies for conditions requiring emergency transport, injuries and obstetric emergencies are responsible for 45 and nine deaths per 100,000 persons per year, respectively.14 Figures from an equivalently sized high-income country, the United Kingdom, are used for reference: 82% live in urban areas; 100% of roads are paved with a total network of 398,350 km2.15 There are 36 injury deaths per 100,000 persons annually. Obstetric emergency deaths are rare (0.1 per 100,000 persons).14
Nearly all of the 216 districts in Ghana have a first-level hospital that is staffed by a general practitioner and provides basic emergency and surgical services (eg, assessment, resuscitation, and cesarean section);16 however, many first-level staff have insufficient emergency care training.17 Further, these facilities often are limited by a lack of human and/or physical resources, which limits their capabilities for more advanced care (eg, diagnostic imaging and general laboratory services).18–20 Patients that require more complex care are referred to a higher level hospital (ie, one of the nine referral hospitals or four tertiary hospitals); the NAS often performs these transfers so that care can be rendered during transport. Referral and tertiary hospitals have specialist providers and offer a greater scope of emergency services and definitive care.
Data Collection
Organizational structure and specific challenges were described in narrative based on prior documentation and the experiences of the authors who work for the NAS.21,22 Additionally, data routinely collected by the NAS were used. After each ambulance response, patient demographics, reason for the call, location of response, and times associated with each part of service delivery were recorded. Data were entered into a database daily and reviewed weekly by station supervisors for accuracy and completeness. After, data were transmitted to NAS headquarters in Accra for archiving and periodic evaluation.
Each data item was not collected for every year since NAS inception. As the ambulance service matured and operational needs changed, certain data items were dropped and others added. Therefore, some data were not recorded for certain years (eg, indicator times for 2004). These gaps are specified in the tables. Use of these routinely gathered, anonymous data for this publication was determined to be exempt from review by the University of Washington (Seattle, Washington USA) Institutional Review Board.
Indicator Definitions
Response time is the time from reception of the call by station personnel to time at the patient’s side. Case holding time is the time from arriving at the patient’s side to leaving the health care facility or scene with the patient. Vehicle engaged time is the total time spent per call, from reception of the call to ready for the next call, including completion of documentation and sanitizing and re-stocking the ambulance.
Data Analysis
Descriptive statistics were performed with Stata v13 (College Station, Texas USA). Station locations were geo-referenced and maps were created using ArcGIS v10 (Redlands, California USA). Coverage representations on the map were generated assuming that, on average, 60km could be covered realistically in one hour from each station given the diversity of road quality, average traffic density, and improved mobility with siren use. Polygons were drawn to represent areas within 200 meters of a primary, secondary, or tertiary road (ie, roads that ambulances are able to traverse safely). Areas were calculated excluding bodies of water. As a gross proxy for unmet prehospital care need, the responses per day per population were calculated using population estimates from the World Bank Group (Washington, DC USA).13 The rates were calculated using available data; therefore, they are not disaggregated by station or region.
Results
Creating an Organizational Structure
With proposal of the NAS Bill in 2004, seven sites in three of Ghana’s 10 regions were selected to pilot the NAS. Fifty-seven members of the National Fire Service and six drivers were trained as emergency medical technicians (EMTs). These personnel staffed the pilot stations for 15 months. Managing these pilot sites unearthed significant challenges related to lack of direct oversight that led the creation of a three-tiered organizational structure.
The first tier was the National Headquarters, which is made up of permanent Ministry of Health staff who are charged with: (1) national and regional operational and financial oversight; (2) policy formation; (3) monitoring and evaluation; (4) purchasing and procurement;(5) human resource development;(6) training and education; (7) management of information systems; and (8) research (Figure 1). Each region has a coordinator, usually a medical officer (ie, medical doctor without specialist training), who liaises between the Regional Health Service (Accra, Ghana), National Fire Service, and Headquarters. In addition, the Regional Medical Coordinator provides medical oversight and supports station operations to ensure quality service delivery. The operational level is the individual station. The EMTs work under a lead EMT and in close collaboration with the District Fire Officers, since they often share infrastructure (eg, station facilities).
Figure 1.
