Abstract
A 56-year old male with ischemic heart disease and an unremarkable preoperative echocardiogram underwent surgical coronary revascularization. An intraoperative post pump trans-esophageal echocardiogram (TOE) performed while the patient was being ventilated at a positive end expiratory pressure (PEEP) of 8 cm H2O demonstrated a right to left interatrial shunt across a patent foramen ovale (PFO). Whereas oxygen saturation was normal, a reduction of the PEEP to 3 cm H2O led to the complete resolution of the shunt with no change in arterial blood gases. Attempts to increase the PEEP level above 3 mmHg resulted in recurrence of the interatrial shunt. The remaining of the TEE was unremarkable. Mechanical ventilation, particularly with PEEP, causes an increase in intrathoracic pressure. The resulting rise in right atrial pressure, mostly during inspiration, may unveil and pop open an unrecognized PFO, thus provoking a right to left shunt across a seemingly intact interatrial septum. This phenomenon increases the risk of paradoxical embolism and can lead to hypoxemia. The immediate management would be to adjust the ventilatory settings to a lower PEEP level. A routine search for a PFO should be performed in ventilated patients who undergo a TEE.
Key words: Mechanical ventilation, patent foramen ovale, positive end expiratory pressure, transesophageal echocardiography
Competing interest statement
Conflict of interest: the authors declare no conflict of interest.
Introduction
A patent foramen ovale is a very common finding in the normal population1 and can be the cause of cryptogenic strokes. Mechanical ventilation (MV), which is used in the 0.27% of the general population in developed countries,2 increases the intrathoracic and right atrial pressures3 and may promote a right to left shunt leading to a paradoxic brain embolism. Commonly transesophageal echo or transcranial doppler are used to detect a PFO.4 As a result of a diffuse anomaly and a common threatment, a large number of patients are at risk of a cryptogenic stroke during mechanical ventilation. Great attention should be paid to the detection of this potentially threatening condition whenever a TOE is performed in ventilated patient.
Case Report
A 56 yo male diabetic and hypertensive patient presented with an ACS and a triple vessel coronary disease at the coronary angiography. At the preopeative echocardiography his EF was 55% without regional wall motion anomalies (RWMA), the exam was otherwise unremarkable. After initial medical stabilization with intravenous nitrates, ß-blockers, aspirin and the infusion of un-fractioned heparin he underwent an uneventful on pump myocardial revascularization. At surgery the LIMA was harvested and the left pleura opened and drained. No inotropes were infused in the postoperative period. The patient was moved to the ICU and the ventilator setting were adjusted to maintain a PaO2 of 150 mmHg with a current volume of 10 mL/kg/min. A positive end expiratory pressure (PEEP) of 8 cmH2O was added to the circuit. At the first postoperative ECG minor changes on the lateral chest leads were noted and a transesophageal echocardiography was order to rule out possible new RWMA.
A complete examination was carried out. The LV function was normal as were the right ventricle, the right atrium and the tricuspid valve. When the middle oesophageal AV SAX view was obtained it showed a right to left intra-cardiac shunt persisting thorough the cardiac cycle through a 8 mm PFO (Figure 1A). The right atrial pressure (RAP) was 12 mmHg. A reduction of the intra-thoracic pressure was considered necessary and the PEEP gradually reduced until the shunt disappeared at a PEEP value of 3 cmH2O (Figure 1B) and a RAP of 8 mmHg. As and adjuvant measure to keep all the left sided pressures higher than the right, a minimal dose of Norepinephrine (NOE) was added to maintain a mean arterial pressure of 75 mmHg and increase the peripheral vascular resistences. A Swang Ganz catheter was not inserted as the clinical conditions were stable and the shunt absent. This setting did not change the PaO2 value and was maintained until the patient could be weaned from the ventilator on postop hr 10. The rest of the hospital stay was clinically unremarkable as was the release of high sensivity troponine. The patient was discharged home on postoperative day 6. A postoperative transthoracic echocardiography at rest did not show any residual shunt.
Figure 1.