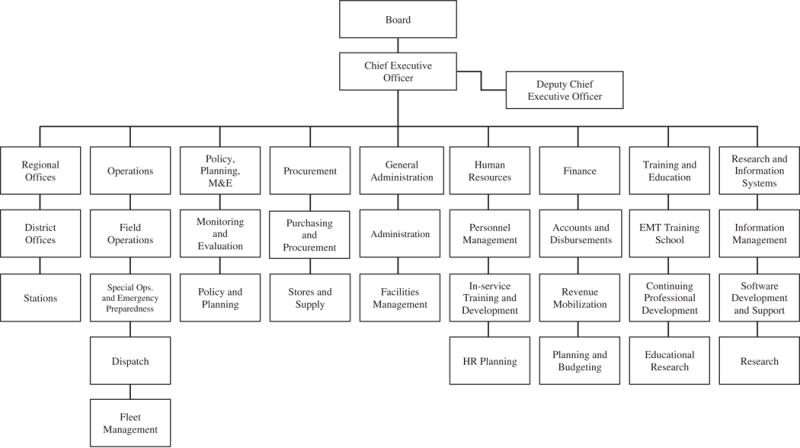
Ghana National Ambulance Service Organogram.
Abbreviations: EMT, emergency medical technician; HR, human resources; M&E, monitoring and evaluation; Ops, operations.
Initially, two control rooms, located in the two most populous cities, responded to calls on the emergency access telephone line and dispatched ambulances from individual stations as appropriate. To meet increasing demand, the NAS has expanded to nine control rooms around the country. This multi-tiered structure has allowed the NAS to grow rapidly while maintaining quality control mechanisms at both the operation level (ie, stations) and within the organization as a whole.
Infrastructure Development
In 2004, the NAS piloted operations with 69 newly trained EMTs, nine ambulances, and seven stations. After the pilot phase demonstrated operational success, the number of EMTs, ambulances, stations, and employees nearly were tripled (Table 1). Save the training of more EMTs, this level of input was maintained until 2012. During the same year, the government was able to increase funding for the NAS, which allowed development of a stand-alone EMT training program, purchase of 100 ambulances, and creation of 97 additional stations. The EMT school used a curriculum that was co-developed by EMT instructors from the North Dakota Army National Guard (Bismarck, North Dakota USA) and experts within the NAS; the curriculum was based on the principles of Basic Life Support, Prehospital Trauma Life Support (PHTLS), and other fundamental prehospital care topics (eg, recognition and care of medical and obstetric emergencies, as well as emergency medical systems operations). The curriculum prepares trainees for the cognitive and psychomotor exams offered for EMT certification by the United States National Registry of Emergency Medical Technicians (NREMT; Columbus, Ohio USA). Additionally, the NAS established continuous professional development education opportunities that allowed EMTs to advance their accreditations from basic EMT to advanced EMT. In 2008, there were no advanced EMTs. Currently, the ratio of advanced to basic EMTs is one to eight, respectively. Since the EMT training school’s formation, nearly 2,000 EMTs have been trained.
Table 1.
Infrastructure and Capacity of the National Ambulance Service in Ghana from 2004 through 2014
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| National Population (millions) | 20.8 | 21.4 | 22.0 | 22.5 | 23.1 | 23.7 | 24.3 | 24.9 | 25.6 | 26.2 | 26.8 |
| Number of EMTs | 69 | 66 | 176 | 228 | 221 | 220 | 220 | 202 | 673 | 911 | 1,651 |
| Number of Ambulances | 9 | 9 | 37 | 37 | 37 | 37 | 38 | 99 | 199 | 199 | 199 |
| Number of Stations | 7 | 7 | 24 | 24 | 24 | 24 | 24 | 24 | 121 | 122 | 128 |
| Total Employees | 69 | 71 | 182 | 232 | 225 | 230 | 228 | 228 | 700 | 956 | 1,698 |
Abbreviation: EMT, emergency medical technician.
Rapid station expansion in 2012 relied on use of existing infrastructure, such as fire stations, municipal buildings, and district hospitals. However, given space constraints at fire stations and the need to be proximate to hospitals, stand-alone and hospital-based stations were developed preferentially.
To oversee and maintain effective operations with this level of input, the NAS required an additional 27 administrative and maintenance employees. However, this still was not sufficient. The EMTs and staff were working excessive hours; coordination and ambulance and station maintenance were lacking. In 2012, the demand for EMTs was great enough to open a formal and self-sustaining EMT school.
Therefore, the NAS continued to train EMTs and recruit staff to meet the demands (1,698 total employees in 2014). As a result of these efforts, the percent of the country’s land covered by the NAS has increased from nine percent in 2004 to 33% in 2008 to 81% in 2014 (Figure 2). Additionally, these changes have improved EMT work hours. The EMTs currently work two 12-hour day shifts, two 12-hour night shifts, and then have two days off.
Figure 2.
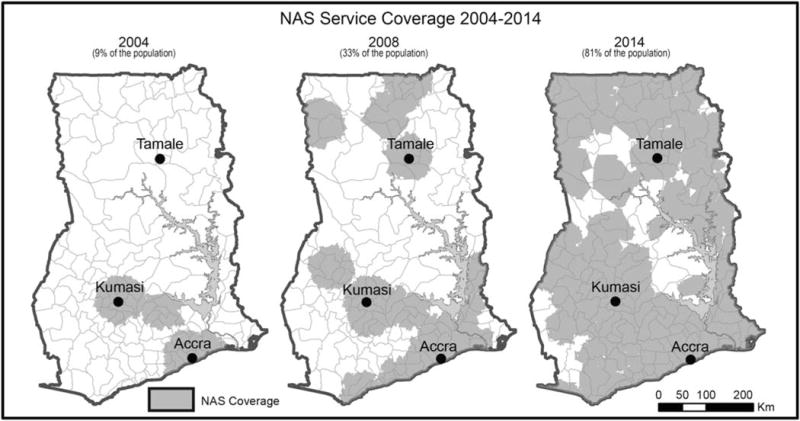
Map of the Expansion of Service Range by the National Ambulance Service in Ghana from 2004 through 2014.
Services Provided
The number of responses increased from 205 in 2004 to 1,598 in 2005 without a change in inputs (eg, EMTs, ambulances, or stations; Table 2). Instead, public and health care provider promotion of the emergency access telephone number and NAS services through television and radio shows and direct-to-provider advertising (eg, hospital visits and brochures) increased demand. After 2006, the number of responses relatively was constant and constrained by the number of staff, ambulances, and stations. With the addition of the inputs described above in 2012, the number of responses more than doubled: 7,810 in 2012; 17,204 in 2013; and 20,236 in 2014.
Table 2.
Characteristics of Patients Cared for by the National Ambulance Service in Ghana from 2004 through 2014
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
| Total Patients | 205 | 1,498 | 4,442 | 7,995 | 8,114 | 6,368 | 5,232 | 4,760 | 7,810 | 17,204 | 20,236 |
| Age | |||||||||||
| < 1 year | 0 (0) | 20 (1) | 560 (13) | 380 (5) | 253 (3) | 545 (9) | 245 (5) | 342 (7) | 390 (5) | 1,000 (6) | 1,826 (9) |
| 1–14 years | 0 (0) | 99 (7) | 457 (10) | 434 (5) | 348 (4) | 678 (11) | 515 (10) | 395 (8) | 139 (2) | 1,149 (7) | 1,681 (8) |
| 15–20 years | 140 (68) | 480 (32) | 777 (17) | 1,754 (22) | 1,235 (15) | 1,009 (16) | 437 (8) | 986 (21) | 2,025 (26) | 2,361 (14) | 11,775 (58) |
| 21–55 years | 65 (32) | 612 (41) | 1,998 (45) | 4,676 (58) | 5,010 (62) | 3,149 (49) | 3,067 (59) | 2,150 (45) | 4,531 (58) | 7,600 (44) | 2,515 (12) |
| ≥ 56 years | 0 (0) | 287 (19) | 650 (15) | 751 (9) | 1,268 (16) | 987 (15) | 968 (19) | 887 (19) | 725 (9) | 5,094 (30) | 2,439 (12) |
| Sex | |||||||||||
| Male | 99 (48) | 489 (33) | 2,230 (50) | 4,478 (56) | 4,597 (57) | 2,258 (35) | 2,498 (48) | 2,384 (50) | 3,782 (48) | 8,072 (47) | 9,201 (45) |
| Female | 106 (52) | 1,009 (67) | 2,212 (50) | 3,517 (44) | 3,517 (43) | 4,110 (65) | 2,734 (52) | 2,376 (50) | 4,028 (52) | 9,132 (53) | 11,035 (55) |
| Condition | |||||||||||
| Medical | 205 (100) | 887 (59) | 1,283 (29) | 5,234 (65) | 4,589 (57) | 2,989 (47) | 3,000 (57) | 2,870 (60) | 3,798 (49) | 6,345 (37) | 8,802 (43) |
| Trauma | 0 (0) | 611 (41) | 1,363 (31) | 1,332 (17) | 1,734 (21) | 1,564 (25) | 573 (11) | 1,560 (33) | 1,320 (17) | 4,562 (27) | 5,639 (28) |
| Obstetric | 0 (0) | 0 (0) | 920 (21) | 895 (11) | 1,000 (12) | 1,345 (21) | 1,028 (20) | 200 (4) | 1,123 (14) | 4,577 (27) | 4,877 (24) |
| Investigation a | 0 (0) | 0 (0) | 876 (20) | 534 (7) | 791 (10) | 470 (7) | 631 (12) | 130 (3) | 1,569 (20) | 1,720 (10) | 918 (5) |
Transfer refers to referral from one health care facility to another for the purpose of obtaining diagnostic evaluation that is not available at the initiating facility or escalation of care.