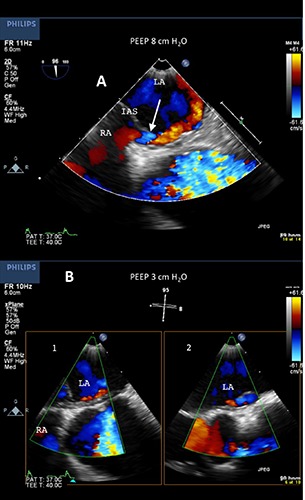
A) Mid-esophageal AV SAX view. The arrows points at the origin of the shunt. LA (left atrium); RA (right atrium); IAS (interatrial septum); B) Absence of shunt in inspiration (1) and expiration (2).
Discussion
A PFO is an anomalous communication between the right and the left atria at the level of the fossa ovalis. A PFO can be detected in 25% to 35% of normal individuals both at autopsy and in community-based TOE study.1 Commonly it is hemodynamically unrelevant because the left atrial pressure exceeds the RAP. A PFO becomes clinically relevant whenever the right atrial pressure outweigths the left as in right sided cardiac defects, physical efforts increasing the intra-thoracic pressure and in patients with pulmonary disease. A PFO is considered a common cause of stroke in otherwise normal patients. In the ICONS study (Identification of the Cause of Silent Cerebral Infarction in Healthy Subjects) 51% of the subjects with silent brain infarcts submitted to a transcranial doppler study had a right to left shunt detected.5
PEEP6 is a well known ventilatory setting aimed to recruit of alveolar space which is decreased after cardiopulmonary by pass. It is therefore routinely used after cardiac and thoracic surgery. By adding a controlled resistance at the end of the expiratory phase, PEEP increases the intra-thoracic pressure (IP) the Right Ventricle (RV) afterload and the RAP, whereas it decreases both the left ventricular preload and after-load and sets the conditions for a right to left shunt. These effects7 may become clinically evident in the usual range of 5 to 10 cmH2O. In the populations at risk some specialized ultrasound techniques such as bubble, contrast or transcranial Doppler studies are required to screen the patient at risk of stroke with right to left shunt.8
On the other hand TEE is now routinely used to monitor the cardiac function in the perioperative period after cardiac surgery. In a large survey investigating on the most commonly used techniques, more than 94% of the respondents indicated the TOE as the main or complimentary tool.9
PFOs detected in patient under mechanical ventilation have been reported as the cause of paradoxical hypoxemia with increasing levels of PEEP10,11 or to cause stroke in patient with pulmonary embolism.12
Although the observation of a right to left shunt at the level of a PFO has been incidental in our patient, the risk of stroke had to be considered as they occur in 2%13 of the general population undergoing coronary surgery. Many of them correlate well with known preoperative risk factors, yet a stroke can still occur in otherwise low-risk patients and many will remain cryptogenic.
Current guidelines14 on perioperative use of TEE give a detailed description of the technique and recommend a bubble or contrast study when searching for a stroke. However, a statement that a PFO should actively rouled out in ventilated patients is not included. On the contrary a weak recommendation for not routinely monitor the right heart with TOE in ARDS has been issued in 2014.15
The 2010 survey in the USA documented that 0.27%2 of the population or 2.8% of the hospitalized patients were under mechanical ventilation. As a consequence considering the incidence of a PFO in the general population, presumably about 1% of those patient are at risk of cryptogenic stroke.
In ventilated patients the TOE is superior to transthoracic echocardiography16 in visualizing PFOs. However, submitting to a TOE the entire immense cohort of ventilated patients is unpractical and probably impossible. Nevertheless it is our opinion that a recommendation for an active search of a PFO whenever a bedside TOE is performed, should be implemented.
In our patient the treatment for this potentially threatening condition consisted in a reduction of the PEEP and the IP until the shunt disappeared at a lower RAP. Notably the PaO2 did not change, probably because the reduction of the intracardiac shunt was balanced by an increase at the capillary level. The the addition of NOE together with a careful fluid management helped to maintain a normal diuresis and preserve the lung function.
In the remaining part of his hospital stay our patient remained stable and the PFO was investigated and not detected in the late postoperative period.