The majority of patients cared for by the NAS were between 15 and 55 years of age (58%–84% by year after 2006; Table 2). However, older adults (ie, those >55 years of age) comprised between nine percent and 30% of responses, and infants (ie, children less than one year of age) accounted for five percent to 13% of responses by year since 2006. Most responses were to health care facilities for inter-hospital transfer (43%–80% by year), followed by the roadside (10%–57% by year; Figure 3). Although the numbers of scene responses (eg, residences, schools, and places of work) have increased, the majority of responses were to health care facilities for all years except 2004.
Figure 3.
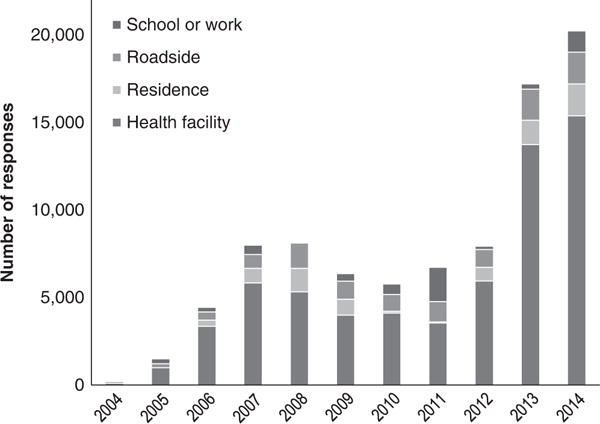
Number and Location of Responses by the National Ambulance Service in Ghana from 2004 through 2014.
Note: Health facility refers to inter-hospital transfer for referral or diagnostic evaluation.
Despite an increase in the absolute number of NAS responses, utilization remained relatively constant: 0.3 responses per ambulance per day in 2006; 0.5 in 2009; and 0.3 in 2014 (not tabled). However, the responses per day per 100,000 population increased across the study period consistent with NAS growth: 0.06 in 2006; 0.07 in 2009; and 0.21 in 2014 (not tabled).
Monitoring and Evaluation System
Response, case holding, and vehicle engaged times have been monitored by the NAS since the pilot phase for monitoring and evaluation of efficiency, quality, and coverage. In the pilot phase, mean response time was 13.1 minutes (SD = 0.18) and mean vehicle was engaged was 200.4 minutes (SD = 0.31; Table 3). Response times generally increased to 19.5 minutes in 2014 (SD = 0.02). This was related, in part, to the greater uptake of the single-access emergency telephone number by individuals and health care facilities, leading to greater travel distances. Nonetheless, gains in efficiency were evidenced by a 10% decrease in the vehicle engaged time to 180.3 minutes (SD = 0.32) in 2014.
Table 3.
Indicator Times for the National Ambulance Service in Ghana from 2004 through 2014
| 2005a | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
|---|---|---|---|---|---|---|---|---|---|---|
| mean (SD) | mean (SD) | mean (SD) | mean (SD) | mean (SD) | mean (SD) | mean (SD) | mean (SD) | mean (SD) | mean (SD) | |
| Run Time (min) | ||||||||||
| Response Time b | 13.1 (0.18) | 13.2 (0) | 12.6 (0.01) | 12.5 (0.02) | 20.0 (0.04) | 17.4 (0.04) | 18.7 (0.20) | 17.1 (0.02) | 17.4 (0.05) | 19.5 (0.02) |
| Case Holding Time c | 20.2 (0.04) | 18.6 (0) | 21.0 (0.03) | 13.5 (0.03) | 17.7 (0.50) | 15.5 (0.04) | 18.6 (0.04) | 17.0 (0.10) | 18.3 (0.01) | 20.3 (0.03) |
| Vehicle Engaged Time d | 200.4 (0.31) | 203.1 (0) | 164.8 (0.24) | 128.0 (0.34) | 155.8 (0.20) | 178.8 (0.23) | 178.8 (0.05) | 188.1 (0.04) | 185.4 (0.13) | 180.3 (0.32) |
Data from 2004 were not available for inclusion.
Response time – time from call received to arrival at the scene/facility.
Case holding time – time from arrival at the scene/facility to leaving scene/facility with patient.
Vehicle engaged time – total time that vehicle is used for a single response.
The above results highlight specific examples and challenges related to the growth of the NAS. Table 4 presents a synthesis of past, current, and future directions of the NAS more generally for each of the 14 components of an ambulance service.23
Table 4.
Evolution and Future Directions of the NAS in Ghana since 2004
| EMS Component | Past and Present | Future |
|---|---|---|
| Integration of Health Services | Ad hoc transfer of patients to nearest facility; limited communication with facility regarding incoming patients. | Selective transfer to capable health facilities based on patient acuity; standardize communication to receiving facilities regarding incoming patients; integrate the care of seriously ill and injured persons with the new emergency medicine training programs. |
| EMS Research | Capacity assessment and advocacy research; establishment and staffing of a research department. | Defining access to care gaps; identifying ways to improve NAS service uptake; supporting the research department efforts to improve NAS care and EMS care in LMICs more broadly. |
| Legislation and Regulation | NAS Bill drafted and proposed to Parliament. | Ratification of NAS Bill, which will increase NAS scope from service delivery to regulation of all ambulances services nationwide. |
| System Finance | Inconsistent/insufficient funding, namely the result of delay in NAS Bill ratification. | Dedicated funding after ratification of NAS Bill. |
| Human Resources | Reliance on cross-trained staff with National Fire Service; steady expansion of EMT pool after opening EMT school. | Keep pace with demand; strategic increase in numbers of EMT-As to provide more advanced care during transport. |
| Medical Direction | Regional medical coordination; insufficient funds and expertise to finance local medical direction. | Provide medical direction at the sub-regional level; performance evaluation; develop a pool of emergency medicine physicians in prehospital care management. |
| Education Systems | Combined education with National Fire Service; opening of EMT school. | Provide continuing education for EMTs and medical directors. |
| Public Education | Television and radio shows regarding NAS services and potential benefits of prehospital care. | Community-based first aid and prehospital care promotion campaigns. |
| Prevention | Television and radio shows regarding ways to prevent injury. | Join efforts with other national and non-governmental organizations that participate in injury and disease prevention initiatives. |
| Public Access | Multiple emergency access telephone numbers for: NAS, National Fire Service, and Police Service; creation of public relations department. | Single emergency access telephone number for all safety and security services. |
| Communication Systems | Telephone-based sub-national communication system for dispatch; toll-free access telephone numbers now recognized by all mobile communication service providers. | Single shared call center for all national safety and security services; standardize communication regarding incoming patients between ambulances and hospitals. |
| Clinical Care | Single level of EMT was expanded to basic and advanced levels. | Increase availability of resources in the ambulance to maximize capabilities of EMTs; performance monitoring and evaluation. |
| Information Systems | Data were compiled with Excel and analyzed manually each month; access-based system now used with built-in macros for automatic analysis; station-level pretabulated data are sent to NAS Headquarters for evaluation. | Develop infrastructure for cloud-based, real-time data collection and reporting; GIS data collection and management to identify “hot spots” and population-based geospatial access gaps. |
| Evaluation | Time and efficiency indicators have been monitored since NAS inception; station locations, staffing requirements, and performance audits have been proposed using these data. | Add indicators for staff performance and patient outcome; telephone-based random assessment of quality of services provided from patients’ perspectives. |
Abbreviations: EMS, Emergency Medical Service; EMT, emergency medical technician; EMT-A, EMT Advanced; GIS, geographic information system; NAS, National Ambulance Service.
Discussion
This report documents the growth of the NAS in the first decade of operations in Ghana. Since completion of the pilot phase in 2006, the NAS has refined an effective organizational and oversight structure, developed an EMT training school, increased its number of responses four-fold, and maintained an active monitoring and evaluation system. However, several challenges remain and require innovative strategies and sustained efforts addressing them moving forward.
Other LMIC Successful Ambulance Systems
Ambulance services can significantly reduce morbidity and mortality of patients with emergency conditions.24 However, few LMICs have developed and implemented a formal prehospital care system due to lack of political will, sufficient capital, local advocacy, and/or strategic planning.25 Another example of a successful prehospital care model in a LMIC is the Green Cross ambulance service in Monterey, Mexico.4 This was a small ambulance service in the mid-1990s with only two stations and medics with limited training. In response to the significant unmet emergency care need with the ambulance service structure at the time, the Green Cross increased the number of stations to four and strategically placed them around the city to minimize response times in 1997. Around the same time, Spanish-language PHTLS was provided semi-annually to all of the Green Cross medics. A subsequent analysis of these improvements demonstrated that the response time nearly halved. Further, successful use of spinal immobilization, airway rescue maneuvers, and fluid resuscitation increased and prehospital mortality decreased from 10% to seven percent.4 The cost of doubling of the number of stations and providing semi-annual PHTLS training to medics was US$75,000 and US$77,600, respectively. These significant improvements only accounted for 16% of the Green Cross annual budget, despite more than doubling its capabilities. Similar improvements in LMIC prehospital care services have been reported in Trinidad and Pakistan.26,27
Several challenges encountered from the Rescue 1122, the Pakistan government-run fire, rescue, disaster response, and ambulance service, are particularly informative. Rescue 1122 relied on local manufacturing benchmarked by international standards for building their ambulance fleet, saving an estimated US$25.6 million on import costs.27 To avoid the capital costs required to create a de novo training platform, they used the Elite Police Training School (Lahore, Pakistan) until they were able to secure infrastructure for a permanent training facility. Additionally, Rescue 1122 constructed ambulance stations based on response times rather than target populations, allowing more people to be served with fewer resources. This is a useful model for many LMICs with poor road infrastructure, significant traffic congestion in urban and peri-urban areas, and limited respect for emergency sirens. Importantly, all of the services ran by Rescue 1122 (ie, fire, rescue, disaster response, and ambulance) were supervised by a single command structure to avoid confusion among response teams during mass causality or disaster situations when communication breakdown is a significant potentiality. Lastly, critical incident reviews and response times were used to monitor and evaluate the effect of program interventions and its growth. These lessons can be condensed: develop within the local context; build on existing infrastructure; and systematically monitor and evaluate the system to inform quality or efficiency improvement initiatives.