Conclusions
The use of PEEP is a standard practice after cardiac surgery to increase the functional residual capacity of the lung, recruit alveolar space and improve oxygenation. PEEP, which increases the RAP and the IP, can produce a right to left shunt and cause a perioperative stroke in patients with a PFO. As TOE has become a standard practice to monitor the cardiac function in cardiac surgery, a PFO should be always ruled out during mechanical ventilation. Conservative treatment of the PFO in this setting includes lowering the PEEP until the shunt disappears and a careful fluid and pharmacologic treatment aimed to increase the LAP.
References
- 1.Hagen P, Scholz D, Edwards W. Incidence and size of patent foramen ovale during the first 10 decades of life: An autopsy study of 965 normal hearts. Mayo Clin Proc 1984;59:17-20. [DOI] [PubMed] [Google Scholar]
- 2.Wush H, Linde-Zwirble WT, Angus DC, et al. The epidemiology of mechanical ventilation use in the United States Critic Care Med 2010;30:1947-53. [DOI] [PubMed] [Google Scholar]
- 3.Daoud E, Farag H, Chatburn R. Airway pressure release ventilation: What do we know? Respir Care 2012;57:282-92. [DOI] [PubMed] [Google Scholar]
- 4.Meissner I, Whisnant J, Khandheria B, et al. Prevalence of potential risk factors for stroke assessed by transesophageal echocardiography and carotid ultrasonography: the SPARC study. Stroke Prevention: Assessment of Risk in a Community. Mayo Clin Proc 1999;74: 862-69. [DOI] [PubMed] [Google Scholar]
- 5.Kim SJ, Shin HY, Ha YS, et al. Paradoxical embolism as a cause of silent brain infarctions in healthy subjects: the ICONS study (Identification of the Cause of Silent Cerebral Infarction in Healthy Subjects). Eur J Neurol 2013;20:353-60. [DOI] [PubMed] [Google Scholar]
- 6.Wild M, Alagesan K. PEEP and CPAP. Br J Anesth 2001;1:89-92. [Google Scholar]
- 7.Luecke T, Pelosi P. Clinical review: Positive end - expiratory pressure and cardiac output. Crit Care 2005;9:607-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tobe J, Bogiatzi C, Munoz C, et al. Transcranial Doppler is complementary to echocardiography for detection and risk stratification of patent foramen ovale. Can J Cardiol 2015. [Epub ahead of print]. [DOI] [PubMed]
- 9.Dobbs HA, Bennett-Guerrero E, White W, et al. Multinational institutional survey on patterns of intraoperative transesophageal echocardiography use in adult cardiac surgery. J Cardiothorac Vasc Anesth 2014;28:54-63. [DOI] [PubMed] [Google Scholar]
- 10.Cujec B, Polasek P, Mayers I, Johnson D. Positive end-expiratory pressure increases the right-to-left shunt in mechanically ventilated patients with patent foramen ovale. Ann Intern Med 1993;119:887-94. [DOI] [PubMed] [Google Scholar]
- 11.Mekontso Dessap A, Boissier F. Prevalence and prognosis of shunting across patent foramen ovale during acute respiratory distress syndrome. Crit Care Med 2010;38:1786-92. [DOI] [PubMed] [Google Scholar]
- 12.Granati GT, Teressa G. Worsening hypoxemia in the face of increasing PEEP: a case of large pulmonary embolism in the setting of intracardiac shunt. Am J Case Rep 2016;17:454-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stamou SG, Hill PC, Dangas G, et al. Stroke after coronary surgery. Incidence,predictors and clinical outcomes. Stroke 2001;32:1508-13. [DOI] [PubMed] [Google Scholar]
- 14.Practice guidelines for perioperative transesophageal echocardiography. An updated report by the American Society of Anestesiology and the Society of Cardiovascular Anesthesiologists task force on transesophageal echocardiography. Anesthesiology 2010;110:1-13. [DOI] [PubMed] [Google Scholar]
- 15.Morris CGT, Burn SA, Richard SB. Modern protective ventilation strategies: impact upon the right heart J Intens Care Soc 2014;15:28-33. [Google Scholar]
- 16.Silvestry FE, Cohen MS, Armsby LB, et al. Guidelines for the echocardiographic assessment of atrial septal defect and patent foramen ovale: from the American Society of Echocardiography and Society for Cardiac Angiography and Interventions. J Am Soc Echocardiogr 2015;28:910-58. [DOI] [PubMed] [Google Scholar]