Ghana NAS Building on Existing Infrastructure
Similar to the Green Cross and Rescue 1122, the lack of qualified EMTs to fill open positions in the rapidly growing ambulance service was a significant challenge. Prior to NAS creation, there was not an EMT training program in the country. For the pilot program, Fire Service members were recruited and trained as EMTs jointly by the Ministry of Health and the National Fire Service. As the NAS and demand for specialized EMTs grew, the Ministry of Health took over recruiting and training from an open applicant pool, though still using National Fire Service facilities. Opening of the stand-alone EMT training school in 2012 significantly increased the number of qualified EMTs and allowed simultaneous expansion in the number of ambulances and stations to better meet the population’s prehospital care demand. In countries without formal EMT training programs, this staged approach and reliance on existing infrastructure may be a useful strategy while plans for training capacity improvements take shape.
Ghana NAS Monitoring and Evaluation
Having learned lessons from previous attempts at developing local or regional ambulance services in Ghana, the NAS was committed to routinely collect, collate, and examine data to monitor and evaluate operational efficiency and the quality of care provided. For each run, EMTs record data that capture the nature of the call (ie, simple demographics, location of scene, and reason for call), care provided, and destination. Indicator times were added in 2005. Station supervisors and Headquarters staff habitually review these data. This database allows monitoring of trends in service utilization and identification of outlier stations that are in need of quality improvement or that are models of successful operations. By doing so, the NAS can better plan training and expansion priorities and adapt services to changing demands. As an example of database use to target priorities for NAS expansion, it was noticed that improvements in mean response and case holding times from 2006 through 2008 were stalled in 2009. After focused discussions with station and Regional Medical Coordinators, it was realized that the rate-limiting factor for improving response times was the number of vehicles currently in operation. With these data, the NAS was able to lobby the Government of Ghana for funds to expand their fleet. At the end of 2012, 100 vehicles were purchased. Resultantly, the number of cases responded to more than doubled in less than one year.
Remaining Challenges and Opportunities for Improved Service Delivery
Despite increases in prehospital capacity, NAS utilization has remained relatively low (0.3 responses per ambulance per day in 2014). For comparison, estimates from other countries, regardless of national income, range from two to 20 responses per ambulance per day varying by rural/urban locale and funding mechanism.28–31 These figures are difficult to compare directly since the NAS utilization rate includes all ambulances, regardless of functionality, and published rates may only include functional ambulances “on duty.” To give a gross estimate of unmet prehospital care need, the number of responses per day per 100,000 population range from 6.0 in Shenzhan, China to 46.7 in New South Wales, Australia, compared to 0.2 in Ghana.32,33 Some possible explanations for low NAS utilization rates and/or significant unmet prehospital care need include: prohibitively expensive health care costs that prevent patient transfers;19 insufficient knowledge of the role of the NAS or emergency access telephone number among the population; frequent need for vehicle servicing and/or repair; and population growth that is exceeding NAS expansion.
Similar to other LMIC prehospital services, the greatest challenge faced by NAS remains insufficient funding to meet the prehospital care needs of the growing population.25 Although the NAS Bill allowed creation the NAS in 2004, it has not been ratified by Parliament. Thus, the funding scheme is ad hoc, namely from remaining Ministry of Health funds. With ratification, two significant changes will occur: (1) dedicated and planned funding for NAS activities; and (2) a regulatory mandate for the NAS to supervise, standardize, and coordinate all ambulance services nationwide.
Emergency Medicine recently has become an accredited specialty in Ghana.34 Two hospitals have Emergency Medicine training programs, one in the south and one in the north. These institutions are important stakeholders in the development of the NAS, particularly with regard to developing protocols aimed at improving the rate at which critically ill or injured patients receive necessary care (eg, destination triage and pre-arrival instructions). Additionally, graduates of these programs who complete fellowships in prehospital/disaster medicine will be important partners in the research the NAS undertakes, as well as its medical direction.
There are several externalities that challenge efficient NAS operations. These include: frequent false alarms and inappropriate inter-hospital transfers;35 lack of street names and house numbers; disrespect of sirens by motorists; and occasional health care facility refusal of emergency cases. While the NAS has attempted to sensitize both the population and health care facility staff, more progress must be made to mitigate some of the aforementioned challenges.
Conclusion
Despite the challenges faced, the steady growth and uptake of NAS services is evidence of both the significant need for Emergency Medical Services and sound operational and financial planning. Several of the challenges faced and solutions employed to overcome them are particularly useful, such as: creating an organizational structure that easily permits information exchange from stations to Headquarters and maintains constant administrative and medical oversight; identifying the need for an EMT training school and systematically escalating educational resources to meet the growing demand; and making routine data collection, monitoring, and evaluation a routine part of daily operations. Notwithstanding duteous effort by the NAS, all of the aforementioned activities have been made possible by sustained political commitment, which will be made concrete by the ratification of the NAS Bill.
Abbreviations
- EMT
emergency medical technician
- LMICs
low- and middle-income countries
- NAS
National Ambulance Service
- PHTLS
Prehospital Trauma Life Support
Footnotes
Conflicts of interest: none
References
- 1.Lozano R, Naghavi M, Foreman K, et al. Global and regional mortality from 235 causes of death for20 age groups in 1990 and2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095–2128. doi: 10.1016/S0140-6736(12)61728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stewart B, Khanduri P, McCord C, et al. Global disease burden of conditions requiring emergency surgery. Br J Surg. 2014;101(1):e9–22. doi: 10.1002/bjs.9329. [DOI] [PubMed] [Google Scholar]
- 3.Mock CN, Donkor P, Gawande A, Jamison DT, Kruk ME, Debas HT. Essential surgery: key messages from Disease Control Priorities. Lancet. (3rd) 2015;385(9983):2209–2219. doi: 10.1016/S0140-6736(15)60091-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Arreola-Risa C, Mock CN, Lojero-Wheatly L, et al. Low-cost improvements in prehospital trauma care in a Latin American city. J Trauma. 2000;48(1):119–124. doi: 10.1097/00005373-200001000-00020. [DOI] [PubMed] [Google Scholar]
- 5.Forjuoh S, Mock C, Freidman D. Transport of the injured to hospitals in Ghana: the need to strengthen the practice of trauma care. Prehosp Immediate Care. 1999;3:66–70. [Google Scholar]
- 6.Mock CN, Tiska M, Adu-Ampofo M, Boakye G. Improvements in prehospital trauma care in an African country with no formal EMS. J Trauma. 2002;53(1):90–97. doi: 10.1097/00005373-200207000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Tiska MA, Adu-Ampofo M, Boakye G, Tuuli L, Mock CN. A model of prehospital trauma training for lay persons devised in Africa. Emerg Med J. 2004;21(2):237–239. doi: 10.1136/emj.2002.002097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mock C, Jurkovich G, nii-Amon-Kotei D. Trauma mortality patterns in three nations at different economic levels: implications for global trauma system development. J Trauma. 1998;44(5):804–814. doi: 10.1097/00005373-199805000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Quansah R, Mock C, Abantanga F. Status of trauma care in Ghana. Ghana Med J. 2004;38:149–152. [Google Scholar]
- 10.Crandon IW, Harding HE, Williams EW, Cawich SO. Inter-hospital transfer of trauma patients in a developing country: prospective descriptive study. Int J Sur. 2008;6(5):387–391. doi: 10.1016/j.ijsu.2008.07.004. [DOI] [PubMed] [Google Scholar]
- 11.Mock C, Juillard C, Joshipura M, Goosen J. Strengthening Care for the Injured: Success Stories and Lessons Learned from Around the World. Geneva, Switzerland: World Health Organization; 2010. [Google Scholar]
- 12.United States Central Intelligence Agency. CIA World Factbook. 2014 http://www.ciaworldfactbook.us/africa/ghana.html. Accessed April 12, 2015.
- 13.World Bank Group. Ghana. 2015 http://data.worldbank.org/country/ghana. Accessed January 14, 2015.
- 14.Institute of Health Metrics and Evaluation. Data Visualizations: Global Burden of Disease Cause Patterns. http://vizhub.healthdata.org/gbd-cause-patterns/. AccessedMay 27, 2015.
- 15.World Bank Group. United Kingdom and Great Britain. 2014 http://www.worldbank.org/en/country. Accessed May 6, 2015.
- 16.Stewart BT, Quansah R, Gyedu A, et al. Serial assessment of trauma care capacity in Ghana in 2004 and 2014. JAMA Surg. 2016;151(2):164–171. doi: 10.1001/jamasurg.2015.3648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rominski S, Bell SA, Yeboah D, Sarna K, Hartney H, Oteng R. Skills and educational needs of accident and emergency nurses in Ghana: an initial needs analysis. African J Emerg Med. 2011;1(3):119–125. doi: 10.1016/j.afjem.2011.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ankomah J, Stewart BT, Oppong-Nketia V, et al. Strategic assessment of the availability of pediatric trauma care equipment, technology, and supplies in Ghana. J Pediatr Surg. 2015;50(11):1922–1927. doi: 10.1016/j.jpedsurg.2015.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stewart BT, Quansah R, Gyedu A, Ankomah J, Donkor P, Mock C. Strategic assessment of trauma care capacity in Ghana. World J Surg. 2015;39(10):2428–2440. doi: 10.1007/s00268-015-3132-3. [DOI] [PubMed] [Google Scholar]
- 20.Japiong KB, Asiamah G, Owusu-Dabo E, et al. Availability of resources for emergency care at second-level hospital in Ghana: a mixed methods assessment. African J Emerg Med. 2016;6(1):30–37. doi: 10.1016/j.afjem.2015.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mock C, Abantanga F, Goosen J, Joshipura M, Juillard C. Strengthening care of injured children globally. Bull World Health Organ. 2009;87(5):382–389. doi: 10.2471/BLT.08.057059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.National Ambulance Service. Accra: Ghana Ministry of Health; 2009. [Google Scholar]
- 23.National Transportation Safety Administration. Emergency Medical Systems: Agenda for the Future. Washington, DC USA: US National Transportation Safety Administration; 1996. [Google Scholar]
- 24.Ryynanen OP, Iirola T, Reitala J, Palve H, Malmivaara A. Is Advanced Life Support better than Basic Life Support in prehospital care? A systematic review. Scand J Trauma Resusc Emerg Med. 2010;18:62. doi: 10.1186/1757-7241-18-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Razzak JA, Kellermann AL. Emergency medical care in developing countries: is it worthwhile? Bull World Health Organ. 2002;80(11):900–905. [PMC free article] [PubMed] [Google Scholar]
- 26.Ali J, Adam RU, Gana TJ, Bedaysie H, Williams JI. Effect of the Prehospital Trauma Life Support (PHTLS) program on prehospital trauma care. J Trauma. 1997;42(5):786–790. doi: 10.1097/00005373-199705000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Waseem H, Naseer R, Razzak JA. Establishing a successful prehospital emergency service in a developing country: experience from Rescue 1122 service in Pakistan. Emerg Med J. 2011;28(6):513–515. doi: 10.1136/emj.2010.096271. [DOI] [PubMed] [Google Scholar]
- 28.Kobusingye OC, Hyder AA, Bishai D, Joshipura M, Hicks ER, Mock C. EMS: Disease Control Priorities in Developing Countries. Washington, DCUSA: World Bank, Group; 2006. [Google Scholar]
- 29.Prinja S, Bahuguna P, Lakshmi PV, et al. Evaluation of publicly financed and privately delivered model of emergency referral services for maternal and child health care in India. PLoS One. 2014;9(10):e109911. doi: 10.1371/journal.pone.0109911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cowell J. Review of Operations of Ground Emergency Medical Services in Alberta. Alberta, Canada: Health Care Quality Council of Alberta; 2013. [Google Scholar]
- 31.Terzi O, Sisman A, Canbaz S, Dundar C, Peksen Y. A geographic information system-based analysis of ambulance station coverage area in Samsun, Turkey. Singapore Med J. 2013;54(11):653–658. doi: 10.11622/smedj.2013228. [DOI] [PubMed] [Google Scholar]
- 32.Man Lo S, Min Yu Y, Larry Lee LY, et al. Overview of the Shenzhen Emergency Medical Service call pattern. World J Emerg Med. 2012;3(4):251–256. doi: 10.5847/wjem.j.issn.1920-8642.2012.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.New South Wales Government. Ambulance services of New South Wales; Australia: 2014. http://www.nsw.gov.au. Accessed June 22, 2015. [Google Scholar]
- 34.Martel J, Oteng R, Mould-Millman NK, et al. The development of sustainable emergency care in Ghana: physician, nursing, and prehospital care training initiatives. J Emerg Med. 2014;47(4):462–468. doi: 10.1016/j.jemermed.2014.04.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gyedu A, Baah EG, Boakye G, Ohene-Yeboah M, Otupiri E, Stewart BT. Quality of referrals for elective surgery at a tertiary care hospital in a developing country: an opportunity for improving timely access to and cost-effectiveness of surgical care. Int J Surg. 2015;15:74–78. doi: 10.1016/j.ijsu.2015.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]


